Abstract
Background
Although menopause is considered a risk factor for depression, no association has been established between the risk of suicidal ideation and age at menopause. This study aimed to evaluate the association between age at menopause and suicidal ideation in middle-aged menopausal Korean women.
Methods
This cross-sectional study used data from the Korea National Health and Nutrition Examination Survey (2013–2018). Women aged 40–65 years were divided into the following three categories: primary ovarian insufficiency (POI), early menopause, and menopause, according to age at natural menopause (< 40, 40–45, and > 45 years, respectively). Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9).
Results
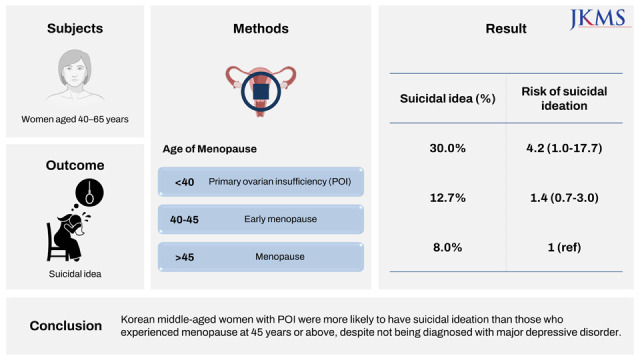
Among 2,232 menopausal women, 25 (1.1%) experienced POI and 114 (5.1%) experienced early menopause. The PHQ-9 items that pertained to low self-esteem and suicidal ideation scored higher in women with POI than in those who experienced menopause after 45 years of age. The prevalence of suicidal ideation differed significantly according to age at menopause (POI, 30.0%; early menopause, 12.7%; menopause, 8.0%; P = 0.016). Logistic regression analysis revealed that POI was significantly associated with suicidal ideation after the adjustment for age, body mass index, and education, household income, and walking levels (odds ratio, 4.2; 95% confidence interval, 1.0–17.7).
Conclusion
Korean middle-aged women with POI were more likely to have suicidal ideation than those who experienced menopause at 45 years or above, despite not being diagnosed with major depressive disorder.
Keywords: Age at Menopause, Depression, Primary Ovarian Insufficiency, Suicidal Ideation
Graphical Abstract
INTRODUCTION
Age at menopause is associated with the development of chronic conditions and multimorbidity in middle-aged postmenopausal women.1 In particular, primary ovarian insufficiency (POI), the cessation of menstruation along with loss of ovarian hormonal function and serum estrogen deficiency before the age of 40 years, are associated with impaired physical and mental health.2 POI is reportedly experienced by 1% of women.3 However, ethnic differences in its prevalence have been reported, and its prevalence in South Korea was relatively high (2.4–2.8%) in previous population-based studies.4,5 POI is reportedly associated with an increased risk of several chronic diseases, including diabetes, hypertension,2 osteoporosis,6 cardiovascular diseases,7 and psychosomatic disorders.8 Therefore, adequate attention and early screening for these complications are needed in women with POI.
Although an inverse association between age at menopause and the risk of subsequent depression has been reported,9 it remains unclear whether depressive symptoms including suicidal ideation are more prevalent in women with POI than in those who experience menopause after 45 years of age.10 Depressive symptoms are major causes of disability among middle-aged women11 and are associated with an increased risk of other chronic diseases.12,13 Suicide, possibly the most negative complication of depression, is a leading cause of death worldwide with a steadily increasing incidence in recent years.14 Thus, it is important that clinicians identify high-risk groups, particularly women with suicidal ideation, regardless of the diagnosis of depressive disorder.
This study aimed to investigate the association between age at menopause and select depressive behaviors, including suicidal ideation, among middle-aged Korean women using population-based data.
METHODS
Data collection and study participants
This study used data from the Korea National Health and Nutrition Examination Survey (KNHANES), a nationally representative cross-sectional population-based survey of health and nutritional status conducted by the Korea Centers for Disease Control and Prevention.15 This study used data from the sixth and seventh KNHANES (2013–2018), which consists of a personal health interview, socioeconomic status assessment, health examination, and nutrition survey conducted by trained investigators.
Among the respondents in this database, postmenopausal women aged ≥ 40 years and ≤ 65 years at the time of the interview were included in this study. The exclusion criteria were as follows: artificial menopause (history of hysterectomy and/or bilateral oophorectomy), history of malignant diseases or major depressive mood disorder, and failure to answer the Patient Health Questionnaire-9 (PHQ-9).
Menopausal status
Menopause was defined as the cessation of menstruation for more than 12 months. The survey was conducted through face-to-face interviews with trained staff of the KNHANES. Menopausal status was classified as POI, early menopause, and menopause according to the women’s self-reported age of natural menopause (< 40, 40–45, and > 45 years, respectively).3
PHQ-9 and suicidal ideation
Depressive symptoms were assessed quantitatively using the PHQ-9, a screening instrument for depressive symptoms with high sensitivity and specificity. The Korean version of the PHQ-9 was used in the survey; it has been used in various investigations in Korea and was validated in a previous study as having significant internal consistency (α = 0.86) with a test-retest reliability coefficient of 0.79.16 It consists of nine questions, each of which is scored 0 (“not at all”), 1 (“several days”), 2 (“more than half the days”), or 3 (“nearly every day”), resulting in a total score of 0–27.17 Suicidal ideation was evaluated based on the participants’ responses to the ninth question of the PHQ-9 (hereafter referred to as the “PHQ-9 suicide item”): “Over the last 2 weeks, how often have you been bothered by the following problem: thoughts that you would be better off dead, or of hurting yourself in some way?” If the PHQ-9 suicide item score was ≥ 1, we classified the participants as having suicidal ideation, and the threshold for the score of this item was suggested as 1.18
Socioeconomic status and other definitions
Participants completed surveys on their lifestyle and demographic factors, including smoking and drinking status, walking habits, and education level. Educational attainment was classified as lower than elementary school, middle school, high school, or college or higher. The KNHANES calculated the household income level based on the standardized classification by sex, residence, and 5-year age groups, and the value was compared with the standard income level of Korean citizens. The total household income was divided into quartiles (from lower to higher income).3 To assess whether the participants had a sedentary lifestyle or lack of physical exercise, we used the KNHANES item asking the number of days per week when they walked for more than 10 minutes. For the statistical analysis, we dichotomized this item as follows: walking ≥ 1 time per week for more than 10 minutes, or none.
Statistical analyses
The characteristics of the study population are described separately for each of the 3 groups according to age at menopause. One-way analysis of variance was used to compare differences in continuous variables among the 3 groups. The χ2 test was used to evaluate the independence of categorical variables. Logistic regression analysis of the relationship between age at menopause and suicidal ideation was performed using the group of women who experienced menopause after 45 years of age as reference. The binary dependent variable was defined as follows: suicidal ideation = 1; and no suicidal ideation = 0. Multivariable regression analysis was used to adjust for several confounding factors that showed statistical significance in this regression model or were clinically assumed as associated with both age at menopause and suicidal ideation, including age, body mass index (BMI), education level, household income level, and walking for more than 10 min at least once a week. Statistical significance was defined as a two-sided P value < 0.05. All analyses were performed using the Statistical Analysis System version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Ethics statement
The KNHANES was approved by the Ethics Committee of the Korea Centers for Disease Control and Prevention, and the study protocol was approved by the Institutional Review Board (IRB) of Korea University Anam Hospital (IRB No. 2020AN0124). The Korea Centers for Disease Control and Prevention obtained informed consent from all participants.
RESULTS
Among a total of 47,217 participants in the KNHANES 2013–2018, 2,232 Korean women aged 40–65 years who experienced natural menopause were included in the final analysis after the exclusion of those with a history of malignant diseases or major depressive disorder. Among the studied menopausal women, 25 (1.1%) experienced POI and 114 (5.1%) experienced early menopause. Baseline patient characteristics according to age at menopause are compared in Table 1. Women with POI were more likely obese and had a higher prevalence of diabetes and higher fasting glucose and triglyceride levels than those in the other groups. There were significant differences in parity, diastolic blood pressure, and education and walking levels between the 3 groups (Table 1).
Table 1. Baseline characteristics according to age at menopause among postmenopausal Korean women.
| Characteristics | Primary ovarian insufficiency (n = 25) | Early menopause (n = 114) | Menopause after 45 yr of age (n = 2,093) | P value | |
|---|---|---|---|---|---|
| Age at time of interview, yr | 57.40 ± 7.58 | 57.10 ± 6.55 | 58.10 ± 4.43 | 0.071 | |
| Parity ≥ 1 | 92.0 | 93.0 | 97.0 | 0.026 | |
| Married | 96.0 | 97.4 | 98.4 | 0.452 | |
| History of hypertension | 52.0 | 34.5 | 34.0 | 0.053 | |
| History of diabetes mellitus | 28.6a | 16.7 | 11.0 | 0.031 | |
| History of dyslipidemia | 12.5 | 19.1 | 22.6 | 0.694 | |
| History of oral contraceptive pill use | 16.0 | 21.1 | 18.4 | 0.732 | |
| BMI, kg/m2 | 25.8 ± 4.4 | 24.4 ± 3.6 | 23.9 ± 3.3 | 0.005 | |
| Waist circumference, cm | 87.3 ± 11.3 | 81.4 ± 9.5 | 80.1 ± 8.8 | < 0.001 | |
| Systolic BP, mmHg | 126.6 ± 19.7 | 118.6 ± 18.5 | 120.4 ± 17.4 | 0.116 | |
| Diastolic BP, mmHg | 77.8 ± 10.7 | 73.7 ± 9.4 | 76.2 ± 9.6 | 0.018 | |
| Fasting glucose, mg/dL | 116.4 ± 41.9 | 107.2 ± 35.2 | 100.5 ± 20.4 | < 0.001 | |
| TC, mg/dL | 195.5 ± 39.6 | 198.0 ± 34.1 | 203.2 ± 37.8 | 0.240 | |
| HDL-C, mg/dL | 55.1 ± 18.2 | 52.9 ± 11.5 | 53.9 ± 12.1 | 0.650 | |
| LDL-C, mg/dL | 105.9 ± 27.9 | 117.7 ± 37.8 | 120.4 ± 34.4 | 0.528 | |
| TG, mg/dL | 167.9 ± 92.5 | 125.6 ± 67.4 | 124.9 ± 78.1 | 0.027 | |
| Education level | 0.029 | ||||
| Elementary school or lower | 56.0 | 32.5 | 26.8 | ||
| Middle or high school | 36.0 | 49.1 | 55.3 | ||
| College or higher | 8.0 | 18.4 | 17.9 | ||
| Income level (quartile) | 0.103 | ||||
| Low | 32.0 | 27.2 | 23.2 | ||
| Lower-middle | 44.0 | 26.3 | 24.5 | ||
| Upper-middle | 12.0 | 25.4 | 25.6 | ||
| High | 12.0 | 21.1 | 26.8 | ||
| Carbohydrate intake | 262.6 ± 105.1 | 271.0 ± 128.3 | 287.7 ± 123.6 | 0.269 | |
| Fat intake | 28.7 ± 22.9 | 32.5 ± 23.6 | 33.6 ± 22.7 | 0.527 | |
| Walking more than 10 min (≥ 1 time/week) | 76.0 | 69.3 | 83.8 | 0.002 | |
Data are expressed as mean ± standard deviation or % as appropriate. Statistical comparisons were conducted using one-way analysis of variance for continuous variables and Pearson’s χ2 test for categorical variables.
BMI = body mass index, BP = blood pressure, HDL-C = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, TC = total cholesterol, TG = triglycerides.
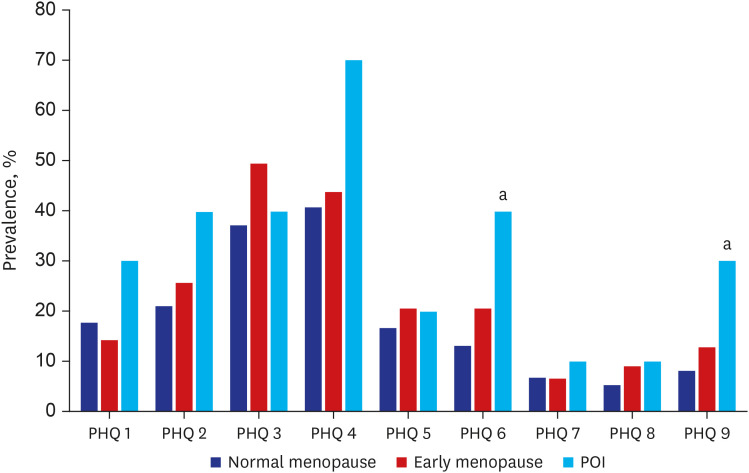
The mean scores for each PHQ-9 item according to age at menopause are compared in Table 2. The mean scores of items 9 (PHQ-9 suicide item) and 6 (PHQ-9 self-esteem item) were significantly different among the 3 groups, while the results of the other items generally showed a high score in the POI group. Fig. 1 compares the prevalence of each symptom among the 3 groups after converting these items to binary values (presence or absence).
Table 2. PHQ-9 scores according to age at menopause among postmenopausal Korean women.
| Characteristics | Primary ovarian insufficiency (n = 25) | Early menopause (n = 114) | Menopause after the age of 45 yr (n = 2,093) | P value |
|---|---|---|---|---|
| 1. Little interest or pleasure in doing things? | 0.3 ± 0.5 | 0.1 ± 0.4 | 0.2 ± 0.4 | 0.424 |
| 2. Feeling down, depressed, or hopeless? | 0.4 ± 0.5 | 0.3 ± 0.4 | 0.2 ± 0.4 | 0.220 |
| 3. Trouble falling or staying asleep, or sleeping too much? | 0.4 ± 0.5 | 0.5 ± 0.5 | 0.4 ± 0.5 | 0.097 |
| 4. Feeling tired or having little energy? | 0.7 ± 0.5 | 0.4 ± 0.5 | 0.4 ± 0.5 | 0.159 |
| 5. Poor appetite or overeating? | 0.2 ± 0.4 | 0.2 ± 0.4 | 0.2 ± 0.4 | 0.638 |
| 6. Feeling bad about yourself or that you are a failure or have let yourself or your family down? | 0.4 ± 0.5 | 0.2 ± 0.4 | 0.1 ± 0.3 | 0.008 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television? | 0.1 ± 0.3 | 0.1 ± 0.2 | 0.1 ± 0.3 | 0.908 |
| 8. Moving or speaking so slowly that other people could have noticed or feeling so fidgety or restless that you have been moving a lot more than usual? | 0.1 ± 0.3 | 0.1 ± 0.3 | 0.1 ± 0.2 | 0.313 |
| 9. Thoughts that you would be better off dead or thoughts of hurting yourself in some way? | 0.3 ± 0.5 | 0.1 ± 0.3 | 0.1 ± 0.3 | 0.016 |
| Total PHQ-9 score | 3.9 ± 2.4 | 3.3 ± 4.0 | 2.6 ± 3.7 | 0.152 |
Data are expressed as mean ± standard deviation. Statistical comparisons were conducted using a one-way analysis of variance for continuous variables and Pearson’s χ2 test for categorical variables.
PHQ-9 = Patient Health Questionnaire-9.
Fig. 1. Prevalence of depressive symptoms according to age at menopause among Korean postmenopausal women. Statistical significance was set at 0.05/3 (= 0.0167), and the P value was adjusted using the Bonferroni method for multiple comparisons.
PHQ = Patient Health Questionnaire, POI = primary ovarian insufficiency.
aSignificantly different from the normal menopause group (menopause after 45 years of age).
The results of crude and multivariate regression analyses for the odds of suicidal ideation, measured using the PHQ-9 suicide item, are presented in Table 3. Women with POI had a significantly higher odds of suicidal ideation than those who experienced menopause after 45 years of age; this association remained significant in 2 multivariable regression models after the adjustment for several confounding factors: model 2 was adjusted for age (odds ratio [OR], 5.9; 95% confidence interval [CI], 1.5–23.8), and model 3 was further adjusted for BMI, and education, household income, and walking levels (OR, 4.2; 95% CI, 1.0–17.7). No significant multicollinearity was observed among the variables included in the multivariate models. The same models were applied to the risk of impaired self-esteem as measured by PHQ-9 item 6, and these results were similar to those of suicidal ideation (Table 3).
Table 3. Logistic regression analyses of the risks of suicidal ideation and impaired self-esteem among study groups.
| Characteristics | Type of menopause | Suicidal ideationa | Impaired self-esteemb | ||
|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Model 1 (unadjusted) | Normal menopause (reference) | - | - | - | - |
| Primary ovarian insufficiency | 4.9 (1.3–19.4) | 0.022 | 4.5 (1.2–15.9) | 0.021 | |
| Early menopause | 1.7 (0.8–3.3) | 0.145 | 1.7 (1.0–3.1) | 0.061 | |
| Model 2 | Normal menopause (reference) | - | - | - | - |
| Primary ovarian insufficiency | 5.9 (1.5–23.8) | 0.012 | 4.7 (1.3–17.0) | 0.018 | |
| Early menopause | 1.7 (0.9–3.4) | 0.133 | 1.8 (1.0–3.1) | 0.055 | |
| Model 3 | Normal menopause (reference) | - | - | - | - |
| Primary ovarian insufficiency | 4.2 (1.0–17.7) | 0.049 | 3.7 (1.0–13.8) | 0.047 | |
| Early menopause | 1.4 (0.7–3.0) | 0.320 | 1.6 (0.9–2.9) | 0.103 | |
The normal menopause group (menopause after 45 years of age) was used as reference.
Model 1 was a crude analysis. Model 2 was adjusted for age. Model 3 was adjusted for age, body mass index, education level, household income level, and walking ≥ 1 time per week for > 10 minutes.
CI = confidence interval, OR = odds ratio.
aSuicidal ideation and bimpaired self-esteem were assessed using PHQ-9 items 9 and 6, respectively.
DISCUSSION
This population-based study using KNHANES data showed that age at menopause is associated with the incidence of suicidal ideation and impaired self-esteem after the adjustment for age, BMI, and several known confounding factors in middle-aged menopausal Korean women who were not diagnosed with major depressive disorder.
Among the Organization for Economic Co-operation and Development countries, Korea has shown the highest suicide rate among adult women in the last decade, and over 10% of adult Korean women were reported to have attempted suicide or feel suicidal ideation.19 In the present study, the incidence of suicidal ideation in women with POI was much higher than that in the general population, reaching approximately 20%. Depressive disorders in Korean women are reportedly not effectively managed by professionals or systems.20 Thus, well-organized screening programs and attentive management are needed in this population.
According to a recently reported systematic review and meta-analysis of 14 studies involving 67,714 women in the United States, Turkey, Israel, and European countries, increasing age at menopause (2-year increments) was associated with a 2% decrease in the risk of depression in menopausal women.9 Furthermore, the results of a meta-analysis of 4 studies representing 3,033 women showed that POI was associated with a 2-fold higher risk of depression than menopause at ≥ 40 years of age.9 The present study additionally revealed that, among women not diagnosed with depressive disorders, age at menopause was associated with select depressive symptoms, particularly suicidal ideation. Although further longitudinal studies are needed to confirm these associations, these findings indicate the need to identify women at a higher risk of suicidal ideation related to POI or early menopause who could benefit from psychiatric management.
Several mechanisms may explain the association between POI and depressive symptoms. First, a prolonged period of estrogen deprivation in women with POI may have negative effects on mood disorders.21,22 Estrogens exert neuroprotective effects via receptors located in the brain; therefore, a younger age at menopause may indicate shorter exposure to the neuroprotective and anti-depressive effects of endogenous estrogens.23 Low serotonergic activity associated with hypoestrogenism appears to increase suicide risk in individuals with predisposing factors.24 Second, the association might be due to various shared risk factors. Suicidal ideation was associated with age, obesity, stress, underlying chronic diseases such as hypertension and diabetes, low education or household income level, and reduced physical activity in previous studies,25,26 which are also frequent in women with POI. In this study, the prevalence of hypertension and diabetes was high in women with POI, and it is possible that the high incidence of suicidal ideation observed in those women might be associated with morbid chronic diseases and their complications. Therefore, further large studies with analyses of various confounding variables should be conducted to confirm our findings.
To the best of our knowledge, this is the first population-based study of East Asian menopausal women using a national database that revealed a significant association between age at menopause and psychosomatic symptoms including suicidal ideation and impaired self-esteem. However, this study has several limitations. First, its cross-sectional design prevented the assessment of causality. Second, the evaluation of suicidal ideation was dependent on patient self-reporting. However, the PHQ-9 has been widely used and validated as a single measure to assess the prevalence of suicidal ideation in research studies.27 Third, although various scales have been used to date in clinical fields to assess psychosomatic symptoms, this study used the results of the PHQ-9 survey, which were available for the sixth and seventh KNHANES datasets. To investigate the relationship of age at menopause with more detailed and variant aspects of depressive symptoms, further studies should be encouraged with a reliable multiple-item measurement to evaluate various psychosomatic symptoms such as a structured clinical interview using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.28 Fourth, the age at menopause was also assessed using self-reported data; there was a potential risk of inaccurate responses and recall bias. Further studies are needed of data on serum hormone levels, which would be an objective indication of menopausal status. Finally, although we adjusted for confounding factors in our study, the possibility of residual confounding factors linking POI and suicidal ideation persists.
In conclusion, age at menopause is independently associated with psychosomatic symptoms, including suicidal ideation and impaired self-esteem, in middle-aged menopausal women who are not diagnosed with major depressive disorder. Clinicians caring for postmenopausal women who experience POI should consider performing comprehensive screening and assessment of risk factors for suicidal ideation and suicide attempts regardless of the definite diagnosis of major depressive disorder.
ACKNOWLEDGMENTS
This research was supported by the Statistical Support Project for Writing Medical Papers using the Korea National Health and Nutrition Examination Survey (KNHANES), Korea University Anam Hospital.
Footnotes
Funding: This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2020R1C1C1013579). This work was supported by the Public Interest Medical Technology Research Project funded by the Ministry of Health and Welfare (MOHW, Korea; grant number HI21C1560). The funders played no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Disclosure: The authors have no potential conflicts of interest to disclose.
Data Availability Statement: Data will be made available on request.
- Conceptualization: Ryu KJ, Park H.
- Data curation: Jeong Y.
- Formal analysis: Ryu KJ, Jeong Y.
- Funding acquisition: Ryu KJ, Park H.
- Investigation: Ryu KJ, Park H, Jeong Y.
- Methodology: Ryu KJ, Jeong Y.
- Supervision: Park H.
- Writing - original draft: Ryu KJ, Park H, Jeong Y, Kim T.
- Writing - review & editing: Ryu KJ, Park H, Jeong Y, Nam S, Jeong HG, Kim T.
References
- 1.Xu X, Jones M, Mishra GD. Age at natural menopause and development of chronic conditions and multimorbidity: results from an Australian prospective cohort. Hum Reprod. 2020;35(1):203–211. doi: 10.1093/humrep/dez259. [DOI] [PubMed] [Google Scholar]
- 2.Santoro N. Mechanisms of premature ovarian failure. Ann Endocrinol (Paris) 2003;64(2):87–92. [PubMed] [Google Scholar]
- 3.Kokcu A. Premature ovarian failure from current perspective. Gynecol Endocrinol. 2010;26(8):555–562. doi: 10.3109/09513590.2010.488773. [DOI] [PubMed] [Google Scholar]
- 4.Lim YM, Jeong K, Lee SR, Chung HW, Lee W. Association between premature ovarian insufficiency, early menopause, socioeconomic status in a nationally representative sample from Korea. Maturitas. 2019;121:22–27. doi: 10.1016/j.maturitas.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Choe SA, Sung J. Trends of premature and early menopause: a comparative study of the US National Health and Nutrition Examination Survey and the Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2020;35(14):e97. doi: 10.3346/jkms.2020.35.e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uygur D, Sengül O, Bayar D, Erdinç S, Batioğlu S, Mollamahmutoglu L. Bone loss in young women with premature ovarian failure. Arch Gynecol Obstet. 2005;273(1):17–19. doi: 10.1007/s00404-005-0029-7. [DOI] [PubMed] [Google Scholar]
- 7.Roeters van Lennep JE, Heida KY, Bots ML, Hoek A collaborators of the Dutch Multidisciplinary Guideline Development Group on Cardiovascular Risk Management after Reproductive Disorders. Cardiovascular disease risk in women with premature ovarian insufficiency: a systematic review and meta-analysis. Eur J Prev Cardiol. 2016;23(2):178–186. doi: 10.1177/2047487314556004. [DOI] [PubMed] [Google Scholar]
- 8.Deeks AA, Gibson-Helm M, Teede H, Vincent A. Premature menopause: a comprehensive understanding of psychosocial aspects. Climacteric. 2011;14(5):565–572. doi: 10.3109/13697137.2011.566390. [DOI] [PubMed] [Google Scholar]
- 9.Georgakis MK, Thomopoulos TP, Diamantaras AA, Kalogirou EI, Skalkidou A, Daskalopoulou SS, et al. Association of age at menopause and duration of reproductive period with depression after menopause: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73(2):139–149. doi: 10.1001/jamapsychiatry.2015.2653. [DOI] [PubMed] [Google Scholar]
- 10.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9(1):90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cuadros JL, Fernández-Alonso AM, Cuadros-Celorrio AM, Fernández-Luzón N, Guadix-Peinado MJ, del Cid-Martín N, et al. Perceived stress, insomnia and related factors in women around the menopause. Maturitas. 2012;72(4):367–372. doi: 10.1016/j.maturitas.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Pérez-López FR, Chedraui P, Gilbert JJ, Pérez-Roncero G. Cardiovascular risk in menopausal women and prevalent related co-morbid conditions: facing the post-Women’s Health Initiative era. Fertil Steril. 2009;92(4):1171–1186. doi: 10.1016/j.fertnstert.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 14.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43(1):69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. 2008;49(2):218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22(11):1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cannon DS, Tiffany ST, Coon H, Scholand MB, McMahon WM, Leppert MF. The PHQ-9 as a brief assessment of lifetime major depression. Psychol Assess. 2007;19(2):247–251. doi: 10.1037/1040-3590.19.2.247. [DOI] [PubMed] [Google Scholar]
- 19.Koo KM, Kim K. Effects of physical activity on the stress and suicidal ideation in Korean adult women with depressive disorder. Int J Environ Res Public Health. 2020;17(10):3502. doi: 10.3390/ijerph17103502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J, Kim JH. A facilitator of leisure activities for stress-related growth experience among middle-aged Korean women with depression. Health Care Women Int. 2014;35(11-12):1245–1266. doi: 10.1080/07399332.2014.946508. [DOI] [PubMed] [Google Scholar]
- 21.Rocca WA, Grossardt BR, Geda YE, Gostout BS, Bower JH, Maraganore DM, et al. Long-term risk of depressive and anxiety symptoms after early bilateral oophorectomy. Menopause. 2008;15(6):1050–1059. doi: 10.1097/gme.0b013e318174f155. [DOI] [PubMed] [Google Scholar]
- 22.Saunders KE, Hawton K. Suicidal behaviour and the menstrual cycle. Psychol Med. 2006;36(7):901–912. doi: 10.1017/S0033291706007392. [DOI] [PubMed] [Google Scholar]
- 23.Arevalo MA, Azcoitia I, Garcia-Segura LM. The neuroprotective actions of oestradiol and oestrogen receptors. Nat Rev Neurosci. 2015;16(1):17–29. doi: 10.1038/nrn3856. [DOI] [PubMed] [Google Scholar]
- 24.Baca-Garcia E, Vaquero C, Diaz-Sastre C, Ceverino A, Saiz-Ruiz J, Fernández-Piquera J, et al. A pilot study on a gene-hormone interaction in female suicide attempts. Eur Arch Psychiatry Clin Neurosci. 2003;253(6):281–285. doi: 10.1007/s00406-003-0441-6. [DOI] [PubMed] [Google Scholar]
- 25.Wie JH, Nam SK, Ko HS, Shin JC, Park IY, Lee Y. The association between abortion experience and postmenopausal suicidal ideation and mental health: results from the 5th Korean National Health and Nutrition Examination Survey (KNHANES V) Taiwan J Obstet Gynecol. 2019;58(1):153–158. doi: 10.1016/j.tjog.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 26.Chang JC, Yen AM, Lee CS, Chen SL, Chiu SY, Fann JC, et al. Metabolic syndrome and the risk of suicide: a community-based integrated screening samples cohort study. Psychosom Med. 2013;75(9):807–814. doi: 10.1097/PSY.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 27.Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, et al. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park SC, Sakong J, Koo BH, Kim JM, Jun TY, Lee MS, et al. Clinical significance of the number of depressive symptoms in major depressive disorder: results from the CRESCEND study. J Korean Med Sci. 2016;31(4):617–622. doi: 10.3346/jkms.2016.31.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]