Abstract
Background
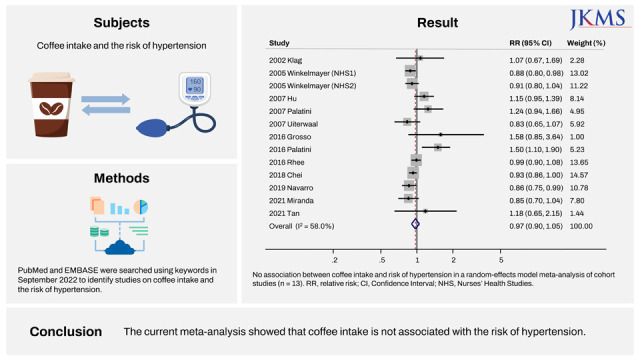
It remains unclear whether coffee intake is associated with the risk of hypertension. This study aimed to investigate the association between coffee intake and the risk of hypertension by using a meta-analysis of cohort studies.
Methods
PubMed and Embase were searched using keywords in September 2022 to identify studies on coffee intake and the risk of hypertension.
Results
We included a total of 13 longitudinal cohort studies, which involved a total of 64,650 incident cases of hypertension among 314,827 participants. In a random effects model meta-analysis of all the studies, coffee intake was not significantly associated with the risk of hypertension (relative risk [RR], 0.97; 95% confidence interval [CI], 0.90–1.05; I2 = 58.0%; n = 13). In the subgroup meta-analysis, coffee intake was associated with a decreased risk of hypertension in studies conducted in America (RR, 0.93; 95% CI, 0.87–0.98; I2 = 4.6%; n = 5) and in low-quality studies (RR, 0.92; 95% CI, 0.88–0.96; I2 = 0.0%; n = 7). In the remaining subgroup meta-analyses by amount of coffee intake, gender, type of coffee (decaffeinated vs. caffeinated), smoking, and years of follow-up, coffee intake was not significantly associated with the risk of hypertension.
Conclusion
The current meta-analysis showed that coffee intake is not associated with the risk of hypertension.
Keywords: Hypertension, Coffee, Cohort Studies, Meta-Analysis
Graphical Abstract
INTRODUCTION
Hypertension is a major global health problem that affects nearly 1 billion people worldwide.1 It serves as a risk factor for cardiovascular disease, stroke, kidney disease, and all-cause mortality.1,2 Having low physical activity, excess body mass index (BMI), and unhealthy dietary habits including excessive salt consumption play an important role in the development of hypertension.3,4
In the meantime, coffee is one of the most widely consumed beverages in the world.5 It contains a mixture of caffeine, phenolic compounds, niacin, minerals (magnesium, potassium), and fiber.6 Caffeine is known to increase blood pressure (BP) by blocking adenosine receptors in blood vessels and by causing vasoconstriction.7 Coffee also contains chlorogenic acids (CGAs) that have been shown to have antihypertensive effects in animal studies and randomized controlled trials (RCTs).8,9,10,11,12 For instance, the oral administration of green coffee bean extract (GCE), which is rich in CGA, reduced BP in spontaneously hypertensive rats in a dose-dependent manner.12 In addition, the ingestion of CGAs from GCE for 3 months was associated with a significant decrease in BP in patients with mild hypertension in the randomized, placebo-controlled trial.9 Though the exact mechanism by which CGAs lower BP is unclear, it has been proposed that CGAs may lower BP by nitric oxide-mediated vasodilation and by downregulating levels of reactive oxygen species, which play an important role in the regulation of vascular tone.10,12
In two meta-analyses of RCTs, increased coffee in-take was associated with a slight increase in BP.13,14 However, these RCTs only had a short duration of coffee exposure (< 85 days) and tested relatively high doses of coffee (median of 5 cups/day).13,14 The long-term effect of coffee constituents on BP is not yet fully understood due to a paucity of long-term RCTs.
The association between chronic coffee intake and the risk of hypertension has been explored in observational epidemiological studies such as prospective cohort studies.15,16,17,18,19,20,21,22,23,24,25,26 However, those findings remain inconsistent: some cohort studies reported a positive association between coffee intake and hypertension,15,17,18,20,21,26 while others showed a negative association.16,19,22,23,24,25
A meta-analysis of cohort studies in 2011 showed an inverse J-shaped association between chronic coffee intake and hypertension, with a maximum risk at 3 cups/day.27 Meanwhile, a meta-analysis of cohort studies in 2012 concluded that chronic coffee intake was not significantly associated with the risk of hypertension.28 On the contrary, recent two dose-response meta-analyses of prospective studies in 2018 and 2019 reported a significant, but trivial protective effect of coffee consumption on hypertension.29,30 Since then, several additional cohort studies that explored the association between long-term coffee intake and incident hypertension have been published.24,25,26
In this study, we aimed to investigate the association between coffee intake and the risk of hypertension by using a meta-analysis of recently published prospective cohort studies with sub-group meta-analysis by various factors.
METHODS
Literature search
We searched PubMed (1970 to September 2022) and Embase (1987 to September 2022) for eligible studies using common keywords related to coffee intake and the risk of hypertension based on predetermined study protocol. The keywords for literature search were as follows: “coffee” and “caffeine” for exposure factors; “hypertension” and “blood pressure” for outcome factors; “cohort study” for study design. We combined the above search terms with AND and OR. We reviewed the bibliographies of relevant articles to find out additional publications from the previous review articles and reference lists.
Selection criteria
We included longitudinal cohort studies that investigated the association between coffee intake and the risk of hypertension reporting outcome measures with adjusted relative risk (RR) and 95% confidence intervals (CI). If the search returned duplicate studies, the duplicate was removed. The language of publication was restricted to English.
Selection of relevant studies
Two of the authors (MJ Han and YJ Oh) independently evaluated the eligibility of all studies retrieved from databases based on the pre-determined selection criteria. Disagreements between evaluators were resolved by discussion. We extracted the following data from the studies included in the final analysis: study name (along with the name of the first author and publication year), country, study period (in years), population (age, gender), definition of coffee intake (highest vs. lowest categories), RR with 95% CI, and adjustments of variables.
Assessment of methodological quality
We assessed the methodological quality of included studies based on the Newcastle-Ottawa Scale (NOS) for assessing the quality of cohort studies in meta-analyses.31 A starring system of the NOS ranges from 0 to 9 and consists of three subscales: selection of studies, comparability, and exposure. In the current study, we considered studies awarded more than the mean score of all studies as high quality, since the criteria for high or low quality studies have not been established.
Main and subgroup analyses
We investigated the association between coffee intake (highest vs. lowest use) and the risk of hypertension by using adjusted RRs with 95% CIs for the main analysis. We also performed subgroup analyses by amount of coffee intake (highest intake defined as quintile 5, quartile 4 or tertile 3; moderate as quintile 4 or quartile 3; lower as quintile 2, quartile 2 or tertile 2 respectively based on each study’s categorization), gender (male vs. female), region (America, Asia, and Europe), methodological quality (high vs. low), type of coffee (decaffeinated vs. caffeinated), smoking (never/ever vs. current smoker) and number of follow-up years (< 5 years, 5 years or longer to less than 10 years, 10 years or longer).
Statistical analyses
To calculate the pooled RR with its 95% CI, we used adjusted RRs and 95% CIs reported in individual articles. We evaluated heterogeneity in results across studies using Higgins I2, which measures the percentage or total variation across studies.32 I2 was calculated as follows:
| I2 = 100% × (Q – df)/Q, |
where Q is Cochran’s heterogeneity statistic, and df is the degrees of freedom. Negative values of I2 are set at zero. I2 lies between 0% (no observed heterogeneity) and 100% (maximal heterogeneity). An I2 value greater than 50% was considered substantial heterogeneity.
A random-effects model meta-analysis on the basis of the DerSimonian and Laird method was used in the current study because individual trials were carried out in the different populations.33
We also examined publication bias regarding the studies included in the final analysis using Begg’s funnel plot and Egger’s test. If publication bias exists, Begg’s funnel plot is asymmetrical or P value is less than 0.05 by Egger’s test. For statistical analysis, Stata SE version 12.1 software package (StataCorp, College Station, TX, USA) was used.
RESULTS
Identification of relevant studies
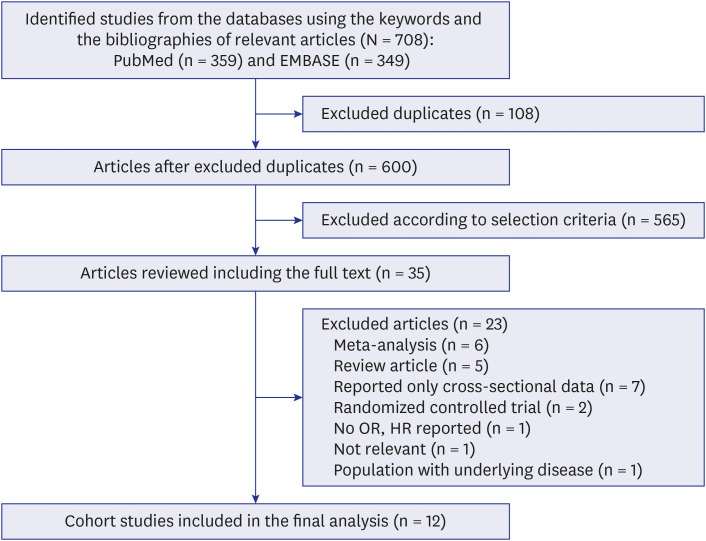
Fig. 1 shows the flow diagram of how we identified relevant studies. A total of 708 studies were identified using PubMed and Embase. We excluded 108 duplicates and an additional 565 articles that did not satisfy the selection criteria. The full texts of the remaining 35 articles were reviewed, and 23 articles were additionally excluded due to several reasons, as shown in Fig. 1. The remaining 12 articles15,16,17,18,19,20,21,22,23,24,25,26 were included in the final analysis.
Fig. 1. Flow diagram of identification of relevant studies.
General characteristics of studies
We identified a total of 13 independent cohort studies from 12 articles, which included 64,650 cases of hypertension amount a total of 314,827 participants. Since the study by Winkelmayer et al.16 included two independent cohorts (Nurses’ Health Study I and II), we considered each cohort study as separate studies. Table 1 shows the general characteristics of the studies in the final analysis. The sample sizes ranged from 1,017 to 94,503. The follow-up period for participants across studies ranged from 3.9 to 33 years. The main characteristics of each study are presented in Table 1.
Table 1. General characteristics of the studies included in the final analysis (n = 12).
| Study (reference) | Region | Total number of subjects | Total number of cases | Sex | Age at baseline,a yr | Duration of follow-up, yr | Measure of coffee intake (highest vs. lowest category) | Definition of coffee consumption (lowest vs. highest category) | HT assessment | RR (95% CI) | Adjusted variables |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Klag et al., 200215 | North America | 1,017 | 281 | M | 26 | 33 | Most recent intake, questionnaire | 0 cups/day vs. ≥ 5 cups/day | Self-reported | 1.07 (0.67–1.69) | Parental incidence of HT, BMI, smoking, alcohol, and physical activity |
| Winkelmayer et al., 2005 (NHS1)16 | North America | 53,175 | 19,541 | F | 55 | 12 | Most recent intake, FFQ | < 1 cup/day vs. ≥ 6 cups/day | Self-reported | 0.88 (0.80–0.98) | Age, BMI, alcohol, family history of HT, physical activity, smoking, and other classes of beverages |
| Winkelmayer et al., 2005 (NHS2)16 | North America | 94,503 | 13,536 | F | 36 | 12 | Most recent intake, FFQ | < 1 cup/day vs. ≥ 6 cups/day | Self-reported | 0.91 (0.80–1.04) | Age, BMI, alcohol, family history of HT, physical activity, smoking, other classes of beverages, and oral contraceptive use |
| Hu et al., 200717 | Europe | 24,710 | 2,505 | M/F | 43 | 13.2 | Baseline coffee intake, questionnaire | 0–1 cups/day vs. ≥ 8 cups/day | Directly measured | 1.15 (0.95–1.39) | Age, sex, study year, education, physical activity, smoking, alcohol, tea, vegetable, fruit, sausage, bread consumption, BMI, history of DM, total cholesterol, and baseline SBP |
| Palatini et al., 200718 | Europe | 1,107 | 561 | M/F | 33 | 6.4 | Most recent intake, questionnaire | Abstainer vs. heavy drinker (≥ 4 cups/day) | Record of HT drug use | 1.24 (0.94–1.66) | Age, sex, lifestyle factors, parental HT, duration of HT, BMI, change in body weight, and recent coffee intake |
| Uiterwaal et al., 200719 | Europe | 6,368 | 956 | M/F | 40 | 11 | Baseline coffee intake, questionnaire, FFQ | 0–3 cups/day vs. > 6 cups/day | Directly measured or record of HT drug use | 0.83 (0.65–1.07) | Age, sex, height, weight, smoking, alcohol, tea consumption, education, occupational status, and total energy intake |
| Grosso et al., 201620 | Europe | 2,725 | 1,735 | M/F | 56.2/55.2 | 5 | Baseline coffee intake, FFQ | < 1 cup/day vs. > 4 cups/day | Directly measured or record of HT drug use | 1.58 (0.85–3.64) | Age, sex, education, occupation, BMI, alcohol, smoking, physical activity, hx of CVD, DM, DL, total energy intake, vitamin supplement use, oral contraceptive use, and Na and K intake |
| Palatini et al., 201621 | Europe | 1,204 | 783 | M/F | 33.1 | 12.6 | Most recent intake, questionnaire | Nondrinker vs. heavy drinker (≥ 4 cups/day) | Directly measured | 1.50 (1.10–1.90) | Age, sex, BMI, ambulatory SBP and DBP, smoking, alcohol use, and follow-up change in body weight |
| Rhee et al., 201622 | North America | 29,985 | 5,566 | F | 62.5 | 3.76 | Baseline coffee intake, questionnaire | 0 cups/day vs. > 4 cups/day | Directly measured | 0.99 (0.90–1.08) | Age, baseline BP, BMI, physical activity, HRT, alcohol, smoking, total caloric intake, Na, Mg, Ca, and K and P intake |
| Chei et al., 201823 | Asia | 63,257 | 13,658 | M/F | 54.9 | 9.5 | Baseline coffee intake, FFQ | 1 cup/day vs. ≥ 3 cups/day | Self-reported | 0.93 (0.86–1.00) | Age at recruitment, year of recruitment, sex, dialect group, BMI, education, smoking, alcohol, physical activity, sleep duration, dietary intake of sodium, vegetables, fruits, dairy products (all in quartiles), and intake of tea |
| Navarro et al., 201924 | Europe | 13,374 | 1,757 | M/F | 35.7 | 9.1 | Baseline coffee intake, FFQ | Never/seldom vs. ≥ 2 cups/day | Self-reported | 0.86 (0.75–0.99) | Age, BMI, alcohol, smoking, family history, Na intake, whole and low-fat dairy product consumption, sugar-sweetened beverage, nonsugared carbonate beverage, physical activity, adherence to Mediterranean diet, personality, time spent watching TV, and fried and fast food consumption |
| Miranda et al., 202125 | North America | 8,780 | 1,285 | M/F | 49 | 3.9 | Baseline coffee intake, FFQ | Never/almost never vs. > 3 cups/day | Directly measured | 0.85 (0.70–1.04) | Age, sex, race, education, income, BMI, physical activity, smoking, alcohol, dietary intake of fruit, vegetable, Na, K, saturated fat, added sugar, total energy intake, supplement use, fasting glucose, total cholesterol, and triglyceride |
| Tan et al., 202126 | Asia | 14,622 | 2,486 | M/F | 53.7/52.6 | 5 | Baseline coffee intake, FFQ | 0 cups/day vs. > 3 cups/day | Directly measured | 1.18 (0.65–2.15) | Age, BMI, energy intake, educational level, current drinking/smoking status, and physical activity |
HT = hypertension, RR = relative risk, CI = confidence interval, M = male, BMI = body mass index, NHS = nurses’ health studies, F = female, FFQ = food frequency questionnaire, SBP = systolic blood pressure, CVD = cardiovascular disease, DM = diabetes mellitus, DL = dyslipidemia, DBP = diastolic blood pressure, BP = blood pressure, HRT = hormone replacement therapy.
aMean or median age.
Overall, the regions where the studies were performed were as follows: Europe (n = 6), America (n = 5), and Asia (n = 2). Both men and women were included in nine of the 13 cohort studies.17,18,19,20,21,23,24,25,26 The remaining studies included only women (n = 3)16,22 or men (n = 1).15 Eight studies defined hypertension as systolic BP ≥ 140 mmHg or/and diastolic BP ≥ 90 mmHg, systolic BP ≥ 130 mmHg or/and diastolic BP ≥ 85 mmHg, or the use of antihypertensive medication, while five defined the outcome as self-reported hypertension.
Coffee intake and risk of hypertension
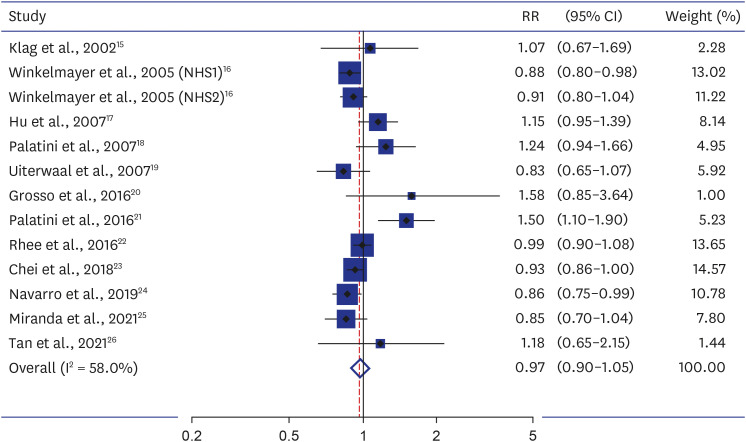
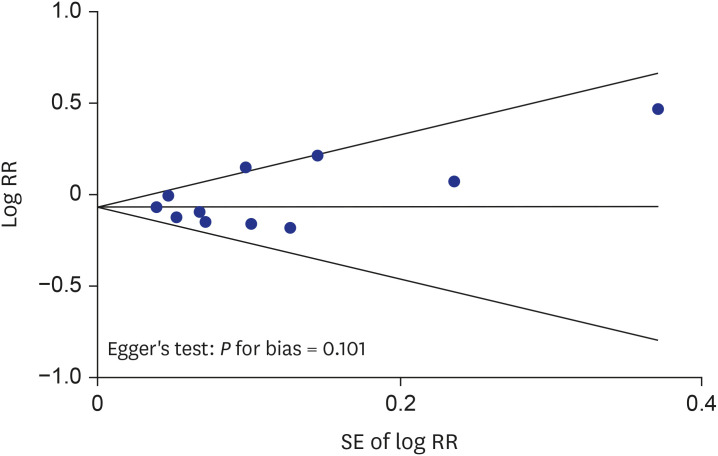
Fig. 2 shows the effect of coffee intake on the risk of hypertension in the meta-analysis of all studies. Coffee intake (highest vs. lowest intake) was not significantly associated with the risk of hypertension in a random-effects model meta-analysis of all 13 cohort studies (RR, 0.97; 95% CI, 0.90–1.05; I2 = 58.0%; n = 13). The Begg’s funnel seems visually asymmetric, but the P for bias from Egger’s test was not statistically significant (P for bias = 0.101) (Fig. 3).
Fig. 2. Association between coffee intake and risk of hypertension in a random-effects model meta-analysis of cohort studies (n = 13).
RR = relative risk, CI = confidence interval, NHS = nurses’ health study.
Fig. 3. Begg’s funnel plots and Egger’s test for identifying publication bias in the meta-analysis of observational studies.
RR = relative risk, SE = standard error.
Methodological quality of studies
Table 2 shows the methodological quality of studies included in the final analysis based on the NOS. The range of quality scores was 6 to 8; the average score was 7.1. The high-quality studies (score of 7 or higher) included six studies.
Table 2. Methodological quality of studies included in the final analysis based on the Newcastle-Ottawa Scalea for assessing the quality of cohort studies (n = 12).
| Cohort studies (N = 12) | Selection | Comparability | Outcome | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Outcome of interest was not present at start of study | Control for important factor or additional factor | Assessment of outcome | Follow-up long enough for outcomes to occur | Adequacy of follow-up of cohorts | ||
| Klag et al., 200215 | 0 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 6 |
| Winkelmayer et al., 2005 (NHS1)16 | 0 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 6 |
| Winkelmayer et al., 2005 (NHS1)16 | 0 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 6 |
| Hu et al., 200717 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| Palatini et al., 200718 | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 |
| Uiterwaal et al., 200719 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
| Grosso et al., 201620 | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 |
| Palatini et al., 201621 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| Rhee et al., 201622 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 |
| Chei et al., 201823 | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 0 | 6 |
| Navarro et al., 201924 | 1 | 1 | 0 | 1 | 2 | 0 | 1 | 1 | 7 |
| Miranda et al., 202125 | 1 | 1 | 1 | 1 | 2 | 1 | 0 | 1 | 8 |
| Tan et al., 202126 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 0 | 7 |
aEach study can be awarded a maximum of one star for each numbered item within the selection and exposure categories, while a maximum of two stars can be given for the comparability category.
Subgroup meta-analyses
Table 3 summarizes the results from the subgroup meta-analyses by several factors. In the subgroup meta-analyses by amount of coffee intake, gender, type of coffee, smoking, and years of follow-up, coffee intake was not significantly associated with the risk of hypertension. The subgroup meta-analysis by region showed a decreased risk of hypertension in America (RR, 0.93; 95% CI, 0.87–0.98; I2 = 4.6%; n = 5), but not in Europe (RR, 1.10; 95% CI, 0.89–1.35; I2 = 76.0%; n = 6) or in Asia (RR, 0.93; 95% CI, 0.87–1.01; I2 = 20.0%; n = 2).
Table 3. Association between coffee intake and the risk of hypertension in subgroup meta-analyses.
| Factors | No. of studies | Summary RR (95% CI) | Heterogeneity, I2 (%) | |
|---|---|---|---|---|
| Amount of coffee (vs. never or rarely drink) | ||||
| Lowest | 1215,16,17,18,19,20,21,22,23,24,25 | 1.02 (0.94–1.10) | 85.1 | |
| Moderate | 1015,16,17,19,20,22,23,24,25 | 0.95 (0.90–1.00) | 59.4 | |
| Highest | 1215,16,17,18,19,20,21,22,23,24,25 | 0.97 (0.90–1.05) | 68.0 | |
| Gender | ||||
| Female | 816,17,19,20,22,24,26 | 0.96 (0.84–1.09) | 78.6 | |
| Male | 615,17,19,20,24,26 | 0.99 (0.88–1.11) | 0.0 | |
| Region | ||||
| Europe | 617,18,19,20,21,24 | 1.10 (0.89–1.35) | 76.0 | |
| America | 515,16,22,25 | 0.93 (0.87–0.98) | 4.6 | |
| Asia | 223,26 | 0.93 (0.87–1.01) | 0.0 | |
| Type of coffee (decaffeinated vs. caffeinated) | ||||
| Caffeinated | 1315,16,17,18,19,20,21,22,23,24,25,26 | 0.97 (0.90–1.05) | 58.0 | |
| Decaffeinated | 222,24 | 0.95 (0.84–1.06) | 0.0 | |
| Smoking | ||||
| Never/ever smoker | 317,20,25 | 1.03 (0.78–1.35) | 51.9 | |
| Current smoker | 317,20,25 | 1.00 (0.73–1.39) | 0.0 | |
| Follow-up, yr | ||||
| < 5 | 222,25 | 0.94 (0.82–1.08) | 46.8 | |
| 5–10 | 518,20,23,24,26 | 0.97 (0.85–1.11) | 48.6 | |
| ≥ 10 | 615,16,17,19,21 | 1.01 (0.87–1.18) | 73.1 | |
| Methodological quality | ||||
| Low quality | 715,16,19,22,23,24 | 0.92 (0.88–0.96) | 0.0 | |
| High quality | 617,18,20,21,25,26 | 1.17 (0.96–1.43) | 62.4 | |
RR = relative risk, CI = confidence interval.
Furthermore, subgroup analyses by methodological quality of study showed that coffee intake was associated with a decreased risk of hypertension in low quality studies (RR, 0.92; 95% CI, 0.88–0.96; I2 = 0.0%; n = 7). In contrast, coffee intake was not significantly associated with hypertension in high quality studies (RR, 1.17; 95% CI, 0.96–1.43; I2 = 62.4%; n = 6).
DISCUSSION
In this meta-analysis of cohort studies, coffee intake was not significantly associated with the risk of hypertension. Also, in the subgroup analyses, coffee intake did not show a significant association with the risk of hypertension, except for the studies conducted in America (RR, 0.93; 95% CI, 0.87–0.98; I2 = 4.6%; n = 5) and low methodological quality studies (RR, 0.92; 95% CI, 0.88–0.96; I2 = 0.0%; n = 7).
Our findings are consistent with those from the previous meta-analysis by Steffen et al.,28 which reported no association between coffee intake and hypertension risk. In contrast, other meta-analyses by Zhang et al.,27 D’Elia et al.,30 and Xie et al.29 reported a significant association between coffee intake and hypertension. Zhang et al.27 found an inverse J-shaped relationship between coffee intake and hypertension risk, with increased risk up to 3 cups/day. D’Elia et al.30 reported that while habitual drinking of 1–2 cups of coffee per day, compared with non-drinking, was not associated with the risk of hypertension, the consumption of more than three cups of coffee per day was associated with a significantly lower risk of hypertension. Xie et al.29 found an inverse association between the risk of hypertension and coffee intake, with a reduction of 2% per one cup/day increment of coffee intake. Such inconsistent results from these meta-analyses may be attributable to differences in study populations, the inclusion of studies reporting different measure of outcomes, and the inclusion of unpublished data.30
Coffee is a mixture of several bioactive elements, such as caffeine, phenolic compounds, and minerals.6 Caffeine is one of the main constituents of coffee. Caffeine, which acts as an adenosine receptor antagonist, is known to cause vasoconstriction and to have an acute pressor effect.34,35 In contrast, CGAs contained in coffee are known to have an antihypertensive effect.36 Experimental studies have shown that CGAs lower BP in hypertensive rats as well as in humans.9,12 The mechanism by which CGAs lower BP might involve antioxidant activity.10 CGAs inhibit NAD(P)H oxidase expression and activity, causing a reduction in free radical production.10 Patients with uncontrolled hypertension have been shown to have elevated levels of hydrogen peroxide and superoxide anions, which deplete nitric oxide (NO) bioavailability in endothelial tissue.37 NO deficiency has been cited as a cause of hypertension, and NO-mediated vascular dilatation is reported to be decreased in hypertensive patients.38,39 Moreover, coffee is rich in minerals such as magnesium and potassium, which are also known to lower BP.6,40 Thus, despite the acute pressor effect of caffeine, other constituents of coffee that have an antihypertensive effect may counteract the effects of caffeine over long periods of ingestion.27 Furthermore, over the long term, tolerance may develop to the acute pressor effects of caffeine by the activation of counterregulatory hormones that maintain homeostasis for BP.34,35,41,42 Thus, this mechanism explains why our study showed no significant association between chronic coffee intake and the risk of hypertension.
Our meta-analysis contains several strengths. We performed a comprehensive meta-analysis including the most recently published cohort studies on coffee intake and hypertension risk. We also included studies that are characterized by high methodological quality, with scores ranging from 6 to 8. In addition, we performed subgroup meta-analyses by various factors such as amount of coffee, gender, region, type of coffee, smoking, years of follow-up, and methodological quality. Thus, we were able to confirm the consistency and robustness of the main results.
However, our study also possesses several limitations. First, since only observational cohort studies were included, this study cannot be used to infer cause and effect. Second, we could not exclude publication bias. The Begg’s funnel seems visually asymmetric, and the P for bias is close to 0.05, although it is not within the range of statistical significance (P for bias = 0.101). It means that coffee intake might have a protective effect against hypertension if we consider unpublished studies showing a protective effect. Third, we were not able to account for differences in cup size and type of coffee (boiled, filtered, etc.), since this information was not given in most of the studies. Similarly, we were not able to differentiate the effects of additives taken with coffee, such as cream or sugar, as certain studies did not assess for the use of these items in survey questions. Last, coffee intake was assessed through self-report in all studies, which may introduce misclassification of exposure. Thus, while we only intended to classify caffeinated coffee as the exposure criteria in this meta-analysis, the potential misclassification due to self-report may have resulted in the inclusion of decaffeinated coffee drinkers among selected participants.
To our knowledge, this is the most recent and comprehensive meta-analysis of cohort studies on the association of coffee intake and the risk of hypertension. Our study demonstrates that long-term coffee intake is not significantly associated with the risk of hypertension. Our study suggests that limiting coffee intake may not have a significant effect on lowering BP, and that coffee intake may not serve as a risk factor for hypertension.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Myung SK.
- Data curation: Han M.
- Formal analysis: Han M.
- Investigation: Han M, Oh Y.
- Methodology: Myung SK.
- Project administration: Myung SK.
- Supervision: Myung SK.
- Validation: Myung SK.
- Writing - original draft: Han M.
- Writing - review & editing: Han M, Oh Y, Myung SK.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.He J, Whelton PK. Epidemiology and prevention of hypertension. Med Clin North Am. 1997;81(5):1077–1097. doi: 10.1016/s0025-7125(05)70568-x. [DOI] [PubMed] [Google Scholar]
- 3.Jones DW. Dietary sodium and blood pressure. Hypertension. 2004;43(5):932–935. doi: 10.1161/01.HYP.0000126610.89002.c6. [DOI] [PubMed] [Google Scholar]
- 4.Geleijnse JM, Kok FJ, Grobbee DE. Impact of dietary and lifestyle factors on the prevalence of hypertension in Western populations. Eur J Public Health. 2004;14(3):235–239. doi: 10.1093/eurpub/14.3.235. [DOI] [PubMed] [Google Scholar]
- 5.Baylin A, Hernandez-Diaz S, Kabagambe EK, Siles X, Campos H. Transient exposure to coffee as a trigger of a first nonfatal myocardial infarction. Epidemiology. 2006;17(5):506–511. doi: 10.1097/01.ede.0000229444.55718.96. [DOI] [PubMed] [Google Scholar]
- 6.Godos J, Pluchinotta FR, Marventano S, Buscemi S, Li Volti G, Galvano F, et al. Coffee components and cardiovascular risk: beneficial and detrimental effects. Int J Food Sci Nutr. 2014;65(8):925–936. doi: 10.3109/09637486.2014.940287. [DOI] [PubMed] [Google Scholar]
- 7.Umemura T, Ueda K, Nishioka K, Hidaka T, Takemoto H, Nakamura S, et al. Effects of acute administration of caffeine on vascular function. Am J Cardiol. 2006;98(11):1538–1541. doi: 10.1016/j.amjcard.2006.06.058. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki A, Yamamoto N, Jokura H, Yamamoto M, Fujii A, Tokimitsu I, et al. Chlorogenic acid attenuates hypertension and improves endothelial function in spontaneously hypertensive rats. J Hypertens. 2006;24(6):1065–1073. doi: 10.1097/01.hjh.0000226196.67052.c0. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe T, Arai Y, Mitsui Y, Kusaura T, Okawa W, Kajihara Y, et al. The blood pressure-lowering effect and safety of chlorogenic acid from green coffee bean extract in essential hypertension. Clin Exp Hypertens. 2006;28(5):439–449. doi: 10.1080/10641960600798655. [DOI] [PubMed] [Google Scholar]
- 10.Zhao Y, Wang J, Ballevre O, Luo H, Zhang W. Antihypertensive effects and mechanisms of chlorogenic acids. Hypertens Res. 2012;35(4):370–374. doi: 10.1038/hr.2011.195. [DOI] [PubMed] [Google Scholar]
- 11.Olthof MR, Hollman PC, Buijsman MN, van Amelsvoort JM, Katan MB. Chlorogenic acid, quercetin-3-rutinoside and black tea phenols are extensively metabolized in humans. J Nutr. 2003;133(6):1806–1814. doi: 10.1093/jn/133.6.1806. [DOI] [PubMed] [Google Scholar]
- 12.Suzuki A, Kagawa D, Ochiai R, Tokimitsu I, Saito I. Green coffee bean extract and its metabolites have a hypotensive effect in spontaneously hypertensive rats. Hypertens Res. 2002;25(1):99–107. doi: 10.1291/hypres.25.99. [DOI] [PubMed] [Google Scholar]
- 13.Jee SH, He J, Whelton PK, Suh I, Klag MJ. The effect of chronic coffee drinking on blood pressure: a meta-analysis of controlled clinical trials. Hypertension. 1999;33(2):647–652. doi: 10.1161/01.hyp.33.2.647. [DOI] [PubMed] [Google Scholar]
- 14.Noordzij M, Uiterwaal CS, Arends LR, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens. 2005;23(5):921–928. doi: 10.1097/01.hjh.0000166828.94699.1d. [DOI] [PubMed] [Google Scholar]
- 15.Klag MJ, Wang NY, Meoni LA, Brancati FL, Cooper LA, Liang KY, et al. Coffee intake and risk of hypertension: the Johns Hopkins precursors study. Arch Intern Med. 2002;162(6):657–662. doi: 10.1001/archinte.162.6.657. [DOI] [PubMed] [Google Scholar]
- 16.Winkelmayer WC, Stampfer MJ, Willett WC, Curhan GC. Habitual caffeine intake and the risk of hypertension in women. JAMA. 2005;294(18):2330–2335. doi: 10.1001/jama.294.18.2330. [DOI] [PubMed] [Google Scholar]
- 17.Hu G, Jousilahti P, Nissinen A, Bidel S, Antikainen R, Tuomilehto J. Coffee consumption and the incidence of antihypertensive drug treatment in Finnish men and women. Am J Clin Nutr. 2007;86(2):457–464. doi: 10.1093/ajcn/86.2.457. [DOI] [PubMed] [Google Scholar]
- 18.Palatini P, Dorigatti F, Santonastaso M, Cozzio S, Biasion T, Garavelli G, et al. Association between coffee consumption and risk of hypertension. Ann Med. 2007;39(7):545–553. doi: 10.1080/07853890701491018. [DOI] [PubMed] [Google Scholar]
- 19.Uiterwaal CS, Verschuren WM, Bueno-de-Mesquita HB, Ocké M, Geleijnse JM, Boshuizen HC, et al. Coffee intake and incidence of hypertension. Am J Clin Nutr. 2007;85(3):718–723. doi: 10.1093/ajcn/85.3.718. [DOI] [PubMed] [Google Scholar]
- 20.Grosso G, Stepaniak U, Polak M, Micek A, Topor-Madry R, Stefler D, et al. Coffee consumption and risk of hypertension in the Polish arm of the HAPIEE cohort study. Eur J Clin Nutr. 2016;70(1):109–115. doi: 10.1038/ejcn.2015.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palatini P, Fania C, Mos L, Garavelli G, Mazzer A, Cozzio S, et al. Coffee consumption and risk of cardiovascular events in hypertensive patients. Results from the HARVEST. Int J Cardiol. 2016;212:131–137. doi: 10.1016/j.ijcard.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Rhee JJ, Qin F, Hedlin HK, Chang TI, Bird CE, Zaslavsky O, et al. Coffee and caffeine consumption and the risk of hypertension in postmenopausal women. Am J Clin Nutr. 2016;103(1):210–217. doi: 10.3945/ajcn.115.120147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chei CL, Loh JK, Soh A, Yuan JM, Koh WP. Coffee, tea, caffeine, and risk of hypertension: the Singapore Chinese Health Study. Eur J Nutr. 2018;57(4):1333–1342. doi: 10.1007/s00394-017-1412-4. [DOI] [PubMed] [Google Scholar]
- 24.Navarro AM, Martinez-Gonzalez MA, Gea A, Ramallal R, Ruiz-Canela M, Toledo E. Coffee consumption and risk of hypertension in the SUN Project. Clin Nutr. 2019;38(1):389–397. doi: 10.1016/j.clnu.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Miranda AM, Goulart AC, Benseñor IM, Lotufo PA, Marchioni DM. Coffee consumption and risk of hypertension: a prospective analysis in the cohort study. Clin Nutr. 2021;40(2):542–549. doi: 10.1016/j.clnu.2020.05.052. [DOI] [PubMed] [Google Scholar]
- 26.Tan LJ, Jeon HJ, Park S, Kim SA, Lim K, Chung S, et al. Association of coffee consumption and its types according to addition of sugar and creamer with metabolic syndrome incidence in a Korean population from the health examinees (HEXA) study. Nutrients. 2021;13(3):1–13. doi: 10.3390/nu13030920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Z, Hu G, Caballero B, Appel L, Chen L. Habitual coffee consumption and risk of hypertension: a systematic review and meta-analysis of prospective observational studies. Am J Clin Nutr. 2011;93(6):1212–1219. doi: 10.3945/ajcn.110.004044. [DOI] [PubMed] [Google Scholar]
- 28.Steffen M, Kuhle C, Hensrud D, Erwin PJ, Murad MH. The effect of coffee consumption on blood pressure and the development of hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30(12):2245–2254. doi: 10.1097/HJH.0b013e3283588d73. [DOI] [PubMed] [Google Scholar]
- 29.Xie C, Cui L, Zhu J, Wang K, Sun N, Sun C. Coffee consumption and risk of hypertension: a systematic review and dose-response meta-analysis of cohort studies. J Hum Hypertens. 2018;32(2):83–93. doi: 10.1038/s41371-017-0007-0. [DOI] [PubMed] [Google Scholar]
- 30.D’Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose-response meta-analysis of prospective studies. Eur J Nutr. 2019;58(1):271–280. doi: 10.1007/s00394-017-1591-z. [DOI] [PubMed] [Google Scholar]
- 31.Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-randomised Studies in Meta-Analyses. [Updated 2021]. [Accessed September 9, 2022]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm .
- 32.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 33.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 34.Myers MG. Effects of caffeine on blood pressure. Arch Intern Med. 1988;148(5):1189–1193. [PubMed] [Google Scholar]
- 35.Nurminen ML, Niittynen L, Korpela R, Vapaatalo H. Coffee, caffeine and blood pressure: a critical review. Eur J Clin Nutr. 1999;53(11):831–839. doi: 10.1038/sj.ejcn.1600899. [DOI] [PubMed] [Google Scholar]
- 36.Ochiai R, Jokura H, Suzuki A, Tokimitsu I, Ohishi M, Komai N, et al. Green coffee bean extract improves human vasoreactivity. Hypertens Res. 2004;27(10):731–737. doi: 10.1291/hypres.27.731. [DOI] [PubMed] [Google Scholar]
- 37.Prabha PS, Das UN, Koratkar R, Sagar PS, Ramesh G. Free radical generation, lipid peroxidation and essential fatty acids in uncontrolled essential hypertension. Prostaglandins Leukot Essent Fatty Acids. 1990;41(1):27–33. doi: 10.1016/0952-3278(90)90127-7. [DOI] [PubMed] [Google Scholar]
- 38.Thomas GD, Zhang W, Victor RG. Nitric oxide deficiency as a cause of clinical hypertension: promising new drug targets for refractory hypertension. JAMA. 2001;285(16):2055–2057. doi: 10.1001/jama.285.16.2055. [DOI] [PubMed] [Google Scholar]
- 39.Calver A, Collier J, Moncada S, Vallance P. Effect of local intra-arterial NG-monomethyl-L-arginine in patients with hypertension: the nitric oxide dilator mechanism appears abnormal. J Hypertens. 1992;10(9):1025–1031. [PubMed] [Google Scholar]
- 40.Higdon JV, Frei B. Coffee and health: a review of recent human research. Crit Rev Food Sci Nutr. 2006;46(2):101–123. doi: 10.1080/10408390500400009. [DOI] [PubMed] [Google Scholar]
- 41.Shi J, Benowitz NL, Denaro CP, Sheiner LB. Pharmacokinetic-pharmacodynamic modeling of caffeine: tolerance to pressor effects. Clin Pharmacol Ther. 1993;53(1):6–14. doi: 10.1038/clpt.1993.3. [DOI] [PubMed] [Google Scholar]
- 42.Nussberger J, Mooser V, Maridor G, Juillerat L, Waeber B, Brunner HR. Caffeine-induced diuresis and atrial natriuretic peptides. J Cardiovasc Pharmacol. 1990;15(5):685–691. doi: 10.1097/00005344-199005000-00001. [DOI] [PubMed] [Google Scholar]