Abstract
Objective
Subarachnoid hemorrhage (SAH) has been reported as a neurological manifestation in 0.1% of COVID-19 patients. This systematic review investigated the outcomes and predictive factors of SAH in patients with COVID-19.
Materials and methods
An electronic literature search was conducted on PubMed, Embase, and Scopus from inception to 10th September 2021. Studies reporting SAH in COVID-19 patients were included. Demographic characteristics, risk factors for disease, severity of COVID-19, and mortality of SAH in COVID-19 patients were analyzed. Subgroup analyses stratified by COVID-19 severity and mortality were conducted.
Results
17 case reports, 11 case series, and 2 retrospective cohort studies, with a total of 345 cases of SAH in COVID-19 patients, were included for analysis. Most published cases were reported in the US. Mean age was 55±18.4 years, and 162 patients (48.5%) were female. 242 patients (73.8%) had severe-to-critical COVID-19, 56.7% had aneurysmal SAH, 71.4% were on anticoagulation, and 10.8% underwent surgical treatment. 136 out of 333 patients (40.8%) died. Among patients with severe-to-critical COVID-19, 11 out of 18 (61.1%) died, and 8 out of 8 (100.0%) were non-aneurysmal SAH.
Conclusions
SAH is a rare but morbid occurrence in COVID-19. The mortality rate of COVID-SAH patients was 40.8%, with a higher prevalence of severe-to-critical COVID-19 (100% versus 53.8%) and non-aneurysmal SAH (85.7% versus 44.6%) among COVID-SAH deaths. Given the changing landscape of COVID-19 variants, further studies investigating the association between COVID-19 and SAH may be warranted to identify the long-term effects of COVID-19.
Key Words: Subarachnoid hemorrhage, COVID-19, Neurosurgery, Systematic review
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which emerged in end-2019 has resulted in an estimated 17.2 million infection-related deaths as of 31 May 2022.30 Neurological manifestations, including headache, impaired consciousness, ataxia, acute cerebrovascular disease, seizures, hyposmia, hypogeusia, and neuralgias have been reported in up to 36.4% of COVID-19 patients.19 , 20
Several reviews have investigated the relationships between COVID-19 and cerebrovascular disease such as stroke32 intracranial hemorrhage,6 and neuropathological findings.26 In COVID-19 patients, the incidence of intracranial hemorrhage and SAH has been reported at 0.7% patients,6 , 27 and 0.1% patients,5 , 28 respectively. SAH and COVID-19 have also been associated with higher morbidity and mortality as compared with isolated disease of either.5 , 28 However, the outcomes and predictive factors of concomitant SAH and COVID-19 (COVID-SAH) have not been adequately reported.
Considering the public health ramifications of COVID-19 transmission, which despite the rollout of vaccines is expected to continue2 with a possible resurgence up to 2024,15 it is important to understand how COVID-19 is associated with SAH. This understanding will help to guide the diagnosis and management of possible COVID-19-related SAH; if a correlation indeed exists, it is imperative to recognize it due to the predicted long-term endemic phases that many countries are predicted to experience with COVID-19.30 Hence, this systematic review aims to investigate the risk factors and outcomes of SAH in COVID-19 patients reported in the international literature.
Materials & methods
Search strategy and study selection
We conducted an electronic literature search from PubMed, Embase, and Scopus from inception to 10th September 2021, in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,25 without language restrictions. The search strategy consisted of search terms involving COVID-19 and SAH concepts [Supplementary Table 1]. References of included articles were also searched for any relevant articles that meet the inclusion criteria of the study. Studies reporting the presence of SAH in COVID-19 patients were included. Conference abstracts, preprints, systematic reviews, meta-analyses, and retrospective cohort studies which included SAH patients but did not report their baseline characteristics were excluded. In addition, bibliographies of included studies were screened, and searches on Google
Scholar and the Web of Science database (1900–2021) using the first and last author of each included study were conducted to ensure inclusion of all relevant studies. The study protocol was published in the International Register of Prospective Systematic Reviews (PROSPERO; reference no. CRD42021259432) prior to initiation of the study.
Two reviewers (KYF and JY) independently screened all retrieved abstracts using the above inclusion and exclusion criteria. Following identification of potentially relevant studies from abstract screening, full-text articles were retrieved. Two reviewers (KYF and JY) independently screened the full-texts and reasons for exclusion were recorded. Risk of bias was assessed using the Joana Briggs Institute Critical Appraisal Tools.21 , 22 Discrepancies at any stage of the screening were resolved by a third reviewer (MLJR).
Data extraction
The following variables were extracted from the studies by two independent reviewers (JY and KYF) using a standardized data collection form with the following fields: age, gender, co-morbidities (hypertension, hyperlipidemia, diabetes mellitus, smoking, anticoagulation), severity of COVID-19, etiology of SAH (aneurysmal or non-aneurysmal), associated intracranial pathologies, treatment (surgical or non-surgical), and outcomes (survived or deceased). Where not reported explicitly, COVID-19 severity was classified into mild, moderate, severe, and critical as defined by the 8th edition of the Novel Coronavirus Pneumonia Diagnosis and Treatment Plan.1
Statistical analysis
A descriptive synthesis of the demographic characteristics, risk factors for disease, severity of disease, and mortality of patients with COVID-19 and SAH (COVID-SAH) was conducted. Continuous variables were reported as mean ± SD or mean (range), while categorical variables were reported as number of patients and their corresponding percentage of total patients.
Where individual patient data (IPD) was provided in studies, subgroup analyses comparing the characteristics of deceased versus survived SAH patients, and severe-to-critical versus mild-to-moderate COVID-19 were conducted. In addition, univariate analysis according to patient characteristics was performed, with results expressed as odds ratios (OR) and 95% confidence intervals (95%CIs).
All analyses were conducted in RStudio (using R-4.0.2) and Review Manager 5.4, with p<0.05 taken to indicate statistical significance.
Results
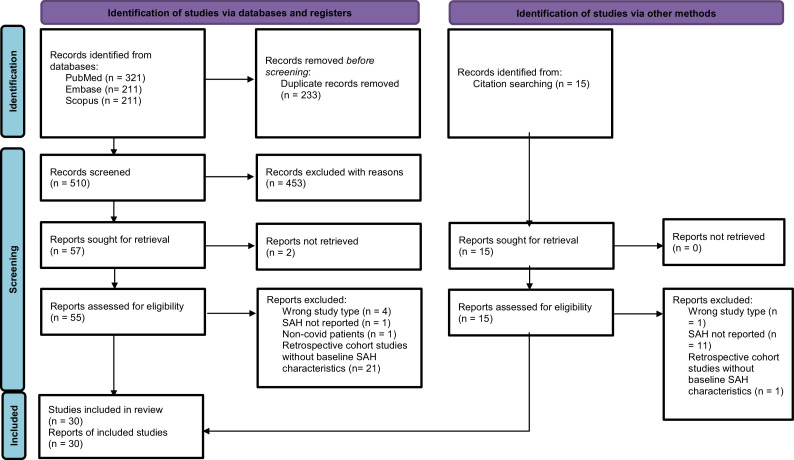
The electronic search strategy retrieved a total of 743 potentially relevant articles (Fig. 1 ). After deduplication and title and abstract screening, 57 articles were sought for full-text eligibility screening, of which 2 articles were not retrievable. Of the 55 articles assessed for eligibility through full-text screening, 27 were excluded with the following criteria: incorrect study type (n = 4), not reporting SAH (n = 1), non-COVID-19 cases (n = 1), and retrospective cohort studies without baseline characteristics of SAH patients (n = 21, comprising 48 patients with SAH). 15 articles identified via citation screening of included articles were sought for retrieval and full-text eligibility screening, of which 2 articles were eventually included for descriptive analysis. Finally, 30 articles were included in the subsequent data extraction and descriptive analysis.
Fig. 1.
PRISMA flowchart of included studies.
Study characteristics
The study characteristics and summary statistics are summarized in Table 1 . Across the 30 articles included in this descriptive analysis (17 case reports, 11 case series, and 2 retrospective studies), a total of 345 COVID-SAH cases were reported.
Table 1.
Baseline characteristics of included studies.
| Authors and study | Location | Study type | Number of COVID-SAH patients (female) | Age (years) | Diabetes Mellitus | Hypertension | Hyperlipidemia | Smoking | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Al Saleigh et al., 2020 | US | Case report | 1 (1) | 31 | 0 | 0 | 0 | 0 |
| 2 | Al-Mufti et al., 2020 | US | Case series | 2 (1) | 31 81 | 0 | 0 | 0 | 0 |
| 3 | Altschul et al., 2020 | US | Case series | 2 (1) | Mean 62 | 1 | 1 | 0 | NR |
| 4 | Avci et al., 2020 | US | Case report | 1 (0) | 50 | NR | NR | NR | NR |
| 5 | Basirjafari et al., 2020 | Iran | Case report | 1 (0) | 9 | 0 | 0 | 0 | 0 |
| 6 | Bradley et al., 2020 | US | Case series | 1 (1) | 76 | 0 | 0 | 1 | 0 |
| 7 | Castillo et al., 2020 | Germany | Case report | 1 (0) | 64 | 0 | 1 | 0 | 1 |
| 8 | Cezar-Junior et al., 2020 | Philippines | Case series | 4 (3) | 36; 53; 61; 71 | NR | NR | NR | NR |
| 9 | Craen et al., 2020 | US | Case report | 1 (1) | 66 | 1 | 1 | 1 | 0 |
| 10 | Dodd et al., 2021 | US | Case series | 10 (5) | NR | 0 | 1 | NR | NR |
| 11 | Esteves-Ordonez et al., 2020 | US | Case report | 1 (1) | 56 | NR | NR | NR | NR |
| 12 | Fabbri et al., 2021 | Italy | Case series | 1 (0) | 74 | 1 | 0 | 0 | 0 |
| 13 | Fayed et al., 2020 | US | Case series | 1 (1) | 54 | 0 | 1 | 0 | 0 |
| 14 | Fernandez et al., 2021 | UK | Case report | 1 (0) | 54 | NR | NR | NR | NR |
| 15 | Gogia et al., 2020 | US | Case report | 1 (0) | 75 | NR | 1 | 1 | 1 |
| 16 | Haider et al., 2020 | Germany | Case report | 1 (0) | 56 | 0 | 1 | 0 | 0 |
| 17 | Harrogate et al., 2020 | UK | Case report | 2 (0) | 74 53 | NR | NR | NR | NR |
| 18 | Kaushik et al., 2020 | US | Case report | 1 (0) | 5 | 0 | 0 | 0 | 0 |
| 19 | Keller et al., 2020 | Switzerland | Case series | 3 (NR) | NR | 2 | 2 | 1 | 1 |
| 20 | Khazaei et al., 2021 | Iran | Case report | 1 (0) | 57 | 1 | 1 | 0 | 0 |
| 21 | Kostrya et al., 2020 | Poland | Case report | 1 (0) | 70 | NR | NR | NR | NR |
| 22 | Li et al., 2020 | China | Case report | 1 (0) | 68 | 0 | 0 | 0 | 0 |
| 23 | Paez et al., 2020 | Ecuador | Case report | 1 (0) | 63 | 0 | 0 | 0 | 1 |
| 24 | Qureshi et al., 2021 | US | Retrospective cohort study | 86 (39) | NR | 29 | 59 | NR | 24 |
| 25 | Ravindra et al., 2021 | US | Retrospective cohort study | 212 (105) | NR | 99 | 122 | 93 | 13 |
| 26 | Rustemi et al., 2020 | Italy | Case report | 1 (1) | 68 | 0 | 0 | 0 | 0 |
| 27 | Sabayan et al., 2020 | Iran | Case series | 1 (0) | 60 | 0 | 1 | 0 | 0 |
| 28 | Saiegh et al., 2020 | US | Caser report | 2 (1) | 31 62 | 0 | 0 | 0 | 0 |
| 29 | Shekhar et al., 2020 | US | Case series | 1 (1) | 38 | 0 | 0 | 0 | 0 |
| 30 | Usman et al., 2020 | US | Case series | 2 (NR) | Mean 53.7 | 0 | 0 | 0 | 0 |
| Total, n (%) | NA | 345 (162, 48.5%) | Mean 55, SD ± 18.4 | 134 (40.9%) | 192 (58.9%) | 97 (40.4%) | 41 (12.62%) | ||
| Study code | Location | Study type | COVID-19 Severity (severe-critical) | Aneurysmal SAH | Anticoagulation | Associated intracranial pathology | Surgical treatment | Deceased | |
| 1 | Al Saleigh et al., 2020 | US | Case report | 0 | 1 | 0 | 1 | 1 | 0 |
| 2 | Al-Mufti et al., 2020 | US | Case series | 0 | 0 | NR | 0 | NR | NR |
| 3 | Altschul et al., 2020 | US | Case series | 0 | NR | 1 | NR | 0 | 0 |
| 4 | Avci et al., 2020 | US | Case report | 1 | NR | NR | 0 | NR | 1 |
| 5 | Basirjafari et al., 2020 | Iran | Case report | 1 | 0 | NR | 0 | 0 | 1 |
| 6 | Bradley et al., 2020 | US | Case series | NR | NR | 0 | NR | NR | 1 |
| 7 | Castillo et al., 2020 | Germany | Case report | 0 | 0 | 0 | 0 | 0 | 0 |
| 8 | Cezar-Junior et al., 2020 | Philippines | Case series | 3 | 1 | NR | 2 | 2 | 1 |
| 9 | Craen et al., 2020 | US | Case report | 1 | 0 | NR | 0 | 0 | 1 |
| 10 | Dodd et al., 2021 | US | Case series | 4 | 10 | NR | NR | 3 | 2 |
| 11 | Esteves-Ordonez et al., 2020 | US | Case report | 0 | 1 | 0 | 0 | 1 | 0 |
| 12 | Fabbri et al., 2021 | Italy | Case series | NR | 0 | 0 | 1 | NR | 1 |
| 13 | Fayed et al., 2020 | US | Case series | 1 | 0 | 1 | 0 | NR | 1 |
| 14 | Fernandez et al., 2021 | UK | Case report | 1 | NR | 1 | 0 | 0 | 1 |
| 15 | Gogia et al., 2020 | US | Case report | 1 | NR | 1 | 0 | 0 | 1 |
| 16 | Haider et al., 2020 | Germany | Case report | 0 | 0 | 1 | 0 | 0 | 0 |
| 17 | Harrogate et al., 2020 | UK | Case report | 2 | NR | 2 | 0 | 0 | 0 |
| 18 | Kaushik et al., 2020 | US | Case report | 1 | 0 | 1 | 0 | 0 | 1 |
| 19 | Keller et al., 2020 | Switzerland | Case series | 3 | NR | 3 | 2 | NR | 1 |
| 20 | Khazaei et al., 2021 | Iran | Case report | 0 | 0 | 1 | 1 | 0 | 0 |
| 21 | Kostrya et al., 2020 | Poland | Case report | NR | 1 | NR | 0 | 1 | 0 |
| 22 | Li et al., 2020 | China | Case report | 1 | 0 | 1 | 0 | 0 | 1 |
| 23 | Paez et al., 2020 | Ecuador | Case report | NR | 1 | 1 | 1 | 0 | 1 |
| 24 | Qureshi et al., 2021 | US | Retrospective cohort study | 75 | NR | NR | NR | 2 | 27 |
| 25 | Ravindra et al., 2021 | US | Retrospective cohort study | 144 | NR | 155 | NR | NR | 91 |
| 26 | Rustemi et al., 2020 | Italy | Case report | NR | 1 | 1 | 0 | 0 | 0 |
| 27 | Sabayan et al., 2020 | Iran | Case series | 1 | NR | 0 | NR | NR | 1 |
| 28 | Saiegh et al., 2020 | US | Caser report | NR | 1 | 0 | 2 | 2 | 0 |
| 29 | Shekhar et al., 2020 | US | Case series | NR | NR | 0 | NR | NR | 1 |
| 30 | Usman et al., 2020 | US | Case series | 0 | NR | 2 | 1 | NR | 1 |
| Total, n (%) | NA | 242 (73.8%) | 17 (56.7%) | 172 (71.4%) | 11 (35.5%) | 12 (10.8%) | 136 (40.8%) |
As not all studies provided demographic details of patients, summary statistics were derived using only studies which clearly reported details of all patients. The mean age was 55 ±18.4 years and 162 out of 334 (48.5%) patients were female. 192 out of 326 patients (55.9%) had hypertension, 97 out of 240 (40.4%) had hyperlipidemia, 134 out of 328 (40.6%) had diabetes mellitus, and 41 out of 325 (12.6%) were smokers. 242 out of 328 patients (73.8%) had severe-to-critical COVID-19. 17 out of 30 patients (56.7%) had aneurysmal SAH, 172 out of 241 patients (71.4%) were on anticoagulation therapy, and 11 out of 31 patients (35.5%) had associated intracranial pathology. 12 out of 111 patients (10.8%) underwent surgical treatment, and 136 out of 333 patients (40.8%) were deceased.
Geographical characteristics of COVID-SAH cases
The geographical characteristics of COVID-SAH cases are summarized in Table 2 . 325 cases (94.2%) were reported in US, of which 228 out of 321 (71.0%) had severe-to-critical COVID-19. 9 cases (2.6%) were reported in Europe, of which 3 out of 5 had severe-to-critical COVID-19. 3 cases (0.9%) were reported in UK, of which all 3 (100.0%) had severe-to-critical COVID-19. 8 cases (2.3%) were reported in Asia, of which 6 (75.0%) had severe-to-critical COVID-19.
Table 2.
Results by geographic location.
| Total patients | Severe-to-critical COVID-19 | |
|---|---|---|
| US | 325 (94.2%) | 228/321 (71.0%) |
| Europe | 9 (2.6%) | 3/5 (60.0%) |
| UK | 3 (0.9%) | 3/3 (100.0%) |
| Asia | 8 (2.3%) | 6/8 (75.0%) |
Survived versus deceased COVID-SAH cases
The subgroup analyses comparing outcomes of survived vs deceased patients are summarized in Table 3 . A total of 138 patients (56.3%) survived, whilst 207 patients (43.7%) died. IPD was reported in up to 18 survivors and 15 deceased. Among the deceased, 11 of 11 patients (100.0%) had severe-to-critical COVID-19, as compared to 7 out of 13 patients (53.9%) among the survivors. Aneurysmal SAH was found in 6 out of 11 survivors (54.6%), whilst non-aneurysmal SAH was found in 6 out of 7 deceased (85.7%). 7 out of 13 survivors (53.9%) and 6 out of 12 deceased were on anticoagulation. Among the survivors, 7 out of 16 patients (43.8%) had associated intracranial pathology, as compared with 4 out of 13 patients (30.8%) among the survivors. Among the survivors, 6 out of 14 patients (42.9%) had undergone surgical treatment, as compared with 1 out of 8 patients (12.5%) among the deceased.
Table 3.
Results comparing Survived vs Deceased.
| Survived | Deceased | |
|---|---|---|
| Total patients, n (%) | 138 (56.3%) | 107 (43.7%) |
| Age (years), mean (SD) | 56 (±14.8) | 54 (±20.9) |
| Female, n (%) | 6 (40.0%) | 6 (42.9%) |
| Hypertension, n (%) | 5 (45.5%) | 5 (41.7%) |
| Hyperlipidemia, n (%) | 1 (9.09%) | 3 (25%) |
| Diabetes Mellitus, n (%) | 3 (27.3%) | 4 (33.3%) |
| Smoking, n (%) | 1 (9.09%) | 2 (16.7%) |
| Severe-critical COVID-19, n (%) | 7 (53.8%) | 11 (100.0%) |
| Aneurysmal, n (%) | 6 (54.5%) | 1 (14.3%) |
| Anticoagulation, n (%) | 7 (53.8%) | 6 (50%) |
| Associated intracranial pathology, n (%) | 7 (43.8%) | 4 (30.8%) |
| Surgical treatment, n (%) | 6 (42.9%) | 1 (12.5%) |
The univariate analyses of patient and SAH characteristics associated with death are summarized in Table 4 . Based on the results, hypertension (OR=0.75, 95% CI, 0.14-3.88, p = 0.729), diabetes mellitus (OR=0.80, 95% CI, 0.12-5.39, p = 0.813), and the use of anticoagulation (OR=0.86, 95% CI 0.17-4.18, p = 0.848) were not significant risk factors for mortality in COVID-SAH. The odds of aneurysmal SAH leading to mortality were not significant (OR=0.14, 95% CI 0.01-1.21, p = 0.111), and surgical treatment was not significantly associated with lower mortality rates (OR=0.19, 95% CI 0.01-1.51, p = 0.166).
Table 4.
Univariate analysis of characteristics in deceased patients.
| Odds Ratio (95% CI) | p-value | |
|---|---|---|
| Age ≥60 | 1.00 (0.23-4.26) | >0.99 |
| Female gender | 1.12 (0.25-5.05) | 0.876 |
| Hypertension | 0.75 (0.14-3.88) | 0.729 |
| Hyperlipidemia | 3.00 (0.32-66.6) | 0.375 |
| Diabetes Mellitus | 0.80 (0.12-5.39) | 0.813 |
| Smoking | 3.00 (0.32-66.6) | 0.375 |
| Aneurysmal SAH | 0.14 (0.01-1.21) | 0.111 |
| Anticoagulation | 0.86 (0.17-4.18) | 0.848 |
| Associated intracranial pathology | 0.57 (0.11-2.60) | 0.476 |
| Surgical treatment | 0.19 (0.01-1.51) | 0.166 |
Mild-to-moderate versus severe-to-critical COVID-19 in COVID-SAH cases
The results of the subgroup analysis comparing outcomes of mild-moderate vs severe-critical COVID-19 are summarized in Table 5 . A total of 75 patients (31.5%) had mild-to-moderate COVID-19, whilst 163 patients (68.5%) had severe-to-critical COVID-19. IPD was reported in up to 7 and 16 patients with mild-to-moderate and severe-to-critical COVID-19, respectively, allowing for the following subgroup analyses. 6 out of 6 patients (100.0%) with mild-to-moderate COVID-19 had survived, whilst 11 out of 18 patients (61.1%) with severe-to-critical COVID-19 passed away. Among patients with severe-to-critical COVID-19, 8 out of 8 (100.0%) had non-aneurysmal SAH, as compared to 3 out of 6 (50.0%) in the mild-to-moderate subgroup.
Table 5.
Results comparing Mild-to-moderate vs Severe-to-critical COVID-19.
| Mild-moderate | Severe-critical | |
|---|---|---|
| Total patients, n (%) | 75 (31.5%) | 163 (68.5%) |
| Age (years), mean (SD) | 48 (±13.7) | 56, (±20.4) |
| Female, n (%) | 4 (57.1%) | 5 (31.3%) |
| Hypertension, n (%) | 3 (50.0%) | 7 (58.3%) |
| Hyperlipidemia, n (%) | 0 (0.0%) | 3 (25.0%) |
| Diabetes Mellitus, n (%) | 2 (33.3%) | 3 (25.0%) |
| Smoking, n (%) | 1 (16.7%) | 1 (8.3%) |
| Aneurysmal, n (%) | 3 (50.0%) | 0 (0.0%) |
| Anticoagulation, n (%) | 2 (40.0%) | 9 (75.0%) |
| Associated intracranial pathology, n (%) | 2 (33.3%) | 4 (22.2%) |
| Surgical treatment, n (%) | 3 (50.0%) | 1 (9.1%) |
| Deceased, n (%) | 0 (0.0%) | 11 (61.1%) |
Discussion
There was a total of 345 COVID-SAH cases reported in the international literature at the time of analysis. This may be underreported, when considering the global decrease in admissions for SAH during the pandemic, attributable to an avoidance in seeking medical care owing to fear of contracting COVID-19.23 , 35 Whilst most (94.2%) of the COVID-SAH cases were reported in the US, this does not reflect the geographical incidence of SAH, known to be highest in Finland and Japan.16 , 24 This could be due to the relatively larger distribution of COVID-19 in US. The mean age of COVID-SAH patients was 55 years-old, in keeping with the peak age of SAH known to be between 50 and 60 years-old.7 Among modifiable risk factors for SAH, hypertension and smoking were apparent in 58.9% and 12.6% the COVID-SAH cohort, respectively. In comparison with non-COVID SAH cohorts, the percentage of hypertensives is lower at 28.0%, whilst the percentage of smokers is higher at 43.0%.4 The predisposition in SAH for the female gender was not apparent in the COVID-SAH cohort, as 48.5% were female.7 Further, whilst the composition of SAH in COVID patients was predominantly aneurysmal (56.7%), it was significantly less than the baseline epidemiology of aneurysmal SAH (85.0% of SAH cases).34
The mortality rate of COVID-SAH patients was 40.8%, in keeping with the literature on SAH mortality.13 This is slightly less than the mortality rates of COVID-19 patients with intracranial hemorrhage (49.0%)3 , 6 comparing the deceased versus survived subgroups, a higher proportion of deceased patients had severe-to-critical COVID-19 (100.0% versus 53.8%) and non-aneurysmal SAH (85.7% versus 44.6%).
Severe-to-critical COVID-19 was the most prevalent factor in COVID-SAH patients (73.8%) and in deceased patients (100.0%). This is consistent with previous literature that have established relationships between severe COVID-19 and neurological manifestations, as well as poorer outcomes.19 The association between severe-to-critical COVID-19 and SAH could possibly be contributed to by the higher rate of anticoagulation therapy in severe-to-critical COVID-19 patients (75.0% versus 40.0%), thereby increasing the risk of SAH.34 Another mechanism that may contribute to coagulopathy in COVID-19 is viral infection of endothelial cells and infiltration with inflammatory cytokines, leading to endothelial injury and coagulopathy.11 The association with death may be contributed to by the higher prevalence of cardiovascular risk factors in severe-to-critical COVID-19 patients, predisposing to systemic disease and poorer outcomes.12
COVID-SAH patients with non-aneurysmal SAH had a higher mortality rate as compared to aneurysmal SAH (54.6% versus 16.7%). This is unexpected, considering that non-aneurysmal SAH is known to have a much better prognosis than aneurysmal SAH.18 , 29 This could be explained by the higher proportion of severe-to-critical COVID-19 patients in the non-aneurysmal SAH subgroup (72.7%), compared to the aneurysmal SAH subgroup (0.0%). In a case series of aneurysmal SAH in COVID-19 patients, 80% of participants were less than 50 years-old, relatively younger than the expected mean age of ruptured aneurysms in non-COVID-19 patients.8 The younger age found in aneurysmal SAH may explain the milder severity of COVID-19 found in these patients. An important caveat to the aforementioned points is that a low number of patients in included studies (12 out of 111) underwent surgical treatment. As mortality naturally increases without surgical treatment to control bleeding and prevent aneurysmal re-rupture, these results do not provide much weight in favor of a COVID-19-specific pathophysiological mechanism contributing to increased mortality.
Along this line, it remains contentious whether COVID-19 is a true cause of SAH. While SAH cases are mainly aneurysmal,34 our findings highlight that the majority of reports of COVID-SAH are non-aneurysmal in nature. One of the reports included a 31-year-old patient with reversible cerebral vasoconstriction syndrome with convexity of SAH in setting of intra-cranial and extra-cranial dissection, as well as an 81-year-old patient also with extra and intra-cranial dissection with diffuse SAH. The two patients had no known risk factors indicative of cerebral dissection such as connective tissue disorders or vasculopathies which could have contributed to the dissection. Furthermore, there was a report of a 9-year-old boy who upon autopsy, had no lesions in the anatomical pathways of cerebral arteries, leading to speculation that the infection may have caused SAH through abnormal coagulation pathways or a cytokine storm. This raises the possibility of COVID-19 being a contributing factor towards the development of spontaneous SAH. Further epidemiological studies in population-based cohorts may be important to further investigate this hypothesis.9 Considering that 71.4% of COVID-SAH patients included in our study were on anticoagulation and despite the non-significant association of anticoagulation use with mortality (OR=0.86, 95%CI=0.17-4.18, p = 0.848), the risk of SAH as a complication of therapeutic anticoagulation therapy in COVID-19 patients cannot be ruled out due to the small sample size analyzed, and hence should be further investigated. This risk should be carefully considered when assessing the mortality benefit of therapeutic anticoagulation in COVID-19 patients, for which evidence from trials is lacking or indeterminate at present.10 , 31
The main strength of this study lies in the systematic review and consolidation of international data on the specific cohort of COVID-19 patients with SAH. This has allowed for deeper analysis by subgroups and better understanding of the impact of COVID-19 on SAH and its characteristics.
As this was a systematic review of mostly case reports, a formal meta-analysis could not be conducted to provide more robust evidence of the association between SAH and COVID-19. Prevalence of concomitant COVID-19 and SAH cases among a general population was reported infrequently among studies, precluding the use of a meta-analysis of incidence rates. Data was also especially lacking in continents outside the US, and further studies are needed to verify that the present results are generalizable to a worldwide population. Variations in healthcare systems and standards of living worldwide will also add considerable heterogeneity to such an analysis.
The gravity of our findings is also limited by the number of cases with IPD reported. Statistical significance was not observed in any of the univariate analyses of factors affecting mortality or COVID-19 severity. Although this could truly reflect null effect, the low number of patients included in the analysis is likely to have contributed to the lack of significance, and quality of evidence is very low as a result. Further, there was insufficient information to categorize COVID-SAH cases according to SAH grading scales for severity or complications (such as Hunt and Hess, World Federation of Neurological Surgeons, and Fisher), which would provide insight to the severity of SAH with concomitant COVID-19.
Additionally, publication bias may have influenced the number and types of reports in this topic, especially because COVID-19 is a heated area of research globally. Moreover, within these studies, there was heterogeneity in the variables reported, limiting the representativeness of proportions analyzed to only what was reported.
Finally, COVID-19 is an ever-changing phenomenon. With the emergence of new variants which have demonstrated enhanced infectious patterns and different receptor binding affinities to earlier variants,14 , 17 , 33 it remains unclear whether these variants will impact the prevalence, severity, and outcomes of SAH in COVID-19 patients, and renders challenge to finding an association between COVID-19 and SAH.
Conclusion
SAH is a rare but morbid occurrence in patients with COVID-19. The mortality rate of COVID-SAH patients was 40.8%, with a higher prevalence of severe-to-critical COVID-19 (100% versus 53.8%) and non-aneurysmal SAH (85.7% versus 44.6%) among COVID-SAH deaths. However, the strength of this evidence is low, due the sparse number of studies and the ever-changing nature of the virus. Further studies investigating the association between COVID-19 and SAH may be warranted to identify the long-term effects of COVID-19.
Statements & declarations
The authors report no conflict of interest. No funding was received for conducting this study.
Declaration of Competing Interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper. No funding was received for conducting this study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jstrokecerebrovasdis.2022.106904.
Appendix. Supplementary materials
References
- 1.Diagnosis and treatment protocol for COVID-19 patients (Tentative 8th Ed.) Infect Dis Immun. 2021;1(1):8–16. doi: 10.1097/01.ID9.0000733564.21786.b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barouch D.H. Covid-19 vaccines — immunity, variants, boosters. N Engl J Med. 2022;387(11):1011–1020. doi: 10.1056/NEJMra2206573. 2022/09/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beyrouti R., Best J.G., Chandratheva A., Perry R.J., Werring D.J. Characteristics of intracerebral haemorrhage associated with COVID-19: a systematic review and pooled analysis of individual patient and aggregate data. J Neurol. 2021;268(9):3105–3115. doi: 10.1007/s00415-021-10425-9. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bonita R. Cigarette smoking, hypertension and the risk of subarachnoid hemorrhage: a population-based case-control study. Stroke. 1986;17(5):831–835. doi: 10.1161/01.str.17.5.831. [DOI] [PubMed] [Google Scholar]
- 5.Cezar-Junior A.B., et al. Subarachnoid hemorrhage and COVID-19: association or coincidence? Medicine. 2020;99(51):e23862. doi: 10.1097/MD.0000000000023862. English. (Baltimore)-e238622020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheruiyot I., et al. Intracranial hemorrhage in coronavirus disease 2019 (COVID-19) patients. Neurolog Sci. 2021;42(1):25–33. doi: 10.1007/s10072-020-04870-z. 2021/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Rooij N.K., Linn F.H.H., van der Plas J.A., Algra A., Rinkel G.J.E. Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg AMP Psychiatry. 2007;78(12):1365–1372. doi: 10.1136/jnnp.2007.117655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodd W.S., et al. Aneurysmal subarachnoid hemorrhage in patients with coronavirus disease 2019 (COVID-19): a case SERIES. World Neurosurg. 2021;153:e259–e264. doi: 10.1016/j.wneu.2021.06.092. 2021/09/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feigin V.L., et al. Risk factors for subarachnoid hemorrhage. Stroke. 2005;36(12):2773–2780. doi: 10.1161/01.STR.0000190838.02954.e8. [DOI] [PubMed] [Google Scholar]
- 10.Goligher E.C., et al. Therapeutic anticoagulation with heparin in critically Ill patients with COVID-19. N Engl J Med. 2021;385(9):777–789. doi: 10.1056/NEJMoa2103417. eng. Aug 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goshua G., et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7(8):e575–e582. doi: 10.1016/S2352-3026(20)30216-7. eng. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grasselli G., et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020;180(10):1345–1355. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hop J.W., Rinkel G.J.E., Algra A., Gijn J.V. Case-fatality rates and functional outcome after subarachnoid hemorrhage. Stroke. 1997;28(3):660–664. doi: 10.1161/01.str.28.3.660. [DOI] [PubMed] [Google Scholar]
- 14.Karim S.S.A., Karim Q.A. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–2128. doi: 10.1016/S0140-6736(21)02758-6. Dec 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368(6493):860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linn F.H.H., Rinkel G.J.E., Algra A., Gijn J.V. Incidence of subarachnoid hemorrhage. Stroke. 1996;27(4):625–629. doi: 10.1161/01.str.27.4.625. [DOI] [PubMed] [Google Scholar]
- 17.Liu H., et al. The lambda variant of SARS-CoV-2 has a better chance than the delta variant to escape vaccines. bioRxiv. 2021;457692:2021. 08.25. [Google Scholar]
- 18.Long B., Koyfman A., Runyon M.S. Subarachnoid hemorrhage: updates in diagnosis and management. Emerg Med Clin N Am. 2017;35(4):803–824. doi: 10.1016/j.emc.2017.07.001. Nov. [DOI] [PubMed] [Google Scholar]
- 19.Mao L., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montalvan V., Lee J., Bueso T., De Toledo J., Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin Neurol Neurosurg. 2020;194 doi: 10.1016/j.clineuro.2020.105921. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moola S., et al. Systematic reviews of etiology and risk. JBI Evid Synth. 2020 [Google Scholar]
- 22.Munn Z., et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–2133. doi: 10.11124/JBISRIR-D-19-00099. Oct. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen T.N., et al. Abstract 14: global impact of the COVID-19 pandemic on subarachnoid hemorrhage. Stroke. 2021;52(Suppl_1):A14. -A14. [Google Scholar]
- 24.Ohkuma H., Fujita S., Suzuki S. Incidence of aneurysmal subarachnoid hemorrhage in Shimokita, Japan, from 1989 to 1998. Stroke. 2002;33(1):195–199. doi: 10.1161/hs0102.101891. [DOI] [PubMed] [Google Scholar]
- 25.Page M.J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pajo A.T., Espiritu A.I., Apor A.D.A.O., Jamora R.D.G. Neuropathologic findings of patients with COVID-19: a systematic review. Neurolog Sci. 2021;42(4):1255–1266. doi: 10.1007/s10072-021-05068-7. 2021/04/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qureshi A.I., et al. Subarachnoid Hemorrhage and COVID-19: an analysis of 282,718 patients. World Neurosurg. 2021;151:e615–e620. doi: 10.1016/j.wneu.2021.04.089. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ravindra V.M., et al. Impact of COVID-19 on the hospitalization, treatment, and outcomes of intracerebral and subarachnoid hemorrhage in the United States. PLoS One. 2021;16(4) doi: 10.1371/journal.pone.0248728. English. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rinkel G.J.E., et al. Outcome in patients with subarachnoid haemorrhage and negative angiography according to pattern of haemorrhage on computed tomography. Lancet N Am Ed. 1991;338(8773):964–968. doi: 10.1016/0140-6736(91)91836-j. 1991/10/19/ [DOI] [PubMed] [Google Scholar]
- 30.Sachs J.D., et al. The lancet commission on lessons for the future from the COVID-19 pandemic. Lancet N Am Ed. 2022;400(10359):1224–1280. doi: 10.1016/S0140-6736(22)01585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Talasaz A.H., et al. Recent randomized trials of antithrombotic therapy for patients with COVID-19: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(15):1903–1921. doi: 10.1016/j.jacc.2021.02.035. eng. Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan Y.K., et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis. 2020;50(3):587–595. doi: 10.1007/s11239-020-02228-y. eng. Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teyssou E., et al. The delta SARS-CoV-2 variant has a higher viral load than the Beta and the historical variants in nasopharyngeal samples from newly diagnosed COVID-19 patients. J Infect. 2021 doi: 10.1016/j.jinf.2021.08.027. 2021/08/19/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Gijn J., Kerr R.S., Rinkel G.J.E. Subarachnoid haemorrhage. Lancet North Am Ed. 2007;369(9558):306–318. doi: 10.1016/S0140-6736(07)60153-6. 2007/01/27/ [DOI] [PubMed] [Google Scholar]
- 35.Westgard B.C., Morgan M.W., Vazquez-Benitez G., Erickson L.O., Zwank M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020;76(5):595–601. doi: 10.1016/j.annemergmed.2020.06.019. 2020/11/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.