Abstract
Aim
In this study, we examine the effect of a high-performance cardiopulmonary resuscitation (HP-CPR) protocol on patient outcomes following out-of-hospital cardiac arrests (OHCA) witnessed by emergency medical services (EMS) personnel.
Methods
We performed a retrospective cohort study of adult, EMS witnessed OHCA patients of medical aetiology in Victoria, Australia. Patients treated after the introduction of a HP-CPR protocol and training programme between February 2019 and January 2020 were compared to historical controls between January 2015 and January 2019. The effect of a HP-CPR protocol on survival to hospital discharge was examined using logistic regression models adjusted for arrest factors.
Results
A total of 1,561 and 420 EMS witnessed OHCA patients were treated in the control and intervention periods, respectively. Baseline characteristics were mostly balanced across study periods, except for an initial arrest rhythm of asystole which was more frequent during the intervention period (20.2% vs 15.9%; p-value = 0.04). Unadjusted survival to hospital discharge was similar across control and intervention periods for the overall population (32.1% vs 29.4%, p-value = 0.27), but significantly higher during the intervention period for initial shockable arrests (76.9% vs 66.6%; p-value = 0.03). After adjustment for confounders, cases in the intervention period were associated with an improvement in the adjusted odds of survival to hospital discharge for overall arrests (adjusted odds ratio [AOR] 1.37, 95% CI: 1.00–1.88) and initial shockable arrests (AOR 1.70, 95% CI: 1.03–2.82).
Conclusion
The implementation of a HP-CPR protocol was associated with a significant improvement in survival from EMS witnessed OHCA. Efforts to improve CPR performance could yield further improvements in patient outcomes.
Keywords: Cardiac arrests, Emergency medical services, Cardiopulmonary resuscitation, Survival
Introduction
Out-of-hospital cardiac arrest (OHCA) witnessed by emergency medical service (EMS) providers is associated with higher rates of survival and neurological recovery.1 This may be due to the elimination of the EMS response interval and therefore, the immediate application of life-saving measures. However, survival to hospital discharge for this group remains disappointedly low with a pooled global estimate of only 20%.2
Recently, there has been growing interest in the advantages of high-quality prehospital resuscitative efforts to achieve optimal OHCA outcomes.3 High-performance cardiopulmonary resuscitation (HP-CPR) practices have been implemented by a number of international EMS systems,4, 5 and typically include the collective strategies of team-based training, real-time feedback on CPR performance, structured choreography and scene leadership, and post-event debriefing. Although some reports have demonstrated significant improvements in patient outcomes, the majority are focussed on initial shockable arrests or non-EMS witnessed populations.4, 5 To date, there are no reports that have examined the value of HP-CPR in EMS witnessed OHCA populations.3 As the majority of EMS witnessed OHCA survivors achieve a return of spontaneous circulation (ROSC) within the first cycle of CPR/defibrillation,1 the value of HP-CPR in these populations is less certain.
Our EMS system adopted HP-CPR in 2019, and showed a significant increase in the risk-adjusted odds of survival for OHCA patients not witnessed by EMS personnel.5 In this study, we examine the effect of the HP-CPR protocol on patient outcomes following OHCA witnessed by EMS personnel.
Methods
Study design
A retrospective cohort study was performed using data from the Victorian Ambulance Cardiac Arrest Registry (VACAR). We included adult (aged ≥ 16 years) OHCA patients witnessed to arrest by EMS personnel and who received an attempted resuscitation by EMS between 1st January 2015 and 31th January 2020. We excluded patients of traumatic aetiology. Ethical approval for this study was obtained from the Monash University Human Research Ethics Committee (#21046).
Setting & data sources
The study was conducted in Victoria, a state of Australia that had a population of approximately 6.1 million people. Ambulance Victoria is the sole provider of EMS in the state.6 Data for this study were extracted from the VACAR, which has been described in detail elsewhere.7 More than 150 data elements are collected by VACAR, including the Utstein-style descriptors, prehospital treatment data, hospital outcome data and in-field quality CPR data (since February 2019).5
Intervention
The implementation of HP-CPR in Victoria has been described in detail elsewhere.5 This study consisted of two periods, a control period (1st January 2015 to 31st January 2019) and an intervention period (1st February 2019 to 31st January 2020) which followed the introduction of a HP-CPR protocol. During the intervention period, the HP-CPR protocol resulted in 1) the introduction of a resuscitation checklist and a designated team leader guiding the flow of the resuscitation, 2) training in resuscitation choreography with designated team roles, 3) the use of real-time CPR monitoring and feedback, and 4) post-event team performance debrief reports. Paramedics received a 4-hour training programme for HP-CPR undertaken over a four-month period (October 2018 to January 2019) prior to its launch, and ‘refresher’ education was again provided in the second half of 2019.
Statistical analysis
All analyses were conducted using Stata 14 (StataCorp, USA) and p-values less than 0.05 were considered statistically significant. The primary study outcome was survival to hospital discharge. Secondary outcomes included event survival (pulse present on hospital arrival) and prehospital ROSC. Differences in arrest characteristics, unadjusted outcomes, out-of-hospital interventions, and CPR quality metrics were assessed using the Chi-squared test, Fisher’s exact test, and Mann-Whitney test, as appropriate.
To examine the impact of the HP-CPR on survival outcomes, we used multivariable logistic regression models adjusting for age in years, male gender, arrest in a public location, arrest aetiology (i.e., cardiac, respiratory, and other), initial arrest rhythm, metropolitan region, and seasonality. We examined the presence of a temporal trend in the control period, and there were no temporal changes in outcomes from medical OHCA; therefore, we did not adjust for the trends in our logistic regression models. The intervention effect was assessed by including an indicator variable in the model denoting the commencement of the intervention period (binary term). As paramedics were being trained in the programme between October 2018 and January 2019, we censored these months from all models to avoid early contamination of the intervention during the control period. We also conducted subgroup analyses according to the initial arrest rhythm (e.g. shockable and non-shockable arrests) to determine whether the changes in protocol might have had heterogeneous effects in these subgroups.
Results
A total of 25,415 non-traumatic OHCAs were attended by EMS during the study period, of which 2,466 (9.7%) were EMS witnessed. Of the attended EMS witnessed cases, 1,981 (80.3%) received an EMS-attempted resuscitation [1,561 (78.8%) and 420 (21.2%) occurred during the control and intervention periods, respectively] (Figure S1).
Arrest characteristics
Baseline characteristics were mostly balanced across study periods, except for an initial arrest rhythm of asystole which was more frequent during the intervention period (20.2% vs 15.9%; p-value = 0.04) (Table 1). Unadjusted survival to hospital discharge was similar across the study periods for the overall population (32.1% vs 29.4%, p-value = 0.27) and initial non-shockable arrests (12.2% vs 10.7%; p-value = 0.46), but significantly higher during the intervention period for initial shockable arrests (76.9% vs 66.6%; p-value = 0.03). There were no differences in the unadjusted rate of event survival and prehospital ROSC across the intervention and control periods in the overall population (49.1% vs 50.0%; p-value = 0.74 and 57.1% vs 61.1%; p-value = 0.14, respectively), initial non-shockable arrests (33.8% vs 34.9%; p-value = 0.74 and 43.9% vs 48.9%; p-value = 0.14, respectively) and initial shockable arrests (82.4% vs 78.8%; p-value = 0.38 and 86.6% vs 84.9%; p-value = 0.66, respectively).
Table 1.
Demographics of EMS-treated OHCA patients across the control and intervention periods.
|
Overall |
Control period | Intervention period | Differences (95% CI) | P-value | Missing | |
|---|---|---|---|---|---|---|
| n = 1,981 | n = 1,561 | n = 420 | ||||
| Age in years, median (IQR) | 69.0 (56.0, 80.0) | 69.0 (56.0, 80.0) | 69.0 (57.0, 79.0) | 0 (−2.8 to 2.8) | 0.97 | 0 |
| Male, n (%) | 1,270 (64.2) | 1,017 (65.2) | 253 (60.5) | −4.7 (−9.9 to 0.6) | 0.08 | 3 (0.2) |
| Public location, n (%) | 145 (7.3) | 117 (7.5) | 28 (6.7) | −0.8 (−3.5 to 1.9) | 0.56 | 0 |
| Presumed cardiac aetiology, n (%) | 1,567 (79.1) | 1,235 (79.1) | 332 (79.1) | −0.1 (−4.5 to 4.3) | 0.98 | 0 |
| Initial arrets rhythm, n (%) | 38 (1.9) | |||||
| Shockable | 637 (32.8) | 518 (33.7) | 119 (29.3) | −4.4 (−9.4 to 0.6) | 0.09 | |
| Pulseless electrical activity | 975 (50.2) | 770 (50.1) | 205 (50.5) | 0.4 (−5.1 to 5.9) | 0.89 | |
| Asystole | 327 (16.8) | 245 (15.9) | 82 (20.2) | 4.3 (−0.1 to 8.6) | 0.04 | |
| Unknown, Non-shockable | 4 (0.2) | 4 (0.3) | 0 | −0.3 (−0.5 to 0) | 0.59 | |
| Metropolitan, n (%) | 1,330 (67.1) | 1,042 (66.8) | 288 (68.6) | 1.8 (−3.2 to 6.8) | 0.48 | 0 |
| Season, n (%) | 0 | |||||
| Summer | 497 (25.1) | 393 (25.2) | 104 (24.8) | −0.4 (−5.1 to 4.2) | 0.86 | |
| Autumn | 480 (24.2) | 364 (23.3) | 116 (27.6) | 4.3 (−0.5 to 9.1) | 0.07 | |
| Winter | 501 (25.3) | 399 (25.6) | 102 (24.3) | −1.3 (−5.9 to 3.4) | 0.59 | |
| Spring | 503 (25.4) | 405 (25.9) | 98 (23.3) | −2.6 (−7.2 to 2.0) | 0.28 | |
| Scene outcomes, n (%) | 0 | |||||
| Died at scene or transit | 791 (39.9) | 613 (39.3) | 178 (42.4) | 3.1 (−2.2 to 8.4) | 0.25 | |
| Transported with CPR | 201 (10.2) | 171 (11.0) | 30 (7.1) | −3.8 (−6.7 to −0.9) | 0.02 | |
| Transported with ROSC | 989 (49.9) | 777 (49.8) | 212 (50.5) | 0.7 (−4.7 to 6.1) | 0.80 | |
| Survival outcomes, n (%) | ||||||
| Pre-hospital ROSC | 1,194 (60.3) | 954 (61.1) | 240 (57.1) | −4.0 (−9.3 to 1.3) | 0.14 | 0 |
| Event survival | 985 (49.8) | 779 (50.0) | 206 (49.1) | −0.9 (−6.3 to 4.5) | 0.74 | 2 (0.1) |
| Discharged alive | 586 (29.9) | 452 (29.4) | 134 (32.1) | 2.8 (−2.2 to 7.8) | 0.27 | 24 (1.2) |
IQR stands for interquartile range; EMS, emergency medical services; and ROSC, return of spontaneous circulation.
Proportion excluded the missing value.
Resuscitation interventions & CPR quality
During the intervention period, patients were more likely to receive laryngeal mask airway (62.1% vs 54.5%; p-value = 0.005) and were less likely to receive crystalloid fluid (46.9% vs 61.6%; p-value < 0.001) (Table 2). In the intervention period, the real-time quality data were available in 174 (40.7%) cases. The median chest compression fraction was 89.4% (interquartile ranges [IQR]: 80.4, 92.8), compression depth was 5.8 centimetres (IQR: 5.2, 6.5), and the compression rate was 116 compression per minute (IQR: 111, 121).
Table 2.
Resuscitation interventions in EMS-treated OHCA across the control and intervention periods.
| Overall | Control period | Intervention period | Differences (95% CI) | P-value | Missing | |
|---|---|---|---|---|---|---|
| n = 1,981 | n = 1,561 | n = 420 | ||||
| Interventions, n (%) | ||||||
| CPR | 1,855 (93.6) | 1,462 (93.7) | 393 (93.6) | −0.1 (−2.7 to 2.6) | 0.95 | 0 |
| Defibrillation | 849 (42.9) | 666 (42.7) | 183 (43.6) | 0.9 (−4.4 to 6.2) | 0.74 | 0 |
| Intubation attempted | 849 (42.9) | 685 (43.9) | 164 (39.1) | −4.8 (−10.1 to 0.4) | 0.08 | 0 |
| Laryngeal mask airway attempted | 1,111 (56.1) | 850 (54.5) | 261 (62.1) | 7.7 (2.4 to 12.9) | 0.005 | 0 |
| Epinephrine | 1,265 (63.9) | 991 (63.5) | 274 (65.2) | 1.8 (−3.4 to 6.9) | 0.51 | 0 |
| Amiodarone | 226 (11.4) | 184 (11.8) | 42 (10.0) | −1.8 (−5.1 to 1.5) | 0.31 | 0 |
| Crystalloid fluid | 1,159 (58.5) | 962 (61.6) | 197 (46.9) | −14.7 (−20.1 to − 9.4) | <0.001 | 0 |
| Number of defibrillations, median (IQR)a | ||||||
| Overall | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 0 (−0.4 to 0.4) | 0.33 | 0 |
| Initial shockable rhythms | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 1.0 (1.0–2.0) | 0 (−0.4 to 0.4) | 0.30 | 0 |
| Initial non-shockable rhythms | 1.0 (1.0–3.0) | 2.0 (1.0–3.0) | 1.0 (1.0–3.0) | −1.0 (−1.5 to − 0.5) | 0.66 | 0 |
| Time intervals in minutes, median (IQR) | ||||||
| EMS response time | 10.3 (7.6, 14.5) | 10.4 (7.6, 14.5) | 9.9 (7.4, 14.6) | −0.4 (−1.0 to 0.2) | 0.42 | 1 (0.1) |
| Call to first shockb | 35.8 (23.6–51.2) | 35.0 (23.6–50.6) | 39.7 (23.9–51.6) | 5.0 (−0.3 to 10.3) | 0.47 | 21 (3.3) |
| Arrest to first shockb | 0 (0, 1.0) | 0 (0, 1.0) | 1 (0, 1.0) | 1 (0.6 TO 1.4) | 0.40 | 21 (3.3) |
| Arrest to intubation attemptedc | 18.0 (11.0, 28.0) | 19.0 (11.0, 28.0) | 16.5 (10.0, 26.0) | −3.0 (−-5.5 to − 0.5) | 0.20 | 40 (4.7) |
| Resuscitation duration | 16.0 (4.0–33.0) | 16.0 (4.0–34.0) | 16.5 (4.0–32.0) | 1.0 (−3.2 to 5.2) | 0.63 | 4 (0.2) |
IQR stands for interquartile range; and EMS, emergency medical services.
Proportion excluded the missing value.
In patients with a defibrillation attempt (n = 849).
In patients with an initial shockable rhythm (n = 637).
In patients with an intubation attempt (n = 849).
Adjusted survival outcomes
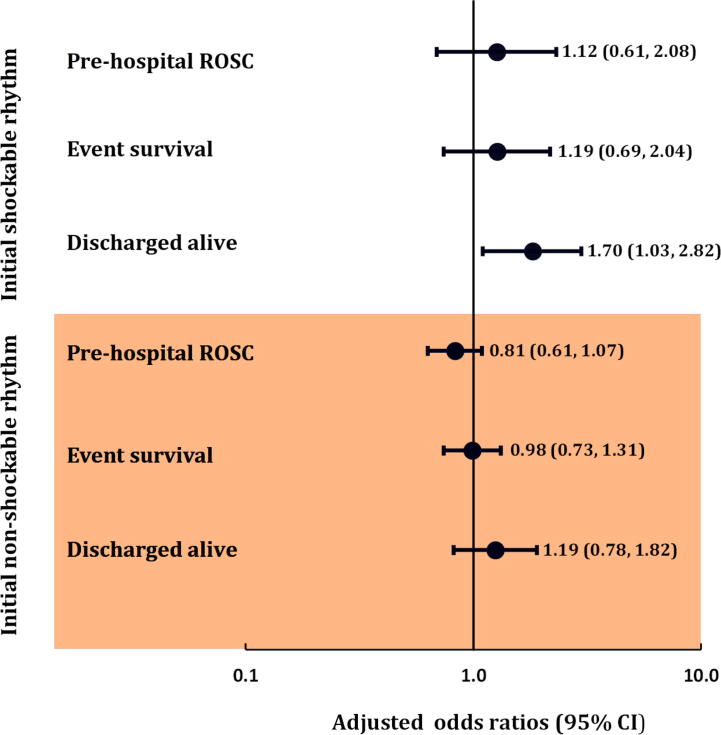
The HP-CPR protocol was associated with higher survival to hospital discharge in overall population (AOR 1.37, 95% CI: 1.00–1.88) (Table 3) and in the subgroup with initial shockable rhythms (AOR 1.70, 95% CI: 1.03–2.82), but not for initial non-shockable rhythms (AOR 1.19, 95% CI: 0.78–1.82) (Fig. 1). There were no significant improvements in event survival or prehospital ROSC for overall population or by subgroups.
Table 3.
The effect of the resuscitation quality improvement intervention on prehospital ROSC, event survival, and discharged alive from hospital after adjustment for arrest characteristics.
| Prehospital ROSC | Event survival | Discharged alive | |
|---|---|---|---|
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| HP-CPR protocol | 0.85 (0.67, 1.10) | 1.03 (0.80, 1.32) | 1.37 (1.00, 1.88) |
| Age in years | 0.99 (0.98, 0.99) | 0.99 (0.98, 0.99) | 0.97 (0.97, 0.98) |
| Male | 0.92 (0.74, 1.15) | 0.91 (0.72, 1.13) | 1.09 (0.82, 1.44) |
| Public location | 1.06 (0.70, 1.60) | 1.35 (0.89, 2.03) | 1.32 (0.81, 2.14) |
| Metropolitan region | 1.50 (1.20, 1.88) | 1.53 (1.22, 1.92) | 1.45 (1.09, 1.92) |
| Arrest aetiology | |||
| Cardiac | Reference | Reference | Reference |
| Respiratory | 1.52 (1.13, 2.06) | 1.38 (1.02, 1.88) | 1.08 (0.69, 1.70) |
| Terminal illness | 0.14 (0.06, 0.30) | 0.11 (0.04, 0.31) | - |
| Other | 2.28 (1.35, 3.85) | 3.03 (1.83, 5.04) | 1.50 (0.79, 2.85) |
| Initial rhythm | |||
| Shockable | Reference | Reference | Reference |
| PEA | 0.14 (0.11, 0.19) | 0.12 (0.09, 0.15) | 0.05 (0.04, 0.07) |
| Asystole | 0.14 (0.10, 0.20) | 0.13 (0.10, 0.19) | 0.07 (0.05, 0.11) |
| Non-shockable | 0.03 (0, 0.34) | 0.04 (0, 0.49) | 0.10 (0.01, 1.02) |
| Season | |||
| Summer | Reference | Reference | Reference |
| Autumn | 0.87 (0.64, 1.17) | 1.10 (0.82, 1.49) | 0.81 (0.57, 1.17) |
| Winter | 0.85 (0.64, 1.14) | 1.03 (0.77, 1.39) | 0.59 (0.41, 0.85) |
| Spring | 0.96 (0.70, 1.32) | 1.32 (0.96, 1.80) | 0.87 (0.60, 1.27) |
AOR stands for adjusted odds ratio; CI, confidence interval; HP-CPR, high performance cardiopulmonary resuscitation; ROSC, return of spontaneous circulation; and PEA, pulseless electrical activity.
Significant figures were bolded.
Fig. 1.
Adjusted logistic regression analysis of the effect of a resuscitation quality improvement intervention on outcomes in EMS-treated OHCA patients for initial shockable and non-shockable rhythms.
Discussion
The findings of this study show that the implementation of a state-wide HP-CPR protocol was associated with a significant increase in survival from EMS witnessed OHCA of non-traumatic aetiology. The multivariable models indicate that the intervention was associated with a 37% improvement in the risk-adjusted odds of survival to hospital discharge for the overall population or a 70 % improvement for initial shockable arrests.
Our results indicate that the relative benefit of HP-CPR on OHCA survival was higher among EMS witnessed arrests compared to our previous examination of non-EMS witnessed arrests,5 with the greatest improvement for cases with a shockable arrest. This could suggest that patients with lower downtimes are more likely to benefit from improvements in resuscitation quality. Interestingly, our reported shockable arrests survival of ∼77 % is higher than that reported by all previous studies, according to a recent published systematic review of 66 studies.2
It is difficult to compare our findings with other regions because the impact of HP-CPR protocol on EMS witnessed OHCA cases have not been reported in the literature. A recent systematic review that examined current evidence on HP-CPR implementation supports the application of such efforts to improve OHCA outcomes such as prehospital ROSC, survival to hospital discharge, and survival with good neurological recovery.3 Although our analysis did not reveal a statistically significant increase in the rate of prehospital ROSC or event survival with the new protocol, we did observe significant increases in survival to hospital discharge that could, partially, be the result of improved resuscitation performance, including the minimisation of interruptions.8 Although we did not have CPR quality data for EMS witnessed OHCA in the control period, our previous analysis demonstrated significant improvements to CPR quality with the implementation of HP-CPR, including an increase in chest compression fraction from 84% to 92%.5
Skill decay from limited exposure to resuscitation is a known contributing factor to poor survival outcomes following OHCA.9, 10, 11 Continuous training and education using various strategies, such as simulation, and provide feedback and post-event debriefing to reinforce the importance of skill retention are essential to improve CPR performance and, subsequently, patient outcomes.12, 13
Limitation
Our study has a number of limitations. Like any retrospective study, our results are subject to inherent errors in data collection and methodological design. It is possible that we were underpowered to show meaningful differences in patient outcomes in subgroup or for the secondary outcomes. We were unable to show that improvements in patient outcomes were associated with changes in CPR quality as this data was not collected during the control period. Information relating to the patient’s in-hospital treatments such as extracorporeal membrane oxygenation or percutaneous coronary interventions were not collected. Therefore, we were unable to examine if in-hospital practices contributed to the better survival rate. Our findings are also limited by the absence of neurological outcomes at hospital discharge, which may be a better measure of patient outcome. Finally, we were unable to evaluate the impact of the intervention beyond January 2020, as the COVID-19 pandemic resulted in significant changes to systems-of-care for OHCA in Victoria.14
Conclusion
The implementation of a HP-CPR quality improvement intervention was associated with a significant improvement in survival from EMS witnessed OHCA. Efforts to monitor and improve CPR performance could yield further improvements in patient outcomes.
Sources of funding
ZN is funded by a National Health and Medical Research Council (NHMRC) Early Career Fellowship (#1146809). DS is supported by a National Heart Foundation Fellowship (#101908).
CRediT authorship contribution statement
Zainab Alqudah: Writing – original draft, Conceptualization, Methodology, Formal analysis, Data curation. Karen Smith: Conceptualization, Methodology, Data curation, Writing – review & editing. Michael Stephenson: Writing – review & editing. Tony Walker: Writing – review & editing. Dion Stub: Writing – review & editing. Ziad Nehme: Conceptualization, Methodology, Formal analysis, Data curation, Writing – review & editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100334.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nehme Z., Andrew E., Bernard S., Smith K. Comparison of out-of-hospital cardiac arrest occurring before and after paramedic arrival: epidemiology, survival to hospital discharge and 12-month functional recovery. Resuscitation. 2015;89:50–57. doi: 10.1016/j.resuscitation.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Gowens P., Smith K., Clegg G., Williams B., Nehme Z. Global variation in the incidence and outcome of emergency medical services witnessed out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2022 doi: 10.1016/j.resuscitation.2022.03.026. [DOI] [PubMed] [Google Scholar]
- 3.Ng Q.X., Han M.X., Lim Y.L., Arulanandam S. A Systematic Review and Meta-Analysis of the Implementation of High-Performance Cardiopulmonary Resuscitation on Out-of-Hospital Cardiac Arrest Outcomes. J Clin Med. 2021;10(10) doi: 10.3390/jcm10102098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McHone A.J., Edsall J., Gunn J., Lineberry E. Implementation of a Team-Focused High-Performance CPR (TF-HP-CPR) Protocol Within a Rural Area EMS System. Adv Emerg Nurs J. 2019;41(4):348–356. doi: 10.1097/TME.0000000000000259. [DOI] [PubMed] [Google Scholar]
- 5.Nehme Z., Ball J., Stephenson M., Walker T., Stub D., Smith K. Effect of a resuscitation quality improvement programme on outcomes from out-of-hospital cardiac arrest. Resuscitation. 2021;162:236–244. doi: 10.1016/j.resuscitation.2021.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Smith K.L., McNeil J.J. Emergency Medical Response Steering C. Cardiac arrests treated by ambulance paramedics and fire fighters. Med J Aust. 2002;177(6):305–309. doi: 10.5694/j.1326-5377.2002.tb04788.x. [DOI] [PubMed] [Google Scholar]
- 7.Perkins G.D., Jacobs I.G., Nadkarni V.M., Berg R.A., Bhanji F., Biarent D., Bossaert L.L., Brett S.J., Chamberlain D., de Caen A.R., et al. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A Statement for Healthcare Professionals From a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Meaney P.A., Bobrow B.J., Mancini M.E., Christenson J., De Caen A.R., Bhanji F., Abella B.S., Kleinman M.E., Edelson D.P., Berg R.A. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 9.An M., Kim Y., Cho W.K. Effect of smart devices on the quality of CPR training: A systematic review. Resuscitation. 2019;144:145–156. doi: 10.1016/j.resuscitation.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 10.Yeung J., Meeks R., Edelson D., Gao F., Soar J., Perkins G.D. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation. 2009;80(7):743–751. doi: 10.1016/j.resuscitation.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Anderson R., Sebaldt A., Lin Y., Cheng A. Optimal training frequency for acquisition and retention of high-quality CPR skills: A randomized trial. Resuscitation. 2019;135:153–161. doi: 10.1016/j.resuscitation.2018.10.033. [DOI] [PubMed] [Google Scholar]
- 12.Bleijenberg E., Koster R.W., de Vries H., Beesems S.G. The impact of post-resuscitation feedback for paramedics on the quality of cardiopulmonary resuscitation. Resuscitation. 2017;110:1–5. doi: 10.1016/j.resuscitation.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 13.Hubner P., Lobmeyr E., Wallmüller C., Poppe M., Datler P., Keferböck M., Zeiner S., Nürnberger A., Zajicek A., Laggner A. Improvements in the quality of advanced life support and patient outcome after implementation of a standardized real-life post-resuscitation feedback system. Resuscitation. 2017;120:38–44. doi: 10.1016/j.resuscitation.2017.08.235. [DOI] [PubMed] [Google Scholar]
- 14.Ball J., Nehme Z., Bernard S., Stub D., Stephenson M., Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–163. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.