Abstract
Background
Mitigation of the COVID-19 pandemic requires continued uptake of SARS-CoV-2 vaccines. To increase vaccination intention and uptake, key determinants of primary and booster vaccination need to be understood and potential effects of vaccination policies examined.
Design
Using experimental data collected in Germany in February 2022 (N = 2701), this study investigated 1) predictors of primary and booster vaccination and 2) potential effects of policies combining vaccination mandates and monetary incentives.
Results
Compared with unvaccinated participants, those with primary vaccination were less complacent, more often understood the collective protection afforded by vaccination, and less often endorsed conspiracy-based misinformation. Compared with participants with primary vaccination, boosted individuals were even less complacent, exhibited fewer conspiracy-based beliefs, perceived fewer constraints by prioritizing vaccination over other things, and more often favored compliance with official vaccination recommendations. Support for and reactance about vaccination mandates depended on vaccination status rather than policy characteristics, regardless of mandate type or incentives (up to 500 EUR). While unvaccinated individuals rejected policy provisions and declined vaccination, boosted individuals indicated mid-level support for mandates and showed high vaccination intention. Among vaccinated individuals, higher incentives of up to 2000 EUR had a considerable positive effect on the willingness to get boosted, especially in the absence of a mandate.
Conclusions
While mandates may be needed to increase primary vaccination, our results indicate that financial incentives could be an alternative to promote booster uptake. However, combining both measures for the same target group seems inadvisable in most cases.
Highlights
Unvaccinated individuals and people with primary and booster vaccinations differ on psychological dimensions, calling for tailored immunization campaigns.
Vaccination intentions depend on vaccination status rather than on mandatory or incentivizing policies.
Incentives are unlikely to persuade unvaccinated individuals but may increase booster uptake.
Positive effects of incentives decrease when vaccination is mandatory, advising against combination.
Keywords: booster, COVID-19, incentives, mandates, vaccination
As SARS-CoV-2 vaccines have been shown to reduce severe infection and death as well as transmission of the pathogen,1,2 vaccination is considered an essential measure in mitigating and ultimately ending the pandemic. Most countries initiated large-scale vaccination campaigns after the first vaccines were licensed, and as of April 2022, about two-thirds of the world’s population had received a first shot.3 While this is an unprecedented achievement in logistical terms, many low-income countries lag behind because of unequal access,4 and vaccine hesitancy—the refusal or delayed acceptance despite availability5—has hindered further uptake in many high-income regions.6 In addition to primary vaccination, booster shots are also important. As natural or vaccine-induced immunity wanes over time, repeated vaccination is necessary to extend protection against hospitalization and death.7,8 Moreover, because first-generation vaccines are less effective against new variants such as Omicron,9 vaccines will need to be updated regularly to maintain immunity10 and so improve protection. While booster shots of first-generation vaccines have been available and recommended in many countries since autumn 2021, uptake has fallen short of expectations. In the United States, for instance, less than 40% of those initially vaccinated had received a booster shot as of April 1, 2022. Rates were higher in European countries such as France (68% of the vaccinated population), the United Kingdom (73%), and Germany (77%), but these levels quickly stagnated,3 and possible reasons for this low booster uptake have been widely discussed, along with intervention strategies to increase both primary and booster uptake.11
Psychological Antecedents of Vaccination Intention and Behavior
To understand and ultimately increase vaccination intention and uptake, it is important to begin from the known key determinants. According to the 7C model of vaccination readiness,12 uptake increases with confidence (perceived vaccine safety and effectiveness), collective responsibility (valuing the protection of others), and compliance (supporting sanctions against those who do not follow official recommendations). Conversely, uptake decreases with complacency (perceived low risk of infection), constraints (structural or psychological barriers), calculation (high need to weigh perceived benefits and risks), and conspiracy beliefs (endorsing misinformation about vaccination).
Importantly, these factors may differ in their effects on primary and booster vaccination. For instance, while confidence in vaccine safety is likely to be a prerequisite in both cases, the effects of complacency and constraints may differ. As primary vaccination provides basic protection from SARS-CoV-2, assuming a low risk of infection may have a stronger negative effect on booster than primary vaccination intention, and the same may be true of perceived barriers to getting vaccinated. By identifying such differences, it may be possible to design effective interventions to improve vaccine uptake.
Indirect and Direct Interventions to Change Vaccination Intention and Behavior
Previous research suggests that measures to address perceptions of disease, vaccination, and related social processes—such as those described by the 7C model—have limited effects on vaccine uptake because they are indirect (see Figure 1).13 For instance, a leaflet designed to increase awareness of the risks associated with contracting COVID-19 may have little impact on primary or booster vaccination intention because the available evidence suggests that risk perception is influenced less by personal knowledge than by variables that are difficult to change, including an individualist worldview, direct experience, and trust in science.14 Even in cases in which educational material mitigates complacency, other factors such as lack of confidence about safety may hinder vaccine uptake. Stagnating vaccination rates reflect the limitations of indirect intervention; despite extensive education and awareness campaigns, levels of primary and booster vaccination have slowed in many countries.
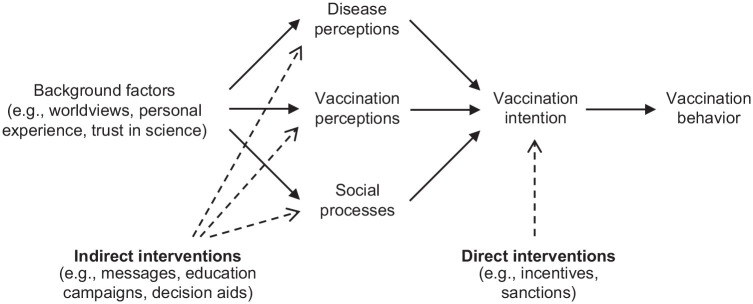
Figure 1.
Determinants of vaccination intention and behavior. Interventions to increase vaccine uptake can affect vaccination intention indirectly by influencing perceptions of the disease and vaccination and social processes or directly by providing additional reasons (incentives, sanctions) for vaccination without changing disease- or vaccination-related perceptions.
Direct intervention strategies such as sanctions (through mandates) and incentives (through financial rewards) avoid these problems by addressing vaccination intention without seeking to influence what people think and feel (Figure 1). Vaccination mandates are regulations that require individuals to get vaccinated, imposing fines or other restrictions as penalties for noncompliance. Over the past decade, many European countries have implemented selective mandates for specific vaccines to increase uptake and prevent outbreaks.15,16 As previous research indicates that mandates effectively increase childhood immunizations17,18 and levels of vaccination among health care workers,19 mandates have also been discussed in relation to COVID-19. Several countries require health care workers to be vaccinated,20,21 and the same requirement has been introduced in Italy and Greece, respectively, for people aged 50 or 60 y and older. Policy makers in Germany and Austria have also debated the introduction of general mandates.22 In Germany, policy proposals included 1) mandated primary and booster vaccination for adults, 2) mandated primary and booster vaccination for people aged 50 y or older (who are more vulnerable to infection), and 3) a mandate combining vaccination for people aged 50 y or older and mandatory consultation for younger adults to promote vaccination and to rebut misinformation (without sanctioning nonvaccination).
Although mandates can improve vaccine uptake, they also have some limitations and downsides. Mandates attract ethical and legal objections because they constrain individual liberty.23,24 There is also evidence that mandated vaccination against SARS-CoV-2 can trigger psychological reactance—feelings of anger that prompt individuals to act against regulation (e.g., by joining a demonstration or signing a petition), to avoid mandated vaccination (e.g., by seeking medical exemption), or to preserve other freedoms (e.g., by declining voluntary vaccination against other diseases).25 Previous studies have also reported that psychological reactance to mandated vaccination is more pronounced among vaccination skeptics.26 As vaccinated individuals (especially those who have received a booster) should exhibit more positive attitudes to vaccination in terms of greater confidence, less complacency, and stronger feelings of collective responsibility, they seem less likely to exhibit negative behaviors or reactance to mandates.
To summarize, while sanctioning nonvaccination may be effective, the associated social and psychological (and potentially behavioral) costs warrant careful consideration, and policy makers should weigh these against other less intrusive strategies. One possible alternative is to incentivize vaccination through payments, gift cards, or tax deductions. However, existing findings regarding the real and potential impacts of monetary incentives on primary vaccination against SARS-CoV-2 are inconclusive. Some studies report positive effects on intention and uptake,27–29 but others differ.30,31
Although the impact of monetary incentives undoubtedly depends on the offered amount,32 the effect may also differ for primary and booster vaccinations. In high-income countries at least, a majority of unvaccinated individuals exhibits low vaccination intention on the grounds that they consider vaccination unsafe and perceive their vaccination status as an important element of their self-concept.33 Being offered several hundred dollars for vaccination is unlikely to increase confidence in vaccination or diminish conspiracy beliefs; indeed, such incentives can prove detrimental when people feel they are being “paid off” for potentially adverse events.34 This suggests that financial incentives may not increase primary vaccination intention.
However, for individuals who have already been vaccinated, incentives may encourage booster vaccination. As argued above, skipping a booster may be more likely for vaccinated individuals who see no need for a booster (because they assume that primary vaccination alone offers sufficient protection), those who perceive constraints (such as everyday stress), and those for whom compliance with vaccination recommendations is not a value in itself. Incentives may help to mitigate such barriers by prioritizing booster vaccination above other behaviors. This assumption is supported by previous evidence of the positive effects of incentives on recurring vaccination for influenza.35 A recent crowdsourcing study provides further support for this view; international experts and representative samples from the United States and the United Kingdom identified financial incentives and tax benefits as among the most effective and acceptable interventions for increasing booster uptake.11
While mandates and incentives are often considered distinct, vaccination policies may combine these interventions. In Austria, for example, it was planned to combine a vaccination mandate with a lottery offering a 1-in-10 chance of winning a voucher worth 500 EUR (about 550 USD).36 However, little is known about the effects of combining legal sanctions and financial incentives in this way.
The Present Research
The present study explores the interplay of sanctions and incentives and seeks to identify the psychological factors that distinguish unvaccinated individuals from those with primary and booster vaccination. Drawing on survey data collected in Germany in February 2022, we first identify differences in the psychological antecedents of vaccination among these 3 groups. We further report the results of an experiment that asked individuals to imagine different mandates and incentives, based on regulations that were under discussion in several countries at that time. Our findings regarding policy support, psychological reactance, and vaccination and avoidance intentions serve to clarify the potential effects of different policies combining sanctions and incentives. Understanding attitudinal differences between unvaccinated individuals and people with primary and booster vaccination can further help to explain varying effects of specific policies in the 3 groups. The results enhance existing understanding of differences in primary and booster vaccine uptake and can help policy makers to design more effective regulations.
Methods
Participants
The study was completed as part of an online panel between February 11 and 23, 2022. Participants were recruited and remunerated by an independent panel provider (Bilendi GmbH). To secure as many participants as possible from the 3 target groups (unvaccinated, vaccinated, boosted), no sociodemographic inclusion criteria were specified. The study was completed by N = 2701 participants from Germany (915 unvaccinated, 316 with primary vaccination, and 1470 with booster vaccination). The mean participant age was 48.96 y (s = 16.46), 48% were female, and most (52%) reported high educational attainment (i.e., university entrance qualifications).
Design
The first part of the experiment employed a 3 (mandate: general mandate v. mandate above 50 y v. combination of mandate above 50 y and mandatory consultation for adults younger than 50 y) × 3 (incentive: no incentive v. 100 EUR v. 200 EUR) factorial between-participant design. In the second part of the experiment, participants were offered various incentives ranging from 0 EUR to 2000 EUR (detailed below).
Materials and Measures
All measures were assessed in the following order.
Antecedents of vaccination
Antecedents were assessed using the short version of the 7C scale,12 which included statements about confidence (“I am convinced the appropriate authorities only allow effective and safe vaccines”), complacency (“I get vaccinated because it is too risky to get infected”), constraints (“Vaccinations are so important to me that I prioritize getting vaccinated over other things”), calculation (“I only get vaccinated when the benefits clearly outweigh the risks”), collective responsibility (“I see vaccination as a collective effort to prevent the spread of diseases”), compliance (“It should be possible to sanction people who do not follow health authority vaccination recommendations”), and conspiracy beliefs (“Vaccinations cause diseases and allergies that are more serious than the diseases they seek to protect us from”).i In each case, participants were asked to indicate their agreement on a 7-point scale ranging from very strongly disagree to very strongly agree. Complacency and constraints ratings were reversed in all analyses to reflect the direction indicated by the wording of the 2 antecedents (i.e., higher values indicating more complacency and constraints, respectively).
Experiment part 1
Participants were randomly assigned to 1 of the 3 mandate and 1 of the 3 incentive conditions.
In the general mandate condition, participants were asked to imagine that vaccination against COVID-19 would soon become mandatory for all adults. In the mandate above 50 y condition, the mandate applied only to people aged 50 y or older, and in the combination condition, unvaccinated adults below this age were required to seek advice from a physician. Across all 3 conditions, participants were told that failure to comply with the specified regulation would result in a fine of up to 2500 EUR (about 2750 USD).
In the no-incentive condition, participants received no further information. In the other 2 incentive conditions, they were asked to imagine that a vaccination bonus would be introduced immediately and that they would receive 100 EUR (about 110 USD) or 500 EUR (about 550 USD) for every past and future vaccination (including booster shots).
After the experimental manipulations, participants were asked to indicate their level of support for the presented regulation and their level of anger on 7-point scales ranging from not at all to very much. Unvaccinated individuals were additionally asked how likely they were to get vaccinated before the regulation came into force. Those who had had a primary or booster vaccination were asked how likely they were to accept a booster shot if available and recommended. Vaccination intention was assessed on a 7-point scale ranging from not getting vaccinated at all to definitely getting vaccinated.
Finally, unvaccinated individuals were told that vaccination could be rejected on the basis of medical exemption. Avoidance intention was assessed by asking whether they would try to obtain such an exemption, and their responses were recorded as a binary yes or no.
Experiment part 2
After a reminder about their mandate condition, participants were offered a series of cash incentives up to 2000 EUR (about 2200 USD), and vaccination intention was recorded for each offered amount. Using a contingent valuation approach,37 the presented amounts depended on the participant’s original incentive condition and responses (Figure 2). Those who exhibited high vaccination intention (conservatively presented by values of 6 or 7 on the 7-point scale) for a specific incentive (e.g., 500 EUR) were offered lower incentives (e.g., 100 EUR). Those who exhibited low to medium vaccination intention (values of 1 to 5) were offered higher incentives (e.g., 800 EUR). This method enabled us to identify individual-level incentive thresholds that would prompt a change from nonvaccination to vaccination.
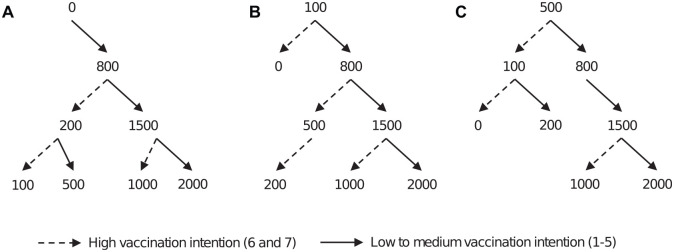
Figure 2.
Contingent valuation decision trees. Participants were asked to indicate vaccination intentions for different incentives ranging between 0 and 2000 EUR (about 2200 USD) on a scale from 1 (not getting vaccinated at all) to 7 (definitely getting vaccinated). The incentives offered depended on initial intentions in the first part of the experiment when presented with (A) no incentive, (B) an incentive of 100 EUR, or (C) an incentive of 500 EUR. Higher amounts were presented when vaccination intention was low to medium (values 1–5, solid line); lower amounts were offered when vaccination intention was high (values 6–7, dashed line).
Ethical Declaration
Ethical clearance was obtained from the University of Erfurt’s institutional review board (#20211215), and all participants provided informed consent to use and share their data for scientific purposes without disclosure of their identities. Funding sources had no role in the study.
Results
Psychological Antecedents of Primary and Booster Vaccination
Figure 3 provides the mean values and 95% confidence intervals for each of the 7C psychological antecedents of vaccination among unvaccinated, primary vaccinated, and boosted participants, respectively. A multinomial regression was performed to identify differences in the antecedents across the 3 target groups (Table 1). Compared with unvaccinated participants, vaccinated individuals were less complacent, felt more collective responsibility, and believed less in misinformation. The results were similar for boosted participants, who also reported more confidence in vaccine safety and efficacy, stronger prioritization of vaccination over other things (perceiving fewer constraints), and greater compliance with vaccination recommendations than unvaccinated individuals. Comparison of boosted and primary vaccination groups showed that boosted participants were less complacent and reported lower conspiracy thinking, they more strongly prioritized vaccination over other things (fewer constraints), and they indicated greater compliance (see Δ in Table 1). While confidence in authorities was stronger among those who had received a booster shot (compared with the nonvaccinated) but not among the primary vaccination group, no significant difference was observed between the two effects. There was no qualitative change in regression results when controlling for participants’ age, gender, education, and employment status (see online supplement).
Figure 3.
7C antecedents of vaccination. Descriptive statistics per group. Bars denote measured means; error bars indicate 95% confidence intervals.
Table 1.
Predictors of Group Membership
| Predictors | Primary Vaccination (v. Unvaccinated) | Boosted (v. Unvaccinated) | Δ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | CI– | CI+ | P | OR | CI– | CI+ | P | ||
| (Constant) | 2.62 | 0.65 | 10.58 | 0.177 | 19.83 | 5.19 | 75.76 | <0.001 | + |
| Confidence | 1.11 | 0.99 | 1.26 | 0.079 | 1.20 | 1.06 | 1.35 | 0.003 | |
| Complacency | 0.74 | 0.66 | 0.84 | <0.001 | 0.67 | 0.60 | 0.76 | <0.001 | – |
| Constraints | 0.87 | 0.74 | 1.01 | 0.068 | 0.72 | 0.62 | 0.84 | <0.001 | – |
| Calculation | 1.07 | 0.99 | 1.16 | 0.090 | 1.03 | 0.95 | 1.12 | 0.436 | |
| Collective responsibility | 1.31 | 1.15 | 1.48 | <0.001 | 1.39 | 1.23 | 1.57 | <0.001 | |
| Compliance | 1.12 | 0.97 | 1.29 | 0.133 | 1.34 | 1.17 | 1.54 | <0.001 | + |
| Conspiracy beliefs | 0.79 | 0.71 | 0.87 | <0.001 | 0.61 | 0.55 | 0.67 | <0.001 | – |
Results from the multinomial logistic regression (reference group: unvaccinated individuals, N = 2701, Cox and Snell’s R2 = 0.61, Nagelkerke’s R2 = 0.72). Bold predictors are statistically significant for P < 0.05. CI– and CI+ denote the lower and upper bounds of the 95% confidence interval, respectively. Δ indicates differences in predictors for both outcomes; + (–) indicates significantly more positive (negative) predictors for booster vaccination as compared with primary vaccination (P < 0.05); see online supplement for the respective regression analysis.
Effects of Mandates and Minor Incentives
After investigating how unvaccinated participants and participants with primary and booster vaccination differ with regard to the 7C, we examined how different vaccination policies affect these 3 groups. To investigate policy effects on support, reactance, and vaccination intention, each of the 3 outcomes was regressed on policy characteristics (mandate and incentive conditions from the first part of the experiment), participant age (up to 50 y or 50 y and older, as these were relevant for policy conditions), and vaccination status (not vaccinated, primary vaccination, or boosted), as well as all possible interactions. Only significant relationships (P < 0.05, not corrected for multiple comparisons) are reported; for details, see the online supplement. For all dependent variables, the main finding was that vaccination status strongly relates to how policies are evaluated and whether people wish to get vaccinated (again). These findings are visualized in Figure 4.
Figure 4.
Policy support, reactance, and vaccination intention. Participants were presented with different policies combining vaccination mandates and incentives. While policy characteristics had little or no effect on support, reactance, or vaccination intention, individual vaccination status was a strong predictor. Bars denote measured means; error bars indicate 95% confidence intervals.
Policy support (R2 = 0.39) was related only to vaccination status. Compared with the unvaccinated, those who had received primary vaccination exhibited greater support for the presented regulation (b = 1.28, 95% CI = [0.38; 2.18], P = 0.005), and this difference was even stronger among boosted individuals (b = 3.33, 95% CI = [2.64; 4.03], P < 0.001). No significant effects were observed for mandate and incentive characteristics, age, or potential interactions.
Reactance (R2 = 0.36) also related solely to vaccination status. Boosted individuals were less angry than the unvaccinated about the presented regulations (b = −3.55, 95% CI = [−4.27; −2.82], P < 0.001). However, there was no significant difference between unvaccinated and primary vaccination participants (b = −0.79, 95% CI = [−1.74; 0.15], P = 0.100). Again, policy characteristics, age, and potential interactions played no significant role. Overall, a strong correlation could be observed between policy support and reactance (r = −0.79, 95% CI = [−0.80; −0.77], P < 0.001).
First or further vaccination intention (R2 = 0.72) was most strongly predicted by vaccination status. Compared with the unvaccinated, those in the primary vaccination group reported higher vaccination intention (b = 2.79, 95% CI = [2.12; 3.46], P < 0.001), and the difference was even greater between the unvaccinated and boosted participants (b = 4.30, 95% CI = [3.78; 4.81], P < 0.001). Four minor interaction effects indicated that policy characteristics and age are somewhat related to vaccination intention. Being 50 y or older was related to stronger vaccination intention among those in the primary (b = 1.71, 95% CI = [0.53; 2.90], P = 0.005) and booster vaccination groups (b = 1.01, 95% CI = [0.30; 1.72], P = 0.005). However, for individuals aged 50 y or older in the primary vaccination group, being assigned to the combination condition (compared with the general mandate condition) had a negative effect on vaccination intention (b = −1.87, 95% CI = [−3.59; −0.15], P = 0.033). Those in the primary vaccination group also reported somewhat lower vaccination intention when offered 100 EUR than when offered no payment at all (b = −1.28, 95% CI = [−2.28; −0.28], P = 0.012). There was no qualitative change in regression results for policy support, reactance, and vaccination intention when controlling for participants’ gender, education, and employment status (see online supplement).
Among unvaccinated individuals, 63% indicated that they would seek medical exemption from vaccination. A binary regression revealed no significant effect of policy characteristics (mandate and incentive conditions) or age (up to 50 y or 50 y and older) on the avoidance intention (see supplement for further detail).
Effects of Mandate Self-relevance and Major Incentives
The above analyses focused on the effects of dedicated policies proposed by some policymakers in different countries (e.g., Germany, Austria). As policy characteristics and participant age played little or no role in explaining the different outcomes, we decided to aggregate mandate characteristics and age information as an indicator of policy self-relevance. For participants assigned to the general mandate condition and those aged 50 y or older, the regulation was considered self-relevant; otherwise, it was coded not self-relevant. This way, statistical power and interpretability of findings could be increased.
Based on their responses in the second part of the experiment, likelihood of getting vaccinated (again) was calculated for each participant and incentive. In line with the decision-tree logic shown in Figure 2, vaccination intention values between 1 and 5 were coded as low likelihood (0), and vaccination intention values of 6 or 7 were coded as high likelihood (1). For incentives that were not presented, likelihood was estimated by assuming monotone decision making, that is, individuals indicating a high (low) chance of vaccination for a specific incentive would do the same for any higher (lower) incentive.
As shown in Figure 5, the share of people indicating high likelihood of vaccination depended not only on vaccination status but also on policy self-relevance and the size of incentive offered. To investigate these effects for each group, we performed linear mixed effects regressions as recommended by Gomila.38 Likelihood of vaccination was regressed on policy self-relevance (between participants), incentive size (within participants, treated as a numeric value between 0 and 2 for incentives from 0 to 2000 EUR), and their interaction (Table 2). As the different intercepts indicate, future vaccination was more likely among vaccinated individuals, especially when they had received a booster shot. The effect of mandate self-relevance was significant only for boosted individuals, who exhibited higher intention to get vaccinated if required to do so. Importantly, greater incentives increased vaccination intention in all 3 groups, especially when the mandate was not self-relevant. In such cases, offering participants the maximum 2000 EUR rather than no incentive increased the share of willing individuals from 0% to 7% (7 pp) for unvaccinated participants, from 23% to 53% (30 pp) for those in the primary vaccination group, and from 57% to 82% (25 pp) for boosted individuals. When participants were affected by the mandate, incentives had less impact. In this case, offering 2000 EUR rather than no incentive increased the share of willing individuals from 1% to 5% (4 pp) for unvaccinated participants, from 34% to 53% (19 pp) for participants in the primary vaccination group, and from 79% to 90% (11 pp) for boosted individuals. To that extent, the overall positive effect of incentives was much smaller for unvaccinated individuals than for vaccinated participants and for those affected by mandatory regulations than for those not affected. There was no qualitative change in regression results when controlling for participants’ age, gender, education, and employment status (see online supplement).
Figure 5.
Effects of incentives and policy self-relevance. Share of participants willing to get vaccinated (i.e., vaccination intention >5 on a scale from 1 to 7), depending on vaccination status, incentive offered, and self-relevance of presented vaccination mandate (measured percentages, assuming monotone decision making).
Table 2.
Predictors of Vaccination Likelihood
| Unvaccinated | Primary Vaccination | Boosted | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | SE | CI– | CI+ | P | b | SE | CI– | CI+ | P | b | SE | CI– | CI+ | P |
| (Constant) | 0.00 | 0.01 | −0.01 | 0.02 | 0.886 | 0.28 | 0.04 | 0.21 | 0.35 | <0.001 | 0.64 | 0.02 | 0.61 | 0.67 | <0.001 |
| Policy: self-relevant (baseline: not self-relevant) | 0.01 | 0.01 | −0.01 | 0.04 | 0.209 | 0.07 | 0.05 | −0.03 | 0.17 | 0.157 | 0.17 | 0.02 | 0.13 | 0.21 | <0.001 |
| Incentive (×1,000 EUR) | 0.03 | 0.00 | 0.03 | 0.04 | <0.001 | 0.14 | 0.01 | 0.12 | 0.16 | <0.001 | 0.11 | 0.00 | 0.10 | 0.12 | <0.001 |
| Interaction effect | −0.02 | 0.00 | −0.02 | −0.01 | <0.001 | −0.04 | 0.01 | −0.06 | −0.01 | 0.005 | −0.06 | 0.01 | −0.07 | −0.05 | <0.001 |
| Marginal R2/conditional R2 | 0.01/0.68 | 0.03/0.81 | 0.04/0.81 | ||||||||||||
Results from mixed-effects regressions investigating the effects of self-relevant (compared with non–self-relevant) mandates and incentives (0 to 2000 EUR) on likelihood of vaccination (v. nonvaccination) for unvaccinated individuals and participants in primary and booster vaccination groups. Bold predictors are statistically significant for P < 0.05. CI– and CI+ denote lower and upper bounds of the 95% confidence interval, respectively.
Discussion
Unvaccinated individuals and those in the primary and booster groups differ in terms of how they think and feel about COVID-19 vaccination and how they perceive and react to direct interventions that seek to change their vaccination intention. Compared with unvaccinated participants, those in the primary vaccination group were less complacent, more likely to understand the issue of collective protection, and less likely to believe in conspiracies. While our data do not allow for causal interpretation, future campaigns to persuade unvaccinated individuals to get vaccinated should focus on communicating individual and collective risks of nonvaccination and on debunking misinformation. Compared with those in the primary vaccination group, boosted individuals were less complacent, believed less in conspiracy-based misinformation, more strongly prioritized vaccination over other things (perceived fewer constraints), and were more likely to favor compliance with official vaccination recommendations. These observations may inform future booster campaigns. First, vaccinated individuals should be reminded that protection can wane over time and that getting vaccinated again can help to prevent severe infection and death. Second, getting a booster shot should be made as easy as possible. In many countries, booster vaccinations are available locally (e.g., in community centers and pharmacies) without having to make an appointment, and this approach should be more widely implemented. Finally, information campaigns to correct conspiracy-based beliefs should target unvaccinated as well as vaccinated individuals. Therefore, misinformation circulating within both groups must be monitored closely.
Lowering barriers and enhancing education may help to increase vaccination intention in some cases. However, prepandemic evidence of the ineffectiveness of these indirect measures13 and the observed slowing of vaccine uptake in many countries in autumn 2021 (despite easy access and extensive information campaigns) highlights their limited impact on future uptake, especially among unvaccinated skeptics. For that reason, we focused on the potential of direct interventions such as vaccination mandates and financial incentives to increase uptake of primary and booster vaccines. Based on real policy proposals in Germany and Austria at the time of data collection, we investigated the combined effects of different mandates and payments on vaccination intentions of unvaccinated participants and people with primary and booster vaccination
In the first part of our experiment, we found that support for and reactance to different policies depended on vaccination status alone rather than on policy characteristics. In other words, it did not matter what kind of mandate was presented or whether vaccination was incentivized with up to 500 EUR per shot. In general, unvaccinated participants rejected every policy and declined vaccination while boosted individuals showed mid-level policy support and high vaccination intention; people with primary vaccination fell somewhere between. Given that overall support for the presented policies was low and that even boosted individuals indicated no clear preference for mandatory vaccination, introducing any of these policies seems likely to backfire. Indeed, we observed considerable reactance, especially among the unvaccinated, and there is evidence that reactance to mandatory vaccination relates to an intention to fight or avoid regulation and resist voluntary vaccination against other diseases.39 In line with earlier findings,25 reactance was not confined to self-relevant mandates; as age and mandate characteristics played no role in predicting anger about the regulations, potential backfire effects must be anticipated and mitigated even among those who are not affected by a given mandate. Previous research suggests that reactance can be reduced by explaining the rationale for a vaccination mandate.25,40 Although this issue was not explored in the present study, explaining a mandate’s benefits for public health or the economy may prove effective for those who have already been vaccinated. However, unvaccinated individuals may oppose coercive measures regardless of explanation because of their stronger conspiracy-based beliefs and low confidence in vaccine safety.
While the incentives of up to 500 EUR offered in the first part of the experiment did not increase vaccination intention, higher incentives of up to 2000 EUR proved more effective. By reclassifying policies as self-relevant or non–self-relevant, we were able to show that higher incentives prompted a stronger increase in vaccination intention, especially when individuals were not affected by the mandate. Among unvaccinated individuals, however, any such difference was negligible, and vaccination intention remained low even for higher payments. This aligns with earlier evidence from Germany, showing that payments of up to 3000 EUR are unlikely to increase primary vaccine uptake.31,32 It seems that negative effects of low confidence and belief in conspiracy-based misinformation cannot be reversed by offering financial incentives. However, for vaccinated individuals, a different picture emerged. When not being affected by a given mandate, an incentive of 2000 EUR increased vaccination intention among individuals in the primary (booster) vaccination groups by 30 (25) percentage points. To that extent, payments seem an effective means of increasing booster uptake by helping to prioritize vaccination over other behaviors and possibly overruling the influence of complacency and constraints. Clearly, appropriate mandates can also be expected to achieve high uptake rates. For instance, the percentage of boosted individuals willing to get vaccinated was comparable for those who were unaffected by a mandate but were offered a 2000 EUR incentive (82%) and those who were mandated but not incentivized (79%). However, as summarized above, mandates are more likely to elicit reactance and detrimental effects. Importantly, limited support could be found for policies combining incentives and mandates (as proposed in Austria) to foster booster uptake. For individuals with primary vaccination, mandating vaccination and offering larger payments did not improve booster intentions compared with offering these payments alone. Only for participants who were already boosted, a positive effect of the combination of mandates and payments could be observed; offering 2000 EUR resulted in more participants willing to receive another booster shot when vaccination was mandatory for them (90%) than when it was not (82%).
Different strategies seem optimal for promoting primary and booster vaccination. Our results indicate that payments and mandates are unlikely to increase primary vaccine uptake. As the limited effect of financial incentives on primary vaccination is also supported by other research including studies with real incentives,27,29,32 policy makers should not seek to incentivize primary vaccination. However, real-world evidence on childhood immunizations and vaccination of health care workers suggests positive effects of mandates over and above what has been observed in our data.17–19 In fact, when real sanctions are in place, more people may conform with a mandate and get their primary vaccinations. While mandates can also help to increase booster uptake, our findings indicate that offering payments may be the better alternative. In comparison to mandates, financial incentives can increase people’s motivation to get (another) booster shot while eliciting less reactance.
In sum, our findings suggest that financial incentives can promote uptake, but their effectiveness depends on vaccination status. People differ in important psychological dimensions, and significant fractions consider vaccination useless, inconvenient, or even as dangerous. While incentives may compensate for inconvenience, money cannot overcome low confidence in vaccine safety and conspiracy-based fears for one’s health. This finding is not only of practical relevance but also helps to improve theories of vaccination decision making. While direct interventions such as financial incentives and mandates aim to bypass what people think and feel about vaccination,13 our results suggest that their effect on vaccination behavior actually depends on these thoughts and feelings. Thus, future theoretical developments should not only investigate additive effects of vaccination-related attitudes and direct interventions on vaccination intention and uptake but also consider interactive relationships.
Limitations
While our findings contribute to the design of effective vaccination policies, they cannot be readily generalized. To oversample unvaccinated individuals, we dispensed with sociodemographic inclusion criteria, and while the sample was reasonably diverse in terms of age, gender, and education, it cannot be considered representative of the general German population. In addition, our results relate to a specific time and context; the data were collected during the less severe Omicron wave, and vaccination intention and support for mandatory regulation may change when more severe strains of SARS-CoV-2 emerge or new vaccines are approved.41 Importantly, too, all variables were self-reported, and our findings may differ from actual behavior. For instance, unvaccinated participants may have understated vaccination intention in the face of mandates and fines. Nevertheless, while vaccine uptake might be higher if mandatory policies were actually implemented, the observed relationships between policy characteristics and vaccine uptake can be considered robust.
Conclusions
The present findings suggest that unvaccinated individuals and people with primary and booster vaccinations form distinct groups both in terms of psychological correlates and reactions to policy measures. For that reason, indirect interventions to improve vaccination intention by raising risk awareness, debunking misinformation, or highlighting collective responsibility must be tailored accordingly. Moreover, financial incentives are unlikely to persuade unvaccinated individuals but may become an important cornerstone of health policies that seek to improve booster uptake. However, our results indicate that reasonable payments need to be offered. Importantly, policy makers should question the combination of mandates and incentives as this means realizing multiple disadvantages (backfire effects due to the mandate and high implementation costs) while achieving only a slight improvement in vaccine uptake as compared with either measure alone.
Note that the 7 items from the short version of the 7C scale were selected from the original 21 items of the full version of scale based on the maximal loading and highest correlations with the willingness to vaccinate.12 Naturally, the wording of the selected items does not cover the full spectrum of the underlying constructs, but the responses to these items are empirically strongly related to the overall constructs they aim to assess.
Footnotes
RB and CB share senior authorship.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support for this study was provided in part by grants from the University of Erfurt and the University of Vienna. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report. The following authors are employed by the sponsors: Philipp Sprengholz, Robert Böhm, and Cornelia Betsch.
ORCID iDs: Philipp Sprengholz  https://orcid.org/0000-0002-9925-1920
https://orcid.org/0000-0002-9925-1920
Robert Böhm  https://orcid.org/0000-0001-6806-0374
https://orcid.org/0000-0001-6806-0374
Data Availability: Materials, data, and the data analysis script are available at DOI: https://dx.doi.org/10.17605/OSF.IO/NGXTQ.
Contributor Information
Philipp Sprengholz, Media and Communication Science, University of Erfurt, Germany; Health Communication, Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany.
Luca Henkel, Department of Economics, University of Bonn, Germany.
Robert Böhm, Faculty of Psychology, University of Vienna, Austria; Department of Psychology, University of Copenhagen, Denmark; Copenhagen Center for Social Data Science, University of Copenhagen, Denmark.
Cornelia Betsch, Media and Communication Science, University of Erfurt, Germany; Health Communication, Bernhard Nocht Institute for Tropical Medicine, Hamburg, Germany; Center for Empirical Research in Economics and Behavioral Sciences, University of Erfurt, Germany.
References
- 1.Haas EJ, Angulo FJ, McLaughlin JM, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021;397:1819–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021;385:585–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ritchie H, Mathieu E, Rodés-Guirao L, et al. Coronavirus pandemic (COVID-19). Our World in Data. 2022. Available from: https://ourworldindata.org/policy-responses-covid. Accessed March 9, 2022. [Google Scholar]
- 4.Schaefer GO, Leland RJ, Emanuel EJ.Making vaccines available to other countries before offering domestic booster vaccinations. JAMA. 2021;326:903. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald NE.Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4. [DOI] [PubMed] [Google Scholar]
- 6.Yin F, Ji M, Yang Z, et al. Exploring the determinants of global vaccination campaigns to combat COVID-19. Humanit Soc Sci Commun. 2022;9:95. [Google Scholar]
- 7.Mattiuzzi C, Lippi G.Primary COVID-19 vaccine cycle and booster doses efficacy: analysis of Italian nationwide vaccination campaign. Eur J Public Health. 2022;32:328–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falsey AR, Frenck RW, Walsh EE, et al. SARS-CoV-2 neutralization with BNT162b2 vaccine dose 3. N Engl J Med. 2021;385:1627–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews N, Stowe J, Kirsebom F, et al. Covid-19 vaccine effectiveness against the Omicron (B.1.1.529) variant. N Engl J Med. 2022;386:1532–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Milne G, Hames T, Scotton C, et al. Does infection with or vaccination against SARS-CoV-2 lead to lasting immunity? Lancet Respir Med. 2021;9:1450–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Böhm R, Betsch C, Litovsky Y, et al. Crowdsourcing interventions to promote uptake of COVID-19 booster vaccines. PsyArXiv. Epub ahead of print 2022. DOI: 10.31234/osf.io/n5b6x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geiger M, Rees F, Lilleholt L, et al. Measuring the 7Cs of vaccination readiness. Eur J Psychol Assess. 2022;38:261–9. [Google Scholar]
- 13.Brewer NT, Chapman GB, Rothman AJ, et al. Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest. 2017;18:149–207. [DOI] [PubMed] [Google Scholar]
- 14.Dryhurst S, Schneider CR, Kerr J, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23:994–1006. [Google Scholar]
- 15.Signorelli C, Odone A, Cella P, et al. Childhood vaccine coverage in Italy after the new law on mandatory immunization. Ann Ig. 2018;30:1–10. [DOI] [PubMed] [Google Scholar]
- 16.Lévy-Bruhl D, Desenclos J-C, Quelet S, et al. Extension of French vaccination mandates: from the recommendation of the Steering Committee of the Citizen Consultation on vaccination to the law. Euro Surveill. 2018;23(17):18-00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee C, Robinson JL.Systematic review of the effect of immunization mandates on uptake of routine childhood immunizations. J Infect. 2016;72:659–66. [DOI] [PubMed] [Google Scholar]
- 18.Hull B, Hendry A, Dey A, et al. Annual immunisation coverage report 2016. Commun Dis Intell. 2019;43. DOI: 10.33321/cdi.2019.43.44 [DOI] [PubMed] [Google Scholar]
- 19.Pitts SI, Maruthur NM, Millar KR, et al. A systematic review of mandatory influenza vaccination in healthcare personnel. Am J Prev Med. 2014;47:330–40. [DOI] [PubMed] [Google Scholar]
- 20.Paterlini M.Covid-19: Italy makes vaccination mandatory for healthcare workers. BMJ. 2021;373:n905. [DOI] [PubMed] [Google Scholar]
- 21.Wise J.Covid-19: France and Greece make vaccination mandatory for healthcare workers. BMJ. 2021;374:n1797. [DOI] [PubMed] [Google Scholar]
- 22.Druml C, Czech H.A pandemic is no private matter: the COVID-19 vaccine mandate in Austria. Lancet Respir Med. 2022;10:322–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frielitz F-S, Wagner IV, Schewe DM, et al. COVID-19: Wäre eine Impfpflicht rechtlich möglich? Dtsch Medizinische Wochenschrift. 2021;146:206–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reiss DR, Caplan AL.Considerations in mandating a new Covid-19 vaccine in the USA for children and adults. J Law Biosci. 2020;7(1):Isaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sprengholz P, Felgendreff L, Böhm R, et al. Vaccination policy reactance: predictors, consequences, and countermeasures. J Health Psychol. 2022;27(6):1394–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Betsch C, Böhm R.Detrimental effects of introducing partial compulsory vaccination: experimental evidence. Eur J Public Health. 2016;26:378–81. [DOI] [PubMed] [Google Scholar]
- 27.Campos-Mercade P, Meier AN, Schneider FH, et al. Monetary incentives increase COVID-19 vaccinations. Science. 2021;374(6569):879–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serra-Garcia M, Szech N.Choice Architecture and Incentives Increase COVID-19 Vaccine Intentions and Test Demand. Discussion Pa per SP II 2021–302 9003. Berlin: Wissenschaftszentrum Berlin für Sozialforschung gGmbH; 2021. [Google Scholar]
- 29.Robertson C, Scheitrum D, Schaefer A, et al. Paying Americans to take the vaccine—would it help or backfire? J Law Biosci. 2021;8(2):Isab027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang T, Jacobson M, Shah M, et al. Financial Incentives and Other Nudges Do Not Increase COVID-19 Vaccinations among the Vaccine Hesitant. Cambridge (MA); National Bureau of Economic Research; 2021. DOI: 10.3386/w29403 [DOI] [Google Scholar]
- 31.Sprengholz P, Eitze S, Felgendreff L, et al. Money is not everything: experimental evidence that payments do not increase willingness to be vaccinated against COVID-19. J Med Ethics. 2021;47:547–8. [DOI] [PubMed] [Google Scholar]
- 32.Sprengholz P, Henkel L, Betsch C.Payments and freedoms: effects of monetary and legal incentives on COVID-19 vaccination intentions in Germany. PLoS One. 2022;17:e0268911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henkel L, Sprengholz P, Korn L, et al. The Association between Vaccination Status Identification and Societal Polarization. ECONtribute Discussion Papers Series 197, University of Bonn and University of Cologne, Germany. [DOI] [PubMed] [Google Scholar]
- 34.Jecker NS.What money can’t buy: an argument against paying people to get vaccinated. J Med Ethics. 2021;medethics-2021-107235. [DOI] [PubMed] [Google Scholar]
- 35.Yamin D, Gavious A.Incentives’ effect in influenza vaccination policy. Manage Sci. 2013;59:2667–86. [Google Scholar]
- 36.Tagesschau. Lotterie soll Lust aufs Impfen machen. 2022. Available from: https://www.tagesschau.de/ausland/europa/impfpflicht-oesterreich-parlament-101.html. Accessed March 29, 2022).
- 37.Carson RT.Contingent valuation: a user’s guide. Environ Sci Technol. 2000;34:1413–8. [Google Scholar]
- 38.Gomila R.Logistic or linear? Estimating causal effects of experimental treatments on binary outcomes using regression analysis. J Exp Psychol Gen. 2021;150:700–9. [DOI] [PubMed] [Google Scholar]
- 39.Sprengholz P, Betsch C, Böhm R.Reactance revisited: consequences of mandatory and scarce vaccination in the case of COVID-19. Appl Psychol Health Well Being. 2021;13(4):986–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sprengholz P, Betsch C.Herd immunity communication counters detrimental effects of selective vaccination mandates: experimental evidence. EClinicalMedicine. 2020;22:100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sprengholz P, Eitze S, Korn L, et al. The power of choice: experimental evidence that freedom to choose a vaccine against COVID-19 improves willingness to be vaccinated. Eur J Intern Med. 2021;87:106–8. [DOI] [PMC free article] [PubMed] [Google Scholar]