Abstract
Subjective cognitive decline (SCD), which precedes Mild Cognitive Impairment and dementia, may be affected by purpose in life (PiL) and loneliness in older adults. We investigated associations among PiL, loneliness, and SCD in US Latino (n = 126), Black (n = 74), Asian (n = 33), and White (n = 637) adults. Higher PiL predicted lower SCD in all groups (p-values < .012), except Black participants. Lower loneliness predicted lower SCD in Latino and White groups (p-values < .05), and PiL moderated this association in White adults. PiL and loneliness may play important roles in cognitive decline. Differential predictors of SCD suggest differential targets for preventing cognitive decline and dementia across ethnoracial groups.
Keywords: purpose in life, subjective cognitive decline, mild cognitive impairment, social isolation, Latinos, loneliness
What this paper adds
• This study examines relationships amongst PiL, loneliness, and SCD in an ethnoracially diverse sample including Black, Asian, and Latino adults, groups not well represented in past work, and White adults.
• This paper adds to the literature by demonstrating that ethnoracial group may moderate the association of greater PiL and lower SCD.
• We also add to current understanding of PiL as a potential protective factor against cognitive decline by demonstrating that there may be differences in self-rated PiL across ethnoracial groups.
Applications of study findings
• Interventions geared toward increasing sense of PiL may help prevent cognitive decline in ethnoracially diverse older adults.
• Increasing PiL and/or reducing feelings of loneliness may help prevent cognitive decline for older adults living in the US.
• As differential predictors of SCD were identified across groups, further investigation of these associations in other ethnoracial groups is warranted to identify targeted prevention strategies or treatments for cognitive decline.
Introduction
Subjective cognitive decline (SCD), the self-reported experience of worsening cognitive abilities with no objective cognitive impairment (Jessen et al., 2020), is associated with increased risk of developing Alzheimer’s disease (AD) and may be an early marker for Mild Cognitive Impairment (MCI), a proposed precursor to AD (Studart Neto & Nitrini, 2016). Purpose in life (PiL), the experience of living a meaningful life where one’s life goals are attainable or being achieved (Boyle et al., 2009), reduces risk of cognitive decline, MCI, and AD (Boyle et al., 2010; Wingo et al., 2020), and is associated with better cognitive functioning across domains (Estrella et al., 2021; Lewis et al., 2017). Relationships between PiL and SCD merit examination, given the proposed link between SCD and AD progression (Jessen et al., 2020).
In contrast, loneliness—an individual’s perceived social isolation (Luhmann & Hawkley, 2016)—is a lifestyle factor associated with worse cognitive functioning and greater risk of cognitive decline, AD, dementia, and SCD (Boss et al., 2015; Lara et al., 2019; Montejo et al., 2020; Sundström et al., 2020). As older adults are vulnerable to experiencing loneliness (Pinquart & Sorensen, 2010), it may be a target for maintaining cognitive health and reducing the risk for cognitive decline.
Addressing modifiable lifestyle risk factors in older adults can reduce the risk of cognitive decline. Social support, online, and group interventions to increase socialization are associated with better objective cognitive functioning and reduced dementia risk (Akhter-Khan et al., 2021; Kelly et al., 2017; Myhre et al., 2016; Pitkala et al., 2011). Targeting PiL may also reduce loneliness (Kang et al., 2021; Neville et al., 2018), as the same neural networks may underlie PiL and loneliness (Mwilambwe-Tshilobo et al., 2019). Although these studies show promise for maintaining healthy cognition with age, there is little research examining ethnoracially diverse groups, who are at greater risk for AD than White adults (Alzheimer’s Association, 2021). Past research in ethnoracially diverse groups has included group classifications that may be considered a racial or an ethnic identity, and compared these groups to one another. While race refers to socially significant physical qualities and ethnicity refers to shared aspects of a culture (e.g., language) (American Psychological Association, 2020), ethnoracial identity describes how individuals label their own race and/or ethnicity. Herein we use the term ethnoracial group when referring to racial and/or ethnic identity. One study found that social support and reduced loneliness associated with better objective cognitive performance in Latino adults (Estrella et al., 2021); another found lower loneliness associated with lower dementia risk after 10-year follow-up in White, Hispanic, and African-American participants (Sutin et al., 2020). It is still unclear how loneliness relates to SCD in these groups.
Given these disparities, including ethnoracially diverse adults when examining risk and protective factors of AD is paramount. SCD also differs across ethnoracial groups: Black, Asian, American Indian/Alaska Native, and Hispanic participants reported greater SCD than White participants (Burns et al., 2019; Jang et al., 2021; Röhr et al., 2020). Hispanic individuals (i.e., with origins from Spanish-speaking countries; Jaimes et al., 2013) have demonstrated greater SCD than African-American and White participants (Faustin & Masurkar, 2020; Harwood et al., 1998; Rodriguez et al., 2021). SCD also related to memory in Caucasian but not African-American participants, suggesting differences in how subjective concerns were reported (Jackson et al., 2017). Studies including Latinos (i.e., with origins in Latin American countries; Jaimes et al., 2013) is sparse overall. Some studies investigated SCD in members of a Colombian kindred with early-onset autosomal dominant AD, where Presenilin-1 mutation carriers showed greater subjective concerns than non-carriers (Norton et al., 2017), and female carriers more than males (Martinez et al., 2021). Though prior research suggests protective benefits of PiL (Wingo et al., 2020) and increased risk of loneliness (Montejo et al., 2020) for SCD, there is a paucity of research investigating these relationships, and differences in these ratings, in ethnoracially diverse samples.
In addition to health and lifestyle factors, sociodemographic factors such as lower socioeconomic status and marital status (i.e., being divorced or widowed) can increase risk of cognitive decline and AD (George et al., 2020; Liu et al., 2019). There is a need to examine sociodemographic predictors of SCD among ethnoracially diverse groups given their greater risk for health disparities including cognitive decline and dementia.
The present study examined: 1 (a) the relationship between PiL and SCD in older Latino, Black, Asian, and White adults living in the United States (US) and whether ethnoracial group moderated this association; 1 (b) associations between PiL and SCD in separate ethnoracial groups; 2 (a) the relationship between loneliness and SCD in these groups, and moderating effects of ethnoracial group; and 2 (b) potential moderation effects of PiL in this association. As exploratory aims, we identified: 3 (a) sociodemographic, motivating and/or modifiable predictors of SCD, and 3 (b) sociodemographic predictors of PiL in these groups. We hypothesized that in all groups, greater PiL and less loneliness would be associated with lower SCD, and that PiL would moderate the association between loneliness and SCD. We hypothesized that relative to the White group, Latino, Black, and Asian groups would report greater SCD and that higher PiL would be more strongly associated with lower SCD.
Methods
Participants
Participants were 870 older adults (average age = 67.0; SD = 7.6; range = 55–94; 76% female), self-identifying as Latino/a/e/x (n = 126), Black (n = 74), Asian (n = 33) or White (n = 637), living in the US, with a college-level education on average (average education = 17.1 years; SD = 3.2; range = 3.0–27.0; Table 1). Participants were part of an international study assessing well-being and cognition in older adults during the COVID-19 pandemic (Babulal et al., 2021). Study participants were recruited through social media, investigator contacts, and virtual meetings. Participants completed a one-hour survey including questionnaires on demographics, PiL, loneliness, and SCD. Ethnoracial group was determined using US Census questions about race (White, Black, Asian) and ethnicity (Latino, Non-Latino). The loneliness measure was added after data collection began; data were available for 828 participants (103 Latino, 71 Black, 33 Asian, 621 White). Data were collected and stored via Research Electronic Data Capture (REDCap). All participants provided online informed consent prior to participating. Study procedures were approved by the Massachusetts General Brigham Human Research Review Board.
Table 1.
Sample Demographic Information.
| Latino | Black | Asian | White | p-value | Eta2 | |
|---|---|---|---|---|---|---|
| (n = 126) | (n = 74) | (n = 33) | (n = 637) | |||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Age (years) | 64.08 (6.79) | 66.34 (7.07) | 65.76 (7.67) | 67.65 (7.80) | <.001 | 0.028 |
| Education (years) | 16.28 (3.96) | 16.80 (2.68) | 17.93 (2.90) | 17.20 (3.12) | .009 | 0.013 |
| Sex (male:female) | 23:102 | 9:63 | 11:22 | 166:471 | .016 | 0.109 |
| Marital status (married:unmarried) | (72:54) | 31:43 | 21:12 | 367:270 | .059 | 0.093 |
| Income (low/middle/high) | 28/81/14 | 7/59/8 | 3/22/8 | 80/441/106 | .019 | 0.094 |
| Life questionnaire | 3.81 (0.74) | 4.01 (0.69) | 3.82 (0.88) | 3.75 (0.74) | .035 | 0.009 |
| Loneliness | 2.92 (1.84) | 2.24 (1.61) | 2.82 (1.67) | 3.07 (2.26) | <.001 | 0.133 |
| ECog | 9.18 (3.63) | 8.54 (2.32) | 9.04 (3.58) | 9.43 (3.22) | .143 | 0.006 |
Note. Loneliness = Gierveld Loneliness Scale; n = 828 for Loneliness ratings. ECog = Everyday Cognition Scale. Three participants did not report sex; 13 did not report income. Values for sex, marital status, and income derived from Chi-square tests; Cramér’s V reported.
Measures
Demographics: Marital status was dichotomized to indicate married or unmarried. Income options were “low income,” “middle income,” and “high income.” The 10-item Life Questionnaire is derived and modified from Ryff’s and Keyes’ scales of Psychological Well-being which has been validated for measuring PiL (Boyle et al., 2009; Ryff, 1989). Participants responded to items such as, “I have a sense of direction and purpose in life” on a 5-point scale from “completely disagree” to “completely agree.” Negatively-worded items were reverse-scored. Responses were averaged to yield the PiL score (possible range: 1–5); higher average ratings denote higher PiL. The 6-item DeJong Gierveld Loneliness Scale, which is validated for use in older adults, was included to measure loneliness (Gierveld & Tilburg, 2006). Respondents answered items such as, “There are enough people I feel close to” with “yes,” “more or less,” “no,” or “no answer.” “Yes” and neutral responses are scored as 1 on negatively-worded items (e.g., “I experience a general sense of emptiness”), while “no” and neutral responses are scored as 1 on positively-worded items (e.g., “There are enough people I feel close to”). Higher scores indicate greater loneliness; total scores ≥2 indicate perceived loneliness (possible range: 0–6). The Measurement of Everyday Cognition (ECog; Farias et al., 2008), measuring SCD over the past decade, includes 39 items mapping onto distinct cognitive domains (memory, language, visuospatial abilities, and executive function). Participants compared current abilities to 10 years ago (e.g., “remembering where I have placed objects”) using a scale from 1 (“better or no change”) to 4 (“consistently much worse”). The total score is the average of items (possible range: 1–39); higher scores indicate greater SCD.
Analyses
Demographic variables, PiL, SCD, and loneliness scores fell within acceptable limits of normality (Kline, 2016). One-way analyses of variance (ANOVA) and chi-square tests were conducted to examine differences between groups. Aim1a: Hierarchical regressions were conducted to assess the relationship between PiL and SCD in the whole sample, with demographic covariates (age, sex, education) in Step 1, Life Questionnaire score in Step 2, and ECog total score as the criterion variable. To examine the moderating effect of ethnoracial group, a hierarchical regression was conducted with demographic covariates that were significantly associated with ECog total scores from the initial regression (i.e., education) entered in Step 1, PiL score and ethnoracial group in Step 2, the interaction between PiL score and ethnoracial group entered in Step 3, and ECog total score as the criterion variable. Ethnoracial group was coded as 0 = White, 1 = Latino, 2 = Black, and 3 = Asian. Aim 1b: The same initial regression was conducted in Latino and White groups only, due to sample size limitations.
Aim 2a: The relationship between loneliness and SCD was examined in the whole sample, including potential moderating effects of ethnoracial group (see analyses and results in Supplementary Material Section A). These associations were then examined in Latino and White groups due to sample size limitations. Hierarchical regressions were conducted with demographic covariates (age, sex, and education) entered in Step 1, loneliness total scores entered in Step 2, and ECog total score serving as the criterion variable. Aim 2b: Due to sample size limitations, the moderating effects of PiL on this relationship were examined in Latino and White groups, using separate hierarchical regressions, with significantly related demographic covariates (i.e., education) entered in Step 1, PiL and loneliness scores entered in Step 2, the interaction between PiL and loneliness entered in Step 3, and ECog total score as the criterion variable. Bonferroni correction for multiple comparisons was applied, with alpha = .0125.
Aim 3a: To examine predictors (sociodemographic, motivating, and/or modifiable factors) of SCD, separate multiple regressions were conducted in Latino and White groups with demographics (age, sex, education, income, marital status), PiL, and loneliness as predictors, with ECog total score as the criterion. Aim 3b: In post-hoc exploratory analyses, we examined sociodemographic predictors of PiL. In Latino and White groups, separate multiple regressions were conducted with sociodemographic characteristics (age, sex, education, income, marital status, living with others, and employment status) as predictors, with PiL (Life Questionnaire total score) serving as the criterion variable. In accord with smaller sample sizes, Pearson correlations were conducted to examine all associations in Black and Asian groups.
Post-hoc standard regressions and correlations were conducted to examine age as a predictor of SCD, PiL, and loneliness (Supplementary Material Section B). Bonferroni corrections for multiple comparisons were not applied in the interpretation of exploratory analyses (aims 3a and 3b, post-hoc analyses). Multicollinearity statistics were acceptable for all regressions (VIF < 2, Tolerance > .500). Analyses were conducted using SPSS version 27 (IBM Corp. 2019).
Results
Sociodemographic Information
White participants were older (F (3,866) = 8.374, p < .001, eta2 = .028) and, along with the Asian group, had higher levels of education (F (3,866) = 3.886, p = .009, eta2 = .013) than Latinos. There were more females than males (X2 (3, N = 867) = 10.39, p = .016, V = .109) and more middle-income participants (X2 (6, N = 857) = 15.194, p = .019, V = .094) in the White group. There were no group differences in distribution of married to unmarried participants (p = .059; Table 1).
SCD, Loneliness, and PiL
Average ECog total scores exceeded the suggested MCI cutoff (Farias et al., 2011) in the overall sample (average = 9.3; SD = 3.2; range = 5.67–26.0) with no group differences (p = .143; for ECog total and domain scores by group see Supplementary Figure 1). Average Loneliness scores indicated all groups experienced loneliness (whole-sample average = 2.8, SD = 1.8, range = 0–6). White participants had higher loneliness scores than Black participants (F (3,824) = 2.662, p = .047, eta2 = .133). Black participants reported higher average PiL ratings than White participants (F (3,866) = 2.883, p = .035, eta2 = .009; Table 1), with no other between-group differences (whole sample average = 3.8, SD = 0.74, range = 1.1–5.0).
PiL Predicting SCD
Only years of education was significantly associated with SCD (β = −.106, p = .002) in the model including demographic covariates. The final model, controlling for demographic covariates, indicated that higher PiL associated with lower SCD in the whole group (F (4,862) = 52.64, p < .001, R2 = .196; β = −.435, p < .001).
Ethnoracial Group Moderating the Relationship between PiL and SCD
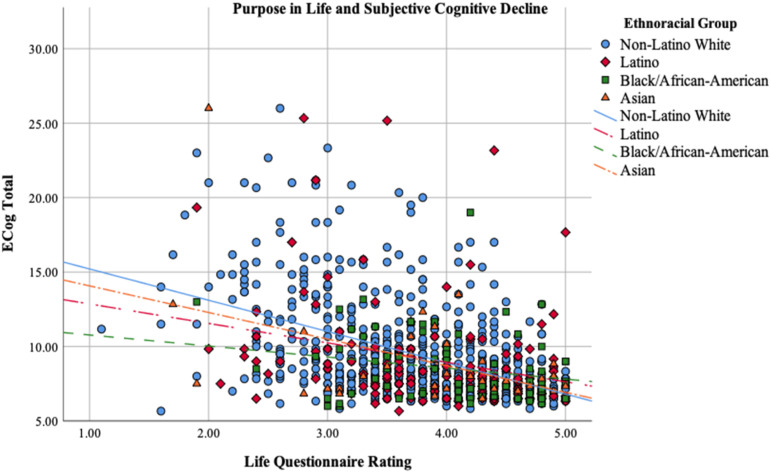
Model 2 of the hierarchical regression examining the relationship between PiL, ethnoracial group, and SCD, controlling for demographics, was significant (F (3,866) = 67.59, p < .001, R2 = .190), indicating that higher PiL (Life Questionnaire; β = −.426, p < .001) is associated with lower SCD (Supplementary Table 1). The final model that included the interaction between PiL and ethnoracial group was significant (F (4,865) = 52.19, p < .001, R2 = .194; β = .078, p = .025); the relationship between PiL and SCD was strongest in White, followed by Asian, then Latino, and finally Black participants (Figure 1, Supplementary Table 1). The interaction effect did not survive correction for multiple comparisons.
Figure 1.
Purpose in life and subjective cognitive decline in whole sample.
PiL and SCD by Ethnoracial Group
The final model controlling for demographic covariates indicated that higher PiL associated with lower SCD in Latino (F (4,120) = 5.62, p < .001, R2 = .158; β = −.303, p = .001) and White groups (F (4,632) = 47.89, p < .001, R2 = .233; β = −.479, p < .001; Table 2). In Asian participants, the correlation between PiL and SCD was significant (r = −.439, p = .011), while in Black participants, there was a trend (r = −.219, p = .061; Supplementary Tables 5 and 6).
Table 2.
Purpose in Life Predicting Subjective Cognitive Decline in Latino and White Participants.
| B | SEB | β | p | R2 | ΔR2 | ΔF | |
|---|---|---|---|---|---|---|---|
| Latino Group | <.001 | 0.158 | 0.088 | 12.58 | |||
| Education | −0.069 | 0.077 | −0.078 | .368 | |||
| Age | 0.008 | 0.044 | 0.016 | .850 | |||
| Sex | −2.264 | 0.772 | −0.248 | .004 | |||
| Life Questionnaire | −1.464 | 0.412 | −0.303 | .001 | |||
| White Group | <.001 | 0.233 | 0.222 | 182.85 | |||
| Education | −0.018 | 0.037 | −0.017 | .634 | |||
| Age | 0.006 | 0.015 | 0.014 | .690 | |||
| Sex | 0.000 | 0.268 | 0.000 | .999 | |||
| Life questionnaire | −2.089 | 0.154 | −0.479 | <.001 |
Note. Final models shown.
Loneliness Predicting SCD
The final model of the hierarchical regression assessing the relationship between loneliness and SCD indicated that higher loneliness associated with greater SCD in the Latino group (F (4,97) = 3.56, p = .009, R2 = .128; β = .196, p = .044; Table 3, Supplementary Figure 2); however, this association did not remain significant after correcting for multiple comparisons. In the White group, the final model indicated that higher loneliness was associated with greater SCD (F (4,616) = 22.07, p < .001, R2 = .125; β = .340, p < .001; Table 3, Supplementary Figure 2). In Black (r = .222, p = .063) and Asian participants (r = .198, p = .269), the correlation between loneliness and SCD was nonsignificant (Supplementary Tables 5 and 6). Whole sample analyses and results are in Supplementary Material Section A.
Table 3.
Loneliness Predicting Subjective Cognitive Decline in Latino and White Participants.
| B | SEB | β | p | R2 | ΔR2 | ΔF | |
|---|---|---|---|---|---|---|---|
| Latino Group | .009 | 0.128 | 0.037 | 4.15 | |||
| Education | −0.148 | 0.098 | −0.146 | .134 | |||
| Age | 0.032 | 0.054 | 0.058 | .546 | |||
| Sex | −2.707 | 0.929 | −0.280 | .004 | |||
| Gierveld Loneliness Scale | 0.411 | 0.202 | 0.196 | .044 | |||
| White Group | <.001 | 0.125 | 0.114 | 80.04 | |||
| Education | −0.081 | 0.040 | −0.078 | .042 | |||
| Age | 0.017 | 0.017 | 0.039 | .315 | |||
| Sex | −0.012 | 0.293 | −0.002 | .967 | |||
| Gierveld Loneliness Scale | 0.620 | 0.069 | 0.340 | <.001 |
Note. Final models shown.
PiL Moderating the Relationship between Loneliness and SCD
Model 2 of the regression examining moderating effects of PiL in the Latino group revealed that greater PiL predicted lower SCD (F (3,99) = 3.60, p = .016, R2 = .098; β = −.230, p = .033). The final model was significant (F (4,98) = 2.90, p = .026, R2 = .106), although the PiL-loneliness interaction was nonsignificant, indicating that PiL did not moderate this relationship (Table 4). Model 2 of this regression in the White group indicated that greater PiL (β = −.416, p < .001) and lower loneliness ratings (β = .119, p = .004) predicted lower SCD (F (3,617) = 66.27, p < .001, R2 = .244). The final model (F (4,616) = 51.87, p < .001, R2 = .252), and the PiL-loneliness interaction were significant; association between loneliness and SCD was weaker for higher PiL ratings in this group (β = −.411, p = .009; Table 4).
Table 4.
Purpose in Life and Loneliness as Predictors of Subjective Cognitive Decline in Latino and White Participants.
| B | SEB | β | p | R2 | ΔR2 | ΔF | |
|---|---|---|---|---|---|---|---|
| Latino Group | .026 | 0.106 | 0.008 | 0.829 | |||
| Education | −0.072 | 0.101 | −0.070 | .479 | |||
| Life questionnaire | −2.045 | 1.090 | −0.395 | .064 | |||
| Loneliness | −0.695 | 1.036 | −0.326 | .504 | |||
| Loneliness*Life questionnaire | 0.249 | 0.274 | 0.404 | .365 | |||
| White Group | <.001 | 0.252 | 0.008 | 6.785 | |||
| Education | −0.017 | 0.037 | −0.017 | .635 | |||
| Life questionnaire | −1.099 | 0.332 | −0.251 | .001 | |||
| Loneliness | 1.065 | 0.334 | 0.583 | .001 | |||
| Loneliness*Life questionnaire | −0.233 | 0.089 | −0.411 | .009 |
Note. Final models shown.
Exploratory Analyses: Sociodemographic and Lifestyle Predictors of SCD
In Latinos, the regression exploring predictors of SCD revealed that female sex (β = −.281, p = .004) and higher PiL (β = −.240, p = .034) predicted lower SCD ratings (F (9,91) = 3.03, p = .003, R2 = .230; Table 5). In Whites, higher PiL (β = −.394, p < .001), and lower loneliness (β = .128, p = .003) predicted lower SCD (F (9,597) = 22.34, p < .001, R2 = .252; Table 5). Correlation analyses revealed no significant associations with SCD in the Black group. There was a trend toward a correlation between loneliness and SCD (r = .222, p = .063; Supplementary Table 5). In the Asian group, greater PiL was associated with lower SCD (r = −.439, p = .011; Supplementary Table 6).
Table 5.
Models Including Sociodemographic Predictors of Subjective Cognitive Decline in Latino and White Participants.
| B | SEB | β | p | R2 | |
|---|---|---|---|---|---|
| Latino Group | .003 | 0.230 | |||
| Age | 0.006 | 0.056 | 0.011 | .911 | |
| Sex | −2.712 | 0.914 | −0.281 | .004 | |
| Education | −0.058 | 0.102 | −0.058 | .568 | |
| Income | −0.609 | 0.720 | −0.090 | .400 | |
| Marital status | 0.408 | 0.967 | 0.053 | .674 | |
| Live with others | −0.360 | 1.180 | −0.040 | .761 | |
| Occupation status | −1.529 | 0.819 | −0.189 | .065 | |
| Life questionnaire | −1.230 | 0.573 | −0.240 | .034 | |
| Loneliness | 0.082 | 0.230 | 0.039 | .722 | |
| White Group | <.001 | 0.252 | |||
| Age | 0.008 | 0.018 | 0.019 | .641 | |
| Sex | −0.008 | 0.280 | −0.001 | .977 | |
| Education | −0.026 | 0.039 | −0.025 | .509 | |
| Income | −0.385 | 0.233 | −0.065 | .099 | |
| Marital status | −0.068 | 0.325 | −0.010 | .834 | |
| Live with others | 0.340 | 0.357 | 0.047 | .341 | |
| Occupation status | −0.277 | 0.274 | −0.040 | .312 | |
| Life questionnaire | −1.711 | 0.188 | −0.394 | <.001 | |
| Loneliness | 0.232 | 0.078 | 0.128 | .003 |
Note. Latino group n = 103. White group n = 621. Loneliness = Gierveld Loneliness Scale.
Exploratory Analyses: Sociodemographic Predictors of PiL
In Latinos, the regression exploring sociodemographic predictors of PiL indicated that employment predicted higher PiL (F (7,93) = 2.564, p = .018, R2 = .162; Table 6). In the White group, higher education (β = .142, p = .001) and higher income (β = .190, p < .001) predicted higher PiL (F (7,599) = 7.675, p < .001, R2 = .082; Table 6). In the Black group, higher income (r = .260, p = .026) and lower loneliness (r = −.445, p < .001) correlated with higher PiL (Supplementary Table 5). In the Asian group, higher education (r = .397, p = .022), higher income (r = .440, p = .010), lower loneliness (r = −.514, p = .002), and lower SCD ratings (r = −.439, p = .011) all correlated with higher PiL (Supplementary Table 6).
Table 6.
Models Including Sociodemographic Predictors of Purpose in Life in Latino and White Participants.
| B | SEB | β | p | R2 | |
|---|---|---|---|---|---|
| Latino Group | .018 | 0.162 | |||
| Age | 0.001 | 0.011 | 0.006 | .957 | |
| Sex | 0.083 | 0.184 | 0.044 | .652 | |
| Education | 0.024 | 0.020 | 0.120 | .246 | |
| Income | 0.207 | 0.143 | 0.156 | .150 | |
| Marital status | 0.121 | 0.193 | 0.080 | .532 | |
| Live with others | −0.378 | 0.223 | −0.214 | .093 | |
| Occupation status | 0.390 | 0.160 | 0.247 | .017 | |
| White Group | <.001 | 0.082 | |||
| Age | 0.005 | 0.004 | 0.049 | .280 | |
| Sex | 0.030 | 0.071 | 0.017 | .677 | |
| Education | 0.034 | 0.010 | 0.142 | .001 | |
| Income | 0.261 | 0.058 | 0.190 | <.001 | |
| Marital status | 0.082 | 0.082 | 0.054 | .323 | |
| Live with others | −0.010 | 0.091 | −0.006 | .908 | |
| Occupation status | 0.106 | 0.070 | 0.066 | .130 |
Correlations among demographic variables, PiL, and SCD in the whole sample and study groups are included in Supplementary Tables 2–6.
Discussion
This was the first study to our knowledge to examine relationships amongst PiL, loneliness, sociodemographic factors, and SCD across ethnoracial groups. Consistent with prior research (Wingo et al., 2020), findings suggest that PiL may be protective against SCD, particularly in Latino, Asian, and White adults, with medium to large effect sizes within these groups. Novel findings include this association in Latinos, an ethnoracial group underrepresented in clinical research to date, and the demonstration that PiL may be more protective against SCD in White individuals than Latino, Black, and Asian groups, and least protective in Black respondents, with a medium to large effect size for these differences.
Consistent with past research (Montejo et al., 2020), our results indicate that loneliness is a risk factor for SCD in Latino and White adults living in the US, though these effect sizes were modest (i.e., small to medium). We did not find an association between loneliness and SCD in Black or Asian subgroups, though this may be due to sample size. We examined whether PiL moderated the relationship between loneliness and SCD. We found a moderating effect in the White respondents, such that for those with higher loneliness ratings, higher PiL had a stronger association with lower SCD (medium to large effect size). This effect was nonsignificant in the Latino group.
Unlike past studies (Burns et al., 2019; Faustin & Masurkar, 2020; Harwood et al., 1998; Jang et al., 2021; Rodrıguez et al., 2021; Röhr et al., 2020), we found no differences in SCD among ethnoracial groups. Our sample was younger on average than those in the aforementioned studies, and correspondingly, our average SCD ratings were lower. Ethnoracial group differences may emerge at older ages, particularly as SCD increases. Our study’s Black and Asian subgroups were also smaller in size than other studies, and we may have been underpowered to detect differences between groups.
Our findings suggest that interventions to increase PiL, such as engaging in meaningful activities and goals, may help stave off SCD. Such interventions may be especially important for groups experiencing loneliness, as observed in the White group. We report the novel finding of ethnoracial differences in PiL among older adults living in the US, where Black adults showed higher PiL and less loneliness than White adults. Individuals experiencing more loneliness may most benefit from higher PiL; there may have been less positive influence of higher PiL ratings for Black adults because they did not experience loneliness to the same degree as the White group. In the Black group, less loneliness showed a medium to large association with higher PiL. Black older adults may be inclined to engage in active behaviors, including socialization, that positively influence PiL and cognitive health. Research examining additional factors contributing to PiL in larger samples may inform strategies to improve PiL, mitigate risk of SCD, and improve overall well-being.
Our exploratory analyses revealed differences in factors best predicting SCD across ethnoracial groups. Greater PiL showed a moderate to strong association with lower SCD in Latino, White, and Asian groups (i.e., medium to large effect sizes), consistent with prior literature demonstrating the protective benefits of PiL against cognitive decline (Wingo et al., 2020). Reducing loneliness and improving PiL may help protect against cognitive decline in White adults, with a small to medium (trending) association of reduced loneliness with lower SCD for Black adults. Our findings revealed that Latino women living in the US report lower SCD than Latino men, though research examining sex differences in SCD reporting is mixed (Heser et al., 2019; Holmen et al., 2013; Martinez et al., 2021; Sundermann et al., 2018). Further investigation into sex differences in the protective or risk factors of SCD in ethnoracially diverse samples may provide insight regarding mixed findings in the literature.
Whereas individuals with lower incomes are reported to have greater risk of SCD or dementia (Gupta, 2021; Peterson et al., 2019), we found small associations between income and SCD in White participants, though were limited by sample sizes for the other groups. Taken together, our findings suggest that increasing PiL and preventing loneliness (e.g., involvement in social groups, or spending time with friends and family) may help mitigate SCD in older adults.
Among White respondents, we found that higher levels of education and self-reported income were associated with higher PiL (small to medium effect size). Some life purpose may be derived from educational and financial attainment in this group, whereas in Latinos, for whom employment and income predicted PiL (medium effect size), the act of working and spending time on meaningful activities may increase PiL, with higher income as a possible effect of holding employment, rather than a unique predictor of PiL. In Black adults, higher income predicted higher PiL ratings (small to medium effect size), and in Asian adults, higher education and income predicted higher PiL (medium to large effect size). As with SCD, there may be differential predictors of PiL among these ethnoracial groups for older adults in the US, though most predictors that emerged in this study were indicators of socioeconomic status. Interventions for improving PiL in these groups may include taking classes or learning a new skill (e.g., learning a new language), or seeking part-time employment to supplement income later in life, particularly in groups showing moderate to strong associations between PiL and higher education and income levels.
As this study was conducted during the COVID-19 pandemic, findings must be interpreted within this context. Social distancing mandates and a transition to working from home likely impacted perceived loneliness and economic well-being for study participants, including employment and income. Public health policies also reduced access to sources from which participants may ordinarily have derived greater PiL, including group/social activities, spending time with family, work, or exercise.
Limitations
This study was cross-sectional, affecting interpretation of the relationships amongst PiL, loneliness, and SCD. Longitudinal data collection is currently ongoing. We faced sample size limitations, particularly in the Black and Asian subgroups, and some analyses examining differences across groups were underpowered and yielded small effect sizes. Research with larger sample sizes is needed to identify additional factors contributing to PiL in these groups, and work is needed in additional groups (e.g., American Indian/Alaska Native; Native Hawaiian). As this study was online, it presents inherent bias for enrolling participants who are comfortable and able to complete questionnaires online, which may have led to a younger sample, with lower SCD. Our study sample overall reported moderately high PiL and moderate ratings of loneliness, which may limit generalizability of these findings; future work should seek to enroll participants reporting lower and higher ratings of both loneliness and PiL. Finally, inclusion of objective measures of cognitive functioning is needed in future studies to better estimate the impact of PiL and loneliness on subsequent cognitive impairment and dementia.
Supplemental Material
Supplementary Material for Associations Among Loneliness, Purpose in Life and Subjective Cognitive Decline in Ethnoracially Diverse Older Adults Living in the United States by Celina F. Pluim, Juliana A. U. Anzai, Jairo E. Martinez, Diana Munera, A. Paola Garza-Naveda, Clara Vila-Castelar, Edmarie Guzmán-Vélez, Liliana Ramirez-Gomez, Julian Bustin, Cecilia M. Serrano, Ganesh M. Babulal, Maira Okada de Oliveira, and Yakeel T. Quiroz in Journal of Applied Gerontology.
Acknowledgments
The authors would all like to thank our participants for their generous contributions of time and effort to this study. C.F.P. was supported by the National Institutes of Health-NIH [5T32HL007901-23], G.M.B. was supported by NIH NIA [R01AG056466, R01AG067428, R01AG068183] and by the BrightFocus Foundation [A2021142S], E.G.V. was supported by NIH NIA [K23AG061276], C.V.C. was supported by the Alzheimer’s Association [2019A005859], J.A.U.A. was supported by Boston University Undergraduate Research Opportunities Program (UROP), and Y.T.Q. was supported by NIH NIA [R01AG054671, R01AG066823], the Alzheimer’s Association and Massachusetts General Hospital ECOR.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Y.T.Q has served as a consultant for Biogen.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the Massachusetts General Hospital ECOR and NIH NIA (R01AG066823).
Ethical Approval: This study was approved by the Massachusetts General Brigham Human Research Review Board (Protocol Approval # 2020P001131).
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Celina F. Pluim https://orcid.org/0000-0002-1834-8983
Yakeel T. Quiroz https://orcid.org/0000-0001-9714-8244
References
- Akhter-Khan S. C., Tao Q., Ang T. F. A., Itchapurapu I. S., Alosco M. L., Mez J., Piers R. J., Steffens D. C., Au R., Qiu W. Q. (2021). Associations of loneliness with risk of Alzheimer’s disease dementia in the Framingham Heart Study. Alzheimer’s & Dementia, 17(10), 1619–1627. 10.1002/alz.12327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Association . (2021). 2021 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 17(3), 327–406. https://www.alz.org/alzheimers-dementia/facts-figures [DOI] [PubMed] [Google Scholar]
- American Psychological Association (2020). Publication manual of the American psychological association (7th ed.). American Psychological Association. [Google Scholar]
- Babulal G. M., Torres V. L., Acosta D., Agüero C., Aguilar-Navarro S., Amariglio R., Ussui J. A., Baena A., Bocanegra Y., Brucki S. M. D., Bustin J., Cabrera D. M., Custodio N., Diaz M. M., Peñailillo L. D., Franco I., Gatchel J. R., Garza-Naveda A. P., González Lara M., Quiroz Y. T. (2021). The impact of COVID-19 on the well-being and cognition of older adults living in the United States and Latin America. EClinicalMedicine, 35, 100848. 10.1016/j.eclinm.2021.100848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boss L., Kang D.-H., Branson S. (2015). Loneliness and cognitive function in the older adult: A systematic review. International Psychogeriatrics, 27(4), 541–553. 10.1017/S1041610214002749 [DOI] [PubMed] [Google Scholar]
- Boyle P. A., Barnes L. L., Buchman A. S., Bennett D. A. (2009). PiL is associated with mortality among community-dwelling older persons. Psychosomatic Medicine, 71(5), 574–579. 10.1097/PSY.0b013e3181a5a7c0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P. A., Buchman A. S., Barnes L. L., Bennett D. A. (2010). Effect of a Purpose in Life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Archives of General Psychiatry, 67(3), 304–310. 10.1001/archgenpsychiatry.2009.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns S. P., Mueller M., Magwood G., White B. M., Lackland D., Ellis C. (2019). Racial and ethnic differences in post-stroke subjective cognitive decline exist. Disability and Health Journal, 12(1), 87–92. 10.1016/j.dhjo.2018.08.005 [DOI] [PubMed] [Google Scholar]
- Estrella M. L., Durazo-Arvizu R. A., Gallo L. C., Tarraf W., Isasi C. R., Perreira K. M., Zeng D., Marquine M. J., Lipton R. B., González H. M., Daviglus M. L., Lamar M. (2021). Psychosocial factors associated with cognitive function among middle-aged and older Hispanics/Latinos: The Hispanic community health study/study of Latinos and its sociocultural ancillary study. Journal of Alzheimer’s Disease, 79(1), 433–449. 10.3233/JAD-200612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias S. T., Mungas D., Harvey D. J., Simmons A., Reed B. R., DeCarli C. (2011). The measurement of everyday cognition: Development and validation of a short form of the Everyday Cognition scales. Alzheimer’s & Dementia, 7(6), 593–601. 10.1016/j.jalz.2011.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias S. T., Mungas D., Reed B. R., Cahn-Weiner D., Jagust W., Baynes K., DeCarli C. (2008). The measurement of everyday cognition (ECog): Scale development and psychometric properties. Neuropsychology, 22(4), 531–544. 10.1037/0894-4105.22.4.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustin A., Masurkar A. V. (2020). Differences in the characteristics, neuropsychiatric comorbidities, and psychometric features of subjective cognitive decline in Hispanics versus non Hispanic Whites: Examining subjective cognitive decline in diverse, ethnoracial populations. Alzheimer’s & Dementia, 16(S6), Article e040431. 10.1002/alz.040431 [DOI] [Google Scholar]
- George K. M., Lutsey P. L., Kucharska-Newton A., Palta P., Heiss G., Osypuk T., Folsom A. R. (2020). Life-course individual and neighborhood socioeconomic status and risk of dementia in the atherosclerosis risk in communities neurocognitive study. American Journal of Epidemiology, 189(10), 1134–1142. 10.1093/aje/kwaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierveld J. D. J., Tilburg T. V. (2006). A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Research on Aging, 28(5), 582–598. 10.1177/0164027506289723 [DOI] [Google Scholar]
- Gupta S. (2021). Racial and ethnic disparities in subjective cognitive decline: A closer look, United States, 2015–2018. BMC Public Health, 21(1), 1173. 10.1186/s12889-021-11068-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood D., Barker W., Ownby R., Duara R. (1998). Memory complaints in the elderly: A comparative analysis of informant and subject reports among Hispanics and White non-Hispanics. Clinical Gerontologist: The Journal of Aging and Mental Health, 18(3), 56–60. https://psycnet.apa.org/record/1998-01325-006 [Google Scholar]
- Heser K., Kleineidam L., Wiese B., Oey A., Roehr S., Pabst A., Kaduszkiewicz H., van den Bussche H., Brettschneider C., König H.-H., Weyerer S., Werle J., Fuchs A., Pentzek M., Mösch E., Bickel H., Maier W., Scherer M., Riedel-Heller S. G., Wagner M. (2019). Subjective cognitive decline may be a stronger predictor of incident dementia in women than in men. Journal of Alzheimer’s Disease, 68(4), 1469–1478. 10.3233/JAD-180981 [DOI] [PubMed] [Google Scholar]
- Holmen J., Langballe E. M., Midthjell K., Holmen T. L., Fikseaunet A., Saltvedt I., Tambs K. (2013). Gender differences in subjective memory impairment in a general population: The HUNT study, Norway. BMC Psychology, 1(1), 1–9. 10.1186/2050-7283-1-1925566353 [DOI] [Google Scholar]
- Jackson J. D., Rentz D. M., Aghjayan S. L., Buckley R. F., Meneide T.-F., Sperling R. A., Amariglio R. E. (2017). Subjective cognitive concerns are associated with objective memory performance in Caucasian but not African-American persons. Age and Ageing, 46(6), 988–993. 10.1093/ageing/afx077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaimes N., Londono V., Halpern A. C. (2013). The term Hispanic/Latino: A note of caution. JAMA Dermatology, 149(3), 274–275. 10.1001/jamadermatol.2013.1304 [DOI] [PubMed] [Google Scholar]
- Jang Y., Choi E. Y., Franco Y., Park N. S., Chiriboga D. A., Kim M. T. (2021). Racial and ethnic differences in cognitive health appraisals: A comparison of non-Hispanic White, non-Hispanic Black, and Hispanic older adults. Aging & Mental Health, 26(3), 519–525. 10.1080/13607863.2021.1899132 [DOI] [PubMed] [Google Scholar]
- Jessen F., Amariglio R. E., Buckley R. F., van der Flier W. M., Han Y., Molinuevo J. L., Rabin L., Rentz D. M., Rodriguez-Gomez O., Saykin A. J., Sikkes S. A. M., Smart C. M., Wolfsgruber S., Wagner M. (2020). The characterisation of subjective cognitive decline. The Lancet Neurology, 19(3), 271–278. 10.1016/s1474-4422(19)30368-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y., Cosme D., Pei R., Pandey P., Carreras-Tartak J., Falk E. B. (2021). PiL, loneliness, and protective health behaviors during the COVID-19 pandemic. The Gerontologist, 61(6), 878–887. 10.1093/geront/gnab081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly M. E., Duff H., Kelly S., McHugh Power J. E., Brennan S., Lawlor B. A., Loughrey D. G. (2017). The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Systematic Reviews, 6(1), 259. 10.1186/s13643-017-0632-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (2016). Principles and practice of structural equation modeling (4th ed.). Guilford Publications. [Google Scholar]
- Lara E., Caballero F. F., Rico Uribe L. A., Olaya B., Haro J. M., Ayuso Mateos J. L., Miret M. (2019). Are loneliness and social isolation associated with cognitive decline? International Journal of Geriatric Psychiatry, 34(11), 1613–1622. 10.1002/gps.5174 [DOI] [PubMed] [Google Scholar]
- Lewis N. A., Turiano N. A., Payne B. R., Hill P. L. (2017). PiL and cognitive functioning in adulthood. Aging, Neuropsychology, and Cognition, 24(6), 662–671. 10.1080/13825585.2016.1251549 [DOI] [PubMed] [Google Scholar]
- Liu H., Zhang Y., Burgard S. A., Needham B. L. (2019). Marital status and cognitive impairment in the United States: Evidence from the national health and aging trends study. Annals of Epidemiology, 38(e22), 28–34. 10.1016/j.annepidem.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann M., Hawkley L. C. (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943–959. 10.1037/dev0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez J. E., Pardilla-Delgado E., Guzmán-Vélez E., Vila-Castelar C., Amariglio R., Gatchel J., Aguirre-Acevedo D. C., Bocanegra Y., Baena A., Henao E., Tirado V., Muñoz C., Giraldo-Chica M., Lopera F., Quiroz Y. T. (2021). Subjective cognitive decline and its relation to verbal memory and sex in cognitively unimpaired individuals from a Colombian cohort with autosomal-dominant Alzheimer’s disease. Journal of the International Neuropsychological Society, 28(6), 541–549. 10.1017/S1355617721000801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montejo P., Crespo D. P., Pedrero-Pérez E., Montenegro-Peña M. (2020). Subjective cognitive decline: Mental health, loneliness, pain and quality of life: Poblational study. Journal of Aging Science, 8(1), 218. 10.35248/2329-8847.20.08.218 [DOI] [Google Scholar]
- Mwilambwe-Tshilobo L., Ge T., Chong M., Ferguson M. A., Misic B., Burrow A. L., Leahy R. M., Spreng R. N. (2019). Loneliness and meaning in life are reflected in the intrinsic network architecture of the brain. Social cognitive and affective neuroscience, 14(4), 423–433. 10.1093/scan/nsz021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myhre J. W., Mehl M. R., Glisky E. L. (2016). Cognitive benefits of online social networking for healthy older adults. The Journals of Gerontology Series B, 72(5), 752–760. 10.1093/geronb/gbw025 [DOI] [PubMed] [Google Scholar]
- Neville S., Adams J., Montayre J., Larmer P., Garrett N., Stephens C., Alpass F. (2018). Loneliness in men 60 years and over: The association with Purpose in Life. American Journal of Men’s Health, 12(4), 730–739. 10.1177/1557988318758807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton D. J., Amariglio R., Protas H., Chen K., Aguirre-Acevedo D. C., Pulsifer B., Castrillon G., Tirado V., Munoz C., Tariot P., Langbaum J. B., Reiman E. M., Lopera F., Sperling R. A., Quiroz Y. T. (2017). Subjective memory complaints in preclinical autosomal dominant Alzheimer disease. Neurology, 89(14), 1464–1470. 10.1212/WNL.0000000000004533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson R. L., Carvajal S. C., McGuire L. C., Fain M. J., Bell M. L. (2019). State inequality, socioeconomic position and subjective cognitive decline in the United States. SSM - Population Health, 7, 100357. 10.1016/j.ssmph.2019.100357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M., Sorensen S. (2010). Influences on loneliness in older adults: A meta-analysis. Basic and Applied Social Psychology, 23(4), 245–266. 10.1207/S15324834BASP2304_2 [DOI] [Google Scholar]
- Pitkala K. H., Routasalo P., Kautiainen H., Sintonen H., Tilvis R. S. (2011). Effects of socially stimulating group intervention on lonely, older people’s cognition: A randomized, controlled trial. The American Journal of Geriatric Psychiatry, 19(7), 654–663. 10.1097/JGP.0b013e3181f7d8b0 [DOI] [PubMed] [Google Scholar]
- Rodrıguez D., Ayers E., Weiss E. F., Verghese J. (2021). Cross-cultural comparisons of subjective cognitive complaints in a diverse primary care population. Journal of Alzheimer’s Disease, 81(2), 545–555. 10.3233/jad-201399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Röhr S., Pabst A., Riedel-Heller S. G., Jessen F., Turana Y., Handajani Y. S., Brayne C., Matthews F. E., Stephan B. C. M., Lipton R. B., Katz M. J., Wang C., Guerchet M., Preux P.-M., Mbelesso P., Ritchie K., Ancelin M.-L., Carrière I., Guaita A., , Sachdev P. S. (2020). Estimating prevalence of subjective cognitive decline in and across international cohort studies of aging: A COSMIC study. Alzheimer’s Research & Therapy, 12(1), 1–14. 10.1186/s13195-020-00734-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C. (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. 10.1037/0022-3514.57.6.1069 [DOI] [Google Scholar]
- Studart Neto A., Nitrini R. (2016). Subjective cognitive decline: The first manifestations of Alzheimer’s disease? Dementia & Neuropsychologia, 10(3), 170–177. 10.1590/S1980-5764-2016DN1003002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundermann E. E., Edmonds E. C., Delano-Wood L., Galasko D. R., Salmon D. P., Rubin L. H., Bondi M. W., & Alzheimer’s Disease Neuroimaging Initiative . (2018). Sex influences the accuracy of subjective memory complaint reporting in older adults. Journal of Alzheimer’s Disease, 61(3), 1163–1178. 10.3233/JAD-170425 [DOI] [PubMed] [Google Scholar]
- Sundström A., Adolfsson A. N., Nordin M., Adolfsson R. (2020). Loneliness increases the risk of all-cause dementia and Alzheimer’s disease. The Journals of Gerontology: Series B, 75(5), 919–926. 10.1093/geronb/gbz139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin A. R., Stephan Y., Luchetti M., Terracciano A. (2020). Loneliness and risk of dementia. The Journals of Gerontology: Series B, 75(7), 1414–1422. 10.1093/geronb/gby112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo A. P., Wingo T. S., Fan W., Bergquist S., Alonso A., Marcus M., Levey A. I., Lah J. J. (2020). Purpose in Life is a robust protective factor of reported cognitive decline among late middle-aged adults: The Emory Healthy Aging Study. Journal of Affective Disorders, 263(3), 310–317. 10.1016/j.jad.2019.11.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material for Associations Among Loneliness, Purpose in Life and Subjective Cognitive Decline in Ethnoracially Diverse Older Adults Living in the United States by Celina F. Pluim, Juliana A. U. Anzai, Jairo E. Martinez, Diana Munera, A. Paola Garza-Naveda, Clara Vila-Castelar, Edmarie Guzmán-Vélez, Liliana Ramirez-Gomez, Julian Bustin, Cecilia M. Serrano, Ganesh M. Babulal, Maira Okada de Oliveira, and Yakeel T. Quiroz in Journal of Applied Gerontology.