Abstract
Clostridium botulinum serotype A produces a neurotoxin composed of a 100-kDa heavy chain and a 50-kDa light chain linked by a disulfide bond. This neurotoxin is part of a ca. 900-kDa complex, formed by noncovalent association with a single nontoxin, nonhemagglutinin subunit and a family of hemagglutinating proteins. Previous work has suggested, although never conclusively demonstrated, that neurotoxin alone cannot survive passage through the stomach and/or cannot be absorbed from the gut without the involvement of auxiliary proteins in the complex. Therefore, this study compared the relative absorption and toxicity of three preparations of neurotoxin in an in vivo mouse model. Equimolar amounts of serotype A complex with hemagglutinins, complex without hemagglutinins, and purified neurotoxin were surgically introduced into the stomach or into the small intestine. In some experiments, movement of neurotoxin from the site of administration was restricted by ligation of the pylorus. Comparison of relative toxicities demonstrated that at adequate doses, complex with hemagglutinins, complex without hemagglutinins, and pure neurotoxin can be absorbed from the stomach. The potency of neurotoxin in complex was greater than that of pure neurotoxin, but the magnitude of this difference diminished as the dosage of neurotoxin increased. Qualitatively similar results were obtained when complex with hemagglutinins, complex without hemagglutinins, and pure neurotoxin were placed directly into the intestine. This work establishes that pure botulinum neurotoxin serotype A is toxic when administered orally. This means that pure neurotoxin does not require hemagglutinins or other auxiliary proteins for absorption from the gastrointestinal system into the general circulation.
Botulinum neurotoxin (BoNT) is synthesized and released by the anaerobic, gram-positive bacterium Clostridium botulinum as seven related but serologically distinct proteins designated serotypes A, B, C, D, E, F, and G. BoNT (∼150 kDa) is composed of a heavy chain and a light chain linked by a disulfide bond, and this dichain molecule is ordinarily a component of a complex formed by noncovalent association with other proteins, including a family of hemagglutinins (HA) and a single nontoxin, nonhemagglutinin subunit (11, 19).
BoNT serotype A (BoNT/A) is an unusually potent neurotoxin that causes the disease botulism, a form of flaccid paralysis that if left untreated can be fatal. Of the several possible routes that neurotoxin can use to enter the body, the oral route is the most common (9, 18, 25, 27). Intoxication usually occurs due to ingestion of preformed neurotoxin contaminating a meal or to ingestion of bacteria that may colonize the gut and produce neurotoxin. In either case, BoNT escapes the gastrointestinal (GI) system to reach the general circulation (lymph and blood). Neurotoxin in blood is then delivered to peripheral cholinergic nerve endings, which are the target for neurotoxin action.
Although absorption of neurotoxin from the gut is essential to the onset of disease, surprisingly little is known about specific mechanisms that contribute to absorption (1). A series of early studies indicated that the upper small intestine is the primary site of absorption (4, 5, 10, 16). This early work also established that neurotoxin which was administered orally or directly into the intestine appeared in lymph and blood. Absorbed neurotoxin was shown to be biologically active, as judged by assays for in vivo toxicity.
One of the obstacles that has hindered work on characterizing the mechanism of absorption is the finding that naturally occurring botulism is not due to pure neurotoxin but instead is due to neurotoxin that is part of a complex with auxiliary proteins. The serotype A complex is composed of several proteins, including neurotoxin, a family of hemagglutinins, and a nontoxin, nonhemagglutinin component. (There may also be a negligible amount of nonprotein, e.g., RNA.) Virtually all of the work that has been done to date indicates that auxiliary proteins probably play a role in protecting the neurotoxin from the harsh conditions of pH and proteolytic enzymes found in the gut (1, 3, 8, 20–22, 29, 30). Unfortunately, there is almost no work describing the role of these auxiliary proteins in the process of neurotoxin absorption (but see reference 7).
In the recent past, we have conducted two types of studies that may help to clarify both the mechanism by which neurotoxin is absorbed and the role of auxiliary proteins in absorption. In the first, molecular biological techniques were used to express a recombinant holotoxin that lacks the ability to poison nerve endings. This holotoxin was found to be an effective oral vaccine that elicited the production of systemic antibodies (13). In the second study, binding and transcytosis of neurotoxin was studied in T-84 cells, which are derived from the gut. This work demonstrated that native holotoxin bound to specific receptors on the mucosal side of cells and was actively transported to the serosal side of these cells (15). Taken together, these studies suggest that pure neurotoxin, in the absence of auxiliary proteins, can be absorbed from the gut.
To test the hypothesis that pure neurotoxin can be absorbed and to gauge the role of auxiliary proteins in this process, a series of experiments were done in mice. Three neurotoxin preparations were examined as follows: (i) pure neurotoxin, (ii) neurotoxin in a complex that contained hemagglutinins, and (iii) neurotoxin in a complex that did not contain hemagglutinins. These preparations were injected directly into the stomachs or intestines of animals with or without ligation of the pylorus. The results of these studies help clarify the efficacy of neurotoxin absorption, both in the presence and in the absence of auxiliary proteins.
MATERIALS AND METHODS
Materials.
Reagents were purchased from Sigma Chemical Co. (St. Louis, Mo.), and additional laboratory supplies were obtained from Fisher Scientific (Malvern, Pa.). Two preparations, BoNT/A complex with hemagglutinins and pure neurotoxin from strain 62A, were purified by procedures described in the literature (6, 24, 28). A third BoNT/A complex without hemagglutinins from strain JMHI-001 (honey isolate) was purified as follows.
Strain JMHI-001, isolated from honey suspected in a case of infant botulism (15a), was grown in 2.0% NZ-Case TT (Quest)–1.0% yeast extract (Difco)–0.5% glucose (Mallinckrodt) medium adjusted to pH 7.2. A 2-liter neurotoxin production culture was grown for 5 days at 37°C, and the neurotoxin was precipitated by addition of 3 N sulfuric acid to pH 3.2. The precipitated neurotoxin was collected by centrifugation and extracted in 0.2 M sodium phosphate buffer (pH 6.0) for 2 h. After centrifugation, the extracted neurotoxin was precipitated by making the solution 60% saturated with ammonium sulfate. The precipitated neurotoxin was collected by centrifugation, dissolved in 0.05 M sodium citrate buffer (pH 5.5), and then clarified by centrifugation and loaded on to a DEAE–Sephadex A-50 column equilibrated with 0.05 M sodium citrate buffer (pH 5.5). The neurotoxin-containing fractions were pooled and precipitated by making a solution 60% saturated with ammonium sulfate. A 2-mg sample of the precipitated toxin was collected by centrifugation and dissolved in 1 ml of 30 mM sodium phosphate–0.2 M sodium chloride (pH 6.8). Neurotoxin samples were gel filtered on a Superose 6 (Pharmacia) column (1.6 by 90 cm), and the complex eluted in fractions representing a molecular size of 270 to 300 kDa.
Animals.
Swiss Webster mice (female, 20 to 25 g), which were purchased from Ace Animals (Boyertown, Pa.), were housed in an accredited animal colony (American Association for Accreditation of Laboratory Animal Care) and allowed unrestricted access to food and water. All procedures involving animals were reviewed and approved by the Thomas Jefferson University Institutional Animal Care and Use Committee.
Surgical procedures.
The preoperative protocol involved fasting animals for 18 h prior to surgery while allowing them free access to water. Preoperative preparation also included shaving the abdominal area and administering a prophylactic, subcutaneous dose of gentamicin sulfate (6 mg/kg; Fujusawa USA, Inc., Deerfield, Ill.). On the day of surgery, the animals were transferred to a veterinary procedure room, and all subsequent steps were performed in an aseptic surgical environment.
Animals were anesthetized by administration of Isoflurane (Iso-thesia; Abbott Laboratories North, Chicago, Ill.)-oxygen, and the same inhalation anesthetic was administrated throughout surgery. An abdominal laparotomy (∼1.5 to 2.5 cm, depending on the size of the mouse) was performed, and either the stomach or the small intestine immediately proximal to the stomach was partially externalized. If required by protocol, a ligature with 3-0 Prolene (polypropylene suture; Ethicon, Inc., Somerville, N.J.) was placed immediately above (proximal to the stomach) the pyloric sphincter. Care was taken that this ligature was sufficient to prevent the flow of stomach juices into the intestine (or reverse flow of intestinal contents into the stomach) but not sufficient to cause mechanical damage to the tissues involved. Neurotoxin was administered through a 1-ml tuberculin syringe with a 0.5-in., 27-gauge needle. Injection volumes were kept constant at 100 μl per animal regardless of the site of administration (stomach or intestine). For all injections, the vehicle consisted of sterile Dulbecco’s phosphate-buffered saline (pH 7.4) with 1 mg of bovine serum albumin per ml. Neurotoxin was administered into the lumen of the stomach by injection through the stomach wall at the greater curvature, with care being taken to avoid the gastro-epiploic vessels. Neurotoxin was administered into the lumen of the small intestine by oblique insertion of the needle parallel to the segment and always in a direction away from the stomach. The time of injection was recorded.
After administration of neurotoxin, the organs were gently repositioned and the incision in the abdominal muscle was sutured using 3-0 Prolene. The skin was closed with several small wound clips, after which the animals received a 2-mg/kg subcutaneous analgesic injection of Buprenorphine hydrochloride (Buprenex injectable; Reckitt & Colman Pharmaceuticals, Inc., Richmond, Va.) and another dose of gentamicin.
The surgical procedure lasted approximately 15 min per animal, and suspension of anesthesia resulted in full recovery within 10 to 15 min. The animals were then transferred to the laboratory, where they were monitored for assay endpoint. The time of death was recorded, and total elapsed time (in minutes) from time of injection to time of death was calculated.
Toxin dosage.
Protein concentrations were routinely determined by the Bradford assay (2). For pure neurotoxin, the concentration was determined spectrophotometrically at 278 nm by using the relationship 1.63A278 = 1 mg/ml, where A278 is the absorbance at 278 nm (6). For dosage calculations involving complexes, the neurotoxin content was estimated to be ∼35% of the total protein in the complex with hemagglutinins (150 kDa/400 kDa) (11, 19), and ∼55% in the complex without hemagglutinins (150 kDa/270 kDa). By using that fraction as an estimate of the amount of neurotoxin in the complex, a concentration of complex was selected that represented an equivalent of 1 μg of pure neurotoxin. Subsequently, 1 μg of pure neurotoxin and a sample of complex containing an equivalent of 1 μg of neurotoxin were run on a gel, and the intensity of the neurotoxin bands was compared. The accuracy of the estimate was further checked by intraperitoneal injection into mice and comparison of survival times. Thus, when pure neurotoxin and complexes were administered in a particular experiment, the samples contained equivalent amounts of neurotoxin although the complexes contained more protein.
Electrophoresis.
Neurotoxin samples were separated in 7.5% polyacrylamide gels by the method of Laemmli (14) under reducing or nonreducing conditions. Gels were stained with Coomassie blue for 30 min, destained, and photographed.
Statistical analyses.
All data derived from three or more separate experiments are presented as means ± standard errors of the mean (SEM). The equality of variances was tested by the F test. Subsequently, P values were calculated by either a two-sample t test for independent samples with equal variances or a two-sample t test for independent samples with unequal variances (Cochran’s method).
Preliminary experiments established that differences in animal cohort, age, and weight could have marked effects on the outcome of experiments. Therefore, statistical significance was tested only when data sets were part of the same experiment.
RESULTS
C. botulinum serotype A neurotoxin and associated proteins.
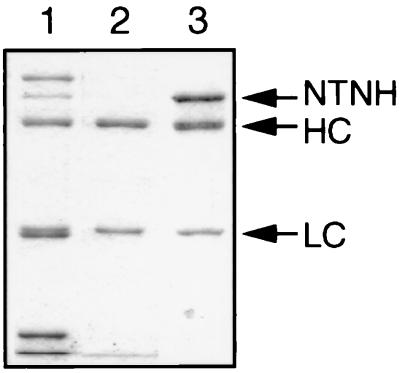
Three neurotoxin preparations were used in this study: neurotoxin not in a complex and two forms of neurotoxin in complex. BoNT/A that is free of auxiliary proteins is not typically found in nature. This material, which was purified in the laboratory, is referred to here as pure neurotoxin. BoNT/A is found in nature as one component of several noncovalently associated complexes (11). One of these is a 16S complex (∼400 kDa) consisting of neurotoxin (∼150 kDa), a nontoxin, nonhemagglutinin protein (∼120 to 140 kDa), and hemagglutinins (∼52, 35, 20, 19, and 15 kDa). This complex is referred to here as HA+ complex. The second complex (∼270 kDa) consists of pure neurotoxin and nontoxin, nonhemagglutinin but does not contain hemagglutinins. Therefore, it is referred to here as HA− complex. Figure 1 illustrates gels of the neurotoxin preparations that were used in this study.
FIG. 1.
Comparison of BoNT components. Neurotoxin samples were prepared in reducing buffer and run on 7.5% polyacrylamide gels. Three samples of serotype A neurotoxin were used in this study. Lane 1, neurotoxin from strain 62A, HA+ complex, showing nontoxin, nonhemagglutinin (NTNH), neurotoxin heavy-chain (HC) and light-chain (LC), and hemagglutinin bands. Lane 2, neurotoxin from strain 62A, pure neurotoxin, showing neurotoxin heavy and light chains. Lane 3, neurotoxin from strain JMH1-001 neurotoxin, HA− complex, showing the nontoxin nonhemagglutinin and neurotoxin heavy and light chains.
Protocols for analysis of in vivo neurotoxin activity.
Two types of experimental approaches were used to evaluate the ability of neurotoxin to escape the GI system and produce neuromuscular blockade. In the first approach, the pyloric sphincter was ligated, after which neurotoxin was injected into the stomach or into the intestine. Neurotoxin was administered in 100 μl of buffered saline solution (pH 7.4) that also contained 1 mg of protein (bovine serum albumin) per ml. The purpose of the ligation was to ensure that neurotoxin absorption could occur only at the site of injection (i.e., stomach or intestine). The purpose of the bolus of buffered solution with protein was to reduce the rate and extent of pH-dependent neurotoxin degradation.
In the second approach, neurotoxin was administered without ligation. This approach allowed the neurotoxin to move from the stomach to the intestine (as would occur in oral poisoning) or from the intestine to the stomach (as might occur following colonization of the bowel by Clostridium botulinum). As before, neurotoxin was administered in a buffered solution with protein to diminish pH-dependent degradation.
Absorption of neurotoxin complexes in ligated preparations.
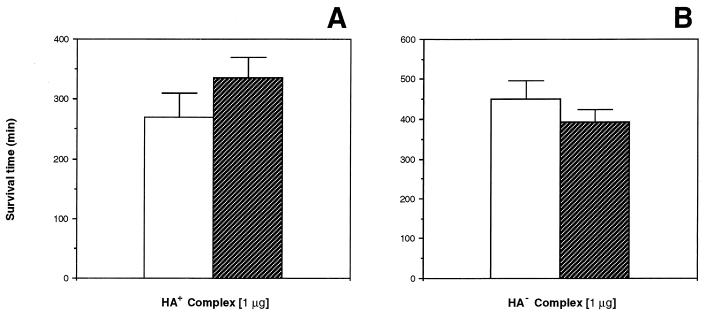
Experiments were done to assess the absorption of HA+ and HA− complexes from the stomach and the intestine. The purpose of the experiments was to determine whether the rates of absorption in the stomach and intestine differed as a function of the presence or absence of hemagglutinin.
Figure 2 illustrates that the apparent toxicity of HA+ complex containing the equivalent of 1 μg of neurotoxin was the same whether administered into the stomach or into the intestine. The difference in survival time for the two groups was not statistically significant (P < 0.30). The figure illustrates that a qualitatively similar result was obtained when HA− complex was injected into stomach or intestine. Once again, the difference in survival times was not statistically significant (P < 0.40). Thus, under conditions that maximize the opportunity for absorption while reducing the potential for degradation, the absorption of each complex was approximately equivalent at both sites of administration.
FIG. 2.
BoNT/A complex absorption from the stomach and the small intestine. The pylorus was ligated, and mice were injected with HA+ complex or HA− complex. Neurotoxin complex introduced into the intestine is represented by the open bars, and complex introduced into the stomach is represented by the hatched bars. (A) HA+ complex with hemagglutinins. (B) HA− complex without hemagglutinins. HA+ complex (equivalent to 1 μg of neurotoxin/animal): stomach, n = 9; intestine, n = 9. HA− complex (equivalent to 1 μg neurotoxin/animal): stomach, n = 10; intestine, n = 12. Results are means and SEM.
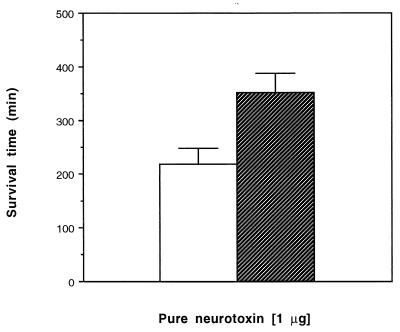
Absorption of pure neurotoxin isolated in ligated preparations.
An identical series of experiments was performed with pure neurotoxin (1 μg/animal). The results, which are illustrated in Fig. 3, demonstrated two things. First, pure neurotoxin was absorbed from both sites, meaning that neither hemagglutinin nor the nontoxin, nonhemagglutinin is absolutely essential for uptake. Second, the survival times of animals receiving pure neurotoxin in the intestine were significantly shorter than those of animals receiving pure neurotoxin in the stomach (P < 0.01). This difference could be due to greater metabolism of pure neurotoxin in the stomach, lesser absorption in the stomach, or a combination of the two.
FIG. 3.
Pure BoNT/A absorption from the stomach and small intestine. Pure neurotoxin (1 μg/animal) was injected into the stomach or into the intestine. Neurotoxin introduced into the intestine is represented by the open bar, and neurotoxin introduced into the stomach is represented by the hatched bar. Pure neurotoxin (1 μg/animal): stomach, n = 14; intestine, n = 18. Results are means and SEM.
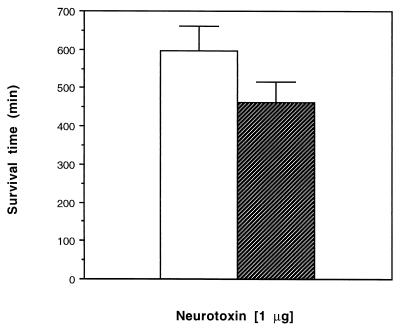
Absorption of pure neurotoxin and HA+ complex in nonligated preparations.
Pure neurotoxin and HA+ complex (equivalent to 1 μg of neurotoxin/animal) were administered in a bolus of buffered solution into the stomach of animals in which the pyloric sphincter was not ligated. As shown in Figure 4, the toxicity of the HA+ complex appeared greater than that of pure neurotoxin. However, the difference in survival times did not attain statistical significance (P < 0.20).
FIG. 4.
BoNT/A complex protection in the stomach. Mice were injected with pure neurotoxin or HA+ complex. Samples were introduced into the stomach and allowed unrestricted passage into the intestine. Pure neurotoxin introduced into the stomach is represented by the open bar, and HA+ complex introduced into the stomach is represented by the hatched bar. HA+ complex (equivalent to 1 μg of neurotoxin/animal), n = 6; pure neurotoxin (1 μg/animal), n = 6. Results are means and SEM.
Dose dependence of pure neurotoxin and HA+ complex uptake in nonligated preparations.
The data presented above indicate that (i) pure neurotoxin can be absorbed from the stomach and (ii) auxiliary proteins may protect neurotoxin, thus giving a greater apparent toxicity for an equivalent amount of neurotoxin. If these points are correct, they suggest that the apparent difference in potency between pure neurotoxin and neurotoxin in complex would be greatest at low neurotoxin concentrations (i.e., the rate of metabolism of pure neurotoxin may exceed the rate of absorption). Therefore, experiments similar to those in the preceding section were done but with a lower neurotoxin concentration (25 ng/animal). In addition, injections were administered in the stomach and in the intestine.
As shown in Table 1, injections of pure neurotoxin and HA+ complex into the stomach produced strikingly different results. There were no deaths among animals receiving pure neurotoxin whereas there was only one survival among 10 animals receiving HA+ complex. By contrast, when pure neurotoxin and HA+ complex were injected into the intestine, the end result was the same (one survival after 4 days).
TABLE 1.
Toxicity of C. botulinum serotype A pure neurotoxin and neurotoxin complex injected into the stomach or intestinea
| Time (h) | Survival (no. alive/total no.) after injection of:
|
|||
|---|---|---|---|---|
| Pure neurotoxin
|
HA+ complex
|
|||
| Stomach | Intestine | Stomach | Intestine | |
| 24 | 0/10 | 1/10 | 5/10 | 7/10 |
| 48 | 0/10 | 6/10 | 9/10 | 9/10 |
| 72 | 0/10 | 9/10 | 9/10 | 9/10 |
| 96 | 0/10 | 9/10 | 9/10 | 9/10 |
Mice were injected with pure neurotoxin or HA+ complex. Samples were introduced directly into the stomach or directly into the intestine. No ligature was used to restrict neurotoxin movement. Animals were monitored, and the number of deaths was recorded at the end of each time period. Pure neurotoxin (25 ng/animal) and HA+ complex (equivalent to 25 ng of pure neurotoxin/animal) were used.
DISCUSSION
BoNT is a remarkably potent substance that acts on the peripheral nervous system to cause a disease characterized by flaccid paralysis. In the overwhelming majority of cases, the disease is due to ingestion of neurotoxin or to ingestion of bacteria that produce the neurotoxin (9, 18, 25, 27). In either case, the neurotoxin escapes the GI system to reach the general circulation and eventually the peripheral nervous system. It acts on cholinergic nerve endings to block the release of acetylcholine, and this in turn produces the characteristic outcome of flaccid paralysis (12, 17, 19, 23, 26).
The fact that the oral route is the primary mode of neurotoxin entry into the body makes it obvious that there must be an effective mechanism for it to cross gut membranes. Unfortunately, there is little information available on the mechanism that accounts for penetration of these membranes. One of the major impediments to studying transcellular movement of the neurotoxin is that this substance by itself rarely if ever causes disease. In nature, botulinum neurotoxin is ordinarily found in a complex with one or more auxiliary proteins (11, 19). These proteins almost certainly help protect the neurotoxin from degradation by low pH and proteolytic enzymes in the gut (1, 3, 8, 20–22, 29, 30). The presence of these proteins in a complex with the neurotoxin, coupled with their ability to protect it from degradation, complicates efforts to assess how and where the neurotoxin is absorbed.
In the present study, an effort was made to gain insight into the mechanisms that govern neurotoxin absorption. For this purpose, three different preparations were used: pure neurotoxin, HA+ complex, and HA− complex. In most experiments, these preparations were administered to animals in which the pylorus was ligated, thus ensuring that neurotoxin absorption could occur only in the vicinity of its administration. In addition, a buffered solution with protein was used as a vehicle to reduce pH-dependent degradation and thus maximize the opportunity for absorption.
The most important observation to emerge from the study was that pure neurotoxin is capable of being absorbed from both the stomach and the intestine. Neither the hemagglutinin proteins nor the nontoxin nonhemagglutinin protein is absolutely essential for absorption. This observation appears to be at odds with the work of Fujinaga et al. (7), who reported that hemagglutinin plays a critical role in intestinal absorption of BoNT/C. However, the observation is consistent with a larger body of findings. To begin with, BoNT from strain JMH1-001 is capable of producing oral poisoning in humans. Indeed, this strain was isolated from honey implicated in an outbreak of infant botulism (15a). Interestingly, the genome of strain JMH1-001 does not contain the gene for hemagglutinin, and therefore it is impossible that hemagglutinin can participate in—let alone be essential for—poisoning due to neurotoxin from this strain.
In a separate line of investigation, Kiyatkin et al. (13) used techniques of molecular biology to generate a botulinum holotoxin that was modified in a site that governs neurotoxicity. Oral administration of this modified holotoxin did not produce any of the signs of botulism but did elicit the production of systemic antibodies that neutralized native neurotoxin. This result strongly implies that the expression product, which was entirely free of hemagglutinin, was capable of being absorbed from the gut.
Finally, Maksymowych and Simpson (15) have reported that homogeneous BoNT binds specifically to T-84 cells and is actively transported from the apical (luminal) to the basal (serosal) side of cells. The product that is released on the basal side is native neurotoxin capable of producing in vivo and in vitro blockade of neuromuscular transmission. Once again, the data indicate that no auxiliary protein is absolutely essential for the neurotoxin to cross gut membranes.
The fact that auxiliary proteins are not required for absorption does not necessarily mean that they do not participate in absorption. The data support the conclusion that pure neurotoxin can cross gut membranes, but they do not rule out the possibility that the neurotoxin-auxiliary protein complex can also cross membranes. It is conceivable that both free neurotoxin and neurotoxin in complex have an exposed domain that can associate with receptors that mediate transcytosis. It would be desirable to determine the comparative rates for transcytosis of free neurotoxin and of neurotoxin-auxiliary protein complex. Experiments on rates of association with cell surface receptors and rates of transcytosis would more appropriately be done on isolated cell systems (e.g., T-84 cells) than on live animals.
It should be noted that nothing in this study challenges the premise that the intestine is a major site, and perhaps the principal site, of neurotoxin absorption. What the work does demonstrate is that under the proper circumstances, the stomach as well as the intestine can be a site of absorption. Furthermore, nothing in the study challenges the widely held belief that auxiliary proteins protect the neurotoxin from degradation, especially in the stomach. However, the work shows that the importance of this protection is dose dependent.
The fact that the protective role of auxiliary proteins depends on the administered dose is not surprising. When pure neurotoxin enters the stomach, it is subject to two processes: (i) metabolism, which reduces the likelihood of poisoning, and (ii) absorption, which increases the likelihood of poisoning. Each of these processes is governed by its respective affinity constants and rate constants. If affinity constants favor metabolism over absorption, then low doses of pure neurotoxin are more likely to be degraded than to produce neuromuscular blockade. However, as the concentration of pure neurotoxin in the stomach approaches or exceeds the affinity constants for metabolism, the fractional concentration available for absorption also increases.
There is a logical extension of these arguments that pertains to auxiliary proteins. Under conditions in which the fractional absorption of neurotoxin is low (i.e., low concentration and substantial metabolism), the potential protective effect of auxiliary proteins could be substantial. However, under conditions in which the fractional absorption of neurotoxin is high (i.e., high neurotoxin concentration), the potential protective effect of auxiliary proteins would not be as obvious. These expectations were reflected in the experimental findings. When administered at a dose of 25 ng/animal, the protective effect of auxiliary proteins was obvious in the survival data (Table 1). Conversely, when the dose was incremented substantially (1 μg/animal), the protective effect of auxiliary protein was difficult to detect.
As indicated above, this work provides the first clear demonstration that homogeneous BoNT can be absorbed from the gut to produce peripheral neuromuscular blockade. The work also highlights the importance of using different experimental preparations and experimental conditions to separate the role of auxiliary proteins in the process of absorption from the role of these proteins in the process of metabolism.
ACKNOWLEDGMENTS
We thank Fred Rock for his advice regarding all surgical aspects and Meghan Gerzevske for preoperative support during the course of this study. We also thank Bibhuti DasGupta for advice and guidance regarding purification of BoNT/A.
This work was supported by NINDS grant NS-22153 to L.L.S. Research in the laboratory of E.A.J. was supported by grants from the USDA, NIH (RO1 AI2226-01A1), and College of Agricultural and Life Sciences.
REFERENCES
- 1.Bonventre P F. Absorption of botulinal toxin from the gastrointestinal tract. Rev Infect Dis. 1979;1:663–667. doi: 10.1093/clinids/1.4.663. [DOI] [PubMed] [Google Scholar]
- 2.Bradford M M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 3.Chen F, Kuziemko G M, Stevens R C. Biophysical characterization of the stability of the 150-kilodalton botulinum toxin, the nontoxic component, and the 900-kilodalton botulinum toxin complex species. Infect Immun. 1998;66:2420–2425. doi: 10.1128/iai.66.6.2420-2425.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman I W. Studies on the oral toxicity of Clostridium botulinum toxin, type A. Can J Biochem Physiol. 1954;32:27–34. [PubMed] [Google Scholar]
- 5.Dack G M. Behavior of botulinum toxin in alimentary tract of rats and guinea-pigs. J Infect Dis. 1926;38:174–181. [Google Scholar]
- 6.DasGupta B R, Sathyamoorthy V. Purification and amino acid composition of type A botulinum neurotoxin. Toxicon. 1984;22:415–424. doi: 10.1016/0041-0101(84)90085-0. [DOI] [PubMed] [Google Scholar]
- 7.Fujinaga Y, Inoue K, Watanabe S, Yokota K, Hirai Y, Nagamachi E, Oguma K. The haemagglutinin of Clostridium botulinum type C progenitor toxin plays an essential role in binding of toxin to the epithelial cells of guinea pig small intestine, leading to the efficient absorption of the toxin. Microbiology. 1997;143:3841–3847. doi: 10.1099/00221287-143-12-3841. [DOI] [PubMed] [Google Scholar]
- 8.Halliwell G. The action of proteolytic enzymes on Clostridium botulinum type A toxin. Biochem J. 1954;58:4–8. doi: 10.1042/bj0580004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hatheway C L. Botulism: the present status of the disease. Curr Top Microbiol Immunol. 1995;195:55–75. doi: 10.1007/978-3-642-85173-5_3. [DOI] [PubMed] [Google Scholar]
- 10.Heckly R J, Hildebrand G J, Lamanna C. On the size of the toxic particle passing the intestinal barrier in botulism. J Exp Med. 1960;111:745–759. doi: 10.1084/jem.111.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inoue K, Fujinaga Y, Wanatabe T, Ohyama T, Takeshi K, Moriishi K, Nakajima H, Inoue K, Oguma K. Molecular composition of Clostridium botulinum type A progenitor toxins. Infect Immun. 1996;64:1589–1594. doi: 10.1128/iai.64.5.1589-1594.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jahn R, Hanson P I, Otto H, Ahnert H G. Botulinum and tetanus neurotoxins: emerging tools for the study of membrane fusion. Cold Spring Harbor Symp Quant Biol. 1995;60:329–335. doi: 10.1101/sqb.1995.060.01.037. [DOI] [PubMed] [Google Scholar]
- 13.Kiyatkin N, Maksymowych A B, Simpson L L. Induction of an immune response by oral administration of recombinant botulinum toxin. Infect Immun. 1997;65:4586–4591. doi: 10.1128/iai.65.11.4586-4591.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laemmli U K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 15.Maksymowych A B, Simpson L L. Binding and transcytosis of botulinum neurotoxin by polarized human colon carcinoma cells. J Biol Chem. 1998;273:21950–21957. doi: 10.1074/jbc.273.34.21950. [DOI] [PubMed] [Google Scholar]
- 15a.Malizio, C. J., and G. A. Johnson. Unpublished data.
- 16.May A J, Whaler B C. The absorption of Clostridium botulinum type A toxin from the alimentary canal. Br J Exp Pathol. 1958;39:307–316. [PMC free article] [PubMed] [Google Scholar]
- 17.Montecucco C, Schiavo G. Mechanism of action of tetanus and botulinum neurotoxins. Mol Microbiol. 1994;13:1–8. doi: 10.1111/j.1365-2958.1994.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 18.Montecucco C, Schiavo G, Rossetto O. The mechanism of action of tetanus and botulinum neurotoxins. Arch Toxicol Suppl. 1996;18:342–354. doi: 10.1007/978-3-642-61105-6_32. [DOI] [PubMed] [Google Scholar]
- 19.Oguma K, Fujinaga Y, Inoue K. Structure and function of Clostridium botulinum toxins. Microbiol Immunol. 1995;39:161–168. doi: 10.1111/j.1348-0421.1995.tb02184.x. [DOI] [PubMed] [Google Scholar]
- 20.Ohishi I. Oral toxicities of Clostridium botulinum type A and B toxins from different strains. Infect Immun. 1984;43:487–490. doi: 10.1128/iai.43.2.487-490.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ohishi I, Sakaguchi G. Oral toxicities of Clostridium botulinum type C and D toxins of different molecular sizes. Infect Immun. 1980;28:303–309. doi: 10.1128/iai.28.2.303-309.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohishi I, Sugii S, Sakaguchi G. Oral toxicities of Clostridium botulinum toxins in response to molecular size. Infect Immun. 1977;16:107–109. doi: 10.1128/iai.16.1.107-109.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossetto O, Deloye F, Poulain B, Pellizzari R, Schiavo G, Montecucco C. The metallo-proteinase activity of tetanus and botulism neurotoxins. J Physiol (Paris) 1995;89:43–50. doi: 10.1016/0928-4257(96)80550-X. [DOI] [PubMed] [Google Scholar]
- 24.Sakaguchi G. Clostridium botulinum toxins. Pharmacol Ther. 1982;19:165–194. doi: 10.1016/0163-7258(82)90061-4. [DOI] [PubMed] [Google Scholar]
- 25.Sanders A B, Seifert S, Kobernick M. Botulism. J Fam Pract. 1983;16:987–1000. [PubMed] [Google Scholar]
- 26.Schiavo G, Rossetto O, Tonello F, Montecucco C. Intracellular targets and metalloprotease activity of tetanus and botulism neurotoxins. Curr Top Microbiol Immunol. 1995;195:257–274. doi: 10.1007/978-3-642-85173-5_12. [DOI] [PubMed] [Google Scholar]
- 27.Simpson L L, editor. Botulinum neurotoxins and tetanus toxin. New York, N.Y: Academic Press, Inc.; 1989. [Google Scholar]
- 28.Simpson L L, Schmidt J J, Middlebrook J L. Isolation and characterization of the botulinum neurotoxins. Methods Enzymol. 1988;165:76–85. doi: 10.1016/s0076-6879(88)65015-4. [DOI] [PubMed] [Google Scholar]
- 29.Sugii S, Ohishi I, Sakaguchi G. Correlation between oral toxicity and in vitro stability of Clostridium botulinum type A and B toxins of different molecular sizes. Infect Immun. 1977;16:910–914. doi: 10.1128/iai.16.3.910-914.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sugii S, Ohishi I, Sakaguchi G. Intestinal absorption of botulinum toxins of different molecular sizes in rats. Infect Immun. 1977;17:491–496. doi: 10.1128/iai.17.3.491-496.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]