Key Points
Question
Is posterior surgery noninferior to anterior surgery for clinical outcomes among patients with cervical radiculopathy?
Findings
In this multicenter randomized clinical trial including 265 patients with cervical foraminal radiculopathy, posterior surgery was noninferior to anterior surgery regarding success rate and arm pain 1 year after surgery. Decrease in arm pain and all secondary outcomes had comparable small between-group differences.
Meaning
These findings suggest noninferiority of posterior surgery compared to anterior surgery and may be used to inform patient counseling and shared decision-making between physicians and patients with 1-sided foraminal radiculopathy.
This randomized clinical trial evaluates the noninferiority of posterior surgery to anterior surgery for outcomes in patients with cervical radiculopathy at 1 year.
Abstract
Importance
The choice between posterior cervical foraminotomy (posterior surgery) and anterior cervical discectomy with fusion (anterior surgery) for cervical foraminal radiculopathy remains controversial.
Objective
To investigate the noninferiority of posterior vs anterior surgery in patients with cervical foraminal radiculopathy with regard to clinical outcomes after 1 year.
Design, Setting, and Participants
This multicenter investigator-blinded noninferiority randomized clinical trial was conducted from January 2016 to May 2020 with a total follow-up of 2 years. Patients were included from 9 hospitals in the Netherlands. Of 389 adult patients with 1-sided single-level cervical foraminal radiculopathy screened for eligibility, 124 declined to participate or did not meet eligibility criteria. Patients with pure axial neck pain without radicular pain were not eligible. Of 265 patients randomized (132 to posterior and 133 to anterior), 15 were lost to follow-up and 228 were included in the 1-year analysis (110 in posterior and 118 in anterior).
Interventions
Patients were randomly assigned 1:1 to posterior foraminotomy or anterior cervical discectomy with fusion.
Main Outcomes and Measures
Primary outcomes were proportion of success using Odom criteria and decrease in arm pain using a visual analogue scale from 0 to 100 with a noninferiority margin of 10% (assuming advantages with posterior surgery over anterior surgery that would justify a tolerable loss of efficacy of 10%). Secondary outcomes were neck pain, disability, quality of life, work status, treatment satisfaction, reoperations, and complications. Analyses were performed with 2-proportion z tests at 1-sided .05 significance levels with Bonferroni corrections.
Results
Among 265 included patients, the mean (SD) age was 51.2 (8.3) years; 133 patients (50%) were female and 132 (50%) were male. Patients were randomly assigned to posterior (132) or anterior (133) surgery. The proportion of success was 0.88 (86 of 98) in the posterior surgery group and 0.76 (81 of 106) in the anterior surgery group (difference, −0.11 percentage points; 1-sided 95% CI, −0.01) and the between-group difference in arm pain was −2.8 (1-sided 95% CI, −9.4) at 1-year follow-up, indicating noninferiority of posterior surgery. Decrease in arm pain had a between-group difference of 3.4 (1-sided 95% CI, 11.8), crossing the noninferiority margin with 1.8 points. All secondary outcomes had 2-sided 95% CIs clustered around 0 with small between-group differences.
Conclusions and Relevance
In this randomized clinical trial, posterior surgery was noninferior to anterior surgery for patients with cervical radiculopathy regarding success rate and arm pain at 1 year. Decrease in arm pain and secondary outcomes had small between-group differences. These results may be used to enhance shared decision-making.
Trial Registration
Netherlands Trial Register Identifier: NTR5536
Introduction
During the next decades, the aging population worldwide is forecasted to increase considerably. This will also increase the frequency of age-related degenerative changes, such as cervical radiculopathy arising from intervertebral disc herniation or osteophyte formation compressing the nerve root. Patients with cervical radiculopathy typically have pain with or without neurological deficit in the innervation area of the nerve root, potentially leading to a physically disabling condition and reduced quality of life.1,2
If conservative treatment fails, the choice of surgical intervention remains controversial. Two widely used interventions are posterior cervical foraminotomy (posterior surgery) or anterior cervical discectomy with fusion (ACDF; anterior surgery). Although posterior surgery involves fewer vital structures than anterior surgery (eg, esophagus, carotid artery, and recurrent laryngeal nerve) and does not require costly implants, surgeons still tend to prefer the latter.3,4 Both techniques have been shown to yield similar clinical outcomes; however, these findings are based on retrospective cohort studies and 1 low-quality randomized clinical trial with few patients.5,6,7,8 A randomized clinical trial with a predefined sample size directly comparing the 2 techniques is needed to elucidate the existing controversy in cervical spine surgery.
The Foraminotomy ACDF Cost-Effectiveness Trial (FACET) was designed to compare the clinical- and cost-effectiveness of posterior vs anterior surgery in patients with cervical radiculopathy due to foraminal nerve root compression. Posterior surgery was hypothesized to be noninferior to anterior surgery. The trial includes a follow-up of 2 years. The current study presents the clinical effectiveness results at 1 year of follow-up.
Methods
Trial Design
FACET is a multicenter investigator-blinded noninferiority randomized clinical trial. The trial design has been described previously9 (Supplements 1-2) and is reported according to the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.10 The study protocol was approved by the research ethical board of the University Medical Center Groningen, the Netherlands. All patients provided written informed consent before randomization.
FACET enrolled patients aged 18 to 80 years with 1-sided single-level cervical foraminal radiculopathy due to soft disc herniation or spondylotic changes requiring surgical decompression from 9 hospitals in the Netherlands. Patients with pure axial neck pain without radicular pain were not eligible. The radiological definition of neuroforaminal compression and full eligibility criteria are described in the protocol (Supplements 1-2).9
Treatment and Randomization
Participants were randomly assigned in a 1:1 ratio using an independent institute web-based block randomization design (Trans European Network for Clinical Trials Services [TENALEA]) stratified by hospital. Due to the nature of the surgical procedures, blinding of patients and surgeons was not possible. Procedures were performed by neurosurgeons acquainted with both surgical techniques. The correct level was verified by fluoroscopy. Anterior cervical discectomy with fusion was performed with a standard ventral approach.11 After discectomy, with reduction of the uncovertebral joint if needed, a cage or bone cement was applied in the intervertebral space (eTable 1 in Supplement 4). Posterior cervical foraminotomy was performed in a prone position. Partial hemilaminectomy and foraminotomy of the involved level was performed.12 Soft disc herniations and osteophytes were removed when necessary. No additional plate fixation or postsurgical neck brace was applied in either technique.
The trial was performed in the context of care as usual, including 1 visit to the outpatient clinic 6 weeks after surgery. Patients were requested to fill out a web-based questionnaire in a secure online environment at each follow-up point, including 1 year after surgery. Patients were contacted via telephone by a blinded interviewer to assess the Odom criteria and occurrence of adverse events. Clinical follow-up to 2 years is ongoing.
Outcomes
The proportion of a successful score (excellent or good) on the modified Odom criteria 4-point rating scale was centrally assessed and treated as primary outcome.12 The Odom criteria was chosen because of its wide adaption as a clinical outcome measure in spine surgery, including the study on which our sample size calculation was based.13 A second primary outcome was decrease in visual analogue scale (VAS) score for self-reported arm pain (0-100, with lower score at 1 year and higher change in score from baseline indicating a greater decrease in pain).14
Secondary outcomes were VAS score for neck pain, Neck Disability Index (10-item index, 0-50; sum of scores doubled to get a percentage), EuroQol 5-Dimensions 5-Level questionnaire (EQ-5D-5L), Work Ability Index Single-item, and treatment satisfaction (1-7 rating scale). Thresholds for minimal clinically important differences are reported in the study protocol (Supplements 1-2).9 Validated Dutch language versions of the questionnaires were used (eMethods in Supplement 4).15,16,17 Adverse events, including any unexpected medical occurrence in a patient without a necessarily causal relationship to the studied treatments, and reoperations were recorded. Adverse events were considered serious if they were lethal or life threatening, required prolongation of hospitalization, caused considerable disability, were a congenital anomaly or birth defect, or any other medically important event that jeopardized the patient or required intervention.
Statistical Analysis
The full statistical analysis plan can be found in Supplement 3. We hypothesized that the proportion of successful outcomes would be similar in posterior and anterior surgery and therefore used an overall success rate of 87% based on the largest available review in the literature13 with a noninferiority margin of 10%. This margin was based on the assumption that posterior surgery has some advantages over anterior surgery (eg, it avoids fusion-related complications, preserves postsurgical range of motion, and incurs lower costs),6,18,19,20,21 that would justify a tolerable loss of efficacy of 10%. A sample size of 308 patients was calculated that would give the trial 80% power to rule out a between-group difference in the success rate with an α of .05 and a dropout ratio of 10%. Unfortunately, a lower inclusion rate than anticipated was observed, partly due to the COVID-19–related cancellation of nonemergent health care. An interim analysis and power calculation (based on the actual proportions of patients with successful operations in the complete and full cases) by a statistician who was not involved in the study design indicated that it was safe to end the inclusion at 86% of the predefined sample size with a low risk of false negatives with a power of 0.98 (complete cases) and of 0.85 (full cases). As the trial was powered on the success rate according to the Odom criteria, an interim power analysis was not performed for decrease in arm pain. Details on post hoc power calculations for both primary outcomes are presented in eTable 2 in Supplement 4.
The main analysis was conducted on the intention-to-treat population, consisting of all the patients who were assigned to a treatment group and had data available at 1-year follow-up. The per-protocol population consisted of patients who were treated with posterior or anterior surgery (including crossovers) and had data available at 1-year follow-up. Sensitivity analyses were performed by simulating various scenarios to account for the missing data. As a measure of robustness, the fragility index—that is, the minimum number of patients whose status according to successful Odom score must change to convert a statistically significant result to nonsignificant—was also calculated.22 This was done by adding patients with successful operations to the anterior surgery group (stacking the odds against posterior surgery) until the noninferiority margin was reached in the above-mentioned scenarios.
A responder analysis of the secondary outcomes was conducted, in which the proportion of patients with a response to treatment was defined as those with an improvement from baseline to 1 year after surgery reaching or exceeding the predefined threshold of the minimal clinically important differences.
Categorical data were summarized as proportions, and continuous data as means with standard deviations, or (if nonnormally distributed) as medians and interquartile ranges. Noninferiority of the primary outcomes were tested with a 2-proportion z test at a 1-sided 95% CI with a noninferiority margin of 10% and Bonferroni correction for multiple testing. Secondary end points were analyzed exploratively at a 2-sided 95% CI, as no noninferiority margin for these outcomes was prespecified, using t tests for continuous data, and z tests for categorical outcomes. CIs for secondary outcomes were not adjusted for multiple comparison. No monitoring committee was incorporated, as the trial was qualified as a low-risk study. Analyses were performed in R version 4.0.5. (R Foundation). A significance level of .05 was used.
Results
Patient Characteristics
From January 2016 to May 2020, 389 patients were screened for eligibility and 265 were randomized (mean [SD] age, 51.2 [8.3]; 133 [50%] female and 132 [50%] male)(see eTables 3-5 in Supplement 4 for baseline characteristics of all randomized patients). Baseline characteristics were similar between treatment groups except for a minimal nonsignificant difference in sex distribution, radiological characteristics, and comorbidities (Table 1). Of the included patients, 265 were randomly assigned to posterior (132) or anterior (133) surgery. Twenty-five patients did not receive the allocated intervention (15 posterior and 10 anterior), most commonly due to spontaneous improvement of symptoms (5 posterior and 6 anterior) (Figure 1). As prespecified in the protocol, patients were considered lost to follow-up at 1 year when there was no information available on their Odom score and VAS-arm score. At 1-year follow-up, 9 patients (8%) in the posterior group and 6 (5%) in the anterior group were lost to follow-up. Thus, 110 patients (92%) in the posterior group and 118 (95%) in the anterior group were included in the 1-year analysis; among them, 98 patients in the posterior group and 106 in the anterior group had available data for the Odom score.
Table 1. Baseline Characteristics of Included Patients.
| Characteristic | No. (%)a | |
|---|---|---|
| Posterior surgery (n = 119) | Anterior surgery (n = 124) | |
| Age, mean (SD), y | 51.6 (8.5) | 51.0 (8.3) |
| Sex | ||
| Female | 66 (55) | 58 (47) |
| Male | 53 (45) | 66 (53) |
| Body mass index, median (IQR)b | 27 (24-30) | 27 (24-30) |
| Dermatome clinical diagnosis | ||
| C5 right | 1 (1) | 1 (1) |
| C5 left | 1 (1) | 0 (0) |
| C6 right | 29 (24) | 37 (30) |
| C6 left | 30 (25) | 24 (19) |
| C7 right | 21 (18) | 26 (21) |
| C7 left | 37 (31) | 36 (29) |
| Symptom duration, median (IQR), wk | 34 (26-52) | 32 (20-52) |
| ASA classificationc | ||
| I | 55 (46) | 66 (53) |
| II | 59 (50) | 53 (43) |
| III | 5 (4) | 5 (4) |
| Current smokingd | 53 (46) | 47 (39) |
| Current use of NSAIDse | 39 (33) | 35 (29) |
| Radiological characteristicsf | ||
| Discogenic (soft disc) | 48 (40) | 38 (31) |
| Spondylotic | 14 (12) | 14 (11) |
| Combined discogenic and spondylotic | 57 (48) | 70 (57) |
| Clinical characteristics | ||
| Radiating arm and neck pain | 56 (47) | 61 (49) |
| Radiating arm pain only | 63 (53) | 63 (51) |
| Loss of strength | 43 (36) | 51 (41) |
| Loss of sensibility | 79 (66) | 82 (66) |
| Tingling in fingers or hand | 93 (78) | 106 (85) |
| Comorbidities, No.g | ||
| Any | 66 (55) | 57 (46) |
| Cardiovascular | 36 | 26 |
| Pulmonary | 22 | 20 |
| Endocrine | 19 | 18 |
| Musculoskeletal | 16 | 14 |
| Gastrointestinal and liver | 7 | 10 |
| Neurological | 3 | 10 |
| Thromboembolic | 5 | 4 |
| Psychiatric | 2 | 2 |
| Oncological | 4 | 1 |
| Nephrological | 2 | 1 |
| Clinically relevant other | 2 | 4 |
Abbreviations: ASA, American Society of Anesthesiologists; NSAID, nonsteroidal anti-inflammatory drug.
Percentages may not total 100 because of rounding.
Calculated as the weight in kilograms divided by the square of the height in meters.
ASA classification ranges from I to VI, where higher classes indicate a greater risk. No patients had an ASA classification of IV or VI.
Data were missing for smoking status for 3 patients in the posterior surgery group and 2 in the anterior surgery group.
Data were missing for NSAID for 1 patient in the posterior and 2 in the anterior surgery group.
Radiological characteristics were missing for 2 patients in the anterior surgery group.
The specification of comorbidities is on event level (not patient level). Therefore, no percentages are given, since several patients had multiple comorbidities. See eTable 4 in Supplement 4 for an overview of the comorbidities per subsection.
Figure 1. Flow Diagram of Randomized Patients, Primary Treatment, and Follow-up Status.
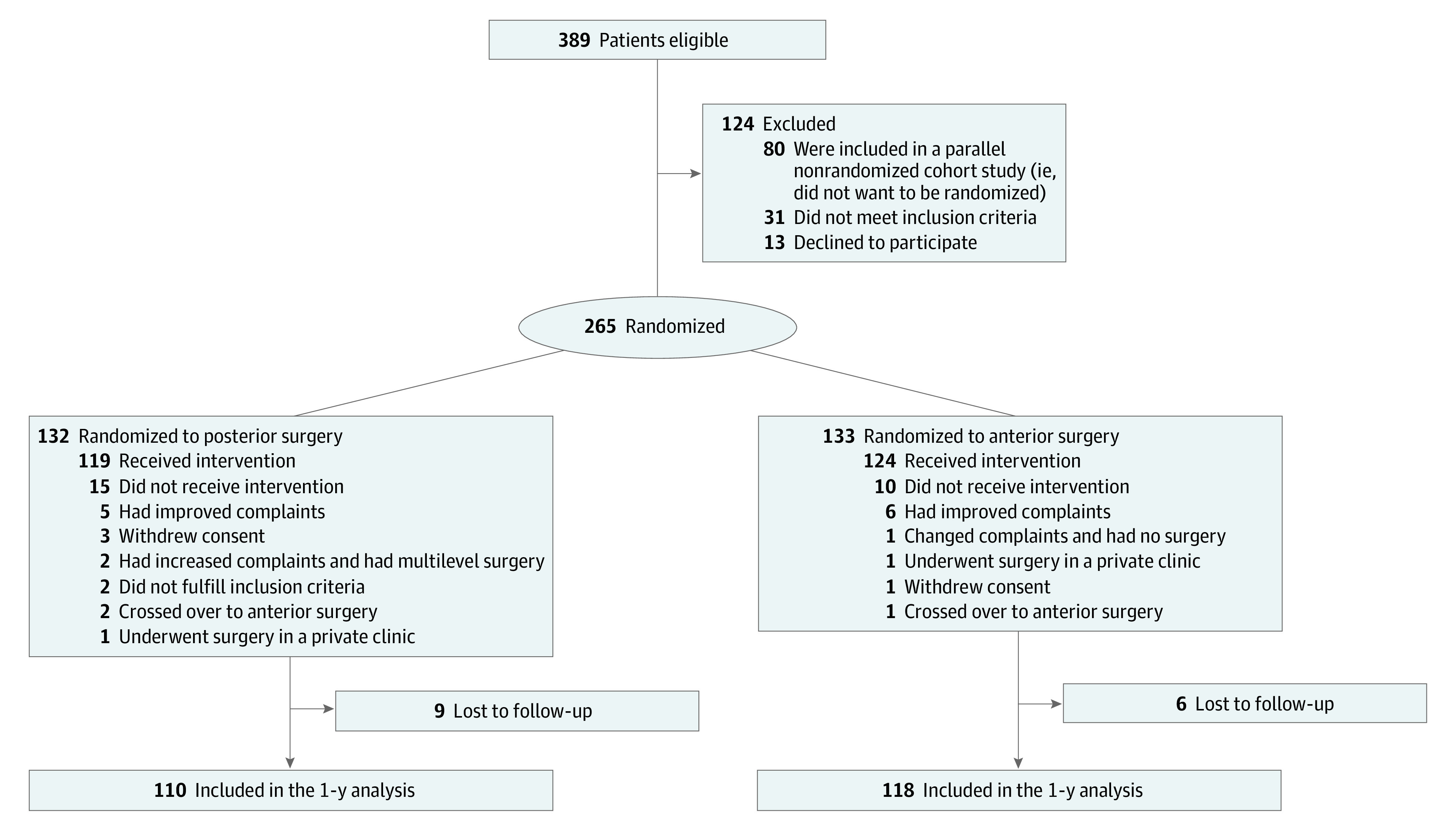
Participants who were included in the 1-year analyses had available data for either the Odom score or the Visual Analogue Score for arm pain, which were prespecified in the study protocol9 as the primary outcome measurements.
Primary Outcomes
In the intention-to-treat analysis with complete cases, the proportion of patients with a successful outcome at 1-year follow-up was 0.88 (86 of 98) in the posterior surgery group and 0.76 (81 of 106) in the anterior surgery group (difference, –0.11 percentage points; 1-sided 95% CI, −0.01) (Figure 2). As the point estimate and CI of the difference were 21% and 11% lower than the noninferiority margin of 10%, respectively, noninferiority of posterior surgery compared to anterior surgery was demonstrated. As the CI did not encompass 0, the superiority margin was also satisfied for this particular outcome measure. With 3 crossover patients, the per-protocol analysis yielded similar results. Sensitivity analyses using full cases with all remaining data coded as unsuccessful and predefined sample sizes indicated robustness of the noninferiority result. The mean (SD) arm pain decreased from 62.3 (20.7) at baseline to 18.6 (22.9) at 1 year in the posterior surgery group and from 60.3 (22.1) to 15.8 (23.7) in the anterior surgery group. The mean (SD) between-group difference in arm pain at 1 year was −2.8 (1-sided 95% CI, −9.4), indicating noninferiority. The mean (SD) between-group difference for the change score in arm pain was 3.4 (1-sided 95% CI, 11.8). As the 1-sided 95% CI crosses the 10% noninferiority margin with 1.8 points, there is insufficient evidence to regard this result as noninferior. The proportions of patients who reached the minimal clinically important differences for this outcome were 0.54 in the posterior surgery group and 0.60 in the anterior surgery group (difference, 0.06 percentage points; 2-sided 95% CI, −0.09 to 0.2), indicating no clinically relevant difference between treatment groups (Table 2; eTable 6 in Supplement 4). The fragility index for the success rate yielded 13 patients (Figure 2).
Figure 2. Sensitivity Analyses of the Primary Outcome.
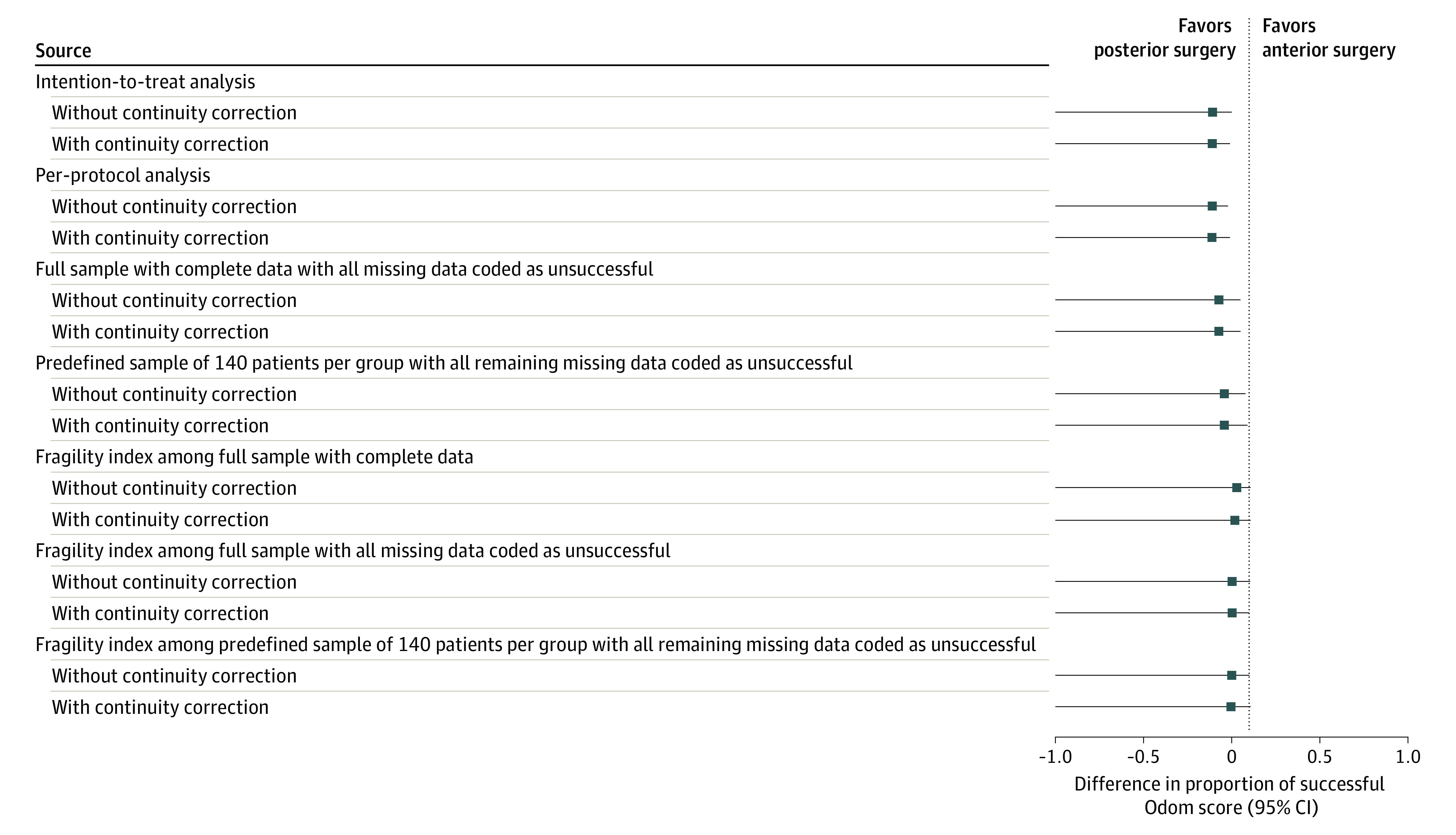
One-sided 95% CIs with Bonferroni corrections are reported. The vertical line indicates the noninferiority margin of 0.1. The intention-to-treat analysis of the primary outcome with complete cases yielded 86 of 98 patients in the posterior surgery group and 81 of 106 patients in the anterior surgery group, without and with continuity correction. There were 3 crossovers in total; therefore, per-protocol analysis yielded similar results without and with continuity correction. Scenarios regarding missing data were calculated in full cases with all missing data coded as unsuccessful in both groups without and with continuity correction and in the predefined sample sizes of 140 patients per group with all remaining missing data coded as unsuccessful without and with continuity correction. In addition, 6 different fragility indices were calculated, showing the minimum number of patients whose status (successful Odom score) must change to convert the noninferior outcome to inferior. The fragility index in the complete cases was 14 without and 13 with continuity correction. In the full cases with missing data coded as unsuccessful, the fragility index was 7 without and 6 with continuity correction. In the predefined sample sizes for both groups with all remaining data coded as unsuccessful, the fragility index was 3 without and with continuity correction.
Table 2. Comparison of Arm Pain and Secondary Outcome Measures Between Posterior and Anterior Surgery.
| Variablea | Mean (SD) | Mean difference (95% CI)b | |
|---|---|---|---|
| Posterior surgery (n = 119) | Anterior surgery (n = 124) | ||
| VAS score, arm | |||
| Baseline | 62.3 (20.7) | 60.3 (22.1) | NA |
| 1 y | 18.6 (22.9) | 15.8 (23.7) | –2.8 (–9.4) |
| Change | 41.9 (29.5) | 45.3 (29.7) | 3.4 (11.8) |
| VAS score, neck | |||
| Baseline | 55.2 (22.4) | 53.6 (23.7) | NA |
| 1 y | 24.4 (27.5) | 21.7 (26.1) | –2.7 (–10.3 to 4.8) |
| Change | 29.5 (33.9) | 31.6 (29.2) | 2.1 (–6.9 to 11.1) |
| NDI score | |||
| Baseline | 43.6 (14.1) | 42.2 (13.5) | NA |
| 1 y | 17.6 (14.6) | 19.2 (16.5) | 1.5 (–2.9 to 5.9) |
| Change | 24.3 (15.8) | 23.1 (16.8) | –1.2 (–5.8 to 3.5) |
| WAS score | |||
| Baseline | 3.8 (2.5) | 3.8 (2.5) | NA |
| 1 y | 6.7 (2.3) | 6.7 (2.6) | –0.09 (–0.80 to 0.60) |
| Change | 2.7 (2.8) | 2.7 (3.1) | –0.01 (–0.90 to 0.80) |
| EQ-5D-5L score | |||
| Baseline | 0.61 (0.18) | 0.62 (0.20) | NA |
| 1 y | 0.84 (0.15) | 0.82 (0.14) | –0.02 (–0.06 to 0.02) |
| Change | 0.20 (0.17) | 0.19 (0.22) | –0.01 (–0.06 to 0.05) |
| Reported satisfied or very satisfied, No. (%)c | |||
| Baseline | NA | NA | NA |
| 1 y | 70 (73) | 76 (77) | 0.04 (–0.09 to 0.20) |
| All adverse events, No. (%)d | |||
| Baseline | NA | NA | NA |
| 1 y | 36 (30) | 35 (28) | –0.02 (–0.10 to 0.10) |
| Surgery-associated adverse events, No. (%)d | |||
| Baseline | NA | NA | NA |
| 1 y | 26 (22) | 22 (18) | –0.04 (–0.10 to 0.07) |
| All serious adverse events, No. (%)d | |||
| Baseline | NA | NA | NA |
| 1 y | 13 (11) | 17 (14) | 0.03 (–0.06 to 0.10) |
| Surgery-associated serious adverse events, No. (%)d | |||
| Baseline | NA | NA | NA |
| 1 y | 7 (6) | 7 (6) | –0.00 (–0.06 to 0.06) |
| Reoperations, No. (%) | |||
| Baseline | NA | NA | NA |
| 1 y | 6 (5) | 4 (3) | –0.02 (–0.08 to 0.04) |
Abbreviations: EQ-5D-5L, EuroQol 5-Dimensions 5-Level questionnaire; NA, not applicable; NDI, Neck Disability Index; VAS, visual analogue scale; WAS, Work Ability Index–single item.
Data on baseline variables were available for 112 in the posterior surgery group and 117 in the anterior surgery group. Data after 1-year follow-up were available for 96 patients in the posterior surgery group and 99 in the anterior surgery group. There were no missing data for serious adverse events and reoperations.
Two-sided 95% CIs are given for the mean difference in change score from baseline to 1 year after surgery for patients in the posterior and anterior surgery groups, except for the following variables: VAS score for arm pain, treatment satisfaction, serious adverse events, and reoperations. For the outcomes in arm pain, a 1-sided 95% CI with Bonferroni correction was reported. For the other outcomes, the reported 95% CI denotes the difference in score after 1 year of follow-up between the posterior and anterior surgery groups, respectively.
In a questionnaire of overall satisfaction at 1-year follow-up, patients responded to the question, “How satisfied are you with the results of the surgery?” The 7-point answer options were “very satisfied,” “satisfied,” “moderately satisfied,” “somewhat satisfied/not satisfied,” “slightly dissatisfied,” “dissatisfied,” and “very dissatisfied.” The number of patients who answered with “very satisfied” and “satisfied” is depicted.
Adverse events were considered serious if lethal, life threatening, required hospitalization, caused considerable disability, were a congenital anomaly or birth defect, or any other medically important event that jeopardized the patient or required intervention. All serious adverse events were calculated at the patient level. For an overview of complication level, see Table 3 and eTable 7 in Supplement 4.
Secondary Outcomes
Results of secondary outcomes are presented in Table 2. Regarding all secondary outcomes, there were small between-group differences in mean change scores, and the 2-sided 95% CIs included 0, indicating comparable outcomes between groups. Additionally, the mean change in score for all except EQ-5D-5L reached the predefined minimal clinically important differences threshold. The responder analysis indicated comparable results among groups (eTable 6 in Supplement 4).
Adverse surgery-associated events occurred in 26 individuals (22%) in the posterior surgery group and 22 (18%) in the anterior surgery group; serious surgery-associated adverse events, including reoperations, occurred in 7 patients (6%) in both groups (Table 3). All CIs for safety-related outcomes included 0. Reoperations occurred in 6 patients (5%) in the posterior group and 4 (3%) in the anterior group (mean difference, 0.01; 95% CI, −0.08 to 0.04) (eTables 7 and 8 in Supplement 4).
Table 3. Serious Surgery-Associated Adverse Eventsa.
| Event | No. | Mean difference in proportions posterior vs anterior (95% CI) | ||
|---|---|---|---|---|
| Posterior (n = 119) | Anterior (n = 124) | Total (n = 243) | ||
| Total | 9 | 8 | 17 | NA |
| Dysphagia or globus sensationb | 1 | 6 | 7 | –0.03 (–0.09 to 0.01) |
| Hoarsenessb | 1 | 2 | 3 | –0.01 (–0.04 to 0.03) |
| Implant malpositionc | NA | 1 | 1 | NA |
| New radicular arm pain without need for surgeryd | 1 | 4 | 5 | –0.02 (–0.07 to 0.02) |
| Persistent radicular arm pain without need for surgeryd | 8 | 2 | 10 | 0.05 (–0.01 to 0.10) |
| Nonradicular symptomse | 0 | 1 | 1 | –0.02 (–0.05 to 0.01) |
| Neck pain | 2 | 1 | 3 | 0.01 (–0.03 to 0.04) |
| Shoulder symptomsf | 9 | 5 | 14 | 0.04 (–0.03 to 0.10) |
| Neck and shoulder symptomsg | 0 | 3 | 3 | –0.02 (–0.06 to 0.01) |
| Cardiothoracic symptomsh | 1 | 0 | 1 | 0.01 (–0.02 to 0.03) |
| Respiratory symptomsi | 0 | 1 | 1 | –0.01 (–0.03 to 0.02) |
| Wound infectionj | 5 | 2 | 7 | 0.03 (–0.02 to 0.08) |
| Allergic reaction to antibioticsk | 1 | 0 | 1 | 0.01 (–0.02 to 0.03) |
| Urinary retention | 1 | 0 | 1 | 0.01 (–0.02 to 0.03) |
| Total | 30 | 28 | 58 | NA |
| Serious adverse events | ||||
| Unresolved dysphagia within 1 y | 0 | 1 | 1 | –0.01 (–0.03 to 0.02) |
| Reoperation | ||||
| Index levell | 4 | 2 | 6 | 0.02 (–0.03 to 0.06) |
| Adjacent level | 0 | 2 | 2 | –0.02 (–0.05 to 0.01) |
| Index and adjacent level | 2 | 0 | 2 | 0.02 (–0.01 to 0.05) |
| Wound infectionj | 2 | 1 | 3 | 0.01 (–0.03 to 0.04) |
| Lung embolus | 0 | 1 | 1 | –0.01 (–0.03 to 0.02) |
| Postoperative hematomak | 1 | 1 | 2 | 0.00 (–0.02 to 0.02) |
Abbreviation: NA, not applicable.
Depicted are serious adverse events reported at the complication level (not patient level). Regarding the association with surgery, serious adverse events were rated as being 0 = definitely associated, 1 = probably associated, 2 = possibly associated, 3 = remotely associated, or 4 = not associated. Only serious adverse events scored as 0, 1, or 2 are depicted in this table. Adverse events were considered serious if they resulted in death, were life threatening, required prolongation of hospitalization, resulted in considerable disability, were a congenital anomaly or birth defect, or any other medically important event that jeopardized the patient or required an intervention.
Dysphagia was temporary in 6 patients and unresolved within 1 year in 1 patient in the anterior surgery group. Hoarseness was temporary in 2 patients in the anterior surgery group. Dysphagia and hoarseness in the posterior surgery group were temporary.
This patient had a slight cage subsidence without symptoms at 6 weeks. No reoperation was performed.
These were new or persistent radicular symptoms without reoperation within 1 year of follow-up. Some of these patients were treated with a selective nerve root blockage, referral to a pain center or pain specialist, or were treated conservatively.
This patient had arm pain without signs of radiculopathy.
Shoulder symptoms included patients with shoulder pain, frozen shoulder, or tendinitis supraspinatus. Some of these patients were treated with a local steroid injection.
Two patients had a combination of neck and shoulder pain after reoperatation.
This was a patient with palpitations during hospitalization.
This was a patient with dyspnea during hospitalization.
This includes patients with wound infections or leakage or swelling of the wound. When reported as an adverse event, wound infection was superficial and treated with oral antibiotics. When reported as serious adverse event, a longer hospitalization was required. None of the wound infections were related to esophageal injury.
This complication occurred during the operation (allergic reaction) or during hospitalization (postoperative hematoma).
One patient in the posterior surgery group had a reoperation at index level for new symptoms at the contralateral side.
Discussion
To our knowledge, this is the first multicenter randomized clinical trial that directly compares posterior cervical foraminotomy to anterior cervical discectomy with fusion in patients with 1-sided single-level foraminal cervical nerve root compression. Posterior surgery demonstrated noninferiority at 1-year follow-up regarding arm pain and success rate, confirmed by sensitivity analyses. The change in arm pain score did not establish noninferiority, but had a small clinically nonrelevant between-group difference of 3.4 on a scale from 0 to 100 (1-sided 95% CI, 11.8). All secondary outcomes had small between-group differences with 95% CIs clustered around 0, indicating comparable results between groups.
Our previous published systematic review and meta-analysis concerning surgical treatments for patients with cervical radiculopathy did not find statistically significant differences between the posterior or anterior approach.9 Two systematic reviews that also incorporated retrospective studies demonstrated similar clinical outcomes between posterior and anterior surgery.5,6 The findings in the present study are consistent with these results, thus adding certainty and robustness to the existing body of knowledge.
The success rates in this trial (88% in the posterior and 76% in the anterior surgery group) were slightly lower than the hypothesized overall success rate of 87%.13 This could be attributed to the assessment by an independent blinded interviewer in our study preventing confirmation bias. As the decrease in arm pain and all secondary patient-reported outcome measures are in accordance with reported rates in literature, it is unlikely that the lower success rates indicate a clinically relevant difference compared to other studies. There was no anterior plating performed, which is common in European countries but differs from countries such as the US. One could argue that this influenced our results; however, systematic reviews and meta-analyses of studies on fusion found no clinical benefit from the use of additional plating.23,24
In contrast to other studies, serious adverse events were meticulously registered and assessed for association with surgery during the trial period. As other studies did not specify whether they reported adverse or serious adverse events, the surgery-associated adverse events in our trial (22% in the posterior group and 18% in the anterior group) were higher than reported in other studies (4% in posterior surgery and 5% in anterior surgery; odds ratio, 1.18; 95% CI, 0.68 to 2.05).6 However, the rates of our serious surgery-associated adverse events (6% in both groups, including reoperations) were comparable to the complications identified in the abovementioned study. As expected, the types of surgery-associated adverse events were different between the 2 groups. For example, dysphagia and hoarseness were more frequent in the anterior surgery group and wound infections were more common in the posterior surgery group.20
There is conflicting evidence regarding reoperation rates after posterior cervical foraminotomy. A higher rate is reported in some studies, with more symptom recurrence on the operated level compared to anterior cervical discectomy with fusion.7,25,26 The average time interval for recurrent symptoms varied between 5 months25 and 42 months7 (without incorporating measures of uncertainty). In our study, the reoperation rate was slightly higher in the posterior surgery group (5%) compared to the anterior surgery group (3%) (mean difference, 0.01; 95% CI, −0.08 to 0.04) but lower overall than reported in other studies. Also, the rate of recurrent symptoms without the need for surgery was higher in the posterior surgery group than the anterior surgery group (eTable 7 in Supplement 4). Therefore, it is possible that the number of reoperations will increase over the remaining study period.
Clinical Implications and Future Research
The clinical effectiveness results after 1 year, including safety outcomes, are not only relevant to patients and spine surgeons, but also to a wide range of specialists involved in treatment of patients with cervical radiculopathy such as neurologists, pain specialists, general practitioners, and physiotherapists. The results may be used to improve patient counseling and enhance shared decision-making between physicians and patients with 1-sided foraminal radiculopathy, taking into account the type of complications per procedure and patient-specific factors.
As there are possible economic benefits of posterior surgery (no implants, shorter procedural length)18,19,20,21, our future research will focus on the cost-effectiveness of both treatments. As posterior and anterior surgery showed similar efficacy in this study, we believe that both treatments should be regarded valid for cervical foraminal radiculopathy and that a careful consideration should be made per individual patient.
Limitations
This study has limitations. The predefined sample size of 308 patients was not reached. However, the interim analysis indicated that it was safe to end the study prematurely with a low risk of a false-negative outcome. The study was powered on the proportion of success (Odom score) and not on the mean decrease in arm pain. This could explain the contrast in outcomes of arm pain at 1 year (confirming noninferiority) and change in arm pain (crossing the noninferiority margin with 1.8 points). However, in our opinion, such small between-group differences can be interpreted as similar results between groups. This is further strengthened by the small differences between groups in all secondary outcomes and in the responder analyses. Furthermore, an evidence-based noninferiority margin for this research question does not exist; therefore, we chose the margin of 10% empirically.
We used basic statistical analysis to present our 1-year results without incorporating the longitudinal aspect of the data. This might be considered a limitation, although the results are relatively simple for clinicians to interpret, and the robustness of the results was clearly demonstrated by the various sensitivity analyses. We also implemented the fragility index in our sensitivity analyses, which demonstrated a high number of patients (n = 13) compared to other surgical spine trials (median [IQR], 2 [1-3]).22
The inability to blind surgeons and patients to the intervention is an important limitation of our study. Also, irrespective of the clearly defined inclusion criteria and instructions, possible selection bias occurred in the assessment of eligible patients. Some surgeons had a strong preference for 1 of the studied interventions, mostly directed toward anterior surgery. This may have negatively influenced the enrollment of participants.
Conclusions
In this randomized clinical trial of patients with cervical radiculopathy due to foraminal nerve root compression, the 1-year clinical effectiveness results demonstrate noninferiority of success rate and arm pain in posterior vs anterior surgery at 1-year follow-up. Decrease in arm pain as well as all secondary outcomes had small between-group differences with CIs clustered around 0, indicating comparable results between groups.
Original trial protocol
Summary of amendments from the original protocol
Statistical analysis plan
eTable 1. Surgical characteristics in the intention-to-treat population
eTable 2. Post-hoc power calculations
eTable 3. Baseline characteristics of all randomized patients
eTable 4. Specification of comorbidities in all randomized patients
eTable 5. Baseline characteristics neurological examination
eTable 6. Responder analyses regarding the MCID
eTable 7. Specification of adverse events in the intention-to-treat population
eTable 8. Reoperations within 1-year of follow-up
eMethods. Supplementary questionnaires
Nonauthor collaborators. FACET investigators
Data sharing statement
References
- 1.Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy. a population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325-335. doi: 10.1093/brain/117.2.325 [DOI] [PubMed] [Google Scholar]
- 2.Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med. 2016;9(3):272-280. doi: 10.1007/s12178-016-9349-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broekema AEH, Groen RJM, Tegzess E, Reneman MF, Soer R, Kuijlen JMA. Anterior or posterior approach in the surgical treatment of cervical radiculopathy; neurosurgeons’ preference in the Netherlands. Interdiscip Neurosurg. 2021;23. doi: 10.1016/j.inat.2020.100930 [DOI] [Google Scholar]
- 4.Mok JK, Sheha ED, Samuel AM, et al. Evaluation of current trends in treatment of single-level cervical radiculopathy. Clin Spine Surg. 2019;32(5):E241-E245. doi: 10.1097/BSD.0000000000000796 [DOI] [PubMed] [Google Scholar]
- 5.Liu WJ, Hu L, Chou PH, Wang JW, Kan WS. Comparison of anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of cervical radiculopathy: a systematic review. Orthop Surg. 2016;8(4):425-431. doi: 10.1111/os.12285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang W, Huang L, Feng F, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy for the treatment of single-level unilateral cervical radiculopathy: a meta-analysis. J Orthop Surg Res. 2020;15(1):202. doi: 10.1186/s13018-020-01723-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wirth FP, Dowd GC, Sanders HF, Wirth C. Cervical discectomy. A prospective analysis of three operative techniques. Surg Neurol. 2000;53(4):340-346. doi: 10.1016/S0090-3019(00)00201-9 [DOI] [PubMed] [Google Scholar]
- 8.Broekema AEH, Groen RJM, Simões de Souza NF, et al. Surgical interventions for cervical radiculopathy without myelopathy: a systematic review and meta-analysis. J Bone Joint Surg Am. 2020;102(24):2182-2196. doi: 10.2106/JBJS.20.00324 [DOI] [PubMed] [Google Scholar]
- 9.Broekema AEH, Kuijlen JMA, Lesman-Leegte GAT, et al. ; FACET study group investigators . Study protocol for a randomised controlled multicentre study: the Foraminotomy ACDF Cost-Effectiveness Trial (FACET) in patients with cervical radiculopathy. BMJ Open. 2017;7(1):e012829. doi: 10.1136/bmjopen-2016-012829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Piaggio G, Elbourne DR, Pocock SJ, Evans SJW, Altman DG; CONSORT Group . Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA. 2012;308(24):2594-2604. doi: 10.1001/jama.2012.87802 [DOI] [PubMed] [Google Scholar]
- 11.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A(3):607-624. doi: 10.2106/00004623-195840030-00009 [DOI] [PubMed] [Google Scholar]
- 12.Frykholm R. Deformities of dural pouches and strictures of dural sheaths in the cervical region producing nerve-root compression. J Neurosurg. 1947;4(5):403-413. doi: 10.3171/jns.1947.4.5.0403 [DOI] [PubMed] [Google Scholar]
- 13.Dohrmann GJ, Hsieh JC. Long-term results of anterior versus posterior operations for herniated cervical discs: analysis of 6,000 patients. Med Princ Pract. 2014;23(1):70-73. doi: 10.1159/000351887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127-1131. doi: 10.1016/S0140-6736(74)90884-8 [DOI] [PubMed] [Google Scholar]
- 15.de Zwart BCH, Frings-Dresen MHW, van Duivenbooden JC. Test-retest reliability of the Work Ability Index questionnaire. Occup Med (Lond). 2002;52(4):177-181. doi: 10.1093/occmed/52.4.177 [DOI] [PubMed] [Google Scholar]
- 16.Jorritsma W, de Vries GE, Dijkstra PU, Geertzen JHB, Reneman MF. Neck Pain and Disability Scale and Neck Disability Index: validity of Dutch language versions. Eur Spine J. 2012;21(1):93-100. doi: 10.1007/s00586-011-1920-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soer R, Reneman MF, Speijer BLGN, Coppes MH, Vroomen PCAJ. Clinimetric properties of the EuroQol-5D in patients with chronic low back pain. Spine J. 2012;12(11):1035-1039. doi: 10.1016/j.spinee.2012.10.030 [DOI] [PubMed] [Google Scholar]
- 18.Tumialán LM, Ponton RP, Gluf WM. Management of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus. 2010;28(5):E17. doi: 10.3171/2010.1.FOCUS09305 [DOI] [PubMed] [Google Scholar]
- 19.Alvin MD, Lubelski D, Abdullah KG, Whitmore RG, Benzel EC, Mroz TE. Cost-utility analysis of anterior cervical discectomy and fusion with plating (ACDFP) versus posterior cervical foraminotomy (PCF) for patients with single-level cervical radiculopathy at 1-year follow-up. Clin Spine Surg. 2016;29(2):E67-E72. doi: 10.1097/BSD.0000000000000099 [DOI] [PubMed] [Google Scholar]
- 20.Witiw CD, Smieliauskas F, O’Toole JE, Fehlings MG, Fessler RG. Comparison of anterior cervical discectomy and fusion to posterior cervical foraminotomy for cervical radiculopathy: utilization, costs, and adverse events 2003 to 2014. Neurosurgery. 2019;84(2):413-420. doi: 10.1093/neuros/nyy051 [DOI] [PubMed] [Google Scholar]
- 21.Mansfield HE, Canar WJ, Gerard CS, O’Toole JE. Single-level anterior cervical discectomy and fusion versus minimally invasive posterior cervical foraminotomy for patients with cervical radiculopathy: a cost analysis. Neurosurg Focus. 2014;37(5):E9. doi: 10.3171/2014.8.FOCUS14373 [DOI] [PubMed] [Google Scholar]
- 22.Tignanelli CJ, Napolitano LM. The fragility index in randomized clinical trials as a means of optimizing patient care. JAMA Surg. 2019;154(1):74-79. doi: 10.1001/jamasurg.2018.4318 [DOI] [PubMed] [Google Scholar]
- 23.Zhang T, Guo N, Gao G, et al. Comparison of outcomes between zero-P implant and anterior cervical plate interbody fusion systems for anterior cervical decompression and fusion: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2022;17(1):47. doi: 10.1186/s13018-022-02940-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheung ZB, Gidumal S, White S, et al. Comparison of anterior cervical discectomy and fusion with a stand-alone interbody cage versus a conventional cage-plate technique: a systematic review and meta-analysis. Global Spine J. 2019;9(4):446-455. doi: 10.1177/2192568218774576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.MacDowall A, Heary RF, Holy M, Lindhagen L, Olerud C. Posterior foraminotomy versus anterior decompression and fusion in patients with cervical degenerative disc disease with radiculopathy: up to 5 years of outcome from the national Swedish Spine Register. J Neurosurg Spine. 2019;32(3):1-9. doi: 10.3171/2019.9.SPINE19787 [DOI] [PubMed] [Google Scholar]
- 26.Korinth MC, Krüger A, Oertel MF, Gilsbach JM. Posterior foraminotomy or anterior discectomy with polymethyl methacrylate interbody stabilization for cervical soft disc disease: results in 292 patients with monoradiculopathy. Spine (Phila Pa 1976). 2006;31(11):1207-1214. doi: 10.1097/01.brs.0000217604.02663.59 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Original trial protocol
Summary of amendments from the original protocol
Statistical analysis plan
eTable 1. Surgical characteristics in the intention-to-treat population
eTable 2. Post-hoc power calculations
eTable 3. Baseline characteristics of all randomized patients
eTable 4. Specification of comorbidities in all randomized patients
eTable 5. Baseline characteristics neurological examination
eTable 6. Responder analyses regarding the MCID
eTable 7. Specification of adverse events in the intention-to-treat population
eTable 8. Reoperations within 1-year of follow-up
eMethods. Supplementary questionnaires
Nonauthor collaborators. FACET investigators
Data sharing statement


