INTRODUCTION
Double lumen tubes (DLTs) remain the gold-standard lung isolation devices to prevent soilage (abscess, blood) of the normal lung or control ventilation in certain thoracic surgeries (bronchopleural fistula, lung-resection, oesophagectomy, etc.).[1] Optimal DLT placement is an art and science garnered by practice and learning from the experience of others. DLTs have evolved from bulky red-rubber devices with carinal hooks (left-sided Carlen’s catheter; right-sided White’s catheter) to roomier lumens (Bryce-Smith, Robertshaw) and modern disposable tubes (Bronchocath; Sheridan; Portex).
Broadly, difficulty in DLT placement may be encountered at four levels: difficulty in manoeuvering the tip of DLT to glottis; DLT impaction at glottis; DLT impaction at cricoid cartilage/bronchial opening and DLT entering the wrong bronchus. We have devised from our clinical experience, an algorithm with stepwise instructions on how to proceed in each of these situations [Figure 1], incorporating recent advances like video laryngoscope-guided DLT insertion,[2] augmentation of the curved bronchial lumen tip of the left-sided DLT to reduce misplacement into the right bronchus,[3] two novel DLTs that do not require a fibreoptic bronchoscope (FOB) for correct positioning and certain bronchial blockers (BBs).[4,5] Importance of preoxygenation and monitoring vital parameters throughout the procedure cannot be over-emphasised. Re-examination of the DLT/BBs using a bronchoscope after lateral positioning is necessary.
Figure 1.
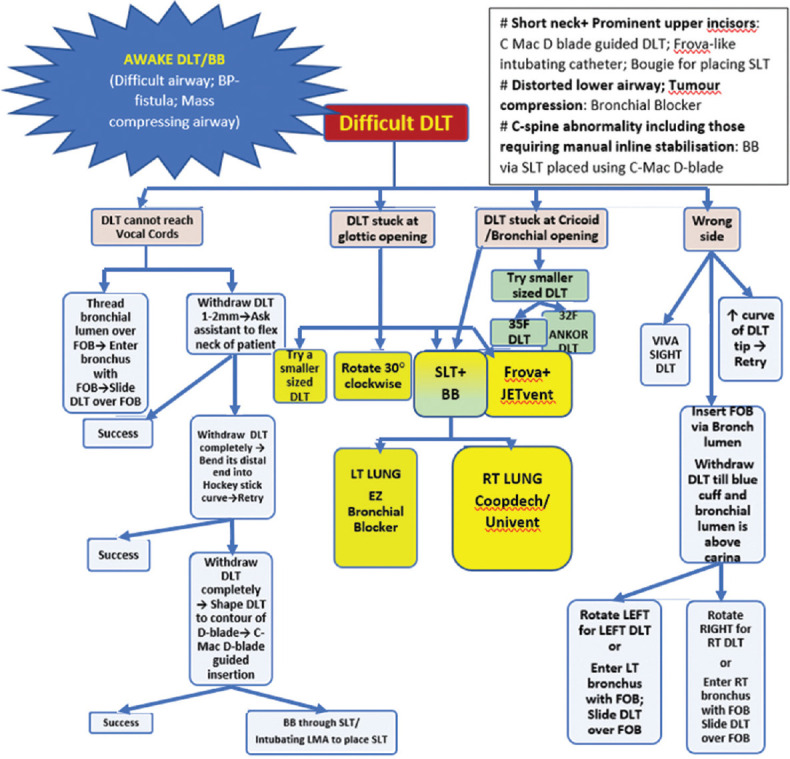
Algorithm for managing difficult DLT placement for one-lung ventilation. (BB = Bronchial blocker; DLT = Double lumen tube; FOB = Fibreoptic bronchoscope; LT = Left; RT = Right; SLT = Single lumen tube; BP=Bronchopleural)
DISCUSSION
Some of the algorithmic steps merit further explanation.
C-Mac D-blade guided DLT placement
The D-blade is known to improve glottic visualisation, improving the Cormack–Lehane grade by at least one grade compared to a normal blade. The distal concavity of the DLT is shaped as per the D-blade concavity, and the DLT blue/bronchial cuff can be visualised on the monitor as it disappears through the vocal cords. Although the rest of the procedure beginning with anticlockwise rotation of the DLT is still blind, this technique has the added advantage of reduced cuff rupture.[2] The incidence of wrong-sided placement is slightly higher but is easily rectified using the FOB.
Ambu VivaSight DLT
These DLTs are an improvement over the blind insertion techniques and have an integrated camera attached at the distal end of the tracheal lumen via which each step of DLT placement is displayed on the designated monitor screen.[4]
Ankor three-cuffed DLT
These may be advantageous where FOB is unavailable/cannot pass through the narrow-lumen DLT (<32 French). Besides the routine tracheal and bronchial cuffs, a third carinal cuff is provided. After the disappearance of the deflated blue cuff through the vocal cords and anticlockwise rotation of the left DLT, the carinal cuff is inflated via the carinal pilot balloon and this third cuff blocks the right bronchial opening, so that the bronchial DLT lumen is directed to the left main bronchus. Once positioned, the tracheal and bronchial cuffs are inflated and the carinal cuff is deflated.[5]
Bronchial blockers (BBs)
They are useful options when difficult anatomy precludes proper DLT placement. BBs may have a single/double cuff and may come with/without a designated single lumen tube (SLT). We describe here the most useful ones (a prototype of each category) for the anaesthesiologists’ armamentarium. Lung isolation using BB and DLT in combination has also been reported.[6]
Single-cuff bronchial blocker (Coopdech BB)
After tracheal intubation with a 7.5 mm SLT, a FOB is inserted through SLT followed by a Coopdech BB. Once the BB is 2 cm above the carina, it is rotated 90° clockwise to enter the right bronchus or anticlockwise to enter the left bronchus.[7] If unsuccessful, then the BB is withdrawn into SLT, FOB is advanced into the required bronchus and SLT is slided over FOB along with the BB. The FOB is withdrawn, and the SLT is withdrawn back into the trachea with counter-pressure on Coopdech BB so that the BB remains in the right bronchus.
Single-cuff bronchial blocker with designated SLT (Univent BB)
Univent BB is passed through a specially crafted channel incorporated in the concavity along the entire length of the designated SLT.[8] A FOB is passed through the main lumen of SLT to visualise the BB which enters the right bronchus by default.
If unable to rotate BB to left bronchus for surgery on the left lung, rotate the entire uninvent tube 30–60° anticlockwise.
Double-cuff bronchial blocker (EZ-BB)
After tracheal intubation with a 7.5 mm SLT, and FOB confirmation of tip resting 4 cm above the carina, the EZ-BB is advanced through the SLT till the two distal branches spring open, its bifurcation rests on the carina and the cuffed branches enter into one bronchus each. The bronchial cuff of the branch entering the lung to be operated on is inflated. Any trapped air is suctioned via the EZ channel to collapse the lung.[8] If the right upper lobe (RUL) is blocked, then the EZ-BB ought to be withdrawn under bronchoscopic imaging. If both the branches enter the same bronchus then it implies inadequate space for distal branches to fan out. In this scenario, the BB is retracted into the SLT, the SLT is withdrawn till 5 cm above the carina and retried.
High-frequency jet ventilation (HFJV) using Frova
HFJV provides a tidal volume of <2 ml/kg at rates ranging from 60 to 900 breaths/min.[9]
HFJV can be administered via Frova-like intubating catheters in difficult airways. Advantages include reduced peak airway pressure and provision for administration through extremely narrow catheters. Specific indications include bronchopleural fistula, surgery on a major conducting airway and where minimising operative-field movement is imperative (robotic surgery). Arterial blood gas analysis is important for monitoring PaCO2 during prolonged jet ventilation.
Troubleshooting a malpositioned left DLT
Using the classic Slinger technique for verifying proper positioning, where a left DLT was considered correctly placed if the left upper lobe (LUL) and left lower lobe (LLL) bronchus could be visualised by FOB through the bronchial lumen, the incidence of DLT malpositioning (leading to hypoxaemia during one-lung ventilation) was traditionally 53%.[10] Even after visualising the shadow of the right bronchial opening through the DLT wall (new Fortier technique) with the FOB in the bronchial lumen, 23% of DLTs are still malpositioned.[10] Since a left DLT is the first choice for surgery on both the left and right lung, we present detailed scenarios of the likely problems encountered (catering to the seven possible DLT malpositions) and also how to troubleshoot them, with schematic diagrams [Table 1]. Each scenario should be sequentially ruled out to pinpoint the malposition site culminating in successful optimal DLT positioning.
Table 1.
Clinical scenarios (auscultatory and fibreoptic bronchoscopic findings) in possible malpositioned configurations of a left-sided DLT with their interpretation, remedy, and schematic diagrams
| Auscultation | FOB view through tracheal lumen | FOB view through bronchial lumen | Interpretation | Remedy | Schematic View |
|---|---|---|---|---|---|
| B/L equal BS on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- BS absent on RT side Clamp BL- BS absent on LT side |
Sharp carina+Rim of blue cuff entering LT bronchus. Enter RT bronchus to visualise the 3 secondary bronchial openings: initially RUL (at 1.5-1.9 cm) with its apical, anterior and posterior openings, then RML and RLL openings seen together | Assistant manually ventilates→Shadow of right bronchial opening can be seen through the wall of DLT before the blue portion of DLT begins; Origins of LUL and LLL are identifiable | Correct placement | Fix DLT adequately so that it does not get displaced on turning the patient to the lateral position |

|
| BS absent on RT side on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- BS absent on RT side Clamp BL- BS absent on LT side |
Broad flat carina+Rim of blue cuff entering bronchus | FOB cannot enter deeper into branches of LUL and LLL | Both Bronchial and tracheal cuffs of DLT are in LT bronchus. FOB view through tracheal lumen→ secondary carina seen with bronchial lumen entering LUL | Withdraw DLT under FOB guidance till the tracheal lumen opening lies in the Clamp TL. trachea |

|
| B/L equal BS on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- B/L equal BS Clamp BL- B/L equal BS |
Tracheal rings are seen on RT side with the bronchial lumen of DLT on the. On moving FOB deeper→Sharp carina with RT and LT bronchial openings are visible and empty | Sharp carina is visible; RT and LT bronchial openings are visible and empty | Both bronchial and tracheal cuffs of DLT are in the trachea | Rotate DLT 90° left (anticlockwise) and push DLT down till the bronchial lumen enters the LT bronchus and a small rim of the blue cuff is seen on inflation |

|
| B/L equal BS on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- BS absent on RT side Clamp BL B/L BS absent |
Sharp carina+Rim of blue cuff is seen entering LT bronchus when bronchial cuff is deflated but herniation of blue cuff into tracheal lumenis visible on its inflation | Assistant manually ventilates→Shadow of right bronchial opening not seen through wall of DLT before the blue portion of DLT begins; Identification of origins of LUL and LLL is possible | Bronchial cuff herniating out of LT bronchus to block RT bronchial opening too (DLT displaced out slightly during fixing/Tracheal carina deviated rightwards/Very narrow LT bronchus | Insert DLT a few mm deeper under FOB guidance till blue cuff disappears into LT bronchus; Use a bronchial blocker if cuff herniation persists probably due to external pressure from carinal lymph nodes/mass |

|
| B/L equal BS on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- BS absent on LT side+RUL Clamp BL- BS absent on RT side |
Only one bronchus seen (LT bronchus not seen); Bronchus seen is to the LT side (9 o’clock); Bronchial lumen of DLT with blue cuff disappearing into RT bronchus | Assistant manually ventilates→Shadow of RUL opening not seen through wall of DLT before the blue portion of DLT begins | DLT placed on the wrong side; Bronchial lumen and bronchial cuff is in RT bronchus; Tracheal lumen is in trachea; Blue cuff blocks RUL opening | Withdraw DLT till bronchial lumen lies above carina; Rotate DLT 90° left and push DLT down till bronchial lumen enters LT bronchus+blue cuff rim is seen |

|
| B/L equal BS on inflating tracheal cuff alone After inflating both cuffs→ Clamp TL- BS absent on LT side+RUL Clamp BL- BS absent in RML+RLL |
Only one bronchus seen (LT bronchus not seen); Bronchus seen is to the LT side (9 o’clock position); Bronchial lumen of DLT disappearing into RT bronchus | Assistant manually ventilates→Shadow of RUL opening seen through the wall of DLT before the blue portion of DLT begins; Openings of RML and RLL seen resembling carina | DLT placed on wrong side; Bronchial lumen and bronchial cuff is in RT bronchus; Blue cuff is distal to RUL opening; Tracheal lumen is in trachea | Withdraw DLT till bronchial lumen lies above carina; Rotate DLT 90° left and push DLT down till bronchial lumen enters LT bronchus+blue cuff rim is seen |

|
| BS absent on LT side on inflating tracheal cuff alone; After inflating both cuffs→ Clamp TL- BS absent on LT side+RUL Clamp BL- BS absent on LT side+RT side |
RML and RLL openings are seen resembling carina; Bronchial lumen is seen disappearing into one of them | Segmental branches are seen if bronchial lumen is in RML or RLL; Difficulty is faced in negotiating the FOB further | DLT is placed on the wrong side; Bronchial lumen and bronchial cuff is in RT bronchus; Tracheal lumen is in RT bronchus; Tracheal cuff blocks the RUL opening | Withdraw DLT till bronchial lumen lies above carina; Rotate DLT 90° left and push DLT down till bronchial lumen enters LT bronchus+blue cuff rim is seen |

|
B/L=bilateral; BS-Breath sounds, DLT=Double lumen tube, FOB=Fibreoptic bronchoscope, LUL=left upper lobe, LLL=left lower lobe, RUL=Right upper lobe, RML=Right middle lobe, RLL=Right lower lobe, RT=right, LT=left
The importance of anatomy, bronchoscopy and chest imaging of lung isolation cannot be over-emphasised.
A for Anatomy
Being well-versed in the segmental anatomy of the tracheobronchial tree is a prerequisite for mental imagery of the DLT positioning/malpositioning in the airway, which is vital for understanding the problem and finding a remedy. The lung segments are distinct surgical units that can be resected while conserving adjoining segments. Also, bronchopneumonia, pulmonary tuberculosis, bronchogenic carcinoma, pus/blood aspiration and pulmonary infarction/sequestration are segmental in distribution. According to the Jackson-Huber nomenclature, the right lung has three lobes (upper; middle; lower), while the left lung has only two lobes (upper; middle).[11]
B for Bronchoscopy
On bronchoscopy, the opening of RUL bronchus appears just 2 cm away from the tracheal/main carina and it trifurcates into three segments (apical; anterior; posterior). After moving another 2 cm distally (along bronchus intermedius), bifurcation into the right middle lobe (RML) (two segments: medial; lateral) and right lower lobe (RLL) (five segments: superior; medial-basal; lateral-basal; anterobasal and posterobasal). The secondary carina between RUL and bronchus intermedius is called right carina-1 and the carina between RML and RLL is called right carina-2.[11]
LUL bronchus gives a larger margin of safety (5 cm distance between the carina and LUL offset), and has an upper division with two segments (apicoposterior; anterior) and a lingular division with another two segments (superior; inferior). LLL bronchus has four branches (superior; anteromedial; lateral-basal; posterobasal). The secondary carina between the upper and lingular divisions of LUL is called left carina-1, while the carina between LUL and LLL is called left carina-2.
C for Chest imaging
Chest imaging pinpoints the exact point of offset of RUL from the right main bronchus and is useful to align it with the corresponding slot in right-sided DLTs. A grossly distorted tracheobronchial tree as evidenced on a computerised tomography (CT) scan favours the use of BBs as lung isolation devices. DLT size is traditionally gauged by the height and gender of the patient. Tracheal diameter and left bronchial diameter on CT/radiography/sonography correlate well with the DLT size.[1,12] Since the clinical practice patterns of the DLT still do not match recommendations from existing literature, the quest for newer determinants of optimal DLT size is still on. The latest correlation studied is the cricoid cartilage diameter.[12]
CONCLUSION
Our algorithm identifies four possible types of difficulty in DLT placement and prescribes practical solutions to each one of them incorporating skilled use of available devices and recent technological advances. An optimal-sized DLT is quintessential to proper DLT positioning. Troubleshooting a malpositioned left DLT is easier by harnessing the A, B and Cs of lung isolation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Purohit A, Bhargava S, Mangal V, Parashar VK. Lung isolation, one-lung ventilation and hypoxaemia during lung isolation. Indian J Anaesth. 2015;59:606–17. doi: 10.4103/0019-5049.165855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shah SB, Bhargava AK, Hariharan U, Mittal AK, Goel N, Choudhary M. A randomized clinical trial comparing the standard Mcintosh laryngoscope and the C-Mac D blade videolaryngoscope™for double lumen tube insertion for one lung ventilation in onco surgical patients. Indian J Anaesth. 2016;60:312–8. doi: 10.4103/0019-5049.181591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seo JH, Yoon S, Min SH, Row HS, Bahk JH. Augmentation of curved tip of left-sided double-lumen tubes to reduce right bronchial misplacement:A randomized controlled trial. PLoS One. 2019;14:e0210711. doi: 10.1371/journal.pone.0210711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schuepbach R, Grande B, Camen G, Schmidt AR, Fischer H, Sessler DI, et al. Intubation with VivaSight or conventional left-sided double-lumen tubes:A randomized trial. Can J Anaesth. 2015;62:762–9. doi: 10.1007/s12630-015-0329-8. [DOI] [PubMed] [Google Scholar]
- 5.Kim N, Byon HJ, Kim GE, Park C, Joe YE, Suh SM, et al. A randomized controlled trial comparing novel triple-cuffed double-lumen endobronchial tubes with conventional double-lumen endobronchial tubes for lung isolation. J Clin Med. 2020;9:977–81. doi: 10.3390/jcm9040977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chennakeshavallu GN, Sruthi S. Use of bronchial blocker to facilitate left double-lumen tube placement. Indian J Anaesth. 2021;65:263–5. doi: 10.4103/ija.IJA_1109_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hariharan U, Shah SB, Mittal A, Bhargava AK. C-Mac guided bronchial blocker (COOPDECH™) insertion for one lung ventilation in an adolescent with difficult airway. J Anaesthesiol Clin Pharmacol. 2014;30:591–2. doi: 10.4103/0970-9185.142909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoşten T, Aksu C, Kuş A, Cesur S, Türkyılmaz N, Solak M. Comparison of univent tube and EZ blocker in one lung ventilation;airway pressures and gas exchange. J Clin Monit Comput. 2018;32:327–33. doi: 10.1007/s10877-017-0028-9. [DOI] [PubMed] [Google Scholar]
- 9.Meyers M, Rodrigues N, Ari A. High-frequency oscillatory ventilation:A narrative review. Can J Respir Ther. 2019;55:40–6. doi: 10.29390/cjrt-2019-004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fortier G, Coté D, Bergeron C, Bussieres JS. New landmarks improve the positioning of the left Broncho-Cath double-lumen tube-comparison with the classic technique. Can J Anaesth. 2001;48:790–4. doi: 10.1007/BF03016696. [DOI] [PubMed] [Google Scholar]
- 11.Muresian H. Pleura, lungs, trachea and bronchi. In: Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. Edinburgh: Churchill Livingstone/Elsevier; 2016. pp. 953–70. [Google Scholar]
- 12.Shiqing L, Wenxu Q, Jin Z, Youjing D. The combination of diameters of cricoid ring and left main bronchus for selecting the “Best fit”double-lumen tube. J Cardiothorac Vasc Anesth. 2018;32:869–76. doi: 10.1053/j.jvca.2017.11.029. [DOI] [PubMed] [Google Scholar]


