Abstract
Background
Intimate partner violence (IPV) is highly prevalent globally and associated with adverse mental health outcomes among women. In IPV-endemic contexts like Bangladesh, previous research has found no association between low levels of IPV and depression. Although IPV and attitudes justifying IPV against women are highly prevalent in this context, nothing is known about how related contextual norms affect associations between individual-level IPV exposure and depression. The present study examines if village-level IPV norms, characterized using village-level (Level 2) prevalence of a) IPV-justifying attitudes (injunctive norms) and b) physical IPV (descriptive norms), modifies the individual-level (Level 1) associations between the severity of recent IPV and major depressive episode (MDE) among women in rural Bangladesh.
Methods
Data were drawn from a nationally-representative sample consisting of 3290 women from 77 villages. Multilevel models tested cross-level interactions between village-level IPV norms and recently experienced individual-level IPV on the association with past 30-day MDE.
Results
The prevalence of IPV was 44.4% (range: 9.6–76.2% across villages) and attitudes justifying IPV ranged from 1.6% to 49.8% across villages. The prevalence of MDE was 16.8%. The risk of MDE at low levels of IPV severity (versus none) was greater in villages with the least tolerant attitudes toward IPV compared to villages where IPV was more normative, e.g., interaction RR = 1.42 (95% CI: 0.64, 3.15) for low physical IPV frequency and injunctive norms.
Conclusions
The association between IPV and depression may be modified by contextual-level IPV norms, whereby it is exacerbated in low-normative contexts.
Keywords: Intimate partner violence, Depression, Major depressive episode, Multilevel analysis, Bangladesh
Introduction
Intimate partner violence (IPV) against women, referring to behaviors in intimate relationships resulting in physical, psychological, or sexual harm [1], is highly prevalent world-wide [2]. Globally, nearly one in three women have ever experienced either physical or sexual IPV [3]. Estimates are higher in South Asia [3], particularly in Bangladesh where one nationally-representative survey found 72.6% of ever-married women experienced at least one form of IPV in their lifetime and 54.7% experienced IPV within the past 12 months [4]. IPV has been associated with numerous negative sequelae, including adverse mental health outcomes [5], among them major depressive disorder [6] and posttraumatic stress disorder [7]. In Bangladesh, the focus of the present study, the association between incident IPV and depressive symptoms is well established [8–11]. Although recent evidence suggests contextual factors—or community-level socially accepted beliefs and behaviors related to IPV—may influence this relationship [12], no study has directly tested this.
Background
Although most studies examining the relationship between IPV and depression are cross-sectional, a causal relationship between IPV and depression is well-supported. Several longitudinal studies testing the directionality of the IPV and depression association suggest IPV exposure precedes depression [13–18], and others have observed a bidirectional relationship [17, 18]. Yet several studies in low- and middle-income countries have also documented a lack of association between IPV and depression [10, 11, 13, 19, 20]. One possible reason for the null results is the use of standard dichotomous indicators of IPV exposure (i.e., any exposure versus none within a given time referent). A recent analysis of the relationship between IPV and depression in rural Bangladesh concluded that this standard measurement approach both (a) underestimates the increased risk of depression among women experiencing relatively high levels of IPV (measured in terms of the frequency and injuriousness of IPV exposure), and (b) obscures the lack of an elevated risk of mental health sequelae associated with relatively low levels of IPV exposure, which are highly prevalent in this context [19]. The latter results are consistent with other studies showing a lack of association between depression and relatively low levels of IPV exposure in Bangladesh [10] and similarly IPV-endemic areas such as Ethiopia [20] and Zimbabwe [21]. In contrast, a study in Canada, where IPV is much less prevalent, found that even one instance of IPV (versus none) was associated with 2.5-times the odds of depression [22]. Overall, these patterns of association across diverse settings suggest contextual factors—including the community prevalence of IPV and the extent to which it is considered normative—may modify the effect of IPV on depression.
Social norms can be characterized as informal social rules regarding what is socially acceptable. Individuals’ adherence to social norms is based on what they perceive is socially expected or accepted—“injunctive norms”—or what they perceive is commonly done—“descriptive norms”—in a particular context [23]. Social norms and individual attitudes related to IPV, have been examined as risk factors for IPV exposure [24, 25]. For instance, women’s acceptance of IPV, measured at both the individual and contextual levels, is associated with an increased risk of experiencing IPV [26–28]. In a nationally-representative sample of women in India, Boyle et al. (2009) found a woman’s own acceptance of husband-perpetrated IPV (versus non-acceptance) was associated with a 29% increased odds of physical IPV and a one percentage point increase of the community-level mean of this variable was associated with a 19% increased odds of physical IPV [26]. Consistent with these results, Clark et al. (2018) found a quarter-point increase in scores on a scale measuring normative expectations related to IPV among women in Nepal at both the individual-level and community-level was associated with an 11% and 23% increased odds of physical IPV, respectively [27]. However, to our knowledge, contextual IPV norms have not been examined as factors that may modify the effects of IPV on mental health. As described above, in LMIC settings, adverse mental health may be less likely to result from relatively “low” levels of IPV exposure, where it is highly prevalent and, therefore, more likely to be considered typical, or normative, in the community [19]. The idea that IPV norms may mitigate the adverse mental health consequences of IPV exposure is also suggested by a recent study in Bangladesh which evaluated the moderating effect of individual-level attitudes. The authors found that the overall two-fold increased odds of screening positive for a mental disorder associated with any physical IPV exposure (versus none) were attenuated among women who justified IPV to a greater degree [12].
In Bangladesh, IPV-justifying attitudes are not uncommon. In the 2014 Bangladesh Demographic and Health Survey, 28.3% of women endorsed at least one scenario justifying IPV [29]. Yet despite the evidence linking individual IPV risk and contextual-level IPV acceptability [25–28], no study to our knowledge has examined the influence of contextual-level IPV norms on the relationship between IPV exposure and depression risk. Building upon prior findings in Bangladesh of no association between low levels of IPV exposure and depression [19], the primary objective of this study is to examine how village-level IPV norms—both injunctive and descriptive separately—may modify the association between IPV severity, measured as the frequency and injuriousness of recent IPV exposure, and major depressive episode (MDE). As illustrated in Fig. 1, we hypothesize that: (1) consistent with previous studies, village-level IPV norms are positively associated with individual-level IPV risk, and (2) village-level norms modify the association between individual-level IPV severity and MDE. Specifically, we hypothesize that the individual-level association between low levels of IPV exposure (versus none) and MDE, which has been null in prior studies, will be positive in low-normative villages compared to high-normative villages.
Fig. 1.
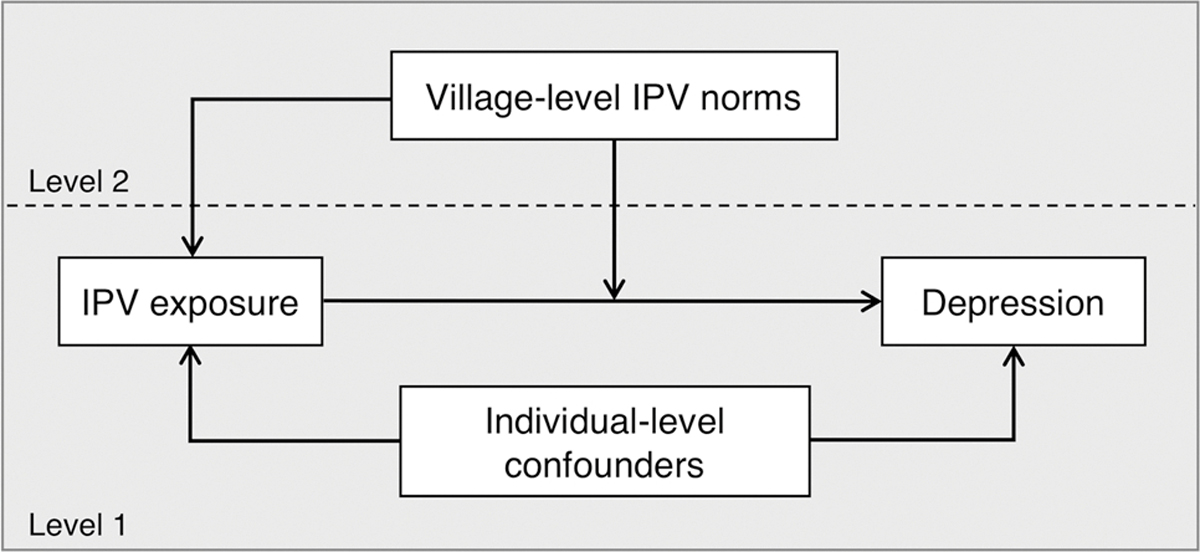
Conceptual framework of the effect of village-level intimate partner violence (IPV) norms on the relationship between IPV exposure and depression
Methods
Study population
Data from a multi-stage, stratified sample of participants residing in 77 villages were collected as part of a nationally-representative study examining individual- and contextual-level risk factors for IPV in rural Bangladesh. For the present study, we use a sample of women who completed both baseline and follow-up interviews. Women of any age were eligible if they married in the prior 4–12 years. Response rates for these participants were 94.7% at baseline in 2013 (n = 3902) and 86.3% at follow-up, which occurred approximately 10 months later in 2014 (n = 3369). Additional details of the study site and sampling frame are described elsewhere [30]. The sample for the present study consists of the women who responded to both waves and have non-missing data for all variables of interest (n = 3290), which corresponds to 79.9% of the original sample.
Outcome
MDE was measured at both baseline and follow-up using a slightly adapted version of the Edinburgh Depression Scale (EDS). The 10-item EDS was originally designed to assess symptoms of postnatal depression [31]. It has been validated for use in Bangladesh [32], and to detect MDE in women beyond pregnancy [33] as well as in men and women in a general population [34, 35]. In this study, participants were asked about the presence of depressive symptoms within the past 30 days and responded on a four-point scale (never = 0, rarely = 1, sometimes = 2, often = 3). Responses were aggregated into a final score, ranging from 0 to 30. We used the cutoff of greater than 9 to indicate MDE, which has been shown to have an 89% sensitivity and 87% specificity for clinical diagnosis of depression among postnatal women [32], and 95% sensitivity and 72% specificity among non-postnatal women [33].
Exposures
To capture the degree of physical IPV exposure (rather than dichotomous “yes/no”), we characterized it using two domains of IPV severity: (1) a physical IPV frequency score and (2) an indicator of whether the IPV experienced was injurious. Both were based on items adapted from the Revised Conflict Tactics Scale [36] and the WHO standardized questionnaire on IPV [37], and assessed at follow up. Incident physical IPV was ascertained with reference to seven acts of escalating violence. Among women reporting any exposure, the frequency of each act experienced, since baseline was also elicited (1–2 times, 3–5 times, 6–10 times, greater than 10 times). Individual acts were scored based on frequency: “0” if no IPV occurred, “1” for 1–2 times, “2” for 3–5 times, “3” for 6–10 times, and “4” for greater than 10 times. Next, these scores were summed across all acts, resulting in a possible range of 0 to 28 and an actual range of 0 to 26. Consistent with our prior study [19], we used these scores to create four categories. Women who did not experience IPV comprised the unexposed category of “none,” and the remaining nonzero values were categorized into “low” (range = 1–2), “medium” (range = 3–4), and “high” (range = 5–26) tertiles of IPV frequency exposure. Although respondents were also asked about exposure to psychological and sexual IPV, the present study focuses only on individual level physical IPV exposure, to be as consistent as possible with the injunctive IPV norms indicator (described in detail in the following section), which only references physical IPV.
Those who responded “yes” to at least one physical or sexual IPV act, since baseline were additionally asked whether they experienced eight types of injury due to said IPV—for example, “have you had a bruise, swelling, or abrasion?” A three-category variable for injurious IPV was created: no IPV, IPV without injury, and IPV with injury. Because of the way injury experiences were elicited, and because some share of women reported both physical and sexual IPV, there was no clear way to distinguish injury resulting from physical versus sexual IPV. However, sexual IPV that results in injury can also be considered a form of physical IPV. Additional details of IPV exposure variables can be found elsewhere [19].
Village-level IPV norms
IPV norms, measured at follow up, were characterized using one indicator each of (1) village-level prevalence of attitudes justifying physical IPV (injunctive norms) and (2) village-level prevalence of any reported physical IPV (descriptive norms). To measure injunctive norms, participants were asked whether they believe a husband is justified in “hitting or beating his wife” based on five vignettes in which a hypothetical woman in the community engages in behavior perceived as transgressing gender norms by (1) going out without telling her husband, (2) neglecting the children, (3) arguing with her husband, (4) refusing to have sex, and (5) disobeying her mother-in-law [38] (See Supplement 1 for full vignettes). As such, only injunctive norms of physical IPV (and not of sexual or psychological IPV) could be ascertained. Participants were classified as justifying IPV if they indicated “yes” in response to any of the vignettes depicting “unintentional” (in contrast to “willful”) transgressions, consistent with the scoring from other studies of IPV-justifying attitudes [39]. Village prevalence of injunctive norms was calculated by dividing the village sample who justified IPV divided by the village sample size. Three respondents with a missing response to one of the five questions responded “no” to the remaining questions; these were categorized as not justifying IPV. To measure descriptive norms, we calculated the village-level prevalence of any reported physical IPV as the share of the sample within each village who responded “yes” to any exposure to any of the physical IPV questions since baseline, divided by the total village sample size. Finally, to better examine the association between IPV and depression in villages where IPV norms are low, village-level injunctive and descriptive norms were classified into quartiles and then dichotomized; villages in the lowest quartile (quartile 1, “Q1”) were coded as “1” and quartiles 2–4 (“Q2-Q4”) were coded as “0.”
Potential confounders
Potential confounders considered for inclusion were variables theorized to precede and be associated with IPV based on the literature [40, 41], and associated with depression based on bivariate analyses. These variables, collected at baseline, were: age in years, years of schooling for the respondent and her husband; tertiles of household wealth (low, medium, high) derived from a principal component analysis of items including household amenities and assets, the respondent’s parents’ schooling attainment and whether the mother worked; MDE (at baseline); and an indicator of whether the respondent ever witnessed her father hit or beat her mother. Variables associated with both exposure and outcome in our sample (age, MDE at baseline, ever witnessed IPV) were subsequently included as confounders.
Data analysis
We examined bivariate associations between individual-level IPV severity measures (physical IPV frequency and injurious IPV) and quartiles of village-level IPV norms (injunctive and descriptive), using Rao-Scott chi-square tests. To estimate the associations between individual-level IPV severity and MDE, we conducted log-binomial regression using weighted generalized estimating equations with robust standard errors, which accounted for the complex survey design. For each individual-level IPV severity measure (physical IPV frequency and injurious IPV), we generated five adjusted models regressing MDE on: individual-level IPV (Model 1); additionally, the village-level injunctive norms (Model 2) and descriptive norms (Model 3) separately using the dichotomous indicators; and, cross-level interaction terms between individual-level IPV (Level 1) and dichotomous village-level norms (Level 2) separately (Models 4 and 5). These analyses were performed using SAS 9.4 (Cary, NC). Finally, we graphed adjusted risk ratios of main effects incorporating village-level interactions to facilitate interpretation of findings; here, we used R version 3.5.0.
Results
The prevalence of MDE was 16.8% at follow-up and the incidence of physical IPV between baseline and follow-up was 44.4% (Table 1). Two-thirds (n = 2176; 66.4%) experienced physical or sexual IPV (with or without injury) and nearly one-third (n = 984; 30.6%) experienced injurious IPV. The prevalence of less severe IPV exposure—“low” physical IPV frequency and IPV without injury—was 23.5% and 35.8%, respectively. Of those exposed to IPV, these relatively low categories were the most prevalent. Table 1 also provides the prevalence of our village-level variables of interest—injunctive norms (village prevalence of attitudes justifying physical IPV ranged from 1.6% to 49.8% (mean = 18.8%), and descriptive norms (village prevalence of any reported physical IPV) ranged from 9.6% to 76.2% (mean = 43.7%).
Table 1.
Individual- and village-level weighted sample characteristics of married women aged 16–37, rural Bangladesh, 2013–2014
| Mean (SD) or N (%) | ||
|---|---|---|
|
| ||
| Individual-level characteristics (n = 3290) | ||
| Age, years | 24.4 | (3.1) |
| Own education, years | 6.4 | (3.3) |
| Husband’s education, years | 5.6 | (4.2) |
| MDE at follow up | 530 | (16.8%) |
| MDE at baseline | 548 | (18.0%) |
| Household Wealth Index | ||
| Low | 1214 | (33.3%) |
| Medium | 1211 | (33.6%) |
| High | 865 | (33.1%) |
| Ever witnessed father hit or beat mother | 470 | (13.7%) |
| Physical IPV frequency | ||
| None (0) | 1852 | (55.6%) |
| Low (range: 1–2) | 770 | (23.5%) |
| Medium (range: 3–4) | 306 | (9.6%) |
| High (range: 5–26) | 362 | (11.3%) |
| Injurious IPV | ||
| No IPV | 1114 | (33.5%) |
| IPV without injury | 1192 | (35.8%) |
| IPV with injury | 984 | (30.6%) |
| Village-level characteristics (n = 77) | ||
| Injunctive norms | 18.8 | (12.1) |
| Quartiles | ||
| Q1 (range: 1.6, 10.0) | 19 | (24.7%) |
| Q2 (range: 10.2, 16.0) | 19 | (24.7%) |
| Q3 (range: 16.5, 25.9) | 20 | (26.0%) |
| Q4 (range: 26.2, 49.8) | 19 | (24.7%) |
| Descriptive norms | 43.7 | (16.4) |
| Quartiles | ||
| Q1 (range: 9.6, 29.7) | 19 | (24.7%) |
| Q2 (range: 29.8, 45.0) | 19 | (24.7%) |
| Q3 (range: 45.0, 55.9) | 20 | (26.0%) |
| Q4 (range: 56.5, 76.2) | 19 | (24.7%) |
MDE major depressive episode; IPV intimate partner violence
Note. Estimates obtained using complex survey design weights; unweighted standard deviations reported
We did not observe an association between village-level injunctive norms and either measure of IPV at the individual level (Fig. 2). Perhaps consistent with this finding, the village-level correlation between injunctive norms and descriptive norms was weak (Pearson r = 0.12, results not shown). And as expected, both individual-level IPV severity measures (physical IPV frequency and injurious IPV) were associated with village-level descriptive norms.
Fig. 2.
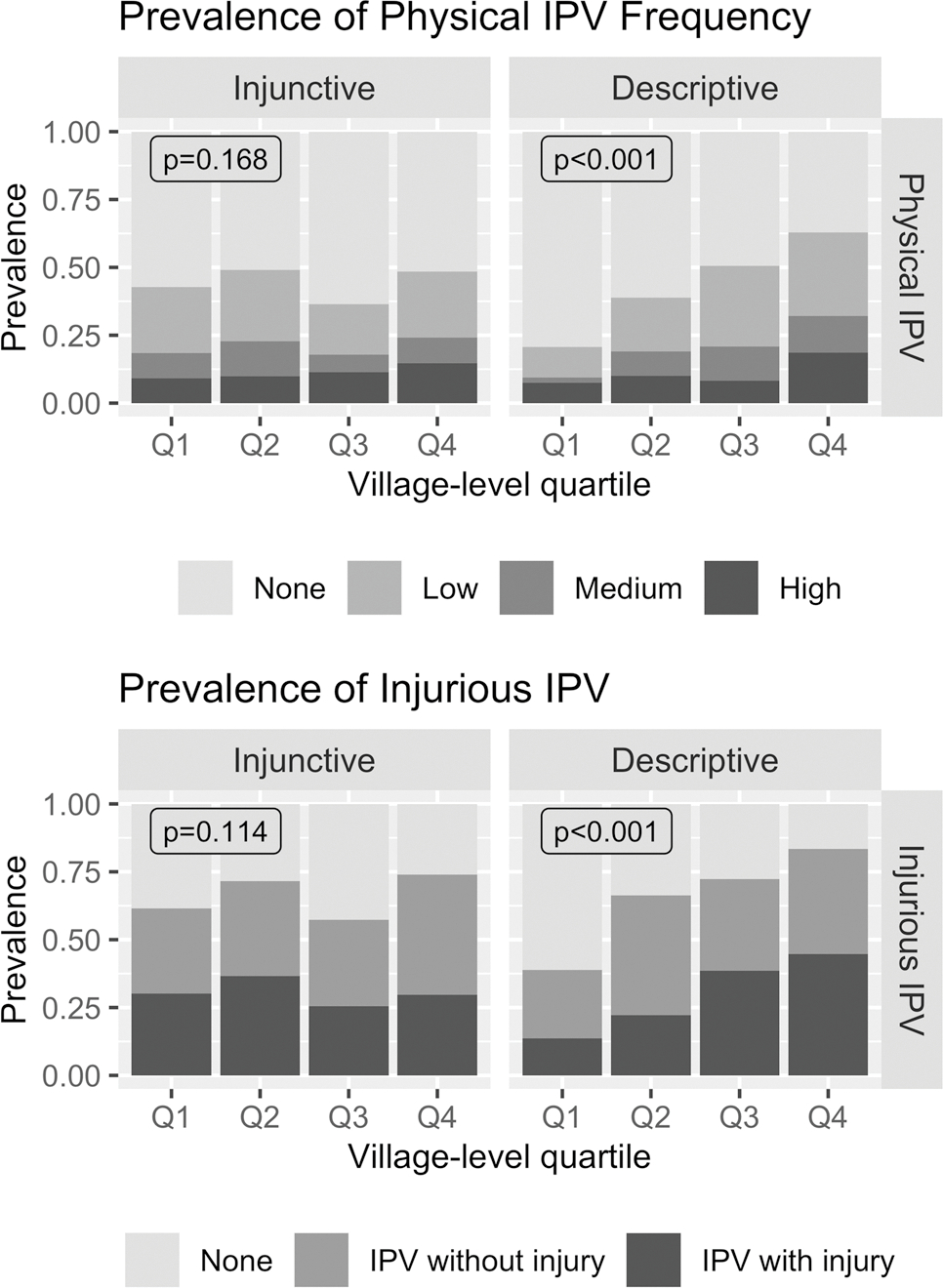
Prevalence of physical IPV severity measures—frequency (top) and injurious IPV (bottom)—by village-level quartiles of injunctive and descriptive norms; p-values were generated from Rao-Scott chi-square tests
In adjusted log-binomial models (Table 2), the risk of MDE increased as the frequency of individual-level IPV worsened (compared to no IPV) across all IPV frequency models. At “low” individual-level physical IPV frequency (versus none) in main effect models, there did not appear to be an elevated risk of MDE (Models 1a, 2a, 3a). Inclusion of injunctive norms as a cross-level interaction term with IPV frequency (Model 4a) resulted in the association between IPV frequency and MDE varying across levels of injunctive norms. Figure 3 illustrates that among women who experienced “low” IPV frequency versus none, those living in villages where IPV is less normative (Q1) have an increased risk of MDE compared to those living in villages where IPV is more normative (Q2–Q4)—interaction RR = 1.42 (95% CI: 0.64, 3.15); RR at Q1 = 1.22; RR at Q2–Q4 = 0.91. This suggests the presence of a contextual-level effect, although estimates for interaction terms are not precise, as indicated by wide confidence bounds. A similar pattern was observed for the cross-level interaction between descriptive norms and IPV frequency of MDE for “low” versus no IPV (Model 5a)—interaction RR = 1.45 (95% CI: 0.82, 2.56); RR at Q1 = 1.48; RR at Q2–Q4 = 0.97. Furthermore, Model 5a also suggests effect modification between descriptive norms and relatively high IPV frequency; that is, the risk of MDE is exacerbated for those exposed to both high IPV frequency (versus none) and living in a village in the lowest quartile of descriptive norms (versus Q2–Q4).
Table 2.
Adjusted risk ratios (RR) of the association between physical IPV frequency and recent MDE among married women aged 16–37, rural Bangladesh, 2013–2014 (n = 3290)
| Model la |
Model 2a |
Model 3a |
Model 4a |
Model 5a |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | |
|
| ||||||||||
| Level 1 | ||||||||||
| Physical IPV frequency | ||||||||||
| None | Ref | Ref | Ref | Ref | Ref | |||||
| Low | 1.01 | (0.80, 1.28) | 1.01 | (0.80, 1.28) | 1.05 | (0.84, 1.30) | 0.91 | (0.67, 1.25) | 0.97 | (0.76, 1.23) |
| Medium | 1.52 | (1.09, 2.12)* | 1.52 | (1.09, 2.12)* | 1.59 | (1.19, 2.13)* | 1.55 | (1.09, 2.20)* | 1.55 | (1.12, 2.15)* |
| High | 2.44 | (1.94, 3.08)*** | 2.44 | (1.94, 3.08)*** | 2.52 | (2.08, 3.07)*** | 2.45 | (1.93,3.12)*** | 2.36 | (1.92, 2.91)*** |
| Level 2 | ||||||||||
| Low injunctive normativity | ||||||||||
| Quartile 1 (lowest) | 0.99 | (0.79, 1.25) | 0.95 | (0.63, 1.43) | ||||||
| Quartiles 2–4 | Ref | Ref | ||||||||
| Low descriptive normativity | ||||||||||
| Quartile 1 (lowest) | 1.19 | (0.87, 1.61) | 1.06 | (0.72, 1.56) | ||||||
| Quartiles 2–4 | Ref | Ref | ||||||||
| Cross-level interactions | ||||||||||
| Low injunctive normativity × physical IPV frequency | Interaction p = 0.489 | |||||||||
| None | Ref | |||||||||
| Low | 1.42 | (0.64,3.15) | ||||||||
| Medium | 0.89 | (0.47, 1.65) | ||||||||
| High | 0.96 | (0.64, 1.43) | ||||||||
| Low descriptive normativity × physical IPV frequency | Interaction p = 0.391 | |||||||||
| None | Ref | |||||||||
| Low | 1.45 | (0.82, 2.56) | ||||||||
| Medium | 0.80 | (0.36, 1.75) | ||||||||
| High | 1.31 | (0.92, 1.86) | ||||||||
All models additionally adjusted for age, MDE at baseline, and ever witnessing father hit/beat mother
Injunctive normativity refers to the prevalence of favorable attitudes toward IPV perpetration among the women interviewed; descriptive normativity refers to the village-level prevalence of physical IPV. Normativity is presented using quartiles, where quartile 1 refers to villages with the least normative views
p<0.001
p<0.01
p<0.05
Fig. 3.
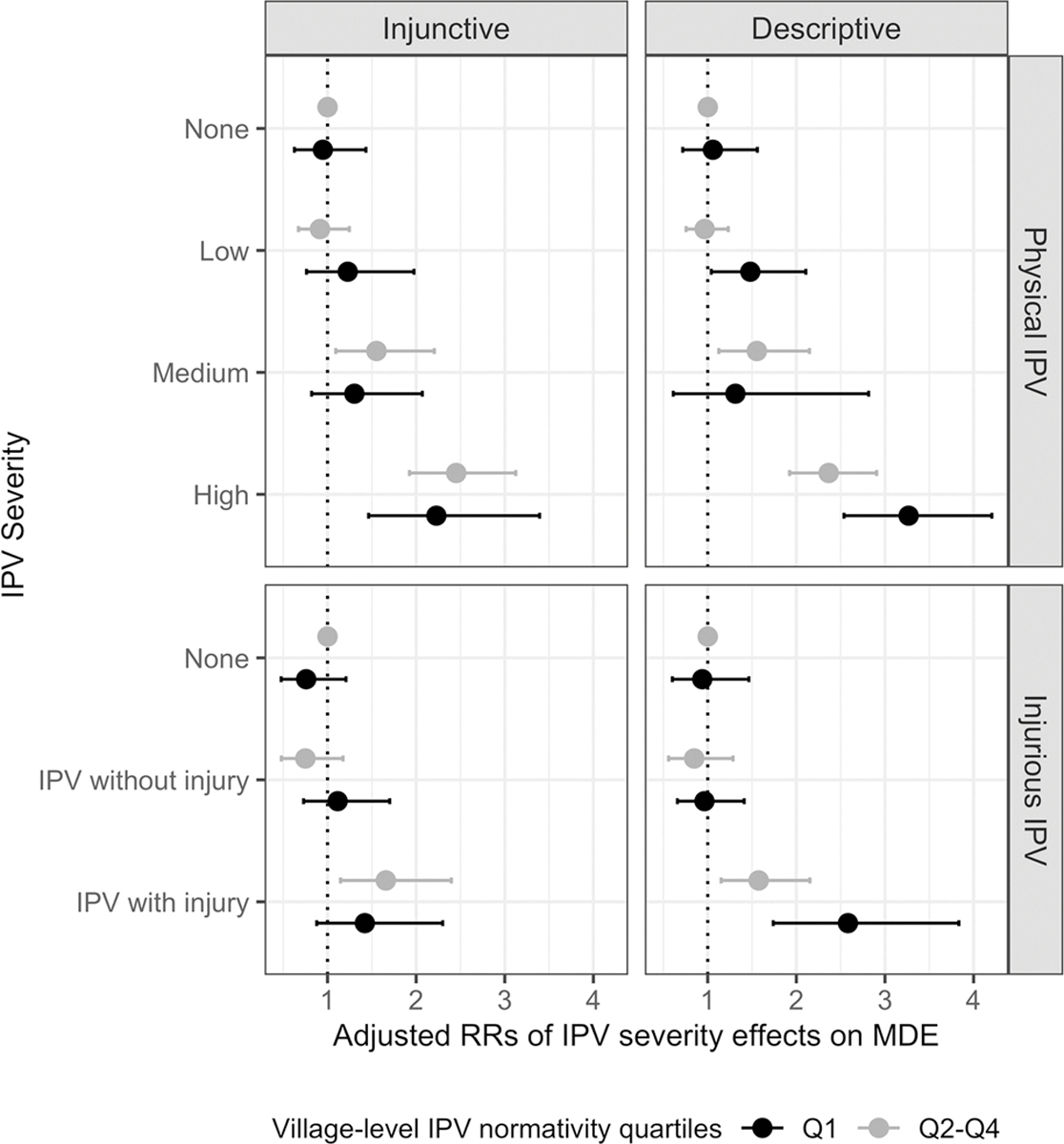
Adjusted RRs of individual-level IPV severity main effects on MDE, incorporating village-level norms interactions: physical IPV frequency and injunctive norms (top left), physical IPV frequency and descriptive norms (top right), injurious IPV and injunctive norms (bottom left), injurious IPV and descriptive norms (bottom right). For all four sets of RRs, reference is “none” at village-level norms quartiles 2–4
Similarly, in models where injurious IPV was the main individual-level exposure (Table 3), the main effect of IPV with injury was associated with an increased risk of MDE, while there was no greater risk associated with IPV without injury, compared to no IPV (Models 1b, 2b, 3b). As observed in the models for physical IPV frequency exposure and in Fig. 3, the inclusion of injunctive norms as a cross-level interaction term with injurious IPV (Model 4b) resulted in a more pronounced positive effect on MDE of individual-level IPV at the lowest level (i.e., non-injurious IPV)—interaction RR = 1.96 (95% CI: 0.97, 3.94); RR at Q1 = 1.11; RR at Q2–Q4 = 0.75. That is, among women who experienced IPV without injury, those living in villages where IPV is less normative (Q1) have an increased risk of MDE compared to those living in villages where IPV is more normative (Q2–Q4), relative to those who report no IPV. This effect, albeit imprecise, was also observed for descriptive norms as a separate cross-level interaction term with the IPV injury variable (Model 5b; interaction RR = 1.21, 95% CI: 0.72, 2.05). Additionally, at the upper end of the interaction, Models 4b and 5b suggest effect modification between village-level norms and injurious IPV—among women who experienced injurious IPV, those living in Q1 villages have an increased risk of MDE compared to those living in Q2-Q4 villages (e.g., Model 5b, comparing injurious IPV to no IPV, interaction RR = 1.75, 95% CI: 1.01, 3.03). However, the risk of MDE was higher, regardless of village context, for those experiencing the greatest severity of IPV across all models. And although patterns are suggestive, statistical tests for heterogeneity of the interaction terms were non-significant (Models 4a, 4b, 5a, 5b).
Table 3.
Adjusted risk ratios (RR) of the association between injurious IPV and recent MDE among married women aged 16–37, rural Bangladesh, 2013–2014 (n = 3290)
| Model lb |
Model 2b |
Model 3b |
Model 4b |
Model 5b |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | |
|
| ||||||||||
| Level 1 | ||||||||||
| Injurious IPV | ||||||||||
| None | Ref | Ref | Ref | Ref | Ref | |||||
| IPV without injury | 0.89 | (0.62, 1.26) | 0.88 | (0.62, 1.27) | 0.93 | (0.66, 1.32) | 0.75 | (0.48, 1.17) | 0.85 | (0.56, 1.29) |
| IPV with injury | 1.72 | (1.23, 2.40)** | 1.72 | (1.23, 2.39)** | 1.84 | (1.35, 2.50)*** | 1.66 | (1.15, 2.40)** | 1.57 | (1.15,2.15)** |
| Level 2 | ||||||||||
| Low injunctive normativity | ||||||||||
| Quartile 1 (lowest) | 0.95 | (0.75, 1.20) | 0.76 | (0.48, 1.21) | ||||||
| Quartiles 2–4 | Ref | Ref | ||||||||
| Low descriptive normativity | ||||||||||
| Quartile 1 (lowest) | 1.22 | (0.92, 1.63) | 0.94 | (0.60, 1.46) | ||||||
| Quartiles 2–4 | Ref | Ref | ||||||||
| Cross-level interactions | ||||||||||
| Low injunctive normativity × injurious IPV | Interaction p = 0.197 | |||||||||
| None | Ref | |||||||||
| IPV without injury | 1.96 | (0.97, 3.94) | ||||||||
| IPV with injury | 1.13 | (0.73, 1.75) | ||||||||
| Low descriptive normativity × injurious IPV | Interaction p = 0.171 | |||||||||
| None | Ref | |||||||||
| IPV without injury | 1.21 | (0.72, 2.05) | ||||||||
| IPV with injury | 1.75 | (1.01,3.03)* | ||||||||
p<0.001
p<0.01
p<0.05
All models additionally adjusted for age, MDE at baseline, and ever witnessing father hit/beat mother
Injunctive normativity refers to the prevalence of favorable attitudes toward IPV perpetration among the women interviewed; descriptive normativity refers to the village-level prevalence of physical IPV. Normativity is presented using quartiles, where quartile 1 refers to villages with the least normative views
Discussion
The purpose of this study was to explore the potential moderating effect of descriptive and injunctive IPV norms on the association between IPV and MDE; it is the first study to our knowledge to do so. In particular, we were interested in explaining the observed null association between MDE and IPV at relatively low levels of IPV severity, which is highly prevalent in South Asia [3].
Regarding the first hypothesis relating the two levels of IPV characterization, we found that village-level descriptive norms (e.g., village IPV prevalence) were associated with both individual-level IPV measures (physical IPV and injurious IPV). However, unlike other studies, we did not observe an association between village-level attitudes justifying IPV (injunctive norms) with either measure of individual IPV severity. This may be due to our measure of IPV attitudes yielding a more conservative estimate of IPV endorsement (19.1%) compared to estimates based on the standard DHS questions (e.g., 28.3% [29]). Levels of IPV-justifying attitudes may vary depending on whether and what type of contextual information is provided—namely, whether the transgression is framed as “willful” or “unintentional” [42, 43]. The present study focused only on IPV-justifying attitudes in reference to unintentional transgressions. In our sample, the prevalence of endorsement when the transgressions were depicted as “willful” was too high and invariant across villages (village-level mean = 93.1; standard deviation = 6.63) to be used in this analysis. Studies based on vignettes depicting unintentional gender transgressions have observed similarly lower estimates compared to the standard DHS questions [38, 43]. Estimates of IPV attitudes based on contextual vignettes can provide important nuanced information about the nature of injunctive norms [38, 42, 43], but actual IPV behavior—which corresponds to descriptive norms—may more closely correlate with measures of attitudes which do not specify the ascribed intentions (e.g., willful or unintentional) of women who are targets of violence.
Regarding the second hypothesis, we found evidence suggestive of effect modification by injunctive norms and descriptive norms, on the association between IPV severity and MDE. Although in Bangladesh IPV is considered a “private matter” and typically not spoken about publicly [44], women living in communities where IPV is tolerated are more likely to tolerate it themselves [45]. Moderating effects of social norms have been observed in studies examining the impacts of mental health on substance use [46, 47] and sexual risk behaviors [48] but the norms pertained to the behavioral outcomes under study. To our knowledge, ours is the first to examine the effect of norms pertaining to the behavioral exposure under study.
One strength of this study is that it was designed to measure village-level determinants of IPV risk prospectively, thus making villages an appropriate contextual-level unit in this study. We characterized contextual norms to measure two different aspects of IPV—what is socially acceptable (injunctive norms), and what is commonly done (descriptive norms). We were also able to control for important confounders, such as previous MDE and witnessing IPV during childhood. Furthermore, our results may be generalized to married women residing in rural villages elsewhere in Bangladesh due to this population-based, nationally-representative rural sample. But there are also some noteworthy limitations. As previously mentioned, our injunctive norms measure may have been too conservative. In addition, injunctive norms could only be ascertained for physical IPV in this study, as respondents were not asked whether they believe a husband is justified in perpetrating psychological or sexual IPV towards his wife. Similarly, although there was no injunctive norm analog for injurious IPV, using one in our analysis would have actually been inconsistent with our primary hypothesis of interest regarding the impact of living in a context, where IPV is less normative, as injurious IPV is universally considered less normative in Bangladesh relative to non-injurious IPV. Overall, the imprecision of the estimates limits the ability to draw definitive conclusions about the role of community norms in moderating the effects of individual-level IPV exposure on mental health outcomes. Although we observed strong variability in norms across the villages in our sample, it is important to note that 66.4% of women in our sample experienced physical or sexual IPV in the past 10 months (with or without injury), and the average village-level IPV prevalence was over 43%, aligning with evidence that IPV risk is higher in South Asia compared to other areas of the world [3]. As a result, we may be somewhat limited to studying the effects of IPV norms—especially descriptive norms—that are potentially above a threshold where they have the biggest impact on the effects of IPV exposure on women’s mental health. Contextual exposures like community norms are important, since they may be more fundamental than individual-level causes for influencing population health, but there are concomitant challenges such as greater measurement error for higher level constructs [49]. Nonetheless, our findings are suggestive and merit investigation in further research, perhaps through the use of measures of community norms without the above-mentioned limitations.
Our results suggest that in IPV-endemic contexts such as rural Bangladesh, the psychological impact of relatively low levels of IPV exposure, which are fairly prevalent, may vary depending on community-level attitudes toward IPV. If replicated in other studies, these findings have important implications for the interpretation of observed null associations between IPV exposure and mental health sequelae. In communities where IPV is less normative, there may be a heightened risk for depression among those experiencing relatively low levels of IPV, compared to communities where IPV is more normative. It follows that these results also suggest IPV prevention strategies aimed at denormalizing IPV may unintentionally worsen mental health among women who continue to experience it.
Supplementary Material
Funding
This work was supported by the National Institute of Child Health and Development (1R01HD061630–01A1; PI: Schuler) and the National Institute of Mental Health (T32-MH1304348; Esie).
Footnotes
Conflict of interest The authors declare no conflict of interest.
Compliance with ethical standards
Ethical statement This study was approved by the Institutional Review Boards of the International Center for Diarrheal Disease Research, Bangladesh (ICDDR,b) and FHI 360.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s00127-021-02044-6.
References
- 1.Heise L, Garcia-Moreno C (2002) Chapter 4: violence by intimate partners. In: Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R (eds) World report on violence and health. World Health Organization, Geneva, Switzerland [Google Scholar]
- 2.Krantz G, Garcia-Moreno C (2005) Violence against women. J Epidemiol Commun Health 59(10):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO (2013) Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization, Geneva, Swizerland [Google Scholar]
- 4.Bangladesh Bureau of Statistics (2016) Report on violence against women (VAW) survey 2015. Bangladesh Bureau of Statistics [Google Scholar]
- 5.Golding JM (1999) Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence 14(2):99–132 [Google Scholar]
- 6.Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB (2012) Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Soc Sci Med 75(6):959–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pico-Alfonso MA (2005) Psychological intimate partner violence: the major predictor of posttraumatic stress disorder in abused women. Neurosci Biobehav Rev 29(1):181–193 [DOI] [PubMed] [Google Scholar]
- 8.Parvin K, Mamun MA, Gibbs A, Jewkes R, Naved RT (2018) The pathways between female garment workers’ experience of violence and development of depressive symptoms. PLoS ONE 13(11):e0207485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gausia K, Fisher C, Ali M, Oosthuizen J (2009) Antenatal depression and suicidal ideation among rural Bangladeshi women: a community-based study. Arch Womens Ment Health 12(5):351. [DOI] [PubMed] [Google Scholar]
- 10.Islam MJ, Broidy L, Baird K, Mazerolle P (2017) Intimate partner violence around the time of pregnancy and postpartum depression: The experience of women of Bangladesh. PLoS ONE 12(5):e0176211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kabir ZN, Nasreen H-E, Edhborg M (2014) Intimate partner violence and its association with maternal depressive symptoms 6–8 months after childbirth in rural Bangladesh. Glob Health Action 7:24725. 10.3402/gha.v3407.24725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De PK, Murshid NS (2018) Associations of intimate partner violence with screening for mental health disorders among women in urban Bangladesh. Int J Public Health 63(8):913–921 [DOI] [PubMed] [Google Scholar]
- 13.Rogathi JJ, Manongi R, Mushi D, Rasch V, Sigalla GN, Gammeltoft T, Meyrowitsch DW (2017) Postpartum depression among women who have experienced intimate partner violence: a prospective cohort study at Moshi, Tanzania. J Affect Disord 218:238–245 [DOI] [PubMed] [Google Scholar]
- 14.Rodriguez MA, Valentine J, Ahmed SR, Eisenman DP, Sumner LA, Heilemann MV, Liu H (2010) Intimate partner violence and maternal depression during the perinatal period: a longitudinal investigation of Latinas. Violence Against Women 16(5):543–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ouellet-Morin I, Fisher HL, York-Smith M, Fincham-Campbell S, Moffitt TE, Arseneault L (2015) Intimate partner violence and new-onset depression: a longitudinal study of women’s childhood and adult histories of abuse. Depress Anxiety 32(5):316–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridings LE, Beasley LO, Bohora SB, Daer JL, Owora A, Silovsky J (2018) Longitudinal investigation of depression, intimate partner violence, and supports among vulnerable families. J Interpers Violence 33(24):3749–3771 [DOI] [PubMed] [Google Scholar]
- 17.Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ (2016) Intimate partner violence and depression symptom severity among South African women during pregnancy and postpartum: population-based prospective cohort study. PLoS Med 13(1):e1001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim J, Lee J (2013) Prospective study on the reciprocal relationship between intimate partner violence and depression among women in Korea. Soc Sci Med 99:42–48 [DOI] [PubMed] [Google Scholar]
- 19.Esie P, Osypuk TL, Schuler SR, Bates LM (2019) Intimate partner violence and depression in rural Bangladesh: accounting for violence severity in a high prevalence setting. SSM Popul Health 7:100368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deyessa N, Berhane Y, Alem A, Ellsberg M, Emmelin M, Hogberg U, Kullgren G (2009) Intimate partner violence and depression among women in rural Ethiopia: a cross-sectional study. Clin Pract Epidemiol Mental Health 5(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shamu S, Zarowsky C, Roelens K, Temmerman M, Abrahams N (2016) High-frequency intimate partner violence during pregnancy, postnatal depression and suicidal tendencies in Harare. Zimbabwe Gen Hosp Psychiatry 38(1):109–114 [DOI] [PubMed] [Google Scholar]
- 22.Miszkurka M, Zunzunegui MV, Goulet L (2012) Immigrant status, antenatal depressive symptoms, and frequency and source of violence: what’s the relationship? Arch Womens Ment Health 15(5):387–396 [DOI] [PubMed] [Google Scholar]
- 23.Cialdini RB (2012) The focus theory of normative conduct. Handbook of theories of social psychology, vol 2. Sage Publications Ltd, Thousand Oaks, CA, pp 295–312 [Google Scholar]
- 24.Vanderende KE, Yount KM, Dynes MM, Sibley LM (2012) Community-level correlates of intimate partner violence against women globally: a systematic review. Soc Sci Med 75(7):1143–1155 [DOI] [PubMed] [Google Scholar]
- 25.Linos N, Slopen N, Subramanian SV, Berkman L, Kawachi I (2013) Influence of community social norms on spousal violence: a population-based multilevel study of Nigerian women. Am J Public Health 103(1):148–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyle MH, Georgiades K, Cullen J, Racine Y (2009) Community influences on intimate partner violence in India: Women’s education, attitudes towards mistreatment and standards of living. Soc Sci Med 69(5):691–697 [DOI] [PubMed] [Google Scholar]
- 27.Clark CJ, Ferguson G, Shrestha B, Shrestha PN, Oakes JM, Gupta J, McGhee S, Cheong YF, Yount KM (2018) Social norms and women’s risk of intimate partner violence in Nepal. Soc Sci Med 202:162–169 [DOI] [PubMed] [Google Scholar]
- 28.Heise LL, Kotsadam A (2015) Cross-national and multilevel correlates of partner violence: an analysis of data from population-based surveys. Lancet Glob Health 3(6):e332–e340 [DOI] [PubMed] [Google Scholar]
- 29.National Institute of Population Research and Training MaA, and ICF International (2016) Bangladesh demographic and health survey 2014. NIPORT, Mitra and Associates, ICF International, Dhaka, Bangladesh and Calverton, Maryland [Google Scholar]
- 30.Yount KM, Crandall A, Cheong YF, Osypuk TL, Bates LM, Naved RT, Schuler SR (2016) Child marriage and intimate partner violence in rural Bangladesh: a longitudinal multilevel analysis. Demography 53(6):1821–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150(6):782–786 [DOI] [PubMed] [Google Scholar]
- 32.Gausia K, Fisher C, Algin S, Oosthuizen J (2007) Validation of the Bangla version of the Edinburgh Postnatal Depression Scale for a Bangladeshi sample. J Reprod Infant Psychol 25(4):308–315 [Google Scholar]
- 33.Cox JL, Chapman G, Murray D, Jones P (1996) Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. J Affect Disord 39(3):185–189 [DOI] [PubMed] [Google Scholar]
- 34.Matijasevich A, Munhoz TN, Tavares BF, Barbosa APPN, da Silva DM, Abitante MS, Dall’Agnol TA, Santos IS (2014) Validation of the Edinburgh postnatal depression scale (EPDS) for screening of major depressive episode among adults from the general population. BMC Psychiatry 14(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santos IS, Tavares BF, Munhoz TN, Manzolli P, de Ávila GB, Jannke E, Matijasevich A (2016) Patient health questionnaire-9 versus Edinburgh postnatal depression scale in screening for major depressive episodes: a cross-sectional population-based study. BMC Res Notes 9(1):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB (1996) The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues 17(3):283–316 [Google Scholar]
- 37.Garcia-Moreno C, Jansen HAFM, Ellsberg M, Heise L, Watts C (2005) WHO multi-country study on women’s health and domestic violence against women: initial results on prevalence, health outcomes and women’s responses. World Health Organization, Geneva, Switzerland [Google Scholar]
- 38.Schuler SR, Lenzi R, Yount KM (2011) Justification of intimate partner violence in rural Bangladesh: what survey questions fail to capture. Stud Family Plann 42(1):21–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krause KH, Haardorfer R, Yount KM (2017) Individual schooling and women’s community-level media exposure: a multilevel analysis of normative influences associated with women’s justification of wife beating in Bangladesh. J Epidemiol Community Health 71(2):122–128 [DOI] [PubMed] [Google Scholar]
- 40.Islam MJ, Mazerolle P, Broidy L, Baird K (2021) Exploring the prevalence and correlates associated with intimate partner violence during pregnancy in Bangladesh. J Interpers Violence. 36(1–2):663–690 [DOI] [PubMed] [Google Scholar]
- 41.Abramsky T, Watts CH, Garcia-Moreno C, Devries K, Kiss L, Ellsberg M, Jansen HAFM, Heise L (2011) What factors are associated with recent intimate partner violence? findings from the WHO multi-country study on women’s health and domestic violence. BMC Public Health 11(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsai AC, Kakuhikire B, Perkins JM, Vořechovská D, McDonough AQ, Ogburn EL, Downey JM, Bangsberg DR (2017) Measuring personal beliefs and perceived norms about intimate partner violence: population-based survey experiment in rural Uganda. PLoS Med 14(5):e1002303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yount KM, Halim N, Schuler SR, Head S (2013) A survey experiment of women’s attitudes about intimate partner violence against women in rural Bangladesh. Demography 50(1):333–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Naved R, Samuels F, Masson V, Talukder A, Gupta T, Yount K (2017) Understanding intimate partner violence in rural Bangladesh: prevention and response. Overseas Development Institute, London, England [Google Scholar]
- 45.Jesmin SS (2015) Married women’s justification of intimate partner violence in Bangladesh: examining community norm and individual-level risk factors. Violence Vict 30(6):984–1003 [DOI] [PubMed] [Google Scholar]
- 46.Pedersen ER, Miles JNV, Hunter SB, Osilla KC, Ewing BA, D’Amico EJ (2013) Perceived norms moderate the association between mental health symptoms and drinking outcomes among at-risk adolescents. J Stud Alcohol Drugs 74(5):736–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zehe JM, Colder CR, Read JP, Wieczorek WF, Lengua LJ (2013) Social and generalized anxiety symptoms and alcohol and cigarette use in early adolescence: the moderating role of perceived peer norms. Addict Behav 38(4):1931–1939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hill LM, Moody J, Gottfredson NC, Kajula LJ, Pence BW, Go VF, Maman S (2018) Peer norms moderate the association between mental health and sexual risk behaviors among young men living in Dar es Salaam, Tanzania. Soc Sci Med 196:77–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roux AVD (2001) Investigating neighborhood and area effects on health. Am J Public Health 91(11):1783–1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


