Abstract
The 2022 outbreak of monkeypox virus infection has expanded far beyond regions in which the disease was previously endemic. Monkeypox has a wide range of manifestations, some of which are unique to this outbreak. Novel clinical presentations, testing limitations, and a lack of available treatments have contributed to delays in recognition, diagnosis, and treatment of monkeypox. As health care workers and governments fight this rare viral infection, which may become a routine diagnosis, early recognition of potential signs and symptoms along with appropriate testing is essential to prevent continuing spread and potential endemicity.
Keywords: monkeypox, MPX, lesions, tecovirimat, Tpoxx, JYNNEOS, proctitis
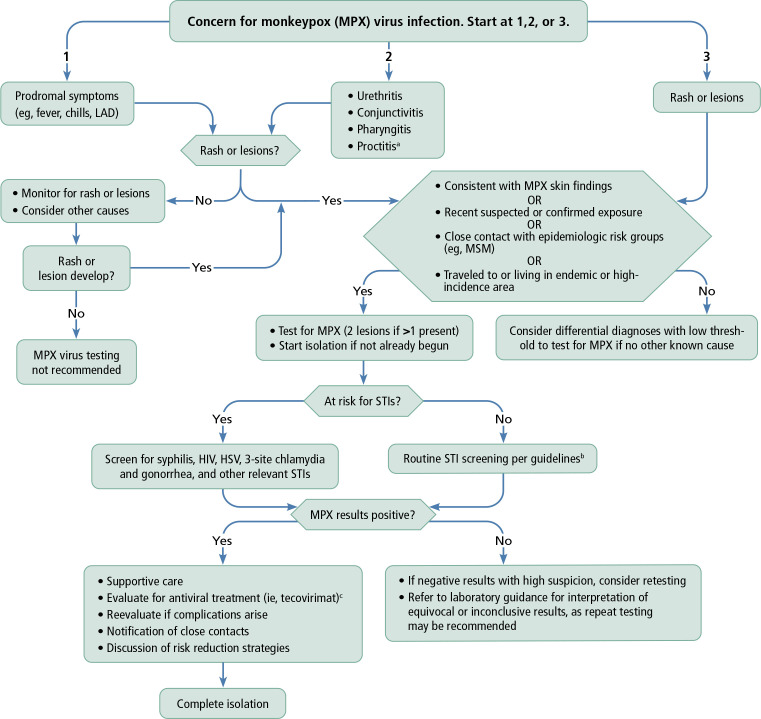
Many parts of the world are currently experiencing an outbreak of monkeypox virus infection, with more than 100 countries reporting cases.1 Monkeypox is a rare viral infection that can cause fever, chills, lymphadenopathy, fatigue, myalgia, cough, and, characteristically, skin lesions or rash.1,2 Patients may present with prodromal symptoms, rash, or lesions, or sometimes unexpected manifestations such as proctitis, urethritis, or conjunctivitis (Figure 1).3,4 The skin lesions seen in monkeypox can vary widely in appearance and may include papules, pustules, umbilicated lesions, ulcers, or morbilliform rash (Figures 2, 3, 4, and 5). Classically, most lesions are deep-seated and well circumscribed and progress through a series of stages.1,2 Lesions or rash can appear anywhere on the body, with predominance in the genital and anorectal areas in the current outbreak.5,6 Interestingly, monkeypox virus has been detected on rectal swabs of at-risk but asymptomatic individuals despite the absence of skin lesions, raising concern about the possibility of asymptomatic transmission of the virus.7
Figure 1.
Flowchart for an approach to monkeypox virus infection.
Abbreviations: HSV, herpes simplex virus; LAD, lymphadenopathy; MSM, men who have sex with men; STI, sexually transmitted infection.
aSome presentations of MPX can start without prodromal symptoms or visible skin changes. As current testing recommends sampling of skin lesions, if a patient presents with symptoms such as urethritis, conjunctivitis, pharyngitis, or particularly proctitis, perform careful evaluation for lesions at areas such as the urinary meatus, inner eyelids, mouth, pharynx, and perirectal region. If no lesions are found, in cases of proctitis consider a rectal mucosal swab to test for monkeypox virus if testing is available.
bRefer to Centers for Disease Control and Prevention STI Treatment Guidelines, 2021.
cRefer to Centers for Disease Control and Prevention guidance for antiviral eligibility criteria.
Figure 2.
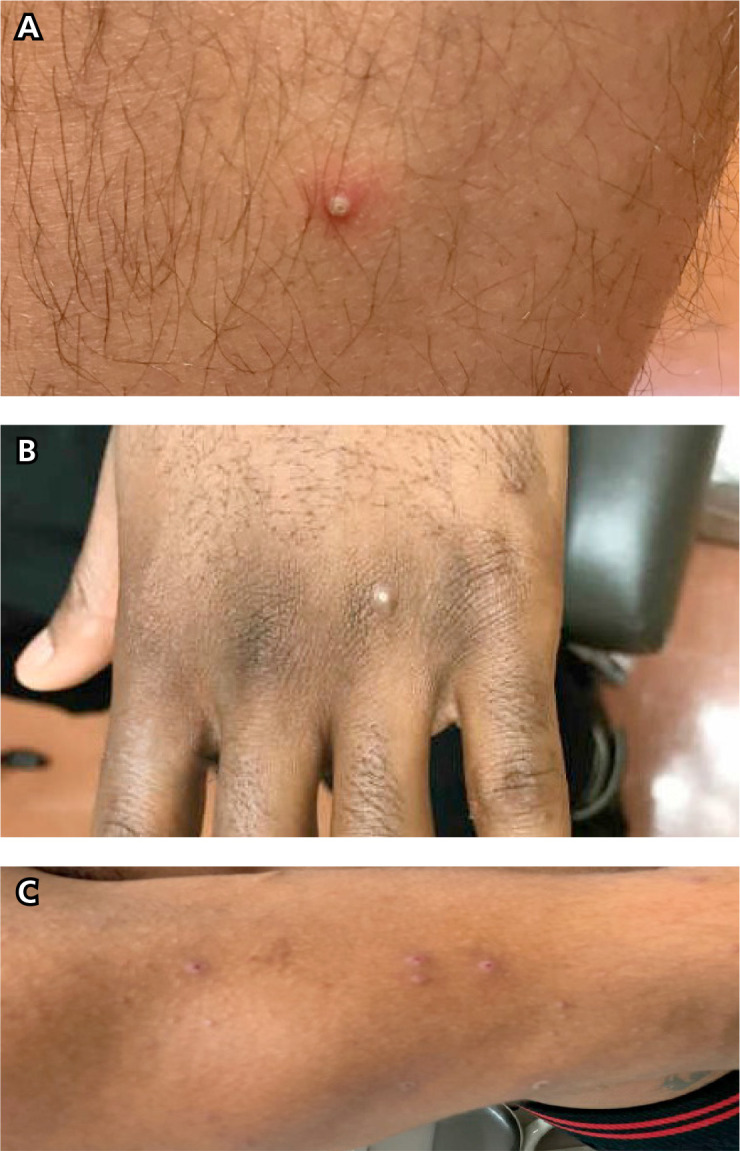
A and B: Pustule-like lesions on a limb and dorsal hand. C: Cluster of papules, some with umbilication.
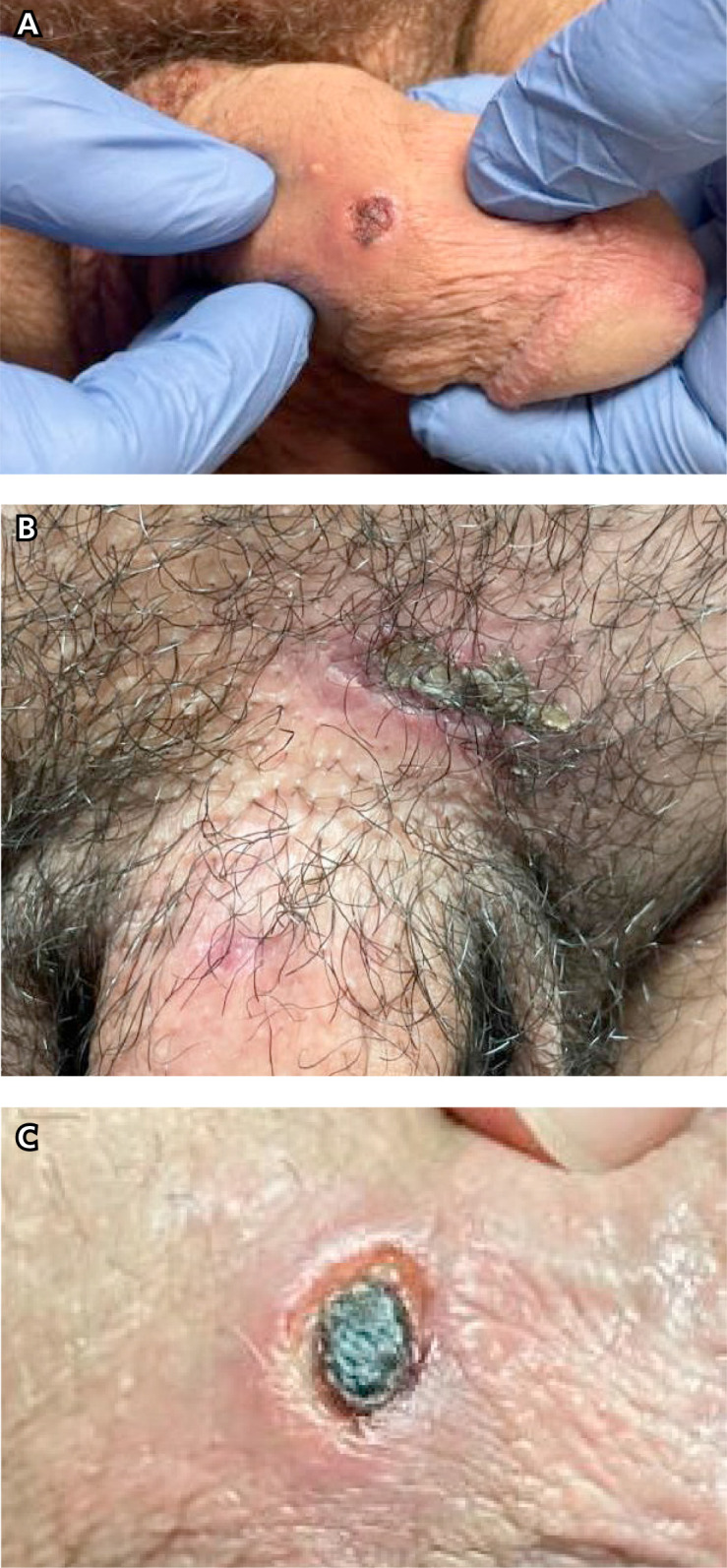
Figure 3.
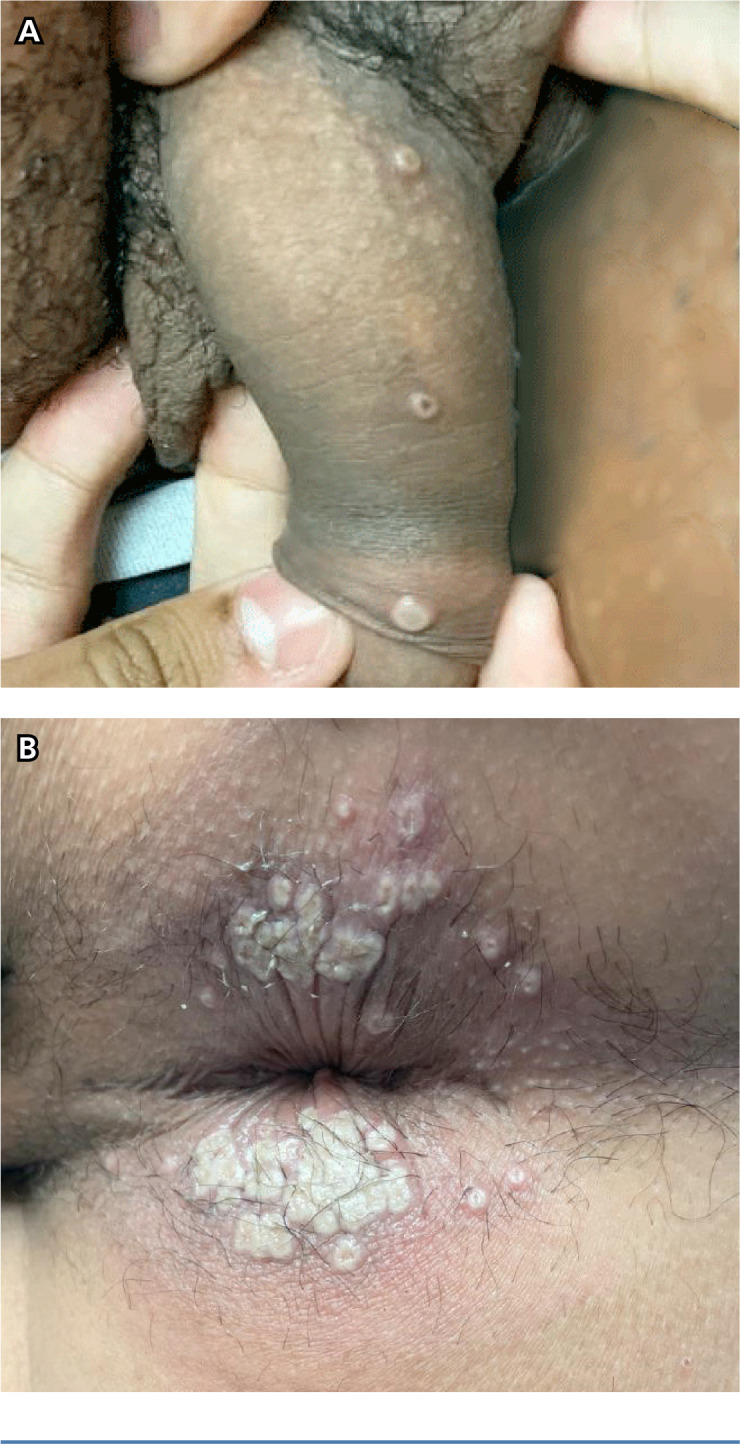
A: Umbilicated lesion on penis. B: Cluster of papules in the perianal region, many with umbilication.
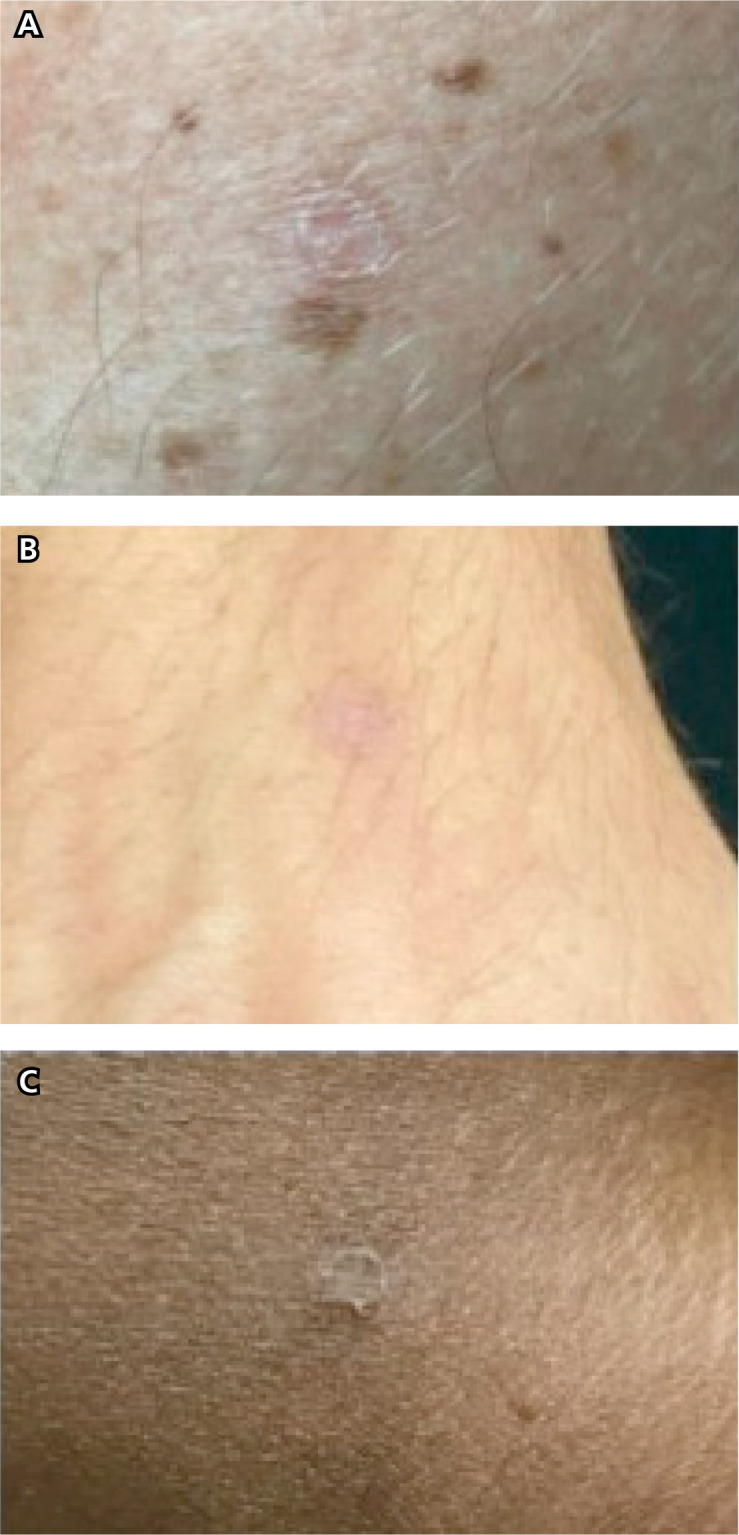
Figure 4.
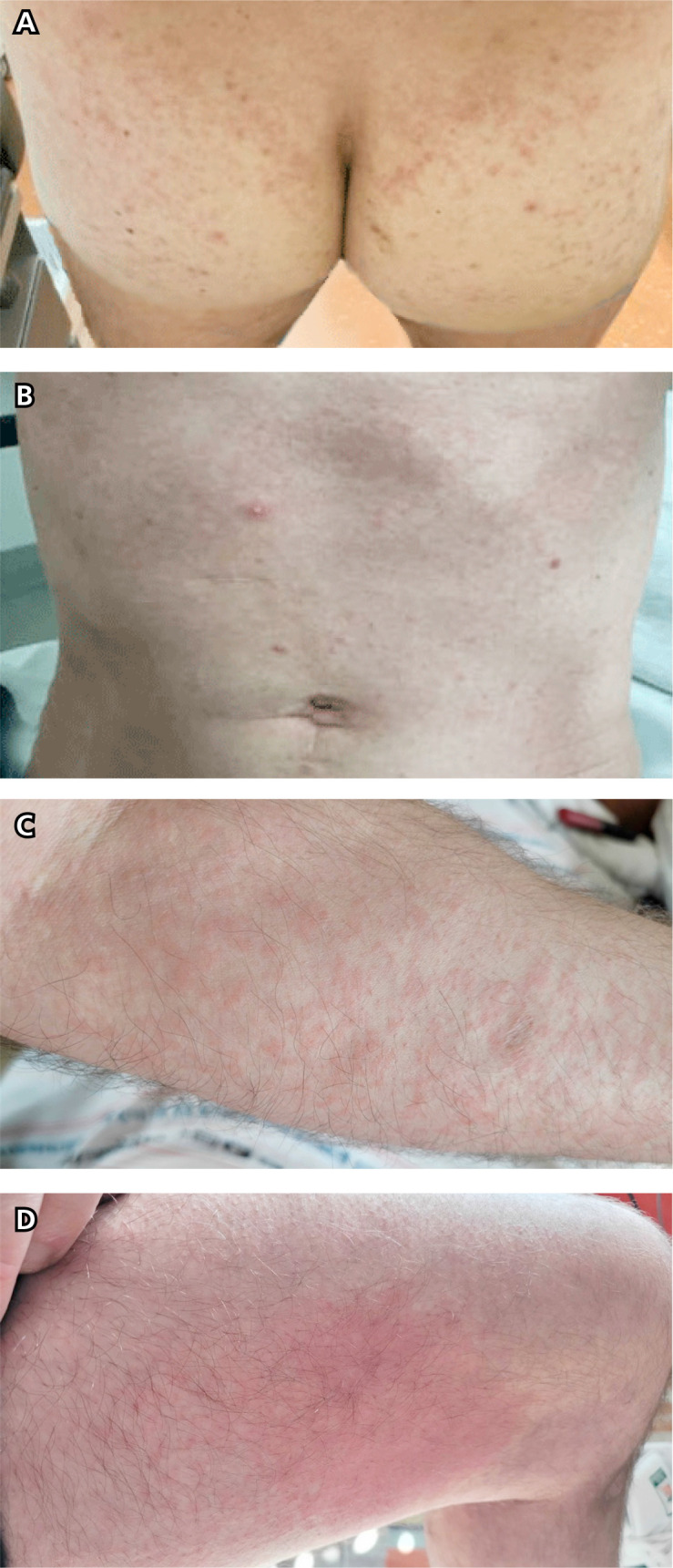
Morbilliform rash on buttocks (A), lower trunk (B), and forearm (C). D: Morbilliform rash on thigh with area of confluent rash.
Figure 5.

A: Ulcerations on palate and tonsil. B: Ulceration on penis. C: Ulcerations on penis and pubis.
The evolving definition of suspected monkeypox according to the Centers for Disease Control and Prevention (CDC) is a rash consistent with monkeypox and a high degree of clinical suspicion in patients who, within 21 days of symptom onset, had contact with a suspected or known case; close contact with men who have sex with men, especially if contact was made via dating or hookup websites, apps, or parties; or traveled to an area where there are confirmed cases or the disease is endemic. Given that tens of thousands of cases have been identified across the United States, having traveled abroad is no longer an essential clue to diagnosis.
Testing for monkeypox virus should be ordered for any suspected case. Although testing for the presence of monkeypox virus can be performed with cerebrospinal fluid, urine, blood, breast milk, or genital swabs in the absence of lesions, the only type of testing that has been cleared by the US Food and Drug Administration (FDA) to date is lesion based because of insufficient clinical data to support other sample types and the risk of inaccurate results.8 This means that, under current recommendations, if a patient presents with prodromal symptoms but without rash or skin changes, they should be monitored for the development of lesions. If none appear within approximately 5 days, they are unlikely to be infected with monkeypox, and testing is not recommended according to current CDC guidelines.1 Similarly, if a patient presents with a manifestation such as proctitis, urethritis, conjunctivitis, or pharyngitis, testing is recommended if they have lesions. A thorough physical examination should be performed in these cases to identify any nonapparent lesions, which may be occult in the inner eyelids, mouth, pharynx, perirectal region, urinary meatus, or other areas, depending on the location of symptoms. An anoscopy to look for deeper lesions in the anal mucosa can be considered if a patient presents with proctitis without visible lesions in the perianal region.4 If no lesions are identified, these patients should be monitored for lesion development in accordance with testing guidance from the CDC. This guidance does have limitations in cases of occult lesions or delayed appearance of lesions, or if asymptomatic transmission of the virus is confirmed. Therefore, while nonlesion monkeypox tests are not currently approved by the FDA, their use could be considered on a case-by-case basis, depending on provider suspicion. However, if a patient does not have major risk factors for monkeypox and their illness seems inconsistent with the disease, differential diagnoses to consider include syphilis, herpes simplex virus, primary varicella virus, varicella zoster virus, molluscum contagiosum, lymphogranuloma venereum, gonorrhea, enterovirus (including coxsackievirus) infection, and fungal infections.
Once a patient is suspected to have a monkeypox virus infection, they should begin isolation while test results are pending. Given high rates of concurrent sexually transmitted infections, it is recommended that patients who are at risk of such infections (ie, those with multiple sexual partners, anonymous partners, or new partners) also be screened for coinfections, which can include syphilis, HIV infection, herpes simplex virus infection, and triple-site pharyngeal, urinary, and rectal gonorrhea and chlamydia.1,5
In suspected or confirmed cases of monkeypox, the mainstay of treatment is symptomatic management. Therapy should target oral, genital, and anorectal pain; pruritus; fever; proctitis, if present; and keeping skin lesions clean. Treatment options include oral salt and anesthetic rinses, topical anesthetics, sitz or oatmeal baths, stool softeners, pain medication, oral or topical antihistamines, or other nonirritant gels or lotions such as calamine or menthol.9 Some patients develop severe pain requiring multimodal oral pain management regimens that may include opioids. Most patients recover with symptom management alone, but those who are at high risk of severe disease, have involvement of anatomic areas that might result in serious sequelae from scarring or strictures, or experience complications should be evaluated for eligibility to receive the antiviral tecovirimat, currently available through a CDC-sponsored expanded access program or clinical trials.10,11 Although tecovirimat may shorten the duration of illness, it is not approved by the FDA, its efficacy is unknown, and its low genetic barrier to resistance has raised concerns.12
Typical illness courses of monkeypox last, on average, 2 to 4 weeks.1,2,6 Complications of this viral infection can include bacterial superinfection of lesions, gastroenteritis, bronchopneumonia, encephalomyelitis, sepsis, uncontrolled pain, spread of infection to eyes, scars, and strictures (Figure 6).1,5,9 Any symptoms that raise concerns about complications should prompt reevaluation. If a patient’s sample tests positive, they should inform recent close contacts so those individuals may monitor themselves for symptoms and be evaluated for postexposure prophylaxis, which in most cases is accomplished with prompt vaccination.
Figure 6.
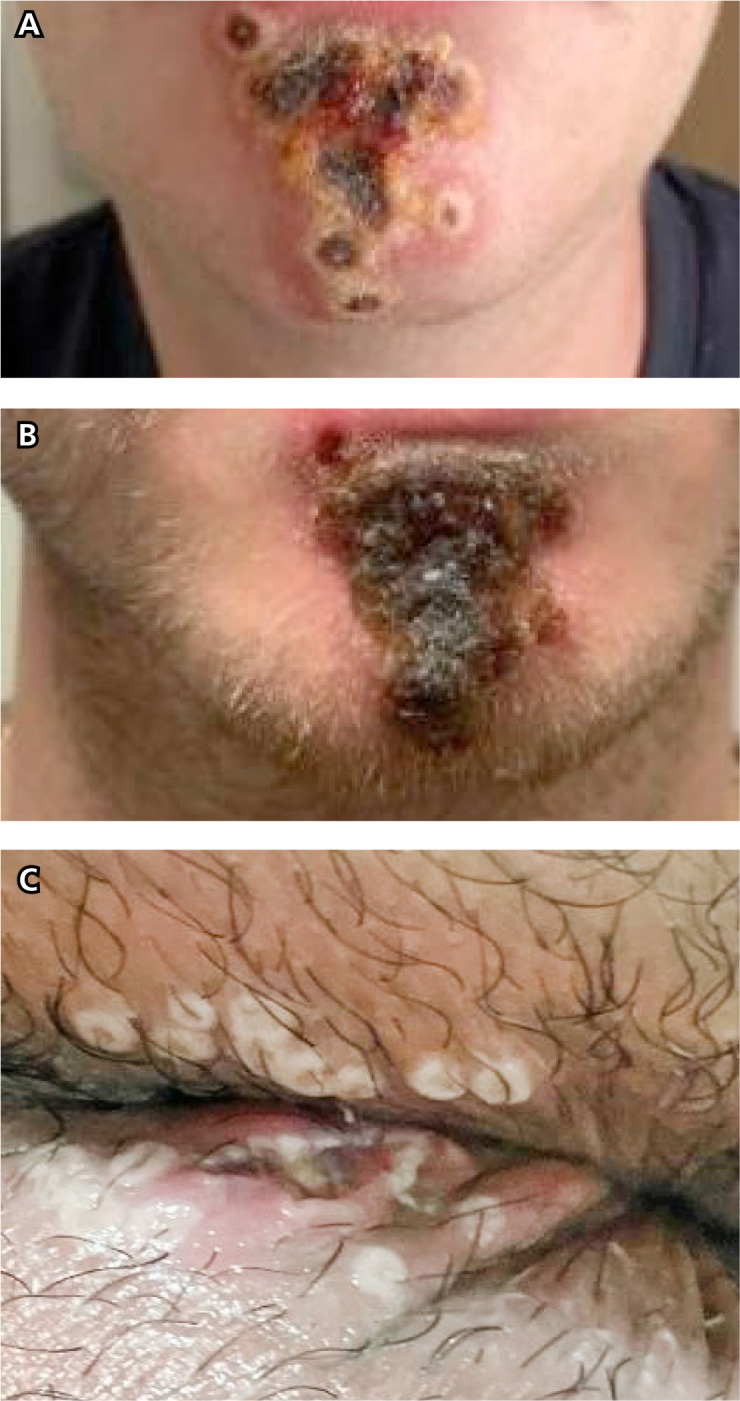
Complications of monkeypox. A: Secondary infection of chin lesions. B: Appearance of infection shown in panel A 5 days later. C: Fissure and ulceration in the perianal region surrounded by papules and umbilicated lesions.
Methods to prevent the spread of monkeypox include vaccination for those who are eligible as well as behavioral changes regarding sex practices to reduce infection risk. JYNNEOS, a live nonreplicating virus vaccine, is the primary vaccine in use in the United States during the current outbreak. Although the efficacy of JYNNEOS in preventing monkeypox virus infection in this outbreak is unknown, early data suggest that there is a lower incidence of infection among individuals with even 1 dose of the 2-dose vaccine series compared with unvaccinated individuals.1,13 Other infection risk reduction strategies include discussing symptoms of monkeypox with partners, avoiding or delaying close or intimate contact with someone who may be symptomatic or has a pending monkeypox test, and avoiding sharing linens, sex toys, and personal grooming items.1,9 Those infected with monkeypox should isolate until all skin lesions have scabbed (Figure 7) and fallen off, with the formation of new skin (Figure 8).
Figure 7.
Scabbed lesions. A: On penis; note the varying stages of lesions present with adjacent pustule. B: Progression of ulcerated lesions shown in Figure 5C; note the reepithelization of the penile shaft lesion and scabbing of the pubic ulceration. C: Scabbed lesion.
Figure 8.
A, B, and C: Resolution of lesions.
Given the many challenges that arose in the early part of this outbreak, some of which continue today, it is unlikely that this infection will be eradicated, which means that ongoing knowledge of and ability to manage monkeypox infections may become part of everyday clinical care.
Footnotes
This invited review was submitted in September 2022 and accepted for publication in September 2022.
Financial relationships with ineligible companies in the past 24 months: Dr Torres has no relevant financial relationships with ineligible companies to disclose. (Updated 8/30/22) Dr Ellsworth has no relevant financial relationships with ineligible companies to disclose. (Updated 4/01/22). Dr Zucker has no relevant financial relationships with ineligible companies to disclose. (Updated 9/21/22) Dr Glesby has received research grants awarded to his institution from Gilead Sciences, Inc., and Regeneron Pharmaceuticals; and has served as a consultant to ReAlta Life Sciences, Inc., and Swedish Orphan Biovitrum. (Updated 8/30/22)
References
- 1. Monkeypox. Centers for Disease Control and Prevention. https://www.cdc.gov/poxvirus/monkeypox/. 2022. Accessed October 15, 2022.
- 2. Monkeypox. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/monkeypox. 2022. Accessed October 15, 2022.
- 3. Benatti SV, Venturelli S, Comi N, Borghi F, Paolucci S, Baldanti F. Ophthalmic manifestation of monkeypox infection. Lancet Infect Dis. 2022;22(9):1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Basgoz N, Brown CM, Smole SC, et al. Case 24-2022: a 31-year-old man with perianal and penile ulcers, rectal pain, and rash. N Engl J Med. 2022;387(6):547–556. [DOI] [PubMed] [Google Scholar]
- 5. Patrocinio-Jesus R, Peruzzu F. Monkeypox genital lesions. N Engl J Med. 2022;387(1):66. [DOI] [PubMed] [Google Scholar]
- 6. Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries — April-June 2022. N Engl J Med. 2022;387(8):679–691. [DOI] [PubMed] [Google Scholar]
- 7. De Baetselier I, Van Dijck C, Kenyon C, et al. Retrospective detection of asymptomatic monkeypox virus infections among male sexual health clinic attendees in Belgium. Nat Med. Published online August 12, 2022. doi: 10.1038/s41591-022-02004-w [DOI] [PMC free article] [PubMed]
- 8. Monkeypox update: FDA takes significant action to help expand access to testing. https://www.fda.gov/news-events/press-announcements/monkeypox-update-fda-takes-significant-action-help-expand-access-testing. 2022. Accessed September 17, 2022.
- 9. Monkeypox: what to do when sick. NYC Health. https://www1.nyc.gov/site/doh/health/health-topics/monkeypox-when-sick.page. 2022. Accessed September 14, 2022.
- 10. O’Laughlin K, Tobolowsky FA, Elmor R, et al. Clinical use of tecovirimat (Tpoxx) for treatment of monkeypox under an investigational new drug protocol-United States, May-August 2022. Morb Mortal Wkly Rep. 2022; 71(37):1190–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Study of tecovirimat for human monkeypox virus (STOMP). ClinicalTrials.gov identifier: NCT05534984. https://clinicaltrials.gov/ct2/show/NCT05534984. September 10, 2022. Accessed September 20, 2022.
- 12. FDA Monkeypox response. U.S. Food and Drug Administration. https://www.fda.gov/emergency-pre-paredness-and-response/mcm-issues/fda-monkeypoxresponse#therapeutics. 2022. Accessed September 16, 2022. [Google Scholar]
- 13. Payne AB, Ray LC, Kugeler KJ, et al. Incidence of monkeypox among unvaccinated persons compared with persons receiving ≥ 1 JYNNEOS vaccine dose — 32 U.S. jurisdictions, July 31-September 3, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(40):1278–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]