Abstract
Human immunoglobulin G2 (IgG2) serum concentrations and the IgG2 antibody response to Actinobacillus actinomycetemcomitans can be influenced by genes, by environmental factors such as smoking, and by periodontal disease status. Examination of the IgG2 response to phosphorylcholine (PC), a response thought to be mainly induced by the C polysaccharide of Streptococcus pneumoniae, suggested that periodontal disease status was also associated with this response. This prompted the hypothesis that PC is an important oral antigen associated with organisms in the periodontal flora and that anti-PC antibody is elevated as a consequence of periodontal disease. Subjects in various periodontal disease diagnostic categories in which attachment loss is exhibited were tested for anti-PC in serum. Those with adult periodontitis, localized juvenile periodontitis, generalized early-onset periodontitis, and gingival recession all had similar levels of anti-PC IgG2 serum antibody which were significantly greater than in the group of subjects with no attachment loss. Analysis of plaque samples from subgingival and supragingival sites in all diseases categories for reactivity with the anti-PC specific monoclonal antibody TEPC-15 revealed that a substantial proportion of the bacteria in dental plaque (30 to 40%) bear PC antigen; this antigen was not restricted to morphotypes resembling only cocci but was also present on rods and branched filamentous organisms. We found that S. mitis, S. oralis, and S. sanguis, as well as oral actinomycetes, including A. viscosus, A. odontolyticus, and A. israelii, incorporated substantial amounts of [3H]choline from culture media. Further analysis of antigens derived from these organisms by Western blot indicated that S. oralis, S. sanguis, A. viscosus, A. odontolyticus, and A. israelii contained TEPC-15-reactive antigens. The data show that many commonly occurring bacterial species found in dental plaque contain PC antigen and that immunization with plaque-derived PC antigens as a consequence of inflammation and periodontal attachment loss may influence systemic anti-PC antibody concentrations.
Previous studies have shown that nearly all human sera contain antibody reactive with phosphorylcholine (PC) and that the response of normal humans to PC is overwhelmingly an immunoglobulin G2 (IgG2) subclass response with more than 80% of all immunoglobulins being IgG2 (19). PC is the immunodominant determinant of the C carbohydrate of Streptococcus pneumoniae, and most of the antibody produced against PC is thought to be induced by this species. The PC determinant in S. pneumoniae is known to be linked to the cell wall polysaccharides and to the lipoteichoic acid (3, 13).
There is little information in the literature on PC antigen in the oral cavity. PC has been identified on Streptococcus mitis (5, 8) and is cross-reactive with PC antigens on S. pneumoniae. Further, a C polysaccharide antigen was identified on Streptococcus oralis by Gillespie et al. (5), but it was not observed on other species, including S. sobrinus, S. salivarius, S. vestibularis, S. sanguis, S. parasanguis, S. gordonii, or S. crista. Additionally, PC is a common antigen on strains of Haemophilus influenzae (4, 8); PC from growth media is incorporated into the lipopolysaccharide (LPS) of this species (26). A study just published by Gmur et al. (6) reported that PC was a relatively common cross-reactive antigen present on a number of oral bacteria species, including a number of actinomycetes, streptococci, and some strains of Actinobacillus actinomycetemcomitans and Fusobacterium nucleatum. However, these authors reported that they found no particular association of PC expression with oral health or inflammatory periodontal disease. In summary, PC has been shown to be present on some commonly occurring gram-positive and gram-negative bacteria found in the oral cavity.
Our interest in bacterial PC stems from a series of studies in which we observed that IgG2 responses in humans appear to be influenced by genetic factors, periodontal clinical status, and other environmental factors such as smoking. We have examined the influence of such factors on serum IgG2 levels and specific IgG2 antibody responses relevant to periodontal disease pathology. We have shown by genetic segregation analysis that serum IgG2 levels are under genetic control by a gene exhibiting codominant expression (11). Additionally, our previous studies on IgG2 subclass responses in periodontitis subjects have demonstrated that concentrations of IgG2 in serum are elevated in certain patient groups, including patients with localized juvenile periodontitis (LJP) (10) and generalized early-onset periodontitis (G-EOP) who are nonsmokers (17). Furthermore, LJP patients and nonsmoking G-EOP patients produce elevated IgG2 responses to the serotype-specific carbohydrates of A. actinomycetemcomitans LPS (22). We have further observed that smokers with G-EOP have significantly lower concentrations of both serum IgG2 and specific IgG2 antibody reactive with A. actinomycetemcomitans.
These observations led us to hypothesize that factors that influenced IgG2 responses to A. actinomycetemcomitans and serum concentrations of IgG2 might also affect other common IgG2 responses, such as that against nonoral antigens such as PC and H. influenzae carbohydrate antigens. To our surprise, we found that anti-PC was lower in health than in EOP (unpublished results). This prompted the hypothesis that periodontal organisms must bear PC and that anti-PC must be associated with a variety of PDs. We also examined the IgG2 anti-PC response in a wide range of periodontally characterized patients and found that subjects in diagnostic groups characterized by attachment loss (AL) (patients with either periodontitis or gingival recession) demonstrated significantly higher anti-PC responses than did subjects without AL. Furthermore, analysis of plaque samples indicated that a large percentage of bacteria in both supragingival and subgingival plaque react with a monoclonal anti-PC antibody and that several common plaque bacteria incorporate choline from growth media. Thus, the oral flora may contribute significantly to serum IgG2 antibody reactive with PC.
MATERIALS AND METHODS
Clinical methods.
Each subject received a complete periodontal evaluation that included assessments of pocket depth, AL, plaque index (20), gingival index (9), bleeding upon probing (14), and suppuration (21). Measurements were performed at four sites per tooth (mesiobuccal, midbuccal, distobuccal, and midlingual). At the time of the examination, a blood sample was taken and processed for serum, which was then stored at −70°C until utilized.
Both individually ascertained volunteers and subjects participating in a study of families with early-onset periodontitis were included in this study. As previously published (18), the subjects were categorized by diagnostic group as follows.
(i) Healthy periodontium (HP).
This group included subjects of any age with no evidence of AL at more than one site or with pockets greater than 3 mm, i.e., who have no detectable periodontitis.
(ii) Gingival recession (GR).
This group included subjects of any age with no evidence of interproximal AL at more than one site or with pockets greater than 3 mm, but who had facial or lingual sites of AL of ≥2 mm.
(iii) Adult periodontitis (AP).
This group included subjects 25 years of age or older with AL of 2 mm or greater in any extent or severity pattern on more than one tooth. In subjects less than 35 years old the AL must appear to have been consistent with debris level and age, be less severe than in LJP or G-EOP, or have had an indication of adult onset. Further, the distribution (extent) of the disease was such as to not suggest localization to first molars and incisors nor be related to teeth affected by trauma, endodontic disorders, or other determinable local etiology other than periodontitis.
(iv) LJP.
This group included subjects with disease of onset from puberty up to age 30 with at least a 4-mm AL on at least two permanent first molars and incisors (at least one molar must have been affected) and no more than two teeth which were not first molars or incisors that were affected by a 5-mm AL or greater.
(v) G-EOP.
Subjects in this group had disease onset at up to age 35 with at least eight teeth affected (a 5-mm AL or more), at least three of which were not first molars and incisors.
Enzyme-linked immunosorbent assay (ELISA) for anti-PC IgG2.
Measurement of serum anti-PC concentrations was carried out as we previously described (22) by using a modification of the method of Scott et al. (19). Briefly, microtiter plates were coated with PC-bovine serum albumin overnight and, after a thorough washing, the plates were incubated with 1% bovine serum albumin to block nonspecific binding. Next, 100 μl of eight twofold dilutions of test serum or standard serum per well were added in duplicate to each plate, such that the final serum concentration for each sample varied from 1/250 to 1/32,000 ml. After overnight incubation at 4°C and a washing, 100 μl of mouse anti-human monoclonal IgG2 (Clone HP-6002; Sigma Chemical Co.) was added to each well for 2 h at room temperature. Next, 100 μl of horseradish peroxidase-conjugated goat anti-mouse IgG was added to each well for 1 h. Finally, 100 μl of peroxidase substrate was added to each well, and the optical density was measured at 450 nm in a microplate reader. To calculate the amount of IgG2 anti-PC antibody in serum samples, we applied heterologous interpolation by using chimeric antibody as described by Wilson and Hamilton (27). First, plots of the optical density versus the amounts of antibody in both the chimeric antibody and a standard serum with a high anti-PC titer were developed, thus establishing the relative concentration of IgG2 antibody in the serum standard. This calibrated serum standard was thereafter utilized in each assay to determine the specific antibody reactive with the PC-BSA conjugate in the patient serum samples.
Immunofluorescence assay.
Supragingival and subgingival plaque specimens were collected with Morse OO scalers and placed in phosphate-buffered saline (PBS). The samples were sonicated for 10 to 20 s in 500 μl of sterilized PBS to disperse the bacteria. Then, 20-μl specimens were dropped onto poly-l-lysine-coated slides and air dried. Mouse anti-PC monoclonal antibody TEPC-15, (M1421; Sigma), at a dilution of 1:30 in PBS, was added to the slides and incubated at 4°C overnight. The specificity was assured by two methods. We utilized MOPC-315 antibody as an isotype control (Sigma, St. Louis, Mo.), and further demonstrated that reactivity of TEPC-15 with bacteria was completely inhibited with free PC-chloride (400 μg/ml). Biotin-conjugated rat anti-mouse IgA monoclonal antibody (02102D; Pharmingen, San Diego, Calif.) was added at a 1:10 dilution for 2 h in PBS after the slides were washed three times for 5 min in PBS. Streptavidin-fluorescein isothiocyanate (13024D; Pharmingen) was added at a 1:20 dilution and incubated at room temperature for 1 h. After three rinses, slides were mounted by using Moviol. Slides were observed by using a light microscope (Olympus BH-2) equipped with Nomarski optics and fluorescence. For each specimen, about 150 bacteria were counted in five randomly chosen microscopic fields. Bacteria were first enumerated by using the Nomarski mode at ×400 magnification, and then PC-positive bacteria were identified in the fluorescence mode. The specificity of the assay for PC was established by using isotype control antibodies (mouse IgA, M2046 [Sigma] and mouse IgA 03101 [Pharmingen]) which failed to bind oral bacteria. Binding of TEPC-15 to oral bacteria was specifically blocked by using PC as an inhibitor at a 100 μM concentration.
[3H]choline uptake.
For semiquantitative determination of relative uptake of choline from culture media, bacterial cultures were grown to log phase in brain heart infusion medium (Difco Laboratories, Detroit, Mich.) containing 1.5 μCi of [3H]choline (3H Choline Chloride; New England Nuclear Life Science Products, Boston, Mass.) per ml. Cultures were washed three times with PBS and resuspended in the same buffer to an optical density of 1.0 at 650 nm. After addition of 5 ml of scintillation cocktail (3270B; Research Products International Corp., Mount Prospect, Ill.) to 1 ml of washed bacterial suspension, the samples were subjected to scintillation counting. Data are reported as mean counts per minute for two experiments.
Western blot analysis.
Samples for Western blot analysis were prepared as follows. For the streptococcal strains, samples were prepared as described by Kolberg et al. (8). Briefly, cells from late-log-phase cultures were washed in PBS and resuspended in 1 to 2 ml of water containing 6% (by volume) 2-mercaptoethanol and placed in a boiling water bath for 5 min. Eluates were collected after centrifugation. For strains of actinomycetes, cells from late-log-phase cultures were washed and resuspended in a minimal volume of PBS containing 6% sodium dodecyl sulfate (SDS) and placed in a boiling water bath for 5 min. Antigens prepared in this manner were first separated by SDS-polyacrylamide gel electrophoresis in 15% separation gels and then transferred to 0.2-μm-pore-size nitrocellulose membranes. Gels were reacted with TEPC-15 (anti-PC) or MOPC-315 (isotype control) (Sigma) diluted to 1:1,000 for 60 min. The specificity of the TEPC-15 was assessed by prior absorption of 100 μl of a 1:10 dilution with 1 ml of 350 mM p-aminophenyl-PC for 2 h at 37°C and then overnight at 4°C. The secondary antibody, human serum-absorbed goat anti-mouse IgA (KPL, Gaithersburg, Md.) labeled with peroxidase was applied to membranes for 60 min. The membrane was then incubated in Western Blot Chemiluminescence Reagent Plus (NEN, Boston, Mass.) according to the manufacturer’s instructions. The membrane was exposed to Fuji Medical S-ray film for 5 to 30 s and developed by using a Kodak M35A X-Omat Processor. As in the immunofluorescence assays, the specificity of reactivity in the Western blots was assured both by utilization of MOPC-315 as an isotype control and by demonstrating inhibition of the binding of TEPC-15 to bacterial antigens by using PC-chloride.
Statistical methods.
The analyses of anti-PC IgG2 levels and of the percentage of plaque bacteria reactive with anti-PC antibody was performed by using analysis of variance (ANOVA) (at alpha = 0.05). The subgroup sample sizes and residual analysis supported the use of parametric methods. In addition to diagnostic category, clinical indices were also included in analyses (gingival index, plaque index, pocket depth, AL, and supra-versus subgingival).
RESULTS
Serum concentrations of anti-PC IgG2 in periodontally characterized subjects.
Serum IgG2 anti-PC levels were determined in 71 nonperiodontitis controls (NP), 44 LJP patients, 100 G-EOP patients, 134 AP patients, and 30 adults with facial and lingual gingival recession and no more than one interproximal site with ≥2-mm AL (GR). As shown in Table 1, NP patients had significantly lower serum concentrations of IgG2 anti-PC IgG2 than did any subject group that demonstrated AL. However, there were no differences in anti-PC levels between subject groups with AL.
TABLE 1.
Anti-PC IgG2 levels in periodontally characterized subject populations
| Diagnostic category | n | Anti-PC IgG2 (μg/ml, SE) | Pa |
|---|---|---|---|
| NP | 71 | 5.92 ± 0.6 | |
| JP | 44 | 8.91 ± 1.0 | <0.03 |
| G-EOP | 100 | 9.59 ± 0.8 | <0.01 |
| AP | 134 | 8.94 ± 0.6 | <0.02 |
| GR | 30 | 9.70 ± 1.5 | <0.02 |
P value compared to NP subjects.
PC antigen in plaque.
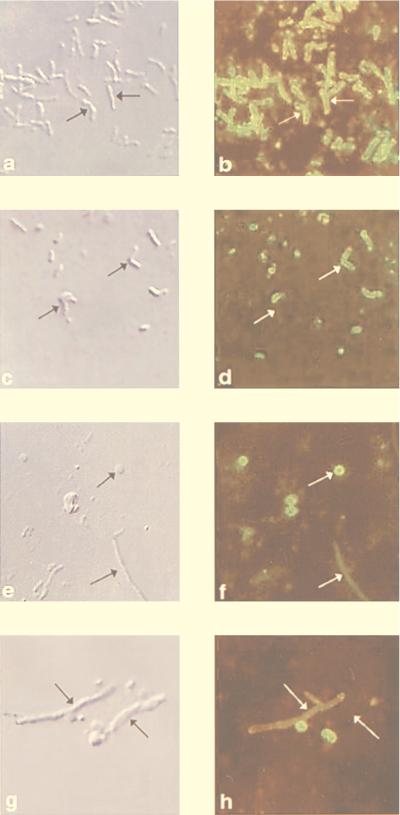
All subject groups with AL, including those with gingival recession, had significantly higher levels of anti-PC than those with no AL. This led us to hypothesize that the source of immunogen for anti-PC could be plaque bacteria. Supragingival and subgingival plaque samples were collected from patients with LJP, G-EOP, AP, and from healthy controls (NP). Smears of these samples were prepared and analyzed by immunofluorescence microscopy for TEPC-15 (anti-PC)-reactive bacteria. Figure 1 shows typical examples of plaque samples stained with TEPC-15 antibody. Figure 1a and b demonstrate the appearance of a pure culture of A. viscosus 15987, a strain strongly reactive with TEPC-15, as visualized with Nomarski optics (Fig. 1a) and by immunofluorescence (Fig. 1b). Figure 1c and d represents a supragingival plaque sample from a periodontally healthy (NP) subject; the arrows in Fig. 1c demonstrate bacteria with similar morphotypes with different reactivity with TEPC-15 (Fig. 1d). Figure 1c to h show analyses of supragingival samples from a patient with G-EOP. The arrows in Fig. 1e and f emphasize the appearance of morphotypes resembling both cocci and long branched rods resembling actinomycetes that react with TEPC-15. Figure 1g and h demonstrate that actinomycete-like organisms did not always react with TEPC-15. Thus, it can be seen that many bacterial morphotypes react with this antibody, including rods, cocci, and branching filamentous organisms resembling actinomycetes.
FIG. 1.
Analyses of reactivity of A. viscosus (a and b) and supragingival plaque samples from a periodontally healthy subject (c and d) and from a patient with G-EOP (e to h) by light microscopy by using Nomarski optics (a, c, e, and g) and indirect immunofluorescence microscopy (b, d, f, and h) after reaction with TEPC-15 antibody.
As shown in Table 2, samples from all disease categories contained significant levels of TEPC-15-positive bacteria. High levels of such bacteria were found in both subgingival (mean, 34.6%; range, 2.3 to 89.7%) and supragingival (mean, 34.6%; range, 4.0 to 70.3%) plaque. No differences in mean percentage of PC-positive bacteria were found between disease categories (P < 0.0748). Within subject groups, sites with or without AL displayed similar levels, as did sites with or without gingival inflammation.
TABLE 2.
Percentage of plaque bacteria reactive with anti-PC antibody (TEPC-15)a
| Diagnostic category | % Reactive subgingival plaque bacteria
|
% Reactive supragingival plaque bacteria
|
||
|---|---|---|---|---|
| n | Mean ± SD (range) | n | Mean ± SD (range) | |
| AP | 23 | 37.9 ± 13.8 (14.9–75) | 28 | 35.6 ± 10.4 (17.8–56) |
| LJP | 38 | 33.0 ± 15.8 (8.3–84.2) | 36 | 29.6 ± 14.2 (4–68) |
| NP | 29 | 31.2 ± 17.2 (2.3–76.9) | 33 | 36.8 ± 15.5 (5.8–70.3) |
| G-EOP | 23 | 38.5 ± 19.4 (12.5–89.7) | 24 | 38.1 ± 15.7 (16–67.8) |
All groups were statistically indistinguishable by ANOVA.
Reactivity of TEPC-15 with purified bacterial cultures.
Indirect immunofluorescence assays were performed to demonstrate PC on bacteria surfaces. Strains of S. pneumoniae, A. viscosus (Fig. 1), A. odontolyticus, A. israelii, S. sanguis, S. mitis, and S. oralis were examined and found to be reactive. L. casei and A. naeslundii failed to react with TEPC-15 in this assay.
[3H]choline uptake by common plaque bacteria.
Since reactivity with TEPC-15 demonstrated that it is likely that many oral microbes may contain PC, we selected a group of commonly encountered plaque bacteria for further analysis. Since a characteristic of PC-bearing bacteria is the ability to incorporate choline from the surrounding media into teichoic acids and LPS, we grew cultures of oral bacteria in medium containing [3H]choline to illustrate relative levels of choline utilization by common oral isolates. Table 3 demonstrates the mean number of counts of choline incorporated into the tested strains in two experiments. Strains of P. gingivalis, A. actinomycetemcomitans, F. nucleatum, and L. casei incorporated only background levels of choline (<1,200 cpm). In contrast, strains of F. nucleatum subsp. nucleatum and A. naeslundii incorporated larger amounts of choline, while S. mitis incorporated more than 20,000 cpm. Finally, S. oralis, S. sanguis, A. israelii, A. odontolyticus, A. viscosus, and S. pneumoniae all incorporated relatively large amounts of [3H]choline (>200,000 cpm). These data, in concert with the high levels of reactivity of bacteria in plaque samples with TEPC-15, argue that a significant proportion of the oral microflora may bear the PC epitope.
TABLE 3.
Uptake of [3H]choline by common oral bacteria
| Bacterial strain | Mean 3H cpm |
|---|---|
| A. actinomycetemcomitans serotype a (SUNY Buffalo 122) | 350 |
| A. actinomycetemcomitans serotype b (SUNY Buffalo 366) | 400 |
| A. actinomycetemcomitans serotype c (SUNY Buffalo 360) | 25 |
| A. israelii VPI D012B-11 | 1,698,135 |
| A. naeslundii (serovar 1) 49340 | 9,164 |
| A. naeslundii (A. viscosus) 15987 | 210,040 |
| A. odontolyticus 29323 | 269,160 |
| F. nucleatum subsp. nucleatum VPI D018B-11 | 4,020 |
| F. nucleatum subsp. polymorphum VPI D049-15B | 1,200 |
| F. nucleatum subsp. vincentii VPI D015B-12A | 510 |
| L. casei 4646 | 954 |
| P. gingivalis W83 | 198 |
| S. mitis 903 | 25,408 |
| S. oralis 35037 | 248,421 |
| S. pneumoniae 39937 | 262,289 |
| S. sanguis 49295 | 307,182 |
Demonstration of anti-PC-reactive antigens in streptococci and actinomycetes.
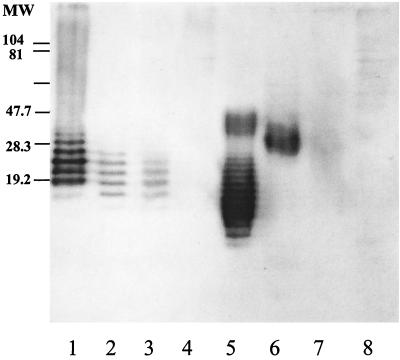
Since several strains of oral streptococci and actinomycetes incorporate choline from culture media, it was of interest to assess whether these organisms express an antigen reactive with TEPC-15. Antigens were eluted from whole cells with either 2-mercaptoethanol (streptococci) or SDS (actinomycetes). As shown in Fig. 2, S. oralis and S. sanguis contained TEPC-15-reactive antigens displaying reactivity patterns similar to that for S. pneumoniae. A. israelii and A. odontolyticus likewise contained anti-PC-reactive antigens. A. viscosus always demonstrated weak reactivity with TEPC-15, while A. naeslundii was consistently negative.
FIG. 2.
Western blot analysis of TEPC-15-reactive antigens of S. pneumoniae (lane 1), S. oralis (lane 2), S. sanguis (lane 3), S. mitis (lane 4), A. israelii (lane 5), A. odontolyticus (lane 6), A. viscosus (lane 7), and A. naeslundii (lane 8).
DISCUSSION
Nearly all human sera contain substantial levels of antibody reactive with PC (5 to 10 μg/ml), and the majority of the IgG anti-PC antibody is of the IgG2 subclass (19). It is thought that most of this antibody is induced by colonization or infection with S. pneumoniae, a gram-positive bacterium that is a major etiologic agent in pneumonia, sepsis, and meningitis (24). Our data indicate that serum levels of IgG2 anti-PC are significantly lower in individuals who have not experienced periodontal AL than in those who have periodontitis or gingival recession. Interestingly, the data indicate that anti-PC levels are similar in all diagnostic groups demonstrating AL and that large numbers of PC-bearing organisms are present in both subgingival and supragingival plaque. These findings may indicate that gingival inflammation in concert with pathological processes that lead to disruption of the attachment apparatus may provide sufficient conditions for exposure of the immune system to PC-bearing oral microorganisms from the supragingival and subgingival plaque. The data indicate that it is possible that such exposure contributes significantly to generation of serum anti-PC and could help explain the serological cross-reactivity among diverse groups of organisms.
The anti-PC response is one of the most thoroughly studied human antibody responses in mice and humans. Nevertheless, the function of human anti-PC is unclear. For example, whether or not anti-PC antibody is protective is as yet unknown. Some existing data indicate that levels of serum anti-PC antibody are associated with susceptibility to fatal pneumonia (16). In elderly patient cohorts, elevated levels of anti-PC may be predictors of such susceptibility. The difficulty in assessing the protective function of anti-PC in pneumococcal infections likely stems from the fact that virulent strains of S. pneumoniae are heavily encapsulated. Human anti-PC antibody has not been previously examined in the context of its relevance to pathology in the periodontal tissues.
Although PC antigen has been previously identified on S. mitis and S. oralis, we have observed that strains of S. sanguis can also contain PC. It is possible that there is strain specificity in this regard, thus explaining the differences between our results and that of Gillespie et al. (5). A second unique observation is that three species of oral actinomycetes (A. viscosus, A. israelii, and A. odontolyticus) incorporate substantial amounts of choline from the culture medium; these actinomycetes also display TEPC-15-reactive antigens on Western blots. As shown in Fig. 1f and h, we commonly observed that branching filamentous organisms in plaque samples reacted with anti-PC, leading us to suspect that actinomycetes could be a significant source of PC in dental plaque. This was borne out by our observations that all three species incorporated radiolabeled choline to various extents and that all three also contained antigens reactive with TEPC-15. Thus, a quantitatively major component of plaque, represented by streptococci and actinomycetes, contains PC.
Gmur et al. (6) recently demonstrated that isolates of a number of species of oral bacteria display PC-containing antigens. Notable is their observation that a number of actinomycetes and streptococci contain this antigen. In contrast to the data presented here, they observed that some strains of A. actinomycetemcomitans and F. nucleatum also are positive. These data are not entirely inconsistent with ours for a number of reasons. Since our purpose was not to catalogue strains with cross-reactivity attributable to PC but rather to explain elevated anti-PC levels in serum by demonstrating that common isolates can bear PC, we tested only a small number of isolates. In addition, we have noticed that some isolates initially appearing to bear PC antigen lose reactivity with TEPC-15 during culture or after subculture, indicating that in some bacteria this property may be regulated. Gmur et al. (8) have noted that strains of S. sanguis do not appear to bear PC antigen. We have noted, however, that fresh clinical isolates of this organism, as well as the strain noted in here, clearly display reactivity with TEPC-15. The data of Gmur et al. strengthen our interpretation that anti-PC levels in sera from patients with periodontal AL are likely induced by oral bacteria.
Most of the bacteria shown to incorporate choline are very common oral isolates. For example, actinomycetes are bacteria very commonly isolated from plaque (12). In addition, the oral streptococci, some of which are closely related to S. pneumoniae, have been shown to bear PC and are also common in plaque (4, 8). S. mitis, in particular, is known to bear PC. Our data demonstrate that a large percentage of both subgingival and supragingival plaque bacteria react with anti-PC antibody. We were intrigued to learn that both subgingival and supragingival plaque samples contained considerable concentrations of such bacteria. Our observations that actinomycetes and oral streptococci can incorporate choline and the fact that these species can account for a substantial proportion of the cultivable flora (12) provide a likely explanation for the finding of high levels of anti-PC in subgingival plaque. The observation by Gmur et al. that about one-third of F. nucleatum strains also bear PC further substantiates this. It is not surprising, therefore, that oral bacteria may make a significant contribution to the total serum anti-PC concentration. It is further likely from results of the immunofluorescence assays that many other bacterial species in both subgingival and supragingival plaque bear the PC epitope and could contribute to the anti-PC response in patients with periodontal AL.
Our data indicate that commonly isolated strains of oral streptococci which are associated with bacteremias and that are commonly retrieved from subacute endocarditis lesions can carry PC (7, 25). We have observed that a significant proportion of the PC-positive flora has a morphological appearance similar to that of streptococci and actinomycetes, though other morphotypes are also present in this population. It has recently been demonstrated that virulent strains of S. pneumoniae, by mimicry of platelet-activating factor (PAF) via its cell-surface PC moiety, enters inflammatory endothelial cells by way of the upregulated PAF receptor. Additionally, bacteremia and sepsis due to S. pneumoniae in an experimental animal model is inhibited by PAF receptor antagonists. Furthermore, cells transfected with the PAF receptor have been shown to gain the ability to promote adherence and entrance of S. pneumoniae intracellularly (1). These observations, plus additional findings demonstrating that S. pneumoniae adheres to epithelial cells via cell surface carbohydrates (2), have led to the hypothesis that S. pneumoniae-related pneumonia and sepsis result from a combination of lectin-like reactions mediating epithelial cell binding plus inflammatory mediator-produced upregulation of PAF receptors that are acceptor sites for the bacteria (23). Since oral streptococcal species that are closely related to S. pneumoniae also bear PC, it is tempting to hypothesize that these organisms could also gain access to the circulation via mimicry of PAF. Additionally, actinomycetes and fusobacteria that coaggregate with many other oral bacteria species could also mediate entry of such coaggregating species into the circulation via this mechanism. This possibility is being actively pursued in our laboratory.
ACKNOWLEDGMENTS
This work was supported by Public Health Service grant DE-10703 from the National Institute of Dental and Craniofacial Research.
We thank C. R. Berry and J.-B. Zhang for their excellent technical assistance and Kimberly Lake for management of the human subjects who participated in this study.
REFERENCES
- 1.Cundell D R, Gerard N P, Gerard C, Idanpaan-Heikkila I, Tuomanen E I. Streptococcus pneumoniae anchor to activated human cells by the receptor for platelet-activating factor. Nature. 1995;377:435–438. doi: 10.1038/377435a0. [DOI] [PubMed] [Google Scholar]
- 2.Cundell D R, Tuomanen E I. Receptor specificity of adherence of Streptococcus pneumoniae to human type-II pneumocytes and vascular endothelial cells in vitro. Microb Pathog. 1994;17:361–374. doi: 10.1006/mpat.1994.1082. [DOI] [PubMed] [Google Scholar]
- 3.Fischer W, Behr T, Hartmann R, Peter-Katalinic J, Egge H. Teichoic acid and lipoteichoic acid of Streptococcus pneumoniae possess identical chain structures. A reinvestigation of teichoid acid (C polysaccharide) Eur J Biochem. 1993;215:851–857. doi: 10.1111/j.1432-1033.1993.tb18102.x. [DOI] [PubMed] [Google Scholar]
- 4.Gillespie S H, Ainscough S, Dickens A, Lewin J. Phosphorylcholine-containing antigens in bacteria from the mouth and respiratory tract. J Med Microbiol. 1996;44:35–40. doi: 10.1099/00222615-44-1-35. [DOI] [PubMed] [Google Scholar]
- 5.Gillespie S H, McWhinney P H M, Patel S, Raynes J G, McAdam K P W J, Whiley R A, Hardie J M. Species of alpha-hemolytic streptococci possessing a C-polysaccharide phosphorylcholine-containing antigen. Infect Immun. 1993;61:3076–3077. doi: 10.1128/iai.61.7.3076-3077.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gmur R, Thurnheer T, Guggenheim B. Dominant cross-reactive antibodies generated during the response to a variety of oral bacterial species detect phosphorylcholine. J Dent Res. 1999;78:77–85. doi: 10.1177/00220345990780011201. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs J A, Schouten H C, Stobberingh E E, Soeters P B. Viridans streptococci isolated from the bloodstream. Relevance of species identification. Diagn Microbiol Infect Dis. 1995;22:267–273. doi: 10.1016/0732-8893(95)00137-y. [DOI] [PubMed] [Google Scholar]
- 8.Kolberg J, Háiby E A, Jantzen E. Detection of the phosphorylcholine epitope in streptococci, Haemophilus and pathogenic neisseriae by immunoblotting. Microb Pathog. 1997;22:321–329. doi: 10.1006/mpat.1996.0114. [DOI] [PubMed] [Google Scholar]
- 9.Löe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 10.Lu H, Wang M, Gunsolley J C, Schenkein H A, Tew J G. Serum immunoglobulin G subclass concentrations in periodontally healthy and diseased individuals. Infect Immun. 1994;62:1677–1682. doi: 10.1128/iai.62.5.1677-1682.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marazita M L, Lu H, Cooper M E, Quinn S M, Zhang J, Burmeister J A, Califano J V, Pandey J P, Schenkein H A, Tew J G. Genetic segregation analyses of serum IgG2 levels. Am J Hum Genet. 1996;58:1042–1049. [PMC free article] [PubMed] [Google Scholar]
- 12.Moore W E C, Moore L V H. The bacteria of periodontal diseases. Periodontology 2000. 1994;5:66–77. doi: 10.1111/j.1600-0757.1994.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 13.Mosser J L, Tomasz A. Choline-containing teichoic acid as a structural component of pneumococcal cell wall and its role in sensitivity to lysis by an autolytic enzyme. J Biol Chem. 1970;245:287–298. [PubMed] [Google Scholar]
- 14.Muhlemann H R, Son S. Gingival sulcus bleeding: a leading symptom in initial gingivitis. Helv Odontol Acta. 1971;15:105. [PubMed] [Google Scholar]
- 15.Musher D M, Chapman A J, Goree A, Jonsson S, Briles D, Baughn R E. Natural and vaccine-related immunity to Streptococcus pneumoniae. J Infect Dis. 1986;154:245–256. doi: 10.1093/infdis/154.2.245. [DOI] [PubMed] [Google Scholar]
- 16.Nordenstam G, Andersson B, Briles D, Brooks J W, Jr, Odèn A, Svanborg A, Edèn C S. High anti-phosphorylcholine antibody levels and mortality associated with pneumonia. Scand J Infect Dis. 1990;22:187–195. doi: 10.3109/00365549009037901. [DOI] [PubMed] [Google Scholar]
- 17.Quinn S M, Zhang J B, Gunsolley J C, Schenkein J G, Schenkein H A, Tew J G. Influence of smoking and race on immunoglobulin G subclass concentrations in early-onset periodontitis patients. Infect Immun. 1996;64:2500–2505. doi: 10.1128/iai.64.7.2500-2505.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schenkein H A, Gunsolley J C, Koertge T E, Schenkein J G, Tew J G. Smoking and its effects on early-onset periodontitis. J Am Dent Assoc. 1995;126:1107–1113. doi: 10.14219/jada.archive.1995.0327. [DOI] [PubMed] [Google Scholar]
- 19.Scott M G, Briles D E, Shackelford P G, Smith D S, Nahm M H. Human antibodies to phosphocholine. IgG anti-PC antibodies express restricted numbers of V and C regions. J Immunol. 1987;138:3325–3331. [PubMed] [Google Scholar]
- 20.Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 21.Singh S, Cianciola L, Genco R J. The suppurative index: an indicator of active periodontal disease, abstr. 593. J Dent Res. 1977;56:B200. [Google Scholar]
- 22.Tangada S D, Califano J V, Nakashima K, Quinn S M, Zhang J B, Gunsolley J C, Schenkein H A, Tew J G. The effect of smoking on serum IgG2 reactive with Actinobacillus actinomycetemcomitans in early-onset periodontitis patients. J Periodontol. 1997;68:842–850. doi: 10.1902/jop.1997.68.9.842. [DOI] [PubMed] [Google Scholar]
- 23.Tuomanen E I. Molecular and cellular mechanisms of pneumococcal meningitis. Ann N Y Acad Sci. 1996;797:42–52. doi: 10.1111/j.1749-6632.1996.tb52948.x. [DOI] [PubMed] [Google Scholar]
- 24.Tuomanen E I, Austrian R, Masure H R. Pathogenesis of pneumococcal infection. N Engl J Med. 1995;332:1280–1284. doi: 10.1056/NEJM199505113321907. [DOI] [PubMed] [Google Scholar]
- 25.Watanakunakorn C, Pantelakis J. Alpha-hemolytic streptococcal bacteremia: a review of 203 episodes during 1980–1991. Scand J Infect Dis. 1993;25:403–408. doi: 10.3109/00365549309008519. [DOI] [PubMed] [Google Scholar]
- 26.Weiser J N, Shchepetov M, Chong S T. Decoration of lipopolysaccharide with phosphorylcholine: a phase-variable characteristic of Haemophilus influenzae. Infect Immun. 1997;65:943–950. doi: 10.1128/iai.65.3.943-950.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wilson M E, Hamilton R G. Immunoglobulin G subclass response of localized juvenile periodontitis patients to Actinobacillus actinomycetemcomitans Y4 lipopolysaccharide. Infect Immun. 1992;60:1806–1812. doi: 10.1128/iai.60.5.1806-1812.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]