Abstract
A pericardial lipoma is a rare benign cardiac tumor, and fat necrosis is an uncommon clinical condition. This is the first reported case of pericardial lipoma with fat necrosis, which showed clinical presentations of a malignant tumor despite imaging findings consistent with benign lipoma. (Level of Difficulty: Advanced.)
Key Words: fat necrosis, hemorrhagic pericardial effusion, pericardial lipoma
Abbreviations and Acronyms: CMR, cardiac magnetic resonance; CT, computed tomography
Graphical abstract
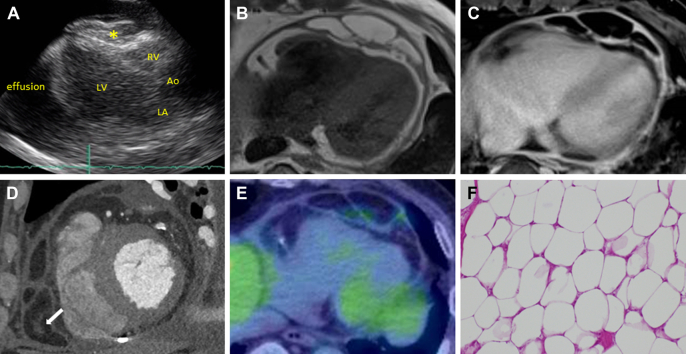
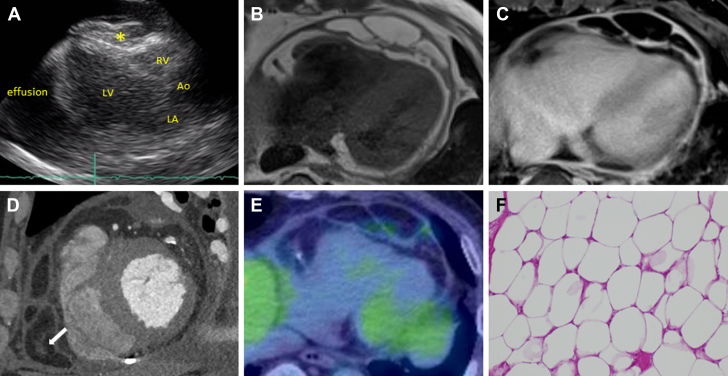
A 61-year-old Japanese man presented to the emergency department with dyspnea on exertion and facial edema. His blood pressure was 146/80 mm Hg, and heart rate was 86 beats/min. The rales in the lung field were not audible. An electrocardiogram showed low voltage on the limb lead. Chest radiography revealed cardiomegaly with pleural effusion. Transthoracic echocardiography revealed a large pericardial effusion, a mass in the pericardial cavity, and right atrial and right ventricular collapse (Figure 1A). There were signs of echocardiographic tamponade; therefore, an emergency percutaneous pericardial drainage was performed. Hemorrhagic pericardial effusion (1,335 mL) was drained. The cytopathological diagnosis of pericardial effusion was classified as Class III. A bacterial culture test was negative. Subsequently, cardiovascular cardiac magnetic resonance (CMR) was performed, which showed a multilobulated and well-defined mass in the pericardial cavity. The mass showed high intensity on T1-weighted image (Figure 1B), low intensity and no enhancement on T1 fat-suppression image with gadolinium administration (Figure 1C). A contrast-enhanced computed tomography (CT) image showed an area of fat with central soft-tissue attenuation (Figure 1D). There was negative 18F-fluorodeoxyglucose uptake on positron emission tomography in the mass (Figure 1E). The tumors were completely resected. Macroscopic inspection revealed a multilobulated fatty mass with a maximum length of 9.5 cm. Histological examination showed that the mass contained fat tissue with necrotic and degenerative changes and confirmed the diagnosis of pericardial lipoma with fat necrosis (Figure 1F). The patient’s postoperative course was uneventful. At the 4-month follow-up, the recurrence of tumor was not observed.
Figure 1.
Imaging and Histological Finding
(A) Echocardiography showed pericardial mass (asterisk) and effusion. (B) T1-weighted cardiac magnetic resonance. (C) T1 fat-suppression cardiac magnetic resonance with gadolinium administration. (D) Contrast-enhanced computed tomography image: There was central soft-tissue attenuation (arrow). (E)18F-fluorodeoxyglucose positron emission tomography computed tomography. (F) Microscopic finding of the mass (high-power field, ×200, hematoxylin and eosin staining). The mass contained necrotic adipocytes that were devoid of nuclei. Ao = aorta; LA = left atrial; LV = left ventricle; RV = right ventricle.
Cardiac lipomas are typically asymptomatic, and pericardial lipomas rarely induce cardiac tamponade.1 In this case, large amounts of hemorrhagic pericardial effusion caused the cardiac tamponade. Hemorrhagic pericardial effusion is a characteristic of malignant tumors; however, CMR and positron emission tomography CT showed evidence of benign pericardial lipoma. An area of fat with central soft-tissue attenuation on CT is one of characteristics of fat necrosis,2 and histological examination confirmed the diagnosis of pericardial lipoma with fat necrosis. Fat necrosis in lipoma is very rare. A case of vulvar lipoma with fat necrosis has been reported,3 and no cases of fat necrosis in pericardial lipoma have been described. CMR should be a reliable modality depending on the characteristics of the mass; however, the reliability of CMR for detecting and differentiating fat necrosis has been challenged. Fat necrosis in a lipoma can change the clinical presentation; therefore, if there is an apparent discordance between clinical presentation and imaging findings, lipoma with fat necrosis should be considered and confirmed by histology.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Restrepo C.S., Vargas D., Ocazionez D., Martínez-Jiménez S., Betancourt Cuellar S.L., Gutierrez F.R. Primary pericardial tumors. Radiographics. 2013;33:1613–1630. doi: 10.1148/rg.336135512. [DOI] [PubMed] [Google Scholar]
- 2.Kamaya A., Federle M.P., Desser T.S. Imaging manifestations of abdominal fat necrosis and its mimics. Radiographics. 2011;31:2021–2034. doi: 10.1148/rg.317115046. [DOI] [PubMed] [Google Scholar]
- 3.Li S., Haag T., McWhorter J., Ge L., Carlan S.J. Unilateral giant vulvar lipoma with fat necrosis not visualized on magnetic resonance imaging (MRI) Am J Case Rep. 2019;20:1760–1764. doi: 10.12659/AJCR.918976. [DOI] [PMC free article] [PubMed] [Google Scholar]