Abstract
Subjects with subclinical respiratory dysfunction who do not meet the chronic obstructive pulmonary disease (COPD) criteria have attracted attention with regard to early COPD intervention. Our aim was to longitudinally investigate the risks for the development of airflow limitation (AFL) and dyspnoea, the main characteristics of COPD, in a large-scale community-based general population study. The Nagahama study included 9789 inhabitants, and a follow-up evaluation was conducted after 5 years. AFL was diagnosed using a fixed ratio (forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) < 0.7). We enrolled normal subjects aged 40–75 years with no AFL, dyspnoea or prior diagnosis of asthma or COPD at baseline. In total, 5865 subjects were analysed, 310 subjects had subclinical respiratory dysfunction (FEV1/FVC < the lower limit of normal; n = 57, and FEV1 < 80% of the predicted value (preserved ratio impaired spirometry); n = 256). A total of 5086 subjects attended the follow-up assessment, and 449 and 1021 subjects developed AFL and dyspnoea, respectively. Of these, 100 subjects developed AFL with dyspnoea. Baseline subclinical respiratory dysfunction was independently and significantly associated with AFL with dyspnoea development within 5 years. Subjects with subclinical respiratory dysfunction are at risk of developing COPD-like features and require careful monitoring.
Subject terms: Medical research, Physiology, Respiration
Introduction
Chronic obstructive pulmonary disease (COPD) is an important cause of morbidity and mortality; however, many COPD cases remain undiagnosed globally1,2. Undiagnosed early COPD and pre-COPD are associated with poor outcomes3–6, therefore, it is necessary to enhance the early identification of COPD3,4. In this context, subjects with subclinical respiratory dysfunction who do not meet the COPD criteria of the Global Initiative for Obstructive Lung Disease (GOLD)7 have attracted attention. Given the age-related decline in lung function, these subjects may require close monitoring for the development of airflow limitation (AFL). Additionally, the development of respiratory symptoms, which are independent features of COPD, is also of great concern. Particularly, dyspnoea is directly connected to inactivity and can cause a cycle of declining health. Dyspnoea also causes early mortality; therefore, special attention should be paid to this condition8,9.
Preserved ratio impaired spirometry (PRISm), characterized by a preserved forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) ratio for proportionate impairments in the FEV1 and FVC, is a type of subclinical respiratory dysfunction. PRISm can be defined as a FEV1 < 80% of the predicted value (%FEV1 < 80%) and FEV1/FVC ≥ 0.76. Ageing, cigarette smoke exposure, increased systemic inflammation and obesity have been reported to be involved in PRISm10. Such patients exhibit aggravated respiratory symptoms, cardiovascular comorbidities and mortality4,11,12. Regarding the development of COPD, patients with PRISm presenting with dyspnoea are at risk of a subsequent diagnosis of COPD13. However, the clinical impact of asymptomatic PRISm is unclear.
Other types of subclinical respiratory dysfunction, such as FEV1/FVC below the lower limit of normal (LLN), defined as the 5th percentile of the predicted value for FEV1/FVC, are also important. As FEV1/FVC commonly exhibits an age-dependent decline14, the definition of AFL based on a fixed ratio of 0.7 could lead to the overestimation of AFL among older subjects and underestimation among younger subjects. Previous studies describing the significance of FEV1/FVC < LLN mainly focused on the potential overdiagnosis of AFL based on the use of a fixed ratio, and in a population-based study, higher rates of morbidity and mortality were observed in subjects with FEV1/FVC < LLN15–18.
We hypothesized that these types of subclinical respiratory dysfunction, including FEV1/FVC < LLN and PRISm, together with smoking status and comorbidities could be risk factors for the development of COPD. The specific goal of this study was to identify the risk factors for the development of AFL; respiratory symptoms, particularly dyspnoea; and both.
Clinically, subjects with AFL and dyspnoea could be diagnosed with COPD; therefore, this investigation may contribute to the early detection of COPD in the general population.
Results
Characteristics of the included subjects
Of the 9804 participants recruited for the Nagahama study, 5865 individuals aged 40–75 years who did not have AFL (FEV1/FVC ≥ 0.7) or dyspnoea (modified Medical Research Council [mMRC] dyspnoea scale = 0) at baseline were included in the current analysis (Fig. 1).
Figure 1.
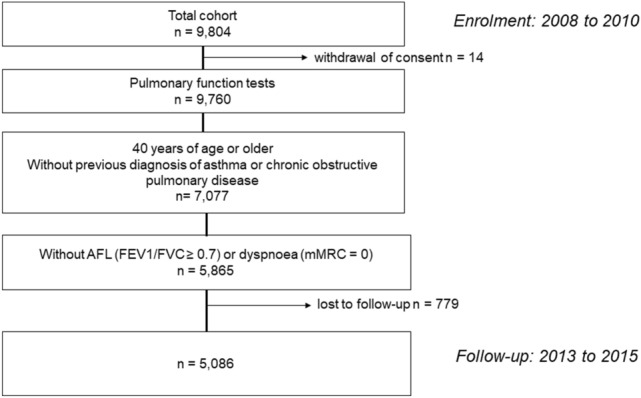
Flowchart of the data extraction process of the Nagahama Study. AFL airflow limitation, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, mMRC modified Medical Research Council (mMRC) dyspnoea scale.
At baseline, 310 subjects had subclinical respiratory dysfunction (based on Japanese predictive equations from the Japanese Respiratory Society (JRS); 57 subjects had FEV1/FVC < LLN and 256 subjects had %FEV1 < 80%) (Table1). Compared with subjects with normal respiratory function (FEV1/FVC ≥ LLN and %FEV1 > 80%), subjects with FEV1/FVC < LLN were younger (mean 49 years vs. 59 years), were predominantly female (81% vs. 67%), and had a lower body mass index (BMI) (21.4 kg/m2 vs. 22.5 kg/m2), whereas subjects with %FEV1 < 80% (PRISm) were older (62 years vs. 59 years), predominantly male (43% vs. 33%), and more likely to have a smoking history (41% vs. 31%).
Table 1.
Characteristics of the subjects without AFL or dyspnoea on exertion at enrolment (N = 5865).
| Total | Normal respiratory function* | Subclinical respiratory dysfunction | ||
|---|---|---|---|---|
| FEV1/FVC < LLN | %FEV1 < 80% | |||
| N | 5865 | 5555 | 57 | 256 |
| Age, year | 59 (± 9) | 59 (± 9) | 49 (± 8)† | 62 (± 9)‡ |
| Female, N (%) | 3887 (66) | 3699 (67) | 46 (81)† | 145 (57)‡ |
| Height, cm | 159 (± 8) | 159 (± 8) | 160 (± 8) | 160 (± 9) |
| Weight, kg | 57 (± 10) | 57 (± 10) | 55 (± 10)† | 59 (± 13) |
| BMI, kg/m2 | 22.5 (± 3.1) | 22.5 (± 3.1) | 21.4 (± 2.6)† | 23.0 (± 3.8) |
| Smoking status, N (%) | 1831 (31) | 1713 (31) | 13 (23) | 105 (41)‡ |
| Current | 668 (11) | 616 (11) | 10 (18) | 42 (16)‡ |
| Former | 1163 (20) | 1097 (20) | 3 (5)† | 63 (25)‡ |
| Pack-years among smokers | 12 (± 20) | 11 (± 19) | 24 (± 23)† | 17 (± 25) |
| Pulmonary function test | ||||
| %FEV1, % | 104 (± 14) | 106 (± 13) | 98 (± 14)† | 73 (± 8)‡ |
| %FVC, % | 101 (± 14) | 102 (± 13) | 111 (± 16)† | 73 (± 9)‡ |
| FEV1/FVC | 0. 82 (± 0.05) | 0. 82 (± 0.05) | 0.72 (± 0.01)† | 0.80 (± 0.06)‡ |
| Comorbidities, N (%) | ||||
| Hypertension | 1395 (24) | 1318 (24) | 5 (9)† | 72 (28) |
| Diabetes | 388 (7) | 364 (7) | 1 (2) | 28 (11)‡ |
| Cardiovascular disease | 264 (5) | 250 (5) | 0 (0) | 14 (5) |
All values are expressed as the mean (± SD) except categorical variables, which are expressed as N (%). SD standard division, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, LLN lower limits of normal, BMI body mass index. *Subjects with FEV1/FVC ≥ LLN and %FEV1 > 80%. †P < 0.05, comparing subjects with FEV1/FVC < LLN to those with normal respiratory function. ‡P < 0.05, comparing subjects with %FEV1 < 80% to those with normal respiratory function.
After 5 years, 5086 subjects underwent follow-up assessments (Fig. 1).
The baseline characteristics of the subjects (N = 779) who were lost to follow-up are presented in Supplementary Table S1.
Development of AFL and dyspnoea
Among the 5086 subjects who attended the 5-year follow-up, AFL was newly identified in 449 subjects (9%); 1021 subjects (20%) had newly developed dyspnoea (mMRC ≥ 1), and 100 subjects developed both AFL and dyspnoea concurrently (AFL with dyspnoea).
Compared with subjects without AFL or dyspnoea at follow-up, subjects who developed AFL were older (mean 63 years vs. 58 years), more likely to be male (55% v 31%), and more likely to smokers (current or former) (49% vs. 28%) at baseline (Table 2), while subjects who developed dyspnoea were older (61 years vs. 58 years), had a higher BMI (23 kg/m2 vs. 22.3 kg/m2), and were more likely to be current smokers (13% vs. 9%). At follow-up, a higher prevalence of comorbidities, especially hypertension, was observed in both AFL patients and dyspnoea patients than in normal controls (29%, 30% and 21%).
Table 2.
Characteristics at enrolment of subjects who had AFL, dyspnoea or both at follow-up (N = 5086).
| AFL at follow-up | Dyspnoea at follow-up | AFL with dyspnoea at follow-up | Normal at follow-up | |
|---|---|---|---|---|
| N | 449 | 1,021 | 100 | 3716 |
| Age, years | 63 (± 8)* | 61 (± 9)* | 64 (± 8)* | 58 (± 9) |
| Female, N (%) | 202 (45)* | 702 (69) | 50 (50)* | 2564 (69) |
| Height, cm | 162 (± 8)* | 158 (± 8) | 161 (± 8)* | 159 (± 8) |
| Weight, kg | 59 (± 10)* | 58 (± 10)* | 59 (± 11)* | 57 (± 10) |
| BMI, kg/m2 | 22.4 (± 2.8) | 23 (± 3.3)* | 22.8 (± 3.3) | 22.3 (± 2.9) |
| Smoking status, N (%) | 219 (49)* | 307 (30) | 48 (48)* | 1052 (28) |
| Current | 98 (22)* | 131 (13) * | 27 (27)* | 328 (9) |
| Former | 121 (27)* | 176 (17) | 21 (21) | 724 (19) |
| Pulmonary function test | ||||
| %FEV1, % | 96 (± 14)* | 103 (± 15)* | 94 (± 14)* | 106 (± 14) |
| %FVC, % | 99 (± 16)* | 99 (± 15)* | 98 (± 15)* | 102 (± 14) |
| FEV1/FVC | 0.76 (± 0.04)* | 0.82 (± 0.05)* | 0.76 (± 0.04)* | 0.83 (± 0.05) |
| Comorbidities, N (%) | ||||
| Hypertension | 128 (29)* | 303 (30)* | 30 (30)* | 792 (21) |
| Diabetes | 31 (7) | 72 (7) | 6 (6) | 229 (6) |
| Cardiovascular disease | 23 (5) | 77 (8)* | 11 (11)* | 133 (4) |
All values are expressed as the mean (± SD) except categorical variables, which are expressed as N (%). SD standard division, AFL airflow limitation, BMI body mass index, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity. *P < 0.05, compared with normal subjects without AFL or dyspnoea at follow-up.
Subjects with AFL with dyspnoea were older (64 years vs. 58 years), more likely to be male (50% vs. 31%) and more likely to be current smokers (27% vs. 9%) than normal subjects. They also had higher prevalence rates of hypertension and cardiovascular disease (30% vs. 21% for hypertension and 11% vs. 4% for cardiovascular diseases).
Figure 2 shows the incidence rates of the development of AFL, dyspnoea, and both at follow-up, according to baseline spirometry characteristics (PRISm, FEV1/FVC < LLN, and any “subclinical respiratory dysfunction”). Subjects with any subclinical respiratory dysfunction at baseline had higher incidence rates of AFL (30%, 47% and 33%) and AFL with dyspnoea (8%, 7% and 8%) than those without them. Regarding the development of dyspnoea, those with PRISm at baseline had a higher incidence than normal subjects.
Figure 2.
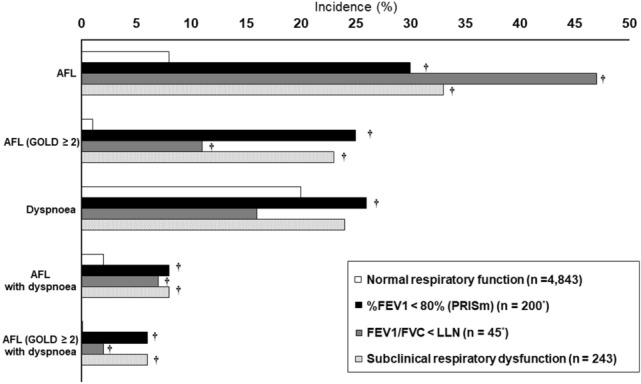
Incidence of the development of AFL, dyspnoea and both among subjects who underwent follow-up assessment. Incidence rates of AFL, dyspnoea, and both (AFL with dyspnoea) at follow-up in groups with normal respiratory function and subclinical respiratory dysfunction at enrolment (N = 5086). A GOLD grade ≥ 2 was defined as the development AFL with %FEV1 < 80%. AFL airflow limitation, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity. *Two subjects had both FEV1/FVC < LLN and %FEV1 < 80% at baseline. †P value < 0.05 compared with normal respiratory function.
The risk factors for the development of AFL (Table 3A), dyspnoea (Table 3B) and AFL with dyspnoea (Table 4) in the univariate and multivariate analyses are shown. Age, current smoking, cardiovascular disease, PRISm and FEV1/FVC < LLN at baseline were significantly associated with the development of AFL with dyspnoea in the multivariate analysis (risk ratio [95% confidence interval]; 1.99 [1.49–2.67] and 2.71 [1.44–5.09], respectively).
Table 3.
Risks associated with the development of AFL (A) and dyspnoea (B) at 5 years.
| (A) | RRb | Adjusted RRb | (B) | RRb | Adjusted RRb |
|---|---|---|---|---|---|
| Age ≥ 60 years | 2.24 (1.84–2.74) | 1.58 (1.40–1.79) | Age ≥ 60 years | 1.41 (1.26–1.58) | 1.22 (1.13–1.31) |
| Female | 0.39 (0.33–0.47) | 0.66 (0.57–0.77) | Female | 1.07 (0.95–1.21) | 1.19 (1.06–1.32) |
| Smoking status | Smoking history | ||||
| Current vs. former | 1.54 (1.20–1.97) | 2.04 (1.45–2.87) | Current vs. former | 1.41 (1.15–1.72) | 1.79 (1.37–2.34) |
| Former vs. never | 1.86 (1.51–2.29) | 1.06 (0.76–1.48) | Former vs. never | 0.82 (0.75–1.01) | 0.93 (0.73–1.19) |
| BMI ≥ 25 kg/m2 | 0.77 (0.61–1.00) | 0.76 (0.65–0.88) | BMI ≥ 25 kg/m2 | 1.39 (1.23–1.57) | 1.21 (1.11–1.32) |
| Hypertension | 1.31 (1.07–1.59) | 1.08 (0.95–1.22) | Hypertension | 1.38 (1.23–1.55) | 1.14 (1.05–1.24) |
| Diabetes | 1.08 (0.76–1.53) | 0.82 (0.67–1.02) | Diabetes | 1.13 (0.92–1.39) | 0.99 (0.85–1.14) |
| Cardiovascular disease | 1.19 (0.80–1.76) | 0.95 (0.75–1.21) | Cardiovascular disease | 1.79 (1.48–2.16) | 1.43 (1.22–1.69) |
| %FEV1 < 80% | 3.74 (2.96–4.73) | 2.17 (1.77–2.67) | %FEV1 < 80% | 1.27 (0.99–1.63) | 1.15 (0.96–1.37) |
| FEV1/FVC < LLN | 5.51 (3.98–7.63) | 4.61 (3.00–7.06) | FEV1/FVC < LLN | 0.77 (0.39–1.53) | 0.96 (0.64–1.43) |
| SP-370 at follow-upa | 2.28 (1.61–3.22) | 1.58 (1.31–1.90) | SP-370 at follow-upa | 1.08 (0.92–1.27) | 1.03 (0.94–1.14) |
RR risk ratio, AFL airflow limitation, BMI body mass index, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, LLN lower limits of normal. aSpirometer used at follow-up. bRR (95% confidence interval).
Table 4.
Risks associated with the development of AFL with dyspnoea at 5 years.
| RRb | Adjusted RRb | |
|---|---|---|
| Age ≥ 60 years | 2.98 (1.86–4.77) | 1.72 (1.34–2.21) |
| Female | 0.48 (0.32–0.71) | 0.84 (0.63–1.11) |
| Smoking status | ||
| Current vs. former | 2.54 (1.44–4.49) | 3.28 (1.79–6.02) |
| Former vs. never | 1.37 (0.82–2.28) | 0.90 (0.46–1.74) |
| BMI ≥ 25 kg/m2 | 1.10 (0.68–1.79) | 0.97 (0.75–1.25) |
| Hypertension | 1.42 (0.93–2.17) | 1.07 (0.85–1.34) |
| Diabetes | 0.94 (0.42–2.14) | 0.76 (0.50–1.15) |
| Cardiovascular disease | 2.74 (1.48–5.05) | 1.54 (1.10–2.15) |
| %FEV1 < 80% | 3.73 (2.12–6.57) | 1.99 (1.49–2.67) |
| FEV1/FVC < LLN | 3.50 (1.15–10.6) | 2.71 (1.44–5.09) |
| SP-370 at follow-upa | 2.38 (1.11–5.11) | 1.47 (1.01–2.15) |
RR risk ratio, AFL airflow limitation, BMI body mass index, FEV1 forced expiratory volume in 1 s, FVC forced vital capacity, LLN lower limits of normal. aSpirometer used at follow-up. bRR (95% confidence interval).
The associations between subclinical respiratory dysfunction and the development of AFL with dyspnoea were consistent in those with GOLD stage 2 or higher AFL (%FEV1 < 80% and FEV1/FVC < 0.7) (see Supplementary Table S2). Classifying FEV1/FVC based on the LLN defined by the European Respiratory Society Global Lung Function Initiative (GLI) produced results similar to those obtained using the LLN defined by the JRS (see Supplementary Table S3).
Serum brain natriuretic peptide (BNP) was also analysed (see Supplementary note). High BNP was associated with the development of AFL (risk ratio [95% confidence interval]; 1.71 [1.30–2.26]), dyspnoea (1.36 [1.13–1.64]) and AFL with dyspnoea (2.10 [1.19–3.73]) and it still had the positive risks for dyspnoea and AFL with dyspnoea in the multivariate general linear models (see Supplementary Table S4).
Discussion
We investigated a population-based cohort with follow-up assessments to evaluate both respiratory symptoms and pulmonary function and found that subclinical respiratory dysfunction, represented by FEV1/FVC < LLN and %FEV1 < 80% (PRISm), was independently associated with the development of AFL, especially AFL with dyspnoea, which is the most important COPD-like feature. Given the need to promote the early detection of COPD, the major finding of the present study is that subjects with subclinical respiratory dysfunction should be observed closely for the development of respiratory symptoms. Moreover, our results revealed the independent impacts of current smoking on the development of all AFL, dyspnoea, and AFL with dyspnoea; therefore, smoking cessation should be encouraged. We also showed that comorbidities and obesity independently contributed to the development of dyspnoea, and a history of cardiovascular disease had an impact on the development of AFL with dyspnoea.
Although the clinical importance of subclinical respiratory dysfunction has been identified, significant associations have been reported with only progression to COPD10,12,13,19–21. Park et al. reported that PRISm in elderly patients or those with existing respiratory symptoms was associated with an increased risk of a physician diagnosis of COPD within 3 years13. However, their study was limited to smokers, and they established only COPD, not the development of respiratory symptoms (dyspnoea) or AFL, as the outcome. Consequently, the relationship between PRISm and the development of COPD is ill-defined, especially in never smokers and those who are not yet symptomatic. Moreover, to our knowledge, no study has assessed the association between FEV1/FVC < LLN but ≥ 0.7 and the development of COPD. The present study builds on previous research on subclinical respiratory dysfunction by clarifying the risks for the development of AFL with dyspnoea at 5 years, which were two- and threefold higher in those with PRISm and FEV1/FVC < LLN, respectively, than in those with normal respiratory function, independent of age or smoking status.
The subjects with PRISm who developed AFL or AFL with dyspnoea mostly had GOLD stage 2 or higher disease (Fig. 2), independent of age, smoking status, or a history of cardiovascular disease. We also found that increased serum BNP was associated with both AFL and dyspnoea. These results were in accordance with those of a study on coronary risk factors for COPD22,23. Together with the heterogenetic characteristics of PRISm10, our results suggest that PRISm in those with a cardiovascular burden requires special attention.
The PRISm patients and control subjects had comparable BMI values, which were much lower than those reported in Western populations12. A similar difference in COPD patients between Japanese and Western populations has been reported24. Differences in several factors, including ethnicity, genetics, environment, lifestyle, and socioeconomic status, have been considered explanations24. These factors could also contribute to the difference in the PRISm rate between the populations. Additionally, the specific causes of low FVC in Japanese PRISm patients could differ from those in Western patients (old tuberculosis for example). The heterogeneity of PRISm should be considered when interpreting our results. Nevertheless, this study is significant in that it suggests that patients with PRISm, regardless of their symptoms or smoking status, could be candidates for early COPD detection in the Japanese population.
Interestingly, the characteristics of subjects with FEV1/FVC < LLN in our study were different from those with PRISm; they were younger, were predominantly female, and had a lower BMI than those with normal respiratory function, though the proportions of smokers were similar. Although these characteristics were also different from the characteristics of patients with COPD25, they were consistent with those in previous studies in subjects with FEV1/FVC between 0.7 and the LLN19,26. Impaired lung development is considered a factor affecting low FEV1/FVC19. The lung function trajectory is characterized by the attainment of maximal pulmonary function, as assessed by FEV1, at the age of 20–25 years and a subsequent decline with ageing27. Impaired lung development can lead to lower peak lung function and an accelerated loss of function, which are associated with future AFL28.
In our study, 9% and 2% of subjects developed AFL and AFL with dyspnoea within 5 years, respectively. These proportions were lower than those in a Western report12,13. This might reflect the larger population of never smokers in Japan. Indeed, a Japanese population-based study reported an incidence of AFL similar to that in our study29. We acknowledge potential bias from loss to follow-up. However, given the lower FEV1 in subjects who were lost to follow-up than in those who were followed, including the lost subjects would increase the incidence of COPD in the group with subclinical respiratory dysfunction. This supports our conclusion that subclinical respiratory dysfunction is a risk factor for the development of COPD.
We observed that different factors were associated with the development of AFL and dyspnoea. Age, male sex, current smoking, low BMI, and subclinical respiratory dysfunction were associated with the development of AFL. However, age, female sex, comorbidities, and obesity were associated with the development of dyspnoea. These differences were previously reported in a cross-sectional study on preclinical COPD5. In our study, we found the important contribution of obesity to the development of dyspnoea, despite several studies reporting controversial results and mechanisms of the association between dyspnoea and obesity3,30–33. Additionally, in our study, a history of cardiovascular disease was independently associated with not only the development of dyspnoea but also the development of AFL with dyspnoea. Although the mechanism is unclear, previous studies reporting the association between cardiovascular disease and COPD suggested the contribution of pulmonary vascular congestion or proinflammatory molecules, including angiotensin 2, in cardiovascular disease to the development of AFL22. On the other hand, there is a possibility that cardiovascular disease itself exacerbates dyspnoea during the process of airway remodelling in COPD. However, AFL, symptoms, and comorbidities are so closely linked in COPD that the GOLD document emphasize the importance of comprehensive management rather than addressing them as separate phenomena. Considering the previous study that found that dyspnoea itself is a risk factor for the development of COPD as well as a cause of morbidity13, our results are important in terms of identifying the population at high risk for COPD.
Significant associations between current smoking but not former smoking at enrolment and the development of dyspnoea and AFL with dyspnoea in 5 years were observed. This was previously suggested in a cross-sectional study that showed an association of current smoking but not pack years with severe respiratory symptoms3. Our study additionally revealed the importance of smoking cessation in subjects without AFL or dyspnoea in terms of prevention of both COPD and related morbidity.
Numerous clinical trials on the prognostic prediction of COPD have used the GOLD criteria25,34, and AFL with dyspnoea in this study comes close to fulfilling those criteria. We believe that identifying subjects at risk of the development of AFL with dyspnoea would be of great benefit in the real world. We found that those with subclinical respiratory dysfunction, including PRISm and FEV1/FVC < LNN, were 2- and 3-times more likely than those with normal function to develop AFL with dyspnoea, respectively. We suggest that more attention should be given to these subjects.
A strength of this study is its evaluation of risk factors using a large longitudinal population-based cohort and the 87% follow-up rate. However, some limitations should be mentioned. First, we had access to only spirometry results without bronchodilation. Therefore, we could not fully exclude subjects with reversible AFL. However, several studies have employed pulmonary function test parameters without bronchodilation as a metric1,35–37. Additionally, the GOLD guidelines accept this as a pragmatic approach to the identification of cases of COPD38. For these reasons, we are confident in our results with regard to the identification of risk factors for the development of COPD. Second, there are no standard reference equations for the Japanese population that are internationally accepted. Therefore, we applied the prediction equations from the JRS to identify FEV1/FVC < LLN in the present study. Additionally, we validated our results with GLI-derived reference equations for “other” ethnicities39. Third, we evaluated dyspnoea considering only the mMRC criteria. This unidimensional estimation of dyspnoea could cause underestimation and limit the interpretation of our study. However, several studies have described mMRC-defined dyspnoea to be a predictive factor for disability and mortality9,40. Therefore, we consider that our study is still of great importance for identifying subjects who may require medical intervention. Additionally, considering that those with an mMRC grade of 1 can be highly symptomatic40,41, we used a grade of 1 instead of 2 for the cut-off of the mMRC grade. This minimized underestimation and was suitable for our purpose of promoting early identification of subjects at risk.
We revealed that individuals with subclinical respiratory dysfunction, including FEV1/FVC < LLN and %FEV1 < 80% (PRISm), are at risk of developing COPD in 5 years. Patients with comorbidities and obesity could develop dyspnoea via mechanisms other than the progression of AFL.
Methods
Study design and subjects
This was a population-based observational study based on the Nagahama Cohort for Comprehensive Human Bioscience (the Nagahama Study); subjects from the general population of Nagahama in Shiga Prefecture, Central Japan, were enrolled from November 2008 to November 2010. Residents aged 30–74 years who were able to live independently and lacked serious health or physical impairment were recruited. The participants in this cohort were invited to participate in a follow-up assessment 5 years after enrolment, from 2013 to 2015.
All clinical measurements, pulmonary function tests and blood sampling were performed at enrolment and follow-up. Medical histories were investigated using a structured questionnaire. Dyspnoea was identified using the mMRC criteria7, and participants with an mMRC grade of 0 were considered to be free from dyspnoea.
Smoking status was classified as current, former, or never smoker. Cardiometabolic comorbidities, including hypertension, diabetes, and cardiovascular disease (a history of heart disease or stroke)42,43, were defined by the responses to the self-reported questionnaires and/or the results of blood tests (fasting blood glucose level ≥ 126 mg/dl, random serum glucose level ≥ 200 mg or HbA1c ≥ 6.5% for the diagnosis of diabetes)18.
Among the 9804 residents recruited from 2008 to 2010, 5868 subjects aged 40–75 years who did not have a history of adult asthma or COPD and who did not have AFL (FEV1/FVC ≥ 0.7) or dyspnoea (mMRC grade of 0) at the time of enrolment were included (Fig. 1).
This study adhered to the principles of the Declaration of Helsinki. All study protocols were approved by the ethics committee of Kyoto University Graduate School of Medicine and the Nagahama Municipal Review Board (Registry ID G0278). Written informed consent was obtained from all participants.
Pulmonary function tests
Pulmonary function was measured during an FVC manoeuvre with an electronic spirometer with automated quality checks (baseline; SP-350 COPD, Fukuda Denshi, Tokyo, Japan). In 15% of the subjects, the same type of spirometer (SP-350) was used to measure FVC at baseline and at follow-up, while a different type of spirometer (SP-370) was used in the remaining subjects.
An FVC manoeuvre was performed more than twice at baseline and at follow-up by trained and certified medical technologists to minimize the influence of incomplete effort. The most relevant data was selected by pulmonologists for analysis. AFL was defined based on a fixed ratio (FEV1/FVC < 0.7). Predicted normal values for FEV1, FVC and the LLN for FEV1/FVC were calculated using the JRS guidelines44. The LLN defined by the GLI was also used to confirm our results39.
Statistical analysis
The Wilcoxon rank-sum test and Pearson chi-square test were used to compare the characteristics of subjects with and without subclinical respiratory dysfunction at baseline and who had or had not developed AFL or dyspnoea at follow-up. To assess the adjusted risk ratio of the development of AFL, dyspnoea (mMRC ≥ 1) and AFL with dyspnoea in 5 years, we used multivariate general linear models with a Poisson distribution and log link function, with adjustment for age, sex, BMI, smoking history, and major comorbidities. Regarding age and BMI, clinically relevant cut-off values (age ≥ 60 years and BMI ≥ 25) were applied30.
A two-tailed P-value < 0.05 was considered statistically significant. All statistical analyses were performed using JMP Pro 14 (SAS Institute, Inc., Cary, NC). Data are presented as means (± standard deviations [SDs]) for continuous variables and percentages for categorical variables.
Ethics approval and consent to participate
This study adhered to the principles of the Declaration of Helsinki. All study protocols were approved by the ethics committee of Kyoto University Graduate School of Medicine and the Nagahama Municipal Review Board (Registry ID G0278). We obtained written informed consent from all the participants.
Supplementary Information
Acknowledgements
We are grateful to Nagahama City Office and the non-profit organization Zeroji Club for their assistance with the Nagahama study. We are grateful to Yoshiro Toyama, Masanori Azuma, Ryo Tachikawa and Morito Inouchi (Kyoto University Graduate School of Medicine, Kyoto, Japan) for their assistance with data collection.
Author contributions
M.K.: contributed to the data analysis, interpreted the data and wrote the draft. S.S.: conceived and designed the study; collected, analysed, and interpreted the data; wrote and edited the manuscript; and takes responsibility for all aspects of the work. S.M., and H.M.: contributed to the study design; collection and interpretation of the data; and the writing of the manuscript. N.N., N.T. and T.O.: contributed substantially to the interpretation of the data and the writing of the manuscript. H.S., and T.N.: contributed to the interpretation of the data and critically revised the manuscript. K.M.: contributed to the study design and data collection and revised the work critically. T.H.: provided overall supervision and critically revised the manuscript. T.K., Y.T., F.M., K.C. and T.H.: contributed to the design of the Nagahama cohort study, recruited subjects, acquired the funding, and critically revised the manuscript. The final manuscript was approved by all the authors.
Funding
This study was funded by a university grant; a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology in Japan (25293141, 26670313, 26293198, 17H04182, 17H04126, 17H04123, 18K18450); and grants from the Center of Innovation Program and the Global University Project from Japan Science and Technology Agency, Japan Agency for Medical Research and Development (AMED) (grant numbers dk0207006, dk0207027, ek0109070, ek0109283, ek0109196, ek0109348, kk0205008, ek0210066, ek0210096, ek0210116, and le0110005). This research was also supported by grants from the Japanese Ministry of Education, Culture, Sports, Science and Technology; the Intractable Respiratory Diseases and Pulmonary Hypertension Research Group from the Ministry of Health, Labour and Welfare of Japan (H29-intractable diseases-general-027); the Takeda Medical Research Foundation; the Mitsubishi Foundation; the Daiwa Securities Health Foundation; the Sumitomo Foundation; the Research Foundation for Healthy Ageing; and the Health, Labour and Welfare Sciences Research Grants, and Research on Region Medical (H28-iryo-ippan-016, H30-iryo-ippan-009). The Department of Respiratory Care and Sleep Control Medicine is funded by grants from Philips-Respironics, Fukuda Denshi, Fukuda Lifetec Keiji, and ResMed provided to Kyoto University.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Competing interests
M. K, S. M, H. M, N. N, N. T, T. O, T.K, and T. H have nothing to disclose. S. S reports a grant from Nippon Boehringer Ingelheim Co. and grants from Philips-Respironics, Fukuda Denshi, Fukuda Lifetec Keiji, and ResMed that did not pertain to the submitted work. H. S, and T. N, report grants from Philips-Respironics, Fukuda Denshi, Fukuda Lifetec Keiji, ResMed. K. M reports grants from Philips-Respironics, Teijin Pharma, Fukuda Denshi, Fukuda Lifetec Keiji, ResMed and Japan Society for the Promotion of Science, none of which pertained to the submitted work. Y. T reports grants from the Japan Agency for Medical Research and Development (AMED) and The Ministry of Education, Culture, Sports, Science and Technology in Japan during the study period. K. C reports grants from the Japanese Ministry of Education, Culture, Sports, Science and Technology; grants from the Intractable Respiratory Diseases and Pulmonary Hypertension Research Group, the Ministry of Health, Labour and Welfare, Japan; grants from the Research Foundation for Healthy Ageing; grants from Health, Labour and Welfare Sciences Research Grants, Research on Region Medical; grants from the Center of Innovation Program and the Global University Project from Japan Science and Technology Agency, Japan Agency for Medical Research and Development during the study period; grants and personal fees from Philips-Respironics, Teijin Pharma, Fukuda Denshi, Fukuda Lifetec Tokyo, Fukuda Lifetec Keiji, GlaxoSmithKline and Resmed; grants from KYORIN Pharmaceutical Co., Ltd. and Nippon Boehringer Ingelheim Co., Ltd; personal fees from MSD, Astellas Pharma and Eisai Co., Ltd; none of these pertained to the submitted work. F. M reports grants from Kyoto University, the Ministry of Education, Culture, Sports, Science and Technology in Japan, Japan Agency for Medical Research and Development (AMED) and The Takeda Medical Research Foundation during the study period.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-24657-w.
References
- 1.Fukuchi Y, et al. COPD in Japan: The Nippon COPD Epidemiology study. Respirology. 2004;9:458–465. doi: 10.1111/j.1440-1843.2004.00637.x. [DOI] [PubMed] [Google Scholar]
- 2.Takahashi T, et al. Underdiagnosis and undertreatment of COPD in primary care settings. Respirology. 2003;8:504–508. doi: 10.1046/j.1440-1843.2003.00501.x. [DOI] [PubMed] [Google Scholar]
- 3.Woodruff PG, et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N. Engl. J. Med. 2016;374:1811–1821. doi: 10.1056/NEJMoa1505971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaz Fragoso CA, et al. Respiratory impairment and mortality in older persons: A novel spirometric approach. J. Investig. Med. 2011;59:1089–1095. doi: 10.2310/JIM.0b013e31822bb213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Remoortel H, et al. Risk factors and comorbidities in the preclinical stages of chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2014;189:30–38. doi: 10.1164/rccm.201307-1240OC. [DOI] [PubMed] [Google Scholar]
- 6.Adibi A, Sadatsafavi M. Looking at the COPD spectrum through "PRISm". Eur. Respir. J. 2020;55:1902217. doi: 10.1183/13993003.02217-2019. [DOI] [PubMed] [Google Scholar]
- 7.Vestbo J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 8.Nici L, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2006;173:1390–1413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 9.Celli BR, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 2004;350:1005–1012. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 10.Wan ES, et al. Epidemiology, genetics, and subtyping of preserved ratio impaired spirometry (PRISm) in COPDGene. Respir. Res. 2014;15:89. doi: 10.1186/s12931-014-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guerra S, et al. Morbidity and mortality associated with the restrictive spirometric pattern: A longitudinal study. Thorax. 2010;65:499–504. doi: 10.1136/thx.2009.126052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wijnant SRA, et al. Trajectory and mortality of preserved ratio impaired spirometry: The Rotterdam Study. Eur. Respir. J. 2020;55:1901217. doi: 10.1183/13993003.01217-2019. [DOI] [PubMed] [Google Scholar]
- 13.Park HJ, et al. Significant predictors of medically diagnosed chronic obstructive pulmonary disease in patients with preserved ratio impaired spirometry: A 3-year cohort study. Respir. Res. 2018;19:185. doi: 10.1186/s12931-018-0896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohamed Hoesein, F. A., Zanen, P., Lammers, J. W. Lower limit of normal or FEV1/FVC < 0.70 in diagnosing COPD: an evidence-based review. Respir. Med.105, 907–915 (2011) [DOI] [PubMed]
- 15.Vaz Fragoso CA, et al. The ratio of FEV1 to FVC as a basis for establishing chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2010;181:446–451. doi: 10.1164/rccm.200909-1366OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomsen M, Nordestgaard BG, Vestbo J, Lange P. Characteristics and outcomes of chronic obstructive pulmonary disease in never smokers in Denmark: A prospective population study. Lancet Respir. Med. 2013;1:543–550. doi: 10.1016/S2213-2600(13)70137-1. [DOI] [PubMed] [Google Scholar]
- 17.Calverley PMA, Mueller A, Fowler A, Metzdorf N, Wise RA. The effect of defining chronic obstructive pulmonary disease by the lower limit of normal of FEV1/FVC ratio in tiotropium safety and performance in respimat participants. Ann. Am. Thorac. Soc. 2018;15:200–208. doi: 10.1513/AnnalsATS.201703-194OC. [DOI] [PubMed] [Google Scholar]
- 18.Garcia-Rio F, et al. Overdiagnosing subjects with COPD using the 0.7 fixed ratio: correlation with a poor health-related quality of life. Chest. 2011;139:1072–1080. doi: 10.1378/chest.10-1721. [DOI] [PubMed] [Google Scholar]
- 19.Colak Y, et al. Young and middle-aged adults with airflow limitation according to lower limit of normal but not fixed ratio have high morbidity and poor survival: A population-based prospective cohort study. Eur. Respir. J. 2018;51:1702681. doi: 10.1183/13993003.02681-2017. [DOI] [PubMed] [Google Scholar]
- 20.Strand M, et al. A risk prediction model for mortality among smokers in the COPDGene(R) study. Chronic Obstr. Pulm. Dis. 2020;7:346–361. doi: 10.15326/jcopdf.7.4.2020.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wan ES, et al. Longitudinal phenotypes and mortality in preserved ratio impaired spirometry in the COPDGene Study. Am. J. Respir. Crit. Care Med. 2018;198:1397–1405. doi: 10.1164/rccm.201804-0663OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petersen H, et al. Rapid lung function decline in smokers is a risk factor for COPD and is attenuated by angiotensin-converting enzyme inhibitor use. Chest. 2014;145:695–703. doi: 10.1378/chest.13-0799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Griffith KA, et al. Predictors of loss of lung function in the elderly: The Cardiovascular Health Study. Am. J. Respir. Crit. Care Med. 2001;163:61–68. doi: 10.1164/ajrccm.163.1.9906089. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi S, Betsuyaku T. The chronic obstructive pulmonary disease comorbidity spectrum in Japan differs from that in western countries. Respir. Investig. 2015;53:259–270. doi: 10.1016/j.resinv.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Alpin DMG, et al. Global Initiative for the diagnosis, management, and prevention of chronic obstructive lung disease: The 2020 GOLD science committee report on COVID-19 & COPD. Am. J. Respir. Crit. Care Med. 2021;203:24–36. doi: 10.1164/rccm.202009-3533SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okada Y, et al. Renewed Japanese spirometric reference variables and risk stratification for postoperative outcomes in COPD patients with resected lung cancer. Nagoya J. Med. Sci. 2019;81:427–438. doi: 10.18999/nagjms.81.3.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Washko GR, et al. Adult life-course trajectories of lung function and the development of emphysema: The CARDIA Lung Study. Am. J. Med. 2020;133:222–230 e211. doi: 10.1016/j.amjmed.2019.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lange P, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N. Engl. J. Med. 2015;373:111–122. doi: 10.1056/NEJMoa1411532. [DOI] [PubMed] [Google Scholar]
- 29.Sato K, et al. Impact of cigarette smoking on decline in forced expiratory volume in 1s relative to severity of airflow obstruction in a Japanese general population: The Yamagata-Takahata study. Respir. Investig. 2018;56:120–127. doi: 10.1016/j.resinv.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 30.Laviolette L, et al. Effect of obesity on constant workrate exercise in hyperinflated men with COPD. BMC Pulm. Med. 2010;10:33. doi: 10.1186/1471-2466-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zewari S, Vos PV, den Elshout F, Dekhuijzen R, Heijdra Y. Obesity in COPD: Revealed and unrevealed issues. COPD. 2017;14:663–673. doi: 10.1080/15412555.2017.1383978. [DOI] [PubMed] [Google Scholar]
- 32.Babb TG, Ranasinghe KG, Comeau LA, Semon TL, Schwartz B. Dyspnea on exertion in obese women: Association with an increased oxygen cost of breathing. Am. J. Respir. Crit. Care Med. 2008;178:116–123. doi: 10.1164/rccm.200706-875OC. [DOI] [PubMed] [Google Scholar]
- 33.Ora J, et al. Combined effects of obesity and chronic obstructive pulmonary disease on dyspnea and exercise tolerance. Am. J. Respir. Crit. Care Med. 2009;180:964–971. doi: 10.1164/rccm.200904-0530OC. [DOI] [PubMed] [Google Scholar]
- 34.Agusti A, et al. Characteristics, stability and outcomes of the 2011 GOLD COPD groups in the ECLIPSE cohort. Eur. Respir. J. 2013;42:636–646. doi: 10.1183/09031936.00195212. [DOI] [PubMed] [Google Scholar]
- 35.Young RP, et al. Airflow limitation and histology shift in the National Lung Screening Trial. The NLST-ACRIN Cohort Substudy. Am. J. Respir. Crit. Care Med. 2015;192:1060–1067. doi: 10.1164/rccm.201505-0894OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogata H, et al. Trends in the prevalence of airflow limitation in a general Japanese population: two serial cross-sectional surveys from the Hisayama Study. BMJ Open. 2019;9:e023673. doi: 10.1136/bmjopen-2018-023673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perez-Padilla R, et al. Lung function decline in subjects with and without COPD in a population-based cohort in Latin-America. PLoS ONE. 2017;12:e0177032. doi: 10.1371/journal.pone.0177032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: A review of the 2018 GOLD report. Mayo Clin. Proc. 2018;93:1488–1502. doi: 10.1016/j.mayocp.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 39.Quanjer PH, et al. Multi-ethnic reference values for spirometry for the 3–95-year age range: the global lung function 2012 equations. Eur. Respir. J. 2012;40:1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ertan Yazar E, et al. How to utilize CAT and mMRC scores to assess symptom status of patients with COPD in clinical practice? Medeni Med. J. 2022;37:173–179. doi: 10.4274/MMJ.galenos.2022.06787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Perez T, et al. Modified Medical Research Council scale vs. Baseline Dyspnea Index to evaluate dyspnea in chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2015;10:1663–1672. doi: 10.2147/COPD.S82408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mannino DM, et al. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur. Respir. J. 2008;32:962–969. doi: 10.1183/09031936.00012408. [DOI] [PubMed] [Google Scholar]
- 43.Triest FJJ, et al. Airflow obstruction and cardio-metabolic comorbidities. COPD. 2019;16:109–117. doi: 10.1080/15412555.2019.1614550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kubota M, et al. Clinical Pulmonary Functions Committee of the Japanese Respiratory S: Reference values for spirometry, including vital capacity, in Japanese adults calculated with the LMS method and compared with previous values. Respir. Investig. 2014;52:242–250. doi: 10.1016/j.resinv.2014.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.


