Abstract
The extent to which power, resources, and responsibilities for public health are centralized or decentralized within a jurisdiction and how public health functions are integrated or coordinated with health care services may shape pandemic responses. However, little is known about the impacts of centralization and integration on public health system responses to the COVID-19 pandemic. We examine how public health leaders perceive centralization and integration facilitated and impeded effective COVID-19 responses in three Canadian provinces. We conducted a comparative case study involving semi-structured interviews with 58 public health system leaders in three Canadian provinces with varying degrees of centralization and integration. Greater public health system centralization and integration was seen by public health leaders to facilitate more rapidly initiated and well-coordinated provincial COVID-19 responses. Decentralization may have enabled locally tailored responses in the context of limited provincial leadership. Opacity in provincial decision-making processes, jurisdictional ambiguity impacting Indigenous communities, and ineffectual public health investments were impediments across jurisdictions and thus appear to be less impacted by centralization and integration. Our study generates novel insights about potential structural facilitators and impediments of effective COVID-19 pandemic responses during the second year of the pandemic. Findings highlight key areas for future research to inform system design that support leaders to manage large-scale public health emergencies.
Keywords: Public health systems, COVID-19, Organizational structure, Governance, Decentralization, Canada
1. Introduction
A strong public health system is critical to the effective management of public health emergencies such the coronavirus disease 2019 (COVID-19) pandemic. A public health system includes public sector organizations mandated to fulfil the essential public health operations of monitoring and response to health hazards and emergencies, disease surveillance and prevention, and health promotion and protection [1,2]. Public health system leaders play a role in directing, advising, implementing, and monitoring national, regional, and local pandemic responses. They include elected officials, government workers involved in health and emergency responses, medical doctors with legislated responsibilities addressing essential public health operations (e.g., medical officers of health), administrators of health services and non-governmental organizations, and scientific specialists (e.g., epidemiologists, microbiologists). Examining how power relations, responsibilities, and resources are distributed and coordinated among public health and other health system leaders and their respective organizations can help explain how systems perform in response to global emergencies. In particular, the extent to which power and responsibilities for public health are centralized versus decentralized and whether and how public health functions are integrated or coordinated with health care services, may impact the effectiveness of pandemic responses.
Centralization and decentralization have been defined as dynamic processes of redistributing powers, responsibilities or resources towards or away from a central government (national or sub-national) [3] or within government, whereby power is redistributed between the head of government and subordinate politicians, civil service members and agency executives [4]. The theoretical arguments for health system decentralization suggest that more local level decision making may allow for health resources and program planning to better reflect needs and preferences of the local population, thereby improving patient/public satisfaction as well as effectiveness [5], [6], [7]. Decentralization may lead to more experimentation and innovation, which could also improve overall health system performance if promising practices or reforms are scaled up. The extent of decentralization is also a key contextual factor influencing the initiation of intersectoral actions to promote health and equity [8,9]. However, more decentralized health systems may also exacerbate geographic inequalities [10], and increase health system costs due to potential duplication of services and functions, and lower economies of scale (e.g., for programs with high fixed costs such as laboratories, and information technology systems). Generally, any positive health system impacts with decentralization will depend on the capacity of the local/regional decision makers, for example, their skill and knowledge in health sector management and their ability to engage with local communities to ensure their needs and priorities inform decisions [5,[11], [12], [13]]. Based on a global review of studies examining the impacts of health system decentralization, decentralized systems appear to benefit from being “close to the ground” whereby leaders have greater access to information on, and experiences with, local community needs which can then translate into more contextually appropriate, efficient, and equitable decisions [3].
During public health emergencies, the potential advantages and disadvantages of decentralization may be different than in normal times. The theoretical benefits of decentralization generally do not apply to public goods with inter-jurisdictional externalities, such as pandemics and public health programs [14,15]. Highly centralized “command and control” style emergency management approaches are thought to be critical for timely decision-making, efficient redistribution of resources to address areas of need, and more effective coordination of the health workforce [16]. However, these approaches do not guarantee that central commanders have sufficient expertise for effective pandemic responses [17]. Within more decentralized systems, regional or sub-regional leadership may be able to compensate for weaknesses of central health system leadership, but may also experience challenges coordinating responses across regions [4,17]. Few studies have examined how public health system performance in a crisis, such as the COVID-19 pandemic, is impacted by centralization and decentralization [3,4,17,18].
The level of integration between public health and acute, or personal, health care systems may also impact pandemic responses. Public health and health care services can be considered administratively integrated when they fall within a common operational leadership structure, share a common mandate, and a shared budget [19]. The delivery of public health programs and services may also be functionally integrated with health care services if they are actively coordinated with one another, they share information systems, and work towards shared performance objectives [19]. The WHO has argued that integrating public health and health care allows for the adoption of a population health perspective in primary care which can lead to improved population health outcomes [20]. Also, during a public health emergency, integration may enable swifter mobilization of resources (e.g., health workforce, personal protective equipment, vaccines) [21,22]. However, the prioritization of resources for allocation to health care services (with a focus on treatment as opposed to prevention) over public health programs and services is a concern with integrating public health and health care sectors, especially in the context of constrained health system resources [23,24]. Whether and how the level and nature of integration between public health and health care services and the extent of centralization of public health systems impact the ability of public health actors to fulfil their roles in a pandemic are thus of critical importance.
1.1. Study Context: Canadian public health systems
Over the past 40 years, most provinces in Canada (except Ontario) have shifted from highly decentralized municipally governed and administered public health systems (e.g., locally-governed Boards of Health) towards more regionalized or centralized structures [25]. “Regionalization” reforms began in the 1990s and both maintained a decentralization of provincial powers but also a consolidation of municipal powers across broader regional geographies and across health service sectors (i.e., reforms reflect elements of both centralization and integration) [25]. Provincial governments have implemented these reforms to varying degrees with sub-provincial regional health authorities generally responsible for administering most public health programs and services. We focus on three provinces in our study with variations in the public health system governance and organizational structure, specifically with varying levels of decentralization and integration between public health and health care. Selecting these cases allowed us to consider whether and how aspects of public health system decentralization and integration impacted pandemic responses from the perspectives of those working in the system. Alberta, Ontario and Québec (see Table 1 ) are three of the most populous provinces in Canada and each have experienced high COVID-19 incidence and mortality relative to other parts of Canada [26,27].
Table 1.
Degree of centralization and integration of public health systems in Alberta, Québec, and Ontario.
| Alberta | Québec | Ontario | |
|---|---|---|---|
| Level of Centralization | Centralized (Alberta Health Services) |
Regionalized (18 Regional Public Health Departments within CISSS/CIUSSS) |
Decentralized (34 local Public Health Units) |
| Level of Integration with Acute Health Care | High | Mediuma | Low |
Notes: Each province's ministry of health (or equivalent) serves as the health system policy lead and houses the Office of Chief Medical Officer of Health (or equivalent) who in every case is a public health expert advisor to the Minister of Health but whose powers (e.g., authority to communicate publicly) and management responsibilities vary across cases; Ontario and Québec also have arm's length public health scientific agencies, Public Health Ontario and Institut national de santé publique du Québec, that are responsible for providing specialized public health advice and support for the public health system, and managing public health laboratories; CISSS – Centres intégrés de santé et de services sociaux (CISSS) (Integrated Health and Social Services Centres); CIUSSS – Centres intégrés universitaires de santé et de services sociaux (Integrated University Health and Social Services Centres).
Medium - having greater administrative integration but limited functional integration.
The Alberta health system underwent successive regionalization reforms starting in the early 1990s [28]. In 2003, 17 regional health authorities were reduced to nine and then in 2008, shortly before the H1N1 influenza pandemic, Alberta centralized its health system [28]. This centralization reform involved the consolidation of nine regional health authorities and the creation of one province-wide arm's-length delegated health authority called Alberta Health Services (AHS) operating with five geographically defined zones [28].
In 2015, the Québec government consolidated 94 Health and Social Service Centres, abolished their regional governance agencies, and integrated 18 Regional Public Health Departments into 22 newly established Integrated Health and Social Service Agencies (Centres intégrés de services de santé et services sociaux [CISSS] and Centres intégrés universitaires de services de santé et services sociaux [CIUSSS]) responsible for the administration and delivery of public health, health care, and social services [29]. This reform was accompanied by regional public health budget reductions and it preserved the regional mandate of Regional Public Health Directors (here forward referred to as regional Medical Officers of Health [MOHs]) which in three regions includes the catchment areas of more than one CISSS/CIUSSS [30], [31], [32].
Ontario is the only province in Canada that maintained its decentralized public health system structure which, from 2007 to 2019, functioned alongside 14 Local Health Integration Networks (LHINs) that were responsible for planning and funding health care services for geographically defined populations [33]. In 2019, LHINs were decommissioned and the province-wide Ontario Health agency along with multi-sectoral Ontario Health Teams (in some regions) were established. The provincial government also began public consultation on plans to consolidate Ontario's 34 local Public Health Units bringing them under ten health regions [34]. These plans were subsequently put on hold due to the COVID-19 pandemic alongside planned reductions in the province's share of funding for local units [35].
In this paper we examine whether and how the characteristics of public health system centralization and integration in Alberta, Ontario, and Québec may have influenced COVID-19 pandemic responses. We are not aware of any study that has examined public health system centralization and integration in Canada in relation to effective public health emergency responses. However, previous experiences with emergencies underscored the tension between the need for centralized administration and coordinated messaging during emergencies with the need for public health leaders to foster strong connection with local communities to maintain trust and design effective, targeted measures [36]. Also, the Severe Acute Respiratory Syndrome (SARS) experience in Ontario revealed the fragmentation between public health and acute/hospital care that was also observed during COVID-19, as well as highlighting major deficiencies in pandemic preparedness and in information systems needed for surveillance [37,38]. Further, during H1N1, there were some challenges noted with the decentralized health systems such as variations in pandemic preparedness and difficulties redeploying health workers across regions [39]. Our objective is to generate insights into potential system-level facilitators and impediments to effective responses that can help inform post-pandemic public health systems reforms.
2. Methods
2.1. Study Design and Research Team
This qualitative multiple case study was nested within a larger research project examining the impacts of financial and organizational restructuring of public health systems in Canada. We conceptualized public health system organization, governance, financing, and workforce using the WHO enabler essential public health operations definitions [40]. Our study involved in-depth semi-structured interviews with 58 participants in three Canadian provinces.
2.2. Theoretical and Conceptual Framework
Constructivist and pragmatic worldviews guided our approach to study design, data collection, and analysis. Accordingly, we assumed that the understandings sought and distilled from participants reflected subjective meanings created by individuals through their experiences in society, their actions and interactions with others, and that meaning is further generated through analyses comparing data shared by multiple individuals [41]. Our methodological approach aligned well with pragmatist principles as we aimed to generate actionable and practical knowledge, gain insight into less observable interconnections between participants’ experiences, knowledge and actions (e.g. unpublished information on organizational processes, or mechanisms underlying the performance of systems), and understand people's varied experiences with certain phenomena (e.g. asking participants about hypothetical consequences of different scenarios) [41,42].
2.3. Participant Selection
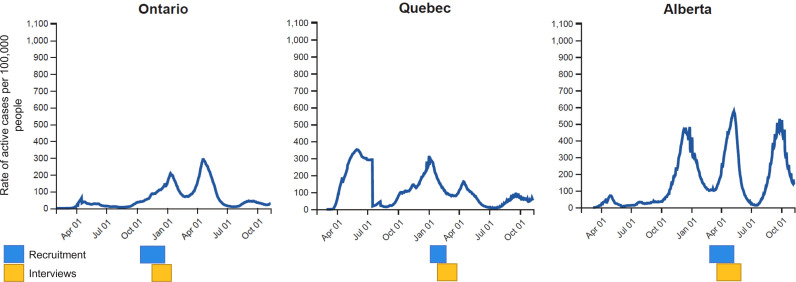
From October 30, 2020, to April 29, 2021, interviews were conducted virtually with participants from Alberta, Ontario, and Québec. Recruitment for this study took place when some provinces were experiencing high and/or increasing COVID-19 case counts (Fig. 1 ). Our recruitment approach included a combination of purposive (maximum variation) and snowball recruiting [43]. To identify interview invitees, we used organizational charts, professional association membership lists, study team recommendations, and manual internet searches. We recruited participants by email based on their current or past employment status in a formal leadership position with organizations with a primary focus on essential public health operations, and professional background and experience (i.e., training, primary areas of work within public health, geographic and urban/rural location of work). Participants working within First Nations or Inuit-led organizations that shared geographic boundaries with one of the three provinces were included (invitees working within Métis-led health organizations were not identified).
Fig. 1.
Recruitment and interview timeframes in relation to the rate of active cases (per 100,000 people) in Ontario, Quebec, and Alberta from February 2020 to October 2021.
We invited 44, 42, and 34 participants from Alberta, Ontario, and Québec, respectively and after accounting for non-response, declines and scheduling conflicts, 21, 18, and 19 participants were interviewed (total n = 58; Table 2 ). The largest shares of participants worked for organizations with primarily urban catchment areas, within local/regional public health departments or health authorities, were registered medical professionals, and served as MOHs (or equivalent) and director or manager-level administrators.
Table 2.
Participant characteristics across three Canadian provinces (Total, n=58).
| Characteristic | Alberta (n=21) | Ontario (n=18) | Québec (n=19) | Total (N=58) | ||
|---|---|---|---|---|---|---|
| Geographya | Urban | 15 | 11 | 14 | 40 (69%) | |
| Rural/Northern | 6 | 7 | 5 | 18 (31%) | ||
| Workplace | Local/regional public health department or health authority | 14 | 15 | 10 | 24 (41 %) | |
| Provincial government or arms-length scientific institute | <5 | <5 | 9 | 15 (26%) | ||
| Other (e.g., federal health agency, professional associations, non-governmental organization) | <5 | <5 | <5 | 4 (7%) | ||
| Disciplineb | Medical or nursing | 11 | 10 | 10 | 31 (40%) | |
| Other (e.g., policy and management, dental, nutrition, health promotion, epidemiology, environmental and occupational health) | 10 | 8 | 9 | 27 (47%) | ||
| Rolec | Senior leadership (e.g., Deputy Minister, CMOH, Chief Executive Officer, executive director) | 6 | 5 | 5 | 16 (28%) | |
| Medical officer of health (federal/ regional/local) | 6 | 5 | 6 | 17 (29%) | ||
| Other (e.g., director, manager, program lead, consultant) | 9 | 8 | 8 | 25 (43%) | ||
Notes:
Refers to the catchment area of the participant's organization.
Registered profession (e.g., medical doctor, Registered nurse) or area of work at time of interview.
Role that the participant was employed within while working in public health system (past or present).
2.4. Data Collection
Semi-structured interviews were conducted virtually (through Microsoft Teams or Zoom videoconferencing) by one study team member with a notetaker present for the Ontario and Québec interviews. The study interview guide was developed based on the conceptual framework for public health system organization, governance, financing, and workforce [44,45]. The present study focuses on responses to questions and prompts regarding the state of each public health system leading up to the COVID-19 pandemic and facilitators and impediments to effective COVID-19 responses. Interviews lasted 60 minutes on average and were audio recorded and transcribed verbatim by a professional service. Interviews conducted in French were transcribed and translated into English by a professional bilingual transcriptionist and then reviewed for accuracy by the interviewer or a bilingual study team member. For the purposes of reflexivity, after each interview, the interviewer debriefed (with and without notetakers) to record ways the interview and their understandings drawn from it may have been influenced by their assumptions, behaviours, beliefs, and ways of knowing [46]. We considered data saturation at the data collection phase using an a priori assumption that 15 to 20 interviews in each province should provide us with a saturation of ideas and themes being presented [47].
2.5. Data Analysis
To strengthen the trustworthiness of our findings, we applied principles of credibility, dependability, confirmability, and transferability throughout data analysis and theming [48]. The study team used a primarily deductive approach to directed content analysis.
To identify and characterize patterns of meaning in the coded text, we conducted in-depth thematic analysis [49]. Synthesized member checking was conducted for each province to ensure views were accurately captured and that themes resonated with respondent experiences [50]. Ten participants reviewed and provided feedback on themes. Comments critiquing or elaborating on presented themes were recorded in the theme reports and considered during cross-case theming. Next, cross-case comparative analysis was conducted to assess the similarities and differences in themes observed across the provinces [51]. The Consolidated Criteria for Reporting Qualitative Research checklist (Supplement 1) guided how we reported our findings [52].
2.6. Research Ethics
This study was approved by the University of Toronto Research Ethics Board (REB-39438).
3. Results
Our thematic analysis of facilitators of, and impediments to, COVID-19 responses generated three themes that varied in their salience within and across jurisdictions. The first two themes address how degrees of public health system centralization and integration impacted COVID-19 responses while the third theme was cross-cutting, and thus less dependent on the extent of centralization and integration. These include: 1) Facilitating timely and coordinated province-wide responses; 2) Constraining aspects of local and regional MOH authority; and 3) Provincial opacity, prior investment, and mandate ambiguity. The following sections present each theme in detail and representative quotations with participants identified by province and identification number (e.g., Alberta participant one: AB-01).
3.1. Theme 1: Facilitating timely and coordinated province-wide responses to the pandemic
The more centralized public health systems in Québec and Alberta were noted to be in a better position to launch and coordinate province-wide response measures during the early part of the COVID-19 pandemic compared to the more decentralized system in Ontario. Specific facilitators thought to contribute to effective responses included faster provincial decision-making, information flow from provincial to regional actors, clearer roles and responsibilities among health system actors, and greater ease in redirecting resources from across the health system to support public health functions. A lack of timely guidance from provincial leaders such as the provincial CMOH and a fully operational provincial health coordinating structure was described as impeding effective COVID-19 responses in Ontario.
In Alberta and Québec, aspects of provincial public health legislation were described as expediting decision-making and creating a clear cascade of authority from Minister to CMOH to MOHs. Participants described how public health and emergency response legislation (e.g., Loi en cas d'urgences sanitaires, Health Emergencies Act):
“defined the functions […] the Health Minister is the one who leads and works collaboratively with the Provincial Public Health Director and Regional Directors. So that structure was pretty clear” (QC-11);
And that,
“There was good, strong leadership, and I think a very effective model that was set up at the provincial level and then cascading down to the zones to respond. And it wasn't perfect but definitely allowed for a lot of impressive work very quickly during the first wave” (AB-05).
Complementing legislated roles and authority of public health leaders within these integrated health systems, were emergency management structures which facilitated role clarity, information flow, and resource redistribution. Explicitly described was a provincial Emergency Coordinating Centre that was operationally interconnected with regional Emergency Operations Centres that had “very strong processes in place about how decisions get made, who's going to be doing what role and communication. So I think that really enabled the response” (AB-01). Regarding public health and health care integration, one participant described:
“We have everything integrated within one CIUSSS, public health, emergency preparedness, general care, nursing, logistics for devices, communications, the fact that we are all under one management structure, everyone can be directed towards the emergency” (QC-01).
Participants in Ontario described the timeliness of provincial guidance regarding public health measures as a perceived impediment to effective pandemic responses. Thus, the perceived absence of fully operational regional or province-wide coordination mechanisms contributed to role confusion and impeded coordination across public health units and health care actors within regions. At least in the earliest stages of the COVID-19 response “it was like, well, I don't know if that's my job. Is that your job? I mean that's literally the kind of conversations that people were having with hospital leads and, you know, [Local Health Integration Network] folks” (ON-08). Participants in Ontario also saw advantages to the integrated systems in other provinces which were believed to have enabled: “them to get up to speed a whole lot quicker... it took Ontario a heck of a lot longer to mobilize […] to deal with the pandemic than was the case in Alberta or British Columbia” (ON-15).
3.2. Theme 2: Constraining aspects of regional Medical Officer of Health authority
Within Ontario's decentralized public health system, participants described the legislated authority and autonomy of local MOH and public health units as a facilitator of COVID-19 responses, allowing for local adaptation and response, particularly important where provincial leadership and coordination was limited or absent. However, regional MOH in Alberta and Québec described authority and autonomy constraints that impacted their ability to communicate publicly and coordinate across sectors regionally and locally.
In Québec, participants described overlap in the authority of regional MOH and CISSS/CIUSSS Chief Executive Officers which impeded collaboration across regional public health departments and some CISSS/CIUSSS, particularly where regional public health departments served multiple CISSS/CIUSSS. Participants described role and responsibility confusion experienced between regional MOH, who have decision-making authority for a geographic region, and CISSS/CIUSSS Chief Executive Officers, who have decision-making authority for their respective institution. One participant exclaimed how this configuration of authority creates:
“a huge potential for distortion especially during a pandemic, when actions needed to happen quickly and targeting the most vulnerable populations specifically...the capacity for CISSS and CIUSSS to intervene was decreased by a public health department that says ’It's my job, not yours.’ So… imagine the disagreements that play out. You send in your remote testing bus, and you see the other team's bus pulling up… come on. That actually happened” (QC-12).
In Québec, few explicitly described regional MOH authority as a facilitator of effective COVID-19 responses. Participants spoke to the regional MOH's authority to mobilize resources from across CISSS/CIUSSS as a facilitator but in member-checking one noted that the Ministry of Health and Social Services maintained significant control over resources (e.g., extra funding and vaccines) and exercised veto power.
Regional MOHs in Alberta described lacking the autonomy to directly communicate with their local communities and to collaborate with multi-sectoral partners. One participant explicitly noted that perceived “political pressures” from the Alberta government on AHS prevented the organization from publicly reporting on COVID-19 inequities (AB-05).
“The independence of local medical officers of health to respond to the local conditions in terms of the pandemic is way down […] the number of MOHs who have given interviews or made statements in public throughout this last year, it's way down compared to a normal year. And it's been operated as a military operation where the chief MOH at the top is the one who speaks for everyone. And there are strengths to that. You know, in a crisis, you don't want confusing messages. But there are also weaknesses because there is… You know, public health is committed to diversity. And there are differences in where the organism is striking and who's at risk. And those should be responded to locally” (AB-07).
These impediments required MOH to rely on informal relationships with partners in other sectors outside of health to devise workarounds for addressing local needs. While discussed as an impediment, participants also expressed an understanding of the importance of AHS communicating consistent messages across regions.
“You know, that issue of not being able to partake in public discourse around mask use was a particularly tricky one that struck us as somewhat problematic. Because normally that would be a core opportunity for MOHs to engage with their communities. And particularly the rural MOHs feel that more because they have those personal connections. […] I think I also don't want to overstate it though. Because a lot of times we can accomplish similar things in terms of our work with partners, just in a less visible way” (AB-05).
In Ontario, the autonomy of local MOHs and connectivity of public health units with multi-sectoral partners (e.g., municipalities, school boards, and community-based organizations) and neighbouring public health units were thought to have enabled prompt local decision-making, collaboration, and coordination of public health measures. Speaking to the legislated decision-making authority of MOHs during emergencies one participant explained:
“Our Medical Officer of Health established the Health Emergency Operations Centre where he is the decision-maker, and he didn't need to go through our regular bureaucratic processes of approval. So, he was able to go straight to council, the regional chairman, if anything occurred. And he was able to independently make decisions” (ON-04).
Another participant gave an example of how early in the pandemic:
“Everybody was worried about schools. And the health care system is like, ‘What do we do about schools?’ We were saying, ‘We meet with schools routinely, we conduct programming in schools, we meet with the Board of Directors. We have multilevel structures that that have communications with all levels of leadership at the school.’ And so we can implement things like infection prevention and control capacity development easily and quickly and successfully because of the relationships that we already have with these important community stakeholders” (ON-18).
Preceding the pandemic, this local connectivity of public health units was described as a key strength of the Ontario public health system particularly because it was thought to enable action on social determinants of health and health equity. Beyond enabling multi-sectoral coordination, particularly with the education sector and departments within municipal government, during the pandemic, there was comparatively little discourse explicitly describing this local connectivity as enabling more equitable COVID-19 responses.
3.3. Theme 3: Challenges with decision making opacity, prior public health investment, and Indigenous health mandate ambiguity
Across jurisdictions, perceived opacity of provincial government decision making, pre-pandemic levels of investment in public health, and unclear provincial roles and responsibilities with respect to First Nations, Inuit and Métis health were thought to have impeded effective COVID-19 responses independent of public health system centralization and integration.
While centralized and integrated public health systems were described as facilitating more timely provincial decision-making and well-coordinated operationalization of those decisions, participants in each province raised concerns about the opacity and perceived politicization of provincial decision making. Participants questioned to what extent decisions were based on scientific advice and how this was weighed against other political interests. In each province, participants questioned to what degree the CMOH was able to act—and in Ontario, effective in acting—as an independent public health advisor to the Minister versus a public health spokesperson for the Minister.
“So you see decisions that are announced, and you're trying to think, well, then how did that align with the [province's public health] measures table, what they recommended? Which is another longstanding Ontario characteristic of having special tables that do things in secrecy” (ON-02).
In each province, the number, and in some areas, types of staff available to respond to COVID-19 (surge capacity) was described as an impediment resulting at least in part from ineffectual investments in public health preceding the pandemic. “Probably the main impediment is resources and staff. I think that probably when you're one system, you're all looking for the same staff, too. And there's a finite number of staff” (AB-22). In Ontario, funding cuts were explicitly described as impeding COVID-19 responses generally and case and contact management specifically. While described less frequently in Alberta compared to Ontario and Québec, the information systems used by public health departments for case and contact management and surveillance early in the pandemic, were described as outdated and not fit for purpose. “It was [from the 1990s] and it wasn't malleable” (QC-13). And when new or upgraded systems needed to be deployed, pre-existing shortages of staff-time for public health operations had to be redirected towards training teams on the new technology. “And so I think those are really the big markers for where the vulnerability in the system is” (ON-14).
Discussing pre-pandemic areas for improvement in the public health system, participants working with First Nations, Inuit and Métis communities in each province described a need for legislation to better clarify the mandate and responsibilities of federal and provincial governments while recognizing First Nations, Inuit and Métis sovereignty in terms of health and wellbeing. Specific to COVID-19 responses, in Ontario, two participants described how challenges accessing provincial COVID-19 funding and case and contact management information systems used by public health units required time intensive workarounds and funding proposal development. In Alberta, two participants described a situation early in the pandemic response, when federal and provincial government agencies as well as AHS were each working with First Nation communities and organizations representing First Nations, on different aspects of the COVID-19 response with limited coordination between them. One specific communication breakdown was seen to have caused setbacks in terms of service delivery and relationship building.
Participants working with Indigenous communities sharing geographic boundaries with Québec described their ability to adapt (including opting-out of) provincial public health measures to their regions’ context as a facilitator of more agile and culturally safe responses. However, this autonomy varied across northern regions and regional Indigenous self-government was described as enabling “easier adaptation of pandemic measures” (QC-15) and enforcement of public health measures. In Alberta, one participant working with a federal agency responsible for advising on-reserve pandemic responses also described their relationship with and operational independence from the Alberta government but recognized authority under the provincial Public Health Act as enabling them to adapt provincial public health measures with advice from First Nation community leaders: “We would have the support, to be honest, of CMOH and our provincial colleagues. Like I think there's an understanding that sometimes [our organization] needs to do it differently” (AB-04).
4. Discussion
Public health professionals and organizations face extraordinary challenges in responding to the COVID-19 pandemic, while striving to continue other essential public health and health care services. These actions and decisions are shaped by the public health system that people work within. Our findings, based on the perspectives of public health leaders in three Canadian provinces, suggest that the more centralized and integrated public health systems in Alberta and Québec were seen to support a more timely and coordinated province-wide COVID-19 response than in Ontario – the most decentralized and least integrated system in Canada. However, the authority afforded to local MOHs in Ontario and public health units’ multi-sectoral relationships were believed to facilitate locally coordinated COVID-19 responses in the absence of an integrated province-wide coordinating structure and delayed provincial decision making. Participants in Alberta and Québec described constraints to the authority of regional MOH which impeded communication and response coordination across sectors within regions. Finally, cross-cutting challenges related to the limited transparency of provincial public health decision-making processes; insufficient prior investment in public health information technology and workforce surge capacity; and the jurisdictional complexities navigated by organizations working with First Nations, Inuit and Métis communities.
Within a wide range of health systems, in response to the COVID-19 pandemic, many nations moved towards more centralized “command and control” emergency response governance structures which concentrated decision making authority among higher levels of government [4]. In the three Canadian provinces we studied, already more centralized and integrated public health systems appeared to enable greater clarity in roles and responsibilities of key actors, cascades of authority and information, and expedience redeploying the workforce and operationalizing COVID-19 response measures. Across jurisdictions in Europe, more centralized health systems were also believed to facilitate more rapid decision making, consistent implementation of public health measures, and redeployment of the health workforce [18]. Despite the advantages of centralization in the context of a pandemic, those who hold the greatest authority are still vulnerable to ineffectual leadership or losing public trust [4]. Decentralization of decision making and administrative authority can thus serve as a fail-safe in the event of ineffectual higher-level leadership [4].
Our findings suggest that decentralized decision-making authority was seen to support effective local responses in Ontario when provincial public health guidance was delayed, perceived to be inadequate, or not coordinated in its delivery across health system sectors. Lacking provincial public health leadership (particularly from within the Ministry of Health), coordination infrastructure, as well as a critical mass of public health expertise were also highlighted as key impediments to Ontario's 2003 SARS outbreak response [38,53]. Public Health Ontario was subsequently established with a mandate “to provide scientific and technical advice and operational support to any person or entity [such as the Government of Ontario] in an emergency or outbreak situation” [54]. However, in our interviews there was limited dialogue around the role of Public Health Ontario specifically. The nature of and factors influencing Public Health Ontario's role during early waves of the COVID-19 pandemic is thus unclear and remains an opportunity for further comparative research with Québec (Institut national de santé publique du Québec) and Alberta (no arms-length public health scientific agency).
Though there were some perceived advantages of the more centralized and integrated public health systems in Alberta and Quebec, there were also some challenges. These included reports of limits to regional MOH authority and misaligned authority (i.e., in relation to other leaders within integrated health system institutions). This limited and misaligned authority was considered to have impeded communicating and coordinating actions across sectors in response to local needs, particularly to respond to and mitigate COVID-19 inequities. Contrary to the theorized benefits of decentralization, our findings did not provide supportive evidence linking MOH authority or local connectivity to more equitable COVID-19 responses in Ontario, even though respondents in Ontario noted the connections with local (municipal and regional) governments, schools and other community partners as enabling potentially more effective pandemic responses. While the limited insights into equity impacts may be a product of interview questions that did not explicitly probe for perceived facilitators and impediments of equitable COVID-19 responses, research also suggests that equity in the outcomes of decentralized systems may depend on moderating factors. These include localized actors having the necessary political authority and institutional capacity (e.g., priorities of leaders, funding, personnel, operational processes) to use resources to promote equity [3]. Within the Canadian context of a public health emergency response, it therefore remains unclear, and it is likely too soon to tell whether decentralized authority and “local connectivity” facilitated more equitable pandemic responses and the role of any moderating factors. These findings highlight a need for research examining what aspects of authority should be strengthened or preserved in order to equip public health leaders to balance the competing priorities of consistent messaging and locally contextualized and equitable public health measures.
Jurisdictional complexity and related health inequities stemming from anti-Indigenous racist policies and gaps in the legislated health mandates of federal and provincial governments are long-standing issues in Canadian health policy [55,56]. Participants in our study highlight how these issues persist and have specifically impacted the emergency response efforts of, and supports requested and made available (or not) to, some organizations working in service of First Nations, Inuit and Métis communities. Given our study team's Western colonial and non-participatory approach to inquiry and narrow recruitment frame, our findings do not offer a comprehensive story about the potential impacts of public health systems structures on COVID-19 responses within the over 228 unique First Nations, Inuit and Métis communities sharing geographies with Alberta, Ontario and Québec. Research detailing the strengths of First Nations, Inuit, and Métis community-specific pandemic responses and how emergency management systems performed through COVID-19 is emerging and underway [57], [58], [59]. Our findings may provide reinforcing evidence of Indigenous self-determination over what we refer to as “public health” decision-making facilitating more effective and culturally safe COVID-19 responses, and the need for legislative or policy solutions addressing long-standing ambiguities in federal, provincial/territorial, and municipal government health mandates pertaining to Indigenous communities [57,60,61].
Concerns raised about the transparency of provincial government decision-making, investment in information systems, and surge capacity constraints suggest that addressing these issues will require changes beyond organizational restructuring of public health systems. These impediments of effective infectious disease emergency management were also highlighted in the largely decentralized public health systems of the United States of America and previously in the Canadian context during SARS outbreak [38,62]. Decision making transparency and proactive investment in public health human resources and information systems may thus be influenced less by public health system organizational structure and more on the political environments dictating patterns of investment and the priorities weighed in government decision-making (e.g., the politics of seeking credit and deflecting blame) [17,63]. Though, arguably navigating these political environments and influencing policy decisions that are considered to be in the best interest of protecting and promoting the public's health is a responsibility of senior public health leaders such as CMOHs [64]. Future research into political factors that necessarily impact pandemic responses, such as “the contested roles” of senior public health leaders and their ability to speak independently may help reveal whether organizational and governance structures could be adapted to better support senior public health leaders to effectively assume their roles [64,65].
A key strength of our study is our purposive recruitment approach of a relatively large sample of leaders with a variety of professional backgrounds and roles in public health across three distinct public health systems. However, our sample may not comprehensively reflect the perspectives of public health leaders across non-medical disciplines nor leaders working within other health system sectors, and we did not have adequate representation of both local and provincial levels of leadership in all provinces to detect any differences in perceptions or experiences depending on whether public health leaders were working in more operational roles versus more strategic ones. Also, our study was not designed from the outset according to First Nations Ownership, Control, Access and Possession or Inuit Tapiriit Kanatami principles for ethical research. To mitigate at least some potential harm from this oversight, the interview transcript and audio recording was offered to participants self-identifying as a First Nations, Inuit or Métis community member. To deepen the relevance and trustworthiness of our results, wide representation of identities and ideas was an implied goal for our methods, however we did not collect data that may have helped assure this (e.g., age, gender, race).
Another limitation relates to the participants we included. Specifically, government officials and more senior health system leaders may have been less willing to participate due to the political sensitivity of COVID-19 responses and availability due to the timing of recruitment (Fig. 1). Also, the candor with which respondents spoke and whether there was over-emphasis on strengths of their systems may have been influenced by their position in relation to more senior leaders. Though by including a range of leaders at various levels of seniority currently and formerly working in public health, we were able to record a range of insights into the perceived challenges and critiques, as well as perceived strengths.
We were also limited in that we could not isolate potential facilitators and impediments of effective COVID-19 responses that were specifically due to centralization versus integration between public health and acute health care and vice versa. Also, our study design did not allow us to capture changes in the perceptions of strengths and weaknesses in pandemic responses over time, and notably during the Omicron phase, which was characterized by heightened transmission and excess mortality, alongside the pressures of mass vaccination. Likely due to the structure of our interview guide, we also did not gain insights into how system structures may have been influenced by past public health emergencies, nor how experiences with COVID-19 may have been similar or different to these past events. Future work may consider addressing these gaps, as well as complementing qualitative insights with other sources of data to examine the impacts of system structures on the variation in pandemic responses. Over time, the pandemic impacted the provinces differently, with the first wave impacting Ontario and Québec more so than the other provinces in terms of COVID-19 cases and deaths [66]. From the period March 2020 to February 2021, while there was a significantly higher rate of deaths directly attributed to COVID-19 in Québec than in all other provinces, there was significantly higher excess mortality in three western provinces (including Alberta) than the rest of the country [67], suggesting future work that looks at these more “objective” assessments of pandemic performance will need to consider a range of indicators.
Finally, the findings of our study may be generalizable to other jurisdictions within Canada, but not necessarily to other countries because of the unique features of Canada's health system and political context (e.g., with a “dualist” yet “cooperative” federation) [68]. Further research could examine whether and how features of de/centralization and integration impacted the emergency responses in other federations with subnational variations in the approach taken to organize public health systems, such as in the United States and Australia. Also, emerging research has uncovered wide variations in the approaches taken to respond to COVID-19 across federal or decentralized systems [69], [70], [71], [72] supporting the need for in-depth analyses within and across countries.
5. Conclusion
Our qualitative multiple case study across three Canadian provinces is among the first to examine the impact of public health system structures, specifically centralization and integration, on COVID-19 pandemic responses from the perspectives of public health leaders. Our findings complement international evidence suggesting that more centralized public health systems may facilitate more rapidly initiated and well-coordinated COVID-19 response measures, though whether these potential benefits persisted over time or can be generalized to other jurisdictions are not known. Theoretical benefits of decentralized systems in ordinary times were also supported to some extent, in the case of enabling timely responses at a local level when provincial leadership was limited. Regardless of organizational and governance structure, the effectiveness and equity of pandemic responses still depends in part on the priorities and politics of those with decision-making authority. Across provinces, participants also indicated that COVID-19 responses were impeded by longstanding health policy challenges obscuring provincial decision-making processes, creating jurisdictional ambiguity impacting First Nations, Inuit and Métis communities, and ineffectual investments in public health. In addition to generating novel insights into potential structural facilitators and impediments of effective COVID-19 responses, our study highlights key areas for future research that may help define how systems can be better designed to support public health leaders in their roles in managing large-scale public health emergencies.
Acknowledgements
We gratefully acknowledge the key informants who generously shared their insights and experiences during the COVID-19 pandemic in Canada. The authors are grateful to Monika Roerig for research coordination, as well as to Dr. Muriel Mac-Seing and Melanie Seabrook for support with data collection in Quebec. Finally, we would like to acknowledge and thank the members of our project advisory group, including Olivier Bellefleur, Greg Marchildon, Susan Chatwood, Mehdi Ammi, Rob Schwartz, and Amélie Quesnel-Vallée, for their support throughout the study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.healthpol.2022.11.011.
Appendix. Supplementary materials
References
- 1.Rechel B, Jakubowski E, McKee M, Nolte E. Conceptual framework. In: organization and financing of public health services in Europe. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2018 [PubMed] [Google Scholar]
- 2.World Health Organization Regional Office For Europe. The 10 essential public health operations [Internet]. [cited 2021 Oct 6]. Available from: https://www.euro.who.int/en/health-topics/Health-systems/public-health-services/policy/the-10-essential-public-health-operations.
- 3.Abimbola S, Baatiema L, Bigdeli M. The impacts of decentralization on health system equity, efficiency and resilience: a realist synthesis of the evidence. Health Policy Plan. 2019;34(8):605–617. doi: 10.1093/heapol/czz055. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Greer SL, Jarman H, Rozenblum S, Wismar M. Who's in charge and why? Centralization within and between governments. Eurohealth. 2020;26(2):99–103. [Google Scholar]
- 5.Costa-Font J, Greer SL. In: Federalism and Decentralization in European Health and Social Care [Internet] Costa-Font J, Greer SL, editors. Palgrave Macmillan UK; London: 2013. Territory and health: perspectives from economics and political science; pp. 13–43. editors. Available from. [DOI] [Google Scholar]
- 6.Peckham S, Exworthy M, Powell M, Greener I. London School of Hygiene and Tropical Medicine; London: 2005. Decentralisation, Centralisation and Devolution in Publicly Funded Health services: Decentralisation as an Organisational Model for Health-Care in England. [Internet]. Decentralisation, Centralisation and Devolution in Publicly Funded Health services: Decentralisation as an Organisational Model for Health-Care in England.https://researchonline.lshtm.ac.uk/id/eprint/3582134 Available from. [Google Scholar]
- 7.Bankauskaite V, Saltman RB. In: Decentralization in Health care: Strategies and Outcomes. Saltman RB, Bankauskaite V, Vrangbæk K, editors. McGraw-Hill, Open University Press (European Observatory on Health Systems and Policies Series); Maidenhead: 2006. Central issues in the decentralization debate; pp. 9–21. editors. [Google Scholar]
- 8.Shankardass K, Renahy E, Muntaner C, O'Campo P. Strengthening the implementation of health in all policies: a methodology for realist explanatory case studies. Health Policy Plan. 2015;30(4):462–473. doi: 10.1093/heapol/czu021. May 1. [DOI] [PubMed] [Google Scholar]
- 9.Diallo T. Five examples of intersectoral action for health at the local and regional level in Canada [Internet] Montréal, Québec: National Collaborating Centre for Healthy Public Policy. 2020:48. http://www.deslibris.ca/ID/10103797 [cited 2020 Jun 18]Available from: [Google Scholar]
- 10.Koivusalo M, Wyss K, Santana P. In: Decentralization in Health care: Strategies and Outcomes. Saltman RB, Bankauskaite V, Vrangbaek K, editors. McGraw-Hill, Open University Press (European Observatory on Health Systems and Policies Series); Maidenhead: 2006. Effects of decentralization and recentralization on equity dimensions of health systems; pp. 189–205. editors. [Google Scholar]
- 11.Bossert TJ, Mitchell AD, Janjua MA. Improving health system performance in a decentralized health system: capacity building in Pakistan. Health Systems & Reform. 2015;1(4):276–284. doi: 10.1080/23288604.2015.1056330. May 19. [DOI] [PubMed] [Google Scholar]
- 12.Bossert TJ, Beauvais JC. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy Plan. 2002;17(1):14–31. doi: 10.1093/heapol/17.1.14. Mar 1. [DOI] [PubMed] [Google Scholar]
- 13.Sumah AM, Baatiema L, Abimbola S. The impacts of decentralisation on health-related equity: a systematic review of the evidence. Health Policy. 2016;120(10):1183–1192. doi: 10.1016/j.healthpol.2016.09.003. Oct 1. [DOI] [PubMed] [Google Scholar]
- 14.Khaleghian P. Decentralization and public services: the case of immunization. Soc Sci Med. 2004;59(1):163–183. doi: 10.1016/j.socscimed.2003.10.013. Jul 1. [DOI] [PubMed] [Google Scholar]
- 15.Besley T, Coate S. National Bureau of Economic Research; Cambridge, MA: 1999. Centralized versus Decentralized Provision of Local Public Goods: A Political Economy Analysis [Internet]http://www.nber.org/papers/w7084 (Working Paper Series). Available from: [Google Scholar]
- 16.World Health Organization . WHO Regional Office for South-East Asia; New Delhi: 2006. Working Together for Health [Internet]https://apps.who.int/iris/handle/10665/205774 [cited 2021 Nov 11]. Available from: [Google Scholar]
- 17.Greer SL, Falkenbach M, Jarman H, Löblová O, Rozenblum S, Williams N, et al. Centralisation and decentralisation in a crisis: how credit and blame shape governance. Eurohealth. 2021;27(1):36–40. [Google Scholar]
- 18.Waitzberg R, Hernández-Quevedo C, Bernal-Delgado E, Estupiñán-Romero F, Angulo-Pueyo E, Theodorou M, et al. Early health system responses to the COVID-19 pandemic in Mediterranean countries: a tale of successes and challenges. Health Policy [Internet] 2021 doi: 10.1016/j.healthpol.2021.10.007. https://pubmed.ncbi.nlm.nih.gov/34711444 Oct 12Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor E, Bailit M, Dyer MB, Hacker K. Vol. 5. Robert Wood Johnson Foundation; 2016. (Integrating Public Health and Health Care: Getting beyond the Theory). [Google Scholar]
- 20.World Health Organization . World Health Organization; Geneva: 2018. Technical Series on Primary Health Care [Internet]https://www.who.int/docs/default-source/primary-health-care-conference/linkages.pdf [cited 2021 Oct 6]. Available from: [Google Scholar]
- 21.Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, et al. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Family Practice [Internet] 2021 doi: 10.1093/fampra/cmaa142. Feb 15 [cited 2021 Jul 11];(cmaa142). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wynn A, Moore KM. Integration of primary health care and public health during a public health emergency. Am J Public Health. 2012/09/20 ed. 2012;102(11):e9–12. doi: 10.2105/AJPH.2012.300957. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donaldson L. United Kingdom Department of Health; London: 2006. On the State of Public health: Annual report of the Chief Medical Officer 2005 [Internet] p. 81.https://www.researchgate.net/publication/319998930_On_the_state_of_public_health_Annual_report_of_the_Chief_Medical_Officer_2005 Available from: [Google Scholar]
- 24.Moloughney B. Toronto Public Health; Toronto, ON: 2016. The Impacts on the Public Health Function with Integration with Regionalized Healthcare Systems [Internet] p. 14.https://www.toronto.ca/legdocs/mmis/2016/hl/bgrd/backgroundfile-88527.pdf Available from: [Google Scholar]
- 25.Barker P, Church J. Revisiting health regionalization in Canada. Int J Health Serv. 2016;47(2):333–351. doi: 10.1177/0020731416681229. [DOI] [PubMed] [Google Scholar]
- 26.Public Health Agency of Canada. COVID-19 daily epidemiology update: total case rate by province and territory [Internet]. 2021 [cited 2021 Dec 14]. Available from: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html?stat=rate&measure=total&map=pt#a2.
- 27.Public Health Agency of Canada. COVID-19 daily epidemiology update: death rate by province and territor [Internet]. 2021 [cited 2021 Dec 14]. Available from: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html?stat=rate&measure=deaths&map=pt#a2.
- 28.Smith RW, Allin S, Luu K, Li J, Jarvis T, Thomas M, et al. Profiles of Public Health Systems in Canada: Alberta. Montréal: National Collaborating Centre for Healthy Public Policy; In press.
- 29.Wankah P, Guillette M, Dumas S, Couturier Y, Gagnon D, Belzile L, et al. Reorganising health and social care in Québec: a journey towards integrating care through mergers. London J Prim Care. 2018;10(3):48–53. doi: 10.1080/17571472.2018.1453957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poirier LR, Pineault R, Gutièrrez M, Vien LP, Morisset J. Institut National de Santé Publique du Québec; Québec: 2019. Évaluation De La Mise En œuvre du Programme national De Santé Publique 2015-2025 – Analyse de L'impact Des Nouveaux Mécanismes De Gouvernance [Internet] p. 64.https://www.inspq.qc.ca/sites/default/files/publications/2552_evaluation_gouvernance_programme_national_sante_publique_2015_2025.pdf [cited 2020 Jul 29]Available from: [Google Scholar]
- 31.Fiset-Laniel J, Guyon A, Perreault R, Strumpf EC. Public health investments: neglect or wilful omission? Historical trends in Quebec and implications for Canada. Can J Public Health. 2020:1–6. doi: 10.17269/s41997-020-00342-1. Jun 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arpin E, Smith RW, Cheung A, Thomas M, Luu K, Li J, et al. National Collaborating Centre for Healthy Public Policy; Montréal: 2022. Profiles of Public Health Systems in Canada: Québec [Internet]https://ccnpps-ncchpp.ca/docs/2022-Profiles-of-Public-Health-Systems-in-Canada-Quebec.pdf Available from. [Google Scholar]
- 33.Office of the Auditor General of Ontario 3.08: LHINs—Local health integration networks. In: Annual Report [Internet]. Toronto: Government of Ontario; 2015:56. https://www.auditor.on.ca/en/reports_en/en15/3.08en15.pdf Available from: [Google Scholar]
- 34.Ontario Ministry of Health . Queen's Printer for Ontario; Toronto, ON: 2019. Discussion Paper: Public Health Modernization; p. 16. [Google Scholar]
- 35.Smith RW, Allin S, Rosella L, Luu K, Thomas M, Li J, et al. National Collaborating Centre for Healthy Public Policy; Montréal: 2021. Profiles of Public Health Systems in Canada: Ontario [Internet]https://ccnpps-ncchpp.ca/profiles-of-public-health-systems-in-canadian-provinces-and-territories/ Available from: [Google Scholar]
- 36.Jones E, MacDougall H, Monnais L, Hanley J, Carstairs C. Royal Society of Canada; Ottawa, ON: 2021. Beyond the COVID-19 crisis: Building on Lost Opportunities in the History of Public Health [Internet] pp. 3–30.https://rsc-src.ca/sites/default/files/History%20PB_EN.pdf Available from: [Google Scholar]
- 37.Campbell A. Commission to Investigate the Introduction and Spread of SARS in Ontario; Toronto: 2006. Spring of fear: the SARS Commission [Internet] pp. 1–62.http://www.archives.gov.on.ca/en/e_records/sars/report/v1.html Available from. [Google Scholar]
- 38.Naylor D, Basrur S, Bergeron MG, Brunham RC, Butler-Jones D, Dafoe G, et al. Health Canada; Ottawa, ON: 2003. Learning from SARS: Renewal of Public Health in Canada [Internet]https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/sars-sras/pdf/chapter8-e.pdf [cited 2021 Oct 6]. Available from: [Google Scholar]
- 39.Fierlbeck K, Hardcastle L. In: Vulnerable: The Law, Policy and Ethics of COVID-19 [Internet] Flood C, MacDonnell V, Philpott J, Thériault S, Venkatapuram S, editors. University of Ottawa Press; Ottawa, ON: 2020. Have the post-SARS reforms prepared us for COVID-19? Mapping the institutional landscape; pp. 31–48.https://muse.jhu.edu/book/76885 editors. Available from. [Google Scholar]
- 40.World Health Organization. Self-assessment tool for the evaluation of essential public health operationsin the WHO European region. Copenhagen, Denmark; 2015.
- 41.Creswell JW. 4th ed. SAGE Publications; Thousand Oaks: 2014. Research design: qualitative, quantitative, and Mixed Methods Approaches. [Google Scholar]
- 42.Kelly LM, Cordeiro M. Three principles of pragmatism for research on organizational processes. Methodol Innov. 2020;13(2) May 1. [Google Scholar]
- 43.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–544. doi: 10.1007/s10488-013-0528-y. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rechel B, Jakubowski E, McKee M, Nolte E. Organization and financing of public health services in Europe. Health policy series, no. 50. European Observatory on Health Systems and Policies. 2018 [PubMed] [Google Scholar]
- 45.Rechel B, Maresso A, Sagan A, Hernandez-Quevedo C, Williams G, Richardson E, et al. WHO Regional Office Europe on behalf of the European Observatory on Health Systems and Policies; Copenhagen: 2018. Organization and Financing of Public Health Services in Europe: Country Reports. [PubMed] [Google Scholar]
- 46.Finlay L. Reflexivity: an essential component for all research? Br J Occup Therap. 1998;61(10):453–456. Oct 1. [Google Scholar]
- 47.Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Houghton C, Casey D, Shaw D, Murphy K. Rigour in qualitative case-study research. Nurse Res. 2013;20(4):12–17. doi: 10.7748/nr2013.03.20.4.12.e326. [DOI] [PubMed] [Google Scholar]
- 49.Braun V, Clarke V. Using thematic analysis in psychology. Qualit Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 50.Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res. 2016;26(13):1802–1811. doi: 10.1177/1049732316654870. Nov 1. [DOI] [PubMed] [Google Scholar]
- 51.Yin RK. 5th ed. SAGE Publications Inc.; Los Angeles: 2014. Case Study research: Design and Methods; p. 282. [Google Scholar]
- 52.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. Sep 16. [DOI] [PubMed] [Google Scholar]
- 53.Campbell A. Government of Ontario; Toronto: 2004. The SARS Commission Interim Report: SARS and Public Health in Ontario [Internet]http://www.archives.gov.on.ca/en/e_records/sars/report/Interim_Report.pdf [cited 2022 Jan 30]. Available from: [DOI] [PubMed] [Google Scholar]
- 54.Government of Ontario Ontario agency for health protection and promotion act [Internet] Sect. 2007;6(24) https://www.ontario.ca/laws/view Available from: [Google Scholar]
- 55.Allan B, Smylie J. the Wellesley Institute; Toronto, ON: 2015. First Peoples, Second Class treatment: The role of Racism in the Health and Well-Being of Indigenous peoples in Canada. [Internet]https://www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf [cited 2021 Oct 6]. Available from: [Google Scholar]
- 56.Lavoie JG. Policy silences: why Canada needs a national first nations, Inuit and Métis health policy. Null. 2013;72(1):22690. doi: 10.3402/ijch.v72i0.22690. Jan 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barnabe C, Montesanti S, Sarin C, White T, Bartel R, Henderson R, et al. Propelled by the pandemic: responses and shifts in primary healthcare models for indigenous peoples. Healthcare Policy. 2022;17(4):48–55. doi: 10.12927/hcpol.2022.26826. May 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smith CR, Enns C, Cutfeet D, Alfred S, James N, Lindbeck J, et al. COVID-19 in a remote first nations community in British Columbia, Canada: an outbreak report. CMAJ. 2021;9(4):E1073. doi: 10.9778/cmajo.20210054. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clark T, Best O, Wilson D, Power T, Phillips-Beck W, Graham H, et al. COVID-19 among indigenous communities: case studies on indigenous nursing responses in Australia, Canada, New Zealand, and the United States. Nurs Praxis Aotearoa N Z. 2021:71–83. Dec 1. [Google Scholar]
- 60.Craft A, McGregor D, Hewitt J. In: Vulnerable: The Law, Policy and Ethics of COVID-19 [Internet] Flood C, MacDonnell V, Philpott J, Thériault S, Venkatapuram S, editors. University of Ottawa Press; Ottawa, ON: 2020. COVID-19 and first nations’ responses; pp. 49–65.https://muse.jhu.edu/book/76885 editors. Available from: [Google Scholar]
- 61.Mashford-Pringle A, Skura C, Stutz S, Yohathasan T. What we heard: indigenous peoples and COVID-19 [Internet]. Ottawa, ON: Public Health Agency of Canada; 2021 p. 32. Available from: https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19/indigenous-peoples-covid-19-report/cpho-wwh-report-en.pdf.
- 62.DeSalvo K, Hughes B, Bassett M, Benjamin G, Fraser M, Galae S, et al. National Academy of Medicine; Washington, DC: 2021. Public Health COVID-19 Impact Assessment: Lessons Learned and Compelling Needs. [Internet] (NAM Perspectives). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rosella LC, Wilson K, Crowcroft NS, Chu A, Upshur R, Willison D, et al. Pandemic H1N1 in Canada and the use of evidence in developing public health policies – a policy analysis. Soc Sci Med. 2013;83:1–9. doi: 10.1016/j.socscimed.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fafard P, McNena B, Suszek A, Hoffman SJ. Contested roles of Canada's chief medical officers of health. Can J Public Health. 2018;109(4):585–589. doi: 10.17269/s41997-018-0080-3. Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brubacher LJ, MdZ Hasan, Sriram V, Keidar S, Wu A, Cheng M, et al. Investigating the influence of institutions, politics, organizations, and governance on the COVID-19 response in British Columbia, Canada: a jurisdictional case study protocol. Health Res Policy Syst. 2022;20(1):74. doi: 10.1186/s12961-022-00868-5. Jun 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Allin S, Fitzpatrick T, Marchildon GP, Quesnel-Vallée A. The federal government and Canada's COVID-19 responses: from ‘we're ready, we're prepared’ to ‘fires are burning. Health Economics, Policy and Law. 2021/06/22 ed. 2022;17(1):76–94. doi: 10.1017/S1744133121000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.McGrail K. Excess mortality, COVID-19 and health care systems in Canada. CMAJ. 2022;194(21):E741. doi: 10.1503/cmaj.220337. May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Poirier J, Michelin J. Facing the coronavirus pandemic in the Canadian Federation: Reinforced dualism and muted cooperation? In: Steytler N, editor. Comparative Federalism and COVID-19 [Internet]. London: Routledge; 2021. p. 200–19. Available from: https://www.taylorfrancis.com/chapters/oa-edit/10.4324/9781003166771-14/facing-coronavirus-pandemic-canadian-federation-johanne-poirier-jessica-michelin.
- 69.Greer SL, King EJ, da Fonseca EM, Peralta-Santos A. The comparative politics of COVID-19: the need to understand government responses. Global Public Health. 2020;15(9):1413–1416. doi: 10.1080/17441692.2020.1783340. [DOI] [PubMed] [Google Scholar]
- 70.Hegele Y, Schnabel J. Federalism and the management of the COVID-19 crisis: centralisation, decentralisation and (non-)coordination. West Eur Polit. 2021;44(5–6):1052–1076. Sep 19. [Google Scholar]
- 71.OECD . Organisation for Economic Co-operation and Development; Paris: 2020. The Territorial Impact of COVID-19: Managing the Crisis Across Levels of Government [Internet] pp. 1–94.https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/ [cited 2022 Oct 23]Available from. [Google Scholar]
- 72.Steytler N. Comparative Federalism and Covid-19: Combating the Pandemic [Internet] Routledge; New York: 2021. Federalism under pressure: federal ‘Health’ factors and ‘Co-morbidities; pp. 396–422.https://www.routledge.com/Comparative-Federalism-and-Covid-19-Combating-the-Pandemic/Steytler/p/book/9780367763961 [cited 2022 Oct 23]Available from: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.