Abstract
The COVID-19 pandemic might have affected older adults’ personal and general views on aging (VoA) because they were frequently, particularly during the early phase of the pandemic, portrayed as a homogeneous, vulnerable group in the media and in public debates. Also, their higher risk of severe COVID-19 disease progression as well as other pandemic-related stressors and restrictions might have impacted how older adults perceive their own aging. In this study, it was examined to which extent middle-aged and older adults’ personal and general VoA changed due to the pandemic by distinguishing between normative age-graded change across multiple measurement occasions and potentially pandemic-specific history-graded change. Multiple VoA indicators (personal VoA: attitude toward own aging, subjective age, awareness of age-related change [gains and losses]; general VoA: domain-specific age stereotypes) of 423 German adults aged 40 years and older were assessed across three pre-pandemic measurement occasions (2012, 2015, 2017) and one occasion after the pandemic’s outbreak (summer 2020). Normative age-graded changes and pandemic-specific changes were estimated and compared using longitudinal multilevel regression analyses. Both perceived age-related gains and age-related losses decreased between 2012 and 2017, but increased thereafter between 2017 and 2020. Further, the overall trend toward less positive attitude toward own aging slowed down from 2017 to 2020. There was also a slight trend toward younger subjective ages from 2017 to 2020. For most age stereotypes, pandemic-specific trends indicated a shift toward more negative stereotypes. These findings suggest that pandemic-specific changes in VoA are multidirectional, comprising perceptions of both losses and gains.
Keywords: subjective age, attitude toward own aging, age stereotypes, awareness of age-related change, COVID-19, normative history-graded life event
During the COVID-19 pandemic, older adults were frequently viewed and portrayed as a homogeneous and highly vulnerable risk group (Ayalon et al., 2021; Kessler & Bowen, 2020), which may have affected how they perceived their own aging. Such portrayals were based on the fact that the risk of severe disease when infected with COVID-19 increases with age, which is empirically confirmed and uncontroversial (e.g., Karagiannidis et al., 2020; Nachtigall et al., 2020; Robert-Koch-Institut, 2020). However, one-sided portrayals of older adults’ vulnverability could also be a trigger promoting less favorable views of aging (VoA). Moreover, such vulnerability-focused portrayals also neglect older adults’ heterogeneity (e.g., Nelson & Dannefer, 1992) as well as their strengths and resilience, particularly during this ongoing pandemic (Lind et al., 2020; Röhr et al., 2020). Also, the pandemic can be regarded as a “multidimensional and potentially toxic stress factor” (Brakemeier et al., 2020), and the impact of stress on VoA is well established (Bellingtier et al., 2017; Kotter-Grühn et al., 2015; Schafer & Shippee, 2010; Wettstein et al., 2021).
This study addresses the research question whether the pandemic impacted older adults’ VoA due to psychological processes such as stereotype embodiment (Levy, 2009), age stereotype internalization/”contamination” (Rothermund & Brandtstädter, 2003; Weiss & Kornadt, 2018) or age-group dissociation (Weiss & Lang, 2012). The umbrella term of VoA is used in this article to cover both personal and general views on aging. Personal VoA refer to individuals’ perceptions, behavioral experiences, and subjective interpretations related to their individual process of growing older. In contrast, general VoA refer to age stereotypes that are non-self-referential (Faudzi et al., 2019) and represent socially shared beliefs related to aging and older adults as a social group (Hess, 2006; Kornadt & Rothermund, 2012; Weiss & Lang, 2012). Of major note, mounting evidence points to the relevance of more negative VoA for lower well-being, health, and longevity (Alonso Debreczeni & Bailey, 2021; Chang et al., 2020; Kotter-Grühn et al., 2009; Levy et al., 2020; Tully-Wilson et al., 2021; Westerhof et al., 2014) as well as increased costs for health care (Levy et al., 2020).
It is conceptually as well as empirically useful to consider the COVID-19 pandemic through the lenses of the macro-model of developmental influences (Baltes et al., 2006; Diehl & Wahl, 2020). The model distinguishes between three major influences on human development, i.e., (1) normative age-graded influences (i.e., “biological and environmental aspects that, because of their dominant age correlation, shape individuals in relatively normative ways for all individuals;” Baltes et al., 2006, p. 586); (2) normative history-graded influences (i.e., “biological and environmental aspects that may make ontogenetic development different across historical cohort and periods;” Baltes et al., 2006, p. 587); ; and (3) non-normative (idiosyncratic) influences (e.g., individual life events). The focus of this article is on the COVID-19 pandemic as an unexpected history-graded influence that started in 2020, and that may have - in addition to normative age-graded influences - affected developmental processes Of note, both influences on development occur in parallel, and “none of these patterns of […] influences is likely to operate independently from the other” (Baltes et al., 2006, p. 587). Research on the COVID-19 pandemic as a developmentally relevant historical event may build on the classic study by Elder (1974) on the impact of the Great Depression as another far-reaching historical event on individuals’ quality of life at the beginning of the 1930’s.
Inspired by Elder’s (1974) study as well as Baltes et al.’s (2006) macro-model of developmental influences, the focus of this study is on the development of VoA in middle-aged and older adults under COVID-19 pandemic conditions. A major gap in the previous empirical research relevant for VoA changes due to the pandemic is the lack of longitudinal data comprising multiple pre-pandemic measurement occasions across several years. However, only the availability of such multiple pre-pandemic occasions allows the separation of normative age-graded change in VoA from potentially pandemic-induced change in terms of the described macro-model (Baltes et al., 2006; Diehl & Wahl, 2020). This study is based on 8-year longitudinal data on VoA comprising three pre-pandemic waves and one peri-pandemic wave. This allows to compare two models: (1) a “normative age-graded model” that specifies only an age-normative change component; and (2) a “normative age-graded change plus history-graded pandemic-change model” that comprises both an age-graded normative change component across the entire 8-year period and a pandemic-specific change component. The second model is based on the assumption that age-graded change and history-graded change co-occur and are not mutually exclusive, which corresponds to the main assumptions of the macro-model of developmental influences (Baltes et al., 2006; Diehl & Wahl, 2020). The pandemic-specific change component is indicated by intra-individual deviations from the general (normative) slope at the 2020 measurement occasion. In addition, taking a much needed distinction of multiple VoA into account, trajectories of both personal VoA (i.e., self-perceptions of aging or self-referential VoA; Faudzi et al., 2019) and general VoA (i.e., age stereotypes or non-self-referential VoA) are investigated. To the best of the authors’ knowledge, this has not been done in any previous study on the effects of the COVID-19 pandemic.
Major Indicators of Views on Aging: Overview
VoA are multidimensional (Kornadt et al., 2019; Spuling et al., 2019). This section provides a detailed description of major indicators of both personal and general VoA. This distinction between different VoA is important, as they might differ with regard to their susceptibility to pandemic-driven changes.
Personal Views on Aging.
A widely used unidimensional indicator of personal VoA is attitude toward own aging (ATOA; Lawton, 1975; Miche et al., 2014; exemplary item: “Things keep getting worse as I get older”). Across multiple studies, ATOA has shown a clear downward trajectory toward an increasingly negative attitude from midlife to old and advanced old age (Kleinspehn-Ammerlahn et al., 2008; Kotter-Grühn et al., 2009; Miche et al., 2014; Siebert et al., 2020).
One of the most frequently applied unidimensional indicators of personal VoA is felt or subjective age (“How old do you feel?”; Kastenbaum et al., 1972; Pinquart & Wahl, 2021). Cross-sectional as well as meta-analytic work indicates that most middle-aged and older individuals feel younger than they are (Pinquart & Wahl, 2021; Rubin & Berntsen, 2006; Uotinen et al., 2006).
Finally, a more recent multidimensional way to measure personal VoA is the concept of awareness of age-related change (AARC; Diehl & Wahl, 2010). The AARC approach assumes that individuals form a cognitive representation of perceived changes such as changed behavior, changed performance, or changed experiences that they attribute to getting older. The AARC conceptualization also posits that this cognitive representation involves both positive and negative perceptions (Diehl et al., 2021). In a recent study with a large sample of over 900 adults aged 80 years and older who were observed over a 2-year period, AARC-Gains showed a significant decrease and AARC-Losses a significant increase (Kaspar et al., 2021).
General Views on Aging.
Studies addressing age-associated change in general VoA have remained rare. Kornadt and Rothermund’s (2011) findings supported the multidimensionality of age stereotypes; Specifically, age stereotypes concerned with family as well as with physical and mental fitness, health and appearance were more positive in older age groups, but age differences were less clear in areas such as friends and acquaintances or leisure activities, social or civic commitments. The age group x stereotype domain interaction was of medium effect size.
In conclusion, existing research suggests multidirectionality of normative, age-related trajectories within and between personal and general VoA (see also Diehl et al., 2021). Next, it is discussed what may happen if these age-graded trends of personal and general VoA encounter the COVID-19 pandemic as a critical history-graded occurrence.
The COVID-19 Pandemic and Personal/General Views on Aging
Starting in early 2020, the COVID-19 pandemic created an unexpected, highly stressful and challenging situation for individuals around the globe, including older adults (Brakemeier et al., 2020; Heid et al., 2021; World Health Organization (WHO), 2020). With regard to VoA, negative stereotyping and ageist commentaries in the (social) media might have, on the one hand, reinforced negative views of older adults. That is, negative stereotypes and ageist commentaries in the (social) media (Jimenez-Sotomayor et al., 2020; Lichtenstein, 2021; Meisner, 2021) may have reinforced views on aging as an exclusive process of increasing health risks and helplessness (Ayalon et al., 2021; Ehni & Wahl, 2021) and may have promoted “COVID ageism” (Kessler & Bowen, 2020). Overall, this might have resulted in more negative –both general and personal - VoA.
This reasoning seems plausible because, according to stereotype embodiment theory (Levy, 2009), age stereotypes are internalized and “contaminate” or affect how individuals perceive their own aging (see Brothers et al., 2021; Rothermund & Brandtstädter, 2003). Also, there may be other aspects related to the pandemic that elicit more negative VoA. In general, higher levels of stress tend to be related to less favorable VoA (Bellingtier et al., 2017; Kotter-Grühn et al., 2015; Schafer & Shippee, 2010; Wettstein et al., 2021), and the pandemic situation represents a significant stressor (Brakemeier et al., 2020; Heid et al., 2021). Also, stressors during the pandemic – the necessity to re-organize work and life (home office) and child-care as long as schools and child-care facilities were closed, or increased social isolation due to physical distancing rules – might have led to more negative VoA.
On the other hand, pandemic-related public discourse about old age, as well as the age-related increase in the risk of severe COVID-19 disease progression when infected, might have infused the tendency in older adults of “age-group dissociation,” thus psychologically distancing themselves from the group of those being “old” (“They are old, but I feel younger;” Weiss & Lang, 2012). Such a psychological distancing effect might have provoked self-enhancement in reaction to the COVID-19 threat and may have made older adults feel younger and think more positively about their own aging or at least about certain aspects thereof. Of note in this context, individuals in the second half of life seem to avoid the social identity of being an older adult whenever this social identity has a negative connotation – which might have been the case during the early phase of the COVID-19 crisis. In particular, the persisting “old-age-as-a-risk-group” debate might have negatively infused of what “being old” means. Further, the COVID-19 pandemic might have generally made negative age stereotypes more salient in the lives of older adults. As a result, individuals might have increased the psychological distance between themselves and same-aged peers as a means to protect a positive self-image at large (Weiss & Freund, 2012).
From a theoretical point of view, it could thus be the case that both perceptions of losses (e.g., more negative general VoA) and gains (e.g., feeling younger during the pandemic as an expression of age-group dissociation) in VoA co-occur as a consequence of the pandemic. Such a co-occurrence would also reflect the multidimensionality and multidirectionality of VoA.
At the empirical level, a major background for this study is the finding that positive VoA seem to facilitate psychosocial adaptation to the pandemic (Avidor et al., 2021; Kornadt et al., 2021; Losada-Baltar et al., 2021; Shrira et al., 2020). However, regarding the potential pandemic-reactivity of individuals’ VoA (i.e., proneness of VoAs to pandemic-caused changes) only very few longitudinal studies are available so far. A study by Terracciano et al. (2021) included U.S. participants 18 years and older and investigated changes in subjective age based on measurement occasions before the COVID-19 outbreak in late January 2020, during the early outbreak in late March 2020, and again in late April 2020. Interestingly, the trajectory of participants’ subjective ages ratings followed a concave curve, with participants overall feeling younger during the outbreak in late March 2020 than in late January and late April. As the authors argued in accordance with the psychological distancing or age-group dissociation effect mentioned earlier, psychological distancing might have become an adaptive mechanism, particularly when the COVID-19 infection rates were dramatically rising in the U.S. in March 2020, but less so when infection rates reached a plateau starting in late April 2020. Also, in a study based on a Russian sample of adults (Berezina & Rybtsov, 2021), individuals’ subjective age in mid-2020 was on average younger than in 2019. However, based on their approach, age-related vs. potentially pandemic-related change in aging expectations cannot be disentangled. Kornadt et al. (2021) assessed older adults from Luxembourg in June and October 2020. Perceived ageism at the first measurement occasion was associated with an increase in self-perceptions of aging as a social loss between June and October 2020. Wettstein and Wahl (2021) investigated trajectories of ATOA and subjective age between 2008 and summer 2020 among middle-aged and older adults. They found that mean-level change toward more negative ATOA became steeper between 2017 and 2020 compared to the change prior to 2017, which might be due to the onset of the pandemic in 2020. In contrast, no evidence was found for an impact of the pandemic on within-person trajectories of subjective age.
In conclusion, findings on the COVID-19 pandemic’s impact on adults’ VoA have remained mixed in nature and limited in scope. In particular, longitudinal assessment intervals of most empirical studies were quite short and did not allow for the estimation of normative (age-graded) trajectories in VoA prior to the pandemic. However, given that no control condition of individuals who were not affected by the pandemic is available due to the history-graded occurrence and normative character of the COVID-19 pandemic, such estimation of normative age-graded trends in VoA prior to the pandemic’s outbreak is key to disentangling normative age-related change from pandemic-related change. In addition, most of prior research did not sufficiently consider the multidimensionality of VoA (i.e., indicators of personal and general VOA were not included simultaneously), as well as their potential multidirectionality. This has limited researchers’ ability to examine the possibility of co-occurring losses and gains in VoA in reaction to the pandemic.
The Present Study
Against this background, the overall aim of this study was to examine whether observed normative 8-year trajectories in multiple VoA were affected by the COVID-19 pandemic and in which way. Individuals in midlife and old age were considered, because VoA have been found to reveal different developmental change patterns in these life periods, with change in VoA already observable from midlife on (e.g., Miche et al., 2014). Moreover, stereotype embodiment theory (Levy, 2009) predicts that negative VoA become increasingly self-relevant from midlife into old age. Therefore, the effects of the pandemic on VoA might be different for middle-aged vs. older adults.
Study hypotheses were as follows:
Personal VoA, except subjective age, show a negative pandemic change effect in that expectable normative decline trajectories will get steeper as a result of the experience of the COVID-19 pandemic and its consequences. In contrast, with respect to subjective age, there might be an age-group dissociation effect as indicated by younger subjective ages during the pandemic (see Terracciano et al., 2021).
General VoA show a negative pandemic change effect in that expectable normative stability or positive trajectories may not have gotten more positive or may even have become more negative as a result of the COVID-19 pandemic.
Based on exploratory analyses, potential predictors of pandemic-related changes in VoA were also investigated. Given the considerable heterogeneity of middle-aged and older adults in general (Nelson & Dannefer, 1992), not all individuals can be expected to reveal the same extent of pandemic-related change in personal and general VoA (e.g., Kornadt et al., 2021; Wettstein & Wahl, 2021). Rather, there may be individual resources and risk factors that affect the extent and direction of VoA changes related to COVID-19. Thus, chronological age, gender, education, self-rated health, and depressive symptoms were examined as potential predictors of pandemic-related changes in personal and general VoA.
Methods
Sample
Data from four measurement occasions were available for analyses (T1 in 2012, n = 423; T2 in 2015, n = 356; T3 in 2017, n = 299; T4 in June-September 2020, n = 233). Data were collected at T1-T3 by means of a paper-and-pencil questionnaire sent out to participants with paid return service. Data at T4 were, to a large extent, collected online (79%); the rest was based on a paper-pencil procedure identical to prior waves. The order of questions/items in the online version and in the paper-and-pencil version of the questionnaire was identical for comparability reasons. The online version was first pilot-tested within the project team. It was then applied to 30 study participants in order to ensure that the online format was functional and easy to use. Those who participated online in 2020 did not significantly differ from those filling out paper-and-pencil questionnaires with regard to baseline age, the proportion of women, and self-rated health (see Table 1). However, the online participants had significantly higher levels of education and lower depressive symptoms scores than the paper-and-pencil participants, and both effects were of medium effect size. Regarding personal VoA, groups did not significantly differ with regard to subjective age and AARC-losses at any of the four measurement occasions, but the online group had significantly more favorable ATOA scores at three of the four measurement occasions as well as significantly lower AARC-loss scores across all measurement occasions than the paper-and-pencil sub-sample. These differences were of small to medium effect size. For general VoA, only two differences were statistically significant. The online group had more favorable age stereotypes regarding health and appearance than the paper-and-pencil group, both in 2012 and in 2020. These differences were of small to medium effect size.
Table 1.
Sample Description
| Total sample (n = 423) | T4 Paper-Pencil Sample (n = 184) | T4 Online Sample (n = 49) | Effect Size of Group Difference (Cohen’s d or φ) | |
|---|---|---|---|---|
|
|
||||
| M±SD or n (%) | M±SD or n (%) | M±SD or n (%) | ||
| Age (2012) | 62.94 ±11.84 | 62.72±12.08 | 59.15±9.08 | d = .44 |
| Women | 272 (64.3%) | 128 (69.6%) | 36 (73.5%) | φ = −.04 |
| Education (years) | 11.53±1.96 | 11.87±1.691 | 10.88±2.102 | d = .63 |
| Self-Rated Health (2012) a | 2.12 ± 0.85 | 2.10±0.86 | 2.06±0.88 | d = .04 |
| Depressive Symptoms (2012) | 7.60± 5.07 | 7.13±4.701 | 9.69±5.932 | d = .61 |
| Personal Views on Aging | ||||
| Subjective Age (2012) b | −0.13±0.10 | −0.14± 0.10 | −0.12± 0.12 | d = .03 |
| Subjective Age (2015) b | −0.12±0.11 | −0.12± 0.10 | −0.11± 0.14 | d = .03 |
| Subjective Age (2017) b | −0.11±0.09 | −0.11± 0.09 | −0.11±0.10 | d = .00 |
| Subjective Age (2020) b | −0.11±0.12 | −0.11±0.11 | −0.11±0.142 | d = .02 |
| ATOA (2012) | 3.54±1.47 | 3.69±1.421 | 3.09±1.502 | d = .45 |
| ATOA (2015) | 3.47±1.54 | 3.66±1.441 | 2.84±1.682 | d = .60 |
| ATOA (2017) | 3.33±1.57 | 3.44±1.52 | 2.97±1.73 | d = .33 |
| ATOA (2020) | 3.32±1.56 | 3.43±1.551 | 2.93±1.562 | d = .34 |
| Age-Related Gains (2012) | 3.29±0.76 | 3.30±0.76 | 3.26±0.75 | d = .05 |
| Age-Related Gains (2015) | 3.19±0.73 | 3.19±0.68 | 3.21±0.63 | d = .03 |
| Age-Related Gains (2017) | 3.19±0.73 | 3.17±0.72 | 3.21±0.70 | d = .05 |
| Age-Related Gains (2020) | 3.61±0.61 | 3.63±0.60 | 3.55±0.61 | d = .12 |
| Age-Related Losses (2012) | 2.16±0.74 | 2.02±0.691 | 2.31±0.742 | d = .38 |
| Age-Related Losses (2015) | 1.93±0.67 | 1.82±0.601 | 2.19±0.752 | d = .53 |
| Age-Related Losses (2017) | 2.02±0.71 | 1.89±0.671 | 2.24±0.742 | d = .47 |
| Age-Related Losses (2020) | 2.20±0.66 | 2.146±0.641 | 2.38±0.712 | d = .32 |
| General Views on Aging | ||||
| Age Stereotypes Family and Partnership (2012) | 4.91±1.56 | 4.80±1.46 | 4.35±1.46 | d = .33 |
| Age Stereotypes Family and Partnership (2015) | 5.14±1.55 | 5.041± 1.43 | 4.89±1.48 | d = .11 |
| Age Stereotypes Family and Partnership (2017) | 5.29±1.39 | 5.31±1.30 | 5.00±1.51 | d = .25 |
| Age Stereotypes Family and Partnership (2020) | 5.11±1.49 | 5.19±1.39 | 4.79±1.83 | d = .30 |
| Age Stereotypes Leisure (2012) | 5.33±1.36 | 5.23±1.41 | 4.81±1.38 | d = .32 |
| Age Stereotypes Leisure (2015) | 5.33±1.37 | 5.40±1.26 | 5.10±1.41 | d = .25 |
| Age Stereotypes Leisure (2017) | 5.44±1.32 | 5.42±1.31 | 5.27±1.39 | d = .12 |
| Age Stereotypes Leisure (2020) | 5.44±1.33 | 5.51±1.27 | 5.15±1.49 | d = .30 |
| Age Stereotypes Personality (2012) | 4.89±1.44 | 4.83±1.32 | 4.56±1.63 | d = .21 |
| Age Stereotypes Personality (2015) | 5.02±1.49 | 4.92±1.41 | 4.83±1.35 | d = .06 |
| Age Stereotypes Personality (2017) | 5.08±1.43 | 5.09±1.40 | 4.90±1.45 | d = .14 |
| Age Stereotypes Personality (2020) | 5.02±1.35 | 5.09±1.28 | 4.73±1.56 | d = .30 |
| Age Stereotypes Health and Appearance (2012) | 4.62±1.39 | 4.58±1.361 | 4.14±1.422 | d = .34 |
| Age Stereotypes Health and Appearance (2015) | 4.80±1.41 | 4.72±1.34 | 4.35±1.33 | d = .29 |
| Age Stereotypes Health and Appearance (2017) | 4.78±1.40 | 4.81±1.44 | 4.70±1.39 | d = .08 |
| Age Stereotypes Health and Appearance (2020) | 4.59±1.39 | 4.71±1.291 | 4.10±1.662 | d = .49 |
Note. M = mean; SD = standard deviation; ATOA = attitude toward own aging.
Different superscripts (1,2) indicate significant group differences.
Lower values indicate better self-rated health.
Subjective age was computed as proportional discrepancy score (Rubin & Berntsen, 2006), corresponding to the extent felt age deviates from chronological age (subjective age = [felt age – chronological age]/chronological age), with lower values indicating a younger subjective age.
Approval for wave 4 of the longitudinal data with the study title “Awareness of Age-Related Change / Subtitle: Opportunities and Challenges of Digital Technologies to Support Older Adults’ Mobility Applying a User-Centered Design Approach” used in this research was received from the Institutional Ethics Review Board of the Faculty of Behavioral and Empirical Cultural Sciences of Heidelberg University (AZ Wahl 2020 1/1). Wave 3 was approved by the same board with the study title “Awareness of Age-Related Change / Subtitle: Mindful vs. Mind Full: Dispositional Cognitive Strategies Moderate the Association Between Views of Aging and Subjective Well-Being” with a letter dating from February 17, 2017 (no protocol no.). Waves 1–2 were approved by the Colorado State University (CSU) Institutional Review Board (IRB) protocol #10–2080H based on a formal cooperation between Heidelberg University and CSU. All individuals were informed that they could change their minds and withdraw their agreement at any time. Contact data of the participants were stored locally on a university computer as a data file with password protection. Study participants were also informed that their data were used and analyzed exclusively for scientific purposes (and not for commercial purposes), and that their data were not shared with any third parties. All data were analyzed with personal identifiers removed. Individuals provided written informed consent prior to study participation. Data are archived for ten years, in agreement with the recommendations of the German Research Foundation. This study was designed and organized in line with all rules and guidelines specified in the “Leitlinien zur Sicherung guter wissenschaftlicher Praxis”, 2019 [GOOD RESEARCH PRACTICE. Guidelines for Safeguarding Good Research Practice, 2019; access via: https://wissenschaftliche-integritaet.de/en/code-of-conduct/) by the German Research Foundation.
The sample description is provided in Table 1. Study participants were between 40 and 98 years old at baseline (M = 62.94 years, SD = 11.84 years). About two thirds (64.3 %, n = 272) of the sample were women. Observations per participant ranged from one to four (M = 3.10, SD = 1.08; individuals with one study participation: n = 53 [12.5 %]; individuals with two study participations: n = 68 [16.1 %]; individuals with three study participations: n = 86 [20.2 %]; individuals with four study participations: n = 216 [51.1%]).
Limited evidence for selective attrition effects was found when comparing the 233 returners in 2020 with those 190 lost during the 8-year observational interval. Differences between these groups with regard to study variables at baseline were all of small effect size, with the exception of the age difference, which was of medium effect size (d = .68). Participants who still took part in 2020 were significantly younger than participants who dropped out of the study before 2020 (mean difference > 6 years). The proportion of women was significantly higher among those still participating in 2020 (70.4%) compared to dropouts (56.8%). Those who dropped out before 2020 had significantly higher AARC-loss scores at baseline, and significantly higher (i.e., more positive) scores on stereotypes regarding family and partnership as well as health and appearance than those who still participated in 2020.
Measures
Personal Views on Aging
Attitude Toward Own Aging (ATOA).
Attitude toward own aging was measured by the subscale of the Philadelphia Geriatric Morale Scale (Lawton, 1975). This subscale has five items (e.g., ‘Things keep getting worse as I get older’) which are answered with either “yes” or “no.” A sum score is computed, ranging from 0 to 5, with higher scores indicating a more favorable ATOA (Cronbach’s αs 2012–2020: .68; .71; .72; .69, respectively).
Subjective Age (SA).
A single-item question (“How old do you feel most of the time?”) was used for the assessment of SA. A proportional discrepancy score between felt age and chronological age was computed (subjective age = [felt age − chronological age] / chronological age; Rubin & Berntsen, 2006) in order to age standardize the SA scores and facilitate their interpretation. A negative proportional discrepancy score indicates a SA that is younger than a person’s chronological age, whereas a positive score indicates a SA that is older than an individual’s chronological age. The scores of 17 outliers (i.e., scores more than 3 standard deviations above or below the mean, which is a common cutoff criterion in subjective age research; e.g., Stephan et al., 2020) were replaced with missing values to avoid biased estimates.
Awareness of Age-Related Change (AARC).
AARC gains and losses were measured with the 10-item AARC short-form questionnaire (AARC-10 SF; Kaspar et al., 2019). Each item begins with “With my increasing age, I realize that…” and describes either a negative (e.g., “…my mental capacity is declining.”) or a positive aging experience (e.g., “…I appreciate relationships and people much more.”) in a specific behavioral domain. Items are answered on a 5-point Likert scale ranging from 1 (not at all) to 5 (very much). Mean scores of AARC gains and losses were computed, with a range from 1 to 5, and with higher scores indicating more AARC gains/losses (Cronbach’s αs: AARC gains 2012–2020: .68; .65; .68; .57, respectively; AARC losses 2012–2020: .78; .77; .80; .78, respectively).
General Views on Aging
The multidimensional, domain-specific age stereotype scale (Kornadt & Rothermund, 2011) was used to measure study participants’ stereotypes regarding older people across different domains. The domains family and partnership; leisure; personality and way of living; health and appearance were included and assessed at all measurement occasions in this study. For each item, an 8-point rating scale was provided that contrasts two poles of opposing statements ranging from negative to positive. For instance, one item belonging to the family and partnership domain is (1) “Old persons have many conflicts in their relationship with family” vs. (8) “Old persons have a harmonious relationship with their family.” Each of the subscales had 3 items, with the exceptions of personality and way of living (4 items). A mean score for each subscale was computed, ranging from 1–8, with higher scores indicating more favorable age stereotypes (Cronbach’s αs: Family and partnership 2012–2020: .76; .82; .75; .81, respectively; leisure 2012–2020: .82; .85; .84; .85, respectively; personality and way of living 2012–2020: .77; .80; .78; .77, respectively; health and appearance 2012–2020: .74; .75;.78; .77, respectively).
Covariates
Chronological age, gender, education, self-rated health, and depressive symptoms (all assessed in 2012) were included as potential confounding variables to check for the robustness of a pandemic-specific change effect across the different VoA. All these variables have been documented to be associated with interindividual differences in intraindividual changes in VoA (Dutt et al., 2018). Moreover, they are also components of the theoretical framework by Diehl et al. (2021). These authors distinguished between different antecedents of VoA, such as awareness of age-related change, including socio-demographic antecedents (age, gender, education), biological/health-related antecedents (self-rated health), and psychological antecedents (depressive symptoms). Education was measured as the number of years of schooling. Self-rated health was measured using a single-item question (“How would you rate your health in general?”) with response options ranging from 1 (excellent) to 5 (poor). A 10-item version of the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977) was used to assess depressive symptoms. The items assess mood and functioning during the past week (e.g., “I could not get going”). The response scale ranges from 1 (Rarely/None of the time) to 4 (Most/All of the Time). A sum score of depressive symptoms in 2012 was computed, with higher scores indicating more severe depressive symptoms (Cronbach’s α in 2012: .85).
Statistical Analyses
Longitudinal multilevel regression models (Hox & Kreft, 1994; Ram & Grimm, 2015) were computed to investigate trajectories of the personal (ATOA, SA, AARC gains and losses) and the general VoA (domain-specific age stereotypes across four domains) between 2012 and 2020. Based on these longitudinal multilevel regression models, which are an extension of common regression analyses, a level (usually the score at baseline) and a slope/trajectory component for each individual is estimated. Interindividual variation in intercept and slope, denoted as random effects in longitudinal multilevel regression models, is estimated, and predictors of interindividual differences in intercept and slope can be specified and tested by means of multilevel modelling (the specific multilevel equations from the analyses are documented in the Online Supplemental Material, Part 1.
The maximum number of observations per individual was 4 for each outcome, but not all individuals took part at all measurement occasions and thus not each study participant provided 4 nonmissing scores on all outcomes. It was therefore decided to specify linear trajectories only. A reliable estimation of nonlinear (quadratic) change might require more measurement occasions per individual, and from an empirical point of view, most existing evidence is in support of linear, rather than quadratic, changes in views of aging over time and age (Kleinspehn-Ammerlahn et al., 2008; Kotter-Grühn et al., 2009; Miche et al., 2014; Uotinen et al., 2006). Time was clocked in months since 2012.
To investigate whether there was a potentially COVID-19-induced change in VoA between the last pre-COVID measurement occasion in 2017 and the last measurement occasion in June-September 2020, when the first infection wave of COVID-19 was still ongoing, models were specified which included a specific change component between 2017 and 2020 in addition to a specification of a general and normative linear change between 2012 and 2020. This change component was specified by generating a time-varying dummy variable (see Online Supplemental Material, part 1) that was set to 0 for all individuals at all measurement occasions prior to 2020 and was restricted to 1 for all individuals in 2020. The regression coefficient of this dummy variable was specified as random effect (unless the estimation did not converge and required omitting the random effect), based on the assumption that intra-individual pandemic-induced change in VoA most likely reveals large inter-individual variation in both direction and magnitude. This pandemic dummy variable, indicating a potential period effect in 2020, is – in a strict sense – not a slope component in its own, but an intra-individual deviation in 2020 from the general slope. This approach, which is adopted from other studies addressing COVID-19 effects (Kivi et al., 2020; Wettstein & Wahl, 2021), was considered as the most appropriate one, as alternative approaches such as piecewise models would require setting a change point in 2017 – which is not exactly when one would expect the COVID-19 effect to set in – and would estimate each of the two slope components based on only two measurement occasions only (slope 1: 2012 and 2015; slope 2: 2017 and 2020). Age-related change and pandemic-related change in VoA were thus considered as two co-occurring change components, which is consistent with the theorizing of the macro-model of developmental influences (Baltes et al., 2006; Diehl & Wahl, 2020). In general, it is not very plausible that the onset of the pandemic stops or replaces age-related change with pandemic-related change. Rather, age-related and pandemic-related change can be expected to operate in parallel.
These models of normative age-related plus pandemic-related change were compared with more parsimonious models that only specified one general linear age-related change component between 2012 and 2020 without an additional 2017–2020 pandemic-related change component. Comparisons were performed by contrasting the Bayesian information criterion (BIC) scores (Kass & Raftery, 1995; 2 (ΔBIC) ≥ 2: positive evidence in favor of the model with a lower BIC score; 2 (ΔBIC) ≥ 6: strong evidence; 2 (ΔBIC) > 10: very strong evidence) of the competing models and by inspecting the relative reduction in residual variance (R²; computed according to Xu, 2003) obtained by each model.
If the model including pandemic-specific change was superior in model fit to a model without this additional change component, and if the random effect of the pandemic-specific change was significant, the role of potential determinants accounting for inter-individual variation in intra-individual COVID-19-driven change was additionally investigated. These potential determinants were chronological age, gender, education, self-rated health, and depressive symptoms. Additional technical details of how the COVID-19 pandemic change effect was modeled can be found in Online Supplemental Material (part 1).
The corresponding author confirms that the data on which this study builds on will be made available at any time. Please contact the corresponding author. This study was not preregistered.
Results
Pandemic-Specific Change in Personal Views on Aging
The study hypotheses were that personal and general VoA would reveal a pandemic-related shift toward more negative attitudes, with the exception of subjective age which was expected to change toward feeling younger as a psychological reaction to the pandemic (i.e., dissociation from an undesirable age group). These expectations were confirmed for most personal VoA –except for ATOA and AARC-gains, which revealed a pandemic-related increase (or – for ATOA – stability) rather than a decrease, and for subjective age, for which a pandemic-related change component did not result in a better fit. Regarding general VoA, most of them were characterized by a pandemic-related change toward more negative age stereotypes, which is in line with the study expectations.
Table 2 shows the estimates of the competing models (pandemic-specific change vs. no pandemic-specific change) for all personal VoA (ATOA, SA, AARC gains and AARC losses). The mean-level trajectories according to these models, as well as the extent of inter-individual variability in intra-individual pandemic-specific change (as far as they could be estimated), are illustrated in Figures 1 and in Supplemental Figure 1.
Table 2.
Longitudinal Multilevel Regression Models of Changes in Personal Views on Aging
| Model Estimates | ATOA linear change | ATOA linear change plus pandemic-related change | Subjective agea linear change | Subjective age linear change plus pandemic-related change | AARC gains linear change | AARC gains linear change plus pandemic-related change | AARC losses linear change | AARC losses linear change plus pandemic-related change |
|---|---|---|---|---|---|---|---|---|
| Fixed Regression Coefficients: | ||||||||
| Intercept [SE] | 3.533*** [0.069] | 3.549*** [0.070] | −0.130*** [0.001] | −0.132*** [0.001] | 3.199*** [0.035] | 3.284*** [0.036] | 2.061*** [0.034] | 2.119*** [0.035] |
| Linear slope 2012–2020 [SE] | −0.003** [0.001] | −0.004** [0.001] | 0.000*** [0.000] | 0.000*** [0.000] | 0.003*** [0.000] | −0.002** [0.001] | 0.000 [0.000] | −0.003*** [0.001] |
| Pandemic-specific slope 2017–2020 [SE] | 0.109 [0.126] | −0.014* [0.007] | 0.540*** [0.058] | 0.379*** [0.049] | ||||
| Random Variances: | ||||||||
| Variance Intercept [SE] | 1.290*** [0.143] | 1.268*** [0.154] | 0.008*** [0.000] | 0.008*** [0.001] | 0.322*** [0.037] | 0.342*** [0.036] | 0.370*** [0.035] | 0.379*** [0.037] |
| Variance Linear Slope [SE] | 0.000 [0.000] | 0.000 [0.000] | 0.000 [0.000] | 0.000 [0.000] | 0.000 [0.000] | 0.000 [0.000] | 0.000* [0.000] | 0.000** [0.000] |
| Variance Pandemic-Specific Slope [SE] | 0.706 [0.497] | 0.066 [0.082] | ||||||
| Residual Variance [SE] | 0.956*** [0.055] | 0.886*** [0.070] | 0.003*** [0.000] | 0.003*** [0.000] | 0.259*** [0.015] | 0.229*** [0.013] | 0.171*** [0.010] | 0.147*** [0.012] |
| BIC | 4,383.7 | 4,401.8 | −2,582.8 | −2,580.7 | 2,581.7 | 2,506.8 | 2,299.9 | 2,262.4 |
| R² | .06 | .12 | 0.20 | 0.21 | .05 | .16 | .09 | .21 |
Note. Time unit is months (since 2012). R² was computed according to Xu (2003). ATOA = attitude toward own aging. The intercepts correspond to the estimated VOA score at baseline (i.e., in 2012). “Linear slope 2012–2020” indicates the mean-level change between 2012 and 2020 in each subjective VoA indicator. The “Pandemic-specific slope 2017–2020“ component indicates the mean-level change between 2017 and 2020 in each subjective VoA indicator that occurred in addition to the general linear change (2012–2020). Models of linear change vs. of linear plus pandemic-related change were compared based on their BIC (Kass & Raftery, 1995) and R² scores. The components “Variance Linear Slope” and “Variance Pandemic-Specific Slope” indicate, if statistically significant, that there is substantial inter-individual variability in the intra-individual trajectories.
p < .05;
p < .01;
p < .001.
Subjective age was computed as proportional discrepancy score (Rubin & Berntsen, 2006), corresponding to the extent felt age deviates from chronological age (subjective age = [felt age – chronological age]/chronological age), with lower values indicating a younger subjective age.
Figure 1. Change in Subjective Views on Aging between 2012 and 2020.
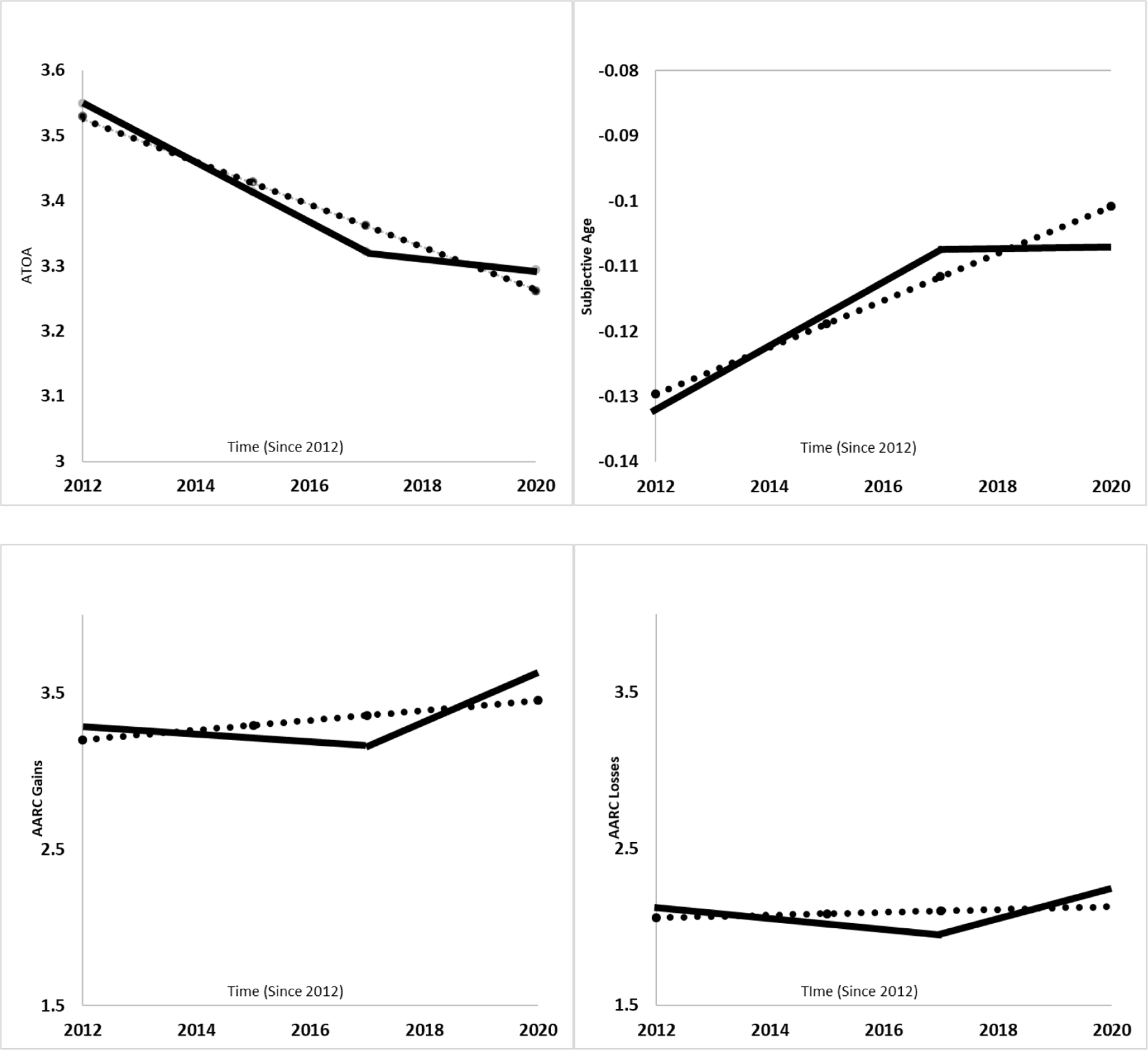
Note. Time unit is years (since 2012). ATOA = attitude toward own aging. Subjective age was computed as a proportional discrepancy score (Rubin & Berntsen, 2006), corresponding to the extent felt age deviates from chronological age (subjective age = [felt age – chronological age]/chronological age), with scores indicating a person’s felt age as a percentage of their chronological age. The solid lines correspond to the mean-level change in VoA according to a model with an additional pandemic-specific change component between 2017 (pre-pandemic measurement occasion) and 2020 (time of the first COVID-19 infection wave) in addition to an overall linear change component across the entire time period of 8 years. The dashed lines correspond to the mean change in VoA according to a model with only one linear change component across the entire 8-year time period.
Attitude Toward Own Aging.
Regarding ATOA, a model assuming a linear change between 2012 and 2020 indicated a significant mean-level decline of 0.003 points per month, amounting to an average annual change of about 0.036 points toward more negative ATOA. In relation to the ATOA score range (0–5), this can be considered as a change of small effect size. The estimated annual mean-level ATOA decline between 2012 and 2020 was steeper and amounted to approximately 0.048 points in a model that additionally specified a pandemic-specific change component. However, in that model, the additional change component between 2017 and 2020 was positive (although the fixed effect itself was not statistically significant), indicating that ATOA remained on average stable between 2017 and 2020, but declined before 2017 (see Figure 1). Although the BIC score indicated a better model fit for the model without a pandemic-specific change component (general change model: BIC = 4,383.7; general change plus pandemic-specific change model: BIC = 4,401.8), the relative reduction in residual variance was higher for the pandemic-specific model (general change model: R² = .06; general change plus pandemic-specific change model: R² = .12). In conclusion, there was at least modest evidence in favor of a pandemic-specific change toward more stable ATOA. The predicted mean ATOA score in 2020 differed only by 0.03 points between both models and was higher in the pandemic-specific change model, which is a very small difference, given the ATOA score range from 0 to 5. In contrast, the predicted change between 2017 and 2020 in ATOA was more discrepant between models. Specifically, the average decline between 2017 and 2020 of about 0.10 points in the general change model was more than three times steeper than the predicted ATOA decline between 2017 and 2020 by .03 points in the pandemic-specific change model.
The random effect of the pandemic-specific slope component failed to reach statistical significance (p = .08), but as shown in Supplemental Figure 1, there was some inter-individual variation in that change. For almost 60% of the sample, the pandemic-specific change indicated a shift toward more positive ATOA, whereas, for more than one third, this estimated change component was negative.
Subjective Age.
Regarding SA, in a model that only specified one general linear change component, mean-level change was significant, with individuals feeling on average 0.4% less young from one year to the next: On average, individuals felt about 13% younger than they were in 2012, whereas in 2020, they felt on average 10% younger than they were.
A model with a pandemic-specific change component in addition to the overall change component also indicated a significant mean-level increase in SA (about 0.5% per year) and additionally a significant mean-level pandemic-specific change toward a younger SA from 2017 to 2020. However, inter-individual variation in the intra-individual pandemic-related change had to be set to zero to achieve model convergence. Comparing both models, the general-change-only model predicted a shift toward an older subjective age between 2017 and 2020 (by 1.1 % of the subjective age discrepancy score, that is from feeling 11.2 % younger than their age in 2017 to feeling 10.1 % younger in 2020). In contrast, in the pandemic-related change model, SA remained stable (i.e., individuals feeling on average 10.7% younger than their age in both 2017 and 2020). The BIC score was in favor of the general change model (BIC general change model: −2,582.8; BIC general plus pandemic-related change model: − 2,580.7), and R² estimates were very similar in both models (R² general change model: .204; R² general plus pandemic-related change model: .207). Evidence in support of pandemic-specific change of subjective age was thus weak, as a more parsimonious model assuming a general change in SA between 2012 and 2020 yielded a model fit that was not worse compared to a model that additionally specified a pandemic-specific change component.
Awareness of Age-Related Gains and Losses.
AARC gains showed a slight mean-level increase in a model specifying only one general change component. Specifically, the mean annual increase amounted to 0.03 points, from a mean AARC gains score of 3.2 in 2012 to a score of 3.45 in 2020. In relation to the score range of AARC gains (1–5), this corresponds to a small increase over time. In a model specifying a pandemic-slope component in addition to a general change component, mean annual change in AARC gains was negative rather than positive, with an annual decline of about 0.03 points, thus again of small effect size. However, this trend was reversed by the significant positive mean-level pandemic-specific change component, leading to a mean-level increase in ATOA gains between 2017 and 2020 (see Figure 1). To achieve model convergence, inter-individual variation in the pandemic-specific change component was set to 0. Model fit indicators were in favor of this pandemic-related change model (BIC general change model: 2,581.7; BIC general plus pandemic-related change model: 2,506.8; R² general change model: .05; R² general plus pandemic-related change model: .16). In the pandemic-specific change model, the mean-level increase in AARC gains between 2017 and 2020 (change = 0.468) was more than 4 times the size than in the model without a pandemic-related slope component specified (change = 0.108).
AARC losses showed, according to a model with a general change component only, a mean-level increase which failed to reach statistical significance (p = .06). The mean annual increase in AARC losses was small and amounted to about 0.008 points (on the AARC loss score range from 1 to 5), with a mean AARC losses score of 2.06 in 2012 and of 2.13 in 2020. In a model that specified a pandemic-related change component in addition to a general change component, mean-level general change in AARC losses was negative rather than positive. On average, AARC losses decreased by 0.03 points per year. Additionally, there was a significant pandemic-specific change component that indicated an increase in AARC losses between 2017 and 2020. Although the random effect of this component was not significant, there was some inter-individual variability in the extent of this pandemic-specific change, as illustrated in Supplemental Figure 1. However, for more than 99% of the sample, pandemic-specific change was positive, although the exact magnitude varied between individuals. Comparing both models, the mean increase in AARC losses between 2017 and 2020 (0.271) was about 10 times steeper in the pandemic-related change model compared to the general change model (0.024). The model fit in terms of BIC and R² was better for the pandemic-specific change model than for the general change model (BIC general change model: 2,299.9; BIC general plus pandemic-related change model: 2,262.4; R² general change model: .09; R² general plus pandemic-related change model: .21).
Pandemic-Specific Change in General Views on Aging
The model comparisons for the four age stereotype domains are shown in Table 3 and illustrated in Figure 2 and Supplemental Figure 2. In a model specifying only one general change component, age stereotypes of family and partnership showed a significant mean-level increase. Specifically, they changed by approximately 0.05 points per year toward more positive stereotypes (predicted mean score in 2012: 4.99; predicted mean score in 2020: 5.38), which is a change of small effect size (score range of age stereotypes family and partnership: 1–8). In a model with an additional pandemic-specific change component, there was also a significant mean-level general change toward the positive, even larger in size than in the comparison model without an additional pandemic-related change component (mean annual increase by 0.1 points per year). However, the additional pandemic-specific change component indicated a trend in the opposite direction, with a significant mean-level decline (2017–2020), indicating a change toward more negative age stereotypes with regard to family and partnership from 2017 to 2020. That is, whereas these age stereotypes became on average more positive between 2017 and 2020 in a general change model, they became more negative during these three years in a pandemic-specific change model. The random effect of the pandemic-specific change component had to be restricted to 0 to obtain model estimates. Comparing the model fit of both models, the pandemic-specific change model resulted both in a better BIC score as well as a (slightly) higher R² value (BIC general change model: 4,326.7; BIC general plus pandemic-related change model: 4,315.6; R² general change model: .09; R² general plus pandemic-related change model: .11). This model thus was superior to a general-change-only model.
Table 3.
Longitudinal Multilevel Regression Models of Changes in General Views on Aging (Age Stereotypes)
| Model Estimates | Family & Partnership linear change | Family & Partnership linear change plus pandemic-related change | Leisure linear change | Leisure linear change plus pandemic-related change | Personality linear change | Personality linear change plus pandemic-related change | Health & Appearance linear change | Health & Appearance linear change plus pandemic-related change |
|---|---|---|---|---|---|---|---|---|
| Fixed Regression Coefficients: | ||||||||
| Intercept [SE] | 4.992*** [0.071] | 4.913*** [0.074] | 5.207*** [0.062] | 5.194*** [0.066] | 4.917*** [0.068] | 4.885*** [0.070] | 4.692*** [0.065] | 4.636*** [0.067] |
| Linear slope 2012–2020 [SE] | 0.004*** [0.001] | 0.009*** [0.001] | 0.002** [0.000] | 0.003* [0.001] | 0.002** [0.001] | 0.004** [0.001] | 0.000 [0.000] | 0.004** [0.001] |
| Pandemic-specific slope 2017–2020 [SE] | −0.516*** [0.123] | −0.008 [0.124] | −0.215 [0.123] | −0.374** [0.115] | ||||
| Random Variances: | ||||||||
| Variance Intercept [SE] | 1.363*** [0.154] | 1.401*** [0.155] | 0.878*** [0.087] | 0.879*** [0.087] | 1.246*** [0.139] | 1.276*** [0.153] | 1.142*** [0.126] | 1.118*** [0.139] |
| Variance Linear Slope [SE] | 0.000* [0.000] | 0.000* [0.000] | 0.000 [0.000] | 0.000* [0.000] | 0.000 [0.000] | 0.000 [0.000] | ||
| Variance Pandemic-Specific Slope [SE] | 0.669 [0.490] | 0.500 [0.433] | ||||||
| Covariance Intercept-Linear Slope [SE] | −0.002 [0.002] | −0.003 [0.002] | −0.002 [0.001] | −0.003** [0.003] | −0.001 [0.001] | −0.002 [0.002] | ||
| Cov. Intercept-Pandemic-Specific Slope [SE] | −0.0554 [0.193] | −0.024 [0.170] | ||||||
| Cov. Lin. Slope Pandemic-Specific Slope [SE] | −0.007 [0.005] | −0.005 [0.005] | ||||||
| Residual Variance [SE] | 0.999*** [0.059] | 0.968*** [0.057] | 1.000*** [0.048] | 1.000*** [0.048] | 0.917*** [0.054] | 0.837*** [0.068] | 0.820*** [0.048] | 0.749*** [0.061] |
| BIC | 4,326.7 | 4,315.6 | 4,176.0 | 4,181.6 | 4,228.1 | 4,245.0 | 4,118.6 | 4,129.7 |
| R² | .09 | .11 | 0.01 | 0.01 | .06 | .14 | .05 | .13 |
Note. Time unit is months (since 2012). R² was computed according to Xu (2003). ATOA = attitude toward own aging.
p < .05;
p < .01;
p < .001.
Figure 2. Change in General Views on Aging (Age Stereotypes) Between 2012 and 2020.
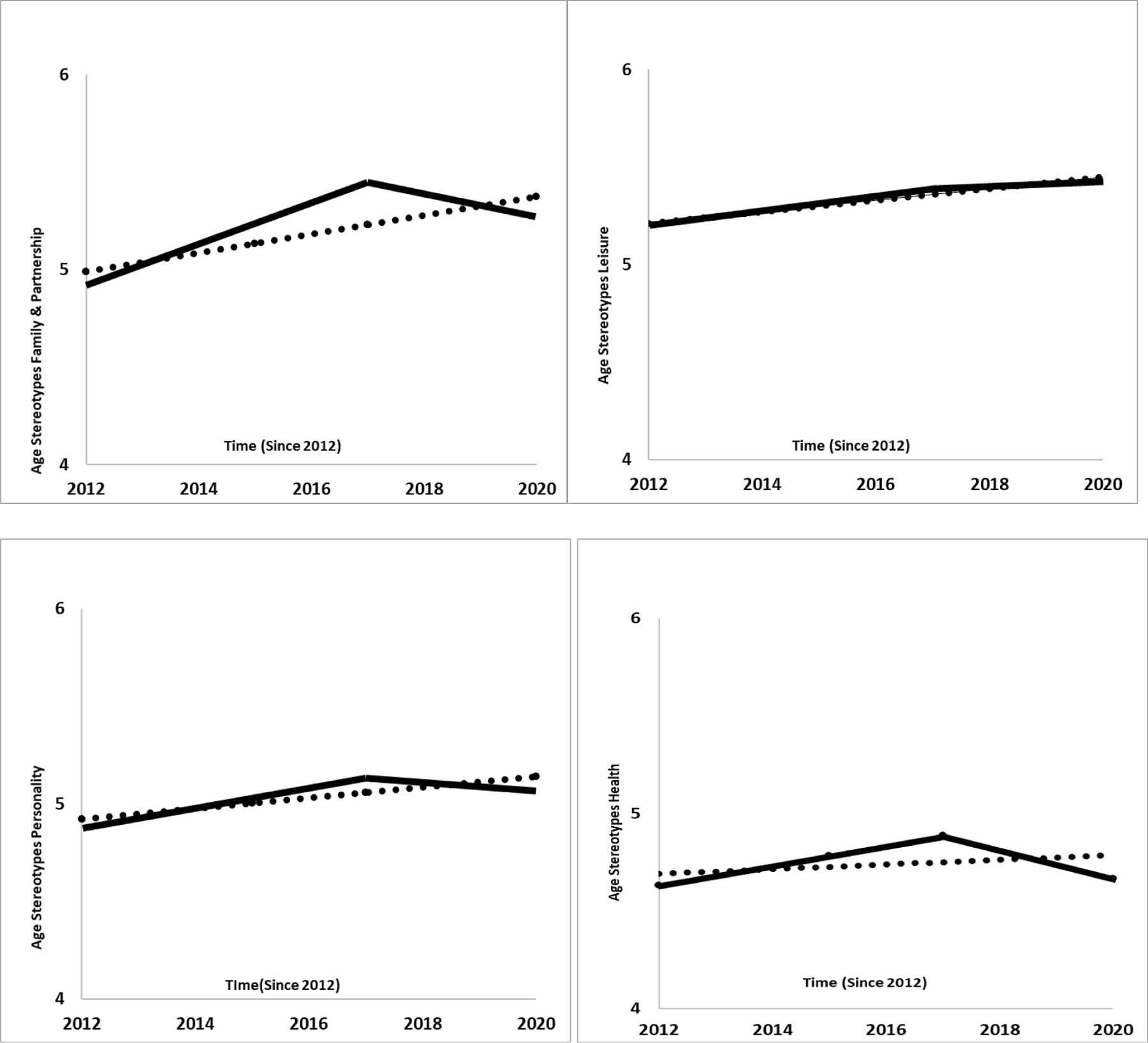
Note. Time unit is years (since 2012). The solid lines correspond to the mean-level change in VoA according to a model with an additional pandemic-specific change component between 2017 (pre-pandemic measurement occasion) and 2020 (time of the first COVID-19 infection wave) in addition to an overall linear change component across the entire time period of 8 years. The dashed lines correspond to the mean change in VoA according to a model with only one linear change component across the entire 8-year time period.
According to the general change model, age stereotypes in the domain of leisure showed a significant but small annual mean-level increase (i.e., a trend toward more positive stereotypes about leisure) by about 0.03 points (again on the scale ranging from 1–8). To obtain converging estimates, inter-individual variation in this change component (i.e., the random change component) had to be restricted to zero. In a model including an additional pandemic-specific change component, there was also a significant general annual mean-level increase in age stereotypes regarding leisure (by about 0.04 points), but the pandemic-specific change component was negative, thus indicating a shift toward more negative stereotypes. However, this component was not significant, and its random effect had to be set to 0 to obtain model parameter estimates. When comparing both models, BIC was better in the general-change-only model (BIC general change model: 4,176.0; BIC general plus pandemic-related change model: 4,181.6), whereas proportional reduction of residual variance was of equal size (R² = .01) in both models. There was thus no convincing evidence supporting pandemic-specific change for age stereotypes regarding leisure.
Age stereotypes with regard to personality and way of living significantly increased (i.e., changed toward the positive) in the general-change-only model by about 0.02 points per year (on the age stereotype scale ranging between 1 and 8), which can be regarded as an increase of small effect size. In a model that additionally specified a pandemic-specific change component, these age stereotypes also revealed a significant general annual mean-level change toward the positive (by about 0.05 points per year). However, there was also a negative, though not significant (p = .08) mean-level pandemic-specific change component. In consequence, the change between 2017 and 2020 corresponded, on average, to a change toward less favorable age stereotypes with regard to personality and way of living. Although the BIC score was better in the more parsimonious, general-change-only model (BIC general change model: 4,228.1; BIC general plus pandemic-related change model: 4,245.0), proportional reduction in residual variance was larger for the pandemic-related change model (R² general change model: .06; R² general plus pandemic-related change model: .14), which can be regarded as modest evidence in favor of the pandemic-related change model. The random effect of the pandemic-specific change component was not significant (p = .09), but – as Supplemental Figure 2 shows – there was some inter-individual variability in the extent of pandemic-specific change. Notably, for more than 80% of the study sample, this change was a shift toward more negative age stereotypes in the domain of personality and way of living, with the magnitude of this negative shift varying between individuals.
Finally, age stereotypes regarding health and appearance remained, on average, stable in a model with only one normative (age-graded) change component. In contrast, in a model additionally specifying a pandemic-specific change component, they became more favorable over time (by 0.05 points per year, which is a small effect) as part of the normative change component but changed toward higher negativity between 2017 and 2020. Although this model had a poorer BIC score compared to a general-change-only model (BIC general change model: 4,118.6; BIC general plus pandemic-related change model: 4,129.7), it contributed to a higher proportional reduction in residual variance (R² general change model: .05; R² general plus pandemic-related change model: .13). This can be interpreted as at least modest evidence in support of pandemic-specific change in these age stereotypes. The random effect of the pandemic-specific change component was not significant, but – as Supplemental Figure 2 shows – there were some inter-individual differences in the extent of pandemic-specific change. However, for more than 94 % of the sample, this change pointed toward less favorable age stereotypes regarding health and appearance between 2017 and 2020, whereas for less than 6%, the change indicated a shift toward more positive stereotypes.
Additional Analyses
All analyses of pandemic-specific changes were repeated by additionally controlling for age, gender, education, self-rated health, and depressive symptoms. These covariates were not only controlled for in all models, they were also specified as predictors of the pandemic-specific change component (only in those models where the random component of this change was not set to 0). Details are reported in the Online Supplemental Material (Part 2). To summarize the findings, the estimates of pandemic-specific changes remained significant or non-significant when controlling for covariates, with one exception (i.e., mean-level pandemic-specific change in age stereotypes regarding health was no longer significant when controlling for the covariates). Moreover, only one effect of the covariates on pandemic-specific changes was significant: Pandemic-specific ATOA change was less positive or even negative among those with more years of education. Age was not a significant predictor of pandemic-related change in any of the VoA measures investigated.
Finally, to investigate the robustness of the study findings, repeated-measure analyses of variance were computed for each outcome as an alternative method to longitudinal multilevel regression models. Although this method does not allow for a direct separation of age-related vs. pandemic-related change, the within-subject effect of time was significant for all outcomes, confirming that there is substantial change in VoA over time. For all personal VoA measures, the measure in 2020 was significantly different from the previous assessments, which is in line with the interpretation of a pandemic-related change effect. Effects of time were largest for AARC-gains and AARC-losses. For general VoA, the within-person effect of time was also significant across all measures, but the measures in 2020 were not significantly different from the previous assessment. The reason for these non-significant differences could be that the increase in age stereotypes toward higher positivity from 2012 to 2017 was reversed from 2017 to 2020. Therefore, mean scores of age stereotypes in 2020 were in a similar range than age stereotypes averaged across 2012, 2015, and 2017 (for details regarding the repeated-measure ANOVA findings, see Online Supplemental Material, Part 3).
Discussion
This study examined whether different domains of middle-aged and older adults’ personal and general VoA showed any pandemic-specific changes, in addition to normative age-graded change observed across eight years (2012–2020). A major distinction in this study has been between personal VoA (self-perceptions of aging or self-referential views on aging; Faudzi et al., 2019) and general VoA (age stereotypes or non-self-referential views on aging).
Pandemic-Related Change in Personal Views on Aging
Regarding personal VoA, there was a general, normative change trend across eight years toward less favorable ATOA that was slowed down in summer/autumn 2020, with a mean decline in ATOA between 2012 and 2017 amounting to more than four times the size of the ATOA decline between 2017 and 2020. This is in contrast to a study based on another data set (Wettstein & Wahl, 2021), where a pandemic-related shift toward less favorable ATOA was found. Assessments in that study (2008, 2014, 2017, 2020) differed somewhat from the present study (2012, 2015, 2017, 2020). Also, the peri-pandemic measurement occasion in that study (June-July 2020) differed from the assessment period in the present study (June-September 2020). These and other differences in study characteristics might have contributed to the discrepant findings with regard to pandemic-related change in ATOA.
Eight-year trajectories in SA did not reveal any substantial pandemic-related change effect; at least, a model not specifying such a pandemic-related change trend resulted in a model fit that was not significantly different from a pandemic-related change model. This is consistent with the findings from the German Ageing Survey reported by Diehl et al. (2021). AARC losses showed a significant pandemic effect in that the mean increase between 2017 and 2020 was about ten times steeper in the pandemic-related change model compared to the estimated change according to the general change model without a pandemic-related change component. Yet, in line with the described reduced ATOA negative change trend between 2017 and 2020, potentially caused by the pandemic, a mean-level increase in AARC gains was identified between 2017 and 2020 in the pandemic-related change model. This pandemic-related increase in AARC gains was more than four times larger than in the model where no pandemic-related slope component was specified.
Pandemic-Related Change in General Views on Aging
In contrast to these findings for personal VoA, rather consistent support was found for the study hypothesis that the COVID-19 pandemic might have moved major age stereotype domains, such as family and partnership, personality and way of living, and health and appearance, toward a more negative direction. The only exception were age stereotypes regarding leisure which did not show a clear pandemic-related change trend and which could just as well be described as following a normative 8-year change trend without an additional COVID-19 period effect.
Shifts toward more negative age stereotypes in 2020 were remarkably universal in the study sample for the domain personality and health, with more than 80% and more than 90% of all individuals, respectively, revealing such as negative shift, though the specific extent of the negative change did vary between individuals. That particularly health-related stereotypes did show such a negative shift among the overwhelming majority of participants might indeed be a result of how old age was frequently portrayed at the beginning of the pandemic, namely as a life stage of high vulnerability and great health risks.
Multidirectionality of COVID-19 Effects on Personal and General Views on Aging
Taken as a whole, the findings of the present study underscore the need to examine the effects of the COVID-19 pandemic on VoA in a multidimensional way. Results also confirm a picture of pronounced multidirectionality across VoA. Thus, gains and losses in VoA went hand in hand as an effect of the COVID-19 pandemic, depending on which specific VoA domain was considered. Also, the observed pandemic-related change trends were found to be robust, with all of them (but one) remaining statistically significant when controlling for socio-demographic and health-related covariates. Also, these covariates, particularly age, were – apart from one exception – not systematically related with the extent of pandemic-related changes across the different VoA. Middle-aged and older adults, thus, exhibited similar pandemic-related VoA changes across the different VoA indicators included in this study. At the same time, remarkable heterogeneity in the extent and direction of pandemic-related change across most VoA was observed, confirming the observation that middle-aged and older adults are a heterogeneous group with regard to various characteristics (e.g., Nelson & Dannefer, 1992). In addition, the stress and coping literature also supports large differences in how individuals of all ages react to stressful occurrences, including the COVID-19 pandemic (Aldwin et al., 2021). Depending on personal resources and risk factors, COVID-19 effects on VoA could be more or less favorable for different individuals. Apart from the potential predictors of pandemic-related changes that were empirically investigated, it might, for instance, also make a difference if individuals have encountered certain life events prior to the pandemic that might either have sensitized them for COVID-19 effects on VoA or rather inoculated or steeled them. More research is needed to explore which determinants account for interindividual differences in individual susceptibility to COVID-19 effects on psychosocial outcomes such as VoA.
The following explanations for the multidirectionality of change in personal VoA are considered. First, if a pandemic-related change in SA in terms of increasing distancing from the group of older adults indeed happened, it may have occurred within a shorter time frame and depending on changing dynamics of the pandemic, such as variations in the COVID-19 infection rate. As noted earlier, Terracciano et al. (2021) indeed observed a younger SA in their U.S. sample in March 2020 compared to January/February 2020 when COVID-19 was not yet widespread. In April 2020, however, the mean SA in the sample was already older again. In another study (Wettstein & Wahl, conditionally accepted), a similar trend was found, with individuals assessed on days with more reported COVID infections reporting a younger subjective age than those assessed on days with fewer infections. Subjective age thus seems to fluctuate on a micro-longitudinal time level (see also Bellingtier et al., 2017; Kornadt et al., in press; Kotter-Grühn et al., 2015). Hence, a similar age-group dissociation effect as reported by Terracciano et al. (2021) might have occurred if assessment had been conducted during a time of high COVID-19 threat (e.g., in March 2020, or from November 2020 on), rather than during this rather “relaxed” pandemic period in summer 2020.
Second, the increase in AARC-gains, as well as the favorable pandemic-related trend that slowed down the normative 8-year decline in ATOA, might reflect that the pandemic has made some positive aspects of being old more salient (e.g., Lind et al., 2021), resulting in improved psychosocial outcomes. For example, Recchi et al. (2020) found that well-being had improved in France during the lockdown compared to the previous years, and they labeled this phenomenon the “eye of the hurricane paradox.” Also, pandemic-related improvements in self-rated health and health satisfaction have been reported in several studies (Entringer & Kröger, 2020; Peters et al., 2020; Recchi et al., 2020). Regarding the AARC-gain items, individuals might respond to items such as “With my increasing age, I realize that I appreciate relationships and people much more” with more favorable evaluations than before the pandemic. Indeed, perceived or potential improvements in social relationships may have occurred during the pandemic, possibly due to socio-emotional selectivity (Carstensen, 2006). That is, individuals who were forced to restrict their contacts during the pandemic may have felt closer to the ones they were still meeting (Gilligan et al., 2020; Pietrzak et al., 2021). Moreover, older adults were less threatened by the pandemic consequences in terms of job security and income and less challenged in their everyday life due to closed child-care facilities compared to younger adults or families with school-aged children. The favorable pandemic-specific change trends in ATOA and in perceived age-related gains may also reflect that older adults have generally shown high levels of resilience during the pandemic (Lind et al., 2021). This has been documented in terms of (largely) maintained mental health (Röhr et al., 2020) and by higher emotional well-being during the early phases of the pandemic compared to younger adults (Klaiber et al., 2021; Wettstein & Wahl, 2021). Yet, it is important to keep in mind that the present study did not have access to a young adult sample for comparisons.
Third, no positive changes happened at the level of general VoA. Instead, all age stereotype domains considered in this study (except leisure) pointed in a more negative direction when a pandemic-related change effect was analyzed. For instance, the large majority of individuals revealed a pandemic-related shift toward more negative personality-related and health-related age stereotypes. Public discourses during the pandemic, driven by a portrayal of older adults as being all alike in terms of being helpless, frail, and unable to contribute to society (Ayalon et al., 2021; Ehni & Wahl, 2021), may be a primary cause for that shift toward more negative age stereotypes. Such an interpretation is consistent with various established conceptual models, such as stereotype embodiment theory (Levy, 2009) or age stereotype internalization/”contamination” (Rothermund & Brandtstädter, 2003; Weiss & Kornadt, 2018), arguing that societal views and portrayals of aging get internalized and shape individuals’ views of their own aging. Counteracting and contradicting such loss-oriented representations and descriptions of older adults may help to prevent or reduce the negative effects of the pandemic on personal and general VoA among middle-aged and older adults.
However, personal VoA might not been negatively affected only due to prevalent negative age stereotyping during the pandemic (Ayalon et al., 2021; Ehni & Wahl, 2021) and concomitant “COVID ageism” (Kessler & Bowen, 2020). It is also plausible that the pandemic as a stressful event (Brakemeier et al., 2020) including pandemic-related stressors such as coronavirus anxiety/COVID-19 phobia (Jungmann & Witthöft, 2020; Traunmüller et al., 2020) or restrictions in everyday activities and social contacts, – has resulted in less favorable personal VoA, at least in some domains. Stress in general and daily stressors in particular have been shown to have a negative impact on VoA (Bellingtier et al., 2017; Kotter-Grühn et al., 2015; Schafer & Shippee, 2010; Wettstein et al., 2021). More research is thus needed to identify the mechanisms, also beyond stress and COVID ageism, that account for the COVID-19 effects on personal and general VoA.
Strengths and Limitations
This study has several strengths and limitations. Among the strengths of this study is the availability of three pre-pandemic measurements and of an extended 8-year observation period. This allowed to disentangle normative, age-graded change in VoA from change that was potentially triggered by the pandemic and therefore represents the effect of a history-graded event. Also, this study took the multidimensionality of VoA into account and considered personal as well as general VoA simultaneously in one study. This approach permitted the examination of the multidirectionality of change for different dimensions of individuals’ personal and general VoA – an endeavor that so far has received little attention. Examining the multidirectionality of change for different dimensions of VoA may be important with regard to interventional efforts that focus on individuals’ personal and general VoA as a potential avenue to optimize healthy aging (Diehl et al., 2021).
In terms of limitations, it may first be questioned whether the observed change can be interpreted as a direct COVID-19 effect on VoA, because it cannot be ruled out that alternative period effects or (historical) events between 2017 and 2020 caused specific changes in VoA and altered the general trajectories observed prior to the pandemic. Yet, it seems unlikely that other factors that might have caused the observed changes between 2017 and 2020 and that were similarly severe, global, and far-reaching as the pandemic. Second, based on the study data, it was not possible to investigate whether estimated COVID-19 effects may either persist, become stronger, or perhaps disappear again across the pandemic period due to long-term adaptation as only one peri-pandemic measurement occasion was available. Another data collection for early 2022 is planned as part of the present study to address such long-term consequences of the pandemic on VoA, including potential habituation effects. Third, due to the limited number of measurement occasions, non-linear changes in participants’ VoA were not specified, although VoA trajectories are not necessarily linear. Fourth, some of the study measures, particularly the AARC-gains assessment at T4, showed rather low internal consistency, potentially limiting the reliability of the findings. However, computing re-test correlations as an alternative reliability estimate for AARC-gains, the correlation between AARC-gains at T1 and T2 (r = .55) was very similar to the correlation between AARC-gains at T3 and T4 (r = .56), with both intervals approximately comprising three years. Therefore, the measurement of AARC-gains at T4 may not necessarily be less reliable compared to the assessments prior to T4, but item heterogeneity could have contributed to the relatively low internal consistency estimate. Still, the findings with regard to AARC-gains should be interpreted with caution. Most other measures of VoA included in this study revealed acceptable internal consistency estimates (Cronbach’s alpha) which were > .70 or even > .80 across most measurement occasions. Fifth, turning to online data collection in 2020 might have resulted in assessment mode effects and thus affected the findings. Although the online questionnaire was thoroughly pretested, paper-and-pencil questionnaires were sent out to those who did not have access toa computer or tablet, and although the item order was the same across both modes of assessment to ensure comparability, there remains still a concern of instrumentation effects, although such effects, when comparing online and paper-pencil assessment, are not necessarily large (Weigold & Russell, 2013). Indeed, when comparing all VoA scores at T4 between those who participated online (n = 184) and those who filled out paper-and-pencil questionnaires (n = 49), all group differences were of small effect size, ranging from d = .06 (subjective age) to d = .35 (AARC-losses). The “non-onliners” scored significantly higher on AARC-losses and significantly lower on ATOA than the “onliners.” They also had significantly less favorable age stereotypes regarding health and appearance. Comparing both groups across all study variables and – for personal and general VoA – across all measurement occasions, only few differences reached a medium effect size and no difference of large effect size was identified.
It is also worth noting that the study sample was restricted to community-dwelling middle-aged and older adults and that particularly vulnerable subgroups of older adults, such as nursing home residents, were not included. Their well-being and their VoA might have changed to a greater extent after the pandemic outbreak compared to community-dwelling adults. Identifying the COVID-19 consequences among such vulnerable subpopulations therefore requires further studies.
Finally, a challenge in nearly all previous behavioral research in the COVID-19 context is that findings may have to some extent been driven by culture- and country-specific dynamics. These dynamics include, but are not limited to, the strictness of protection measures, mask policies, the length of COVID-19 waves, and, more recently, the spread of new virus mutations as well as the speed of vaccinations. Therefore, the generalization of the present study findings across countries beyond Germany is clearly limited.
Study Implications and Conclusion
In conclusion, the COVID-19 pandemic may offer a prime example of how perceived loss and growth experiences may go together in older adults’ lives (Pietrzak et al., 2021). However, replication is needed to make such an interpretation still more robust and to track the effects of the COVID-19 pandemic beyond the year 2020. Given the psychosocial and health implications of individual and general VoA in general (Alonso Debreczeni & Bailey, 2021; Levy et al., 2020; Tully-Wilson et al., 2021;Westerhof et al., 2014) as well as during the COVID-19 pandemic specifically (Avidor et al., 2021; Kornadt et al., 2021; Losada-Baltar et al., 2021; Shrira et al., 2020), this study is of relevance for prevention and intervention to foster healthy aging. For instance, older adults may be educated on how to not adopt overly negative VoA, which circulated during the initial stage of the pandemic. They may also be educated on how positive VoA may protect them against the undermining effects of ageist messages and may enhance the achievement of important life goals, including better health (Diehl et al., 2021; Wolff et al., 2014). Also, reducing COVID-19-related stressors or helping individuals to better cope with such stressors, such as virus anxiety or restrictions in everyday activities and contacts, might be of additional importance to prevent or reduce detrimental COVID-19 effects on outcomes of psychosocial functioning, such as VoA or well-being.
Supplementary Material
Acknowledgement
The data collection for this study was made possible by funding from the Carl Zeiss Foundation (Project No. P2017-01-002; HEIAGE, Heidelberg University, Germany) and a Humboldt Research Award to Manfred Diehl and Hans-Werner Wahl based on their Transcoop funding scheme. Manfred Diehl’s and Han-Yun Tseng’s work on this article was supported by a grant from the National Institute on Aging, National Institutes of Health (R01 AG 051723; Principal Investigator: Manfred Diehl).
Footnotes
Competing interests
Authors declare that they have no competing interests.
References
- Aldwin CM, Yancura LA, & Lee H (2021). Stress, coping, and aging. In Schaie KW & Willis S (Eds.), Handbook of the psychology of aging (9th ed., pp. 275–286). Academic Press. [Google Scholar]
- Alonso Debreczeni F, & Bailey PE (2021). A systematic review and meta-analysis of subjective age and the association with cognition, subjective well-being, and depression. The Journals of Gerontology: Series B, 76(3), 471–482. 10.1093/geronb/gbaa069 [DOI] [PubMed] [Google Scholar]
- Avidor S, Abu Hamam A, & Lahav Y (2021). The toll of feeling older: Subjective age moderates the associations between anxiety sensitivity and symptoms of anxiety and depression during the COVID-19 epidemic. The Journals of Gerontology: Series B, 1–6. 10.1093/geronb/gbab082 [DOI] [PMC free article] [PubMed]
- Ayalon L, Chasteen A, Diehl M, Levy B, Neupert S, Rothermund K, Tesch-Römer C, & Wahl H-W (2021). Aging in times of the COVID-19 pandemic: Avoiding ageism and fostering intergenerational solidarity. The Journals of Gerontology: Series B, 76(2), e49–e52. 10.1093/geronb/gbaa051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltes PB, Lindenberger U, & Staudinger UM (2006). Life span theory in developmental psychology. In Lerner RM & Damon W (Eds.). Handbook of child psychology: Vol. 1. Theoretical models of human development (6th ed., pp. 569–664). Wiley. 10.1002/9780470147658.chpsy0111 [DOI] [Google Scholar]
- Bellingtier JA, Neupert SD, & Kotter-Grühn D (2017). The combined effects of daily stressors and major life events on daily subjective ages. The Journals of Gerontology: Series B, 72(4), 613–621. 10.1093/geronb/gbv101 [DOI] [PubMed] [Google Scholar]
- Berezina TN, & Rybtsov S (2021). Acceleration of biological aging and underestimation of subjective age are risk factors for severe COVID-19. Biomedicines, 9(8). 10.3390/biomedicines9080913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brakemeier E-L, Wirkner J, Knaevelsrud C, Wurm S, Christiansen H, Lueken U, & Schneider S (2020). Die COVID-19-Pandemie als Herausforderung für die psychische Gesundheit. Zeitschrift für Klinische Psychologie und Psychotherapie, 49 (1), 1–31. 10.1026/1616-3443/a000574 [DOI] [Google Scholar]
- Brothers A, Kornadt AE, Nehrkorn-Bailey A, Wahl H-W, & Diehl M (2021). The effects of age stereotypes on physical and mental health are mediated by self-perceptions of aging. The Journals of Gerontology: Series B, 76 (5), 845–857. 10.1093/geronb/gbaa176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL (2006). The influence of a sense of time on human development. Science, 312(5782), 1913–1915. 10.1126/science.1127488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang ES, Kannoth S, Levy S, Wang S-Y, Lee JE, & Levy BR (2020). Global reach of ageism on older persons’ health: A systematic review. PloS One, 15(1), e0220857. 10.1371/journal.pone.0220857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Brothers A, & Wahl H-W (2021). Self-perceptions and awareness of aging: Past, present, and future. In Schaie KW & Willis SL (Eds.), Handbook of the psychology of aging (9th ed., pp. 155–179). Academic Press. 10.1016/B978-0-12-816094-7.00001-5 [DOI] [Google Scholar]
- Diehl M, Nehrkorn-Bailey A, Thompson K, Rodriguez D, Li K, Rebok GW, Roth DL, Chung S-E, Bland C, Feltner S, Forsyth G, Hulett N, Klein B, Mars P, Martinez K, Mast S, Monasterio R, Moore K, Schoenberg H, Thomson E, & Tseng H-Y (2021). The AgingPLUS trial: Design of a randomized controlled trial to increase physical activity in middle-aged and older adults. Contemporary Clinical Trials, 96, 106105. 10.1016/j.cct.2020.106105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, Smyer MA, & Mehrotra CM (2020). Optimizing aging: A call for a new narrative. American Psychologist, 75(4), 577–589. 10.1037/amp0000598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl MK & Wahl H-W (2020). The psychology of later life: A contextual perspective Washington: American Psychological Association Books. [Google Scholar]
- Diehl M, Wettstein M, Spuling SM, & Wurm S (2021). Age-related change in self-perceptions of aging: Longitudinal trajectories and predictors of change. Psychology and Aging, 36(3), 344–359. 10.1037/pag0000585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutt AJ, Wahl H-W & Diehl KM (2018). Awareness of aging processes. In Knight B (Ed.), Oxford research encyclopedia of psychology and aging (S. 1053–1072). Oxford University Press. Online Publication Date: Mar 2018. doi: 10.1093/acrefore/9780190236557.013.397 [DOI] [Google Scholar]
- Elder G (1974). Children of the Great Depression University of Chicago Press. [Google Scholar]
- Ehni HJ, & Wahl HW (2021). Six propositions against ageism in the COVID-19 pandemic. Journal of Aging and Social Policy, 32(4–5), 515–525. 10.1080/08959420.2020.1770032 [DOI] [PubMed] [Google Scholar]
- Entringer T, & Kröger H (2020). Einsam, aber resilient – Die Menschen haben den Lockdown besser verkraftet als vermutet [Lonely but resilient – Individuals have coped better with the lockdown than expected]. DIW Aktuell, 46. [Google Scholar]
- Faudzi FNM, Armitage CJ, Bryant C, & Brown LJE (2019). A systematic review of the psychometric properties of self-report measures of attitudes to aging. Research on Aging, 41(6), 549–574. 10.1177/0164027518825117 [DOI] [PubMed] [Google Scholar]
- Gilligan M, Suitor JJ, Rurka M, & Silverstein M (2020). Multigenerational social support in the face of the COVID-19 pandemic. Journal of Family Theory & Review, 12(4), 431–447. 10.1111/jftr.12397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heid AR, Cartwright F, Wilson-Genderson M, & Pruchno R (2021). Challenges experienced by older people during the initial months of the COVID-19 pandemic. Gerontologist, 61(1), 48–58. 10.1093/geront/gnaa138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess TM (2006). Attitudes toward aging and their effects on behavior. In Birren In J. E. & Schaie KW (Eds.). Handbook of the psychology of aging (6th ed., pp. 379–406). Academic Press. 10.1016/B978-012101264-9/50020-3 [DOI] [Google Scholar]
- Hox JJ, & Kreft IGG (1994). Multilevel analysis methods. Sociological Methods & Research, 22(3), 283–299. 10.1177/0049124194022003001 [DOI] [Google Scholar]
- Jimenez-Sotomayor MR, Gomez-Moreno C, & Soto-Perez-de-Celis E (2020). Coronavirus, ageism, and twitter: An evaluation of tweets about older adults and COVID-19. Journal of the American Geriatrics Society, 68(8), 1661–1665. 10.1111/jgs.16508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jungmann SM, & Witthöft M (2020). Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders, 73, 102239. 10.1016/j.janxdis.2020.102239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karagiannidis C, Mostert C, Hentschker C, Voshaar T, Malzahn J, Schillinger G, Klauber J, Janssens U, Marx G, Weber-Carstens S, Kluge S, Pfeifer M, Grabenhenrich L, Welte T, & Busse R (2020). Case characteristics, resource use, and outcomes of 10,021 patients with COVID-19 admitted to 920 German hospitals: An observational study. The Lancet Respiratory Medicine, 8(9), 853–862. 10.1016/s2213-2600(20)30316-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaspar R, Gabrian M, Brothers A, Wahl H-W, & Diehl M (2019). Measuring awareness of age-related change: Development of a 10-item short form for use in large-scale surveys. Gerontologist, 59(3), e130–e140. 10.1093/geront/gnx213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaspar R, Wahl H-W, Diehl M, & Zank S (2021). Two-year change in subjective views of aging in very-old age: The predictive role of health, functional status, cognitive performance, and engagement with life. Psychology and Aging Manuscript submitted for publication.
- Kass RE, & Raftery AE (1995). Bayes factors. Journal of the American Statistical Association, 90(430), 773–795. 10.1080/01621459.1995.10476572 [DOI] [Google Scholar]
- Kastenbaum R, Derbin V, Sabatini P, & Artt S (1972). “The ages of me”: Toward personal and interpersonal definitions of functional aging. Aging and Human Development, 3(2), 197–211. 10.2190/TUJR-WTXK-866Q-8QU7 [DOI] [Google Scholar]
- Kessler E-M, & Bowen CE (2020). COVID ageism as a public mental health concern. The Lancet Healthy Longevity, 1(1), e12. 10.1016/s2666-7568(20)30002-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivi M, Hansson I, & Bjälkebring P (2020). Up and about: Older adults’ well-being during the COVID-19 pandemic in a Swedish longitudinal study. The Journals of Gerontology: Series B, 76(2), e4–e9. 10.1093/geronb/gbaa084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaiber P, Wen JH, DeLongis A, & Sin NL (2021). The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. The Journals of Gerontology: Series B, 76(2), e30–e37. 10.1093/geronb/gbaa096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinspehn-Ammerlahn A, Kotter-Grühn D, & Smith J (2008). Self-perceptions of aging: Do subjective age and satisfaction with aging change during old age? The Journals of Gerontology: Series B, 63(6), P377–P385. 10.1093/geronb/63.6.P377 [DOI] [PubMed] [Google Scholar]
- Kornadt A, & Rothermund K (2012). Internalization of age stereotypes into the self-concept via future self-views: A general model and domain-specific differences. Psychology and Aging, 27, 164–172. 10.1037/a0025110 [DOI] [PubMed] [Google Scholar]
- Kornadt AE, Albert I, Hoffmann M, Murdock E, & Nell J (2021). Ageism and older people’s health and well-being during the Covid-19-pandemic: The moderating role of subjective aging. European Journal of Ageing, 18, 173–184. 10.1007/s10433-021-00624-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornadt AE, & Rothermund K (2011). Contexts of aging: Assessing evaluative age stereotypes in different life domains. The Journals of Gerontology: Series B, 66B(5), 547–556. 10.1093/geronb/gbr036 [DOI] [PubMed] [Google Scholar]
- Kornadt AE, Kessler E-M, Wurm S, Bowen CE, Gabrian M, & Klusmann V (2019). Views on ageing: a lifespan perspective. European Journal of Ageing, 17(4), 387–401. 10.1007/s10433-019-00535-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornadt AE, Weiss D, Gerstorf D, Kunzmann U, Luecke AJ, Schilling O, Katzorreck M, Siebert J, & Wahl H-W (in press). “I felt so old this morning.” Short-term variations in subjective age and the role of trait subjective age: evidence from the ILSE/EMIL ecological momentary assessment data. Psychology and Aging [DOI] [PubMed]
- Kornadt AE, Albert I, Hoffmann M, Murdock E, & Nell J (2021). Perceived ageism during the Covid-19-crisis is longitudinally related to subjective perceptions of aging. Frontiers in Public Health, 9(976). 10.3389/fpubh.2021.679711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotter-Grühn D, Kleinspehn-Ammerlahn A, Gerstorf D, & Smith J (2009). Self-perceptions of aging predict mortality and change with approaching death: 16-year longitudinal results from the Berlin Aging Study. Psychology and Aging, 24(3), 654–667. 10.1037/a0016510 [DOI] [PubMed] [Google Scholar]
- Kotter-Grühn D, Neupert SD, & Stephan Y (2015). Feeling old today? Daily health, stressors, and affect explain day-to-day variability in subjective age. Psychology & Health, 30(12), 1470–1485. 10.1080/08870446.2015.1061130 [DOI] [PubMed] [Google Scholar]
- Lachman M (2004). Development in midlife. Annual Review of Psychology, 55, 305–331. 10.1146/annurev.psych.55.090902.141521 [DOI] [PubMed] [Google Scholar]
- Lawton MP (1975). The Philadelphia Geriatric Center Morale Scale: A revision. Journal of Gerontology, 30(1), 85–89. 10.1093/geronj/30.1.85 [DOI] [PubMed] [Google Scholar]
- Levy B (2009). Stereotype embodiment: A psychosocial approach to aging. Current Directions in Psychological Science, 18(6), 332–336. 10.1111/j.1467-8721.2009.01662.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B, Slade MD, Chang E-S, Kannoth S, & Wang S-Y (2020). Ageism amplifies cost and prevalence of health conditions. The Gerontologist, 60(1), 174–181. 10.1093/geront/gny131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein B (2021). From “Coffin Dodger” to “Boomer Remover”: Outbreaks of ageism in three countries with divergent approaches to coronavirus control. The Journals of Gerontology: Series B, 76, e206–e212, 10.1093/geronb/gbaa102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind M, Bluck S, & McAdams DP (2021). More vulnerable? The life story approach highlights older people’s potential for strength during the pandemic. The Journals of Gerontology: Series B, 76 (2), e45–e48. 10.1093/geronb/gbaa105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Baltar A, Jiménez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, & Márquez-González M (2021). “We’re staying at home.” Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. The Journals of Gerontology: Series B, 76 (2), e10–e16. 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meisner BA (2021). Are you OK, Boomer? Intensification of ageism and intergenerational tensions on social media amid COVID-19. Leisure Sciences, 43, 56–61. 10.1080/01490400.2020.1773983 [DOI] [Google Scholar]
- Miche M, Elsässer VC, Schilling OK, & Wahl H-W (2014). Attitude toward own aging in midlife and early old age over a 12-year period: Examination of measurement equivalence and developmental trajectories. Psychology and Aging, 29(3), 588–600. 10.1037/a0037259 [DOI] [PubMed] [Google Scholar]
- Nachtigall I, Lenga P, Jóźwiak K, Thürmann P, Meier-Hellmann A, Kuhlen R, Brederlau J, Bauer T, Tebbenjohanns J, Schwegmann K, Hauptmann M, & Dengler J (2020). Clinical course and factors associated with outcomes among 1904 patients hospitalized with COVID-19 in Germany: An observational study. Clinical Microbiology and Infection, 26, 1663–1669. doi: 10.1016/j.cmi.2020.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EA, & Dannefer D (1992). Aged heterogeneity: fact or fiction? The fate of diversity in gerontological research. Gerontologist, 32(1), 17–23. doi: 10.1093/geront/32.1.1 [DOI] [PubMed] [Google Scholar]
- Peters A, Rospleszcz S, Greiser KH, Dallavalle M, & Berger K (2020). COVID-19-Pandemie verändert die subjektive Gesundheit [The COVID-19 pandemic changes subjective health]. Deutsches Ärzteblatt International, 117(50), 861–867. https://www.aerzteblatt.de/int/article.asp?id=216950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Tsai J, & Southwick SM (2021). Association of symptoms of posttraumatic stress disorder with posttraumatic psychological growth among US veterans during the COVID-19 pandemic. JAMA Network Open, 4(4), e214972–e214972. 10.1001/jamanetworkopen.2021.4972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, & Wahl H-W (2021). Subjective age from childhood to advanced old age: A meta-analysis. Psychology and Aging, 36(3), 394–406. 10.1037/pag0000600 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Ram N, & Grimm KJ (2015). Growth curve modeling and longitudinal factor analysis. In Lerner RM (Ed.), Handbook of child psychology and developmental science: Volume 1. Theory and method (7 ed., pp. 758–788). Wiley. 10.1002/9781118963418.childpsy120 [DOI] [Google Scholar]
- Recchi E, Ferragina E, Helmeid E, Pauly S, Safi M, Sauger N, & Schradie J (2020). The “Eye of the Hurricane” paradox: An unexpected and unequal rise of well-being during the Covid-19 lockdown in France. Research in Social Stratification and Mobility, 68, 100508. 10.1016/j.rssm.2020.100508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert-Koch-Institut. (2020). SARS-CoV-2 Steckbrief zur Coronavirus-Krankheit-2019 (COVID-19) https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief.html
- Röhr S, Reininghaus U, & Riedel-Heller SG (2020). Mental well-being in the German old age population largely unaltered during COVID-19 lockdown: Results of a representative survey. BMC Geriatrics, 20(1). 020–01889. 10.1186/s12877-020-01889-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothermund K, & Brandtstädter J (2003). Age stereotypes and self-views in later life: Evaluating rival assumptions. International Journal of Behavioral Development, 27(6), 549–554. 10.1080/01650250344000208 [DOI] [Google Scholar]
- Rubin DC, & Berntsen D (2006). People over forty feel 20% younger than their age: Subjective age across the lifespan. Psychonomic Bulletin & Review, 13(5), 776–780. 10.3758/bf03193996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer MH, & Shippee TP (2010). Age identity in context: Stress and the subjective side of aging. Social Psychology Quarterly, 73(3), 245–264. 10.1177/0190272510379751 [DOI] [Google Scholar]
- Shrira A, Hoffman Y, Bodner E, & Palgi Y (2020). COVID-19-related loneliness and psychiatric symptoms among older adults: The buffering role of subjective age. The American Journal of Geriatric Psychiatry, 28(11), 1200–1204. 10.1016/j.jagp.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siebert J, Braun T, & Wahl H-W (2020). Change in attitudes toward aging: Cognitive complaints matter more than objective performance. Psychology and Aging, 35, 357–368. 10.1037/pag0000451 [DOI] [PubMed] [Google Scholar]
- Spuling SM, Klusmann V, Bowen CE, Kornadt AE, & Kessler E-M (2019). The uniqueness of subjective ageing: convergent and discriminant validity. European Journal of Ageing, 17(4), 445–455. 10.1007/s10433-019-00529-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephan Y, Sutin AR, & Terracciano A (2020). Physical activity and subjective age across adulthood in four samples. European Journal of Ageing, 17(4), 469–476. 10.1007/s10433-019-00537-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Stephan Y, Aschwanden D, Lee JH, Sesker AA, Strickhouser JE, Luchetti M, & Sutin AR (2021). Changes in subjective age during COVID-19. Gerontologist, 61(1), 13–22. 10.1093/geront/gnaa104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traunmüller C, Stefitz R, Gaisbachgrabner K, & Schwerdtfeger A (2020). Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health, 20(1), 1395. 10.1186/s12889-020-09489-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tully-Wilson C, Bojack R, Millear PM, Stallman HM, Allen A, & Mason J (2021). Self-perceptions of ageing: A systematic review of longitudinal studies. Psychology and Aging, 36(7), 773–789. 10.1037/pag0000638 [DOI] [PubMed] [Google Scholar]
- Uotinen V, Rantanen T, Suutama T, & Ruoppila I (2006). Change in subjective age among older people over an eight-year follow-up: ‘Getting older and feeling younger’? Experimental Aging Research, 32(4), 381–393. 10.1080/03610730600875759 [DOI] [PubMed] [Google Scholar]
- Weigold A, Weigold IK, & Russell EJ (2013). Examination of the equivalence of self-report survey-based paper-and-pencil and internet data collection methods. Psychological Methods, 18(1), 53. 10.1037/a0031607. [DOI] [PubMed] [Google Scholar]
- Weiss D, & Freund AM (2012). Still young at heart: Negative age-related information motivates distancing from same-aged people. Psychology and Aging, 27(1), 173–180. 10.1037/a0024819 [DOI] [PubMed] [Google Scholar]
- Weiss D, & Lang F (2012). “They” are old but “I” feel younger: age-group dissociation as a self-protective strategy in old age. Psychology and Aging, 27, 153–163. 10.1037/a0024887 [DOI] [PubMed] [Google Scholar]
- Weiss D, & Kornadt AE (2018). Age-stereotype internalization and dissociation: Contradictory processes or two sides of the same coin? Current Directions in Psychological Science, 27(6), 477–483. 10.1177/0963721418777743 [DOI] [Google Scholar]
- Westerhof GJ, Miche M, Brothers AF, Barrett AE, Diehl M, Montepare JM, Wahl H-W, & Wurm S (2014). The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychology and Aging, 29(4), 793–802. 10.1037/a0038016 [DOI] [PubMed] [Google Scholar]
- Wettstein M, & Wahl HW (2021). Die Corona-Pandemie und ihre psychosozialen Konsequenzen für ältere Menschen in Deutschland: Ein Zwischenresümee aktuellverfügbarer Evidenz. In Lines E (Ed.), Post-pandemic populations. Discussion paper No. 13 (pp. 42–50). Max Planck Society/Population Europe. https://population-europe.eu/files/documents/pe_discussion-paper_final_1.pdf [Google Scholar]
- Wettstein M, Wahl H-W, & Kornadt AE (2021). Longitudinal associations between perceived stress and views on aging: Evidence for reciprocal relations. Psychology and Aging, 36(6), 752–766. 10.1037/pag0000632 [DOI] [PubMed] [Google Scholar]
- Wettstein M, & Wahl HW (2021). Trajectories of attitude toward own aging and subjective age from 2008 to 2020 among middle-aged and older adults: Partial evidence of a “COVID-19 effect”, Psychology and Aging, 36, 790–805. 10.1037/pag0000649 [DOI] [PubMed] [Google Scholar]
- Wettstein M, & Wahl H-W (conditionally accepted). Contextual determinants of subjective age in midlife and old age: The example of daily variations in COVID-19 infection rates. Psychology and Aging [DOI] [PubMed]
- Wolff JK, Warner LM, Ziegelmann JP, & Wurm S (2014). What do targeting positive views on ageing add to a physical activity intervention in older adults? Results from a randomised controlled trial. Psychology & Health, 29(8), 915–932. 10.1080/08870446.2014.896464 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2020, March). WHO Director-General’s opening remarks at the media briefing on COVID-19 https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- Wurm S, Diehl M, Kornadt A, Westerhof G, & Wahl H-W (2017). How do views on aging affect health outcomes in adulthood and late life? Explanations for an established connection. Developmental Review, 46, 27–43. 10.1016/j.dr.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R (2003). Measuring explained variation in linear mixed effects models. Statistics in Medicine, 22(22), 3527–3541. 10.1002/sim.1572 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


