Abstract
Patient: Male, 45-year-old
Final Diagnosis: Cervical facet syndrome • radiation induced fibrosis
Symptoms: Headache • neck pain and stiffness
Medication: —
Clinical Procedure: Neck stretches • soft tissue manipulation • spinal manipulation • therapeutic ultrasound
Specialty: Chiropractic • Rehabilitation
Objective:
Rare disease
Background:
Pineal gland tumors are rare central nervous system tumors, and while neck pain and headaches may be common among those who have had these tumors removed, there is little research regarding management of these symptoms.
Case Report:
A 45-year-old man with a history of pineal germinoma treated with pinealectomy, chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement at age 21 presented with chronic neck pain and headaches, which initially improved following his surgery and concurrent therapies, yet progressively worsened over the following years. He required thyroid and testosterone medication because of radiation-induced hypopituitarism, yet was employed, and until recently, active with playing tennis. He had previously seen his primary care provider, orthopedist, and neurologist, and had been cleared of severe pathology via brain magnetic resonance imaging and was referred to the chiropractor. On examination, the patient had severely limited passive cervical spine range of motion, yet hat no neurologic deficits, and radiographs showed mild cervical spondylosis and cervicothoracic scoliosis. His history and presentation were suggestive of radiation-induced fibrosis. The patient’s neck pain, headaches, and quality of life improved with multimodal treatments including spinal and soft-tissue manipulation, stretches, and yoga.
Conclusions:
This case illustrates long-term sequelae of a pineal gland tumor and its treatment, including neck pain and headache, and improvement with multimodal chiropractic therapies. Despite the success in this case, these results are not broadly generalizable. Further research is needed to understand the natural history of symptoms and effectiveness of multimodal therapies among patients who have had pineal tumor surgery.
Keywords: Chiropractic; Manipulation, Spinal; Neck Pain; Pineal Gland; Radiotherapy
Background
Pineal gland tumors are a rare type of brain tumor typically diagnosed in younger individuals and most often present with headaches and nausea or vomiting [1,2]. While patients may expect significant improvements in pain and disability after surgery and other treatments to remove pineal gland tumors, there is limited research examining long-term outcomes or multidisciplinary pain management for these patients [3]. Research indicates that patients undergoing pineal gland surgery may be at a heightened risk for degenerative disc pathology and scoliosis [4,5], while adverse effects of other treatments for these patients related to chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement also may contribute to pain [6–8]. To date, there is a limited understanding of the spectrum of symptoms and their treatment in patients who have undergone surgery and other concurrent therapies for pineal gland tumors.
Pineal gland tumors make up 0.4% to 1% of all brain tumors [9]. These have a male predominance, which is even stronger for germ cell tumors such as germinomas (12: 1 male to female ratio) [10]. The median age of diagnosis is age 17 years [10]. Surgery for these tumors in the early 20th century was associated with high rates of mortality, but with newer advancements such as cerebrospinal fluid shunting and radiotherapy, the mortality rate has reduced [11]. According to a large-database study in 2009, patients with germ cell pineal tumors (eg, germinoma) have a 5-year survival rate of 79±2% [10].
Presenting features of pineal gland tumors often include headaches, nausea and vomiting, polyuria, and diplopia, but may also include neck pain or a range of other neurological symptoms [1]. However, the symptoms following surgery for pineal gland tumors are not well described [3]. In a study of patients who underwent surgery for pineal gland lesions, patients reported a significant reduction in pain on average [3]. However, at 6 months or more following surgery, patients’ mean pain severity was 12±20 out of 100, indicating that pain relief was variable, and some patients had higher levels of ongoing pain than others [3].
Based on studies in animals, pinealectomy has been suggested to accelerate disc degeneration and increase the risk of scoliosis [4,5]. The suggested mechanism is via the loss of melatonin, a hormone produced by the pineal gland [4,5]. Melatonin is involved in sleep-wake cycles, but also acts as an antioxidant, an anti-inflammatory, and a neural signaling molecule, and helps modulate pain [12]. In addition, there are melatonin receptors in the intervertebral disc, which suggest it plays a role in spine health [13].
Treatments used alongside surgery for pineal gland tumors may also contribute to pain syndromes. Radiation therapy can induce muscle fibrosis, which typically develops 4 to 12 months following radiation and can progress over the span of several years [14]. Radiation-induced fibrosis is painful and can significantly limit range of motion [6]. Chemotherapy also commonly causes pain in general [6,7]. While rare, complications related to an implanted ventriculoperitoneal shunt can cause neck pain [8,15].
Chiropractors are healthcare providers that often treat neuromusculoskeletal conditions such as neck pain and headache [16]. There is limited but encouraging evidence that chiropractors can serve a role in helping manage pain in patients who have neoplastic conditions or who are dealing with painful sequelae related to these conditions [17–19]. Chiropractors utilize a range of manual therapy (hands-on) treatment techniques that alleviate pain and improve range of motion, as well as guide patients through rehabilitative exercises [16,20].
As pineal gland tumors are rare, there is little research regarding long-term follow-up or treatments for patients with neck pain or headaches following their surgical removal and treatment. Accordingly, we report a case of a patient who suffered from chronic neck pain and headaches persisting then worsening after pineal tumor surgery, which significantly improved with multimodal chiropractic interventions.
Case Report
Patient Information
A 45-year-old male pineal gland tumor survivor presented to a chiropractor reporting intermittent, moderate headache and neck pain and severe neck stiffness (Figure 1). His neck pain was bilateral, but more severe on the right side, and involved the cervical-thoracic region (upper trapezius) and occasionally the periscapular borders. He also noted severe neck stiffness and difficulty turning, bending, or extending his neck. His headache was described as bilateral, mostly occipital, and occasionally temporal, and did not involve any aura, dizziness, nausea, or vomiting. His self-reported pain intensity of his neck pain and headache was 6 out of 10 on the numeric pain rating scale. His World Health Organization Quality of Life (WHOQOL) score was 70%.
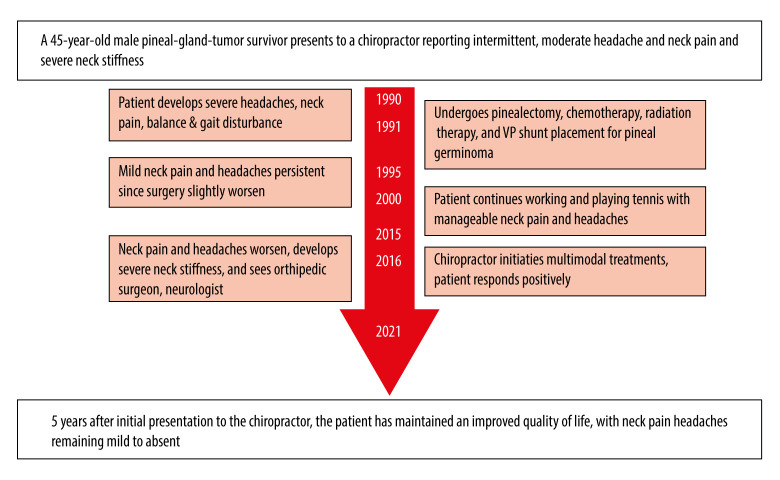
Figure 1.
Timeline of care. Abbreviations: ventriculoperitoneal (VP).
The patient worked as a construction company owner. Aside from his previous pineal tumor surgery and sequelae of subsequent radiation therapy, hypopituitarism, dental caries, and occasional dry mouth, he was otherwise healthy. He was a non-smoker, occasionally drank alcohol, and had no significant family history, including cancer or spinal disorders.
At age 20, 25 years prior to presenting to the chiropractor, he developed severe neck pain and headaches, nausea, and difficulty with balance and walking. After extensive testing, he was diagnosed with a pineal germinoma (Figure 2). At age 21, he underwent pinealectomy, chemotherapy, and external beam radiation therapy, and had a ventriculoperitoneal shunt implanted to prevent hydrocephalus. Following treatment, there were abnormalities in his hormone levels suggestive of radiation-induced hypopituitarism, which required the prescription of several medications. He was accordingly treated with desmopressin (60 mcg per os), levothyroxine (100 mg per os), and testosterone undecanoate (40 mg per os). He also had been prescribed febuxostat (40 mg) for elevated uric acid levels, but denied a history of gout.
Figure 2.
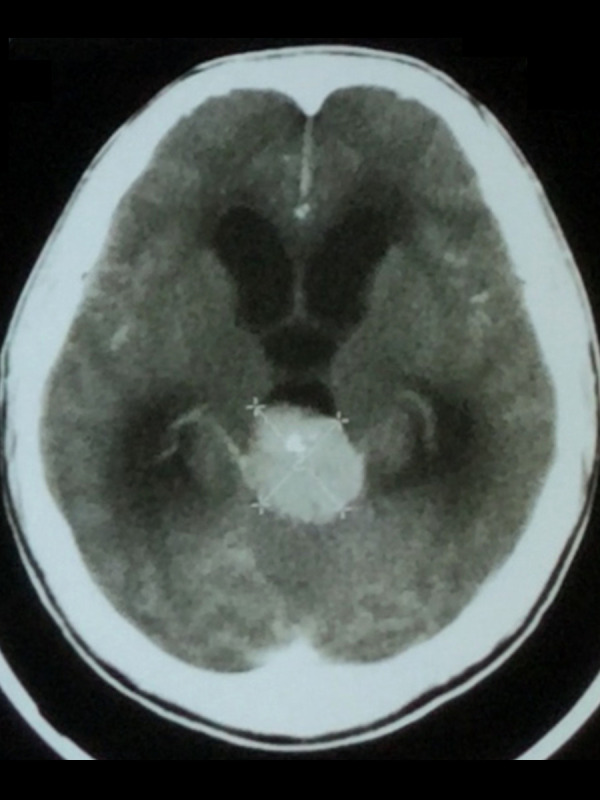
Computed tomography of brain, coronal section with contrast, 25 years prior to presentation. A 3.2×3.7-centimeter soft-tissue mass lesion with a central focus of calcification is noted in the pineal region. The mass bulges into the posterior aspect of the 3rd ventricle, resulting in obstructive hydrocephalus with moderate-to-severe dilation of the 3rd and lateral ventricles. The lesion homogenously enhanced with contrast.
Following the pineal surgery and other treatments, he noted that his balance and gait returned to normal, and he no longer had nausea, but had mild residual headaches and neck pain. These symptoms were not limiting, and he was able to work and play tennis regularly. He had been followed up with a yearly appointment by a neurologist since his pinealectomy.
At age 25, 5 years after his pinealectomy, he reported a slight worsening of his symptoms, including neck pain and stiffness and headaches, without specific injury, which persisted at a mild-to-moderate level for 20 years. Despite this, he was able to continue working and playing tennis.
Over the 6 months preceding his chiropractic visit, his neck pain and headaches again worsened without specific injury, interfered with his sleep quality, and negatively impacted his social and quality of life. He had to stop playing tennis due to his symptoms. Due to lack of sleep and pain, he also reported difficulty focusing while at work. He had been taking ibuprofen over the past 3 months without success in managing his symptoms. The patient was evaluated by an orthopedic surgeon and neurologist, who had reportedly ruled out major pathology such as germinoma recurrence and hematoma via testing, including brain magnetic resonance imaging (MRI), which was reportedly normal. His primary care provider referred him for physical therapy, where he underwent rehabilitative exercises. These included active bilateral cervical rotation and lateral flexion range of motion exercises, repeated active cervical retractions, and passive stretching for the upper trapezius and levator scapulae muscles bilaterally. However, he had minimal improvement with this care. He had not undergone acupuncture. His primary care provider then referred him to the chiropractor.
Clinical Findings
Upon initial evaluation by the chiropractor, the patient was tall and had an athletic build, and had a guarded neck posture with an elevated left shoulder. Muscle spasm was evident in the paraspinal and cervicothoracic muscles, more prominently on the right side. His cervical range of motion was limited, with pain at 10° passive extension (normal ≥50°) and restricted at 40° of bilateral passive rotation (normal ≥80°) [21,22]. Tenderness and trigger points were identified at the right upper trapezius and sternocleidomastoid muscles. Segmental joint motion as assessed by motion palpation revealed restriction and tenderness at the C1/2, C5/6, C7/T1, T1/2, and T5/6 spinal levels. A neurologic examination, including cranial nerve testing, sensation, strength, muscle stretch reflexes, and Romberg’s balance test, showed no abnormalities.
The chiropractor’s differential diagnosis for neck pain included radiation fibrosis syndrome and cervical facet syndrome, while a differential for his headache included cervicogenic headache in relation to his potential cervical radiation fibrosis or occipital neuralgia. More serious intracranial pathology had been recently ruled out by neurology and orthopedics and a normal brain MRI. Symptoms related to the patient’s ventriculoperitoneal shunt could also be considered. However, he did not display chest wall pain along the shunt pathway [8], nor did he demonstrate signs of hypersensitivity to the shunt such as pruritus [15]. Given the patient’s complex medical history, and severely limited range of motion, the chiropractor obtained cervical radiographs performed that week.
Radiographs demonstrated a reduced cervical lordosis, mild-to-moderate intervertebral disc space narrowing at C5/C6 with marginal osteophytes, and scoliosis (Figures 3, 4). The visualized portion of the ventriculoperitoneal shunt was intact. The clinical working diagnosis was cervical zygapophy-seal joint pain (facet syndrome) with underlying radiation fibrosis. While the exact parameters of the patient’s radiation therapy were unavailable, he matched the typical pattern for radiation-induced fibrosis with a history of ionizing beam radiation, and progressive worsening of symptoms and loss of range of motion over the years following radiation [14]. As he was skeletally mature, his chief concern was neck pain and headaches, and as there was no obvious rib hump on forward bending, further full-spine radiography was deemed unnecessary at the time.
Figure 3.
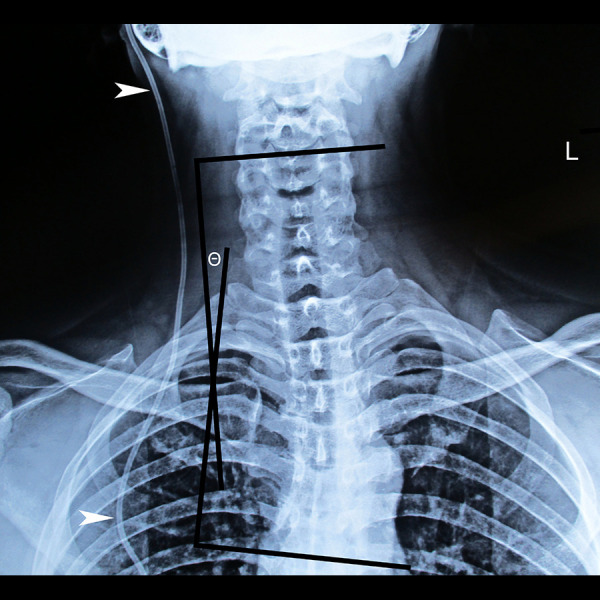
Anteroposterior cervical spine radiograph. The patient’s cervical spine is deviated to the right side of the midline, and a levoconvex cervicothoracic scoliosis is evident, extending from C4 to T6, measuring 11° (θ). A radiopaque ventriculoperitoneal shunt is also noted on the patient’s right side (arrowheads).
Figure 4.
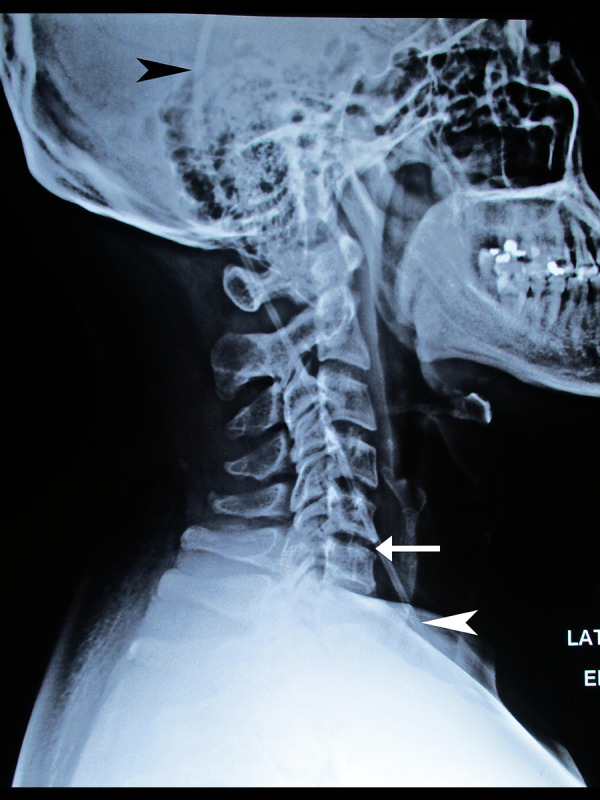
Lateral cervical spine radiograph. The cervical lordosis is visibly reduced (straightened cervical curve), and there is mild disc space narrowing at C5–6 (arrow). The ventriculoperitoneal shunt is also evident (arrowheads).
Given the postural findings, limited range of motion, and presence of neck pain, spinal manipulation was recommended. While there is little research or guidance on the use of spinal manipulation in patients with ventriculoperitoneal shunts, this was generally considered safe as the shunt is not directly attached to the spine. The patient consented to a trial of care, which initially began with 3 visits per week.
Multimodal chiropractic treatments consisted of spinal manipulation of the restricted segments identified on examination in the cervical, cervicothoracic, and thoracic regions, using high-velocity, low-amplitude manual diversified technique (Figure 5). Thermal ultrasound therapy and instrument-assisted soft-tissue manipulation (Figure 6) were also administered to alleviate neck muscle tightness and restore mobility. The chiropractor advised the patient to perform neck stretches at home, 3 times per day, including lateral flexion with and without rotation for 10 seconds each, to target the upper trapezius and levator scapulae muscles bilaterally. The chiropractor also advised the patient to attend a yoga class, which he did regularly for 6 months.
Figure 5.

Cervical spine manipulation demonstration. The chiropractor contacts the left articular pillar of the cervical articulations (C5 shown), preloads the spine by ipsilaterally laterally flexing and contralaterally rotating the cervical spine, then provides a brief, high-velocity, low-amplitude thrust in a vector oriented lateral to medial and posterior to anterior (arrow). Additional manipulations were performed in the current case at the cervicothoracic junction and thoracic spine (not shown).
Figure 6.

Instrument-assisted soft-tissue manipulation. The chiropractor applies a thin layer of emollient and gently strokes a massage tool with a beveled edge against the targeted muscle groups (arrows). Treatment of the upper trapezius is shown.
The patient reported that his pain lessened from the second week onward, reaching a mild to absent level within 4 weeks. However, his neck stiffness was improving slowly. Treatment sessions were continued at a frequency of 3 visits per week for a duration of 3 months as the patient experienced benefits from the therapies provided yet was still limited by neck stiffness and recurrences of pain. By the end of the third month, he consistently reported his neck pain remained absent following care, and his WHOQOL score had improved to 96%. At this time, his neck range of motion had improved to 20° of passive extension and 50° of passive rotation bilaterally.
The patient was subsequently under chiropractic care with monthly appointments. His neck pain and headache symptoms remained mild to absent through the follow-up period of 5 years. From 1- to 5-years follow-up, his WHO-QOL scores were maintained at an improved level and ranged from 90% to 96%. The patient occasionally would have gaps in care when he felt better, then return for appointments when his symptoms returned. At 5-year follow-up, his cervical range of motion had continued to improve to 30° passive extension and 50° passive rotation bilaterally, neither of which provoked pain. There were no adverse events in relation to the therapies provided. The patient gave written consent for the publication of this case report and any accompanying images.
Discussion
This case illustrates a male patient with chronic headaches, neck pain, and severe neck stiffness that had persisted at a mild level after pineal tumor surgery, chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement, then progressively worsened. As serious pathology had been ruled out by previous investigations, the chiropractor recommended a multimodal approach, including soft-tissue and spinal manipulation, stretches, and yoga. The patient responded positively, and his pain levels reduced quickly while his range of motion recovered more slowly.
Although animal studies have suggested that pinealectomy accelerates disc degeneration and increases the risk of scoliosis [4,5], it is unclear if these mechanisms were directly involved in the patient’s clinical presentation. He had degenerative disc changes at C5–6, which is common among individuals in their 40s [23], and thus not necessarily due to the pinealectomy or a direct cause of symptoms. However, he did have scoliosis, which is less common among males (prevalence of 6% [24]), and could potentially be related to his previous germinoma and pinealectomy.
Post-radiation fibrosis is another mechanism for neck pain and stiffness that occurs in patients who have undergone head or neck radiation therapy and was implicated in the current case. This condition has been suggested to result from overproduction of collagen fibers in response to radiation damage [25]. While this diagnosis is more of a clinical one, the patient did have hallmark findings of severely limited range of motion (including passive range), which had progressively worsened [14,26]. While the records detailing the patient’s radiation therapy were unavailable, it is likely that the targeted area also included the cervical spine. The mainstay of treatment for intracranial germinomas has traditionally been cranio-spinal external beam radiation therapy [27,28], thus including at least part of the cervical spine. Post-radiation fibrosis occurs in about one-third of patients who have undergone chemotherapy and radiation for head and/or neck cancer and is more common with older radiation therapy techniques [25], as in the current case.
Clinically, we suggest the patient had cervical facet syndrome given his typical features for this condition including mostly axial pain with some radiation into the cervicothoracic region, lack of neurological deficits, and limited passive range of motion [29]. There is limited research describing an association between cervical facet syndrome and radiation-induced fibrosis. However, joint fibrosis, also called arthrofibrosis, is a well-known sequela of radiation-induced fibrosis [30], and could explain the patient’s apparent facet syndrome.
Postoperative health-related quality of life has gained importance as an outcome parameter after brain tumor treatment [3]. However, there is a paucity of data available on quality of life for patients with pineal region tumors, with the bulk of the evidence based on retrospective studies with limited long-term follow-up [3]. One recent publication suggested that oncologists and their allied health teams should routinely monitor patients who have undergone chemotherapy and radiotherapy for head and/or neck cancer, and offer relevant rehabilitative and multimodal therapies to patients in need [31].
Although manual therapies, including spinal manipulation and myofascial therapy, have been shown to be beneficial for spine-related disorders and headaches, there is limited research on their use in survivors of head and/or neck cancer [18,19,32]. However, the effects of these therapies could be useful in patients with limited cervical spine range of motion and possible radiation-induced fibrosis, as in the current case. Spinal manipulation has been hypothesized to break up intra-articular facet joint adhesions, which restrict mobility [33]. In a recent study, cervical spine high-velocity low-amplitude manipulation was found to increase cervical spine intervertebral motion and cause facet joint gapping, as observed via biplane radiography [34]. Instrument-assisted soft-tissue manipulation has also been suggested to help break down myofascial adhesions and fibrosis [35,36], and has been recommended for cases of radiation-induced fibrosis [26].
We encourage other authors to report the long-term patient outcomes, symptoms, and quality of life in pineal tumor survivors, as well as their response to various treatment regimens. Hopefully, a research database can be built for such patients so that they can have options to manage recurrent or persistent pain following tumor treatment. Given the rarity of these tumors, such research could be built at first using observational study designs, such as case reports, series, or retrospective chart reviews, before progressing to experimental study designs.
Limitations
As a single case, the current report has limited generalizability. The current patient was generally in good health and was physically active, which may have improved his prognosis with such multimodal therapies. Although he had progressively worsened, his improvement could also be attributed to the natural history of such symptoms and could have resolved without care. Second, his brain MRI performed preceding chiropractic care was unavailable upon request. Third, full-spine radiography was not performed to further evaluate his scoliosis and was deemed to be clinically unnecessary for his current concern. Fourth, the diagnosis of radiation-induced fibrosis was suggested by his presentation and history but was not objectively confirmed by biopsy. Fifth, it is not clear which therapy helped the patient the most, or if it was a combination of manual therapies, stretches, and yoga. Also, the patient had previously undergone physical therapy without much success, but it is possible that ongoing physical therapy could have afforded him more relief.
Conclusions
This case report describes the effectiveness of multimodal chiropractic treatments in alleviating chronic neck pain and stiffness and headaches in a patient with chronic symptoms following pinealectomy, chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement. Further research is needed to better characterize the long-term symptoms and treatment options for patients experiencing neck pain and headaches after treatment for pineal tumors. Despite the apparent success in the current case, our findings should be interpreted with caution, and patients with similar symptoms should discuss the appropriateness of such multimodal therapies with their providers on a case-by-case basis.
Footnotes
Department and Institution Where Work Was Done
New York Chiropractic and Physiotherapy Centre, EC Healthcare, Kowloon, Hong Kong.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Tamaki N, Yin D. Therapeutic strategies and surgical results for pineal region tumours. J Clin Neurosci. 2000;7:125–18. doi: 10.1054/jocn.1999.0164. [DOI] [PubMed] [Google Scholar]
- 2.Pettorini BL, Al-Mahfoud R, Jenkinson MD, et al. Surgical pathway and management of pineal region tumours in children. Childs Nerv Syst. 2013;29:433–39. doi: 10.1007/s00381-012-1954-y. [DOI] [PubMed] [Google Scholar]
- 3.Fedorko S, Zweckberger K, Unterberg AW. Quality of life following surgical treatment of lesions within the pineal region. J Neurosurg. 2018;130:28–37. doi: 10.3171/2017.7.JNS17260. [DOI] [PubMed] [Google Scholar]
- 4.Turgut M, Başaloğlu HK, Yenisey Ç, Özsunar Y. Surgical pinealectomy accelerates intervertebral disc degeneration process in chicken. Eur Spine J. 2006;15:605–12. doi: 10.1007/s00586-005-0972-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wai MGC, Jun WWW, Yee YAP, et al. A review of pinealectomy-induced melatonin-deficient animal models for the study of etiopathogenesis of adolescent idiopathic scoliosis. Int J Mol Sci. 2014;15:16484–99. doi: 10.3390/ijms150916484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baldoman D, Vandenbrink R. Physical therapy challenges in head and neck cancer. Multidiscip Care Head Neck Cancer Patient. 2018;174:209–23. doi: 10.1007/978-3-319-65421-8_12. [DOI] [PubMed] [Google Scholar]
- 7.Pearce A, Haas M, Viney R, et al. Incidence and severity of self-reported chemotherapy side effects in routine care: A prospective cohort study. PLoS One. 2017;12:e0184360. doi: 10.1371/journal.pone.0184360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salim AD, Elzain MA, Mohamed HA, Zayan BEMI. Shunt tube calcification as a late complication of ventriculoperitoneal shunting. Asian J Neurosurg. 2015;10:246. doi: 10.4103/1793-5482.161321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mottolese C, Szathmari A, Beuriat P-A. Incidence of pineal tumours. A review of the literature. Neurochirurgie. 2015;61:65–69. doi: 10.1016/j.neuchi.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Al-Hussaini M, Sultan I, Abuirmileh N, et al. Pineal gland tumors: Experience from the SEER database. J Neurooncol. 2009;94:351–58. doi: 10.1007/s11060-009-9881-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudhry O, Gupta G, Prestigiacomo CJ. On the surgery of the seat of the soul: the pineal gland and the history of its surgical approaches. Neurosurg Clin. 2011;22:321–33. doi: 10.1016/j.nec.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Xie S, Fan W, He H, Huang F. Role of melatonin in the regulation of pain. J Pain Res. 2020;13:331–43. doi: 10.2147/JPR.S228577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng Z, Xiang Q, Wang J, Zhang Y. The potential role of melatonin in retarding intervertebral disc ageing and degeneration: A systematic review. Ageing Res Rev. 2021;70:101394. doi: 10.1016/j.arr.2021.101394. [DOI] [PubMed] [Google Scholar]
- 14.Straub JM, New J, Hamilton CD, et al. Radiation-induced fibrosis: Mechanisms and implications for therapy. J Cancer Res Clin Oncol. 2015;141:1985–94. doi: 10.1007/s00432-015-1974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lanlokun MA, Guerriero E, Friedlander RM, Fajt ML. A case series of hyper-sensitivity reactions to ventriculoperitoneal shunt material. J Clin Neurosci. 2021;91:84–87. doi: 10.1016/j.jocn.2021.06.030. [DOI] [PubMed] [Google Scholar]
- 16.Beliveau PJH, Wong JJ, Sutton DA, et al. The chiropractic profession: A scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Ther. 2017;25:35. doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chu EC-P, Trager RJ, Chen ATC. Conservative management of low back pain related to an unresectable aggressive sacral hemangioma: A case report. Am J Case Rep. 2022;23:e936984. doi: 10.12659/AJCR.936984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alcantara J, Alcantara JD, Alcantara J. The chiropractic care of patients with cancer: A systematic review of the literature. Integr Cancer Ther. 2012;11:304–12. doi: 10.1177/1534735411403309. [DOI] [PubMed] [Google Scholar]
- 19.Laoudikou MT, McCarthy PW. Patients with cancer. Is there a role for chiropractic? J Can Chiropr Assoc. 2020;64:32. [PMC free article] [PubMed] [Google Scholar]
- 20.Hinkeldey N, Okamoto C, Khan J. Spinal manipulation and select manual therapies: Current perspectives. Phys Med Rehabil Clin. 2020;31:593–608. doi: 10.1016/j.pmr.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Seacrist T, Saffioti J, Balasubramanian S, et al. Passive cervical spine flexion: The effect of age and gender. Clin Biomech. 2012;27:326–33. doi: 10.1016/j.clinbiomech.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 22.Sukari AAA, Singh S, Bohari MH, et al. Examining the range of motion of the cervical spine: Utilising different bedside instruments. Malays J Med Sci. 2021;28:100–5. doi: 10.21315/mjms2021.28.2.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tao Y, Galbusera F, Niemeyer F, et al. Radiographic cervical spine degenerative findings: A study on a large population from age 18 to 97 years. Eur Spine J. 2021;30:431–43. doi: 10.1007/s00586-020-06615-0. [DOI] [PubMed] [Google Scholar]
- 24.Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: Results from the First National Health and Nutrition Examination Survey. Int J Epidemiol. 1987;16:537–44. doi: 10.1093/ije/16.4.537. [DOI] [PubMed] [Google Scholar]
- 25.Ramia P, Bodgi L, Mahmoud D, et al. Radiation-induced fibrosis in patients with head and neck cancer: A review of pathogenesis and clinical outcomes. Clin Med Insights Oncol. 2022;16:11795549211036898. doi: 10.1177/11795549211036898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brook I. Late side effects of radiation treatment for head and neck cancer. Radiat Oncol J. 2020;38:84. doi: 10.3857/roj.2020.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haas-Kogan DA, Missett BT, Wara WM, et al. Radiation therapy for intracranial germ cell tumors. Int J Radiat Oncol. 2003;56:511–18. doi: 10.1016/s0360-3016(02)04611-4. [DOI] [PubMed] [Google Scholar]
- 28.Reddy MP, Saad AF, Doughty KE, et al. Intracranial germinoma. Proc Bayl Univ Med Cent. 2015;28:43–45. doi: 10.1080/08998280.2015.11929183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirpalani D, Mitra R. Cervical facet joint dysfunction: A review. Arch Phys Med Rehabil. 2008;89:770–74. doi: 10.1016/j.apmr.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 30.Rodman SN, Kluz PN, Hines MR, et al. Sex-based differences in the severity of radiation-induced arthrofibrosis. J Orthop Res. 2022;40(11):2586–96. doi: 10.1002/jor.25297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chauhan NS, Samuel SR, Meenar N, et al. Sarcopenia in male patients with head and neck cancer receiving chemoradiotherapy: A longitudinal pilot study. Peer J. 2020;8:e8617. doi: 10.7717/peerj.8617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pattanshetty RB, Patil SN. Role of manual therapy for neck pain and quality of life in head and neck cancer survivors: A systematic review. Indian J Palliat Care. 2022;28:99–112. doi: 10.25259/IJPC_10_2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cramer GD, Henderson CNR, Little JW, et al. Zygapophyseal joint adhesions after induced hypomobility. J Manipulative Physiol Ther. 2010;33:508–18. doi: 10.1016/j.jmpt.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 34.Anderst WJ, Gale T, LeVasseur C, Raj S, et al. Intervertebral kinematics of the cervical spine before, during, and after high-velocity low-amplitude manipulation. Spine J. 2018;18:2333–42. doi: 10.1016/j.spinee.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 35.Cheatham SW, Lee M, Cain M, Baker R. The efficacy of instrument assisted soft tissue mobilization: a systematic review. J Can Chiropr Assoc. 2016;60:200. [PMC free article] [PubMed] [Google Scholar]
- 36.Chu ECP, Wong AYL, Sim P, Krüger F. Exploring scraping therapy: Contemporary views on an ancient healing – a review. J Fam Med Prim Care. 2021;10:2757. doi: 10.4103/jfmpc.jfmpc_360_21. [DOI] [PMC free article] [PubMed] [Google Scholar]