Abstract
Injuries from stingray fish are among the most common fish stings, and their frequency is increasing with the increase in global tourism. It most commonly causes injuries to the extremities and causes morbidity if not treated appropriately. Less commonly, life-threatening injuries can be observed due to injuries in the thorax and abdomen and damage to large vessels and vital organs. In addition to severe pain, tissue necrosis, and secondary infection after injury, systemic symptoms may occur. Since these injuries can occur in both fresh and salt water, it is possible to encounter such a case at any time. Flat spines are sharp, with backward barbs or serrations that make them difficult to extract once they penetrate tissue. After first aid, surgical extraction of the stingray spine with minimal damage is essential in addition to local and systemic treatments. In the literature, there are studies on envenomation and other systemic findings after stingray spine injuries, but few publications are available on the stingray spine extracted technique after injury. This case report presents a new and helpful technique for stingray spine extraction.
Keywords: Marine envenomation, Stingray injury, Stingray spine extraction technique
Highlights
Injuries from stingray fish are among the most common among fish stings. Surgical extraction of the stingray spine with minimal damage is important in addition to local and systemic treatments.
Although there are case report level publications about stingray injuries, sufficient information has not been shared about the removal of the thorn part that penetrates the tissue.
In this case report, the experience of surgical removal of the stingray needle, especially in hand injuries, was described.
Introduction
The stingrays are a group of cartilaginous fish that can live in tropical marine waters and fresh waters. Stingray-related injuries are among the most common causes of fish stings.1 When stingrays are stepped on or contacted, they can harm people with their tail. Because stingrays camouflage in the sand, stingray stings are most commonly seen as lower extremity injuries due to contact of swimmers, especially in shallow waters. It is possible to encounter a stingray injury at any time in the emergency services of hospitals in coastal areas. Stingray fish have backward barbs or serrations on both sides of the flat spines. Stingray barbs extending in the opposite direction of the entry direction of the stingray spine make it difficult to remove the spine fragment remaining in the tissues after stingray stings. Since stingray spines are radiopaque, direct radiographs are helpful in terms of localization. Magnetic resonance imaging or ultrasound can be used to detect radiolucent cartilage or sheath fragments.2 Since these injuries are mostly seen in young people and ulcerated lesions can heal in 2-3 months, they cause morbidity and increase health costs and loss of work.3
In this case report, a patient with right hand thumb injury after touching a stingray caught in a net, which the fisherman thought to be dead, is presented. The experience of surgical removal of the stingray needle, especially in hand injuries, was shared.
Case Presentation
A 41-year-old male patient was admitted to the emergency department of our hospital due to injury from the volar face of the distal phalanx of the right thumb, with a stingray spine. From the patient’s story, it was understood that he was a fisherman and that he was pulling the dead stingray, which he thought was dead, from the net in the morning. It was learned that the patient had severe pain at the time of the first injury and decreased over time. Anterior posterior and lateral hand radiographs were taken. It was observed that the stingray spine advanced to the distal phalanx bone of the right thumb and came into contact with the bone (Figure 1A, B). Neurovascular examination was normal.
Figure 1. A, B.
(A) Stingray spine in the thumb. (B) Penetration of the spine up to the bone in the distal phalanx on the right hand AP radiograph.
Verbal informed consent was obtained from the patient.
Surgical technique
After the patient’s hand was irrigated with saline, skin antisepsis was provided with povidone iodine in the emergency room. Digital block was applied to the thumb of the right hand with local anesthetic. The surgical procedure performed is shown with an illustration (Figure 2A-D). The incision was widened approximately 0.5 cm in both longitudinal directions from the wound in which the stingray spine was inserted. Backward barbs or serrations flat at spine of the stingray make it impossible to extract the spine from penetrating tissue. The tissues wrapped around the barbs or serrations extending in the opposite direction in the tail of the stingray were removed from the spines with the help of clamp and scalpel. A second clamp was placed on the cleaned side by the assistant for retraction so that the removed tissues would not become entangled in the needles again. Then, the spine was removed after the same procedure was applied to the other side. After irrigation of the wound site with saline, the skin wound was left to heal secondary. A tetanus vaccine was administered. The patient was followed for 6 h, since no pathology was detected in the routine blood tests and electrocardiography taken at the first visit. After that, he was discharged with the prescription of antibiotics and the recommendation of outpatient control for wound follow-up and dressing. The patient was seen in the outpatient clinic on the 3rd and 14th postoperative days. Wound healing was achieved without complications. The removed spine is shown (Figure 3).
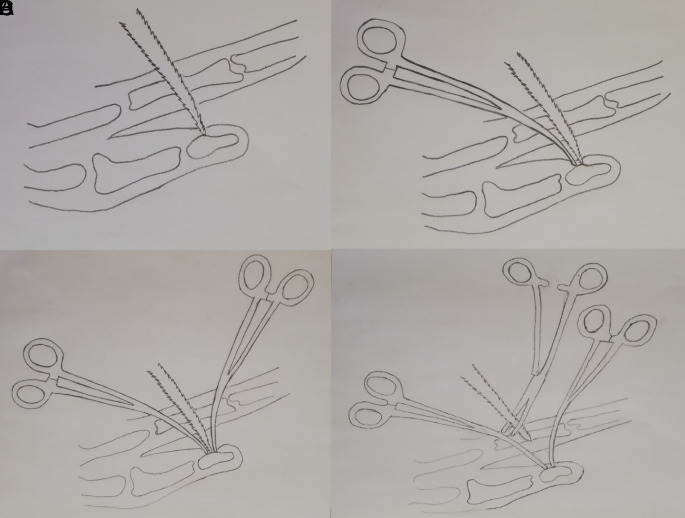
Figure 2. A-D.
Illustration of the surgical procedure is shown. (A) After the patient was prepared for the surgical procedure, the wound was extended 0.5 cm distally and proximal in its longitudinal axis. (B) After the soft tissues around the spine were released with the help of a clamp, the clamp was left in place so that the released soft tissues would not become entangled with the thorns again. (C) The same procedure was done with a second clamp on the other side of the spine, and both clamps were left in place. (D) After the soft tissues were released from both sides of the spine and retraction was done with the help of clamps, the spine was safely removed without damaging the tissues.
Figure 3.
The extracted stingray spine.
Discussion
There are 750-2000 stingray injuries each year in the United States, and stingray fish account for 92.2% of 2317 water-related injuries in the Amazon River.4 There are approximately 150 species of stingrays in the world.5 Their length varies from a palm to 12 feet, and their spines can be 42 cm.1 Stingrays are commonly found in shallow intertidal waters, including sheltered bays, lagoons, estuaries, and sandy areas, and stay between reefs in tropical, subtropical, and warm temperate oceans.6 Stingray victims are generally divided into 2 categories: swimmers or fishermen who walk in shallow water and accidentally step on the fish, often injuring their feet or legs when the fish pushes its tail up and forward in self-defense. Fishermen who remove stingrays from their nets and hooks also often injure their upper extremities. Shoes or clothing do not provide adequate protection.7
On the underside of the spine, there are 2 furrows along the spine longitudinally filled with venom-secreting cells. All these structures are covered with a thin cover sheath. When the stingray spine penetrates the victim’s tissues, the venom-containing sheath ruptures and the venom is released into the wound.8 Stingray injuries cause locally severe pain, erythema, edema, ulceration, and skin necrosis and may result in secondary infections and retention of spine fragments in the wound. The spines left in the wound may continue to release venom and may predispose to delayed wound healing, septic wound necrosis, foreign body reaction, osteomyelitis, and, rarely, necrotizing fasciitis. It has been shown that intervention in wounds in the first 24 hours is important in reducing the risk of infection.9 Irrigation of the wound in 43-46°C water for 30-90 minutes is very important for the inactivation of the heat-labile toxin and for the relief of pain. It is necessary to be wary of thermal damage. Pain can be reduced by narcotic analgesics, local anesthetic infiltration, or nerve block.10 Although infection is common in these injuries, prophylactic antibiotic use is controversial, but it is often necessary. Tetracycline, quinolones, third-generation cephalosporins, chloramphenicol, and trimethoprim/sulfamethoxazole (co-trimoxazole) are suitable options for empirical therapy. Tetanus vaccine should be administered.5
Conclusion
Although there are case report level publications about stingray injuries, sufficient information has not been shared about the removal of the thorn part that penetrates the tissue. As far as we know, there is only 1 publication in the literature on surgical extraction of the stingray spine. Cappa et al11 suggested placing curved-type forceps on both sides of the spine for stingray spine extraction. In our case experience, it is very difficult to separate the tissues wrapped around the spines extending in the opposite direction without the aid of a scalpel and clamp. After the tissues are separated from one side of the spine with the help of a clamp and scalpel, when the other side is passed, the tissues are re-wrapped around the spines in the first cleaned areas. Therefore, we think that the surgical technique we applied in this case may be beneficial. It is important that the surgical method to be applied with the help of the technique we recommend in these injuries, which are common throughout the world, can be applied with simple equipment. We emphasize that in our technique, after the tissues are separated on one side, a clamp can be placed between them for retraction, to prevent the soft tissues from re-wrapping the spine. In our technique, we think that if the spine perforates a tendon, artery, nerve, or joint tissue, spine can be extracted with the same surgical technique. The main problem here is that the barbs become entangled in the surrounding tissues again. We emphasize that with the technique we have described, a smaller approach and clamps can be a solution to this problem. In large artery and organ injuries, the stingray spine can be removed with a larger approach. It may require vascular and nerve repairs. If the spine impales inside the bone tissue, it can be extracted from bone tissue with a larger approach and with the help of osteotomes or drill-like instruments.
Footnotes
Informed Consent: Verbal informed consent was obtained from the patient.
Author Contributions: Concept - M.S.A.; Design - M.S.A.; Supervision - M.S.A.; Materials - M.S.A.; Data Collection and/or Processing - M.S.A.; Analysis and/or Interpretation - Ş.Y.; Literature Review - S.A.U., F.D.; Writing - S.A.U., F.D., Ş.Y.; Critical Review - M.S.A., Ş.Y.
Acknowledgments: Special thanks should be given to Ms. Gülfer ÇAVLI for her drawing of Figure 2.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Rensch GP, Elston DM. Aquatic antagonists: stingray injury update. Cutis. 2019;103(3):138 140. [PubMed] [Google Scholar]
- 2. Docter TA, Altschuh LB, Medak AJ.et al. Comparison of radiographic, ultrasound, and magnetic resonance imaging for the detection of retained stingray barb: a cadaveric study. Wilderness Environ Med. 2021;32(3):302 307. 10.1016/j.wem.2021.03.012) [DOI] [PubMed] [Google Scholar]
- 3. Monteiro WM, Oliveira SS, Sachett Jde A, Silva IM, Ferreira LC, Lacerda MV. Hallux amputation after a freshwater stingray injury in the Brazilian Amazon. Rev Soc Bras Med Trop. 2016;49(3):389 392. 10.1590/0037-8682-0333-2015) [DOI] [PubMed] [Google Scholar]
- 4. Holanda MNd, Câmara OF, Silva DDd.et al. Accident and vascular injury with stingray in the Alto Juruá, Acre, Brazil: a case report. J Hum Growth Dev. 2019;29(3):427 432. 10.7322/jhgd.v29.9542) [DOI] [Google Scholar]
- 5. Haigh K, Delbridge P, Meda K, Chilamkurthi R. Stingray envenomation in a returning traveller: a complicated disease course. BMJ Case Rep. 2019;12(7):e228644. 10.1136/bcr-2018-228644) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Germain M, Smith KJ, Skelton H. The cutaneous cellular infiltrate to stingray envenomization contains increased TIA+ cells. Br J Dermatol. 2000;143(5):1074 1077. 10.1046/j.1365-2133.2000.03848.x) [DOI] [PubMed] [Google Scholar]
- 7. Meyer PK. Stingray injuries. Wilderness Environ Med. 1997;8(1):24 28. 10.1580/1080-6032(1997)008[0024:si]2.3.co;2) [DOI] [PubMed] [Google Scholar]
- 8. Diaz JH. The evaluation, management, and prevention of stingray injuries in travelers. J Travel Med. 2008;15(2):102 109. 10.1111/j.1708-8305.2007.00177.x) [DOI] [PubMed] [Google Scholar]
- 9. Sachett JAG, Sampaio VS, Silva IM.et al. Delayed healthcare and secondary infections following freshwater stingray injuries: risk factors for a poorly understood health issue in the Amazon. Rev Soc Bras Med Trop. 2018;51(5):651 659. 10.1590/0037-8682-0356-2017) [DOI] [PubMed] [Google Scholar]
- 10. Yılmaz F, Tülübaş GA, Selvi F, Bağlı Doku Laserasyonu VBS, Bulgular S. Olgu sunumu. Acta Med Alanya. 2018;2(3):215 217. [Google Scholar]
- 11. Cappa G, Barcella B, Pettenazza P. Extraction procedure of a stingray spine. J Travel Med. 2020;27(6):taaa137. 10.1093/jtm/taaa137) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a