Introduction
Globally, as one of the leading causes of mortality among human beings, acute myocardial infarction (AMI) brings threatens even younger individuals. Although it has been widely noted that plaque rupture is the most common etiology of MI, several other classifications of MI resulting from different etiologies are more prevalent in special subsets, including coronary embolism, spontaneous coronary artery dissection, and coronary spasm.1 Graft-versus-host disease (GVHD) is an adverse immunologic phenomenon following allogenic hematopoietic stem cell transplantation. Chronic GVHD accounts for a much higher, long-term mortality, morbidity, and poorer prognosis.2 The bone marrow transplantation (BMT) has been demonstrated as an advantageous therapeutic approach for these patients, while the preparative regimen for allogeneic BMT and the subsequent long-term immunosuppression may induce atherosclerosis of coronary artery.3 In this case report, a young patient diagnosed with AMI is described, which was ascribed to intra-coronary thrombosis due to GVHD after excluding any other causes.
Case Report
A 13-year-old patient was admitted to our hospital due to persistent chest pain for about 4 hours. He was first diagnosed with acute T lymphocyte leukemia at the age of 5 and received 9 cycles of chemotherapies. Harvested from his father, the mediastinal radiotherapy and semi-compatible bone marrow stem cell transplantation were performed in 2016 (when he was 8) due to leukemia recurrence accompanied by extramedullary mediastinal infiltration. The classical multiorgan chronic GVHD involving the liver and skin occurred after 3 years.
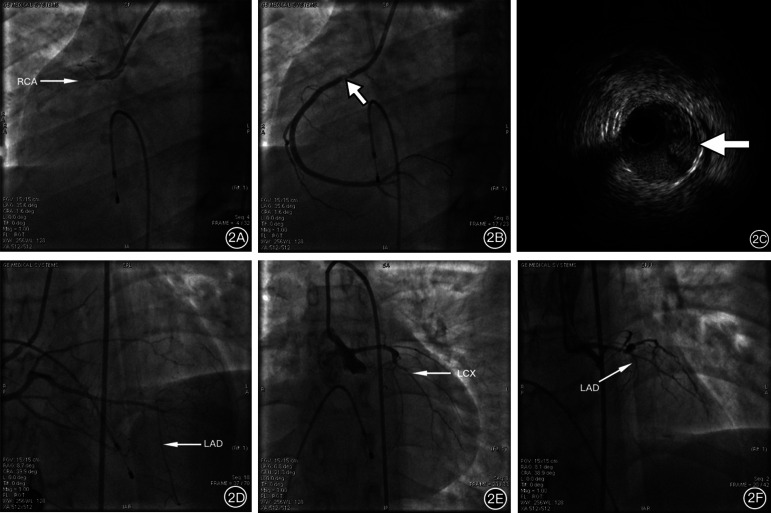
On admission, physical examination and laboratory detection were performed. Through electrocardiogram (ECG), ST-segment elevation in the leads of II, III, and arteriovenous fistula (aVF) (Figure 1A) was observed. The hypokinesis of the inferior wall and posterior wall in the left ventricle was suggested via ultrasonic cardiogram, while no specific findings were shown by computed tomography angiography of pulmonary artery and thoracic aorta. In addition, a gradual increase in trend toward the serum myocardial injury markers and abnormal liver function was detected. The patient then underwent emergency coronary angiography (CAG) for the suspicion of acute myocardial infarction (AMI). As expected, diffused coronary artery lesions were observed (Figure 2), and a thrombotic occlusion was located in the opening of the right coronary artery (RCA, Figure 2A, Video 1). At the same time, severe chronic diffuse lesions of the left coronary artery (LCA) cannot be ignored, which was manifested as diffuse stenosis of the left circumflex (LCX) (Figure 2E, Video 2) and chronic occlusion of the left anterior descending artery (LAD) (Figure 2F, Video 3). The percutaneous coronary intervention (PCI) in the RCA was then proposed. After crossing the guidewire, angiography showed a significant hypodensity shadow in the opening and proximal segment of RCA (Figure 2B, Video 4). The intravascular ultrasound (IVUS) was performed for further detection with a finding of multiple thrombus in the proximal segment of RCA (Figure 2C, Video 5). After balloon dilation and thrombus aspiration, the blood flow was restored to thrombolysis at myocardial infarction grade 3 level, while collateral circulation to the LAD was observed (Figure 2D, Video 6). Electrocardiogram further showed a decrease of ST segment in the leads of II, III, and aVF (Figure 1B). With the above diagnosis, the patient was treated with secondary preventive drugs for coronary artery disease as appropriate and discharged without any symptoms a few days later.
Figure 1.
Results of electrocardiogram before (A) and after (B) PCI [A: ST segment of II, III, and aVF leads was significantly elevated; B: ST segments of II, III, and aVF leads decreased after operation]. PCI, percutaneous coronary intervention; aVF, arteriovenous fistula.
Figure 2.
Results of coronary angiography and IVUS [A: RCA opening occluded (arrow); B: Low-density shadow can be seen in the near segment after RCA opening (arrow); C: IVUS confirmed acute intra-coronary thrombosis (arrow); D: Collateral circulation from RCA to LAD can be seen after RCA opening (arrow); E: Diffuse stenosis from mid-segment to distal segment of LCX (arrow); 2F: proximal chronic occlusion of the LAD (arrow)]. IVUS, intravascular ultrasound; RCA, right coronary artery; LAD, led anterior descending artery; LCX, left circumflex.
Discussion
The case presented herein reported the youngest-ever patient with GVHD and diagnosed with AMI, without any coronary atherosclerotic risk factors. Rather than caused by the rupture of atherosclerotic plaque, the development of acute thrombosis in the culprit vessel is suggested to be related to GVHD-induced endothelial injury based on the IVUS results.
Bone marrow transplantation (BMT) is a potential curative therapy strategy for a variety of malignant or benign hematological diseases, while GVHD is a common complication (40%-60%) and a leading cause of increased morbidity and mortality among patients receiving BMT. With limited reports of coronary artery as the target organ, it had been reported that GVHD could most notably occur in the skin, lungs, gastrointestinal tract, liver, mucosa, and musculoskeletal system.4 Regarding this case, the causes of acute coronary thrombosis were analyzed, and the chronic liver damage was suggested based on the observation of liver enlargement and elevated alanine aminotransferase (ALT) level after receiving BMT in 2016. In recent years, literature about GVHD-related acute adverse cardiovascular events has been increasing.5-9 Ascribed to AMI as well, Chan et al5 once reported sudden death of a 19-year-old patient with refractory leukemia 30 months after BMT, who suffered from severe GVHD. In addition, Rackley et al6 reported 3 cases of GVHD-related sudden death, which was confirmed to be related to serious coronary artery disease by autopsy. Further, Prevost et al7 reported a case of GVHD-related AMI, for which the acute coronary occlusion was confirmed in terms of histology through detection of subintimal inflammatory cell infiltration and fibrous proliferation. Regarding the above-reported diagnosis, coronary endothelia is then suggested as a potential target of graft-versus-host immune responses in GVHD patients.
Another concern about this case is the diffused stenosis in the LCA (Figure 2E-2F). Mediastinal radiotherapy received by this patient and the possibility of related radio-related cardiovascular disease should then be considered. Patients with radio-related cardiovascular disease typically presented among a younger age group without traditional risk factors of coronary atherosclerosis, a history of radiotherapy, or symptoms associated with myocardial ischemia. Generally, the opening and proximal segments of the coronary artery are always observed with severe and diffuse stenosis via CAG, while IVUS and optical coherence tomography will show infiltration of non-calcified fibrous and fibrous fatty plaques in the relevant lesions. In this case, the CAG suggested diffuse lesion of LCX and proximal occlusion of LAD. According to the expert consensus from the European Association of Cardiovascular Imaging and American Society of Echocardiography,10 the relevant risk factor for the young patient received 2 courses of mediastinal radiotherapy near the heart, and the cumulative radiotherapy dose was 34 Gy. As a result, except for AMI, the patient could also be diagnosed with radiation-related cardiovascular disease.
Conclusion
The intra-coronary thrombosis was believed to be induced by chronic GVHD, thus contributing to the occurrence and progression of AMI in this patient. With a reminder of more attention required to be paid to the particularity in younger populations with AMI with respect to the etiology, for the young age group with radiotherapy history, the radiation injury of coronary artery cannot be ignored as well based on this case. In general, this case provides a meaningful experience to improve cognition and thus avoid misdiagnosis and missed diagnoses in the clinic.
Footnotes
Informed Consent: Informed consent was signed and given by the patient’s parent.
Acknowledgments: The authors would like to acknowledge the support from the Department of Cardiology, Northern Jiangsu People’s Hospital.
References
- 1. Gulati R, Behfar A, Narula J.et al. Acute myocardial infarction in young individuals. Mayo Clin Proc. 2020;95(1):136 156. 10.1016/j.mayocp.2019.05.001) [DOI] [PubMed] [Google Scholar]
- 2. Ramachandran V, Kolli SS, Strowd LC. Review of graft-versus-host disease. Dermatol Clin. 2019;37(4):569 582. 10.1016/j.det.2019.05.014) [DOI] [PubMed] [Google Scholar]
- 3. Miura T, Izawa A, Kumazaki S.et al. Acute myocardial infarction in a 16-year-old girl with chronic GVHD. Bone Marrow Transplant. 2010;45(10):1576 1577. 10.1038/bmt.2010.21) [DOI] [PubMed] [Google Scholar]
- 4. Munir SZ, Aylward J. A review of ocular graft-versus-host disease. Optom Vis Sci. 2017;94(5):545 555. 10.1097/OPX.0000000000001071) [DOI] [PubMed] [Google Scholar]
- 5. Chan KW, Taylor GP, Shepherd JD, Shepherd WE. Coronary artery disease following bone marrow transplantation. Bone Marrow Transplant. 1989;4(3):327 330. [PubMed] [Google Scholar]
- 6. Rackley C, Schultz KR, Goldman FD.et al. Cardiac manifestations of graft-versus-host disease. Biol Blood Marrow Transplant. 2005;11(10):773 780. 10.1016/j.bbmt.2005.07.002) [DOI] [PubMed] [Google Scholar]
- 7. Prevost D, Taylor G, Sanatani S, Schultz KR. Coronary vessel involvement by chronic graft-versus-host disease presenting as sudden cardiac death. Bone Marrow Transplant. 2004;34(7):655 656. 10.1038/sj.bmt.1704625) [DOI] [PubMed] [Google Scholar]
- 8. Huang S, Martin P, Campbell MJ. Coronary artery occlusion secondary to graft versus host disease after bone marrow transplant in a 21-year-old. Cardiol Young. 2018;28(12):1484 1486. 10.1017/S1047951118001592) [DOI] [PubMed] [Google Scholar]
- 9. Scudiero L, Soriano F, Morici N.et al. Allogeneic peripheral blood stem cell transplantation and accelerated atherosclerosis: an intriguing association needing targeted surveillance. Lessons from a rare case of acute anterior myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2020. ;9(7):NP3 NP7. 10.1177/2048872616652311) [DOI] [PubMed] [Google Scholar]
- 10. Lancellotti P, Nkomo VT, Badano LP.et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14(8):721 740. 10.1093/ehjci/jet123) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a