Abstract
Objective:
The aims were to study the time course and underlying causes of deaths in children under 1 year of age in a high Human Development Index municipality. We also sought to define the relationship between the timing of death and the neonatal age range and observed the extent to which deaths were avoidable.
Materials and Methods:
Retrospective study of women living in the city of Niterói, Brazil, between 2012 and 2018. Data were collected from death certificates provided by hospitals. The chi-square test was used for categorical variables, while continuous variables were first analyzed descriptively (mean, standard deviation), followed by parametric or non-parametric methods.
Results:
A total of 455 deaths were recorded, with a normal distribution over time (P = .120). The mean age at death was 212.70 days [30 weeks = 7.5 months], with 17 children dying before age 28 days (3.7%). The sample was predominantly male (55.6%) and white (48.4%). The average gestational age was 31.2 weeks and the average birth weight was 1733.95 g, with 305 infants weighing < 2499 g (70.1%). Bacterial sepsis ([International Classification Diseases-10 P36.9]; n = 35; 7.7%) was the most commonly cited cause of death. International Classification Diseases-10 Chapters XVI (conditions—perinatal period [P00-P96]; n = 229; 50.3%) predominated. Infants who died in the neonatal period had a lower mean gestational age (P < .001) and weight (P < .001) compared to post-neonatal deaths.
Conclusion:
Infant mortality has remained stable at tolerable levels in this municipality. Sepsis remains the leading cause of death, and mortality is directly associated with prematurity/ low birth weight, a multifactorial problem.
Keywords: Avoidable causes of death, infant mortality, morbidity, newborn, preterm
What is already known on this topic?
Although mortality in the first year of life is decreasing, causes of death related to poor antenatal, perinatal, and neonatal care remain prevalent.
Early neonatal death is often related to asphyxia in the delivery suite.
Most neonatal causes of death are preventable, mainly those due to inadequate maternal care during pregnancy.
What this study adds on this topic?
Deaths in children under 1 year of age in Niterói have been rare, and the mortality curve is expected to remain stable.
ICD-10 Chapters XVI and XVII accounted for most causes of death, and sepsis was the leading cause.
Prematurity, including extreme prematurity, was the core factor implicated in mortality.
Introduction
Since 1990, worldwide neonatal, infant (<1 year), and child (<5 years) mortality rates have declined and continue to decline rapidly, and childhood life expectancy over the past three decades has been remarkably positive.1 In Brazil, over the same period, infant mortality rates fell 70%, although they remain unevenly distributed across the different regions of the country.2 It is still of paramount importance to analyze data related to cases of infant mortality, with particular attention to their potential avoidability, which, when present, is closely linked to the quality of medical intervention. Furthermore, it is essential that human development in the region from which the data were obtained should be evaluated in parallel.
Despite some improvements in the public Unified Health System (SUS—Sistema Único de Saúde) in several cities across Brazil, such as Rede Cegonha,3,4 the Mobile Emergency Care System (Sistema de Atendimento Móvel de Urgência) and the implementation of freestanding urgent care centers (Unidades de Pronto Atendimento),5 the municipality of Niterói, in the state of Rio de Janeiro, has experienced a steady decline in mortality rates over the years.6 The search for a 0-death scenario remains desirable, and within this context, some questions and hypotheses remain, including whether adverse maternal parameters are directly related to death and whether respiratory causes have a direct relationship with neonatal death. Additional information was also sought regarding the age groups most represented among deaths within the first year of life, to establish whether there was a neonatal predominance among infant deaths.
Therefore, the aims were to study the root causes of infant death through an analysis of the corresponding International Classification of Diseases (ICD-10) codes and define which deaths had a close relationship with prematurity, low birth weight, and young maternal age, as well as ascertain the avoidability of lethal outcomes. We also sought to identify maternal and child characteristics associated with neonatal deaths and establish a temporal correlation between birth and death in the city.
Materials and Methods
Study Design, Setting, and Participants
This was a retrospective review of data contained in death certificates as provided by hospitals. All deaths of children under 1 year of age occurring between January 2012 and December 2018 in the municipality of Niterói, Rio de Janeiro, Brazil. The study database was constructed from information provided by the Coordination of the Health Observatory (Coordenação do Observatório da Saúde, COOBS). This operational sector of the Municipal Health Department is responsible for controlling and relaying to the state governments’ all official information regarding births and deaths which take place within the municipality. Data were collected from all children of all women living within the municipality of Niterói during the study period (Research Ethics Committee: 23136714.7.0000.5243).
Data Sources
Data were obtained from death certificates,7 which record a total of 59 variables distributed across 9 blocks. For this study, 47 of these 59 variables were analyzed: 7 continuous (age of child and mother, number of living and dead children, number of pregnancies, age in gestational weeks, and child weight) and all others categorical (some dichotomous, others with multiple categories). The variables set aside for analysis were contained in block I (field 1: manner of death; 2: date and time of death; 8: date of birth; 9: age in days; 10: sex; 11: race/skin color), block III (field 20: place of death; 21: facility, with National Register of Health Establishments (CNES) number; 25: municipality of death), block IV (field 27: age in years; 28: educational attainment; 29: usual occupation, with 2002 Brazilian Classification of Occupations (CBO) code8; 30: number of live births and fetal losses; 31: weeks of gestation; 32: type of pregnancy; 33: mode of delivery; 34: death in relation to childbirth; 35: birth weight in grams), and block V (field 40). Field 40 recorded the cause of death, with part I used to describe the disease or condition that directly caused the death and any antecedent causes (morbid conditions that led to the proximate cause, and ultimately, the underlying cause) and part II set aside for other significant conditions that contributed to the death but were not part of the actual causal chain. Morbid conditions were described by their ICD-10 codes.9
Variables and Groups
The continuous variables maternal (age, gestational age, and birth weight) were recorded into categorical variables. Maternal age was recorded into categories of 20, 18, and 16 years. For analysis of gestational age, the following classification was used: 1 = <27.6 weeks (extreme prematurity); 2 = 28-31.6 weeks (moderate prematurity); 3 = 32-36.6 weeks (late prematurity)10; 5 = 37-41.6 weeks (full term); 6 = >42 weeks (post-term). Birth weights were recorded using the following classification: <1000 g (extremely low birth weight); 1000-1499 g (very low birth weight); 1500-2499 g (low birth weight) (World Health Organization—WHO); and ≥4000 g (macrosomia). Age at death was recorded as early neonatal death (0-6 days), late neonatal death (7-27 days), neonatal death (0-27 days), post-neonatal death (28-364 days), and infant death (0-364 days),11 and the month in which the death occurred was established. Two dichotomous variables were created to verify the association between maternal, birth, and neonatal data with the occurrence of death before or after 28 days of life (neonatal vs. post-neonatal) and before or after 182 days (first vs. second semester of life).
To calculate the death rate per 1000 live births, the following formula was used: total number of deaths under 1 year of age/total number of live births in the city of Niterói × 1000.
In addition to define the main frequencies of underlying causes for the entire study group, the various ICD codes recorded were defined for groups of preterm versus not preterm (0/1), low birth weight versus non-low birth weight (0/1), mothers under 16 and 18 years of age (0/1), and death in the neonatal period or outside this period (0/1).
The concept of avoidability as described by Malta et al12 was adopted for purposes of analysis, and the 2010 update of their list of avoidable causes of death was used as a theoretical framework for discussing the data found.
Statistical Analysis
Continuous variables, in addition to general descriptive statistics (mean, median, minimum [min] and maximum [max], 95% CI, standard deviation [SD]), were tested for normality of distribution (Shapiro–Wilk method) to define whether subsequent methods would be parametric (t-test or ANOVA—variables: number of births and deaths in the city) or non-parametric (Mann–Whitney or Kruskal–Wallis test—variables: maternal and child age, number of living and deceased children, number of pregnancies, gestational age, and birth weight). Likewise, Pearson’s or Spearman’s tests were used to verify the correlation between the frequencies of births and deaths over time. The correlation coefficients were categorized as follows: >0.9, very strong; 0.7-0.9, strong; 0.5-0.7, moderate; 0.3-0.5, weak; and 0-0.3, negligible. A generalized model followed by Bonferroni’s post hoc test was used to verify significant differences in birth and death scores (dependent variables—continuous) between years (independent variable—categorical). Model type (linear, gamma, or Poisson) was defined according to the lowest Akaike information criterion (AIC). For graphic representation, estimation curves for births and deaths (dependent variable) over the 7-year study period (independent variable) were plotted since both variables showed a normal distribution.
Scatter plots were also generated to assess the relationship of birth weight (dependent variable) with maternal age and number of pregnancies (independent variables), seeking the best model (linear, quadratic, or cubic) from the R2 values; the higher the values, the more suitable the curves.
The frequency and valid percentages for binary or non-binary categorical variables were taken into account. Pearson's chi-square and Fisher's exact test verified, from cross-tabulations, the relationship between the binary categorical variable (death <28 days vs. >28 days) and maternal, birth, and neonatal characteristics.
The significance value was set at P < .05 for all tests. Statistical analyses were performed in International Business Machines Statistical Package for the Social Sciences Statistics®, Version 24.0 and Excel (Microsoft)®.
Results
Period of Analysis
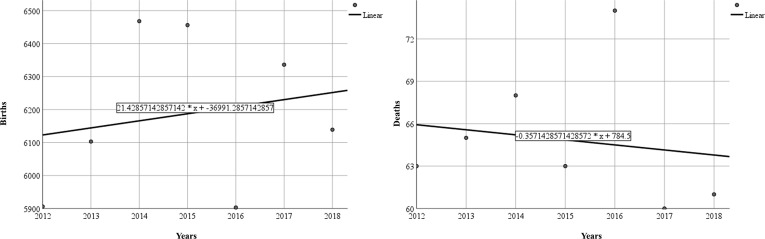
During the period of analysis, there were 43 311 births in the city, with an annual average of 6187.29 births (95% CI: 5966.32-6408.25; median: 6139.00; SD: 238.92; min: 5903; max: 6468). There were 455 deaths during the period of analysis, with an annual average of 64.86 (95% CI: 60.41-69.31; median: 63.00; SD: 4.81; min: 60; max: 74). Calculation of infant mortality rates in the period revealed an average of 10.5 deaths per 1000 live births. When the correlation with the timeline was tested, it was established to be positive and non-significant (r = 0.194) in relation to births and negative and non-significant in relation to deaths (r = −0.133), which was well demonstrated by the annual distributions (Figure 1).
Figure 1.
Scatter plots between births and deaths with timeline.
Using the Poisson probability distribution, the estimated means showed significant variations in births over the years (particularly a progressive rise from 2012‐2015 and a significant decline in 2016), while deaths did not show any major differences in annual rates (P > .05). A cubic equation best represented the dispersion of points between low birth weight and maternal data (maternal age and number of pregnancies) (Figure 2).
Figure 2.
Scatter curves of correlation between maternal age (A) and number of pregnancies (B) with birth weight.
Infant Data
Analysis of death certificate fields (block 1) showed that all 455 deaths were non-fetal and occurred predominantly during the day (n = 227; 51.0% valid). The mean age at death was 212.70 days ([30 weeks = 7.5 months]; 95% CI: 204.71-220.70; median: 210.00; SD: 86.78; min: 1; max: 311). The distribution was non-normal, and only 17 children died before 27 days of age (3.7%). Of these, only 1 child died within the first 24 hours of life (0.2%), while 8 deaths occurred in the first 6 days (1.8%) and 9 between 7and 27 days (2,0%), characterizing early and late neonatal deaths. Among deaths occurring <27 days, the median age at death was 10 days, while among deaths occurring >28 days, the median age at death was 211 days. Deaths occurred predominantly in the post-neonatal period (n = 438; 96.3%) and there were only 109 deaths (24.0%) in the first 6 months (182 days); the majority occurred in the second half of the first year (n = 346; 76.0%). The age range in which most fatalities occurred was between 301and 330 days of life (10-11 months: n = 165; 36.3%), followed by 181-210 days (6-7 months: n = 126; 27.7 %), and 91-120 days (3-4 months: n = 69; 15.2%).
Decedents were predominantly male (n = 253, 55.6%; of the 17 who died within the first 27 days of life, 15 were boys) and White (n = 202; 48.4%), followed by Brown (n = 166; 39.8%) and Black (n = 49; 11.8%) infants.
Regarding the site of death (block III), among the 56 facilities listed in the medical records, 1 hospital (a state-run facility) accounted for a plurality of deaths (n = 129; 29.7% valid), followed by the federal hospital located in the municipality (n = 51; 11.8%) and by a private hospital (n = 33; 7.6% valid). Most deaths occurred in public hospitals (n = 278; 64.1% valid) in the municipality of Niterói (n = 331; 76.3% valid), followed by the municipality of Rio de Janeiro (n = 75; 17.3%).
Maternal Data
Regarding maternal data (block IV), the mean age was 27.36 years (95% CI: 26.63-28.08; median: 27.00; SD: 7.60; min: 13; max: 45). This parameter was not normally distributed. Overall, 13 mothers were under age 16 (3.1% valid), 47 (11.1%) were under age 18, and 84 were under 20 years old (19.8%); conversely, 25 mothers were over age 40 (5.9%). Most mothers had completed secondary education (high school) (n = 160; 38.4% valid), followed by middle school (fifth to eighth grade) (n = 95; 22.8%); 85 women in the sample (20.4%) had a higher education. Most had completed more than 8 years of formal education (n = 268; 68.0%). Surprisingly, 7 women (1.7%) had no schooling. Regarding occupation, homemaker [CBO 2002 code 999992] was the most common (n = 148; 44.2% valid), followed by student [CBO 2002 code 999991] (n = 38; 11.3%) and lawyer [CBO 2002 code 241005] (n = 14; 4.2%). The average gestational age was 31.29 weeks (95% CI: 30.68-31.90; median: 31.00; SD: 6.20). Singleton pregnancies were predominant (n = 392; 89.7% valid), with only 43 (9.8%) twin pregnancies. Only 123 pregnancies (30.6%) exceeded a gestational age of 37 weeks. On the other hand, 141 (35.2%) represented extreme prematurity (gestational age <27 weeks and 6 days). Late prematurity represented only a small portion of pregnancies (n = 43; 10.7%) among those born below 36 weeks and 6 days (n = 278; 69.3%). Cesarean section was the predominant mode of delivery (n = 246; 56.4%), and all deaths occurred after birth.
The mean birth weight was 1733.95 g (95% CI: 1631.03-1836.87; median: 1390.00; SD: 1092.15; min: 308; max: 4492), with 305 newborns weighing less than 2499 g (70.1% valid) and 7 weighing more than 4000 g (1.6%). Among those weighing less than 2500 g, extremely low birth weight (<1 kg) was prevalent (n = 167; 38.4%); 36 infants were born weighing less than 499 g (8.3%). Average birth weight did not differ significantly across the various years of the study period (2012 = 1621.98; 2013 = 1706.88; 2014 = 1615.94; 2015 = 2069.26; 2016 = 1869.51; 2017 = 1552.61; 2018 = 1671.07; P = .142).
International Classification of Diseases
Among the 153 alphanumeric ICD-10 codes cited as underlying causes of death (block V), the most common ones were bacterial sepsis ([P36.9]; n = 35; 7.7%; mean of 5 deaths per year) and neonatal respiratory distress syndrome ([P22.0]; n = 21; 4.6%, mean of 3 deaths per year). ICD-10 Chapters XVI (certain conditions originating in the perinatal period [P00-P96]; n = 229; 50.3%) and XVII (congenital malformations, deformations, and chromosomal abnormalities [Q00-Q99]; n = 120; 26.3%) (Table 1) were those most represented.
Table 1.
International Classification of Diseases Chapters Implicated in Deaths
| Chapters | Groups | N | % |
|---|---|---|---|
| Chapter XVI: certain conditions originating in the perinatal period (P00-P96) | P | 229 | 50.33 |
| Chapter XVII: congenital malformations, deformations, and chromosomal abnormalities (Q00-Q99) | Q | 120 | 26.37 |
| Chapter I: certain infectious and parasitic diseases (A00-B99) | A+ B | 29 | 6.374 |
| Chapter XX: external causes of morbidity and mortality (V01-Y98) | V W X Y | 23 | 5.055 |
| Chapter X: diseases of the respiratory system (J00-J99) | J | 21 | 4.615 |
| Chapter XVIII: symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (R00-R99) | R | 9 | 1.978 |
| Chapter VI: diseases of the nervous system (G00-G99) | G | 8 | 1.758 |
| Chapter IX: diseases of the circulatory system (I00-I99) | I | 5 | 1.099 |
| Chapter II: neoplasms (C00-D48) | C+D | 4 | 0.879 |
| Chapter IV: endocrine, nutritional, and metabolic diseases (E00-E90) | L | 4 | 0.879 |
| Chapter XIV: diseases of the genitourinary system (N00-N99) | N | 2 | 0.44 |
| Chapter XI: diseases of the digestive system (K00-K93) | K | 1 | 0.22 |
| Total | 12 | 455 | 100 |
Timeline analysis showed that the number of ICD-10 codes recorded as causes of death per year ranged from 36 to 54 and that Chapter XVI codes (bacterial sepsis, premature rupture of membranes, maternal urinary tract problems, respiratory distress syndrome) predominated in all years, with the exception of 2015, in which Chapter XVII codes (chromosomal abnormalities) prevailed. Underlying cause of death was homogeneous across maternal age ranges (under 15, 18, or 20 years) and sex of the newborn, with sepsis always ranked first. In neonates with a gestational age >37 weeks and birth weight > 2500 g, unspecified congenital malformation of the heart [ICD-10 code Q24.9] was the most frequent cause. Interestingly, among deaths occurring after the 28th day of life, sepsis was the predominant cause, while in newborns under 28 days old, the most common causal factor was very low birth weight [P07.0]. When age at death in days and weight in grams at birth were defined by the leading underlying causes of death, wide variation was observed. For instance, sepsis [P36.9] was associated with a mean age at death of 204.31 days (95% CI: 187.98-220.65; median 206.00; SD: 47.54) and birth weight of 1341.00 g (95% CI: 1028.13-1653.87; median 945.00; SD: 896.69), while respiratory distress syndrome [P22.0] was associated with a mean age at death of 149.95 days (95% CI: 113.52-186.38; median 201.00; SD: 80.03) and birth weight of 811.71 g (95% CI: 535.10-1088.33; median 610.00; SD: 607.68).
Infant and Neonatal Deaths
When the cut-off was shifted to 28 days, there were significant differences in gestational age (>28 days: median = 31.64 weeks; <27 days: median = 22.94 weeks), number of pregnancies (>28 days: median = 4.00; <27 days: median = 1.00), and birth weight (>28 days: median = 1535.00; <27 days: median = 492 g) (Table 2).
Table 2.
Relationship Between Neonatal or Post-neonatal Death and Maternal, Birth, and Infant Characteristics
| Variable | Binary Death Age | |||
|---|---|---|---|---|
| Categorical | >28 Days | <27 Days | P (Fisher) | |
| Mother | ||||
| Mother under 20 | <19 | 95 | 4 | .755 |
| >20 | 343 | 13 | ||
| Educational attainment | <8 years | 153 | 3 | .289 |
| >9 years | 285 | 14 | ||
| Hospital—place of death | Non-SUS | 162 | 4 | .316 |
| SUS | 276 | 13 | ||
| Birth route | Vaginal | 183 | 15 | <.001 |
| Cesarean | 255 | 2 | ||
| Day vs. night death | Day | 227 | 6 | .130 |
| Night | 211 | 11 | ||
| Continuous | >28 days | <27 days | P ( M.W) | |
| Maternal age | Mean/SD | 27.32/7.62 | 28.12/7.32 | .621 |
| Number of children alive | Mean/SD | 1.88/1.99 | 1.71/0.72 | .559 |
| Number of deceased children | Mean/SD | 0.93/7.18 | 0.67/0.81 | .146 |
| Gestational age in weeks | Mean/SD | 31.64/6.06 | 22.94/2.72 | <.001 |
| Number of pregnancies | Mean/SD | 3.60/1.65 | 1.56/0.72 | <.001 |
| Infant | ||||
| Categorical | >28 days | <27 days | P ( Fisher) | |
| Sex | Male | 238 | 15 | .006 |
| Female | 200 | 2 | ||
| Low birth weight | <2499 | 298 | 17 | .003 |
| >2500 | 140 | 0 | ||
| Underlying cause of death | ICD | P36.9 | P07.0 | |
| Continuous | >28 days | <27 days | P ( M.W) | |
| Birth weight | Mean/SD | 1780.61/1087.63 | 586.82/263.03 | <.001 |
| Age at death (days) | Mean/SD | 220.51/78.64 | 11.47/7.15 | - |
SUS, unified health system; SD, standard deviation; P-value; M.W, Mann–Whitney test; Fisher, Fisher’s test; NB, newborn; ICD, International Classification of Diseases; P36.9, bacterial sepsis of newborn, unspecified; P07.0, extremely low birth weight newborn.
Discussion
To address our initial research questions, it is clear that adverse maternal parameters (young age, number of deceased children, poor educational attainment, too many children) were not directly associated with deaths and that respiratory conditions were not the main causes of death in the neonatal period. We also found that only a minority of deaths occurred in the neonatal age range.
One extraordinarily important finding was that deaths in the first year of age in the city of Niterói have been declining significantly in recent decades; as the literature shows, the rate was 50.8/1000 live births in 1979 falling to 19.35/1000 live births in 1995.13 In the present study, the rate was 10.5 deaths per 1000 live births, below the estimated 17 deaths per 1000 live births in 2020 (first month of life) and 11 deaths per 1000 births (after the first month and before reaching age 1) reported in global data released by UNICEF.14 The rates were also below the Brazilian averages described by the same agency, namely, 14.7 per 1000 live births under 5 years of age and 13.0 per 1000 in those under 1 year of age.15 Preliminary evidence has shown that a strong role of physicians in primary care has reduced infant mortality in Brazil; increasing staffing to 1 primary care physician per 10 000 people population was associated with a decrease in deaths of children under 1 year of age.16 The relationship between mortality rates and municipal HDI has also been demonstrated. This rate should be a good predictor of infant mortality, and medium and low HDIs are associated with infant mortality.17 The municipality in which this study was conducted was not only one of the first in Brazil to implement the Family Health program but also has one of the finest primary care networks in the country and has consistently ranked among the top 10 cities in Brazil by HDI.18
Maternal data showed an interesting profile: most mothers were at a healthy age for reproduction (27 years), had more than 8 years of formal schooling (secondary/higher education), were occupied as homemakers, had only 1 pregnancy, no previous deceased children, and underwent cesarean delivery of a preterm, singleton child, during the day. Unlike Anele et al.17 who found an association between infant mortality and low maternal education, this group of mothers mostly had a higher level of educational attainment, which may be explained by the high average per capita income in the municipality, large number of educational institutions, and proximity to the city of Rio de Janeiro. Newborns, on the other hand, were predominantly premature, weighing an average of 1700 g, male and white, died in the second semester of life, with sepsis as the predominant cause (remaining as the leading cause in most years of the study period). This is consistent with the findings of Rodrigues et al19 in their report on the progression of infant mortality caused by sepsis in Brazil. In contrast, among infants who died before 28 days of age (the minority of deaths), very low birth weight was the predominant cause. In a study carried out in São Paulo, with a rate of 8 deaths per 1000 live births during the study period, the underlying causes of death were, in order of frequency, respiratory disorders, malformations, infections, and perinatal asphyxia.10
These profiles helped demonstrate the core role of preterm birth—present in 70% of cases in this group—in the causation of infant mortality. Our findings also show that many of the deaths occurring in the first year of life in the city of Niterói could be considered avoidable, as they could be prevented by adequate care during pregnancy and the neonatal period.20 Likewise, Ramalho et al.21 studying infant mortality in Rio Branco, Acre, demonstrated that perinatal diseases—followed by malformations, infectious/parasitic diseases, and respiratory diseases—were the main causes of death. It is worth noting that several strategies have been proposed to mitigate the effects of prematurity, and in a study conducted in Pernambuco, Brazil, Lima et al4 showed the positive impacts of working with 2 such programs (Mãe Coruja Pernambucana and Rede Cegonha) on prenatal and neonatal care to reduce preventable deaths in the state.
Concerning the timing of death, the majority of deaths occurred after the post-neonatal period (93.7%), especially after the second semester of life (76.0%); this group (post-neonatal) had a gestational age and birth weight higher than those infants who died before 28 days (32 vs. 22 weeks and 1.780 vs. 586 g, respectively). In contrast, in Asia and Africa, neonatal health is improving slowly compared to that of other childhood groups, and in the last decade, most children still died within the first 28 days of life.22
Regarding the performance of the hospital network, children who died in non-Unified Health System facilities had significantly older mothers, and deaths predominated significantly in the Unified Health System network at every month throughout the study period.
Some limitations of the present study must be noted. Several other factors that could be involved in mortality of children under 1, include socioeconomic conditions; low education, low income, poor obstetric care for high-risk pregnancies; complications at the time of delivery; infrastructural inadequacies, and lack of resources for medical intervention. However, these data are not included in death certificates, and the operating cost of surveying the medical records of children in various hospitals within the city and outside it to collect this information would have made the study unfeasible. Information on the absence of antenatal care and the presence of maternal problems, in addition to other indicators of poor quality of antenatal care, delivery care, or neonatal care, would be important to ascertaining and consolidating the true reasons for the phenomena observed.
Conclusion
Deaths of children under 1 year of age have remained stable at tolerable levels in the municipality of Niterói. The highest frequency of deaths occurred outside the neonatal period, and young maternal age did not show an association with deaths before or after the neonatal period. Sepsis was the leading cause of mortality, and deaths were directly associated with prematurity and low birth weight. Analysis of the extent to which infant deaths were avoidable was challenging, as mortality was related to prematurity, a multifactorial problem.
Footnotes
Ethics Committee Approval: The study was approved by the Ethics Committee of Federal Fluminense University (CAAE: 23136714.7.0000.5243).
Informed Consent: Informed consent was not necessary due to the retrospective nature of this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – İ.F.J., S.B.; Design – İ.F.J., V.F.; Supervision – İ.F.J.; Materials – S.B.; V.F.; Data Collection and/or Processing – İ.F.J.; S.B.; V.F.; Analysis and/or Interpretation – İ.F.J.; V.F.; Literature Search – S.B.; V.F.; Writing – İ.F.J.; S.B.; V.F.; Critical Reviews – İ.F.J.
Acknowledgments: The authors would like to thank the Coordination of the Health Observatory (Coordenação do Observatório da Saúde de Niterói, COOBS) for their collaboration in this survey.
Declaration of Interests: The authors have no conflict of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Whitty CJ. Harveian Oration 2017: triumphs and challenges in a world shaped by medicine. Clin Med (Lond). 2017;17(6):537 544. 10.7861/clinmedicine.17-6-537) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonatti AF, Silva AMCD, Muraro AP. Infant mortality in Mato Grosso, Brazil: trend and causes of death between 2007 and 2016. Cien Saude Colet. 2020;25(7):2821 2830. 10.1590/1413-81232020257.28562018) [DOI] [PubMed] [Google Scholar]
- 3. Brasil. Portaria no 371. Minitério da Saúde; 2014. Available at: http://bvsms.saude.gov.br/bvs/saudelegis/sas/2014/prt0371_07_05_2014.html. [Google Scholar]
- 4. Lima SS, Braga MC, Vanderlei LCM, Luna CF, Frias PG. Assessment of the impact of prenatal, childbirth, and neonatal care on avoidable neonatal deaths in Pernambuco State, Brazil: an adequacy study. Cad Saude Publica. 2020;36(2):e00039719. 10.1590/0102-311X00039719) [DOI] [PubMed] [Google Scholar]
- 5. Costa G, Cabral O, Santana E, Lima G, Figueiredo I. Mobile emergency care service: a time-course assessment and characterization of demand. Int Emerg Nurs. 2018;41:45 50. 10.1016/j.ienj.2018.06.006) [DOI] [PubMed] [Google Scholar]
- 6. Niterói. Taxa de mortalidade infantil, por mil nascidos vivos. In: Saúde, Nit O.eds. Prefeitura Municipal de Niterói; 2022. Available at: http://observa.niteroi.rj.gov.br/lista-indicadores/23-taxa-de-mortalidade-infantil. [Google Scholar]
- 7. Brasil. Ministério da Saúde. A Declaração de Óbito: Manual de Instruções Para Peenchimento. Brasília: Ministério da Saúde; 2022. Available at: http://bvsms.saude.gov.br/bvs/publicacoes/declaracao_obito_manual_preenchimento.pdf [Google Scholar]
- 8. Brasil. Classificação Brasileira de Ocupações (CBO). In: Trabalho Md.ed. Brasília: Ministério do Trabalho; 2017. Available at: http://www.mtecbo.gov.br/cbosite/pages/home.jsf. [Google Scholar]
- 9. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th revision. Geneva: World Health Organization; 2019. Available at: https://icd.who.int/browse10/2019/en. [Google Scholar]
- 10. Guinsburg R, Sanudo A, Kiffer CRV.et al. Annual trend of neonatal mortality and its underlying causes: population-based study - Sao Paulo State, Brazil, 2004-2013. BMC Pediatr. 2021;21(1):54. 10.1186/s12887-021-02511-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Paixao ES, Blencowe H, Falcao IR.et al. Risk of mortality for small newborns in Brazil, 2011-2018. A National Birth Cohort Study of 17.6 Million Records from Routine Register-Based Linked Data. Lancet Reg Health Am 2021; 3: None. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Malta DC, Sardinha LM, Moura L.et al. Update of avoidable causes of deaths due to interventions at the Brazilian Health System. Epidemiol Serv Saúde. 2010;19:173 176. [Google Scholar]
- 13. Tomassini HC, Alves MG, Claro LB, Pacheco AG, de Almeida MT. Demographic and mortality trends in Niteroi, Rio de Janeiro, Brazil, 1979 to 1997. Cad Saude Publica. 2003;19(6):1621 1629. 10.1590/s0102-311x2003000600007) [DOI] [PubMed] [Google Scholar]
- 14. Unicef. Neonatal mortality; 2021. Available at: https://data.unicef.org/topic/child-survival/neonatal-mortality/#:~:text=Children%20face%20the%20highest%20risk,deaths%20per%201%2C000%20in%201990. [Google Scholar]
- 15. Unicef. Brazil: key demographic indicators; 2021. Available at: https://data.unicef.org/country/bra. [Google Scholar]
- 16. Russo LX, Scott A, Sivey P, Dias J. Primary care physicians and infant mortality: evidence from Brazil. PLoS One. 2019;14(5):e0217614. 10.1371/journal.pone.0217614) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Anele CR, Hirakata VN, Goldani MZ, da Silva CH. The influence of the municipal human development index and maternal education on infant mortality: an investigation in a retrospective cohort study in the extreme south of Brazil. BMC Public Health. 2021;21(1):194. 10.1186/s12889-021-10226-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lima D, Lima G, Cersosimo A, Figueiredo I. Out-of-hospital deliveries: a case-control study. Turk Arch Pediatr/Türk Pediatr Ars. 2018;53:87 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodrigues LDS, Rodrigues LDS, Costa LC, Fontoura GMG, Maciel MCG. Trend in infant mortality rate caused by sepsis in Brazil from 2009 to 2018. Rev Inst Med Trop Sao Paulo. 2021;63:e26. 10.1590/S1678-9946202163026) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Freitas JLG, Alves JC, Pereira PPDS, Moreira KFA, Farias EDS, Cavalcante DFB. Child mortality for avoidable causes in Rondonia: temporal series study, 2008-2018. Rev Gaucha Enferm. 2021;42:e20200297. 10.1590/1983-1447.2021.20200297) [DOI] [PubMed] [Google Scholar]
- 21. Ramalho AA, Andrade AM, Martins FA, Koifman RJ. Infant mortality trend in the city of Rio Branco, AC, 1999 to 2015. Rev Saude Publica. 2018;52:33. 10.11606/S1518-8787.2018052000280) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. GBD 2019 Under-5 Mortality Collaborators. Global, regional, and national progress towards Sustainable Development Goal 3.2 for neonatal and child health: all-cause and cause-specific mortality findings from the Global Burden of Disease Study 2019. Lancet. 2021;398(10303):870 905. 10.1016/S0140-6736(21)01207-1) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a