Abstract
Background:
The effect of chronic noise on the middle ear is not fully known. This study aimed to evaluate the middle ear functions of metal workers exposed to chronic noise using wideband tympanometry.
Methods:
In this study, 62 male workers exposed to chronic noise and 30 healthy men were included. Workers exposed to chronic noise were divided into 2 groups according to their pure tone averages. Totally 30 workers (60 ears) with pure tone average less than 20 dB were included in group I, and 32 workers (64 ears) with pure tone average more than 20 dB were included in group II. All individuals were subjected to wideband tympanometry. Tympanometric peak pressure, equivalent ear canal volume, static acoustic admittance, resonance frequency, and absorbance ratios at peak pressure and ambient pressure values were analyzed.
Results:
There was no difference between the groups in terms of traditional tympanometric parameters such as tympanometric peak pressure, equivalent ear canal volume, and static acoustic admittance (P >.05). Resonance frequency of workers exposed to chronic noise (group I and group II) was lower than the control group (P <.05). The absorbance ratios of workers exposed to chronic noise at approximately 4 kHz were lower in both peak pressures and ambient pressures (P <.05).
Conclusion:
Chronic noise does not only damage the inner ear but also causes changes in the middle ear structures. Wideband tympanometry can be used to detect minor auditory damage due to noise that cannot be detected by audiogram early. In this way, necessary measures can be taken in the early period before noise-induced hearing loss occurs.
Keywords: Wideband tympanometry, middle ear, stiffness, absorbance, chronic noise
Main Points
Stiffness and mass are important factors that determine the conduction properties of the middle ear.
Wideband tympanometer, unlike traditional tympanometer, can detect the resonance frequency and absorbance value of the middle ear.
Some causes such as aging may affect the conductivity properties of the middle ear without causing any pathology in the middle ear. In addition, noise may affect middle ear conduction properties.
In this study, it was observed that there was a decrease in RF and 4 kHz absorbance ratios of workers with both noise-induced hearing loss and those with normal hearing despite chronic noise exposure compared to healthy individuals.
Wideband tympanometry can be used to detect minor auditory damage due to noise that cannot be detected by audiogram early.
Introduction
Inner ear disorders, such as sensorineural hearing loss, tinnitus, hyperacusis, and balance problems, can occur in workers exposed to chronic noise.1,2 Outer hair cells are the first to be affected by noise. In longer and more severe exposures, these damages directly spread to the inner hair cells, stria vascularis, and endolymphatic sac.3,4 In addition to direct damage to hearing structures, noise can also cause metabolic damage by producing reactive oxygen, reactive nitrogen species, and other free radical molecules in the cochlea.5 The most important finding of noise-induced hearing loss (NIHL) is hearing loss at high frequencies, which is characterized by the acoustic notch at 3, 4, or 6 kHz in a pure tone audiometry test. Although rare, noise can also affect the tympanic membrane and middle ear. Excessively severe acute noise (acoustic trauma) can perforate the eardrum and disrupt the ossicular chain.6 In addition, a study with multifrequency tympanometry reported that noise can cause loosening of the annular ligament without causing any obvious middle ear damage.7
Wideband tympanometry (WBT) uses click stimuli, unlike the single-probe tone used in traditional tympanometry. Thus, WBT allows imitansmetric measurements in the range of 226‐8000 Hz, with both ambient and outer ear canal pressure.8 The acoustic absorbance value in WBT refers to the sound energy absorbed by the middle ear. On the contrary, the acoustic reflectance value refers to the sound energy reflected from the eardrum.9 Another parameter is the resonance frequency (RF), which expresses the frequency at which the mass and stiffness components of the middle ear are equal. At the RF, the middle ear is only affected by friction, and sound energy is transmitted better at this frequency than at other frequencies. Resonance frequency, which shows the conduction properties of the middle ear, is also affected by the mechanical impedance of the cochlea. Studies have reported that RF changes significantly in cases such as inner ear anomaly, superior semicircular canal dehiscence (SSCD), and Meniere’s disease.8,10,11 Hence, WBT can offer a non-invasive, simple, fast, and reliable method for evaluating the middle and inner ears.
Traditional tympanometry (226 Hz) uses a low-frequency tone to evaluate changes in the mass effect properties of the middle ear, but multifrequency tones are a much more sensitive method for controlling small changes in the transmission properties of the tympano-ossicular system.12 Although chronic noise affects inner ear structures, it can also cause minor changes in middle ear structures. However, to the best of our knowledge, no studies have investigated the findings of WBT in workers exposed to chronic noise. This study aimed to investigate WBT parameters in workers exposed to chronic noise.
Methods
Study Design and Setting
This prospective case–control study was conducted in a university hospital otorhinolaryngology outpatient clinic between January 2021 and May 2021. Approval was obtained from the local ethics committee of the university for the study (protocol number: 2021/557). Written and verbal consent was obtained from all individuals included in the study.
Participants and Eligibility Criteria
The 70 participants in the study group were metal workers who worked together at the same workplace for at least 4 years. All workers were exposed to Lex 93.2 dBA values, measured annually in accordance with international ISO 9612 standards. A total of 70 workers were examined by an otorhinolaryngologist. Eight of them were excluded due to asymmetric hearing loss in 5 workers, eardrum perforation in 2 workers, and type C tympanogram in 1 worker. The remaining 62 male workers who met the inclusion criteria were included in the study. These workers were divided into 2 groups according to their pure tone averages (PTA) (average of 500, 1000, 2000, and 4000 Hz). Thirty workers (60 ears) with bilateral PTA less than 20 dB were included in group I. Thirty-two workers (64 ears) with an acoustic notch of more than 15 dB at 4 or 6 kHz and bilateral PTA of more than 20 dB were included in group II. Thirty healthy male (60 ears) office workers with similar age distribution to these workers were included in the study as the control group. All control group individuals were exposed to Lex 35.2 dBA noise measured in accordance with ISO 9612 standards. Participants with eardrum pathology, previous otologic surgery, and type B and C tympanograms were not included in the study. Hearing and WBT measurements of all individuals in the study (group 1 and group 2) and control group (92 workers) were performed by a specialist audiologist in the audiology clinic at the weekend.
Noise Exposure Measurements
Personnel-based noise measurements (Lex dBA, 8 hours/working day daily noise exposure level; P peak dBC) were performed in the machine area. Personal noise dosimeter (SV104, Svantek; Warsaw, Poland) device was used for noise measurement. For personnel-based noise measurement, the device was placed on the shoulders of the participants and recorded between 08:00 am and 05:00 pm in 1 working day. In personnel-based measurements, the average Lex was 93.2 dB (A) and the P peak C was 137.98 dB (C). Workers were included in the study according to the Lex dB (A). The noise level of the machinery area where the workers in the study group worked was Lex 93.2 dBA. The noise level of the office area where the workers in the control group worked was 35.2 dBA. The specified noise measurements were made annually according to the international standards ISO 9612.
Audiological Evaluation
Bilateral air conduction thresholds between 250 and 8000 Hz and bone conduction thresholds between 500 and 4000 Hz of all participants were determined by a pure tone audiometry test (Madsen Astera; 2 GN Otometrics, Taastrup, Denmark) in a quiet cabin. Pure tone average of the participants was calculated by taking the average of air conduction hearing thresholds at 500, 1000, 2000, and 4000 Hz. Pure tone average < 20 dB was considered normal hearing.
Wide band Tympanometry
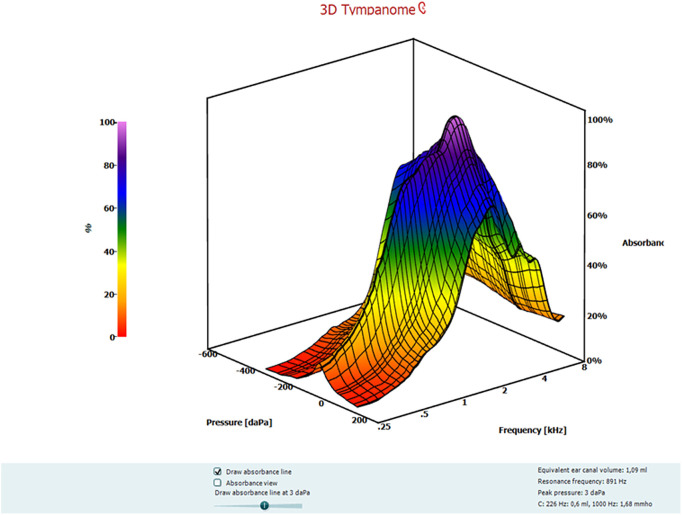
Wideband tympanometry was measured between 226 and 8000 Hz octave frequencies (107 different frequencies) and 100 peSPL intensity level (Interacoustics Titan version 3.1; IMP440, Denmark) in a quiet environment (Figure-1). The test was started after placing the appropriate probe in the outer ear canal of the participants. The data were saved in the database as a .xls file created by the system. Traditional tympanometry (226 Hz) parameters, such as tympanometric peak pressure (TPP), equivalent ear canal volume (Veq), and static acoustic admittance (Ytm) and WBT parameters, such as RF, ambient pressure absorbance ratios (APAR), and peak pressure absorbance ratios (PPAR), were analyzed.
Figure 1.
Three-dimensional wideband tympanogram plotted according to frequencies.
Statistical Analysis
The Inernational Business Machines Statistical Package for the Social Science 21 (IBM SPSS Corp.; Armonk, NY, USA) program was used for statistical analysis. The distribution of normality was analyzed using the Shapiro–Wilk test. Normally distributed data were presented with mean ± standard deviation (SD), and data not showing normal distribution were presented with median (min-max). To compare the 3 groups, the one-way analysis of variance test, one of the parametric tests, was used in cases where the assumptions of normality and homogeneity of variances were provided, while Tukey, one of the post hoc tests, was used to compare the groups among themselves. In cases where assumptions were not met, the Kruskal–Wallis test, one of the non-parametric tests, was used. A P <.05 was considered statistically significant.
Results
The mean age of group I was 38.67 ± 8.47 (range, 27-54), the mean age of group II was 42.84 ± 7.25 (range, 30-57), and the mean age of the control group was 40.73 ± 8.37 (range, 24-55). There was no difference in age distribution between the groups (P = .132). The average working time of the workers in group I in noisy environments was 14.57 ± 8.35 (4-24) years, while the working time of the workers in group II in noisy environments was 18.19 ± 8.48 (4-35) years.
There was no difference between the groups in terms of TPP, Ytm, and Veq (P > 0.05, Table 1). A comparison of RF values among the groups revealed that workers in group I and group II had lower RF values than those of the healthy group (P < 0.05, Table 2). When the mean RF values of group I and group II were compared among themselves, there was no significant difference between the groups, although the RF value of group II was worse than group I (P > .05)
Table 1.
Traditional Tympanometry Parameters According to Groups
| Group I (Mean ± SD) or (Min-Max) n = 60 Ears | Group II (Mean ± SD) or (Min-Max) n = 64 Ears | Control Group (Mean ± SD) or (Min-Max) n = 60 Ears | P * | |
| TPP (daPa) | 2.0 (−52 to 47) | 2.5 (−90 to 46) | 2.50 (−88 to 44) | .691 |
| Veq (mL) | 1.47 ± 0.25 | 1.52 ± 0.23 | 1.37 (1.03 to 1.98) | .069 |
| Ytm (mL) | 0.70 (0.32 to 2.80) | 0.60 (0.30 to 2.60) | 0.60 (0.34 to 1.50) | .864 |
*Kruskal−Wallis test.
TPP, tympanometric peak pressure; Veq, equivalent ear canal volume; Ytm, static acoustic admittance.
Table 2.
Resonance Frequencies and Absorbance Values of Individuals According to Groups
| Frequency | Group I (Mean ± SD) or (Min-Max) n = 60 Ears | Group II (Mean ± SD) or (Min-Max) n = 64 Ears | Control Group (Mean ± SD) or (Min-Max) n = 60 Ears | P | P (Post Hoc) | |
| RF (Hz) | 755 (498-1406) | 761 ± 137.0 | 875 (447-2686) | .034 b | .531x
.047y .012z |
|
| 226 | APAR | 0.18 ± 0.06 | 0.17 ± 0.07 | 0.15 (0.06-0.38) | .275b | |
| PPAR | 0.18 (0.07-0.46) | 0.17 (0.08-0.35 | 0.15 (0.06-0.34) | .225b | ||
| 500 | APAR | 0.37 (0.13-0.95) | 0.34 ± 0.13 | 0.34 ± 0.12 | .205b | |
| PPAR | 0.41 ± 0.13 | 0.38 ± 0.12 | 0.36 ± 0.12 | .124a | ||
| 1000 | APAR | 0.65 ± 0.13 | 0.61 ± 0.15 | 0.64 ± 0.13 | .287a | |
| PPAR | 0.72 (0.31-0.90) | 0.65 ± 0.14 | 0.68 ± 0.13 | .221b | ||
| 2000 | APAR | 0.66 ± 0.15 | 0.58 ± 0.18 | 0.63 (0.01-0.95) | .090b | |
| PPAR | 0.65 ± 0.15 | 0.60 ± 0.16 | 0.63 (0.10-0.95) | .141b | ||
| 4000 | APAR | 0.45 ± 0.19 | 0.42 ± 0.18 | 0.54 ± 0.18 | .001a | .735x
.017y .001z |
| PPAR | 0.45 ± 0.19 | 0.38 (0.09-0.95) | 0.54 ± 0.18 | <.001b | .652x
.023y <.001z |
|
| 8000 | APAR | 0.45 ± 0.18 | 0.47 ± 0.19 | 0.42 ± 0.14 | .187a | |
| PPAR | 0.44 ± 0.18 | 0.47 ± 0.18 | 0.41 ± 0.14 | .117a | ||
| Mean | APAR | 0.48 ± 0.09 | 0.45 ± 0.10 | 0.49 ± 0.07 | .023a | .079x
.920y .030z |
| PPAR | 0.50 ± 0.09 | 0.47 ± 0.09 | 0.50 ± 0.07 | .185a |
aOne-way ANOVA; bKruskal–Wallis test; XGroup I-group II; YGroup I-control group; ZGroup II-control group.
RF, resonance frequancy; APAR, ambient pressure absorbance ratio; PPAR, peak pressure absorbance ratio; ANOVA, analysis of variance. Bold data indicates statistical significance.
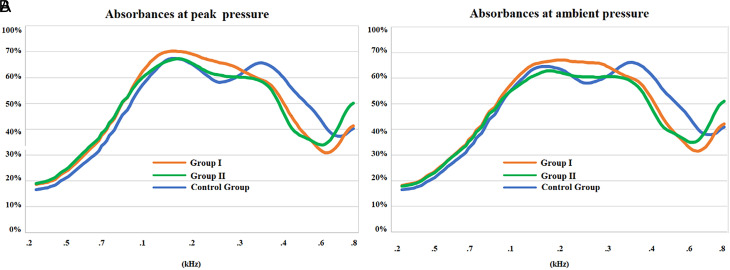
In comparing the absorbance values, we observed no differences between the groups in terms of 226, 500, 1000, 2000, and 8000 Hz APAR and PPAR values (P > .05). However, both the APAR and PPAR values of group I and group II were lower than those of the healthy group at 4000 Hz (P <.05). Assessment of the average absorbance values (average of 107 frequencies) showed that the APAR values of group II were worse than those of the other groups (P <.05); however, there was no difference between the PPAR values of the groups (P > .05). When the mean absorbance values of group I and group II were compared among themselves, although the absorbance value of group II was worse than group I, there was no significant difference between the groups. The absorbance values between the groups are presented in Table 2. The absorbance graphs of the groups are presented in Figure-2.
Figure 2.
Absorbance values according to frequencies at both peak pressure and ambient pressure.
There were no differences between the groups in terms of 500, 1000, and 2000 Hz air-bone gaps (ABG) (P > .05). However, the ABG at 4000 Hz in group I and group II were worse than in the control group (P = .002, <.001, respectively). Air conduction thresholds, bone conduction thresholds, and air-bone gaps by groups are shown in Table 3.
Table 3.
Pure Tone Averages According to Groups and Correlation Coefficient (P-Value) Between Ambient Pressure Absorbance Ratios, Peak Pressure Absorbance Ratios, and Air-Bone Gap According to Frequencies
| Hz | Group I | Group II | Control Group | ||||
| PTA (dB) | APAR/PPAR | PTA (dB) | APAR/PPAR | PTA (dB) | APAR/PPAR | ||
| Correlation coefficient (P-value) | Correlation coefficient (P-value) | Correlation coefficient (P-value) | |||||
| 500 | ACT | 11.67 ± 4.38 | 15.89 ± 6.17 | 6.42 ± 4.79 | |||
| BCT | 8.92 ± 4.79 | 13.63 ± 6.53 | 4.75 ± 3.61 | ||||
| ABG | 2.75 ± 3.95 | −0.09 (0.45)/−0.07 (0.55) | 2.26 ± 4.21 | 0.02 (0.86)/0.01 (0.88) | 1.66 ± 2.54 | −0.23 (0.06)/−0.30 (0.01) | |
| 1000 | ACT | 10.92 ± 4.55 | 15.73 ± 6.82 | 7.92 ± 4.98 | |||
| BCT | 9.17 ± 4.79 | 13.31 ± 5.50 | 5.75 ± 3.99 | ||||
| ABG | 1.75 ± 2.88 | −0.21 (0.93)/−0.30 (0.01) | 2.42 ± 4.12 | 0.01 (0.91)/−0.12 (0.31) | 2.16 ± 3.60 | 0.02 (0.82)/0.05 (0.66) | |
| 2000 | ACT | 10.83 ± 5.61 | 24.19 ± 13.76 | 6.50 ± 5.31 | |||
| BCT | 9.50 ± 5.18 | 22.18 ± 11.36 | 5.50 ± 4.75 | ||||
| ABG | 1.33 ± 3.03 | −0.18 (0.16)/−0.07 (0.57) | 2.02 ± 4.56 | −0.11 (0.36)/−0.10 (0.41) | 1.00 ± 2.21 | 0.11 (0.40)/−0.01 (0.90) | |
| 4000 | ACT | 20.67 ± 10.55 | 52.15 ± 15.50 | 8.08 ± 6.18 | |||
| BCT | 15.33 ± 8.53 | 46.45 ± 12.42 | 6.16 ± 4.98 | ||||
| ABG | 5.33 ± 5.51 | −0.30 (0.02)/−0.29 (0.02) | 6.53 ± 6.11 | −0.37 (<0.01)/−0.30 (0.01) | 1.91 ± 2.77 | 0.00 (0.98)/0.01 (0.91) | |
Significant r and P-values are shown with highlight-bold font. ACT, pure tone average; ACT, air conduction threshold; BCT, bone conduction threshold; ABG, air-bone gap; APAR, ambient pressure absorbance ratios; PPAR, peak pressure absorbance ratios.
In addition, we performed a correlation test for the relationship between PPAR, APAR, and ABGs at 500, 1000, 2000, and 4000 Hz. A moderate negative correlation was observed between ABG and both PPAR and APAR at 4000 Hz in group I and group II. In addition, a moderate negative correlation was observed between PPAR and ABG at 500 Hz in the control group and at 1000 Hz in group I. The correlation coefficients and P-values between APAR, PPAR, and ABG according to the frequencies within the groups are presented in Table 3.
Discussion
When noise comes to the outer ear canal, it is transmitted to the inner ear by the middle ear ossicles, which act as a bridge between the tympanic membrane and the inner ear. The most important factor affecting the transmission properties of noise in the middle ear is the mass and stiffness effects of the middle ear and cochlear.13 Mass and stiffness determine the resonance frequency of objects. Mass enables low-frequency sounds to be transmitted, while stiffness enables high-frequency sounds to be transmitted. Therefore, the transmission of sound energy is maximum at the frequency where the mass and stiffness effect are equal, which is the RF. The cochlea is an important structure that determines RF due to the mass and stiffness of the middle ear.7 Increased pressure in the cochlea can push the stapes base and annular ligament, which can reduce the movement of the ossicular chain. In other words, a decrease in pressure in the cochlea can increase flexibility in the ossicular chain. In addition to RF, middle ear absorbance ratios can also be evaluated according to frequencies in WBT. Therefore, WBT is a more reliable test method in diagnosing middle and inner ear pathologies.8,10,11
The effectiveness of WBT has been investigated in some middle ear and inner ear pathologies.10,11,14-16 Karuppannan et al14 compared the WBT results of individuals with otosclerosis and healthy individuals. In the study, it was reported that the absorbance ratios in the otosclerosis group were lower between 250 and 2000 Hz compared to the control group, and individuals with otosclerosis had higher RF. The authors also reported that the absorbance rate of 1000 Hz has a high diagnostic rate (>90% sensitivity and specificity). Kelava et al15 reported that the absorbance ratio between 432 and 1059 Hz was lower in individuals with otosclerosis, and the absorbance ratio between 4238 and 8000 Hz was higher than in healthy individuals. In these studies, it was stated that WBT may be useful for detecting otosclerosis.14-16
In inner ear pathologies investigating WBT, findings related to Meniere’s disease and inner ear anomalies were generally evaluated.10,11 Demir et al10 investigated the results of WBT in individuals with Meniere’s disease. The authors stated that hydrops formed in the inner ear due to Meniere’s disease creates resistance against the passage of sound energy, and therefore, the absorbance ratio at low frequencies (250-1000 Hz) decreases, similar to the low-frequency hearing loss in the audiogram. Some studies have reported a low-frequency ABG in individuals with Meniere’s disease.17,18 Absorbance rates may decrease depending on this ABG in Meniere’s disease. In addition, Meniere’s disease also affects RF. Resonance frequencies due to hydrops increase during an acute attack19 and a decrease in RF was observed due to a decrease in pressure between attacks.10 Kaya et al11 evaluated 157 patients with different inner ear anomalies (cochlear hypoplasia, incomplete partition I, incomplete partition II, cochlear aplasia, complete labyrinthine aplasia) with WBT. They stated that the wideband absorbance ratio was lower in individuals with inner ear anomalies than in healthy individuals, especially at high frequencies. It was also stated that RF was higher in complete labyrinth aplasia compared to other groups and that WBT could be used to differentiate inner ear anomalies. In our study, we divided the workers exposed to chronic noise into 2 groups as those with NIHL and those without hearing loss and compared the WBT results of these workers with healthy individuals. In our study, there was no difference between the groups in terms of traditional tympanometry parameters (TPP, Veq, Ytm). However, we found that workers exposed to chronic noise (group I and group II) had a decrease in RF and absorbance ratios at mid-high frequencies (especially 4 kHz). In this respect, WBT can be used to detect minor auditory damage due to noise that cannot be detected by audiogram early. In this way, necessary measures can be taken in the early period before NIHL occurs.
Broadband stimulation is used in WBT, and the absorbance value can be determined between 226 and 8000 Hz. Absorbance measurements can be made at both peak pressure and ambient pressure. Therefore, non-pressure tests are useful for evaluating the condition of the middle ear in situations where tests cannot be performed under pressure, such as after middle ear surgery. Wideband tympanometry graphs the absorbance value at the frequencies it evaluates. Morgalis et al20 reported that the absorbance ratio is maximum at 1.2 kHz and 3.5 kHz in adults and begins to decrease as it goes below and above these values. The authors also stated that absorbance measurements made by changing the pressure were more sensitive to middle ear pathologies than measurements made at ambient pressure. In our study, we found that consistent with the study by Morgalis et al.20 the absorbance ratio in healthy adults made a double peak in both APAR (ambient) and PPAR (pressurized) in the region of about 1.2 kHz and 3.5 kHz, and the absorbance in these regions was maximum (Figure-2). In our study, the configurations of the APAR and PPAR graphics were also similar. However, unlike Morgalis’ study,20 we found that APAR results were lower in workers exposed to noise than in healthy individuals. This may be an indication that these 2 measurements are sensitive to different pathologies, as stated by other authors.11
In addition to the ossicles, there are muscles and ligaments in the middle ear. Therefore, small changes in these structures that cannot be detected in traditional tympanometry may affect RF and absorbance ratios. Darrouzet et al7 evaluated the middle ears of guinea pigs with multifrequency tympanometry before and after exposure to noise at 4 different intensities (105 dB SPL or 115 dB SPL for 2 or 3 hours). The authors reported that RF did not change in the guinea pigs, but there were changes in the admittance, susceptance, and conductance graphics of the guinea pigs. It has been stated that these changes resemble graphs of decreased perilymphatic pressure and may occur due to the "loosening" of the annular ligament. As a result, the authors reported that the noise caused temporary damage to the middle ear structures; these damages healed after exposure, and RF should be investigated with chronic noise in subsequent studies.
In our study, group I and group II had worse ABG at 4000 Hz than the control group, and there was a moderate negative correlation between ABG and absorbance values, similar to the literature.21 Similar to our study, it has been reported that elderly individuals with presbycusis also have ABG that affects mid-high frequencies besides the sensorineural component.22,23 This transmission component appears as an ABG of approximately 6-12 dB in the 4 kHz region on the audiogram.23,24 Feeney et al24 investigated WBT findings in elderly individuals and reported that middle ear absorbance increased between 800 and 2000 Hz and decreased especially at 4000 Hz in individuals with presbycusis. The authors explained this change in absorbance ratio in elderly individuals with a decrease in middle ear stiffness. In our study, the absorbance values of workers exposed to chronic noise were lower than healthy individuals, especially at 4 kHz. In addition, although there was no statistically significant difference, the PPAR of workers exposed to chronic noise was higher than healthy individuals, especially between 226 and 3000 Hz (Figure-2). Therefore, severe chronic noise and aging may affect the middle ear system in a similar way. However, more studies investigating noise and WBT findings are needed.
The limitation of our study is that the effect mechanism of noise on the middle ear has not been fully revealed. More morphological studies are needed on this subject.
Conclusion
We observed a decrease in RF and mid-high frequencies absorbance ratios in workers with both noise-induced hearing loss and those with normal hearing despite chronic noise exposure compared to healthy individuals. Our study shows that chronic noise does not only damage the inner ear but also causes changes in the middle ear structures. Wideband tympanometry can be used to detect minor auditory damage due to noise that cannot be detected by audiogram early. In this way, necessary measures can be taken in the early period before NIHL occurs.
Footnotes
Ethics Committee Approval: Ethical committee approval was received from the local ethics committee of Karabuk University (2021/557).
Informed Consent: Written and verbal informed consent was obtained from all participants who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – E.S., N.Y.; Design – E.S., N.Y.; Supervision – O.Y., N.Y.; Funding – E.S., N.Y.; Materials – E.S., N.Y.; Data Collection and/or Processing – T.S., M.B.S.; Analysis and/or Interpretation – O.Y., N.Y.; Literature Review – T.S., M.B.S.; Writing Manuscript – T.S., M.B.S.; Critical Review – O.Y., N.Y.
Declaration of Interests: The authors declare that they have no conflict of interest.
Funding: The authors declared that this study has received no financial support.
References
- 1. Basner M, Babisch W, Davis A.et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383(9925):1325 1332. 10.1016/S0140-6736(13)61613-X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Basner M, Brink M, Bristow A.et al. ICBEN review of research on the biological effects of noise 2011-2014. Noise Health. 2015;17(75):57- 82. 10.4103/1463-1741.153373) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bohne BA. Mechanisms of noise damage in the inner ear. In: Henderson D, Hamernik RR, Dosanjh D, Mills JH.eds., Effects of Noise on HEARing, New York. Raven Press; 1976:41- 68. [Google Scholar]
- 4. Kumagami H. Endolymphatic hydrops induced by noise exposure. Auris Nasus Larynx. 1992;19(2):95 104. 10.1016/s0385-8146(12)80097-6) [DOI] [PubMed] [Google Scholar]
- 5. Kopke RD, Coleman JK, Liu J, Campbell KC, Riffenburgh RH. Candidate’s thesis: enhancing intrinsic cochlear stress defenses to reduce noise-induced hearing loss. Laryngoscope. 2002;112(9):1515 1532. [DOI] [PubMed] [Google Scholar]
- 6. Jahrsdoerfer R. The effects of impulse noise on the eardrum and middle ear. Otolaryngol Clin North Am. 1979;12(3):515 520. 10.1016/S0030-6665(20)32440-3) [DOI] [PubMed] [Google Scholar]
- 7. Darrouzet V, Dulon D, Franco-Vidal V. Multifrequency immittancemetry in experimentally induced stapes, round window and cochlear lesions. Audiol Neurootol. 2007;12(2):85 100. 10.1159/000097795) [DOI] [PubMed] [Google Scholar]
- 8. Demir E, Afacan NN, Celiker M.et al. Can wideband tympanometry be used as a screening test for superior semicircular canal dehiscence? Clin Exp Otorhinolaryngol. 2019;12(3):249 254. 10.21053/ceo.2018.01137) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Feeney MP, Grant IL, Marryott LP. Wideband energy reflectance measurements in adults with middle-ear disorders. J Speech Lang Hear Res. 2003;46(4):901 911. 10.1044/1092-4388(2003/070)) [DOI] [PubMed] [Google Scholar]
- 10. Demir E, Celiker M, Aydogan E, Balaban GA, Dursun E. Wideband tympanometry in Meniere’s disease. Indian J Otolaryngol Head Neck Surg. 2020;72(1):8 13. 10.1007/s12070-019-01709-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kaya Ş, Çiçek Çınar B, Özbal Batuk M.et al. Wideband tympanometry findings in inner ear malformations. Auris Nasus Larynx. 2020;47(2):220 226. 10.1016/j.anl.2019.09.001) [DOI] [PubMed] [Google Scholar]
- 12. Colletti V. Tympanomety from 200 to 2000 Hz probe tone. Audiology. 1976;15(2):106 119. 10.3109/00206097609071767) [DOI] [PubMed] [Google Scholar]
- 13. Kim J, Koo M. Mass and stiffness impact on the middle ear and the cochlear partition. J Audiol Otol. 2015;19(1):1 6. 10.7874/jao.2015.19.1.1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Karuppannan A, Barman A. Wideband absorbance tympanometry: a novel method in identifying otosclerosis. Eur Arch Otorhinolaryngol. 2021;278(11):4305 4314. 10.1007/s00405-020-06571-x) [DOI] [PubMed] [Google Scholar]
- 15. Kelava I, Ries M, Valent A.et al. The usefulness of wideband absorbance in the diagnosis of otosclerosis. Int J Audiol. 2020;59(11):859 865. 10.1080/14992027.2020.1785644) [DOI] [PubMed] [Google Scholar]
- 16. Niemczyk E, Lachowska M, Tataj E, Kurczak K, Niemczyk K. Wideband tympanometry and absorbance measurements in otosclerotic ears. Laryngoscope. 2019;129(10):E365 E376. 10.1002/lary.27747) [DOI] [PubMed] [Google Scholar]
- 17. Yetişer S, Kertmen M. Cochlear conductive hearing loss in patients with Meniere’s disease. Kulak Burun Bogaz Ihtis Derg. 2007;17(1):18 21. [PubMed] [Google Scholar]
- 18. Muchnik C, Hildesheimer M, Rubinstein M, Arenberg IK. Low frequency air-bone gap in Menière’s disease without middle ear pathology. A preliminary report. Am J Otol. 1989;10(1):1 4. [PubMed] [Google Scholar]
- 19. Bianchedi M, Croce A, Neri G, Moretti A. Multifrequency tympanometry in Meniere’s disease: preliminary results. Acta Otorhinolaryngol Ital. 1996;16(1):1 5. [PubMed] [Google Scholar]
- 20. Margolis RH, Saly GL, Keefe DH. Wideband reflectance tympanometry in normal adults. J Acoust Soc Am. 1999;106(1):265 280. 10.1121/1.427055) [DOI] [PubMed] [Google Scholar]
- 21. Yüksel Aslıer NG, Gürkan S, Aslıer M, Kirkim G, Güneri EA, Ikiz AÖ. Sound energy absorbance characteristics of cartilage grafts used in type 1 tympanoplasty. Auris Nasus Larynx. 2018;45(5):985 993. 10.1016/j.anl.2018.02.007) [DOI] [PubMed] [Google Scholar]
- 22. Nondahl DM, Tweed TS, Cruickshanks KJ, Wiley TL, Dalton DS. Aging and the 4-kHz air-bone gap. J Speech Lang Hear Res. 2012;55(4):1128 1134. 10.1044/1092-4388(2011/11-0204)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nixon JC, Glorig A, High WS. Changes in air and bone conduction thresholds as a function of age. J Laryngol Otol. 1962;76:288 298. 10.1017/s0022215100059314) [DOI] [PubMed] [Google Scholar]
- 24. Feeney MP, Sanford CA. Age effects in the human middle ear: wideband acoustical measures. J Acoust Soc Am. 2004;116(6):3546 3558. 10.1121/1.1808221) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a