Summary
Background
Hong Kong followed a strict COVID-19 elimination strategy in 2020. We estimated the impact of the COVID-19 pandemic responses on all-cause and cause-specific hospitalizations and deaths in 2020.
Methods
Interrupted time-series analysis using negative binomial regression accounting for seasonality and long-term trend was used on weekly 2010–2020 data to estimate the change in hospitalization risk and excess mortality occurring both within and out of hospitals.
Findings
In 2020, as compared to a 2010–2019 baseline, we observed an overall reduction in all-cause hospitalizations, and a concurrent increase in deaths. The overall hospitalization reduction (per 100,000 population) was 4809 (95% CI: 4692, 4926) in 2020, with respiratory diseases (632, 95% CI: 607, 658) and cardiovascular diseases (275, 95% CI: 264, 286) contributing most. The overall excess mortality (per 100,000 population) was 25 (95% CI: 23, 27) in 2020, mostly among individuals with pre-existing cardiovascular diseases (12, 95% CI: 11, 13). A reduction in excess in-hospital mortality (−10 per 100,000, 95% CI: −12, −8) was accompanied by an increase in excess out-of-hospital mortality (32, 95% CI: 29, 34).
Interpretation
The COVID-19 pandemic might have caused indirect impact on population morbidity and mortality likely through changed healthcare seeking particularly in youngest and oldest individuals and those with cardiovascular diseases. Better healthcare planning is needed during public health emergencies with disruptions in healthcare services.
Funding
Health and Medical Research Fund, Collaborative Research Fund, AIR@InnoHK and RGC Senior Research Fellow Scheme, Hong Kong.
Keywords: COVID-19, Hospitalization, Excess mortality, In-hospital mortality, Out-of-hospital mortality
Research in context.
Evidence before this study
In addition to the respiratory morbidity and mortality caused by SARS-CoV-2 infection, increasing attention has been focused on the indirect impact of the COVID-19 pandemic and related policy responses on a broader range of public health outcomes. Studies have described hospitalization reductions, including for cardiovascular and respiratory diseases, which logically would be accompanied by increased mortality if life-threatening events fail to receive timely medical intervention. We (HX and JW) searched PubMed on 30 September 2022 using the following search terms: “((“COVID-19”) OR (“SARS-CoV-2”)) AND ((“hospital”) OR (“hospitalization”) OR (“hospitalizations”)) AND ((“reduction”) OR (“reduce”) OR (“reductions”) OR (“decline”) OR (“declining”) OR (“declines”) OR (“change”) OR (“changes”) OR (“different from”)) AND ((“deaths”) OR (“mortality”)) AND (“excess”)”. After title, abstract and full text screening on the 135 studies searched, we identified 31 studies (Summary information of these studies were listed in Supplementary Table 1) that evaluated the impact of the COVID-19 pandemic on overall or cause-specific excess mortality or hospitalizations/procedures/emergency visits, among which two studies described both the changes in hospitalization rates and concurrent changes in cause-specific excess deaths. However, most studies describing all-cause and cause-specific COVID-19 related excess deaths were in jurisdictions applying mitigation rather than containment or strict elimination strategies as employed in Hong Kong where excess health burden can therefore be more reliably attributed to pandemic responses rather than to SARS-CoV-2 infection.
Added value of this study
We analysed all-cause and cause-specific hospitalizations and deaths between 2010 and 2020 in Hong Kong and identified an absolute reduction of 359,790 (4809 per 100,000 population, a 23% reduction) hospitalizations and 1873 (25 per 100,000 population) excess deaths in 2020 which would not have been expected in the absence of the COVID-19 pandemic and associated policy and population responses. Most excess mortality was associated with cardiovascular diseases and among high-risk population groups, indicating target groups for public health intervention in case of future COVID-19 or other epidemics. The observation of decreased in-hospital and increased out-of-hospital mortality in 2020 was suggested to result from the lack of/inability to seek urgent medical care during the pandemic.
Implications of all the available evidence
The indirect impact of the COVID-19 pandemic, likely resulting from concern about SARS-CoV-2 exposure or other challenges to timely access of medical services has caused reduced hospitalization and excess deaths in some jurisdictions and high-risk population groups which may outweigh even the direct consequences of SARS-CoV-2 infection. With the possible emergence of more virulent or transmissible strains of SARS-CoV-2, medical institutions and policymakers should prepare adequate resources, including risk communication, to provide better healthcare for patients with non-COVID-19 diseases.
Introduction
Beyond the direct COVID-19 disease burden, estimated at >500 million cases and 6 million deaths by July 2022, there are growing concerns about the indirect impact of interventions to control COVID-19, pandemic-related lifestyle changes, adverse consequences of reorganized health-care systems, and the potential secondary complications of SARS-CoV-2 infections.1, 2, 3, 4 Public health and social measures such as stay-at-home advisories and movement restrictions have led to delays in healthcare seeking.5 Medical facilities have been forced to defer routine hospitalizations, consultations or screening appointments to maintain treatment capacity for COVID-19 patients, many of whom require resource-intensive isolation and clinical management, while preventing nosocomial infections.3 Some individuals may also have hesitated to seek medical care due to fear of COVID-19.3,6 Treatment-seeking delays risk exacerbation of untreated, non-COVID disease and a more severe average clinical presentation at hospital. Studies from the United States, France and Italy have observed excess deaths in- and out-of-hospital from cardiovascular diseases, diabetes, and other conditions during the pandemic.2,3,7
Hong Kong implemented a strict COVID-19 elimination strategy in the initial period of the pandemic.8 After the first imported case was detected on 23 January 2020 followed by an increasing number of imported cases, the government raised the Preparedness and Response Plan to the emergency level.9 Measures including strict isolation of cases in hospitals or isolation facilities, strict quarantine of close contacts outside the home, travel restrictions, primary and secondary school class suspension, mask mandates, and compulsory social distancing were introduced.9,10 Hong Kong has an advanced public and private healthcare system whereby private clinics comprise most primary care and government hospitals provide approximately 90% of hospital and related medical services, via the Hospital Authority (HA), at very low cost to patients.11,12 To minimize hospital congestion and reduce the risk of cross infection, the HA in Hong Kong adjusted service provision to focus on emergency, essential and inpatient services. The number of elective surgeries and selected outpatient services were reduced by approximately half; appointments for non-emergency examinations such as endoscopy and gastroscopy were rescheduled, and some patients were diverted to private hospitals for treatment.13,14 These measures successful restricted SARS-CoV-2 transmission in the early pandemic to just 7057 local confirmed cases (1 per 1000) and 181 deaths (2 per 100,000) in 2020. However, limited studies addressing the indirect effects of COVID-19 in Hong Kong suggested delays from illness onset to medical contact and from hospital admission to laboratory testing for patients with acute myocardial infarction, and a drastic reduction of pediatric hospitalizations for acute respiratory virus infections.9,15
The medical impacts of the adjusted healthcare services and behavioural responses to COVID-19 epidemic waves in Hong Kong have not been described. We explored the indirect impact of the COVID-19 pandemic on healthcare use and population health, indicated by the change in all-cause and cause-specific hospitalizations and deaths in 2020.
Methods
Sources of data
Hospitalizations in this study referred to the admissions to public hospitals managed by the HA. Weekly hospitalization data from 2010 to 2020 were collected from the HA. Admissions were aggregated by age (0–4, 5–14, 15–44, 45–64 and over 65 years), sex, residential district, admission year, admission week, admitted via accident & emergency department or not, discharge destination (home; transfer to other HA hospitals; death; other) and primary discharge diagnosis coded according to the International Classification of Diseases Tenth Revision (ICD-10) and grouped into: all causes (A00–Z99), and the following major causes for hospitalization and death: malignant neoplasms (C00–C97), kidney diseases (N00–N07, N17–N19, N25–N27), cardiovascular diseases (I00–I99), respiratory diseases (J00–J99, including COVID-19 cases), diabetes mellitus (E10–E14), septicemia (A40–A41), chronic liver diseases (K70, K73–K74), and degenerative diseases of the nervous system (G30–G32). Cardiovascular and respiratory diseases were further subcategorized into four groups: heart diseases (I00–I09, I11, I13, I20–I51), cerebrovascular diseases (I60–I69), pneumonia & influenza (J09–J18), and chronic lower respiratory diseases (J40–J47).
Individual death data recorded in Hong Kong from 2010 to 2020, including age, sex, date, primary cause of death and residence, were collected from the Census and Statistics Department of Hong Kong. The age- and sex-specific mid-year population from 2010 to 2020 were extracted from official statistics of the annual census data published by the Census and Statistics Department of Hong Kong.16
Statistical analysis
Weekly hospitalization and mortality risk was calculated by dividing the number of weekly hospitalizations and deaths by mid-year populations, respectively, by age, sex and cause of admission or death, while the annual risk was estimated using the annual number of hospitalizations and deaths as the numerator. An interrupted time-series analysis was used to estimate the hospitalization reductions and excess mortality occurring in 2020 through a counterfactual which assumed trends from 2010 to 2019 would continue in 2020.17 Weekly hospitalization and death data from 2010 to 2018 were fitted to negative binomial regression models separately accounting for seasonality and temporal trends, using the population in Hong Kong as an offset. A group of models were developed using different Fourier terms with or without the variable “week” to explore the impact of seasonality and using calendar year and the week sequence (from the first week of 2010 to the last week of 2018) to indicate the temporal trends. Selection of the final model was based on the model performance which was examined by comparing the model-predicted values with the observed values in 2019 (full model selection process described in Supplementary Materials). The COVID-19-associated annual hospitalization reduction and excess mortality risk in 2020 and the weekly average hospitalization reduction and excess mortality risk during an epidemic wave were estimated from the variances of the weekly hospitalization and mortality risk predicted by the selected model (Supplementary Materials). The results were presented as overall estimates as well as by sex, age, and cause of admission or death. These analyses were repeated to explore the impact of health seeking and access on mortality patterns, using overall and cause-specific a) in-hospital mortality, and b) out-of-hospital mortality, with the Hong Kong population as an offset (Supplementary Materials).
Hong Kong experienced four COVID-19 “epidemic waves” in 2020, each defined as an epidemic after which the local transmission was suppressed, although the fourth wave which started in November 2020 did not end until the spring of 2021. We defined weeks 5–9 as epidemic wave 1, weeks 10–19, weeks 20–42, and weeks 43–53 as wave 2, wave 3 and wave 4, respectively. The weekly average all-cause and cause-specific hospitalization reduction and excess mortality were estimated for waves 1 and 2 (combined), wave 3, and wave 4, using the same aforementioned method, including in- and out-of-hospital mortality estimates for each wave (Supplementary Materials).
The proportion of deaths occurring in hospital was calculated by dividing the in-hospital deaths by the total number of deaths in Hong Kong, and we compared the proportions between 2020 and 2010–2019 using Pearson's chi-square test. We calculated the weekly in-hospital mortality risk from 2010 to 2020 by dividing the number of in-hospital deaths by the number of hospitalizations occurring in each week of the year. To identify the change in in-hospital mortality risk in 2020, we estimated the overall, age- and sex-specific excess in-hospital mortality risk using a similar negative binomial regression model as used for the overall excess mortality estimation, with the number of hospitalizations as an offset (Supplementary Materials). Analyses were conducted in R version 4.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
Role of the funding source
The funding bodies had no role in the design of the study, the collection, analysis, and interpretation of data, or writing of the manuscript. This project was supported by a commissioned grant from the Health and Medical Research Fund of the Hong Kong SAR Government (grant no. CID-HKU2), the Collaborative Research Fund (project no. C7123-20G) of the Research Grants Council of the Hong Kong SAR Government, and AIR@InnoHK administered by Innovation and Technology Commission of the Hong Kong SAR Government. BJC is supported by the RGC Senior Research Fellow Scheme grant (HKU SRFS2021-7S03) from the Research Grants Council of the Hong Kong Special Administrative Region, China.
Results
Hospitalization reduction
A total of 1,536,587 patients were hospitalized in HA facilities in 2020. The overall hospitalization risk (per 100,000 population per year) was 20,538, highest in adults over 65 years (54,394), followed by those aged 0–4 (24,490), 45–64 (19,269), 15–44 (8479) and 5–14 years (4147). The most common causes of hospitalization were malignant neoplasms (2782 per 100,000 per year), kidney diseases (2361), cardiovascular diseases (1450), respiratory diseases (1268), and septiceamia (129).
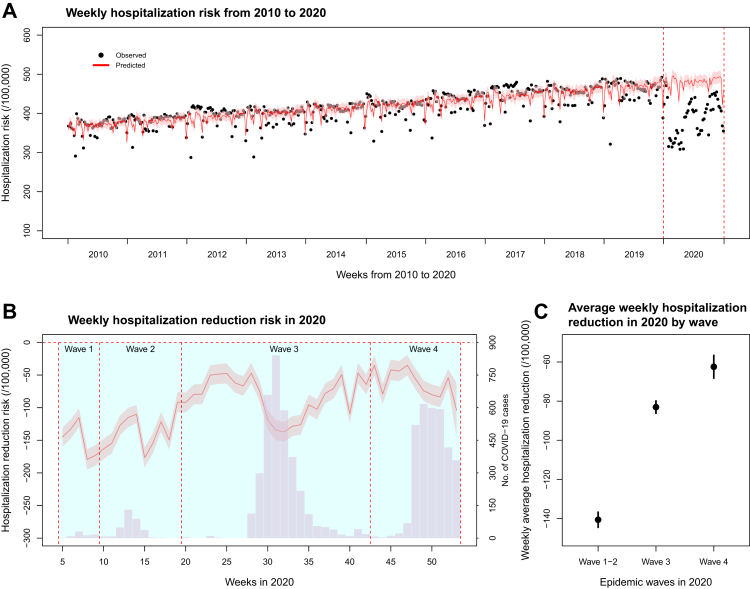
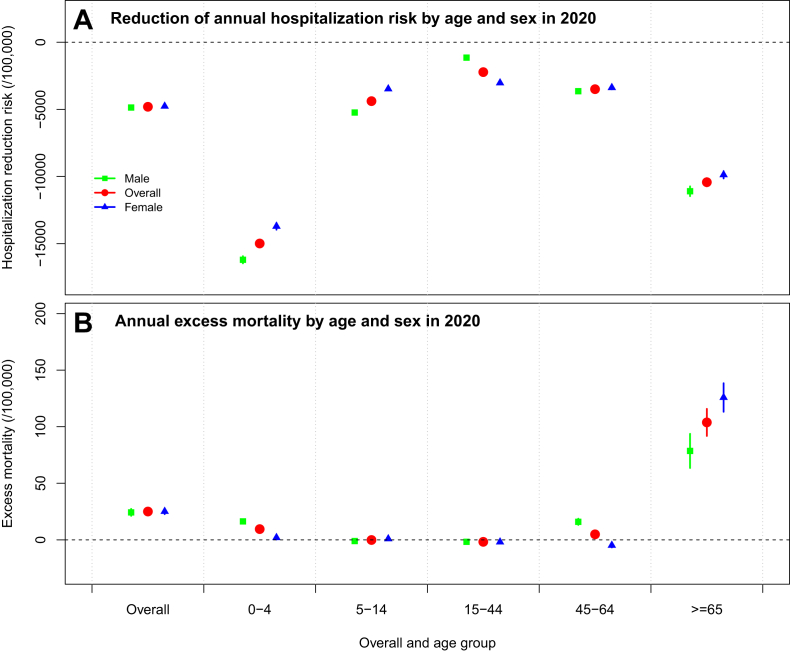
A steadily increasing trend in annual hospitalization risk was identified from 2010 (19,055 per 100,000 population per year) to 2019 (23,942) (Fig. 1A). In 2020, we predicted a hospitalization risk of 25,347 (95% CI: 24,229, 25,464) per 100,000 per year, compared with 20,538 observed, a reduction of 4809 (95% CI: 4692, 4926), a 23% (95% CI: 22%, 24%) reduction, or an absolute reduction of 359,790 (95% CI: 351,009–368,570) hospitalizations. Greater reductions were observed between week 5 and week 19 during the beginning of the epidemic; and during the peaks of COVID-19 waves 3 and 4 (Fig. 1B). While estimates of the weekly hospitalization risk were lower than expected throughout 2020, the difference was greater in waves 1–2 at 141 (95% CI: 137, 144) fewer hospitalizations per 100,000 population per week, but only 83 (95% CI: 80, 86) fewer in each week in wave 3 and 62 fewer (95% CI: 57, 68) in wave 4 (Fig. 1C). Patients aged 0–4 (14,990 fewer per 100,000 per year, 95% CI: 14,745, 15,235) and over 65 (10,426, 95% CI: 10,117, 10,734) showed higher reductions in hospitalization compared to other age groups, in both males and females (Fig. 2A). The highest proportional reductions were observed in children aged 5–14 (51% reduction, 95% CI: 50, 52), followed by those aged 0–4 (38%, 95% CI: 37, 39).
Fig. 1.
Overall trend of hospitalization risks and reduction of hospitalization risk in Hong Kong. (A) Observed (black dots) and predicted (red solid line represents the mean predicted weekly hospitalization risk, and pink area represents the 95% confidence interval [95% CI]) weekly hospitalization risks from 2010 to 2020. (B) Reduction of weekly hospitalization risk (red solid line represents the mean hospitalization reduction risk, and pink area represents the 95% CI) in 2020, with grey bars indicating weekly numbers of locally infected COVID-19 cases in Hong Kong. (C) Average reduction of weekly hospitalization risk by epidemic wave of COVID-19 in 2020.
Fig. 2.
Overall and age- and sex-specific reduction of annual hospitalization risk (A) and annual excess mortality (B) in Hong Kong during 2020.
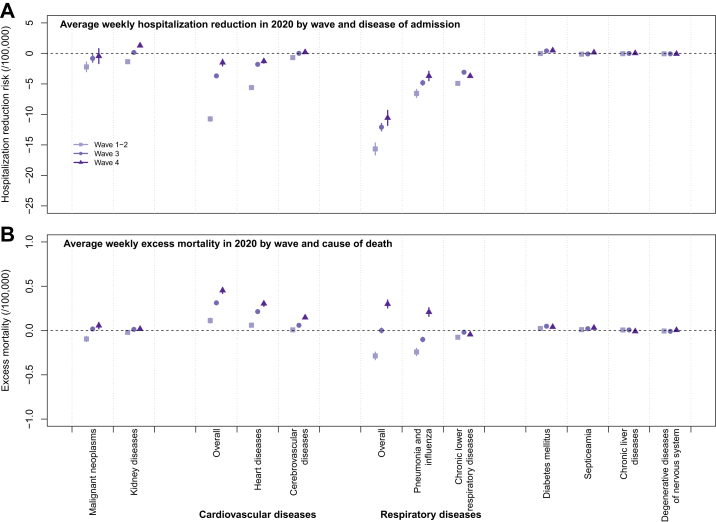
By cause, the highest reduction in hospitalization was observed in respiratory diseases (632, 95% CI: 607, 658, per 100,000 population per year) (Figure S1A), within which the reduction was 244 (95% CI: 227, 260) and 192 (95% CI: 188, 196) for pneumonia & influenza and chronic lower respiratory diseases, respectively. Cardiovascular diseases contributed a reduction of 275 (95% CI: 264, 286) per 100,000 per year, within which the reduction of heart diseases and cerebrovascular diseases was 147 (95% CI: 141, 153) and 8 (95% CI: 7, 10), respectively (Figure S1A). Except for respiratory diseases particularly pneumonia and influenza in which the largest reductions appeared in children, the highest reductions in other major disease groups were identified for patients over 65 years (Figure S2). Analyzed by cause and wave, we found a recovery trend of hospitalizations for most diseases over the COVID-19 epidemic waves, with the weekly average reduction decreasing from 16 (95% CI: 15, 17) per 100,000 per week in waves 1–2 to 12 (95% CI: 11, 13) in wave 3 and 11 (95% CI: 9, 12) in wave 4 for respiratory diseases, and from 11 (95% CI: 10, 12) to 4 (95% CI: 3, 4) and 2 (95% CI: 1, 2) for cardiovascular diseases (Fig. 3A).
Fig. 3.
Cause-specific average weekly hospitalization reduction risk (A) and excess mortality (B) by epidemic wave of COVID-19 in Hong Kong, causes of hospitalization are in a descending order of the cause-specific hospitalization risk in 2020.
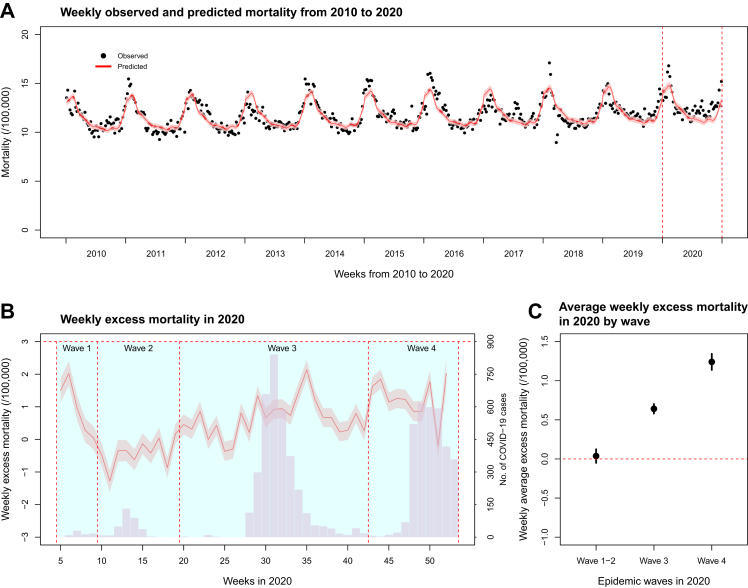
Excess deaths
Between 2010 and 2019, a slightly increasing trend in population mortality risk was identified from 589 (per 100,000 population per year) in 2010 to 639 in 2019 (Fig. 4A). In 2020, the mortality risk was 661 per 100,000, higher for males (796) than females (548). The three leading causes of death were malignant neoplasms (197 per 100,000 per year), respiratory diseases (151), and cardiovascular diseases (137).
Fig. 4.
Overall trend of mortality and excess mortality in Hong Kong. (A) Observed (black dots) and predicted (red solid line represents the mean predicted weekly mortality, and pink area represents the 95% CI) weekly mortality from 2010 to 2020. (B) Weekly excess mortality (red solid line represents the mean excess mortality, and pink area represents the 95% CI), with grey bars indicating weekly numbers of locally infected COVID-19 cases in Hong Kong. (C) Average weekly excess mortality by epidemic wave of COVID-19 in 2020 in Hong Kong.
The overall excess mortality (per 100,000 population per year) was 25 (95% CI: 23, 27) in 2020, equating to 1873 (95% CI: 1,698, 2047) excess deaths, increasing over time from a weekly average excess mortality of 0.04 (95% CI: −0.05, 0.1) in waves 1 and 2 to 0.6 (95% CI: 0.5, 0.7) in wave 3 and 1.2 (95% CI: 1.1, 1.3) in wave 4 (Fig. 4B and C). Most excess mortality occurred in people aged over 65 years (104 per 100,000 per year, 95% CI: 92, 116), and to a lesser extent among children (9, 95% CI: 8, 11) (Fig. 2B). Most excess mortality was from cardiovascular diseases (12 per 100,000 per year, 95% CI: 11, 13), mostly from heart (9, 95% CI: 8, 10) and cerebrovascular (3, 95% CI: 2, 3) diseases (Figure S1B). The highest weekly average excess mortality caused by cardiovascular diseases was in wave 4 (0.5 per 100,000, 95% CI: 0.4, 0.5), and a reduction in respiratory excess mortality was observed in waves 1–2 (−0.3, 95% CI: −0.3, −0.2) (Fig. 3B).
In-hospital mortality and out-of-hospital mortality
A total of 32,550 in-hospital deaths were recorded in 2020, accounting for 66% of total deaths in Hong Kong, lower than the average proportion in 2010–2019 (68%, P < 0.01) (Figure S3A). In 2020, 2156 deaths were observed in public hospitals every 100,000 hospitalizations leading to 360 (95% CI: 352, 367) excess in-hospital deaths per 100,000 hospitalizations annually compared with the predicted in-hospital mortality of 1796 (95% CI: 1789, 1804) deaths per 100,000 hospitalizations in the same year (Figure S3B and C).
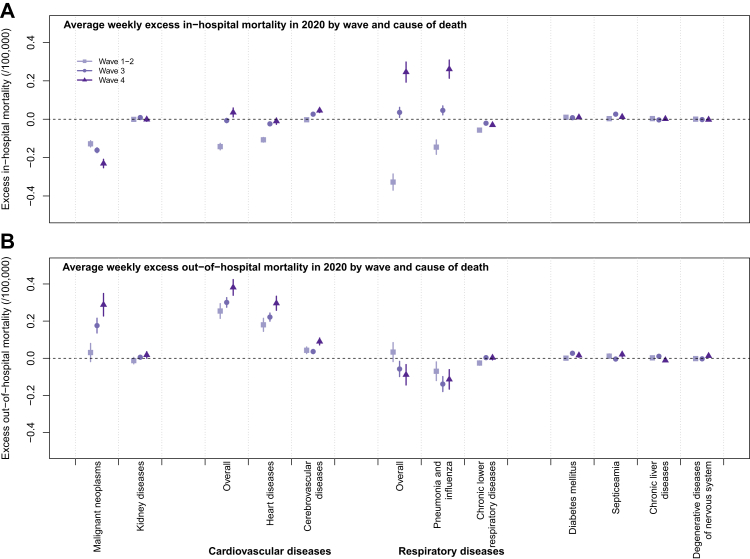
The observed annual in-hospital mortality (per 100,000 population per year) was 435 in 2020, lower than the predicted (445, 95% CI: 444, 447) from our model, and the annual excess in-hospital mortality was estimated to be −10 (95% CI: −12, −8) per 100,000 population (Figure S4). The highest reductions in-hospital mortality was observed for malignant neoplasms (−9 per 100,000 per year, 95% CI: −9, −7), followed by cardiovascular diseases (−3, 95% CI: −3, −2) (Figure S5A), with slight variations across the epidemic waves (Fig. 5A).
Fig. 5.
Cause-specific average weekly excess in-hospital (A) and out-of-hospital (B) mortality by epidemic wave of COVID-19 in 2020 in Hong Kong.
A total of 16,927 out-of-hospital deaths (226 per 100,000 population per year) was observed in 2020, accounting for 34% of overall deaths in Hong Kong, higher than the proportion in 2010–2019 (32%) (P < 0.01) (Figure S6A). In contrast to in-hospital mortality, the observed out-of-hospital mortality (226 per 100,000 per year) was higher than the predicted (195, 95% CI: 192, 197), with an estimated excess of 32 (95% CI: 29, 34) (Figure S6B and C), mainly from cardiovascular causes (14, 95% CI: 13, 15) and particularly heart diseases (11, 95% CI: 10, 12), followed by malignant neoplasms (7, 95% CI: 5, 8), with some variation across epidemic waves (Fig. 5B, Figure S5B).
Discussion
We conducted an interrupted time-series analysis of hospitalizations and deaths from 2010 to 2020 in Hong Kong and identified a significant reduction in hospital admission, an increase in mortality and changing patterns of deaths coinciding with SARS-CoV-2 circulation and accompanying public health and social measures. These findings are indicative of changing patterns of healthcare use associated with the COVID-19 pandemic as observed elsewhere,6,18, 19, 20, 21 which may have resulted in an increase in preventable, non-COVID-19 mortality in Hong Kong.
Our study observed an overall reduction of 4809 (95% CI: 4692, 4926) hospitalizations per 100,000 population in 2020 particularly in respiratory diseases at the two extremes of age (Fig. 2, Fig. 3). The observed decline in respiratory infections during the pandemic was likely due to the public health responses to the COVID-19 pandemic10 while changes in healthcare seeking behaviors might also contribute to the observed disease burden. While we lack data to describe the underlying population behaviour or healthcare factors potentially contributing to these changes, data from Hong Kong and other countries may have suggested some likely mechanisms. First, individuals might have a fear of exposure to SARS-CoV-2 by changing their behavior to minimize social contacts, and were reluctant to seek medical care. These behavioral modifications were likely magnified during periods of the strictest social distancing including school suspensions and restricted public gathering, concurrent with alarming media reports on exposure risk and its consequences.3,6,22,23 This effect has been documented by a study in the UK describing reluctance to seek medical care due to fear of COVID-19,24 the consequence of which would be a more serious average clinical presentation at hospital and a proportion of patients failing to receive the treatment that they needed.25 Second, the difficulty in accessing medical care due to reorganized healthcare services, deferral of milder cases, elevated emergency triage thresholds and reduced ICU capacity would have resulted in lower utilization of non-COVID healthcare.6 Although these measures helped control nosocomial infection of COVID-19, the stringent infection control measures might have discouraged patients from accessing care, resulting in elevated fatality risk from acute and life-threatening conditions such as myocardial infarction.15 We identified a notable hospitalization reduction and a higher in-hospital mortality risk in 2020, indicative of reluctance to seek healthcare and perhpas an increased severity among admitted patients, particularly older adults, which supports the hypothesis of changing care-seeking and stricter admission thresholds during the outbreak. Telemedicine may be a useful alternative to improve access to healthcare during the pandemic26 while the implementation barriers should be addressed to ensure health equity in the population.27 We also observed a declining trend of hospitalization reduction through 2020 consistent with declining adherence to voluntary social distancing measures and “epidemic fatigue” resulting in healthcare use patterns more similar to previous years.10,28 Besides, the experience from the early COVID-19 pandemic suggested that better management in healthcare system might help mitigate the indirect negative impact of the pandemic on population health.29
Despite the hospitalization reductions identified among cardiovascular and respiratory diseases, we did not observe comparable reductions in hospitalization for other causes, particularly the malignant neoplasms and kidney diseases with a higher hospitalization rate than cardiovascular and respiratory diseases in 2020. This is likely because while there was a planned reduction in almost half of the elective surgeries and some outpatient services in public hospitals, treatment of some diseases such as cancer was unaffected.13,14 The perceived severity and clinical consequences of untreated diseases such as malignant neoplasms and kidney diseases might also have outweighed any impulse to avoid healthcare facilities for fear of SARS-CoV-2 infection.
In a scenario with reduced and delayed hospitalizations as outlined above, it is reasonable to expect an increase in mortality caused by late treatment seeking for potentially life-threatening disorders. Excess deaths were observed in our study concurrent with COVID-19 epidemics, in agreement with studies conducted in other regions.7,17,30 While COVID-19 may aggravate existing cardiovascular disease,31,32 infections were closely tracked in Hong Kong, and we believe the most likely explanation for excess deaths was the indirect impact of the COVID-19 pandemic. Most excess deaths occurred among older people with cardiovascular diseases without inpatient treatment, consistent with an Italian study indicating a significant increase in out-of-hospital cardiac deaths during the pandemic.33 The risk of mortality can increase over time due to clinical complications for conditions such as atrial fibrillation, and early use of reperfusion therapy is needed for patients with acute coronary syndromes34 and delays in reperfusion following some acute cardiac conditions have contributed to a significant increase in out-of-hospital cardiac deaths during the COVID-19 pandemic.6 This treatment dynamic possibly explains the lag effect observed in our study whereby reduced hospitalizations in early 2020 were followed by excess cardiovascular deaths later in the year, but other reasons such as postponed scheduled interventions or consultations in older adults with existing illness, and increased psychological stress triggering cardiac events, are also possible.3
We studied the indirect impact of the COVID-19 pandemic using a comprehensive sample of cause-specific hospitalizations and deaths in a region where a strict elimination strategy was implemented to cope with COVID-19 but our study has four distinct limitations. First, it is possible some observed reductions in hospitalization sought care in private hospitals while our study was based on hospitalizations in public hospitals which constituted over 90% of all hospital admissions in Hong Kong. The declined hospitalization illustrated in our study might have overestimated reductions in care-seeking during the COVID-19 pandemic. Second, our analysis on in-hospital deaths did not include deaths in accident & emergency or private hospitals, potentially leading to an underestimate of the in-hospital mortality and an overestimate in the out-of-hospital mortality. Third, we did not model concurrent healthcare system or behavioural changes occurred in 2020 in Hong Kong that might also have contributed to the changing patterns in hospitalization and death. Finally, we included only the primary diagnosis for hospitalization or the disease or condition leading directly to death, omitting contributing causes which in some fatalities may provide additional information on the relationship between changes in hospitalization and deaths.
In conclusion, the hospitalization reductions and excess deaths identified in Hong Kong in 2020 indicated the potential indirect impact of the COVID-19 pandemic on population morbidity and mortality. Studies during future COVID-19 epidemics and other public health emergencies are needed to provide further evidence on the relationship between healthcare seeking and health impact in the population.
Contributors
All authors meet the ICMJE criteria for authorship. The study was conceived by BJC and PW. HX, PW, JN and JYW analyzed the data. HX wrote the first draft of the manuscript. All authors provided critical review and revision of the text and approved the final version.
Data sharing statement
Restrictions apply to the availability of these data. The hospitalization and mortality data are available for access with the permission from the Hospital Authority and the Census and Statistics Department of Hong Kong.
Declaration of interests
BJC consults for AstraZeneca, Fosun Pharma, GlaxoSmithKline, Moderna, Pfizer, Roche and Sanofi Pasteur. JN previously worked for, and owns shares in, Sanofi. The other authors report no other potential conflicts of interest.
Acknowledgements
The authors thank Julie Au for technical support.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2022.100645.
Appendix A. Supplementary data
References
- 1.Rosenbaum L. The untold toll - the pandemic's effects on patients without Covid-19. N Engl J Med. 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 2.Baldi E., Sechi G.M., Mare C., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marijon E., Karam N., Jost D., et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Modin D., Claggett B., Sindet-Pedersen C., et al. Acute COVID-19 and the incidence of ischemic stroke and acute myocardial infarction. Circulation. 2020;142(21):2080–2082. doi: 10.1161/CIRCULATIONAHA.120.050809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huynh K. Reduced hospital admissions for ACS - more collateral damage from COVID-19. Nat Rev Cardiol. 2020;17(8):453. doi: 10.1038/s41569-020-0409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiss P., Carcel C., Hockham C., Peters S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7(1):18–27. doi: 10.1093/ehjqcco/qcaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. 2020;324(5):510–513. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker M.G., Wilson N., Blakely T. Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. BMJ. 2020;371:m4907. doi: 10.1136/bmj.m4907. [DOI] [PubMed] [Google Scholar]
- 9.Chiu S.S., Cowling B.J., Peiris J.S.M., Chan E.L.Y., Wong W.H.S., Lee K.P. Effects of nonpharmaceutical COVID-19 interventions on pediatric hospitalizations for other respiratory virus infections, Hong Kong. Emerg Infect Dis. 2022;28(1):62–68. doi: 10.3201/eid2801.211099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cowling B.J., Ali S.T., Ng T.W.Y., et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GovHK Overview of the health care system in Hong Kong. https://www.gov.hk/en/residents/health/hosp/overview.htm
- 12.Wu P., Presanis A.M., Bond H.S., Lau E.H.Y., Fang V.J., Cowling B.J. A joint analysis of influenza-associated hospitalizations and mortality in Hong Kong, 1998-2013. Sci Rep. 2017;7(1):929. doi: 10.1038/s41598-017-01021-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hospital Authority Hospital authority calls on healthcare staff to stay on duty. https://www.ha.org.hk/haho/ho/pad/200202Eng3.pdf
- 14.Hospital Authority HA adjusts service provision to focus on combatting epidemic. https://www.ha.org.hk/haho/ho/pad/200210Eng.pdf
- 15.Tam C.F., Cheung K.S., Lam S., et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Census and Statistics Department Population estimates. https://www.censtatd.gov.hk/en/scode150.html
- 17.Islam N., Shkolnikov V.M., Acosta R.J., et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137. doi: 10.1136/bmj.n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia S., Albaghdadi M.S., Meraj P.M., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Filippo O., D'Ascenzo F., Angelini F., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020;383(4):400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braiteh N., Rehman W.U., Alom M., et al. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. 2020;226:147–151. doi: 10.1016/j.ahj.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moroni F., Gramegna M., Ajello S., et al. Collateral damage: medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020;2(10):1620–1624. doi: 10.1016/j.jaccas.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wessler B.S., Kent D.M., Konstam M.A. Fear of coronavirus disease 2019-an emerging cardiac risk. JAMA Cardiol. 2020;5(9):981–982. doi: 10.1001/jamacardio.2020.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.British Heart Foundation Lives at risk due to 50% drop in heart attack A&E attendances. https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-break
- 25.De Rosa S., Spaccarotella C., Basso C., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greiwe J. Telemedicine lessons learned during the COVID-19 pandemic. Curr Allergy Asthma Rep. 2022;22(1):1–5. doi: 10.1007/s11882-022-01026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kronenfeld J.P., Penedo F.J. Novel coronavirus (COVID-19): telemedicine and remote care delivery in a time of medical crisis, implementation, and challenges. Transl Behav Med. 2021;11(2):659–663. doi: 10.1093/tbm/ibaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gao H., Du Z., Tsang T.K., et al. Pandemic fatigue and attenuated impact of avoidance behaviours against COVID-19 transmission in Hong Kong by cross-sectional telephone surveys. BMJ Open. 2021;11(12) doi: 10.1136/bmjopen-2021-055909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marijon E., Karam N., Jouven X. Cardiac arrest occurrence during successive waves of the COVID-19 pandemic: direct and indirect consequences. Eur Heart J. 2021;42(11):1107–1109. doi: 10.1093/eurheartj/ehab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kontopantelis E., Mamas M.A., Webb R.T., et al. Excess deaths from COVID-19 and other causes by region, neighbourhood deprivation level and place of death during the first 30 weeks of the pandemic in England and Wales: a retrospective registry study. Lancet Reg Health Eur. 2021;7 doi: 10.1016/j.lanepe.2021.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Driggin E., Madhavan M.V., Bikdeli B., et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li B., Yang J., Zhao F., et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campo G., Fortuna D., Berti E., et al. In- and out-of-hospital mortality for myocardial infarction during the first wave of the COVID-19 pandemic in Emilia-Romagna, Italy: a population-based observational study. Lancet Reg Health Eur. 2021;3 doi: 10.1016/j.lanepe.2021.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jabre P., Roger V.L., Murad M.H., et al. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123(15):1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.