Abstract
BACKGROUND:
Work in informational technology (IT) professionals is highly competitive and stressful, leading to job stress. This can lead to burnout, effort-reward imbalance (ERI), and poor sleep quality.
MATERIALS AND METHODS:
The present study examined associations of ERI, burnout, and poor sleep quality among IT professionals using data from 200 software engineers (mean age of 29.3 ± 4 years, 32% women). ERI and overcommitment were assessed using Siegrist's “effort-reward” questionnaire. The Oldenburg Burnout Inventory (OLBI) was used to assess burnout and Pittsburgh Sleep Quality Index (PSQI) to assess sleep quality.
RESULTS:
ERI, burnout and poor sleep quality were present in 72%, 60%, and 70%, respectively. Females had higher ERI, burnout, and poor sleep quality compared to males. ERI is significantly associated with burnout (r = 0.45, P < 0.01) and poor sleep quality (r = 0.31, P < 0.01). Linear regression to assess the ability of ERI to predict levels of burnout yielded a statistically significant (R2 = 0.206, P < 0.01) indicating ERI to be a unique incremental predictor of burnout (b = 0.454, t = 7.16, P < 0.01). ERI tends to be a predictive factor of poor sleep quality with Odd's ratio = 3.5, 95%CI (1.81–6.73), P < 0.01.
CONCLUSION:
In summary, Intervention programs both at the individual and at the organization level have to be designed to combat ERI, burnout, and poor sleep quality among IT professionals.
Keywords: Burnout, effort-reward imbalance, IT professionals, poor sleep quality
Introduction
India has the fastest growing informational technology (IT) market involving a large proportion of its population, thus becoming a hub of IT industries. Jobs in IT have become highly competitive and stressful in terms of their high achieving and demanding nature. They are characterized by prolonged working hours, an almost trademark lack of distinction between work and home life, night shift, increasing market pressures, insecurity about the job, upgradation of new technology, insight into technological innovations, greater understanding of the business process, time-constrained projects, and continuous visual focusing of monitors, budgetary constraints that frequently lead to under-staffing and consequently overworking and management policies that often lack an understanding of IT operations which can all lead to occupational stress.[1,2,3] Occupational stress – also called work stress, job stress, or stress in organizations – “is a condition wherein job-related factors interact with the worker to change, either disrupt or enhance, his or her psychological or physiological conditions such that the individual's mind and/or body are forced to deviate from normal functioning.” Occupational stress symptoms are not limited to the workplace but remain with the human being impacting the broader psychosocial domain.[4] Stress is a physiological and psychological response of the brain to any demand. Stress can lead to stimulation of the hypothalamus pituitary adrenal (HPA) axis and sympathetic–adrenal–medullary axis. Stress produces mental or physical changes, which are mostly harmful, and sometimes the signs of psychological or physical defects are observed. Stress and circadian misalignment from a disturbed sleep-wake cycle can result in metabolic diseases leading to an increase in glucose intolerance, blood pressure, triglycerides, and cardiorespiratory stress. Several studies have demonstrated that sleep quality and quantity are important determinants of whole-body metabolism. Sleep deprivation can affect the metabolic processes and may be responsible for the increasing prevalence of metabolic disorders such as obesity and diabetes.[5] All these have a detrimental effect on the body. Insufficient recovery from sleep deprivation due to long working hours is considered an essential component of the pathway leading to health problems.[6] In addition, the experience of a lack of reciprocity in terms of high “costs” and low “gains” elicits negative emotions in exposed people. In a person, the feelings of not being adequately appreciated or being treated unfairly and disappointments can result in inappropriate rewards, which can cause sustained strain reactions in the autonomic nervous system. This is because the recurrent experience of reward deficiency in a core social role impairs successful self-regulation. In the long term, the imbalance between high effort and low reward at work may increase illness susceptibility due to continued strain reactions.[7] These situations put pressure on the professionals resulting in professional stress.[3] Burnout is a psychological syndrome that arises when employees are exposed to a stressful working environment with high job demands and low resources. Most of the study agrees that burned-out employees are characterized by high levels of exhaustion and negative attitudes toward their work. Burnout results from “social interactions between helpers and recipients,” that is, the prevalence of the stress condition appeared to be confined to caring professions such as teachers, social workers, and health workers. So many of the previous research related to burnout was done on people involved in human service. This assumption excludes the fact that burnout could also be prevalent in “non-human service” professions that do not necessarily require emotional involvement with people. Even people involved in “non-human service” such as information technology are prone to emotional exhaustion, detachment from one's work and a lack of a sense of personal accomplishment and are susceptible to lowered productivity, declining employee morale, and an increase in absenteeism.[5] Occupational stress in white-collar jobs, especially IT professionals, is often underestimated in developing countries like India, which is not well documented. Thus, the main purpose of this study is to bring to the limelight the level of effort-reward imbalance (ERI), burnout, and poor sleep quality among IT employees.
Materials and Method
Study design and setting
This is a cross-sectional survey implemented through online questionnaires.
Study participants and sampling
Software professionals with more than 2-year experience who have consented to participate in the study were recruited by a convenient random sampling technique. 200 IT professionals completed an anonymous web-based questionnaire.
Data collection tools and technique
Sociodemographic details were collected, such as age, gender, years of work experience, time spent on the computer per day, and the number of night shifts per month. Medical history included questions on CVD, such as angina pectoris, myocardial infarction, stroke, heart failure, and other diseases, such as diabetes mellitus, hypertension, and drug treatment. Smoking behavior was assessed by the frequency of smoking, this being divided into daily smokers, ex-smokers, and non-smokers. Alcohol consumption was calculated as grams of pure alcohol per week using the recall of the preceding week. The study included three dependent variables
ERI was measured by a standardized, psychometrically validated questionnaire by Siegrist et al.[8] which has Cronbach's alpha of 0.70. It is composed of three scales: effort, reward, and over-commitment. The effort scale is composed of five questions that refer to perceived demanding aspects of the work, work pressure, responsibility, and over time. The reward is measured by ten items. In reward, three factors result from factor analysis: (a) financial reward, (b) esteem reward, and (c) reward related to promotion prospects. Reward measures financial rewards in terms of income and esteem rewards in terms of appreciation, respect, and support from superiors and colleagues. Promotion related to job benefits, job security, and personal satisfaction. Effort–reward ratio is calculated as (e/r) × c; where “e” is the sum score of the effort scale, “r” is the sum score of the reward scale, and “c” is the correction factor for different numbers of items in the nominator and denominator. The correction factor in this study is 0.5 (5/10). A value of 1, indicates no imbalance, and values >1.0 indicate a high amount of effort spent that is not met by the rewards received or expected.
Overcommitment questionaries measure personal coping characteristics by six questions measuring preoccupation with work and inability to switch off from work.
Response format for all the questions was a four-point Likert scale from 1 = “Strongly disagree, 2 = Disagree, 3 = Agree, 4 = Strongly agree” was used
Oldenburg Burnout Inventory (OLBI) which is psychometrically precise, was used to measure burnout[9] with Cronbach's alpha of 0.85. OLBI measures the two core dimensions of burnout: exhaustion and disengagement from work, using both positively and negatively framed sentences. Exhaustion is defined as a long-term consequence of prolonged exposure to certain job demands. OLDI covers affective, physical, and cognitive aspects of work strain. Disengagement refers to detachment oneself from one's work in general, work object, and work content (e.g., disinterested, no longer challenging, but also “disgusting,” and withdrawal from work). It consists of 16 questions in total, 8 questions in exhaustion, and 8 in disengagement. Each item is scored on a fourpoint Likert scale from 1 = “Strongly agree, 2 = Agree, 3 = Disagree, 4 = Strongly disagree” was used. The exhaustion dimensions and disengagement dimensions are scored separately. The cut-off value of 2.25 for emotional exhaustion and 2.1 for disengagement was considered. Scoring above the cutoffs for both exhaustion and disengagement is considered for the presence of burnout.[10]
Sleep quality was measured using validated Pittsburgh Sleep Quality Index (PSQI) questionnaire with Cronbach's alpha of 0.83. It evaluates sleep quality during a preceding month. It contains 19 self-answered questions belonging to 1 of the 7 subcategories: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each item was scored ranging from 0 for non-difficulty to 3 for severe difficulty and the combination of 7 subcategories yields the global PSQI score which ranges from 0 to 21. Scores > 5 indicates poor sleep quality.[11]
Ethical consideration
This study was approved by the Institutional Research Committee and the Institutional Human Ethics committee (IHEC No: 12/2020/10). The Declaration of Helsinki and National Ethical Guidelines for Biomedical and Health Research 2017 by the Indian Council of Medical Research were followed throughout the study
Statistical analysis
Statistical analysis was done using the Statistical Package for the Social Sciences (SPSS) 17.0 (IBM Corp., Armonk, NY, USA) software. Shapiro–Wilk test was done to check for data normality. All normally distributed data were represented as mean and standard deviation. Pearson correlation coefficient was done to find the association between ERI, burnout, and sleep disturbance. Gender difference in ERI, burnout, and sleep quality component was assessed using an independent t-test. The exhaustion means exceeding disengagement means, and effort means exceeding reward means were compared by paired t-test. The number of respondents with exhaustion means higher than disengagement versus the opposite pattern, and the numbers of respondents with higher effort means than reward versus the opposite pattern were compared with a sign test. Multiple linear regression analyses were performed. P < 0.05 with two-tailed tests was considered significant.
Results
The characteristics of the study population are shown in Table 1, 200 IT professionals participated in the study with a mean age of 29.3 ± 4 and were predominantly male, around 68%. Table 2 shows effort-reward scores of the study population, and ERI is present in 144 (72%) of the study population. The sum of effort scores was not different in both gender, and women tended to have less sum of reward scores compared to male (P < 0.01), and overcommitment was higher in females (P < 0.01), the mean for effort exceeded that for reward by (0.414 ± 0.686) range 0.318–0.509, 95% confidence interval, t (199) = 8.5 P < 0.01 by paired t-test.
Table 1.
Characteristics of study population
| Parameter | (n=200) |
|---|---|
| Age (years) | 29.3±4 (Mean±SD) |
| Gender | |
| Male | 137 |
| Female | 63 |
| Work experience (years) | 8±3.5 (mean±SD) |
| Time spent in computer per day (hours) | 9.3±1.5 (mean±SD) |
| Smoking | 18.5% |
| Alcohol | 28% |
| Hypertensive | 16.5% |
| Diabetic | 8% |
| Night shift | 33% |
Table 2.
Effort reward scores of study population
| Parameters | Mean±SD |
|---|---|
| Effort | 2.82±0.44 |
| Reward | 2.40±0.44 |
| Overcommitment | 2.22±0.43 |
| ERI | 1.21±0.29 |
The values of effort versus reward for each respondent are plotted in Figure 1. More respondents (N = 146, 73%) had a higher mean for effort than reward (points above the diagonal line) than the opposite pattern (N = 50, 25%, points below the diagonal line), P < 0.0001 by sign test. The other N = 4 (12%) had equal effort, and reward means. Effort means were generally negatively associated with reward means, r = −.204, P < 0.004 by Pearson correlation coefficient. The Cronbach alpha for the ERI scale in this sample was 0.77.
Figure 1.
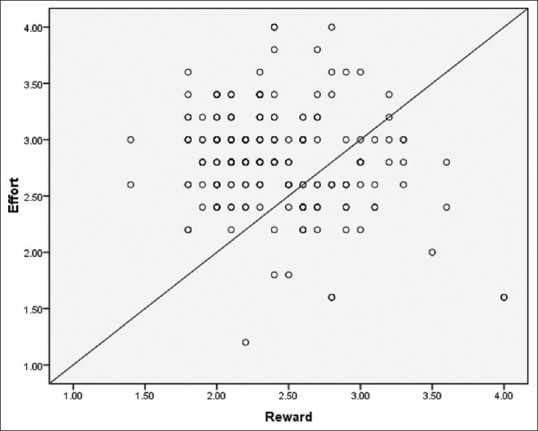
Showing scatter plots for Effort means versus Reward means
Burnout scores of the study population were presented in Table 3. 60% of the participants (N = 120), recorded scores consistent with burnout, the mean for exhaustion exceeded that for disengagement by 0.239 ± 0.384 (range 0.185–0.293 95% confidence interval, t (199) = 8.803 P < 0.01 by paired t-test. Exhaustion means score was higher in females compared to males (P < 0.05), and some of the disengagement scores did not show any gender difference.
Table 3.
Burnout score of the study population
| Parameters | Mean±SD |
|---|---|
| Exhaustion | 2.46±0.47 |
| Disengagement | 2.22±0.34 |
| Burnout score | 2.34±0.37 |
The values of exhaustion versus disengagement for each respondent are plotted in Figure 2. More respondents (N = 140, 70%) had a higher mean for exhaustion than disengagement (points above the diagonal line) than the opposite pattern (N = 28, 17.5%, points below the diagonal line), P < 0.0001 by sign test. The other N = 25 (12.5%) had equal exhaustion and disengagement means. Higher exhaustion means were generally associated with higher disengagement means, r = 0.59, P < 0.0001 by Pearson correlation coefficient. The internal reliability of the scale used in this study was 0.805.
Figure 2.
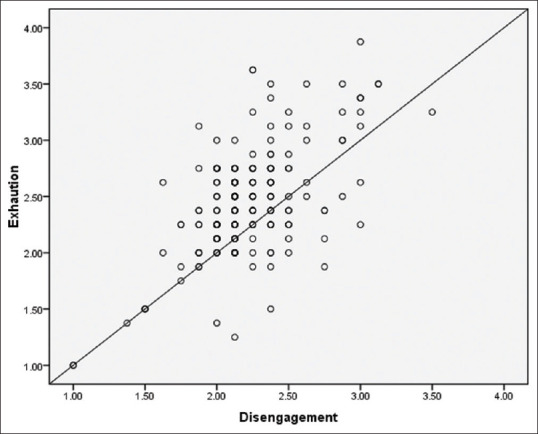
Showing scatter plots for exhaustion means versus disengagement means
Table 4 shows the PQSI component score of the study population. 70% of the study population were found to be poor sleepers (PQSI sleep score > 5), and 12% of the total population's sleep duration was less than 6 hours. The Cronbach alpha for the PQSI scale in this sample was 0.71. Sleep quality dimension of subject sleep quality (P < 0.05), sleep latency (P < 0.01), habitual sleep efficiency (P < 0.05), daytime dysfunction (P < 0.01) were worse in female compared to males. Sleep disturbance, use of sleeping medication, and sleep duration dimension were similar in both genders.
Table 4.
PQSI component score of the study population
| Parameters | Mean±SD |
|---|---|
| Sleep quality | 1.35±0.74 |
| Latency | 1.53±0.99 |
| Duration | 1.22±0.87 |
| Habitual sleep efficiency | 0.69±0.95 |
| Disturbance | 1.19±0.62 |
| Use of medication | 0.35±0.83 |
| Daytime dysfunction | 1.04±0.89 |
| PQSI global score | 7.39±3.61 |
The level of burnout scores and PQSI increased with increasing ERI. The correlation coefficient for ERI to burnout and PQSI score were r = 0.454 and 0.314, respectively, P < 0.01.
Though age and years of experience are strongly intercorrelated (r = 0.86, P < 0.01) were not associated with burnout, work life imbalance, and PQSI sleep score.
Both exhaustion and disengagement correlated with PSQI sleep scores (r = 0.378, P < 0.01) and (r = 0.287, P < 0.01). On further analysis, we also found that exhaustion and burnout correlated with all the sleep components (P < 0.01). We notice that disengagement correlates with most of the sleep components except sleep latency and sleep duration.
Sum of reward was negatively correlated with PQSI sleep score (r = −0.261, P < 0.01), overcommitment (r = −0.436, P < 0.01), disengagement (r = −0.404, P < 0.01), exhaustion (r = −0.453, P < 0.01), and on average hours on computer on a day (r = −0.155, P < 0.05). Positive correlation between overcommitment and PQSI score (r = 0.40, P < 0.001) indicates overcommitment leads to poor quality of sleep. There was a significant association between ERI with sleep disturbance (x2 = 14.81, P < 0.01) and burnout category (x2 = 11.61, P = 0.001), Higher effort, lower reward, and greater overcommitment were associated with higher burnout and greater PQSI score.
Gender differences in ERI, burnout, and sleep score are depicted in Table 5, which shows that females have a higher ERI, burnout, and poor sleep quality compared to males.
Table 5.
Gender difference in ERI, burnout, and sleep score
| Parameter | Male | Female | P |
|---|---|---|---|
| ERI | 1.14±0.29 | 1.35±0.25** | 0.000 |
| Burnout | 2.28±0.38 | 2.46±0.37* | 0.002 |
| PSQI | 6.91±3.4 | 8.44±3.8* | 0.005 |
*P<0.05, **P<0.01
Table 6 shows the Regression analysis
Table 6.
Regression analysis
| Dependent variable | R 2 | Corrected R2 | F (196.3) | β coefficient | t | P |
|---|---|---|---|---|---|---|
| Emotional exhaustion | 0.550 | 0.543 | 79.713 | <0.01 | ||
| Independent variable | ||||||
| Effort | 0.136 | 2.743 | 0.009 | |||
| Reward | −.160 | −2.979 | 0.003 | |||
| Overcommitment | 0.609 | 11.26 | <0.01 | |||
| Dependent variable | R 2 | Corrected R2 | F (198.1) | β coefficient | t | P |
| Burnout | 0.238 | 0.234 | 61.81 | 0.488 | 7.864 | <0.01 |
| Independent variable | ||||||
| ERI | ||||||
| Dependent variable | R 2 | Corrected R2 | F (198.1) | β coefficient | t | P |
| PQSI | 0.099 | 0.094 | 21.70 | 0.314 | 4.65 | <0.01 |
| Independent variable | ||||||
| ERI |
Emotional exhaustion was predicted by all ERI scales entered in the model, that is, effort, reward, and overcommitment; this model explained 55% of the variance. As expected, effort and overcommitment contributed positively to the model, while the reward was negatively associated with emotional exhaustion. Linear regression to assess the ability of ERI to predict levels of burnout yielded a statistically significant (R2 = 0.206, P < 0.01) indicating, ERI to be a unique incremental predictor of burnout (b = 0.454, t = 7.16, P < 0.01). ERI tends to be a predictive factor of poor sleep quality with an odd's ratio of 3.5, 95%CI (1.81–6.73), P < 0.01
Discussion
In India, with the development of economic globalization, growing competition, and the development of new technology, today's working life has changed enormously, leading to work-related stress.[12] It has led to a growth in high flexibility and mobility, short-term contracts, and increasing job insecurity among IT professionals.[13] From this specific viewpoint, reward plays a vital role in current job content, which is influenced significantly by unfair or inadequate salaries, lack of esteem, poor promotion prospects, or job insecurity.[7] Consistent with the theoretical assumption of the ERI model, our study showed that ERI was more likely to explain burnout and poor sleep quality among IT workers.
The objective of the present study was to investigate associations between the experience of work stress among IT professionals, as measured by the model of ERI, burnout, and poor-quality sleep. We hypothesized that higher effort and ERI would be positively associated with emotional exhaustion, disengagement, and poor sleep quality. The reward component would be negatively associated with emotional exhaustion, disengagement, and poor sleep quality.
In this study, we found that higher ERI resulted in higher exhaustion and higher disengagement resulting in burnout. In a study by Takaki et al.[14] in IT professionals, higher ERI and overcommitment score was associated with fatigue, Violanti et al.[15] also showed that ERI and overcommitment were positively and significantly associated with burnout assessed among police officers. ERI and overcommitment were significant risk factors for self-reported health for men and women. Niedhammer et al.[16] reported a significant association between ERI and poor physical functioning in both genders.
A study by Siegris et al. showed ERI individuals have a high risk of coronary artery disease.[17] According to the ERI model in this study, burnout is due to the recurrent experience of a failed reciprocity between the effort spent at work and the rewards received. In addition to remuneration and salary, rewards include nonmaterial aspects, such as respect, recognition, promotion prospects, and job security. There are several studies demonstrating a link between ERI and burnout.[18,19,20,21] So, consistent with other studies, our study showed that an increase in ERI results in increased burnout in IT professionals.
In a pressure predominant environment, IT professionals find themselves in a vicious cycle of cutting down on sleep to cope and adjust to increasing workloads. Poor sleep quality is critically linked to burnout.[22] Both the quality and quantity of sleep affect an individual's ability to cope with emotional challenges. Sleep deprivation and sleep disturbances trigger negative emotional reactivity and diminish the effect of positive emotions.[23] We found that 70% of the sampled Indian IT professionals tested positive for poor sleep quality (mean: 7.39 ± 3.61). Sleep disturbances may promote the onset of burnout because they compromise the restorative function of sleep. Sleep is necessary for restoring energy for everyday functioning, whereas sleep disturbance augments one's sensitivity to negative emotions and stressful events.[24] In a study by Zadeh et al.[25] in software engineers reported insomnia around 56% of the study population, and this percentage was higher compared to the general population, Nishikitani et al.[26] also showed sleep duration in software engineers was negatively related to anxiety level. The relationship between poor sleep quality and burnout in our study is compatible with other studies, In a study by Nelson et al.[27] demonstrates that sleep monitored over 7 months by activity tracker in burnout individuals experienced decreased sleep quality, sleep duration, and light sleep compared to their health participants. A prospective study by Armon et al.[28] showed that burnout and insomnia predicted each other's development and incremented over time, thus suggesting that each might be a risk factor for the other over the time, it showed burnout predicted subsequent cases of insomnia (OR = 1.93) and changes in levels of insomnia (b = 0.05, P < 0.05), and that insomnia predicted subsequent cases of burnout (OR = 1.64) and changes in levels of burnout (b = 0.07, P < 0.05) at 18-month follow-up thus shows the association between burnout and insomnia is bidirectional.
From a physiological point of view, burnout leading to poor sleep quality and vice versa may develop; burnout and poor sleep quality may predict each other's development. Association between burnout and insomnia is bidirectional. For example, difficulties in falling asleep, unrefreshing sleep, and waking up exhausted may lead to profound exhaustion, which may exacerbate the symptoms of fatigue among those already burned out, leading to sustained burnout. High pressure during the day, working late, long working hours, or an inability to detach from work-related issues lead to poor sleep quality. This suggests that burnout and insomnia are reciprocally related. Burnout and poor sleep quality share similar underlying physiological mechanisms. Evidence suggests that burnout is associated with the disturbance of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathovagal disturbance system.[29] Similarly, dysregulation of the HPA axis and the sympathetic nervous system was also observed in insomnia.[30] In most studies, poor sleep was found to be linked to altered plasma cortisol levels,[31,32] similar to the burnout studies.[33]
Our study reported that higher scores on ERI components were associated with poor sleep quality. In line with our study Fahlén et al.[34] reported that higher effort, ERI, and higher overcommitment were associated with sleep disturbances. A study by Rugulies et al.[35] reported that a higher ERI quartile demonstrated an Odds ratio of 2.26 (95% CI = 1.56–3.27, P <.001) for sleep disturbances. In our study, ERI tends to be a predictive factor of poor sleep quality with an Odds ratio = 3.5, 95%CI (1.81–6.73), P < 0.01. A prospective study by Kudielka et al.[36] demonstrated that poor sleep quality and disturbed sleep were associated with higher effort, overcommitment, and lesser reward. Higher overcommitment was associated with sleep disturbances among men, while sleep disturbances among women were related to lower reward and higher overcommitment. In a study by Utsugi et al.[37] it was reported that ERI, higher effect, and overcommitment were independently associated with insomnia with odds ratios of 2.47, 1.65, and 1.89 in males and 1.77, 1.48, and 1.63 in females, respectively. Similar to many other studies,[38,39] our study results showed that females reported poor quality of sleep compared to males. The present study thereby supports the finding from previous studies about the consequences of ERI and overcommitment on sleep disturbances. The physiological mechanism between ERI and poor sleep quality may be due to ERI that is associated with cortisol elevation.[40] Cortisol and HPA axis disturbances are also associated with sleep disturbances.[31] Thus the HPA axis disturbance may be related to sleep disturbances induced by occupational stress. In summary, this study found that an increased ERI among IT professionals was associated with significantly increased levels of burnout and poor quality of sleep.
Limitation and recommendation
This study relied on a self-reported measure of both independent and dependent variables; therefore, the common method variance might bias the associations in this study. The lack of an objective measure of impaired health or functional capacity is this study's other limitation. ERI, burnouts are dynamic processes, and results may vary when the assessment was conducted in a different period or on multiple occasions.
Conclusion
This study is the first of its kind to employ ERI to predict burnout and sleep disturbance among IT professionals in South India. Further research is needed to assess the importance of monitoring work environments systematically and regularly at the company level and implementing measures to reduce any adverse effects of detected ERI. Some of the interventions that can be included are securing better wage and promotion opportunities, developing better methods for recognition and supportive leadership, reducing working time and workload, and improving control and autonomy at work. These measures may be reinforced nationally and internationally to reduce burnout among IT professionals. Adding stress management training could help the IT professionals to deal more effectively with the work strain, develop personal techniques for helping themselves to improve their professional path, and potentially prevent upcoming burnout and sleep disturbances.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors acknowledge their gratitude to all the participants of this study.
References
- 1.Kumar MS. A study on occupational stress among it professionals chennai. Int J Enterpr Innov Manag Stud (IJEIMS) 2011;2:119–24. [Google Scholar]
- 2.Darshan MS, Raman R, Rao TS, Ram D, Annigeri B. A study on professional stress, depression and alcohol use among Indian IT professionals. Indian J Psychiatry. 2013;55:63–9. doi: 10.4103/0019-5545.105512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maudgalya T, Wallace S, Daraiseh N, Salem S. Workplace stress factors and 'burnout’ among information technology professionals: A systematic review. Theor Issues Ergon Sci. 2006;7:285–97. [Google Scholar]
- 4.Bolhari A, Rezaeian A, Bolhari J, Bairamzadeh S. Occupational stress level among information technology professionals in Iran. Int J Inf Electron Eng. 2012;2:682–5. [Google Scholar]
- 5.Maudgalya T, Wallace S, Daraiseh N, Salem S. Workplace stress factors and 'burnout’ among information technology professionals: A systematic review. Theor Issues Ergon Sci. 2006;7:285–97. [Google Scholar]
- 6.Nakashima M, Morikawa Y, Sakurai M, Nakamura K, Miura K, Ishizaki M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res. 2011;20:110–6. doi: 10.1111/j.1365-2869.2010.00852.x. [DOI] [PubMed] [Google Scholar]
- 7.Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, et al. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. 2004;58:1483–99. doi: 10.1016/S0277-9536(03)00351-4. [DOI] [PubMed] [Google Scholar]
- 8.Siegrist J, Li J, Montano D. Germany: Duesseldorf University; 2014. Jun 4, Psychometric properties of the effort-reward imbalance questionnaire. [Google Scholar]
- 9.Halbesleben JRB, Demerouti E. The construct validity of an alternative measure of burnout: Investigating the English translation of the Oldenburg Burnout Inventory. Work Stress. 2005;19:208–20. [Google Scholar]
- 10.Demerouti E, Bakker AB. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. Handbook of stress and burnout in health care. 2008 Jan;65(7) [Google Scholar]
- 11.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 12.Ramesh N, Joseph B, Kiran P, Kurian J, Babu A. Perceived professional stress levels among employees in an information technology company, Bangalore. Stress. 2016;9:11–2. [Google Scholar]
- 13.Karamchandani K, Dubule DVK. Job anxiety and occupational stress among employees of IT sector: Impact on their attitude towards management. Int J Eng Manag Res. 2020;10:37–44. [Google Scholar]
- 14.Takaki J, Nakao M, Karita K, Nishikitani M, Yano E. Relationships between effort-reward imbalance, over-commitment, and fatigue in Japanese information-technology workers. J Occup Health. 2006;48:62–4. doi: 10.1539/joh.48.62. [DOI] [PubMed] [Google Scholar]
- 15.Violanti JM, Mnatsakanova A, Andrew ME, Allison P, Gu JK, Fekedulegn D. Effort-reward imbalance and overcommitment at work: Associations with police burnout. Police Q. 2018;21:440–60. doi: 10.1177/1098611118774764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niedhammer I, Tek ML, Starke D, Siegrist J. Effort-reward imbalance model and self-reported health: Cross-sectional and prospective findings from the GAZEL cohort. Soc Sci Med. 2004;58:1531–41. doi: 10.1016/S0277-9536(03)00346-0. [DOI] [PubMed] [Google Scholar]
- 17.Siegrist J. Effort-reward imbalance at work and cardiovascular diseases. Int J Occup Med Environ Health. 2010;23:279–85. doi: 10.2478/v10001-010-0013-8. [DOI] [PubMed] [Google Scholar]
- 18.Diekmann K, Böckelmann I, Karlsen HR, Lux A, Thielmann B. Effort-reward imbalance, mental health and burnout in occupational groups that face mental stress. J Occup Environ Med. 2020;62:847–52. doi: 10.1097/JOM.0000000000001978. [DOI] [PubMed] [Google Scholar]
- 19.Jachens L, Houdmont J, Thomas R. Effort-reward imbalance and burnout among humanitarian aid workers. Disasters. 2019;43:67–87. doi: 10.1111/disa.12288. [DOI] [PubMed] [Google Scholar]
- 20.Bakker AB, Killmer CH, Siegrist J, Schaufeli WB. Effort-reward imbalance and burnout among nurses. J Adv Nurs. 2000;31:884–91. doi: 10.1046/j.1365-2648.2000.01361.x. [DOI] [PubMed] [Google Scholar]
- 21.Colindres CV, Bryce E, Coral-Rosero P, Ramos-Soto RM, Bonilla F, Yassi A. Effect of effort-reward imbalance and burnout on infection control among Ecuadorian nurses. Int Nurs Rev. 2018;65:190–9. doi: 10.1111/inr.12409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arora RS, Thawani R, Goel A. Burnout and sleep quality: A cross-sectional questionnaire-based study of medical and non-medical students in India. Cureus. 2015;7:e361. doi: 10.7759/cureus.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 24.Vandekerckhove M, Wang YL. Emotion, emotion regulation and sleep: An intimate relationship. AIMS Neurosci. 2018;5:1–17. doi: 10.3934/Neuroscience.2018.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zadeh SS, Begum K. Association between insomnia and quality of life: An exploratory study among software engineers. Appl Res Qual Life. 2011;6:335–47. [Google Scholar]
- 26.Nishikitani M, Nakao M, Karita K, Nomura K, Yano E. Influence of overtime work, sleep duration, and perceived job characteristics on the physical and mental status of software engineers. Ind Health. 2005;43:623–9. doi: 10.2486/indhealth.43.623. [DOI] [PubMed] [Google Scholar]
- 27.Nelson EC, Keijzer RD, Vollenbroek-Hutten MM, Verhagen T, Noordzij ML. In EAI International Conference on Body Area Networks 2019 Oct 2. Springer, Cham; The relationship between diagnosed burnout and sleep measured by activity trackers: four longitudinal case studies; pp. 315–331. [Google Scholar]
- 28.Armon G, Shirom A, Shapira I, Melamed S. On the nature of burnout-insomnia relationships: A prospective study of employed adults. J Psychosom Res. 2008;65:5–12. doi: 10.1016/j.jpsychores.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Academic Psychiatry. 2014 Aug;38(4):438–44. doi: 10.1007/s40596-014-0093-z. [DOI] [PubMed] [Google Scholar]
- 30.Nicolaides NC, Vgontzas AN, Kritikou I, Chrousos G. HPA axis and sleep. Endotext [Internet] 2020 Nov 24; [Google Scholar]
- 31.Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865–70. [PubMed] [Google Scholar]
- 32.Vgontzas AN, Zoumakis M, Bixler EO, Lin HM, Prolo P, Vela-Bueno A, et al. Impaired nighttime sleep in healthy old versus young adults is associated with elevated plasma interleukin-6 and cortisol levels: Physiologic and therapeutic implications. J Clin Endocrinol Metab. 2003;88:2087–95. doi: 10.1210/jc.2002-021176. [DOI] [PubMed] [Google Scholar]
- 33.Kudielka BM, Bellingrath S, Hellhammer DH. Cortisol in burnout and vital exhaustion: An overview. G Ital Med Lav Ergon. 2006;28(1 Suppl 1):34–42. [PubMed] [Google Scholar]
- 34.Fahlén G, Knutsson A, Peter R, Åkerstedt T, Nordin M, Alfredsson L, et al. Effort-reward imbalance, sleep disturbances and fatigue. Int Arch Occup Environ Health. 2006;79:371–8. doi: 10.1007/s00420-005-0063-6. [DOI] [PubMed] [Google Scholar]
- 35.Rugulies R, Norborg M, Sørensen TS, Knudsen LE, Burr H. Effort-reward imbalance at work and risk of sleep disturbances. Cross-sectional and prospective results from the Danish Work Environment Cohort Study. J Psychosom Res. 2009;66:75–83. doi: 10.1016/j.jpsychores.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 36.Kudielka BM, Von Känel R, Gander ML, Fischer JE. Effort-reward imbalance, overcommitment and sleep in a working population. Work Stress. 2004;18:167–78. [Google Scholar]
- 37.Utsugi M, Saijo Y, Yoshioka E, Horikawa N, Sato T, Gong Y, Kishi R. Relationships of occupational stress to insomnia and short sleep in Japanese workers. Sleep. 2005 Jun 1;28(6):728–35. doi: 10.1093/sleep/28.6.728. [DOI] [PubMed] [Google Scholar]
- 38.Panda S, Taly AB, Sinha S, Gururaj G, Girish N, Nagaraja D. Sleep-related disorders among a healthy population in South India. Neurol India. 2012;60:68–74. doi: 10.4103/0028-3886.93601. [DOI] [PubMed] [Google Scholar]
- 39.Fatima Y, Doi SAR, Najman JM, Al Mamun A. Exploring gender difference in sleep quality of young adults: Findings from a large population study. Clin Med Res. 2016;14:138–44. doi: 10.3121/cmr.2016.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steptoe A, Siegrist J, Kirschbaum C, Marmot M. Effort-reward imbalance, overcommitment, and measures of cortisol and blood pressure over the working day. Psychosom Med. 2004;66:323–9. doi: 10.1097/01.psy.0000126198.67070.72. [DOI] [PubMed] [Google Scholar]


