Abstract
Background
The COVID-19 pandemic has changed the landscape of healthcare service delivery. This review aims to describe telemedicine-delivered substance use disorder (SUD) treatments and services along the cascade of care in the U.S. after the start of the COVID-19 pandemic.
Methods
A literature review was conducted on PubMed, Embase, Web of Science, and Cochrane Library (Wiley). English-language articles that describe any healthcare services for patients with SUDs using telemedicine in the U.S. since the onset of the COVID-19 pandemic were identified (N = 33). We narratively summarized telemedicine-based service provision along the cascade of SUD care, such as screening/assessment, prescription, monitoring, recovery support, and other services.
Results
Soon after the onset of COVID-19 and mandated restrictions, cadres of healthcare providers from different specialties mobilized to ramp up video- and audio-based services to remotely treat patients with SUDs. Medication prescription (48.5%) and individual counseling (39.4%) were the most frequently reported services delivered via telemedicine. Other steps of SUD care delivered by telemedicine characterized in our review included SUD screening and assessment (30.3%), induction (21.2%), medication management (27.3%), monitoring (27.3%), recovery support (15.2%), and referral (24.2%). Feasibility issues and challenges to implementing telemedicine included patients’ lack of access to technology and health insurance coverage, providers’ capacity limits and concerns, and clinics’ financial and office-space constraints.
Conclusion
The COVID-19 pandemic has offered a window of opportunity to advance telemedicine expertise by formalizing clinical guidance and routinizing provider in-service training in virtual SUD treatment. Findings suggest enhanced efforts to reduce disparities in telemedicine-based services.
Keywords: Telemedicine; Substance use disorder; COVID-19, Healthcare services
1. Introduction
The COVID-19 pandemic that started in early 2020 has brought unprecedented challenges to the provision of essential health services globally and in the U.S. (U.S. Department of Health & Human Services, 2021, World Health Organization, 2021). Individuals with substance use disorders (SUDs) face a heightened risk of severe COVID-19 infection, attributable to their underlining health conditions (Center for Disease Control and Prevention, 2021). Moreover, during the pandemic, individuals with SUD faced intensified difficulties accessing SUD treatment, which resulted in increased drug use and more drug overdose fatalities (Panchal et al., 2021, Ornell et al., 2020).
Fortunately, many healthcare systems in the U.S. made prompt adaptations to ensure continued service delivery for patients with SUDs (Pinals et al., 2020, Leahy and Caverly, 2022). Policy and regulation changes were made at federal and state levels to allow flexibility in SUD care during the pandemic (Andraka-Christou et al., 2021, Hughes et al., 2021, Lin et al., 2020, Pessar et al., 2021, Uscher-Pines and Martineau, 2021). With the federal declaration of a nationwide public health emergency as the result of COVID-19, the Drug Enforcement Administration (DEA) announced that DEA-registered providers could legally prescribe controlled substances to a patient without requiring an in-person evaluation (Lin et al., 2020, U.S. Department of Justice and Drug Enforcement Administration, 2020). The Substance Abuse and Mental Health Services Administration (SAMHSA) provided clinical guidance for virtual buprenorphine induction (Substance Abuse and Mental Health Services Administration, 2020). Many states also revised insurance policies to improve reimbursement parity for telemedicine-delivered services, compared to in-person care (National Academy for State Health Policy, 2021, Pessar et al., 2021). Supported by these policies and regulations, the use of telemedicine rapidly accelerated in SUD treatment services in the U.S. (Oesterle et al., 2020). It was reported that telemedicine-based mental health and SUD visits increased from less than 1% before the pandemic to approximately 40% in October 2020 (Busch et al., 2021).
Several review articles describe the impact of COVID-19 on outcomes of SUDs and other diseases, healthcare settings’ responses to the pandemic, potential impacts of telemedicine in SUD treatment, and specific populations’ healthcare and emotional needs (Batra et al., 2020, Chan et al., 2022; De Vargas et al., 2021; Kumar et al., 2022). This article contributes to the literature by examining the current landscape of telemedicine-based SUD treatment services that have been provided in the U.S. since the onset of the COVID-19 pandemic.
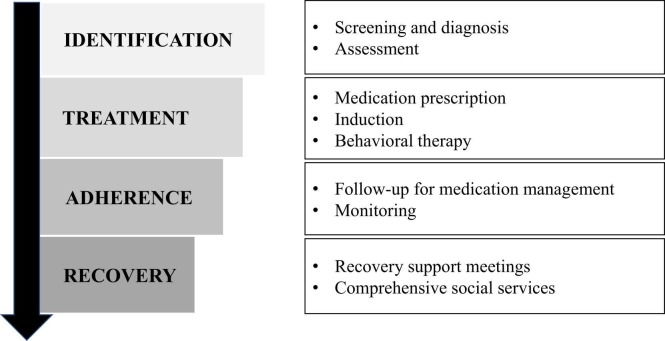
The ‘cascade of care’ model provides a framework to categorize healthcare services and identify gaps in healthcare services, including as adapted for SUD care ( Fig. 1. National Institute on Drug Abuse, 2019; Socías et al., 2016; Williams et al., 2019). The “cascade of care” model, which was originally developed to track key stages of HIV/AIDS control, has been used to evaluate population-level indicators of SUD care efforts by estimating the proportion of patients who are in salient stages from identification, linkage to care, treatment initiation, retention, to recovery (Socías et al., 2016; Williams et al., 2019). Telemedicine can play major roles along the cascade, being used to deliver screening, diagnosis, treatment, and recovery (Wang et al., 2021). Guided by the cascade of care model, we conducted a literature review regarding existing SUD services delivered via telemedicine. We summarized findings within steps of the cascade of care for SUD: identification, treatment, adherence, and recovery. Within each step, we discussed service types, models of service delivery, settings, and providers. We discussed the frequencies of telemedicine utilization among patients and providers, and summarized barriers and challenges for telemedicine along each step of the SUD cascade of care. This review summarizes the current knowledge base regarding the management of care for persons with SUDs via telemedicine, sheds light on gaps in that knowledge, and suggests priorities for future studies and public health.
Fig. 1.
SUD Cascade of Care Framework for Telemedicine Service.
2. Methods
2.1. Search strategy
The literature search, screening, selection, coding, and reporting were guided by the framework by Tong et al. (2012), enhancing transparency in reporting the synthesis of qualitative research (ENTREQ). We conducted comprehensive searches on electronic databases including PubMed, Embase, Web of Science, and Cochrane Library (Wiley). The search was conducted using four major concepts: 1) telemedicine (including telehealth, telepsychiatry, telepsychology, telemental health, live video- or phone counseling); 2) substance use (substance use disorder, addiction, substance abuse, substance dependence, opioid, marijuana, stimulant, cannabis, hallucinogen); 3) substance use treatment and services along the cascade of care (including screening, medication prescription, behavioral therapy, urine drug screening [UDS], recovery); and 4) COVID-19 (COVID; SARS-CoV-2). With the assistance of a professional librarian, specific keywords and indexing terms (e.g., MeSH terms for PubMed, Emtree for Embase) were created to guide the systematic search and additional hand searches were conducted using Google Scholar. Identified records were imported into a Mendeley Reference Manager folder to identify and remove duplicates. The ending day of searching was March 31, 2022.
2.2. Screening criteria
After the duplicated records were removed, a total of 508 individual records were imported into Rayyan (a web and mobile app for systematic reviews developed by Rayyan Systems Inc. Ouzzani et al., 2016) for initial screening. During the screening process, the articles were excluded if they met any of the following criteria: 1) data were collected before the declaration of public health emergency due to COVID-19 on January 31, 2020; 2) the study was conducted outside the U.S.; 3) the topic was not related to telemedicine healthcare services for SUDs; 4) the article did not report primary data collection (i.e., we excluded review articles and protocol papers); 5) the article was not published in a peer-reviewed journal; and 6) the full-text article was not available.
2.3. Data extraction and analysis
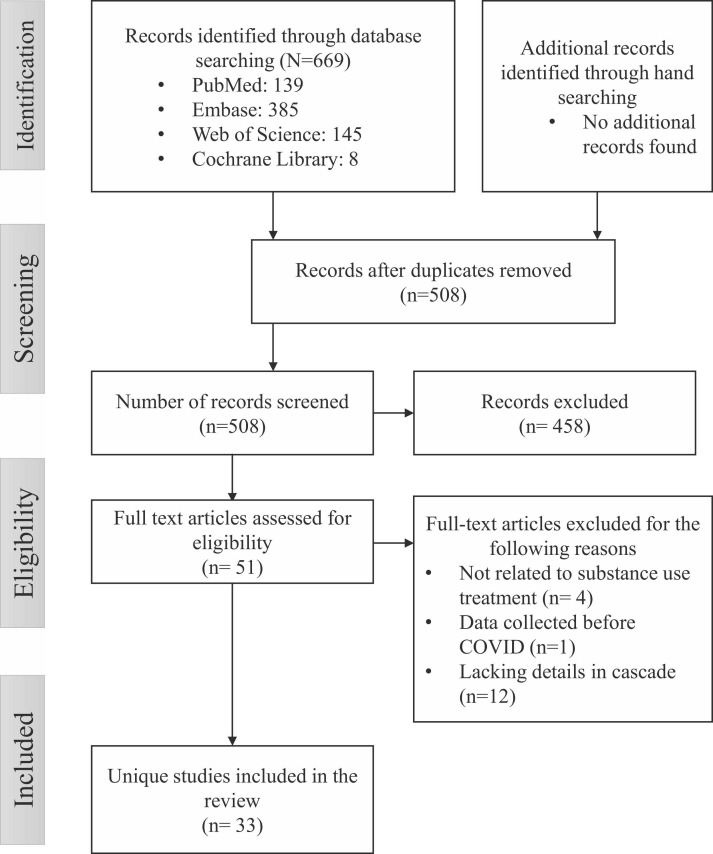
The screening process yielded 51 studies that potentially met eligibility criteria. Full-text articles were downloaded and imported into Atlas.ti (Version 22.0) for content analysis. Guided by the cascade of care framework, initial code lists were developed to characterize the study and capture the SUD cascade of care described in the published article. The priori codes evolved throughout the coding process to capture additional steps of the cascade of care, as well as themes around service delivery and barriers that emerged from the articles. The coding was performed by four PhD-level addiction health service researchers. During the coding process, an additional 18 articles were removed due to a lack of focus on SUD care or insufficient details on telemedicine use across the SUD cascade of care ( Fig. 2) We categorized the 33 papers in the final list according to type, study design, location, setting, provider and patient populations, steps within the cascade of care, and main findings, then generated descriptive statistics. Each article record was cross-checked by two coders to ensure the correctness and completeness of the extracted data. The descriptions of telemedicine service provision in the selected articles were synthesized in accord with the SUD cascade of care.
Fig. 2.
Flowchart of the Selection of Studies.
3. Results
3.1. Study characteristics
The study characteristics are summarized in Table 1. Approximately two-thirds (69.7%) of the articles were published in 2021. Over half (57.5%) were original research articles, 7 (21.2%) were commentaries, and the rest were brief reports or letters. Over half (51.5%) of the articles were descriptions of practice changes and approximately one-third of the studies (30.3%) collected data from service providers/clinic administrators through in-depth interviews, focus groups, or surveys; and the remaining studies evaluated patients’ perspectives using surveys, case studies, or secondary data analysis. The majority (66.7%) of studies were conducted in coastal states: California (15.2%), Massachusetts (12.1%), Rhode Island (12.1%), Maryland (9.1%), Florida (6.1%), New York (6.1%), Pennsylvania (3.0%), and Oregon (3.0%). The studies covered a variety of settings, including large, comprehensive medical centers (18.2%), primary care clinics (15.2%), SUD outpatient clinics (12.1%), "bridge" clinics (9.1%), SUD residential clinics (3.0%), detention centers (3.0%), etc., with 30.3% of the studies involving multiple settings.
Table 1.
Summary of characteristics of included studies.
| Number of articles (33 total) | % of the 33 articles | |
|---|---|---|
| Year of publication | ||
| 2020 | 4 | 12.1% |
| 2021 | 23 | 69.7% |
| 2022 (January to March) | 6 | 18.2% |
| Type of publication | ||
| Original article | 19 | 57.5% |
| Commentary | 7 | 21.2% |
| Brief report | 5 | 15.1% |
| Letter | 2 | 6.1% |
| Study design | ||
| Description | 17 | 51.5% |
| Survey of stakeholder/provider | 6 | 18.2% |
| Focus group/interview with providers | 4 | 12.1% |
| Survey of patients | 1 | 3.0% |
| Case study | 2 | 6.1% |
| EHR or claims data analysis | 2 | 6.1% |
| Cohort study | 1 | 3.0% |
| Location | ||
| Nationwide | 2 | 6.1% |
| More than one state | 3 | 9.1% |
| CA | 5 | 15.2% |
| MA | 4 | 12.1% |
| RI | 4 | 12.1% |
| MD | 3 | 9.1% |
| FL | 2 | 6.1% |
| NY | 2 | 6.1% |
| DC | 1 | 3.0% |
| KS | 1 | 3.0% |
| OH | 1 | 3.0% |
| OR | 1 | 3.0% |
| PA | 1 | 3.0% |
| VT | 1 | 3.0% |
| Setting | ||
| Multiple settings | 10 | 30.3% |
| Medical centers | 6 | 18.2% |
| Primary care clinic | 5 | 15.2% |
| Bridge clinic | 3 | 9.1% |
| Outpatient clinic | 4 | 12.1% |
| SUD residential setting | 1 | 3.0% |
| Detention center | 1 | 3.0% |
| Mobile clinic | 1 | 3.0% |
| Other types | 2 | 6.1% |
| Cascade of care | ||
| Screening and assessment | 10 | 30.3% |
| Prescription | 16 | 48.5% |
| Induction | 7 | 21.2% |
| Medication management/between visit care | 9 | 27.3% |
| Individual/group counseling | 16 | 48.5% |
| Monitoring | 10 | 30.3% |
| Recovery | 5 | 15.2% |
| Care for comorbidities | 2 | 6.1% |
| Referral | 10 | 30.3% |
3.2. Overall implementation of telemedicine for SUD
The articles consistently indicated a rapid transition to telemedicine to continue treatment and care for patients with SUD since the onset of the COVID-19 pandemic. Multiple cadres of healthcare professionals, including clinicians with a DEA X-waiver to prescribe buprenorphine (Jones et al., 2021; Uscher-Pines et al., 2020), medical students (Castillo et al., 2020), counselors (Martin et al., 2021), case managers (Harris et al., 2022), outreach volunteers (Levander et al., 2022), and third-party telemedicine vendors (Hser et al., 2021), were mobilized to enable the provision of telemedicine-delivered SUD treatment services. The two major modalities of telemedicine delivery included telephone (audio only) and video (Jones et al., 2021, Rahman et al., 2021). In a nationwide survey of 457 organizations treating SUD, telephone- and video-based telemedicine delivery was reported by 84.4% and 68.8% of the organizations, respectively, with more than 70% of the organizations reported using both (Molfenter et al., 2021). Telephone-delivered telemedicine was mainly offered as an option for patients who had limited computer literacy, lacked devices, or encountered other technological problems with video visits (Uscher-Pines et al., 2020). Video-based telemedicine was delivered via HIPAA-compliant platforms, including Zoom, FaceTime, Google Meet, Google Duo, GoToMeeting, Doximity, WebEx, Microsoft Team, RingCentral, and Uber Conference (Belcher et al., 2021, Lin et al., 2022, Polles et al., 2021); two articles cited platforms embedded in the electronic health record system (e.g., eClinicalWork; Lin et al., 2022; Uscher-Pines et al., 2020).
3.3. Screening and assessment
This section covers services related to routine screening for SUDs, as well as the use of specific assessments evaluating the nature and severity of use or specific symptoms. In a national survey of administrators and personnel from SUD treatment and recovery organizations, drug and alcohol screening was found to be the most common telephonically-delivered service, offered in 84.6% of the organizations (Molfenter et al., 2021). Common assessment instruments, such as the clinical opiate withdrawal scale (COWS, Wesson and Ling, 2003), were administered by providers during video conferences with patients (Castillo et al., 2020, Barney et al., 2020). Similar video-based assessments and diagnoses of SUD were conducted in a detention center remotely by physicians based at the University of Maryland (Belcher et al., 2021). Telephone (audio-only) assessment for patients who were unhoused was described in a case study (Levander et al., 2022). Virtual assessments could also include overall evaluations of substance use history, current status, episodes of cravings, stressors, and triggers (O’Gurek, 2021; Mehtani et al., 2021). According to Tolfighi and colleagues’ article, initial screening and assessment in a telemedicine visit could take between 30 and 45 min to complete (Tofighi et al., 2022). However, other articles included in this review did not provide details regarding the length of telemedicine-based screening and assessment.
3.4. Medication prescription
This section covers medications for SUD prescribed over telemedicine. Since guidance from the DEA and SAMHSA supporting telehealth-delivery of medication treatment for OUD with buprenorphine without in-person evaluation (Substance Abuse and Mental Health Services Administration, 2020), the practice of telehealth (both video and audio-only) for buprenorphine pharmacotherapy for new and existing patients has been widely adopted in various SUD treatment settings (Komaromy et al., 2021; Tofighi et al., 2022; Yeo et al., 2021). Sixteen of the 33 included articles described buprenorphine prescription, three articles mentioned naloxone prescription for overdose prevention (Harris et al., 2022, Jones et al., 2021; Wightman et al., 2021), and one article mentioned other medications including ondansetron, clonidine, hydroxyzine, and loperamide for OUD (Mehtani et al., 2021). For example, in a harm-reduction-focused primary care clinic in New York, 56% of the patients had initiated buprenorphine by phone or video between March and December 2020 (Dunham et al., 2021). In an online survey among 10,238 providers, 33% reported remote buprenorphine prescribing to new patients without an in-person examination (Jones et al., 2021). The number of days of medication supply prescribed via telemedicine varied across studies from 7 to 30 days, depending on clinical judgment of patients’ risk (Duncan et al., 2021, Nordeck et al., 2021; Uscher-Pines, 2020). In correctional systems, most new patients tended to be opioid-free for more than a week, so they often received electronically delivered prescriptions of buprenorphine at a starting dose of 4–8 mg (Belcher et al., 2021). The same article commented that methadone was not prescribed in the correctional system because it can only be dispensed through federally regulated opioid treatment programs (Belcher et al., 2021). The predictors of remote prescribing included previous experiences with remote prescribing and closure of the practice setting because of the shutdowns mandated during the COVID pandemic (Jones et al., 2021). Reasons for not offering remote prescribing included providers’ preference to see patients in person and treatment sites remaining physically open (Jones et al., 2021).
3.5. Induction
This section describes strategies of initiating buprenorphine for OUD treatment via telemedicine that were described in the reviewed articles. To mitigate buprenorphine diversion by patients in a detention setting, clinicians employed video-based telemedicine to observe medication dosing and water consumption (before and after dosing) (Belcher et al., 2021). In a youth outpatient substance use program, remote buprenorphine induction was planned only for adolescent and young adult patients who could enlist a loved one to provide support (Barney et al., 2020). Remote buprenorphine induction instructions were communicated via email and/or verbally during telemedicine visits (Clark et al., 2021; Tofighi et al., 2022; Wightman et al., 2021; Yeo et al., 2021). In some instances, patients were required to reiterate the remote induction instructions back to their providers to ensure that they understood the home-induction process (Mehtani et al., 2021). Medical students were mobilized in the induction process: they provided consultation regarding the logistics of buprenorphine induction, and then remained in frequent contact with patients early in treatment to monitor their medication efficacy and side effects (Castillo et al., 2020).
3.6. Behavioral therapy
This section summarizes the modality, frequency, length, and satisfaction with telemedicine-delivered behavioral treatment for SUDs. Telemedicine was considered to be an especially effective method to deliver behavioral treatments for SUDs and mental disorders due to its convenience and accessibility (Martin et al., 2021). Since federal- and state-level declarations of the public health emergency due to the COVID-19 pandemic, patients with SUD in some settings could choose from a menu of recommended individual and group therapies, at a higher frequency than what would be available in traditional outpatient care (Sugarman et al., 2021). In a survey of specialty addiction treatment providers in California, 67% and 63% of the providers reported an increase in the number of Medicaid patients who received telemedicine-delivered individual and group counseling, respectively (Henretty et al., 2021). A few papers reported anecdotal increases in patient attendance rates with telemedicine sessions (O'Gurek, 2021; Patton et al., 2021; Polles et al., 2021). Hughto and colleagues commented that telemedicine counseling was delivered with the same length and intensity as in-person counseling, thereby offering the potential to optimize treatment engagement (Hughto et al., 2021). Levels of satisfaction with behavioral therapies via telemedicine varied; for example, in a survey of patients with SUD, 90% of the respondents felt “very satisfied” with individual therapy, but only 58% felt the same about group therapies (Sugarman et al., 2021).
3.7. Follow-up for medication management
This section is a description of how telemedicine was used to follow up with patients. Patients were followed up by trained medical students, clinic coordinators, and outreach volunteers to tackle unanticipated clinical and administrative issues, especially after patients had received prescribed medication for OUD (Tofighi et al., 2022). In some settings, follow-up phone calls were also utilized to discuss and address patients’ comprehensive health needs, such as smoking cessation (Levander et al., 2022). One of the benefits of video-based follow-up visits was the ability to observe patients’ living and supporting environments (Uscher-Pines et al., 2020; Hunter et al., 2021; Patton et al., 2021). In a survey of 270 adult patients receiving outpatient SUD treatment, approximately half (48%) of patients with OUD preferred telemedicine-delivered medication management (Sugarman et al., 2021).
3.8. Monitoring
This section illustrates how remote patient monitoring was conducted during the COVID-19 pandemic to track patients’ treatment progress. Some SUD treatment sites reduced the frequency of UDS, administering UDS only when required by patients' health insurance and to minimize patients' risks of COVID-19 exposure (Tofighi et al., 2022; Yeo et al., 2021). Other clinics implemented alternatives to in-clinic UDS collection such as working with local laboratories or specialty pharmacies to collect urine samples (Hunter et al., 2021, Mehtani et al., 2021, Uscher-Pines et al., 2020). In-home testing was also implemented by mailing testing supplies to patients and having specimen (e.g., saliva) collection verified by video records (Polles et al., 2021). Descriptions of video-based urine sample collection processes are scant in the literature, with Brett’s article being an exception: pre-assembled UDS kits were sent to patients, and, during the virtual appointment, patients were instructed to place the mobile device to capture the profile view of patients’ urinating, as opposed to the frontal view. A phone holder was provided to the patient to make the process easier. To ensure patients’ privacy, providers monitored video-based UDS sample collection in a lockable private room with no access to their cellphones during the session. After the sample collection, patients shipped back the specimen to the laboratory using pre-printed shipping labels (Brett et al., 2021). Other innovative strategies, such as breath, hair, nail, and blood testing, emerged as techniques to monitor substance use in a virtual environment (Polles et al., 2021).
3.9. Recovery support
The transition of recovery services from in-person to virtual is covered in this section. During the first year of the pandemic, there were reports of reduced access to peer support resources, such as Narcotics Anonymous meetings (Uscher-Pines et al., 2020), which later became available virtually (Polles et al., 2021). For instance, a volunteer-facilitated in-person recovery program that existed pre-COVID-19, SMART Recovery, quickly transitioned to a telephone-based recovery line in the Spring of 2020 (Liese and Monley, 2021); however, because the services were delivered without video, the facilitators had to receive additional training in rapport building during an audio contact, and administration of recovery tools without physically or virtually presenting diagrams, handouts, and worksheets (Liese et al., 2021). A retrospective chart review in an urban community health center revealed that the telehealth peer recovery services were underutilized due to personal technology restrictions, perception of reduced impact, and no physical presence of the recovery coach and peers (Rahman et al., 2021).
3.10. Other services
Beyond the aforementioned cascade of care examples, service providers proactively utilized telehealth formats to ensure the patients’ comprehensive service needs were met. For example, a harm reduction-focused primary care clinic in New York utilized its telemedicine program to facilitate linkage to hepatitis C treatment and medication adherence monitoring (Dunham et al., 2021). In a low-threshold buprenorphine program in Baltimore, an additional phone line was established for patients to contact the clinical team to discuss issues such as lack of insurance and food/housing insecurity, which would be followed up and addressed by the outreach team (Nordeck et al., 2021). Similarly, a "bridge" clinic in California also worked with pharmacists to assist under-insured patients to enroll in health plans to provide access to psychiatric medications for patients receiving care in safety net programs (Mehtani et al., 2021).
3.11. Acceptability, challenges, solutions, and lessons learned
Many of the articles spoke to the feasibility and acceptability of telemedicine-delivered services from both patients’ and providers’ perspectives. Patients noted several positive benefits of telemedicine, including increased access and convenience, flexibility to visit doctors outside of business hours, lessened travel-related costs and anxiety, and reduced waiting time (Uscher-Pines et al., 2020). Providers also appreciated the flexibility, broader access, ease of use, and various innovative features available on telemedicine platforms (e.g., breakout sessions, whiteboard, ability to share screens and videos) (Sugarman et al., 2021, Martin et al., 2021, Molfenter et al., 2021). In addition, video-based visits enabled providers to observe patients’ home environments and family dynamics (Uscher-Pines et al., 2020; Sugarman et al., 2021). Clinicians perceived patients as feeling more at ease at home, which increased patients’ comfort level discussing their conditions and thus improved therapeutic alliance (Sugarman et al., 2021). Nonetheless, some patients still preferred the traditional in-person clinic so that they would have the opportunity to interact with other clinical team members and peers (Harris et al., 2022). Approximately one-fifth of providers waivered by the DEA to prescribe buprenorphine stated a preference to see patients in person, which was cited as one of the deterring factors of virtual buprenorphine prescription (Jones et al., 2021).
The most prominent challenges to telemedicine service provision discussed in these articles were insufficient computer literacy, limited access to devices, and technical challenges (Belcher et al., 2021; Uscher-Pines et al., 2020; Lin et al., 2020; McKiever et al., 2020). Government-subsidized phones offered limited data plans and some phone models were not compatible with telemedicine applications (Lin et al., 2021). Creative strategies were employed to overcome these barriers, such as partnering with local pharmacies to lend telephones to patients to access telemedicine (Nordeck et al., 2021), applying for grant funding and soliciting donations to cover the program costs (Pagano et al., 2021), mobilizing medical students to assist with the phone setups, disseminating pamphlets, and organizing Zoom webinars to guide phone use (Dunham et al., 2021). Patients’ complex social needs, such as unstable housing, having no private and quiet space, and lack of health insurance coverage were also frequently cited as barriers (Hser et al., 2021, Hughto et al., 2021, Patton et al., 2021; Tofighi et al., 2022; McKiever et al., 2020). In some instances, providers offered assistance with enrollment in insurances plans or with safety-net drug-pricing programs to obtain discounts on the medications (Castillo et al., 2020, Mehtani et al., 2021).
Provider capacity also limited telemedicine implementation, especially during the early months of the pandemic when there was an increase in patient flow while some clinic staff were furloughed (Harris et al., 2022, Hser et al., 2021). Providers reported confusion about new clinical procedures and workflows, concerns about telemedicine’s negative impact on service quality due to the challenges of engaging patients in a virtual environment, and questions about their liability and heightened risks of methadone diversion (Hser et al., 2021, Hughto et al., 2021). These concerns impacted providers’ willingness to intake new patients by telemedicine, and their perceived sustainability of the service delivery modality (Caton et al., 2021, Hunter et al., 2021, Molfenter et al., 2021). Providers were also facing difficulties and compromised productivity due to “Zoom fatigue,” which resulted from not only the increased volume of video visits but also longer staff time to coordinate and the increased need for technical support to prepare the virtual sessions than in-person visits (Hunter et al., 2021).
At the system level, interviews with directors of residential SUD treatment programs in California revealed financial challenges of telemedicine programs due to reduced reimbursement associated with patient no-shows or abbreviated virtual visit appointments (Pagano et al., 2021). Providers were paid less for working from home (Caton et al., 2021). Some of the clinic settings had difficulties securing private rooms to provide telemedicine services (Hser et al., 2021, Pagano et al., 2021). Additional challenges compromising the utility of telemedicine for arranging treatment medication occurred when electronic prescriptions reached local pharmacies that lacked medication supplies (Castillo et al., 2020, Tofighi et al., 2022). In some cases, naloxone had to be prescribed as a precautionary measure to counter potential opioid overdose because buprenorphine was not available in the local pharmacy (Levander et al., 2022).
4. Discussion
Innovative technology and telemedicine-based service delivery models are crucial to ensure access to treatment and care for patients with SUD (de Vargas et al., 2021, Li and Zhao, 2021). In this review, we described telemedicine utilization across the steps of the SUD cascade of care in the U.S. during the COVID-19 pandemic. An array of providers, including DEA-waivered buprenorphine prescribers, counselors, case managers, and medical students, has contributed to the adaptation of delivery of clinical procedures via telemedicine. As a result, telemedicine for SUD care has been widely implemented in various types of settings, including primary care, specialty care, outpatient/residential, emergency departments, and correctional systems. The feasibility of medication prescription and induction without in-person visits using either video or audio-only platforms has been demonstrated in real-world descriptions in the reviewed articles, which included similar reports of successful telemedicine-based delivery of individual counseling and group counseling for patients with SUDs. Furthermore, the literature suggests telemedicine’s pivotal role in bridging patients to comprehensive services for SUD care and treatment of comorbidities during COVID-19, including perinatal care (Dunham et al., 2021, McKiever et al., 2020).
In spite of these telemedicine advancements noted above, challenges reported in the literature indicate needs for improvement. Prominent issues included providers’ concerns about their liability, patients’ adherence to medication and program requirements, perceived risks of medication diversion, and difficulties engaging patients in a virtual environment. To address these issues, improved training curricula are needed for healthcare professionals in telemedicine-based evaluation, prescription, counseling, monitoring, and referral (Drake et al., 2020). The concept of "tele-expertise" has emerged to mitigate the impact of the pandemic on the healthcare system for SUD providers to provide distant care for patients with SUD (López-Pelayo et al., 2020). In the tele-expertise framework (Delaigue et al., 2018), in-service training is needed to ensure telemedicine-based SUD care services are delivered in a clinically appropriate manner. Areas needing additional training include clinical guidance in online counseling, facilitating group meetings via remote conferencing, utilization of in-person/virtual hybrid approaches in various clinical scenarios, and engagement with family members in support of patients’ treatment-seeking (Kedia et al., 2021, Martin et al., 2021).
The literature review found that telemedicine-based UDS was less commonly used during the COVID pandemic, as most treatment settings either reduced the frequency of UDS or referred patients to local laboratories to perform the test. Standard operating procedures to guide providers in virtual UDS collection, which could include video-based biological sample collection processes (when observation is necessary), and privacy protection measures described in Brett and colleagues’ article (Brett et al., 2021), could be developed and more widely implemented within telemedicine-based SUD treatment programs. The American Society of Addiction Medicine (ASAM) published an adjusted drug testing protocol that suggested clinicians carefully weigh the risks and benefits of drug testing and avoid ordering UDS tests if the results were not likely to change a patient’s management plan (ASAM, 2020). Alternative biological specimen testing strategies emerged to monitor substance use remotely, including saliva testing, fingerprints, and hair analysis (Kuwayama et al., 2016, Rotolo et al., 2021). A recently published telehealth for OUD toolkit also suggested the importance of other approaches to monitoring clinical progress, including clinical and functional assessment, remote pill counts via video, and collateral information from family and friends, to be used to supplement in-person and/or virtual point-of-care UDS (Providers Clinical Support System, 2021). These alternative monitoring approaches can also be considered in telemedicine programs, given their higher level of acceptability than directly observed urine sample collection during virtual visits.
Whether telemedicine increases or decreases the existing disparities in access, delivery, and outcomes of SUD care remains a concern in the field (Chan et al., 2022). Articles included in this review reported telemedicine being underutilized by racial and ethnic minorities, older patients, and those in poverty (Pagano et al., 2021; Sugarman et al., 2021), which was attributable to the lack of digital access and mistrust of the effectiveness of telemedicine (Hser et al., 2021). It is worth noting that two-thirds of the included papers described telemedicine services in coastal and metropolitan regions, and relatively fewer papers reported telemedicine services in rural areas. Rural communities suffer disproportionately from substance use and overdose rates due to shortages of local capacity to treat SUD and long distances to obtain in-person care (Rural Health Information Hub, 2020; Hser et al., 2021). Telemedicine has reduced these barriers and demonstrated its usefulness in addressing rural SUD-related disparities (Hirko et al., 2020). Multipronged efforts are needed to enhance patients’ access to and utility of telemedicine, including expanding broadband coverage, promoting access and connectivity of government-subsidized internet/telephone services for low-income families (e.g., Lifeline Programs), providing step-by-step written or audible instructions for patients who are uncomfortable with mobile technology digital support, and overcoming patient mistrust of technology (Ramsetty and Adams, 2020; Lin et al., 2021).
Many authors of the articles in our literature review advocated for the extension and promotion of the relaxed telemedicine policies to allow telemedicine-delivered treatment access to continue beyond the COVID-19 pandemic (Belcher et al., 2021, Castillo et al., 2020, Hughto et al., 2021, Mehtani et al., 2021). In addition, policy amendments to support audio-only services were recommended since it was a widely used strategy to ensure treatment access for patients without proper devices and internet connectivity (Clark et al., 2021). However, researchers argued that relaxation of the Ryan Haight requirements of in-person medical evaluation before prescription of controlled medication (U.S. Department of Justise, 2008), when done without additional incentives and support for utilization of telemedicine, may not have resulted in a widespread increase in telemedicine-delivered SUD treatment because providers had varying comfort levels adopting this new delivery model (Huskamp et al., 2022). Patients also were hesitant due to technical challenges and lack of private locations (McKiever et al., 2020). There were also concerns that the relaxation of the in-person visit requirement may have increased buprenorphine diversion (Barsky et al., 2022). Rigorously designed evaluation of the pandemic-precipitated policy adaptations on service quality, equity in access, patient outcomes, and adverse events are warranted to inform the refinement and implementation of telemedicine policies and regulations (Caton et al., 2021; Levander et al., 2022). Future telemedicine policymaking should also be locally tailored by taking into account geographic factors, epidemiological profiles, local service capacity, and patients’ needs and preferences (Jones et al., 2021, Molfenter et al., 2021).
There are several limitations of this literature review. We are aware that many clinic settings may have implemented telemedicine services for patients with SUD during the COVID-19 pandemic but did not report their practice changes or outcomes in peer-reviewed journals during this short period of time, and such publication bias can result in a lack of comprehensiveness of data and even misleading conclusions. In addition, our search was limited to articles published until March 2022. Given the rapid evolution of technology and policy/regulation, some of the most recent telemedicine implementations that happened in the field may not have been included in the review. It is worth noting that the studies covered by this preliminary review were primarily descriptive and exploratory. Without rigorous study designs, findings around the feasibility, acceptability, and effectiveness of telemedicine-delivered SUD services cannot be empirically confirmed and cannot be generalizable to other areas and patient groups.
In conclusion, the COVID-19 pandemic has propelled the advancement of telemedicine service delivery along the cascade of SUD treatment and care. These responses to the COVID-19 crisis, and their impacts on healthcare delivery, are likely to be maintained to some degree after the pandemic is over. Researchers should seize this unprecedented opportunity to evaluate the quality and impact of telemedicine-delivered SUD care and build the knowledge base to inform future policies and practices. Expanded access to the internet and digital devices, comprehensive services to provide stable housing and health insurance for those in need, and provider training in all aspects of telemedicine-based service delivery are necessary to ensure telemedicine services for SUD are equitably and effectively delivered. ( Table 2).
Table 2.
Summary of included studies describing telemedicine for SUD cascade of care during COVID.
| Article | Article type | Location | Setting | Design | Provider | Patient | Cascade step (s) | Main findings |
|---|---|---|---|---|---|---|---|---|
| Barsky et al. (2022) | Research letter | Nationwide | Multiple settings | Cross-sectional design of claims data | Induction | Rapid increase of telemedicine in response to COVID | ||
| Belcher et al. (2021) | Brief report | Maryland | Rural detention center | Description | Detention center's intensive outpatient treatment psychiatrists, referral to buprenorphine providers | Detainees (n = 7) | Screening/assessment, prescription, induction, referral | Successful implementation of telemedicine for OUD in a rural detention center |
| Brett et al. (2021) | Research article | Vermont | Laboratory centered on care for SUD | Description | New (n = 56) and returning (n = 81) patients on telemedicine | Monitoring | Description of a patient-centered approach to collect urine collection via telehealth | |
| Castillo et al. (2020) | Research article | Florida | Syringe service program housed within an academic medical center | Description | Medical students | Screening/assessment, prescription, and induction | Feasibility of student-run telehealth program | |
| Caton et al. (2021) | Research article | California | Primary care clinics (n = 57) | Survey | Clinicians (n = 338) | Screening/assessment, prescription, individual counseling | Increased telehealth visits for established patients; hesitancies to establish care with new patients by telemedicine | |
| Clark et al. (2021) | Commentary | Rhode Island | Unclear | Description | Induction, prescription and referral | Description of a 24/7 telephone hotline as a "tele-bridge" clinic for OUD treatment during COVID | ||
| Dunham et al. (2021) | Short report | New York | Primary care for harm-reduction | Description | Prescription, HCV treatment | Transition to telemedicine in a harm reduction-focused primary care clinic | ||
| Harris et al. (2022) | Short communication | Maryland | Street-based mobile clinic | Description | Providers/case managers (n = 4) | 150 patients | Prescription | Transition of buprenorphine services to telemedicine of a mobile clinic during COVID |
| Henretty et al. (2021) | Short report | California | Multiple settings | Survey | Specialty addiction treatment providers (n = 133) | Individual/group counseling, monitoring | Addiction specialists' reports of telemedicine utility during COVID | |
| Hughto et al. (2021) | Commentary | Rhode Island | Outpatient Substance use and mental health treatment program | Description | Individual counseling | Telemedicine improved access to counseling, with challenges to be tackled | ||
| Hser et al. (2021) | Commentary | Three states | Seven rural primary care clinics | Description | Clinic champion, coordinator, an outside telemedicine vendor | Patients with OUD | Prescription, individual/group counseling, monitoring, referral | Challenges such as low rates of patient identification and referral, digital/internet issues, workflow and capacity barriers, and insurance coverage highlighted the lack of empirical guidance for the best telemedicine practice |
| Hunter et al. (2021) | Research article | 13 States | Opioid treatment programs | Interview | Clinicians (n = 20) | Group counseling, monitoring | Clinicians reported benefits (flexibility) and concerns (increased risk of diversion and overdose) of telemedicine | |
| Huskamp et al. (2022) | Research article | Nationwide | Multiple settings | Survey | Clinicians who treat OUD (n = 602) | Prescription | Varying levels of telemedicine for medication initiation suggested additional support for clinicians | |
| Jones et al. (2021) | Research article | Nationwide | Multiple settings | Survey | Waivered prescribers (n = 10,238) | Prescription, induction, individual/group counseling | Multilevel factors associated with remote prescription buprenorphine among waivered clinicians | |
| Komaromy et al. (2021) | Commentary | Massachusetts | Grayken Center for Addiction at Boston Medical Center | Description | Prescription, medication management, monitoring, referral | Transition of an addiction treatment program to telemedicine with high levels of acceptability and retention | ||
| Levandar et al. (2022) | Research article | Oregon | Bridge clinic working with syringe exchange and harm reduction | Case study | Patients with OUD (n = 3) | Screening/assessment, prescription, medication management, other services (smoking cessation) | Three patient cases to demonstrate the possibility of buprenorphine initiation without in-person assessment of vulnerable patients. | |
| Liese and Monley (2021) | Commentary | Kansas | Community recovery program | Description | Recovery and referral to community services | Description of an in-person recovery program transitioning to virtual and lessons learned | ||
| Lin et al. (2022) | Research article | California | SUD treatment sites (n = 16) | Focus groups | SUD providers (n = 61) | Medication management, individual counseling, screen/assessment | Telemedicine services provided in SUD treatment settings and the challenges | |
| Martin et al. (2021) | Research article | Rhode Island | Behavioral healthcare | Survey | Counselors (n = 42) | Individual counseling | Counselors reported positive and negative valences of telemedicine counseling | |
| McKiever et al. (2020) | Research letter | Ohio | Maternal and addiction specialists co-located in an office-based outpatient program | Description | Pregnant women with OUD | Group counseling | Implementation of telemedicine-delivered integrated care for pregnant women with OUD | |
| Mehtani et al. (2021) | Research article | California | Telehealth Addiction treatment program created under a bridge clinic providing service for COVID-19 quarantine sites | Description | Screening/assessment, prescription, induction, individual counseling, monitoring, and assistance with insurance | Demonstrated feasibility of telephone-based management of OUD among marginalized patients | ||
| Molfenter et al. (2021) | Research article | 43 states | 457 organizations treating SUD, 58.6% specialty care | Survey | Screening/assessment, medication management, recovery services | Report of organizational-level telemedicine usage, acceptability, readiness, and sustainability | ||
| Nordeck et al. (2021) | Original article | Maryland | Low threshold buprenorphine program | Description | Medication management, individual counseling, and other services | The loosening of federal guidelines for buprenorphine prescribing, particularly via telehealth, is a viable opportunity to expand low-threshold and flexible care. | ||
| O'Gurek (2021) | Brief report | Pennsylvania | Primary care | Description | Individual counseling, treatment of comorbidities, referral, screen/assessment | Describe the development/implementation of a disaster-preparedness protocol incorporating telemedicine during the COVID-19 pandemic | ||
| Pagano et al. (2021) | Research article | California | Residential SUD treatment program (n = 20) | Interview | 17 Directors | Individual counseling | Challenges and drawbacks of telemedicine reported by directors of residential SUD treatment programs | |
| Patton et al. (2021) | Commentary | Massachusetts | Boston Medical Center | Description | Pregnant women who use substances | Medication management, individual counseling, integrated perinatal services, monitoring | Description of integrated substance use and prenatal care delivery utilizing telemedicine during the COVID-19 pandemic | |
| Polles et al. (2021) | Commentary | Florida | Physician health program supporting physicians suffering from SUD | Description | Group counseling, monitoring, recovery support group, and local hotline | Implementation of telemedicine services and alternative toxicology testing options | ||
| Rahman et al. (2021) | Original article | Massachusetts | Urban community health center affiliated with a larger hospital system | Retrospective chart review | Recovery meetings | Utilization and reasons for underutilizing telemedicine serviced in an urban community health center | ||
| Sugarman et al. (2021) | Original article | Massachusetts | Outpatient alcohol, drug, and addiction treatment program | Survey | Adult patients receiving SUD outpatient treatment (n = 270) | Medication management, individual/group counseling | Patients with OUD’s satisfaction with individual telemedicine visits and challenges with group therapy | |
| Tofighi et al. (2022) | Brief report | New York | NYC Health + Hospital and Bellevue Hospital | Description, EHR analysis | Prescription, medication management, individual counseling, referrals, screening/assessment, monitoring | Safety and feasibility of telemedicine-based opioid treatment with buprenorphine among a mostly underserved urban population. | ||
| Uscher-Pines et al. (2020) | Research article | 10 states | Multiple settings | Interview | Waived prescribers including (n = 18) | Prescription, recovery support groups | Buprenorphine prescribers' rapid transition to providing telemedicine in early 2020 and their concerns about quality and safety of telemedicine for OUD treatment | |
| Wightman et al. (2021) | Research article | Rhode Island | Emergency department collaborating with multiple settings | Retrospective cohort | Prescription, induction, referral to local resources, screening/assessment | Post-emergency department follow-up telephone call protocol is an opportunity to improve treatment engagement and access to buprenorphine for patients at risk of overdose | ||
| Yeo et al. (2021) | Case study | D.C | Community-based harm reduction program | Case study | Clinic coordinators, medical providers, community health workers, most with lived experiences | Prescription, induction, follow-up, monitoring, referral to relevant services, medication management | Low-threshold, audio-only telehealth model of MAT was successfully implemented during the COVID-19 pandemic and demonstrated satisfactory patient retention rates. |
Funding
The efforts of the authors were supported by the National Institute of Health - National Institute on Drug Abuse (UG1DA049435 and UG1DA040314) and National Institute of Mental Health (P30MH058107).
CRediT authorship contribution statement
The authors confirm their contribution to the paper as follows: Study conception and design: YIH, CL: Design of literature search strategy: LAL, SM, CIC, TRS, YL, Literature search and screening: CL, HP, YZ, SEC, Analysis and result presentation: CL, HP, YZ, SEC, Interpretation of results: LAL, SMM, CIC, TRS, YL, LJM, YIH, Manuscript preparation: CL, HP, YZ, SEC, YIH, All authors reviewed the results and approved the final version of the manuscript.
Declaration of Interest
Dr. Lewei (Allison) Lin has consulted on telehealth for substance use disorder treatment for Providers Clinical Support System with funding from the Substance Abuse and Mental Health Services Administration and for National Center for Quality Assurance with funding from Alkermes. Dr. Cynthia I. Campbell has received support managed through her institution from the Industry PMR Consortium, a consortium of companies working together to conduct post-marketing studies required by the Food and Drug Administration that assesses risks related to opioid analgesic use. Other authors declare no conflict of interests.
Acknowledgments
We would like to acknowledge the National Institute on Drug Abuse Clinical Trial Network Telemedicine Special Interest Group for their support of this literature review.
References
- Andraka-Christou B., Bouskill K., Haffajee R.L., Randall-Kosich O., Golan M., Totaram R., Gordon A.J., Stein B.D. Common themes in early state policy responses to substance use disorder treatment during COVID-19. Am. J. Drug Alcohol Abus. 2021;47(4):486–496. doi: 10.1080/00952990.2021.1903023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AnonU.S. Department of Justise. (2008). Implementation of the Ryan Haight Online Pharmacy Consumer Protection Act of 2008. 〈https://www.deadiversion.usdoj.gov/fed_regs/rules/2020/fr0930_2.htm〉. [PubMed]
- AnonNational Institute on Drug Abuse (January 25, 2019). Cascade of Care model recommended for opioid crisis. 〈https://nida.nih.gov/news-events/news-releases/2019/01/cascade-of-care-model-recommended-for-opioid-crisis〉.
- AnonAmerican Society of Addiction Medicine (ASAM). (September 18, 2020). Adjusting drug testing protocols. 〈https://www.asam.org/quality-care/clinical-recommendations/covid/adjusting-drug-testing-protocols〉.
- AnonRural Health Information Hub (December 9, 2020). Substance Use and Misuse in Rural Areas. 〈https://www.ruralhealthinfo.org/topics/substance-use〉.
- AnonU.S. Department of Justice and Drug Enforcement Administration. (2020). How to Prescribe Controlled Substances to Patients During the COVID-19 Public Health Emergency. 〈https://www.deadiversion.usdoj.gov/GDP/(DEA-DC-023)(DEA075)Decision_Tree_(Final)_33120_2007.pdf〉.
- AnonSubstance Abuse and Mental Health Services Administration (April 2020). FAQs: Provision of methadone and buprenorphine for the treatment of Opioid Use Disorder in the COVID-19 emergency. 〈https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf〉.
- AnonU.S. Department of Health & Human Services. (2021). COVID-19 Healthcare Delivery Impacts. 〈https://asprtracie.hhs.gov/technical-resources/resource/8658/covid-19-healthcare-delivery-impacts〉.
- AnonWorld Health Organization. (April 3, 2021). Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. 〈https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1〉.
- AnonNational Academy for State Health Policy. (August 15, 2021). States Provide Payment Parity for Telehealth and In-Person Care. 〈https://www.nashp.org/states-provide-payment-parity-for-telehealth-and-in-person-care/〉.
- AnonCenter for Disease Control and Prevention. (July 13, 2021). COVID-19 and People at Increased Risk. 〈https://www.cdc.gov/drugoverdose/resources/covid-drugs-QA.html〉.
- Barney A., Buckelew S., Mesheriakova V., Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J. Adolesc. Health.: Off. Publ. Soc. Adolesc. Med. 2020;67(2):164–171. doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky B.A., Busch A.B., Patel S.Y., Mehrotra A., Huskamp H.A. Use of Telemedicine for Buprenorphine Inductions in Patients With Commercial Insurance or Medicare Advantage. JAMA Netw. Open. 2022;5(1) doi: 10.1001/jamanetworkopen.2021.42531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batra K., Morgan A.E., Sharma M. COVID-19 and social isolation endangering psychological health of older adults: implications for telepsychiatry. J. Anaesth. Intensive Care Emerg. Med. 2020:1–6. doi: 10.22514/sv.2020.16.0070. [DOI] [Google Scholar]
- Belcher A.M., Coble K., Cole T.O., Welsh C.J., Whitney A., Weintraub E. Buprenorphine induction in a rural maryland detention center during COVID-19: implementation and preliminary outcomes of a novel telemedicine treatment program for incarcerated individuals with opioid use disorder. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.703685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett A., Foster H., Joseph M., Warrington J.S. Patient-Centered telehealth solution for observed urine collections in substance use disorder care delivery during COVID-19 and beyond. J. Patient Exp. 2021;8 doi: 10.1177/23743735211033128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch A.B., Sugarman D.E., Horvitz L.E., Greenfield S.F. Telemedicine for treating mental health and substance use disorders: reflections since the pandemic. Neuropsychopharmacol.: Off. Publ. Am. Coll. Neuropsychopharmacol. 2021;46(6):1068–1070. doi: 10.1038/s41386-021-00960-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castillo M., Conte B., Hinkes S., Mathew M., Na C.J., Norindr A., Serota D.P., Forrest D.W., Deshpande A.R., Bartholomew T.S., Tookes H.E. Implementation of a medical student-run telemedicine program for medications for opioid use disorder during the COVID-19 pandemic. Harm Reduct. J. 2020;17(1):88. doi: 10.1186/s12954-020-00438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caton L., Cheng H., Garneau H.C., Fisher T., Harris-Mills B., Hurley B., Newman S., McGovern M.P. COVID-19 adaptations in the care of patients with opioid use disorder: a survey of California primary care clinics. J. Gen. Intern. Med. 2021;36(4):998–1005. doi: 10.1007/s11606-020-06436-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan B., Bougatsos C., Priest K.C., McCarty D., Grusing S., Chou R. Opioid treatment programs, telemedicine and COVID-19: a scoping review. Subst. Abus. 2022;43(1):539–546. doi: 10.1080/08897077.2021.1967836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark S.A., Davis C., Wightman R.S., Wunsch C., Keeler L., Reddy N., Samuels E.A. Using telehealth to improve buprenorphine access during and after COVID-19: a rapid response initiative in Rhode Island. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2021.108283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaigue S., Bonnardot L., Steichen O., Garcia D.M., Venugopal R., Saint-Sauveur J.F., Wootton R. Seven years of telemedicine in Médecins Sans Frontières demonstrate that offering direct specialist expertise in the frontline brings clinical and educational value. J. Glob. Health. 2018;8(2) doi: 10.7189/jogh.08.020414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake C., Yu J., Lurie N., Kraemer K., Polsky D., Chaiyachati K.H. Policies to improve substance use disorder treatment with telehealth during the COVID-19 pandemic and beyond. J. Addict. Med. 2020;14(5):e139–e141. doi: 10.1097/ADM.0000000000000727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan A., Sanders N., Schiff M., Winkelman T. Adaptations to jail-based buprenorphine treatment during the COVID-19 pandemic. J. Subst. Abus. Treat. 2021;121 doi: 10.1016/j.jsat.2020.108161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunham K., Giardina M., Kolod B., McBratney E., Medina Blanco P., Riazi F., Tineo-Komatsu K., Toribio W., Wang L., Woods E., Weiss J. Transitioning clinical care for people who use drugs to telemedicine: lessons learned one year into the COVID-19 pandemic. Telemed. J. e-Health.: Off. J. Am. Telemed. Assoc. 2021;27(8):929–933. doi: 10.1089/tmj.2021.0130. [DOI] [PubMed] [Google Scholar]
- Harris R., Rosecrans A., Zoltick M., Willman C., Saxton R., Cotterell M., Bell J., Blackwell I., Page K.R. Utilizing telemedicine during COVID-19 pandemic for a low-threshold, street-based buprenorphine program. Drug Alcohol Depend. 2022;230 doi: 10.1016/j.drugalcdep.2021.109187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henretty K., Padwa H., Treiman K., Gilbert M., Mark T.L. Impact of the coronavirus pandemic on substance use disorder treatment: findings from a survey of specialty providers in California. Subst. Abus.: Res. Treat. 2021;15 doi: 10.1177/11782218211028655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirko K.A., Kerver J.M., Ford S., Szafranski C., Beckett J., Kitchen C., Wendling A.L. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J. Am. Med. Inform. Assoc.: JAMIA. 2020;27(11):1816–1818. doi: 10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser Y.I., Ober A.J., Dopp A.R., Lin C., Osterhage K.P., Clingan S.E., Mooney L.J., Curtis M.E., Marsch L.A., McLeman B., Hichborn E., Lester L.S., Baldwin L.M., Liu Y., Jacobs P., Saxon A.J. Is telemedicine the answer to rural expansion of medication treatment for opioid use disorder? Early experiences in the feasibility study phase of a national drug abuse treatment clinical trials network trial. Addict. Sci. Clin. Pract. 2021;16(1):24. doi: 10.1186/s13722-021-00233-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes P.M., Verrastro G., Fusco C.W., Wilson C.G., Ostrach B. An examination of telehealth policy impacts on initial rural opioid use disorder treatment patterns during the COVID-19 pandemic. J. Rural Health: Off. J. Am. Rural Health Assoc. Natl. Rural Health Care Assoc. 2021;37(3):467–472. doi: 10.1111/jrh.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughto J., Peterson L., Perry N.S., Donoyan A., Mimiaga M.J., Nelson K.M., Pantalone D.W. The provision of counseling to patients receiving medications for opioid use disorder: telehealth innovations and challenges in the age of COVID-19. J. Subst. Abus. Treat. 2021;120 doi: 10.1016/j.jsat.2020.108163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter S.B., Dopp A.R., Ober A.J., Uscher-Pines L. Clinician perspectives on methadone service delivery and the use of telemedicine during the COVID-19 pandemic: a qualitative study. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2021.108288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huskamp H.A., Riedel L., Uscher-Pines L., Busch A.B., Barnett M.L., Raja P., Mehrotra A. Initiating opioid use disorder medication via telemedicine during COVID-19: implications for proposed reforms to the ryan haight act. J. Gen. Intern. Med. 2022;37(1):162–167. doi: 10.1007/s11606-021-07174-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C.M., Diallo M.M., Vythilingam M., Schier J.G., Eisenstat M., Compton W.M. Characteristics and correlates of U.S. clinicians prescribing buprenorphine for opioid use disorder treatment using expanded authorities during the COVID-19 pandemic. Drug Alcohol Depend. 2021;225 doi: 10.1016/j.drugalcdep.2021.108783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedia S.K., Schmidt M., Dillon P.J., Arshad H., Yu X. Substance use treatment in Appalachian Tennessee amid COVID-19: challenges and preparing for the future. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2020.108270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komaromy M., Tomanovich M., Taylor J.L., Ruiz-Mercado G., Kimmel S.D., Bagley S.M., Saia K.M., Costello E., Park T.W., LaBelle C., Weinstein Z., Walley A.Y. Adaptation of a system of treatment for substance use disorders during the COVID-19 pandemic. J. Addict. Med. 2021;15(6):448–451. doi: 10.1097/ADM.0000000000000791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N., Janmohamed K., Nyhan K., Martins S.S., Cerda M., Hasin D., Scott J., Sarpong Frimpong A., Pates R., Ghandour L.A., Wazaify M., Khoshnood K. Substance, use in relation to COVID-19: a scoping review. Addict. Behav. 2022;127 doi: 10.1016/j.addbeh.2021.107213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuwayama K., Miyaguchi H., Yamamuro T., Tsujikawa K., Kanamori T., Iwata Y.T., Inoue H. Effectiveness of saliva and fingerprints as alternative specimens to urine and blood in forensic drug testing. Drug Test. Anal. 2016;8(7):644–651. doi: 10.1002/dta.1831. [DOI] [PubMed] [Google Scholar]
- Leahy L.G., Caverly S.E. COVID-19: changing the landscape of substance use. J. Am. Psychiatr. Nurses Assoc. 2022;28(1):5–8. doi: 10.1177/10783903211059532. [DOI] [PubMed] [Google Scholar]
- Levander X.A., Wheelock H., Pope J., Lee A., Hartmann K., Abuelkhair S., Gregg J.L., Buchheit B.M. Low-threshold buprenorphine via community partnerships and telemedicine-case reports of expanding access to addiction treatment during COVID-19. J. Addict. Med. 2022;16(1):e56–e58. doi: 10.1097/ADM.0000000000000811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Zhao M. Maintaining treatment and prevention programs for opioid use disorders during the coronavirus disease 2019 pandemic. Curr. Opin. Psychiatry. 2021;34(4):369–375. doi: 10.1097/YCO.0000000000000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liese B.S., Monley C.M. Providing addiction services during a pandemic: lessons learned from COVID-19. J. Subst. Abus. Treat. 2021;120 doi: 10.1016/j.jsat.2020.108156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C., Clingan S.E., Cousins S.J., Valdez J., Mooney L.J., Hser Y.I. The impact of COVID-19 on substance use disorder treatment in California: service providers' perspectives. J. Subst. Abus. Treat. 2022;133 doi: 10.1016/j.jsat.2021.108544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.A., Fernandez A.C., Bonar E.E. Telehealth for substance-using populations in the age of coronavirus disease 2019: recommendations to enhance adoption. JAMA Psychiatry. 2020;77(12):1209–1210. doi: 10.1001/jamapsychiatry.2020.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Pelayo H., Aubin H.J., Drummond C., Dom G., Pascual F., Rehm J., Saitz R., Scafato E., Gual A. "The post-COVID era": challenges in the treatment of substance use disorder (SUD) after the pandemic. BMC Med. 2020;18(1):241. doi: 10.1186/s12916-020-01693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin R., Kang A.W., DeBritz A.A., Walton M.R., Hoadley A., DelaCuesta C., Hurley L. Medication for opioid use disorder service provision and telephone counseling: a concurrent mixed-methods approach. Int. J. Environ. Res. Public Health. 2021;18(11):6163. doi: 10.3390/ijerph18116163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKiever M.E., Cleary E.M., Schmauder T., Talley A., Hinely K.A., Costantine M.M., Rood K.M. Unintended consequences of the transition to telehealth for pregnancies complicated by opioid use disorder during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. 2020;223(5):770–772. doi: 10.1016/j.ajog.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehtani N.J., Ristau J.T., Snyder H., Surlyn C., Eveland J., Smith-Bernardin S., Knight K.R. COVID-19: a catalyst for change in telehealth service delivery for opioid use disorder management. Subst. Abus. 2021;42(2):205–212. doi: 10.1080/08897077.2021.1890676. [DOI] [PubMed] [Google Scholar]
- Molfenter T., Roget N., Chaple M., Behlman S., Cody O., Hartzler B., Johnson E., Nichols M., Stilen P., Becker S. Use of telehealth in substance use disorder services during and after COVID-19: online survey study. JMIR Ment. Health. 2021;8(2) doi: 10.2196/25835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordeck C.D., Buresh M., Krawczyk N., Fingerhood M., Agus D. Adapting a low-threshold buprenorphine program for vulnerable populations during the COVID-19 pandemic. J. Addict. Med. 2021;15(5):364–369. doi: 10.1097/ADM.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oesterle T.S., Kolla B., Risma C.J., Breitinger S.A., Rakocevic D.B., Loukianova L.L., Hall-Flavin D.K., Gentry M.T., Rummans T.A., Chauhan M., Gold M.S. Substance use disorders and telehealth in the COVID-19 pandemic era: a new outlook. Mayo Clin. Proc. 2020;95(12):2709–2718. doi: 10.1016/j.mayocp.2020.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Gurek D.T. Designing and evaluating COVID-19 protocols for an office-based opioid treatment program in an urban underserved setting. J. Am. Board Fam. Med.: JABFM. 2021;34(Suppl):S136–S140. doi: 10.3122/jabfm.2021.S1.200207. [DOI] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F., von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-a web and mobile app for. Syst. Rev. Syst. Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano A., Hosakote S., Kapiteni K., Straus E.R., Wong J., Guydish J.R. Impacts of COVID-19 on residential treatment programs for substance use disorder. J. Subst. Abus. Treat. 2021;123 doi: 10.1016/j.jsat.2020.108255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal, N., Garfield, R., Cox, C., & Artiga, S. (August 12, 2021). Substance Use Issues Are Worsening Alongside Access to Care. 〈https://www.kff.org/policy-watch/substance-use-issues-are-worsening-alongside-access-to-care/〉.
- Patton E.W., Saia K., Stein M.D. Integrated substance use and prenatal care delivery in the era of COVID-19. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2020.108273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pessar S.C., Boustead A., Ge Y., Smart R., Pacula R.L. Assessment of state and federal health policies for opioid use disorder treatment during the COVID-19 pandemic and beyond. JAMA Health Forum. 2021;2(11) doi: 10.1001/jamahealthforum.2021.3833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinals D.A., Hepburn B., Parks J., Stephenson A.H. The behavioral health system and its response to COVID-19: a snapshot perspective. Psychiatr. Serv. (Wash., D. C.) 2020;71(10):1070–1074. doi: 10.1176/appi.ps.202000264. [DOI] [PubMed] [Google Scholar]
- Polles A., Bundy C., Jacobs W., Merlo L.J. Adaptations to substance use disorder monitoring by physician health programs in response to COVID-19. J. Subst. Abus. Treat. 2021;125 doi: 10.1016/j.jsat.2021.108281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Providers Clinical Support System. (October 2021). Telehealth for Opioid Use Disorder Toolkit: Guidance to Support High-Quality Care. https://pcssnow.org/wp-content/uploads/2021/10/OUD-Toolkit_FINAL_10.2021.pdf.
- Rahman F., Evans N., Bernhardt J. Access to OUD treatment and maintenance of sobriety amid the COVID-19 pandemic. Subst. Use Misuse. 2021;56(7):1005–1009. doi: 10.1080/10826084.2021.1901935. [DOI] [PubMed] [Google Scholar]
- Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J. Am. Med. Inform. Assoc.: JAMIA. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotolo M.C., Pacifici R., Pellegrini M., Cardullo S., Pérez L., Cuppone D., Gallimberti L., Madeo G. Hair testing for classic drugs of abuse to monitor cocaine use disorder in patients following transcranial magnetic stimulation protocol treatment. Biology. 2021;10(5):403. doi: 10.3390/biology10050403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Socías M.E., Volkow N., Wood E. Adopting the 'cascade of care' framework: an opportunity to close the implementation gap in addiction care? Addict. (Abingdon, Engl.) 2016;111(12):2079–2081. doi: 10.1111/add.13479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman D.E., Busch A.B., McHugh R.K., Bogunovic O.J., Trinh C.D., Weiss R.D., Greenfield S.F. Patients' perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID-19 pandemic. Am. J. Addict. 2021;30(5):445–452. doi: 10.1111/ajad.13207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi B., McNeely J., Walzer D., Fansiwala K., Demner A., Chaudhury C.S., Subudhi I., Schatz D., Reed T., Krawczyk N. A telemedicine buprenorphine clinic to serve new york city: initial evaluation of the NYC public hospital system's initiative to expand treatment access during the COVID-19 pandemic. J. Addict. Med. 2022;16(1):e40–e43. doi: 10.1097/ADM.0000000000000809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A., Flemming K., McInnes E., Oliver S., Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med. Res. Methodol. 2012;12:181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uscher-Pines L., Martineau M. Rand Corperation; Santa Monica, CA: 2021. Telehealth After COVID-19: Clarifying Policy Goals for a Way Forward.〈https://www.rand.org/pubs/perspectives/PEA1089-1.html〉 [Google Scholar]
- Uscher-Pines L., Sousa J., Raja P., Mehrotra A., Barnett M., Huskamp H.A. Treatment of opioid use disorder during COVID-19: Experiences of clinicians transitioning to telemedicine. J. Subst. Abus. Treat. 2020;118 doi: 10.1016/j.jsat.2020.108124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vargas D., Pereira C.F., Volpato R.J., Lima A., da Silva Ferreira R., de Oliveira S.R., Aguilar T.F. Strategies adopted by addiction facilities during the coronavirus pandemic to support treatment for individuals in recovery or struggling with a substance use disorder: a scoping Review. Int. J. Environ. Res. Public Health. 2021;18(22):12094. doi: 10.3390/ijerph182212094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L., Weiss J., Ryan E.B., Waldman J., Rubin S., Griffin J.L. Telemedicine increases access to buprenorphine initiation during the COVID-19 pandemic. J. Subst. Abus. Treat. 2021;124 doi: 10.1016/j.jsat.2020.108272. https://doi.org/10.101F6/j.jsat.2020.108272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesson D.R., Ling W. The clinical opiate withdrawal scale (COWS) J. Psychoact. Drugs. 2003;35(2):253–259. doi: 10.1080/02791072.2003.10400007. [DOI] [PubMed] [Google Scholar]
- Wightman R.S., Jacka B., Uber J., McKenzie M., Reddy N.G., Winters R., Jordison Keeler L.A., Samuels E.A. Tele-buprenorphine for emergency department overdose visit follow up and treatment initiation. Am. J. Emerg. Med. 2021;50:409–412. doi: 10.1016/j.ajem.2021.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams A.R., Nunes E.V., Bisaga A., Levin F.R., Olfson M. Development of a Cascade of care for responding to the opioid epidemic. Am. J. Drug Alcohol Abus. 2019;45(1):1–10. doi: 10.1080/00952990.2018.1546862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo E.J., Kralles H., Sternberg D., McCullough D., Nadanasabesan A., Mayo R., Akselrod H., Catalanotti J. Implementing a low-threshold audio-only telehealth model for medication-assisted treatment of opioid use disorder at a community-based non-profit organization in Washington, D.C. Harm Reduct. J. 2021;18(1):127. doi: 10.1186/s12954-021-00578-1. [DOI] [PMC free article] [PubMed] [Google Scholar]