Abstract
Background
Wasting is perhaps one of the signs of malnutrition that has been linked to the deaths of children suffering from malnutrition. As a result, understanding its correlations and drivers is critical. Using quantile regression analysis, this research aims to contribute to the discussion on under-5 malnutrition by analyzing the predictors of wasting in Bangladesh.
Methods and materials
The dataset was extracted from the 2017–18 Bangladesh demographic and health survey (BDHS) data. The weight-for-height (WHZ) z-score based anthropometric indicator was used in the study as the target variable. The weighted sample constitutes 8,334 children of under-5 years. However, after cleaning the missing values, the analysis is based on 8,321 children. Sequential quantile regression was used for finding the contributing factors.
Results
The findings of this study depict that the prevalence of wasting in children is about 8 percent and only approximately one percent of children are severely wasted in Bangladesh. Age, mother’s BMI, and parental educational qualification, are all major factors of the WHZ score of a child. The coefficient of the female child increased from 0.1 to 0.2 quantiles before dropping to 0.75 quantile. For a child aged up to three years, the coefficients have a declining tendency up to the 0.5 quantile, then an increasing trend. Children who come from the richest households had 16.3%, 3.6%, and 15.7% higher WHZ scores respectively than children come from the poorest households suggesting that the risk of severe wasting in children under the age of five was lower in children from the wealthiest families than in children from the poorest families. The long-term malnutrition indicator (wasting) will be influenced by the presence of various childhood infections and vaccinations. Furthermore, a family’s economic position is a key determinant in influencing a child’s WHZ score.
Conclusions
It is concluded that socioeconomic characteristics are correlated with the wasting status of a child. Maternal characteristics also played an important role to reduce the burden of malnutrition. Thus, maternal nutritional awareness might reduce the risk of malnutrition in children. Moreover, the findings disclose that to enrich the nutritional status of children along with achieving Sustainable Development Goal (SDG)-3 by 2030, a collaborative approach should necessarily be taken by the government of Bangladesh, and non-governmental organizations (NGOs) at the community level in Bangladesh.
Introduction
Childhood undernutrition has long-term consequences such as reduced attainment of schooling, lessened economic potential, and chronic illness in adulthood. It is more common in underdeveloped nations and is linked to child fatalities. Therefore, as we move forward with the Sustainable Development Goals (SDGs), we should promote and maintain nutritional wellbeing. Malnutrition is acting as a leading cause of death among under-5 children, as well as one of the most widespread causes of deterioration in children’s health and well-being, resulting in impaired learnability, incompetence, and inefficiency to acquire skills [1]. Childhood malnutrition is a major contributor to the global burden of illness and a primary cause of mortality and morbidity observed among under-5 children in poor and middle-income countries like Bangladesh [2–4]. Moreover, nutritional deficiencies raise the likelihood of death from frequent infections, the prevalence of infections, and may cause infection recovery to be prolonged [4–6].
Among the indicators of malnutrition, wasting is one of the signs of malnutrition that has been linked to the deaths of children suffering from malnutrition [7, 8]. Wasting decreased overall across low-and middle-income countries (LMICs) between 2000 and 2017, from 8.4% to 6.4%, however, it is still above the World Health Organization’s Global Nutrition Target of less than 5% [9]. A previous study mentioned that the prevalence of wasting is 15.49% in district Rahimyar Khan, Pakistan [10] and the probability of child malnutrition was lower among the children of mothers who had high mothers’ nutritional and health awareness [11]. In 2020, more than 45 million of under-5 children were influenced by wasting, among them 13.6 million children have been severely wasted. However, these figures are impacted by COVID-19 and because of degradation in household wealth and interruptions in the availability and cost of nutritious food as well as vital nutrition services, it is anticipated that 1.15 times more children will be impacted by wasting in 2020 than previously estimated [12].
The nutritional status of a country’s children is a barometer of its socio-economic development. Poor nutritional status, on the other hand, is one of Bangladesh’s most profound health as well as welfare issues. Bangladesh has made strenuous efforts to minimize child malnutrition and has had some results. According to BDHS2017-18 reports, the level of wasting decreased by about half of the previous years [13]. Several studies have found a link between childhood malnutrition and a variety of factors such as an individual’s socioeconomic status, demographic features, environmental factors, household factors, parental attributes, child-feeding habits, child morbidity, vitamin intake and vaccination coverage, geographic location, and residency [14–29].
Previous studies, on the other hand, have largely looked at the predictors using multiple linear regression or logistic regression models. However, at different points, the mean effect may overestimate or underestimate the contribution of the covariates. Another notable drawback of logistic regression models is that they assess observations that are below or above a cut-off point equally, ignoring the magnitude of deviations from that threshold level. As a result, statistical information that could be useful for intervention along with health promotion initiatives could be lost. However, the quantile regression (QR) model has the benefit that it is robust in the preference of outliers [30]. Previous studies highlighted that mean and variance are affected by outliers and proposed mean and variance in the presence of outliers [31, 32]. In addition, the QR model yielded more unbiased estimates for skewed data than the linear regression model [33]. Previous studies applied the QR model for exploring the contributing factor of the age of the mother at first birth and age at first marriage because of its non-normality nature [34–36]. Moreover, several researchers applied the QR model to examine the core socio-demographic factors of child nutritional status [37–41]. A prior study used a simultaneous quantile regression model to identify significant risk factors for severe stunting in children under the age of five [42]. Researchers also explored the risk factors linked with malnutrition among under-5 children using the multilevel, spatial-temporal model, and geostatistical analysis [43–46].
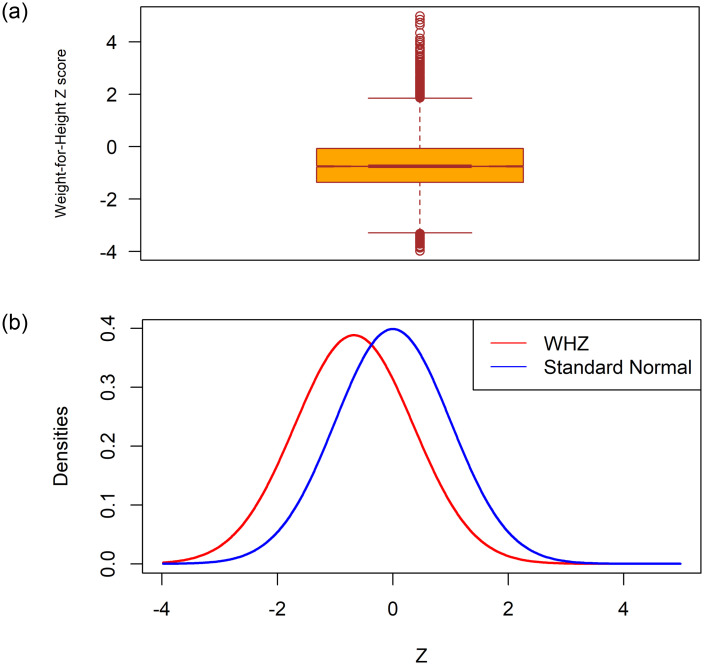
The authors are well known about the three different dimensions used indicators of nutritional status of under-5 children. Stunting measures chronic nutritional deficiency, wasting is a measure of acute nutritional deficiency, and underweight is a composite measure of both acute and chronic statuses. According to a prior study, there are 45.4 million wasted children under the age of five [47, 48]. Despite the fact that the global prevalence of wasting has gradually decreased, however, only more than a quarter of 194 countries are on track to meet the World Health Assembly’s (WHA) 2025 target of keeping the prevalence of wasting under 5.0 percent [48, 49]. It has the greatest short-term case fatality rate of any form of malnutrition [50, 51]. There’s also evidence that wasting can be a ’harbinger of stunting,’ with episodes of wasting impairing linear growth [52]. Hence, the skewness coefficient, and the Boxplot of the WHZ-scores investigated in this study, shown in Fig 1, demonstrate the existence of outliers and their distribution does not fully match the normal distribution. Moreover, the authors do not find any study on wasted children based on BDHS-2017/18 data considering QR regression. These reasons are working behind for using the QR model to explore the contributing predictors of wasting among children aged less than 5 years in Bangladesh considering the most recent BDHS-2017-18 data.
Fig 1. Box and density plot of the weight-for-height (WHZ) Z-scores with the standard normal variate.
Methods and materials
Data and variables
In this study, the secondary data is obtained from a nationally representative survey called the 2017–18 Bangladesh Demographic and Health Survey (BDHS-2017/18). The BDHS-2017-18 is the complete survey that covers the enumeration areas (EAs) of the entire country. This survey used stratified sampling and selection is made in two stages. Firstly, 675 EAs were chosen with probability proportional to the size of the EA. In the second phase of selection, 30 households per cluster were carefully chosen with a systematic procedure from the list of households. However, due to natural disasters, data were not collected from 3 EAs. These three clusters were in Rajshahi (one rural cluster), Rangpur (one rural cluster), and Dhaka (one urban cluster). The full data set is accessible via the following link http://dhsprogram.com/data/available-datasets.cfm. Before starting the analysis the authors use a weighted sample to make sure the country representative sample. The details of the sampling procedure and methods of the weighted sample (mathematically adjusted) are available in the published report of BDHS-2017/18 in detail [13]. The weight-for-height Z-score (WHZ) is the target variable, and several child characteristics such as sex, age, duration of breastfeeding, birth order; maternal attributes such as age, maternal educational qualification and BMI; father’s education, and attributes related to the child’s health are the explanatory variables in this study.
A child is termed wasted if his or her weight-to-height ratio is more than two standard deviations below the reference population’s median weight-to-height ratio. This situation indicates an acute nutritional deficiency. This study considers the Z-score of weight-for-height as the target variable. In this paper, the WHZ score is used as the outcome and several characteristics of a child such as sex, age, birth order, breastfeeding length; mother’s attributes like age, educational qualification and BMI; factors related to household, and child’s health are considered as covariates in this paper. The choice of covariates used in this study was influenced by the availability in the BDHS dataset, self-efficacy as well as guided by existing relevant literature.
Quantile regression
The quantile regression (QR) model was initially introduced by Koenker and Basset in 1978, and nowadays it is extensively applied in various research areas, particularly in Statistics, Econometrics, and health sciences [34, 36, 42, 53–55]. Suppose, Y be a random (response) variable having cumulative distribution function (CDF) FY (y), i.e. FY (y) = P(Y ≤ y) and X is the p-dimensional vector of predictor variables. Then the τth (quantile level) conditional quantile of Y is described as
where τ varies from 0 to 1. A detailed description of the QR model is presented in S1 Appendix.
We conducted quantile regression for various quantiles (0.1, 0.20, 0.25, 0.5, 0.75 and 0.90) as motivated the literature available in literature. However, in order to determine the importance of performing multiple quantile regressions, we consider the following hypothesis.H0:
H0: all of the estimated coefficients for all quantiles are equal versus
H1: all of the estimated coefficients for all quantiles are not equal.
Ethics approval
This study was based on an analysis of existing public domain survey data sets that are freely available online with all identifier information removed. The survey was approved by the Ethics Committee of the ICF Macro at Calverton in the USA and by the Ethics Committee in Bangladesh.
Results
Firstly, we examine the summary statistics of our main target variable i.e., the Z-scores weight-for-height and the findings of WHZ are mean: -0.67, SD: 1.03, skewness: 0.60, and kurtosis: 1.36.
The mean of the WHZ-scores is less than 0 (i.e., a negative mean value for wasting), which indicates that the index’s distribution has switched downward and that the majority, if not all, of the children in the population, are malnourished in comparison to the reference group. The coefficient of skewness of the Z-scores depicts that the distribution of the WHZ-scores is slightly positively skewed and fully unmatched with standard normal density and the boxplot presented in Fig 1 revealed that outliers are present in the dataset. Table 1 illustrates the prevalence of wasting among children of under-5 years of age according to selected socio-demographic characteristics. The findings depict that the prevalence of wasting (WHZ-score < -2 SD) in children is about 8 percent and only approximately one percent of children are severely wasted (WHZ-score < -3 SD) in Bangladesh.
Table 1. Percent distribution of child malnutrition according to wasting by background characteristics.
| Background characteristics | Percent | Weight-for-Height (Wasted) in % | p-value of Chi-square | ||
|---|---|---|---|---|---|
| Z-score <-3 SD | Z-score <-2 SD | ||||
| Child’s sex | Male | 52.16 | 0.82 | 7.96 | 0.020 |
| Female | 47.84 | 0.45 | 6.68 | ||
| Age of the child | ≤6 months | 13.14 | 0.38 | 1.82 | <0.001 |
| 7 months-12 months | 9.94 | 0.50 | 4.08 | ||
| 13–24 months | 18.45 | 1.20 | 12.02 | ||
| 25–36 months | 19.87 | 0.97 | 8.06 | ||
| 37–48 months | 19.16 | 0.54 | 7.65 | ||
| 49–59 months | 19.44 | 0.20 | 7.39 | ||
| Birth order | 1st | 38.31 | 0.60 | 7.34 | 0.137 |
| 2nd-3rd | 49.22 | 0.54 | 7.35 | ||
| 4th or higher | 12.46 | 1.13 | 7.16 | ||
| Duration of breastfeeding | Never breastfeed | 41.28 | 0.34 | 7.42 | <0.001 |
| < = 12 months | 2.05 | 0.61 | 7.93 | ||
| 13 or more | 6.97 | 0.95 | 6.27 | ||
| Still breastfeeding | 49.70 | 0.85 | 7.40 | ||
| Mother’s age | Up to 18 years | 7.23 | 1.73 | 9.67 | 0.008 |
| 19–24 | 40.24 | 0.44 | 6.86 | ||
| 25–34 | 44.68 | 0.51 | 7.40 | ||
| 35+ | 7.86 | 1.17 | 7.05 | ||
| Mother’s BMI | Underweight (<18.5) | 13.60 | 1.00 | 12.68 | <0.001 |
| Normal (18.5–24.9) | 59.21 | 0.67 | 6.94 | ||
| Overweight (> = 25) | 27.18 | 0.34 | 5.41 | ||
| Mother’s Education level | No Education | 7.15 | 1.06 | 9.73 | 0.056 |
| Primary | 28.40 | 0.88 | 7.74 | ||
| Secondary and above | 64.45 | 0.47 | 6.89 | ||
| Father’s Education level | No Education | 14.85 | 0.61 | 8.74 | 0.002 |
| Primary | 34.29 | 0.75 | 7.31 | ||
| Secondary and above | 50.86 | 0.48 | 6.90 | ||
| Type of place of residence | Rural | 73.04 | 0.60 | 7.38 | 0.020 |
| Urban | 26.96 | 0.72 | 7.24 | ||
| Religion | Muslim | 91.96 | 0.65 | 7.43 | 0.291 |
| Non-Muslim | 8.04 | 0.62 | 6.46 | ||
| Place of delivery | With Health Facility | 49.91 | 0.58 | 6.55 | 0.153 |
| Respondent’s Home | 50.09 | 1.02 | 7.88 | ||
| Number of ANC visits | None | 13.13 | 0.82 | 7.04 | 0.005 |
| 1–3 | 44.66 | 0.86 | 7.54 | ||
| 4–7 | 16.18 | 0.76 | 6.91 | ||
| 8 or more | 6.03 | 1.09 | 8.70 | ||
| Had diarrhea recently | No | 95.26 | 0.65 | 7.22 | 0.159 |
| Yes | 4.74 | 0.27 | 9.55 | ||
| Had fever in last two weeks | No | 66.79 | 0.54 | 6.24 | <0.001 |
| Yes | 33.21 | 0.83 | 9.48 | ||
| Had cough in last two weeks | No | 64.01 | 0.56 | 6.80 | 0.049 |
| Yes | 35.99 | 0.76 | 8.28 | ||
| Received BCG | No | 6.92 | 0.61 | 2.75 | <0.001 |
| Yes | 93.08 | 0.83 | 7.58 | ||
| Received Vitamin A | No | 30.04 | 0.61 | 5.04 | <0.001 |
| Yes | 69.96 | 0.88 | 8.19 | ||
| Wealth index | Poorest | 21.44 | 0.87 | 8.44 | <0.001 |
| Poorer | 20.33 | 0.43 | 7.38 | ||
| Middle | 18.86 | 0.93 | 7.15 | ||
| Richer | 19.88 | 0.51 | 7.92 | ||
| Richest | 19.48 | 0.41 | 5.54 | ||
| Total | 0.64 | 7.98 | |||
Table 1 shows that, in comparison to their male counterparts, female children are slightly less wasted. After the age of two years, the prevalence of wasting reduced, indicating an inverse link between age and the prevalence of wasting. Duration of breastfeeding of child portrayed a positive relationship with the index of wasting. The prevalence of wasting is more frequent among children whose mother’s age is less than 18 years compared to others. The prevalence of wasting, a symptom of child malnutrition, is adversely connected to the mother’s nutritional status as evaluated by BMI and parental educational qualification, as the prevalence of wasting reduced as the mother’s nutrition and parental education levels increased. Results show that non-Muslim children are wasted than their counterparts. Vaccination status and the status of suffering from childhood diseases are also vital in deciding the wasted level of children in Bangladesh. However, in some cases, we observed unexpected results. Moreover, the place of delivery has an impact on a child’s nutritional intake like whether they are wasted or not. A child delivered in a health facility has a decreased risk of wasting than a child born at home. A kid’s nutritional state is linked to his or her current health status, as a child with diarrhea and fever is more likely to be wasted than a healthy child. Furthermore, the wealth index has significantly positively linked to the wasted level of a child in Bangladesh [Table 1].
The authors test the hypothesis of the equality of coefficients of covariates of Q10 and Q20. It is clear that the p-value of this hypotheses is less than 0.001. As a result, at the 0.1 percent level of significance, the test substantially rejects equality of the estimated coefficients for the quantiles. Now, it can be said that the quintiles with bigger difference will be surely significant. This suggests that in this study, multiple quantile regression approaches are appropriate.
Weight-for-height is thought to be a good short-term indicator of a child’s nutritional and health status. Table 2 shows that the WHZ-score at the upper edge of the condition distribution (i.e. after the 50th quantile) is not significant at the 5% significance level, and the score is about half points less in the 90th quantile than the 10th quantile among female child. Results depict that age of the child is also highly significantly associated with the WHZ score at different quantiles. At different quantiles, the child’s age was significantly related to the WHZ score. The WHZ-score increases considerably at all quantiles, i.e. 10th, 20th, 25th, 50th, 75th, and 90th quantiles, as the mother’s BMI improves. Moreover, parental educational status is a significant factor in WHZ score. The results show that current residence has a significant influence on the child’s WHZ score at the 10th, 50th, and 75th quantiles, but the coefficient is significant at the 20th, 25th, and 90th quantiles. The vaccination and status of suffering from childhood diseases are the contributing factors for determining the level of wasting. Moreover, families economic condition is an indispensable factor in determining the WHZ score of a child [Table 2].
Table 2. Results of quantile regression analysis for WHZ score for under-5 Bangladeshi children.
| Characteristics | Labels | Q10 | Q20 | Q25 | Q50 | Q75 | Q90 |
|---|---|---|---|---|---|---|---|
| Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | ||
| Child’s sex | Male (Ref.) | ||||||
| Female | 0.07* (-0.016,0.156) | 0.099** (0.026,0.172) | 0.074* (0.001,0.146) | 0.037* (-0.011,0.085) | 0.022 (-0.052,0.095) | 0.046 (-0.068,0.16) | |
| Age of the child | < = 6 months (Ref.) | ||||||
| 7–12 months | -0.062 (-0.376,0.251) | -0.289* (-0.645,0.068) | -0.251* (-0.596,0.095) | -0.272** (-0.486,-0.059) | -0.101* (-0.308,0.107) | 0.234* (-0.155,0.623) | |
| 13–24 months | -0.506*** (-0.844,-0.168) | -0.71*** (-1.006,-0.414) | -0.701*** (-0.992,-0.41) | -0.733*** (-0.917,-0.549) | -0.51*** (-0.741,-0.279) | -0.177* (-0.5,0.146) | |
| 25–36 months | -0.44** (-0.767,-0.113) | -0.699*** (-1.013,-0.385) | -0.706*** (-1.009,-0.404) | -0.807*** (-1.008,-0.606) | -0.708*** (-0.924,-0.492) | -0.492** (-0.878,-0.105) | |
| 37–48 months | 0.35* (0.025,0.676) | 0.14 (-0.246,0.527) | 0.306* (-0.073,0.685) | 0.226* (-0.032,0.484) | 0.231* (-0.047,0.508) | 0.2* (-0.235,0.636) | |
| 49–59 months | -0.35* (-0.833,0.132) | -0.14* (-0.551,0.27) | -0.306** (-0.565,-0.047) | -0.226* (-0.437,-0.015) | -0.231** (-0.448,-0.014) | -0.2** (-0.474,0.074) | |
| Birth order | 1st (Ref.) | ||||||
| 2nd-3rd | -0.007 (-0.105,0.092) | 0.032* (-0.035,0.099) | -0.02 (-0.083,0.042) | -0.075* (-0.158,0.007) | -0.111** (-0.196,-0.026) | -0.152* (-0.334,0.029) | |
| 4th and higher | 0.037* (-0.174,0.248) | 0.046 (-0.099,0.192) | -0.041 (-0.175,0.093) | -0.145** (-0.265,-0.026) | -0.226** (-0.378,-0.074) | -0.244** (-0.475,-0.012) | |
| Duration of breastfeeding | Never breastfeed (Ref.) | ||||||
| < = 12 months | -0.027 (-0.956,0.903) | 0.031 (-0.877,0.939) | -0.001 (-0.895,0.893) | 0.135 (-0.816,1.085) | -0.178 (-1.509,1.101) | 0.081 (-98.846,99.008) | |
| 13 or more | -0.103 (-1.06,0.854) | 0.03* (-0.87,0.931) | -0.036* (-0.855,0.783) | -0.162* (-1.18,0.857) | -0.414* (-1.673,0.797) | -0.457* (-99.429,98.514) | |
| Still breastfeeding | -0.234* (-1.182,0.715) | -0.084 (-0.997,0.829) | -0.101 (-0.931,0.729) | -0.097 (-1.109,0.915) | -0.281 (-1.494,0.933) | -0.272 (-99.191,98.646) | |
| Religion | Muslim (Ref.) | ||||||
| Non-Muslim | 0.011 (-0.121,0.144) | 0.052 (-0.099,0.202) | 0.049 (-0.095,0.193) | -0.01 (-0.146,0.127) | -0.055 (-0.236,0.126) | -0.092 (-0.299,0.115) | |
| Mother’s age | Up to 18 years (Ref.) | ||||||
| 19–24 | 0.193* (-0.039,0.425) | 0.086** (-0.036,0.208) | 0.067* (-0.054,0.189) | 0.02 (-0.069,0.109) | 0.036 (-0.187,0.259) | 0.008 (-0.242,0.258) | |
| 25–34 | 0.142* (-0.07,0.354) | -0.012 (-0.128,0.104) | -0.018 (-0.146,0.111) | 0.029* (-0.089,0.146) | 0.035* (-0.211,0.28) | -0.026* (-0.323,0.27) | |
| 35+ | 0.09 (-0.273,0.453) | -0.117* (-0.36,0.126) | -0.06* (-0.273,0.153) | -0.031* (-0.205,0.142) | -0.069** (-0.342,0.205) | 0.254** (-0.315,0.823) | |
| Mother’s Education level | No Education (Ref.) | ||||||
| Primary | -0.054* (-0.259,0.151) | 0.004 (-0.221,0.228) | 0.03 (-0.195,0.256) | 0.051 (-0.13,0.232) | 0.098* (-0.075,0.272) | 0.272*** (-0.044,0.589) | |
| Secondary and above | -0.006 (-0.192,0.18) | 0.04* (-0.156,0.237) | 0.069* (-0.132,0.269) | 0.118** (-0.027,0.264) | 0.064* (-0.106,0.234) | 0.262** (-0.026,0.55) | |
| Mother’s BMI | Underweight (<18.5) (Ref.) | ||||||
| Normal (18.5–24.9) | 0.206*** (0.052,0.36) | 0.305*** (0.186,0.425) | 0.309*** (0.191,0.426) | 0.292*** (0.194,0.391) | 0.33*** (0.197,0.463) | 0.398*** (0.187,0.609) | |
| Overweight (> = 25) | 0.327*** (0.18,0.473) | 0.417*** (0.304,0.53) | 0.425*** (0.307,0.542) | 0.386*** (0.267,0.504) | 0.596*** (0.439,0.754) | 0.612*** (0.331,0.893) | |
| Father’s Education level | No Education (Ref.) | ||||||
| Primary | 0.083 (-0.09,0.257) | -0.005 (-0.148,0.139) | -0.027 (-0.147,0.093) | -0.047 (-0.144,0.049) | -0.002 (-0.12,0.117) | -0.058 (-0.306,0.189) | |
| Secondary and above | 0.087* (-0.048,0.223) | 0.059* (-0.078,0.195) | 0.033 (-0.117,0.184) | -0.003 (-0.118,0.112) | 0.047* (-0.095,0.189) | 0.02 (-0.162,0.203) | |
| Type of place of residence | Rural (Ref.) | ||||||
| Urban | -0.077* (-0.172,0.018) | -0.018 (-0.123,0.086) | 0.012 (-0.093,0.116) | 0.049* (-0.035,0.133) | 0.083** (-0.057,0.224) | 0.01 (-0.155,0.175) | |
| Place of delivery | With Health Facility (Ref.) | ||||||
| Respondent’s Home | -0.003 (-0.099,0.094) | -0.001 (-0.127,0.124) | 0.008 (-0.108,0.125) | -0.004 (-0.086,0.078) | -0.08* (-0.174,0.014) | -0.061* (-0.211,0.089) | |
| Number of ANC visits | None (Ref.) | ||||||
| 1–3 | -0.111** (-0.225,0.003) | -0.032* (-0.159,0.094) | -0.047 (-0.175,0.081) | -0.04 (-0.166,0.087) | -0.095* (-0.244,0.055) | -0.21** (-0.398,-0.021) | |
| 4–7 | -0.127* (-0.293,0.04) | -0.016 (-0.14,0.108) | -0.048* (-0.173,0.077) | -0.033* (-0.148,0.083) | -0.099* (-0.252,0.054) | -0.208** (-0.419,0.003) | |
| 8 or more | -0.093 (-0.325,0.14) | 0.024* (-0.212,0.259) | 0.011* (-0.176,0.197) | -0.053* (-0.291,0.185) | -0.029 (-0.267,0.21) | 0.023 (-0.384,0.43) | |
| Had diarrhea recently | No (Ref.) | ||||||
| Yes | -0.027 (-0.151,0.097) | -0.06 (-0.219,0.099) | -0.016 (-0.165,0.134) | 0.012 (-0.118,0.142) | -0.055 (-0.246,0.135) | -0.035 (-0.225,0.155) | |
| Had fever in last two weeks | No (Ref.) | ||||||
| Yes | -0.226*** (-0.304,-0.147) | -0.207*** (-0.27,-0.144) | -0.209*** (-0.261,-0.156) | -0.212*** (-0.295,-0.129) | -0.21** (-0.349,-0.071) | -0.134** (-0.322,0.053) | |
| Had cough in last two weeks | No (Ref.) | ||||||
| Yes | -0.019 (-0.103,0.065) | 0.041 (-0.053,0.135) | 0.04* (-0.032,0.112) | 0.057* (-0.021,0.135) | 0.112* (-0.027,0.251) | 0.073 (-0.157,0.303) | |
| Received BCG | No (Ref.) | ||||||
| Yes | 0.027 (-0.169,0.224) | -0.091* (-0.253,0.07) | -0.062 (-0.263,0.138) | -0.138* (-0.333,0.056) | -0.273** (-0.504,-0.041) | -0.653** (-1.235,-0.07) | |
| Received Vitamin A | No (Ref.) | ||||||
| Yes | -0.155** (-0.292,-0.018) | -0.094** (-0.172,-0.016) | -0.107** (-0.191,-0.024) | -0.168*** (-0.284,-0.053) | -0.29*** (-0.397,-0.183) | -0.353*** (-0.523,-0.184) | |
| Wealth index | Poorest (Ref.) | ||||||
| Poorer | 0.132* (-0.008,0.272) | 0.073* (-0.054,0.201) | 0.048 (-0.081,0.176) | -0.067** (-0.181,0.047) | -0.055* (-0.194,0.084) | -0.041* (-0.194,0.113) | |
| Middle | 0.146* (-0.006,0.297) | 0.08* (-0.069,0.23) | 0.1** (-0.055,0.255) | 0.059* (-0.072,0.191) | -0.01 (-0.114,0.094) | 0.024 (-0.162,0.209) | |
| Richer | 0.111* (-0.096,0.319) | 0.038 (-0.08,0.157) | 0.065** (-0.043,0.172) | 0.066** (-0.066,0.197) | 0.029** (-0.112,0.169) | 0.16** (-0.055,0.375) | |
| Richest | 0.163** (0.009,0.317) | 0.036* (-0.097,0.168) | 0.021* (-0.133,0.174) | 0.027* (-0.137,0.191) | 0.09** (-0.164,0.344) | 0.157** (-0.11,0.425) | |
Notes: Ref.: Reference category;
*** refers p-value <0.001,
** refers p-value <0.05 and
* refers p-value <0.1.
The effect of age of a child is inversely connected to the quantile of WHZ score. The coefficient changes over the range of about 0.07 to approximately 0.046 for the quantile varies from 0.1 to 0.90 for the children whose age lies between 07–12 months compared to children of age less than 06 months. In the case of the birth order of a child, the influence on WHZ score initially increases, however, gradually decreases after the 20th quantile. Duration of breastfeeding also shows as an important determinant of wasting of a child and depicts a negative relationship on WHZ score. The age of the mother had a positive and statistically significant relationship with WHZ, however, in some quantile, it shows a negative association; children whose mothers’ age lies between 19–24 years age group had a greater WHZ than mothers’ who married in their early age (<18 years). The impact of the mother’s BMI on the conditional distribution of the WHZ score is statistically significant and fluctuated from quantile to quantile. As for the influence of parental education level, children whose parents had higher educational qualifications are taller than children whose parents are illiterate. Moreover, the findings of quantile regression reveal a positive correlation between household financial status and WHZ score. Children who come from the richest households had 0.163, 0.036, and 0.157 times higher WHZ scores respectively than children who come from the poorest households in the 10th, 20th, and 90th quantiles [Table 2].
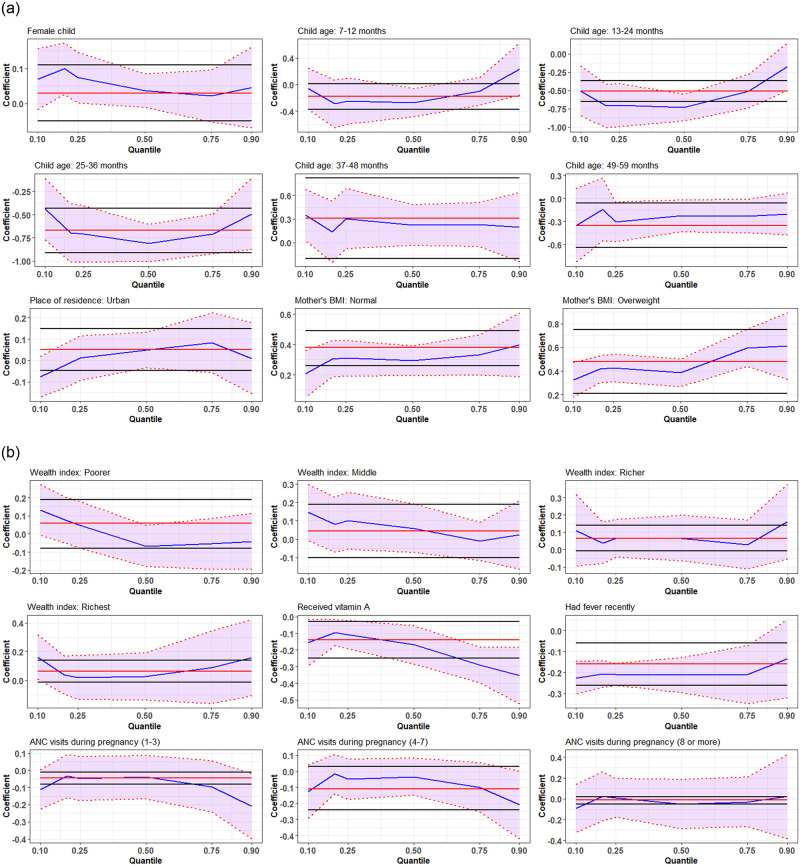
The coefficients of selected significant covariates obtained by using a simultaneous quantile regression model ranges 0.10 to 0.90 quantiles of WHZ are presented in Fig 2. The findings reveal that the coefficients vary across quantiles. For example, the coefficient of the female child increased from 0.1 quantile to 0.2 quantile, and then it declined up to 0.75 quantile. The coefficients have declined trend up to 0.5 quantile and thereafter an increasing trend is observed for a child aged up to 3 years. The impact of the mother’s BMI on WHZ was lower at the lower quantiles of WHZ, however, but higher at the upper tail, i.e., as the quantile increased the coefficient of the mother’s BMI is also increased. It is suggesting that children at the lower tail of the WHZ distribution are more likely to be severely wasted than those in the upper end of the distribution. Children from the richest families had a lower risk of under-five severe wasting than the children of the poorest families [Fig 2].
Fig 2. Plot of covariate effects on quantiles from multivariable simultaneous quantile regression (blue line) and their associated 95% confidence interval (purple shaded regions).
The solid red lines are the ordinary least square regression lines with their 95% confidence intervals (black lines).
Discussion
The nutritional status of a child included in the survey is compared to WHO Child Growth Standards, which are focused on a culturally, ethnically, genetically diverse, and internationally representative sample of healthy children living in optimum settings conducive for achieving a child’s full genetic growth potential. Wasting is considered as severe if the WHZ score of a child is more than 3 SD (standard deviation) below the reference median. Also, severe wasting is strongly connected to mortality risk. Bangladesh is doing a great job to lessen the burden of wasting over the two decades and a study projected that the prevalence of wasting will decrease by one-quarter by 2030 [56]. There were also significant differences in child nutritional status based on demographic and socio-economic factors. The findings of the quantile regression revealed that the relationship between socio-demographic variables and WHZ varied depending on the conditional WHZ distribution.
The age of a child was found to be strongly connected to wasting in children under the age of five, with the odds of wasting decreasing as the child’s age increased, which is consistent with previous research [56, 57]. This could be due to the fact that children are more vulnerable to infections throughout their first year of life [58, 59]. The duration of breastfeeding also shows as an important determinant of wasting of a child and depicts a negative relationship on WHZ score. Breastfeeding is protective against various childhood infectious diseases. The potential reason working behind is that breast milk is the sole natural and primary source of optimum sustenance for newborn babies’ physical and neurological growth, and cognitive development, it also boosts the child’s immune system at their early age [60–62]. As a result, it is critical to limit the risk of wasting by exclusively breastfeeding up to the first six months of a children’s life. The residential status shows a significant relation with WHZ score only at 10th and 20th quartiles in urban areas than rural areas. The environment, choices, employment conditions, social and family networks, access to health care and other services of urbanites differ greatly from those of rural dwellers [63].
Parental education has a significant influence on the level of malnutrition of under-5 children and our findings are consistent with previous studies [40, 42, 57]. The significance of parental education in mitigating the risk of wasting can be explained by enhancing knowledge and understanding about nutrition and health for their children, the possibility of better household income, and the responsibility in food selection decision-making. Moreover, education also offers an opportunity for acquiring protective childcare behaviors such as completing childhood vaccines, improving feeding and sanitation practices, and so on [40, 56, 64]. A study pointed out that higher educational attainment among mothers is effective at promoting women’s empowerment and participation in household decision-making, which has been ascertained to lessen malnutrition indices in Bangladesh [65]. To combat malnutrition, programmes for mothers’ nutritional education and awareness are essential [11]. Children who suffer from different infectious disease in their life has an impact on wasting. Moreover, the children who consumed vitamin-A and received BCG vaccination had a lower likelihood of wasting than their counterparts [66]. The findings of the quantile regression exhibited wealth index is statistically significant with the discrepancy in WHZ score. Researchers pointed out that wealthier households can manage to pay for better medical care and additional nutritious food as well as ensure a healthier living environment [40, 56]. The high prevalence of malnutrition is correlated with overall socio-economic deprivation [10].
Strengths and limitations of this study
The most recent dataset is used in this study and it is a nationally representative cross-sectional survey. This study used quantile regression in order to measure the determinants of malnutrition in Bangladesh. The results from this sample are not transferable to other populations with different characteristics, because socioeconomic factors were only assessed at the one-time point. Moreover, the application of multilevel quantile regression analysis would be a potential topic in a further study that will be helpful to improve the quality of the findings in a future study.
Conclusion
The effects of covariates included in this study such as a child’s age, birth order, parental educational status, and mother’s BMI, as well as the status of vaccination and suffering from childhood diseases on child nutrition at various points of the conditional distributions of WHZ-score, were investigated utilizing quantile regressions. Age, mother’s BMI, parental educational status, and income index are all major factors of a child’s Z score of weight-for-height. To accelerate the reduction of malnutrition or lessen the burden of malnourishment among children by 2030, the authors think that a combined effort should necessarily be taken by the government and public-private owner organizations at the community level. In addition to current programs aimed at improving child health, the government may desire to develop targeted nutrition remediation strategies in order to eliminate childhood malnutrition and prioritize the target group of the population. Furthermore, a healthy mother may give birth to healthy children which indicates the prevalence of undernutrition transfer generation to generation, thus, early intervention programs should not only target children but also their moms in order to improve children’s nutritional status. The authors would like to recommend that nutrition and health-related education should be integrated into the educational process in Bangladesh. The authors believe that the findings of this paper will assist policymakers in accelerating the achievement of the SDG-3 in Bangladesh.
Supporting information
(DOCX)
Acknowledgments
The authors are grateful to ICF International, Rockville, Maryland, USA, for providing the Bangladesh DHS data sets for this analysis. Authors are thankful to the academic editor and two reviewers for their valuable comments and suggestions that help to enhance the manuscript’s quality.
Data Availability
The access link of data set is http://dhsprogram.com/data/available-datasets.cfm.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.World Health Organization. Children: improving survival and well-being. 2020. https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality
- 2.Demissie S, Worku A. Magnitude and Factors Associated with Malnutrition in Children 6–59 Months of Age in Pastoral Community of Dollo Ado District, Somali Region, Ethiopia. Sci J Public Heal. 2013;1: 175–183. doi: 10.11648/J.SJPH.20130104.12 [DOI] [Google Scholar]
- 3.Pravana NK, Piryani S, Chaurasiya SP, Kawan R, Thapa RK, Shrestha S. Determinants of severe acute malnutrition among children under 5 years of age in Nepal: a community-based case–control study. BMJ Open. 2017;7: e017084. doi: 10.1136/bmjopen-2017-017084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black RE, Alderman H, Bhutta ZA, Gillespie S, Haddad L, Horton S, et al. Maternal and child nutrition: building momentum for impact. Lancet. 2013;382: 372–375. doi: 10.1016/S0140-6736(13)60988-5 [DOI] [PubMed] [Google Scholar]
- 5.Talbert A, Thuo N, Karisa J, Chesaro C, Ohuma E, Ignas J, et al. Diarrhoea Complicating Severe Acute Malnutrition in Kenyan Children: A Prospective Descriptive Study of Risk Factors and Outcome. PLoS One. 2012;7: e38321. doi: 10.1371/journal.pone.0038321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kliegman RM, Geme J St. Nelson Textbook of Pediatrics. 21st Editi. Elsevier Health Sciences; 2019. https://www.uk.elsevierhealth.com/nelson-textbook-of-pediatrics-9780323568890.html
- 7.Fotso JC, Kuate-Defo B. Household and community socioeconomic influences on early childhood malnutrition in Africa. J Biosoc Sci. 2006;38: 289–313. doi: 10.1017/S0021932005026143 [DOI] [PubMed] [Google Scholar]
- 8.Katona P, Katona-Apte J. The interaction between nutrition and infection. Clin Infect Dis. 2008;46: 1582–1588. doi: 10.1086/587658 [DOI] [PubMed] [Google Scholar]
- 9.LBD Double Burden of Malnutrition Collaborators. Mapping local patterns of childhood overweight and wasting in low- and middle-income countries between 2000 and 2017. Nat Med. 2020;26: 750–759. doi: 10.1038/s41591-020-0807-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shahid M, Ahmed F, Ameer W, Guo J, Raza S, Fatima S, et al. Prevalence of child malnutrition and household socioeconomic deprivation: A case study of marginalized district in Punjab, Pakistan. PLoS One. 2022;17: e0263470. doi: 10.1371/journal.pone.0263470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahid M, Cao Y, Ahmed F, Raza S, Guo J, Malik NI, et al. Does Mothers’ Awareness of Health and Nutrition Matter? A Case Study of Child Malnutrition in Marginalized Rural Community of Punjab, Pakistan. Front Public Heal. 2022;10: 101. doi: 10.3389/FPUBH.2022.792164/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.UNICEF, WHO, The World Bank. Levels and trends in child malnutrition: key findings of the 2021 edition of the joint child malnutrition estimates. 2021. https://www.who.int/publications/i/item/9789240025257
- 13.National Institute of Population Research and Training (NIPORT), ICF. Bangladesh Demographic and Health Survey 2017–18. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF; 2020. https://dhsprogram.com/pubs/pdf/FR344/FR344.pdf
- 14.Rabbani A, Khan A, Yusuf S, Adams A. Trends and determinants of inequities in childhood stunting in Bangladesh from 1996/7 to 2014. Int J Equity Health. 2016;15: 186. doi: 10.1186/s12939-016-0477-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biadgilign S, Shumetie A, Yesigat H. Does Economic Growth Reduce Childhood Undernutrition in Ethiopia? PLoS One. 2016;11: e0160050. doi: 10.1371/journal.pone.0160050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohsena M, Goto R, Mascie-Taylor N. Regional variation in maternal and childhood undernutrition in Bangladesh: evidence from demographic and health surveys. WHO South-East Asia J Public Heal. 2015;4: 139–149. Available: http://www.searo.who.int/ doi: 10.4103/2224-3151.206683 [DOI] [PubMed] [Google Scholar]
- 17.Rahman A, Chowdhury S, Karim A, Ahmed S. Factors associated with nutritional status of children in Bangladesh: A multivariate analysis. Demogr India. 2008;37: 95–109. [Google Scholar]
- 18.Rahman A, Chowdhury S. Determinants of chronic malnutrition among preschool children in Bangladesh. J Biosoc Sci. 2007;39: 161–173. doi: 10.1017/S0021932006001295 [DOI] [PubMed] [Google Scholar]
- 19.Rahman A, Hossain MM. Prevalence and determinants of fever, ARI and diarrhea among children aged 6–59 months in Bangladesh. BMC Pediatr. 2022;22: 117. doi: 10.1186/s12887-022-03166-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hossain MM, Sobhan MA, Rahman A, Flora SS, Irin ZS. Trends and determinants of vaccination among children aged 06–59 months in Bangladesh: country representative survey from 1993 to 2014. BMC Public Health. 2021;21: 1578. doi: 10.1186/s12889-021-11576-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hossain MM, Yeasmin S, Abdulla F, Rahman A. Rural-urban determinants of vitamin a deficiency among under 5 children in Bangladesh: Evidence from National Survey 2017–18. BMC Public Health. 2021;21: 1569. doi: 10.1186/s12889-021-11607-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Das S, Gulshan J. Different forms of malnutrition among under five children in Bangladesh: A cross sectional study on prevalence and determinants. BMC Nutr. 2017;3: 1. doi: 10.1186/s40795-016-0122-2 [DOI] [Google Scholar]
- 23.Ahsan KZ, Arifeen S El, Al-Mamun MA, Khan SH, Chakraborty N. Effects of individual, household and community characteristics on child nutritional status in the slums of urban Bangladesh. Arch Public Heal. 2017;75: 9. doi: 10.1186/s13690-017-0176-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chowdhury MH, Mim FN, Satu SA. Prevalence and Risk Factors of Child Malnutrition in Bangladesh. Res Rev J Stat Math Sci. 2018;4: 59–66. Available: https://www.rroij.com/open-access/prevalence-and-risk-factors-of-child-malnutrition-in-bangladesh.php?aid=87019 [Google Scholar]
- 25.Ntenda PAM, Chuang YC. Analysis of individual-level and community-level effects on childhood undernutrition in Malawi. Pediatr Neonatol. 2018;59: 380–389. doi: 10.1016/j.pedneo.2017.11.019 [DOI] [PubMed] [Google Scholar]
- 26.Mukabutera A, Thomson DR, Hedt-Gauthier BL, Basinga P, Nyirazinyoye L, Murray M. Risk factors associated with underweight status in children under five: an analysis of the 2010 Rwanda Demographic Health Survey (RDHS). BMC Nutr. 2016;2: 40. doi: 10.1186/S40795-016-0078-2 [DOI] [Google Scholar]
- 27.Manda J, Gardebroek C, Khonje MG, Alene AD, Mutenje M, Kassie M. Determinants of child nutritional status in the eastern province of Zambia: the role of improved maize varieties. Food Secur. 2015;8: 239–253. doi: 10.1007/S12571-015-0541-Y [DOI] [Google Scholar]
- 28.Vollmer S, Bommer C, Krishna A, Harttgen K, Subramanian S V. The association of parental education with childhood undernutrition in low- and middle-income countries: comparing the role of paternal and maternal education. Int J Epidemiol. 2017;46: 312–323. doi: 10.1093/ije/dyw133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akram R, Sultana M, Ali N, Sheikh N, Sarker AR. Prevalence and Determinants of Stunting Among Preschool Children and Its Urban–Rural Disparities in Bangladesh. Food Nutr Bull. 2018;39: 521–535. doi: 10.1177/0379572118794770 [DOI] [PubMed] [Google Scholar]
- 30.Yeh CC, Wang KM, Suen YB. Quantile analyzing the dynamic linkage between inflation uncertainty and inflation. Probl Perspect Manag. 2009;7: 21–28. [Google Scholar]
- 31.Hossain MM. Proposed Mean (Robust) in the Presence of Outlier. J Stat Appl Probab Lett. 2016;3: 103–107. doi: 10.18576/jsapl/030301 [DOI] [Google Scholar]
- 32.Hossain MM. Variance in the Presence of Outlier: Weighted Variance. J Stat Appl Probab Lett. 2017;4: 57–59. doi: 10.18576/jsapl/040203 [DOI] [Google Scholar]
- 33.Olsen CS, Clark AE, Thomas AM, Cook LJ. Comparing least-squares and quantile regression approaches to analyzing median hospital charges. Acad Emerg Med. 2012;19: 866–875. doi: 10.1111/j.1553-2712.2012.01388.x [DOI] [PubMed] [Google Scholar]
- 34.Hossain MM, Majumder AK. Determinants of the age of mother at first birth in Bangladesh: quantile regression approach. J Public Health (Bangkok). 2019;27: 419–424. doi: 10.1007/S10389-018-0977-6 [DOI] [Google Scholar]
- 35.Talukder A, Khan ZI, Khatun F, Tahmida S. Factors associated with age of mother at first birth in Albania: application of quantile regression model. Heliyon. 2021;7: E06547. doi: 10.1016/j.heliyon.2021.e06547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hossain S, Hossain MM, Yeasmin S, Bhuiyea MSH, Chowdhury PB, Khan MTF. Assessing the Determinants of Women’s Age at First Marriage in Rural and Urban Areas of Bangladesh: Insights From Quantile Regression (QR) Approaches. J Popul Soc Stud. 2022;30: 602–624. [Google Scholar]
- 37.Borooah VK. The height-for-age of Indian children. Econ Hum Biol. 2005;3: 45–65. doi: 10.1016/j.ehb.2004.12.001 [DOI] [PubMed] [Google Scholar]
- 38.Aturupane H, Deolalikar AB, Gunewardena D. Determinants of Child Weight and Height in Sri Lanka: A Quantile Regression Approach. In: McGillivray M, Dutta I, Lawson D, editors. Health Inequality and Development. Studies in Development Economics and Policy, Palgrave Macmillan, London; 2011. doi: 10.1057/9780230304673_4 [DOI] [Google Scholar]
- 39.Fenske N, Burns J, Hothorn T, Rehfuess EA. Understanding child stunting in India: A comprehensive analysis of socio-economic, nutritional and environmental determinants using additive quantile regression. PLoS One. 2013;8: e78692. doi: 10.1371/journal.pone.0078692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharaf MF, Mansour EI, Rashad AS. Child nutritional status in Egypt: a comprehensive analysis of socio-economic determinants using a quantile regression approach. J Biosoc Sci. 2019;51: 1–17. doi: 10.1017/S0021932017000633 [DOI] [PubMed] [Google Scholar]
- 41.Rahman FI, Ether SA, Islam MR. Upsurge of Dengue Prevalence During the Third Wave of COVID-19 Pandemic in Bangladesh: Pouring Gasoline to Fire. Clin Pathol. 2022;15. doi: 10.1177/2632010X221076068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aheto JMK. Simultaneous quantile regression and determinants of under-five severe chronic malnutrition in Ghana. BMC Public Health. 2020;20: 644. doi: 10.1186/s12889-020-08782-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aheto JMK, Alangea DO. Multilevel analysis of risk factors associated with severe underweight among children under 5 years: evidence from the 2014 Ghana Demographic and Health Survey. Heal Sci Investig J. 2021;2: 166–172. doi: 10.46829/HSIJOURNAL.2021.6.2.1.166-172 [DOI] [Google Scholar]
- 44.Aheto JMK, Dagne GA. Geostatistical analysis, web-based mapping, and environmental determinants of under-5 stunting: evidence from the 2014 Ghana Demographic and Health Survey. Lancet Planet Heal. 2021;5: e347–e355. doi: 10.1016/S2542-5196(21)00080-2 [DOI] [PubMed] [Google Scholar]
- 45.Aheto JMK, Keegan TJ, Taylor BM, Diggle PJ. Childhood Malnutrition and Its Determinants among Under-Five Children in Ghana. Paediatr Perinat Epidemiol. 2015;29: 552–561. doi: 10.1111/ppe.12222 [DOI] [PubMed] [Google Scholar]
- 46.Aheto JMK, Taylor BM, Keegan TJ, Diggle PJ. Modelling and forecasting spatio-temporal variation in the risk of chronic malnutrition among under-five children in Ghana. Spat Spatiotemporal Epidemiol. 2017;21: 37–46. doi: 10.1016/j.sste.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 47.WHO. Levels and trends in child malnutrition: UNICEF/WHO/The World Bank Group joint child malnutrition estimates: key findings of the 2019 edition. 2019. https://www.who.int/publications/i/item/WHO-NMH-NHD-19.20
- 48.Development Initiatives. 2021 Global Nutrition Report-The state of global nutrition. Bristol, UK; 2021. https://globalnutritionreport.org/reports/2021-global-nutrition-report/executive-summary/
- 49.Frison S, Angood C, Khara T, Bahwere P, Black RE, Briend A, et al. Prevention of child wasting: Results of a Child Health & Nutrition Research Initiative (CHNRI) prioritisation exercise. PLoS One. 2020;15: e0228151. doi: 10.1371/JOURNAL.PONE.0228151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hossain M, Chisti MJ, Hossain MI, Mahfuz M, Islam MM, Ahmed T. Efficacy of World Health Organization guideline in facility-based reduction of mortality in severely malnourished children from low and middle income countries: A systematic review and meta-analysis. J Paediatr Child Health. 2017;53: 474–479. doi: 10.1111/jpc.13443 [DOI] [PubMed] [Google Scholar]
- 51.Maitland K, Berkley JA, Shebbe M, Peshu N, English M, Newton CRJC. Children with Severe Malnutrition: Can Those at Highest Risk of Death Be Identified with the WHO Protocol? PLOS Med. 2006;3: e500. doi: 10.1371/journal.pmed.0030500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Isanaka S, Hitchings MDT, Berthé F, Briend A, Grais RF. Linear growth faltering and the role of weight attainment: Prospective analysis of young children recovering from severe wasting in Niger. Matern Child Nutr. 2019;15: e12817. doi: 10.1111/mcn.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Koenker R, Bassett G. Regression Quantiles. Econometrica. 1978;46: 33–50. doi: 10.2307/1913643 [DOI] [Google Scholar]
- 54.Rahman A, Hossain MM. Quantile regression approach to estimating prevalence and determinants of child malnutrition. J Public Health (Bangkok). 2022;30: 323–339. doi: 10.1007/S10389-020-01277-0 [DOI] [Google Scholar]
- 55.Faruq A, El-Raouf MMA, Azizur R, Ramy A, Mohamed MS, Hossain MM. Prevalence and determinants of wasting among under- Egyptian children: Application of quantile regression. Food Sci Nutr. 2022; 1–11. doi: 10.1002/fsn3.3144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Islam MR, Rahman MS, Rahman MM, Nomura S, de Silva A, Lanerolle P, et al. Reducing childhood malnutrition in Bangladesh: the importance of addressing socio-economic inequalities. Public Health Nutr. 2020;23: 72–82. doi: 10.1017/S136898001900140X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Darteh EKM, Acquah E, Darteh F. Why are our children wasting: Determinants of wasting among under 5s in Ghana. Nutr Health. 2017;23: 159–166. doi: 10.1177/0260106017722924 [DOI] [PubMed] [Google Scholar]
- 58.Illi S, von Mutius E, Lau S, Bergmann R, Niggemann B, Sommerfeld C, et al. Early childhood infectious diseases and the development of asthma up to school age: a birth cohort study. BMJ. 2001;322: 395. doi: 10.1136/BMJ.322.7283.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdulla F, Hossain MM, Karimuzzaman M, Ali M, Rahman A. Likelihood of infectious diseases due to lack of exclusive breastfeeding among infants in Bangladesh. PLoS One. 2022;17: e0263890. doi: 10.1371/journal.pone.0263890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lawrence R, Lawrence R. Breastfeeding: A Guide for the Medical Professional-Expert Consult. 7th Editio. Elsevier Health Sciences; 2010. http://books.google.es/books?id=c4BnozBW3EMC [Google Scholar]
- 61.Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. Evid Reports/Technology Assessments. 2007;153: 1–186. Available: https://www.ncbi.nlm.nih.gov/books/NBK38337/ [PMC free article] [PubMed] [Google Scholar]
- 62.Oddy WH. Breastfeeding protects against illness and infection in infants and children: a review of the evidence. Breastfeed Rev. 2001;9: 11–18. Available: https://pubmed.ncbi.nlm.nih.gov/11550600/ [PubMed] [Google Scholar]
- 63.Smith LC, Ruel MT, Ndiaye A. Why Is Child Malnutrition Lower in Urban Than in Rural Areas? Evidence from 36 Developing Countries. World Dev. 2005;33: 1285–1305. doi: 10.1016/J.WORLDDEV.2005.03.002 [DOI] [Google Scholar]
- 64.Hasan MT, Soares Magalhaes RJ, Williams GM, Mamun AA. The role of maternal education in the 15-year trajectory of malnutrition in children under 5 years of age in Bangladesh. Matern Child Nutr. 2016;12: 929–939. doi: 10.1111/mcn.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rahman MM, Saima U, Goni MA. Impact of Maternal Household Decision-Making Autonomy on Child Nutritional Status in Bangladesh. Asia-Pacific J public Heal. 2015;27: 509–520. doi: 10.1177/1010539514568710 [DOI] [PubMed] [Google Scholar]
- 66.Covián C, Fernández-Fierro A, Retamal-Díaz A, Díaz FE, Vasquez AE, Lay MK, et al. BCG-Induced Cross-Protection and Development of Trained Immunity: Implication for Vaccine Design. Front Immunol. 2019;10: 2806. doi: 10.3389/fimmu.2019.02806 [DOI] [PMC free article] [PubMed] [Google Scholar]