Abstract
Objective
Our objective was to estimate the prevalence and risk factors for long COVID symptoms among polymerase chain reaction–confirmed COVID-19 patients (hospitalised and community) in Malta.
Study design
This was a national cross-sectional survey among COVID-19 patients in Malta during 2020.
Methods
Patients were sent a questionnaire 3–6 months after testing positive. Data were analysed descriptively to estimate symptom prevalence, and multivariable logistic regressions were used to determine the risk factors for long COVID symptoms. Age, sex, initial symptoms, hospitalisation, and healthcare worker status were used as risk factors and symptoms (cough, shortness of breath, fatigue, anxiety, sadness, and memory loss) 2.5 months or more after COVID-19 onset were used as outcomes.
Results
Of 8446 eligible participants, 2665 (31.55%) responded with a median age of 37 years. Initial symptoms were reported in 82% of responders, and 7.73% were hospitalised. Among the long COVID symptoms, fatigue persisted among most non-hospitalised responders, whereas anxiety, shortness of breath, and sadness were the most common symptoms. Female sex, hospitalisation, and initial symptoms were associated with higher odds of fatigue, shortness of breath, cough, anxiety, sadness, and memory loss as long COVID symptoms.
Conclusions
Our study is the first to highlight long COVID symptoms and risk factors in Malta, showing that long COVID is common among hospitalised and non-hospitalised patients. These data should increase awareness of long COVID and facilitate support to those affected nationally.
Keywords: COVID-19 infection, Cross-sectional survey, Long COVID
Introduction
Long COVID has been defined in several ways. Recently, the World Health Organization used the Delphi method to agree on a definition.1 Observations from various studies have indicated a significant variation in reported symptoms ranging from fatigue, dyspnoea, joint pains, chest pain, headaches, hair loss and changes in hearing with or without tinnitus to psychological disorders such as memory loss, anxiety, depression, disorders of sleep and concentration and attention disorders.2
However, the extent of the impact of long COVID in Malta is still unknown, and a better understanding of these long-term effects could aid in policymaking and resource allocation. Our objective was to estimate the prevalence and risk factors for long COVID symptoms and complications among polymerase chain reaction (PCR)-confirmed COVID-19 patients in Malta.
Methods
Study design
A cross-sectional survey was carried out using an online self-administered questionnaire via a Google form. Demographics, COVID-19-episode information (e.g. symptoms experienced, hospitalisation) and long COVID symptoms persisting for more than 2.5 months after the COVID-19 episode (Supplementary Table 1).
Participants
Participants were eligible if they had tested PCR positive for SARS-CoV-2 in Malta during 2020, had COVID-19 only once, had a registered working email address and were not asylum seekers/refugees or deceased. The questionnaire was sent to 8446 eligible participants 3–6 months after their positive PCR test result. A second email was sent after 2.5 weeks. In addition, based on the government definition (personal communication), two waves were defined in our study: wave 1, from 6 March 2020 to 17 July 2020; and wave 2, from 18 July to 31 December 2020.
Data analysis
Data were analysed descriptively to estimate symptom prevalence. Although no preselection strategy was used to adjust for response bias, the respondents' age, gender and hospitalisation during the first and second waves were compared among all cases testing positive in Malta, those eligible to participate and the study responders. Specifically, the proportion of patients in each demographic group was compared descriptively to the sampling frame to assess potential data gaps or overrepresentation. Logistic regression was used to determine the risk factors for long COVID symptoms. Age, sex, wave number, healthcare worker status, initial symptoms, and hospitalisation due to COVID-19 were used as covariates. Symptoms persisting for more than 2.5 months from the COVID-19 episode were modelled as a dichotomous outcome on each model. Six models were fitted using the following outcomes: fatigue, shortness of breath, cough, anxiety, sadness and memory loss. All analyses were performed using R studio (R version: R 4.1.2)11.
Results
Response rate
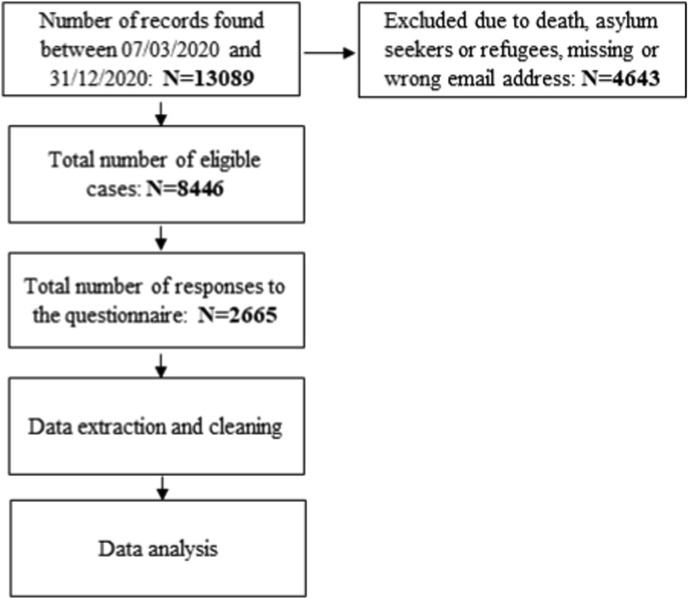
There were 13,089 COVID-19 cases recorded during 2020 in Malta. Of these, 4643 records were excluded, and 2665 replies were received (response rate = 31.55%; Fig. 1 ).
Fig. 1.
Flowchart of inclusion and exclusion criteria of a national survey of long COVID in Malta.
Description of the data
The median age was 37 years (interquartile range = 21 years), 56% were female, and 7.73% of the responders had been hospitalised during their initial COVID-19 episode. Supplementary Table 1 compares the characteristics (age, gender, wave, and hospitalisation) of all cases in 2020, the eligible participants, and those who responded to our questionnaire. Most characteristics were observed to be similarly represented in the three groups, signifying minimal selection and response bias.
Symptoms reported after isolation discharge from public health
The most common long COVID symptoms affecting more than 10% of respondents were anxiety, fatigue, and feeling of sadness (Supplementary Table 2). One in four patients (25.4%) persisted with at least one long COVID symptom, whereas 28.7% and 14.0% reported at least three or more and five or more long COVID symptoms, respectively. These numbers were higher among patients initially hospitalised: 44.2% reported at least one symptom a month after discharge, and 33.0% and 18.4% of patients presented three or more and five or more long COVID symptoms, respectively.
Risk factors for long COVID symptoms
Wavenumber was not associated with our discharge symptoms, and there was no significant interaction between age and hospitalisation. Female patients, initial hospital admission, and initial symptoms were associated with higher odds of fatigue, shortness of breath, cough, anxiety, sadness, and memory loss (Table 1 ). Participants in the 30–59 years age group were associated with higher odds of fatigue, cough, and memory loss than those in the less than 30 years age categories. However, there was no association between age and shortness of breath (Table 1). Conversely, patients aged 60 years were associated with lower odds of sadness and anxiety than those younger than 30 years (Table 1). Finally, healthcare workers were associated with lower odds of sadness than non-healthcare workers (Table 1).
Table 1.
Multivariable analysis (odds ratio [95% confidence interval]) of risk factors for fatigue, shortness of breath, cough, memory loss, anxiety, and sadness as long COVID symptoms from a national survey in Malta (N = 2665).
| Risk factor | Fatigue | Shortness of breath | Cough | ||||
|---|---|---|---|---|---|---|---|
| Prevalence | N (%) | 258 (9.7%) | 378 (14.2%) | 141 (5.3%) | |||
| OR |
P-value |
OR |
P-value |
OR |
P-value |
||
| Hospitalisation (no) | 2459 (92.3%) | Ref | <0.01 | Ref | <0.01 | Ref | <0.01 |
| Yes | 206 (7.7%) | 2.99 (2.04–4.31) | 3.36 (2.37–4.71) | 3.18 (1.89–5.15) | |||
| Sex (female) | 1493 (56.0%) | Ref | <0.01 | Ref | <0.01 | Ref | <0.01 |
| Male | 1172 (44.0%) | 0.4 (0.3–0.54) | 0.41 (0.31–0.53) | 0.45 (0.29–0.68) | |||
| Initial symptoms (no) | 475 (17.8%) | Ref | <0.01 | Ref | <0.01 | Ref | 0.12 |
| Yes | 2190 (82.2%) | 2.08 (1.38–3.27) | 2.61 (1.75–4.05) | 1.6 (0.92–3.04) | |||
| Age (<30) | 771 (28.9%) | Ref | Ref | Ref | |||
| 30–59 | 1615 (60.6%) | 1.86 (1.36–2.6) | <0.01 | 1.25 (0.96–1.65) | 0.11 | 1.66 (1.06–2.68) | 0.03 |
| >59 |
279 (10.5%) |
1.35 (0.79–2.27) |
0.26 |
0.82 (0.49–1.31) |
0.41 |
0.92 (0.38–2.01) |
0.84 |
| Risk factor | Memory loss | Anxiety | Sadness | ||||
| Prevalence | N (%) | 147 (5.5%) | 293 (11.0%) | 287 (10.8%) | |||
| OR |
P-value |
OR |
P-value |
OR |
P-value |
||
| Hospitalisation (no) | 2459 (92.3%) | Ref | <0.01 | Ref | <0.01 | Ref | <0.01 |
| Yes | 206 (7.7%) | 2.00 (1.17–3.25) | 3.34 (2.31–4.77) | 3.3 (2.28–4.72) | |||
| Sex (female) | 1493 (56.0%) | Ref | <0.01 | Ref | <0.01 | Ref | <0.01 |
| Male | 1172 (44.0%) | 0.41 (0.28–0.6) | 0.35 (0.26–0.47) | 0.41 (0.31–0.54) | |||
| Initial symptoms (no) | 475 (17.8%) | Ref | <0.01 | Ref | <0.01 | Ref | <0.01 |
| Yes | 2190 (82.2%) | 2.49 (1.42–4.8) | 3.15 (2–5.27) | 2.74 (1.77–4.47) | |||
| Age (<30) | 771 (28.9%) | Ref | <0.01 | Ref | Ref | ||
| 30–59 | 1615 (60.6%) | 2.35 (1.54–3.71) | <0.01 | 1.2 (0.91–1.6) | 0.20 | 1.26 (0.95–1.68) | 0.11 |
| >59 | 279 (10.5%) | 1 (0.41–2.16) | 1.00 | 0.51 (0.27–0.89) | 0.02 | 0.48 (0.25–0.85) | 0.02 |
| Healthcare worker (no) | 2401 (90.1%) | Ref | NA | Ref | 0.12 | Ref | 0.03 |
| Yes | 264 (9.9%) | NA | NA | 0.7 (0.43–1.08) | 0.58 (0.34–0.91) | ||
OR, odds ratio.
Discussion
We evaluated the distribution of long COVID symptoms and their risk factors among COVID-19 patients diagnosed during the first year of the pandemic in Malta. We found that a large proportion of hospitalised and non-hospitalised COVID-19 patients presented with long COVID symptoms, and that as disease severity increased, patients had higher odds of presenting with long COVID.
Our study's prevalence of long COVID symptoms was similar to other studies. For example, a study in Germany with a similarly low hospitalisation rate and follow-up time found that 9.7% and 8.6% of patients presented with fatigue and shortness of breath, respectively.3 In our study, female patients presented higher odds of long COVID symptoms than males (fatigue, shortness of breath, cough, anxiety, sadness and memory loss). Although patients in other reported studies were all hospitalised, they also observed female sex as a risk factor for myalgia, fatigue and anxiety.4 One possible explanation is that because of cultural reasons, in Malta, females were impacted by restriction measurements in higher proportions than males, given that they are the usual carers of their children and elderly relatives, which might explain the higher odds of anxiety and sadness observed in the data when compared with other studies.4
Younger age categories were associated with higher odds of anxiety and depression when compared with the older age categories. This was consistent with other studies carried out elsewhere.5 , 6 One study linked these observations to increased use of social media by younger age groups, which could lead to more exposure to news about COVID-19.5 Another possible explanation accounting for the differences between age groups could be the different presentation of sadness and anxiety in older persons, leading to misdiagnose by clinicians and lack of awareness by the sufferers themselves.7
Conversely, people in the 30–59 years age category had higher odds of developing fatigue, cough, and memory loss than those younger than 30 years. This is not surprising, given that those in the 30–59 years age category tend to have more severe symptoms than those in the younger category. Studies reviewed in the literature indicated that older patients had a higher risk of developing long COVID-19 symptoms;8 however, our study did not show similar results. Although lack of association does not prove independence, a two-fold reason could account for this. First, older patients were more likely to die from COVID-19, thus leading to survivor bias. Second, younger patients were more likely to be reached by email, therefore causing selection bias.
It is well known that frontline workers are at higher risk of infection than the general population when a new unknown disease emerges. Therefore, it is surprising that although higher odds of mental health problems were identified during previous health emergencies, being a healthcare worker was associated with lower odds of sadness. A potential explanation could be that most studies compare the risk of mental health disorders among the whole population rather than COVID-19–positive patients. Therefore, although this study does not refute the previous evidence, it is necessary to continue investing in frontline workers' mental health.
Limitations and strengths
As we conducted this study, long COVID has been defined further. Currently, the accepted definition includes symptoms 3 months from COVID-19 onset. In our study, patients were classified as having symptoms for 2.5 months or more. The small difference between the currently accepted definition and ours should not limit our interpretation, as patients were interviewed 3–6 months after their initial episode.
There were other limitations in our study. First, we did not collect information regarding comorbidities or underlying health conditions. These were not part of the initial protocol but have been demonstrated to be confounders or effect modifiers on the association of risk factors and long COVID-19 symptoms.9 Second, treatments were not evaluated in this study, and it is known that dexamethasone and oxygen treatment could reduce some of the symptoms in hospitalised patients. However, 93% of our study participants were non-hospitalised patients and were unlikely to be under these treatments. Third, the number of factors explored in our analyses was limited. For example, future studies could also consider socio-economic factors and access to health care as potential risk factors for long COVID. And fourth, as no COVID-19 vaccinations were available at the time, our study population was limited to unvaccinated individuals.
Our study had several strengths. First, except for some large registry-based studies similar to the one by Estiri et al.,10 most studies have a smaller sample size. Second, we presented data from a national survey, and national data can leverage policy when presented to decision-makers. Third, we used a comprehensive sampling frame that allowed us to identify differences between respondents and not respondents, which can help identify potential sources of bias.
Conclusion
It is essential to understand the characteristics and risk factors for long COVID to effectively communicate with the local population. In addition, the associations between hospitalisation and symptom severity with long COVID symptoms are important for follow-up of discharged COVID-19 patients and resource allocation. National evidence-based decisions could aid in COVID-19 case management, helping increase clinicians' awareness regarding long COVID, offering support to COVID-19 survivors to re-establish their pre-COVID-19 health.
Author statements
Ethical approval
Ethical approval for this study (HEC18/2020) was obtained from the Health Ethics Committee, Malta.
Funding
No funding was available for this study.
Competing interests
None declared.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.09.021.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.World Health Organization . WHO; 2020. A clinical case definition of post COVID-19 condition by a Delphi consensus. [Google Scholar]
- 2.Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P.A., Cuapio A., et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):1–14. doi: 10.1038/s41598-021-95565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Augustin M., Schommers P., Stecher M., Dewald F., Gieselmann L., Gruell H., et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. Lancet Reg Heal - Eur. 2021;6:1–8. doi: 10.1016/j.lanepe.2021.100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sykes D.L., Holdsworth L., Jawad N., Gunasekera P., Morice A.H., Crooks M.G. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. 2021;199(2):113–119. doi: 10.1007/s00408-021-00423-z. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nwachukwu I., Nkire N., Shalaby R., Hrabok M., Vuong W., Gusnowski A., et al. COVID-19 pandemic: age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Publ Health. 2020;17:6366. doi: 10.3390/ijerph17176366. 2020 Sep;17(17):6366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saúde Pública. 2020;36(4) doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 7.Christensen H., Jorm A.F., Mackinnon A.J., Korten A.E., Jacomb P.A., Henderson A.S., et al. Age differences in depression and anxiety symptoms: a structural equation modelling analysis of data from a general population sample. Psychol Med. 1999;29(2):325–339. doi: 10.1017/s0033291798008150. [DOI] [PubMed] [Google Scholar]
- 8.Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., et al. Attributes and predictors of long COVID. Nat Med. 2021;27(4):626–631. doi: 10.1038/s41591-021-01292-y. 2021 274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yong S.J. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Auckl) 2021;53(10):737–754. doi: 10.1080/23744235.2021.1924397. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Estiri H., Strasser Z.H., Brat G.A., Semenov Y.R. (4CE) TC for C of C 19 by E, Patel CJ, et al. Evolving Phenotypes of non-hospitalized Patients that Indicate Long Covid. medRxiv. 2021;25 doi: 10.1186/s12916-021-02115-0. 2021.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.