Abstract
An abortion is a procedure defined by termination of pregnancy, most commonly performed in the first or second trimester. There are several means of classification, but the most important includes whether the abortion was maternally “safe” (performed in a safe, clean environment with experienced providers and no legal restrictions) or “unsafe” (performed with hazardous materials and techniques, by person without the needed skills, or in an environment where minimal medical standards are not met). Complication rates depend on the procedure type, gestational age, patient comorbidities, clinician experience, and most importantly, whether the abortion is safe or unsafe. Safe abortions have significantly lower complication rates compared to unsafe abortions. Complications include bleeding, retained products of conception, retained cervical dilator, uterine perforation, amniotic fluid embolism, misoprostol toxicity, and endometritis. Mortality rates for safe abortions are less than 0.2%, compared to unsafe abortion rates that range between 4.7–13.2%. History and physical examination are integral components in recognizing complications of safe and unsafe abortions, with management dependent upon the diagnosis. This narrative review provides a focused overview of post-abortion complications for emergency clinicians.
INTRODUCTION
Abortion techniques and contraception have been described throughout history.1–3 In the current era, multiple countries place no restrictions on abortion, but most have an upper gestational age limit for when abortion can be performed, ranging from 6–24 weeks.3 However, as of 2021, 24 countries have issued a complete ban on abortions. The World Health Organization (WHO) classifies abortions as maternally “safe” or “unsafe”; “safe” abortion are ones performed in a setting where abortion laws are not restrictive, or if there is a formal law, safe abortion is still available.3,4 An “unsafe” abortion is performed by a person without the needed skills, performed with hazardous materials and techniques, or performed in an environment where minimal medical standards are not met.3,5–7
Unsafe abortions are a preventable pandemic, endangering females in locations where abortion is highly restricted by law or in countries where, even if legally permitted, safe abortion is not easily accessible.8,9 In this setting, females with an unintended pregnancy often self-induce abortions or obtain clandestine abortions from medical practitioners, paramedical workers, or traditional healers.5,6 Due to the risk of complications and potential risks associated with abortions, especially unsafe abortions, emergency clinicians must be able to recognize and manage these complications in the emergency department (ED) setting.
METHODS
We searched PubMed and Google Scholar for articles using the keywords “abortion” OR “post-abortion” AND “complication” from January 1, 1950–June 7, 2022. We also searched the first 200 articles resulted by Google Scholar for each of the keywords. Articles reviewed included case reports and series, retrospective studies, prospective studies, systematic reviews and meta-analyses, and other narrative reviews. Literature searches were restricted to studies published in English. The gray literature including conference abstracts was not searched. Two emergency clinicians with experience in critical appraisal of the literature reviewed the articles and decided which to include for review by consensus, with a focus on emergency medicine-relevant articles. We preferentially selected systematic reviews and meta-analyses, followed by prospective studies, retrospective studies, case reports, and other narrative reviews. We included 123 resources for construction of this narrative review. Of these, there were zero guidelines, five systematic reviews and meta-analysis, 20 prospective studies, 27 retrospective studies, 26 case reports, and 35 narrative reviews. We also included 10 online resources from international organizations such as WHO and the US Centers for Disease Control and Prevention (CDC).
DISCUSSION
Epidemiology
Abortion rates vary based on several factors. From 2010–2014, the worldwide abortion rate was estimated at 35 per 1,000 females between the ages of 15–44 years.10,11 Rates approximate 37 per 1,000 in low- and middle-income countries (LMIC) and 27 per 1,000 in resource-rich countries.10,11 The highest rate of abortions occurs in those aged 20–29 years (18.5–19.1 per 1,000).10–12 In 2019, 629,898 abortions were reported to the CDC throughout the United States.11 Over 85% of these abortions occurred in unmarried patients, and abortion rates were highest in non-Hispanic Blacks.10–13 There are documented disparities in abortion rates, with higher rates in women of color, lower income, and less education, which may be associated with systemic hardships including reduced access to healthcare, racial discrimination, poorer living and working conditions, and greater stress.13
The majority of US abortions occur in the first trimester, with 92% performed at ≤13 weeks gestation, 8% at 14–20 weeks, and 1% at ≥ 21 weeks.14 Worldwide, second-trimester abortions comprise 10–15% of all abortions. Medication-induced abortion are responsible for 39% of abortions prior to nine weeks of gestation, while for those with gestational age ≥14 weeks, over 92% of abortions are surgical.11,12
Prior to 2022, over 26 million safe abortions and 20–25 million unsafe abortions were performed annually.10–12,15–17 Approximately 97% of unsafe abortion occur in LMIC.9 Complete data is limited due to the restrictions on abortions and the secrecy involved, but the highest rates appear to occur in Latin America and Africa at 31 per 1,000 females per year and 28 per 1,000 females per year, respectively.18 This is followed by Asia at rates of 11 per 1,000 females, although hospital admissions are highest in Asia, at 8.2 per 1,000 females.18
Patients can present to the ED after an abortion, some with complications from the abortion. Although abortion-related complications are rare in the US, there is a paucity of data regarding national-level estimates of abortion-related ED visits.19 Within California’s Medicaid program, 0.03% of abortions were followed by an immediate ambulance transfer to an ED, and 2.6% of abortions were followed by an abortion-related ED visit within six weeks of the abortion, while ED visit rates in New York and Philadelphia following an abortion were 0.3%, congruent with Planned Parenthood data from 2009.20–22
Complication rates depend on the procedure type, gestational age, patient comorbidities, clinician experience and, most importantly, whether the abortion was performed in a safe or unsafe manner.8,9,19,23 The majority of complications associated with abortion are minor, but major complications can occur including severe hemorrhage, endometritis, non-uterine organ injury, and disseminated intravascular coagulation (DIC). 8,9,19,23 A study evaluating 54,911 abortions found an overall complication rate of 2.1%.19 Medication abortions had a 5.2% complication rate (4.9% minor, 0.3% major), with rates of 1.3% in the first trimester and 1.5% for the second trimester.19 First-trimester aspiration had a complication rate of 2.3% (1.1% minor, 0.2% major).19 In the US, the overall mortality rate is less than 1 per 100,000 abortions performed, and in 2010 10 females died from a legally induced abortion.11,12,21,24,25 Mortality rates are lowest in the first nine weeks of gestation (<0.3 per 100,000 abortion), with an increase after this period (7 per 100,000 at 16–20 weeks of gestation and 11 per 100,000 at >21 weeks).24,25 This is similar to the rate of mortality associated with dental procedures (0–1.7 deaths per 100,000).21,24,25 Overall mortality rates for safe abortions are less than 0.2%, but for unsafe abortions the mortality rate is significant.20,21 Approximately 68,000 females die annually due to a complication from an unsafe abortion.8,9,15 Countries with less training of and access to abortion clinicians have higher maternal mortality rates.25 Annual maternal mortality rates associated with unsafe abortion range from 4.7–13.2%.8,9 In countries with significant resources, 30 females per 100,000 unsafe abortions die annually, but the incidence rises to 220 deaths per 100,000 unsafe abortions in settings with limited resources.8,9,23 Mortality associated with an unsafe abortion is most commonly due to septic abortion and hemorrhage.8,9,23
Abortion Methods
There are several methods for safe abortions. The procedure may be medication-based or interventional, depending on the gestational age, patient preferences, experience of the clinician, and access to resources. Patients within the first trimester may undergo medical or interventional abortion (eg, aspiration). There are several differences between the two types, detailed in Table 1.26–29 In the second trimester, patients may undergo induction with medications or intervention with dilation and evacuation (D&E). Following termination of the pregnancy, patients typically experience vaginal bleeding similar to or slightly heavier than normal menstruation along with mild lower abdominal or pelvic cramping. Serum human chorionic gonadotropin (hCG) levels return to undetectable levels 7–60 days after the abortion.26
Table 1.
Safe abortion types.
| 1st trimester: Medication (Induction) |
|
| 1st trimester: Uterine aspiration |
|
| 2nd trimester: Medication (Induction) |
|
| 2nd trimester: Dilation and evacuation |
|
mg, milligram; mcg, microgram.
There are several methods by which unsafe abortions are performed.3,6 The method chosen depends on the patient, available resources, and any assistance the patient receives. The various forms are detailed in Table 2.
Table 2.
Unsafe abortion types and complications.
| Forms of unsafe abortion | Abortion Complications* |
|
|
These complications may occur in both safe and unsafe abortions.
Evaluation in the Emergency Department
The primary goal of the ED assessment is evaluation for dangerous post-abortion complications. A focused history and physical examination can provide important information and determine the need for further testing and treatment. History should include gestational history, estimated gestational age at the time of abortion, current symptoms (eg, bleeding, vaginal discharge, fever, chills, rigors, abdominal or pelvic pain), details of the abortion procedure (eg, procedure date, whether a surgical procedure was performed, medications used, whether any procedural complications occurred), and comorbidities.6 Medical history including known coagulopathy, diabetes, immunocompromised state, and prior abdominal and obstetric/gynecologic (OB/GYN) procedures should be obtained. Of note, females with a self-induced abortion may be hesitant to disclose the attempt due to perceived legal or social repercussions. Emergency clinicians must remain vigilant and inquire in a nonjudgmental fashion concerning any abortion attempt. Directed questions about where and how the abortion was performed are necessary to guide further evaluation and management.6 History should be obtained without the patient’s partner in the room.
Examination requires assessment of the patient’s hemodynamic status. Abdominal examination should assess for focal tenderness or evidence of peritonitis (eg, guarding or rigidity). Speculum and bimanual examinations should also be performed, evaluating for bleeding, vaginal discharge, trauma or laceration, uterine tone, tenderness, retained tissue, and masses.6 Laboratory analysis should include the following: complete blood count; electrolytes; renal and liver function; hCG level; coagulation panel, and blood type and screen (with crossmatch if bleeding) although this can be adjusted for the severity of presentation.30 If there is evidence of severe infection, blood and cervical cultures should be obtained, as well as lactic acid level.31,32 Fibrinogen, fibrin split products, and D-dimer should be obtained in patients with concern for DIC based on history and examination. The need for imaging evaluation is based on the suspected complication.30,33
Ultrasound can help identify retained products of conception (RPOC), ongoing pregnancy, ectopic masses, echogenic material within the uterus, hematoma formation, and intra-abdominal free fluid, which may suggest a uterine perforation, rupture, or vascular injury. An initial point-of-care ultrasound would be valuable to assess for intrauterine pregnancy and free fluid as part of the initial management, although many patients may need a more comprehensive radiologic ultrasound to assess for more advanced or complex findings. Computed tomography (CT) may help in the evaluation of uterine rupture, pelvic abscess, bowel injury, hematoma, or uterine myonecrosis.
Bleeding
Vaginal bleeding is common after an abortion and is usually similar to or heavier than a normal menstrual cycle. Patients with medical abortions typically have more bleeding compared to surgical abortions and may present similarly to those having a spontaneous abortion.6,29 One study reported that blood loss ranged between 84–101 milliliters (mL) in patients undergoing safe medical abortion and 53 mL in abortion via aspiration.34 This bleeding does not typically require additional therapy or intervention, with less than 1% of first-trimester patients who underwent a safe abortion requiring acute intervention and 0.05% requiring a blood transfusion.20,21,35,36 Bleeding is usually bimodal, with moderate or heavy bleeding that is worse 3–8 hours after medication administration.37,38 After this time frame, bleeding lessens but can last up to 17 days, followed by bleeding 30–60 days that marks the resumption of menses.39–42 Initial bleeding most commonly lasts for 9–12 days following medical abortion, but this is less for those undergoing surgical abortion.42,43 In unsafe abortions, the rate of severe hemorrhage increases to 3%, with non-severe bleeding occurring in up to 44% of patients.23 The differential diagnosis for patients with post-abortion bleeding is demonstrated in Table 3.
Table 3.
Post-abortion bleeding etiologies.
More common:
|
Patients should seek medical evaluation if they soak through two pads per hour for two consecutive hours, which is suggestive of severe hemorrhage.30,36,44,45 Evaluation and management of hemorrhage in the post-abortion setting is similar to that of the postpartum period, with consideration of the differential listed in Table 3. If the physical examination does not reveal a readily apparent source (e.g., vaginal laceration), pelvic ultrasound should be performed to evaluate for RPOCs, uterine blood, or evidence of uterine perforation (eg, free fluid or air in the pelvis).30,33,45
Cervical or vaginal lacerations are typically repaired in the postoperative period. If a small laceration is discovered on ED evaluation, apply direct pressure or consider silver nitrate cauterization.30,33,45 Extensive lacerations may require OB/GYN consultation and placement of absorbable sutures.30,33,45 If an etiology is not discovered on physical examination or ultrasound, consider uterine atony. Uterine atony is treated with uterine massage and administration of uterotonic agents (Table 4). If uterotonic medications and bimanual massage are not effective, intrauterine tamponade can be performed, including a Bakri balloon or Foley catheter.30,45
Table 4.
Management of uterine atony.
| Intervention | Dosing, route, and side effects |
| Initial30 | Bimanual massage *Ensure that the placenta is evacuated completely |
| Medical | |
| Physical tamponade30,45 |
|
mcg, microgram; SL, sublingual; PR, by rectum; IM, intramuscular; ml, milliliter.
Patients with severe bleeding and/or hemodynamic instability should receive blood products. Emergency consultation with OB/GYN and surgical specialists is recommended. Activation of a massive transfusion protocol may be required. Tranexamic acid (TXA) should also be considered.30 Literature has demonstrated that TXA may reduce the risk of postpartum hemorrhage and does not increase the risk of developing thromboses.49 If bleeding remains refractory to other therapies or in the setting of abnormal vascular bleeding, interventional radiology may need to perform uterine artery embolization.30,50–52 Some patients may also require surgical management in the operating room.30
Retained products of conception
Retained products of conception occur more commonly with medical abortions compared to surgical abortions and are more common after the first trimester (2–10% of those undergoing abortion in the second trimester).53,54 Patients may report tissue passage even without passing the fetal tissue itself, as decidualized endometrium can shed with ongoing pregnancy.6,29 RPOCs are also more common in unsafe abortions, especially if self-induced, if the procedure is performed by an inexperienced individual or in later gestational ages, or uterine abnormality is present.19,20,30,55 Patients with RPOCs may present with vaginal bleeding, abdominal or pelvic pain, fever, and uterine tenderness.55 While bleeding is common after an abortion, large volume bleeding (≥2 pads per hour for ≥ 2 hours), sustained fever, worsening pain, or persistent pain lasting for multiple days is abnormal and should raise concern for RPOCs.19,20,30,37,38
Ultrasound has a more limited ability to diagnose RPOCs as necrotic decidua and blood clots within the uterus following abortion can mimic RPOCs, with significant overlap between findings in asymptomatic and symptomatic patients.56,57 The uterus may demonstrate irregular and thickened lining with prominent color Doppler flow in patients with RPOCs, as well as those recovering after a successful abortion.56,58 However, a hyperechoic endometrial mass or solid component in the endometrium found on ultrasound in the setting of abnormal bleeding or evidence of infection is sensitive for RPOCs (Figure 1).59–62 Low-resistance Doppler flow within the myometrium or just below the endometrium is also suspicious for RPOCs.62,63 Emergent consultation with OB/GYN is recommended, as treatment includes RPOC removal through vacuum aspiration or D&E.30,45,56
Figure 1.
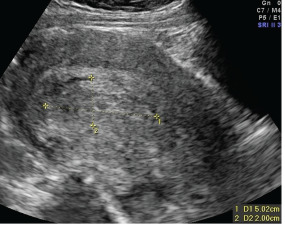
Ultrasound showing evidence of retained products of conception, demonstrated by echogenic, heterogeneous, and vascular intrauterine contents. Case courtesy of Dr Alexandra Stanislavsky, Radiopaedia.org, rID: 13852. Accessed at https://radiopaedia.org/cases/retained-products-of-conception-2?lang=us.
Misdiagnosed Ectopic Pregnancy
Ectopic pregnancy is associated with significant morbidity and mortality. However, ectopic pregnancy occurs in less than 1% of patients who present for abortion, which is close to three times lower than the overall rate of ectopic pregnancy.64–66 The literature suggests an ectopic pregnancy rate of 7=20 per 100,000 procedures.21,67 Ectopic pregnancy is most likely to occur in an abortion performed in a pregnancy of unknown location (ie, no yolk sac or fetal pole present on ultrasound).68 Patients with ectopic pregnancy most commonly present with abdominal pain or vaginal bleeding.69–71 Evaluation should include an ultrasound for intrauterine and extrauterine masses. In the post-abortion setting, ectopic pregnancy can be excluded by identifying products of conception after the aspiration.68 If an extrauterine mass is found on ultrasound, emergent consultation with OB/GYN is necessary.69–71
Uterine Perforation
Uterine perforation is a potential complication of any intrauterine procedure and is the most common site of upper genital tract injury.35,72,73 Injury to the bowel, bladder, and surrounding vasculature may accompany uterine perforation.35,72–75 Data on these injuries is scarce, with three case series of 92 total uterine perforations reporting bowel or bladder injury in six cases.76–78 Overall, uterine perforation is uncommon, with rates ranging between 0.1–2.3% in safe medical abortions.29,30,35,79,80 Rates of uterine perforation are higher in unsafe abortions due to the instruments used and inexperience of the person performing the procedure.23 Factors associated with an increased risk of uterine perforation include surgeon inexperience and inadequate preoperative cervical dilation.35,38 Other factors include those that create difficulty in accessing the endometrial cavity (eg, cervical stenosis, uterine anteflexion/retroflexion) and those that alter the myometrial wall integrity and strength (eg, prior cesarean delivery, uterine scarring), particularly for those undergoing medication-induced abortion in the second trimester.72,73,81 While patients often experience mild-to-moderate abdominal or pelvic cramping for several hours after the procedure, continued and severe pain is atypical.75
Of note, patients can present up to several weeks after the procedure, which depends on the site of uterine injury and concomitant organ injuries.82,83 Symptoms include focal or diffuse abdominal/pelvic pain, abdominal distension, heavy or persistent vaginal bleeding, hematuria, and fever. Patients may also present with tachycardia and hypotension.23 Loops of bowel can become incarcerated within the uterine defect and result in bowel obstruction and subsequent perforation.84–88 Initial imaging includes ultrasound, which may demonstrate a defect in the uterine wall, abdominal free fluid, or abnormal contents within the uterus including fetal tissue (Figure 2).86,89
Figure 2.
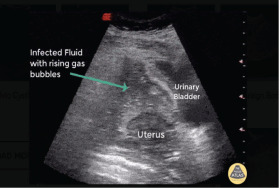
Ultrasound demonstrating pelvic free fluid and rising gas bubbles, indicative of uterine perforation. Image courtesy of Robert Jones, DO, POCUS Atlas. Available at https://www.thepocusatlas.com/ob-gyn-atlas.
However, ultrasound should not be used to exclude uterine perforation; if the ultrasound is non-diagnostic, further imaging with CT of the abdomen/pelvis is recommended (Figure 3).29,80,86 Computed tomography is also recommended in the setting of suspected bowel perforation, as CT is highly sensitive and specific and can localize the site of perforation.90–93 If uterine perforation is suspected, emergent consultation with OB/GYN and general surgery is recommended. Patients with isolated uterine perforation can be managed surgically or expectantly, depending upon the patient’s hemodynamic status.88 Patients with concomitant bowel perforation require surgical specialist consultation, intravenous (IV) fluid resuscitation and symptomatic management, and broad-spectrum antibiotics.
Figure 3.
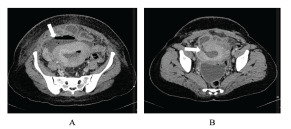
Computed tomography demonstrating a) fluid collection anterior to the uterus that communicates with the endometrial cavity and b) defect in the anterior wall of the uterus. Case courtesy of Dr Hidayatullah Hamidi, Radiopaedia.org, rID: 90743. Available at https://radiopaedia.org/cases/uterine-rupture-with-postpartum-infection?lang=us.
Retained Cervical Dilator
Osmotic dilators are typically placed the day prior to D&E. Complications are rare but can occur while the dilator is in place. These complications include bleeding, infection, rupture of membranes, and allergic reaction.94 Cases of retained cervical dilators have been reported, in which patients presented with pelvic pain and vaginal bleeding. In these cases, the retained dilator was found on imaging and removed surgically.95,96
Amniotic Fluid Embolism
Amniotic fluid embolism (AFE) is a life-threatening obstetric complication following abortion or delivery.97,98 Patients develop sudden and refractory circulatory collapse with DIC, the latter of which occurs in up to 80% of patients.97,99 While AFE more commonly occurs in full-term deliveries, it can occur following abortion.100–105 An AFE secondary to abortion appears to be rare, but it accounted for approximately 5.5% of mortality in abortions within 2011–2013 Pregnancy Mortality Surveillance System analysis, with 1 of 111 AFEs occurring following an abortion.106,107
The American Society for Maternal-Fetal Medicine set forth four diagnostic criteria to improve recognition for this disease, which carries a mortality risk of 11–61%, The criteria include the following: 1) sudden hypotension or cardiopulmonary collapse; 2) DIC; 3) symptom development during labor and/or delivery of products of conception; and 4) absence of fever.98,108,109 Treatment requires prompt recognition of AFE, triggering immediate evacuation of the fetus or products of conception and aggressive maternal cardiopulmonary support to include fluid administration, vasopressor and inotropic support, as well as consideration of phosphodiesterase inhibition for right ventricular optimization.110 Venoarterial extracorporeal membrane oxygenation (ECMO) has demonstrated positive outcomes for severe cases in high-volume ECMO centers, although considerable risk is incurred with cannulation during profound coagulopathy.111,112 In a study of 10 AFEs treated with ECMO, there was a 70% survival-to-hospital-discharge rate.113
Misoprostol Toxicity
Toxicity from misoprostol, a prostaglandin E analogue, is uncommon in safe abortion settings but is more likely in unsafe abortions. Toxic doses between 3–8 milligrams (mg) may result in severe fever, rigors, abdominal pain and cramping, vomiting and diarrhea, agitation, altered mental status, hypotension, hypoxemia, and rhabdomyolysis.114–117 These signs and symptoms typically develop quickly after initial ingestion, as misoprostol is completely absorbed from the stomach within 1.5 hours. Management includes removing remaining tablets from the stomach (e.g., gastric lavage) or vagina, along with supportive care including IV fluids and antiemetics. Vasopressors may be needed in those patients who are refractory to IV fluids. Symptoms typically resolve in 12 hours, but doses over 12 mg may result in multiorgan failure and death.114,116–118
Post-abortion Infection and Endometritis
Septic abortion is defined by any uterine infection that complicates a spontaneous or induced abortion. This is a potential complication of both medication and surgical abortions and can be due to RPOCs or the procedure itself (eg, trauma, nonsterile technique). Importantly, post-abortion infection is a clinical diagnosis in the setting of a patient who presents with signs and symptoms of uterine infection following abortion. Septic abortion occurs in less than 0.4% of patients undergoing first trimester uterine aspiration and safe abortions, but this rate is much higher in those undergoing unsafe abortions.20,21 Non-severe infection occurs in 24% of those undergoing unsafe abortions, while severe infection occurs in 5.1%.21
The most common microbes include Enterobacteriaceae, streptococci, staphylococci, and enterococci, which are common endogenous vaginal and gastrointestinal flora.31 Other causative organisms include Chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis from pre-existing infections.31 Group A streptococcus and clostridium species can result in serious infections with rapid deterioration associated with toxic shock syndrome.31,32,107,107,119 Patients with post-abortion infections including endometritis typically present with pelvic and/or abdominal pain, nausea, vomiting, uterine tenderness, vaginal discharge and/or bleeding, and fever. Vaginal discharge is often sanguinopurulent.20,31,32 If history and examination suggest septic abortion, broad-spectrum antibiotics should be administered along with symptomatic management and resuscitation.
Antibiotic regimens are provided in Table 5.20,31,32 Consultation with OB/GYN is necessary if the diagnosis is suspected and should occur prior to imaging. Ultrasound can be used to evaluate for RPOCs, but a normal ultrasound should not be used to exclude septic abortion. Ultrasound may demonstrate intrauterine tissue, enhanced myometrial vascularity, hydrosalpinges, or an adnexal mass, which may suggest an abscess.120 Computed tomography may be used if the clinician is concerned for another condition or intra-abdominal abscess. If RPOCs are present, vacuum aspiration dilation and curettage is necessary.32 Patients may rapidly progress to acute respiratory distress syndrome, DIC, and acute renal injury.8,9,19,23,121,122
Table 5.
Antibiotic regimens for post-abortion infection or endometritis.
| Imipenem 500 mg IV |
| Piperacillin-tazobactam 4.5 g IV |
| Levofloxacin 500 mg IV + metronidazole 500 mg IV |
| Gentamicin 5 mg/kg IV + ampicillin 2 g IV + metronidazole 500 mg IV |
| Gentamicin 5 mg/kg IV + ampicillin 2g IV + clindamycin 900 mg IV |
IV, intravenous; mg, milligram; kg, kilogram; g, gram.
Mental Health
While emergency clinicians must focus on the medical management of abortion complications, they must also be mindful of the patient’s mental health and wellbeing. Women who undergo an abortion may have increased rates of mental health issues as compared to women who do not; the highest risk population includes women undergoing an abortion who have pre-existing mental health issues.123 Regardless of the clinician’s personal views, they must approach these patients with compassion and address any mental health concerns.123
LIMITATIONS
This is a narrative review, and thus no pooling of data from individual studies was conducted. Neither did we assess article quality or risk of bias. Much of the included literature consists of studies conducted in non-emergent settings; thus, generalizing these studies to the ED setting is challenging. Much of the information and resources come from society guidelines.
CONCLUSION
Abortion complications present a spectrum of emergencies ranging from small lacerations to life-threatening complications requiring immediate control. Unsafe abortions have a far higher rate of complications. Complications include bleeding, retained products of conception, retained cervical dilator, uterine perforation, amniotic fluid embolism, misoprostol toxicity, and endometritis. Supportive and nonjudgmental history and physical examination are integral in recognizing complications of safe abortions as well as issues that arise from unsafe abortions. Prompt recognition of the specific emergency with immediate stabilization and potential specialist consultation can mitigate morbidity and mortality.
Supplementary Information
ACKNOWLEDGMENTS
BL, REB, TM, and MG conceived the idea for this manuscript and contributed substantially to the writing and editing of the review. This review does not reflect the views or opinions of the US government, Department of Defense, US Army, US Air Force, Defense Health Agency, Brooke Army Medical Center, or SAUSHEC EM Residency Program.
Footnotes
Section Editor: Nicholas Pettit, DO, PhD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. No author has professional or financial relationships with any companies that are relevant to this study. There are no conflicts of interest or sources of funding to declare.
REFERENCES
- 1.Joffe C. Management of Unintended and Abnormal Pregnancy: Comprehensive Abortion Care. John Wiley and Sons; 2009. Abortion and Medicine: A Sociopolitical History; pp. 1–9. [DOI] [Google Scholar]
- 2.Riddle Suojanen JN, John M. Contraception and Abortion from the Ancient World to the Renaissance. Natl Cathol Bioeth Q. 2001;1(1):116–118. doi: 10.5840/ncbq20011187. [DOI] [Google Scholar]
- 3.Abortion. [Accessed June 27, 2022]. https://www.who.int/news-room/fact-sheets/detail/abortion .
- 4.World Population Review. Countries Where Abortion Is Illegal 2022. World Population Review. [Accessed June 27, 2022]. https://worldpopulationreview.com/country-rankings/countries-where-abortion-is-illegal. Published 2022.
- 5.Haddad LB, Nour NM. Unsafe Abortion: Unnecessary Maternal Mortality. [Accessed June 27, 2022];Rev Obstet Gynecol. 2009 2(2):122. /pmc/articles/PMC2709326/ [PMC free article] [PubMed] [Google Scholar]
- 6.Harris LH, Grossman D. Complications of Unsafe and Self-Managed Abortion. N Engl J Med. 2020;382(11):1029–1040. doi: 10.1056/NEJMRA1908412. [DOI] [PubMed] [Google Scholar]
- 7.Fawcus SR. Maternal mortality and unsafe abortion. Best Pract Res Clin Obstet Gynaecol. 2008;22(3):533–548. doi: 10.1016/j.bpobgyn.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Heal. 2014;2(6) doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 9.Ganatra B, Gerdts C, Rossier C, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. 2017;390(10110):2372–2381. doi: 10.1016/S0140-6736(17)31794-4/ATTACHMENT/D5100FC1-A915-4107-87DC-9DE7C3ADBFB3/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones RK, Witwer E, Jerman J. Abortion Incidence and Service Availability in the United States, 2017. 2019 September; doi: 10.1363/2019.30760. [DOI] [Google Scholar]
- 11.Kortsmit K, Jatlaoui TC, Mandel MG, et al. Abortion Surveillance — United States, 2018. MMWR Surveill Summ. 2021;69(7):1–30. doi: 10.15585/MMWR.SS6907A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kortsmit K, Mandel MG, Reeves JA, et al. Abortion Surveillance — United States, 2019. MMWR Surveill Summ. 2021;70(9):1–29. doi: 10.15585/MMWR.SS7009A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dehlendorf C, Harris LH, Weitz TA. Disparities in abortion rates: a public health approach. Am J Public Health. 2013;103(10):1772–1779. doi: 10.2105/AJPH.2013.301339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jatlaoui TC, Boutot ME, Mandel MG, et al. Abortion Surveillance — United States, 2015. MMWR Surveill Summ. 2020;67(13):1–45. doi: 10.15585/MMWR.SS6713A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sedgh G, Bearak J, Singh S, et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. 2016;388(10041):258–267. doi: 10.1016/S0140-6736(16)30380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prata N, Sreenivas A, Vahidnia F, Potts M. Saving maternal lives in resource-poor settings: Facing reality. Health Policy (New York) 2009;89(2):131–148. doi: 10.1016/j.healthpol.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Addante AN, Eisenberg DL, Valentine MC, Leonard J, Maddox KEJ, Hoofnagle MH. The association between state-level abortion restrictions and maternal mortality in the United States, 1995–2017. Contraception. 2021;104(5):496–501. doi: 10.1016/j.contraception.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. WHO | Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. 5th editio. Who; 2014. [Accessed June 27, 2022]. pp. 1–67. http://whqlibdoc.who.int/publications/2011/9789241501118_eng.pdf . [Google Scholar]
- 19.Upadhyay UD, Johns NE, Barron R, et al. Abortion-related emergency department visits in the United States: An analysis of a national emergency department sample. BMC Med. 2018;16(1) doi: 10.1186/s12916-018-1072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Upadhyay UD, Desai S, Zlidar V, et al. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125(1):175–183. doi: 10.1097/AOG.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 21.Cleland K, Creinin MD, Nucatola D, Nshom M, Trussell J. Significant adverse events and outcomes after medical abortion. Obstet Gynecol. 2013;121(1):166–171. doi: 10.1097/AOG.0b013e3182755763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bennett IM, Baylson M, Kalkstein K, Gillespie G, Bellamy SL, Fleischman J. Early abortion in family medicine: Clinical outcomes. Ann Fam Med. 2009;7(6):527–533. doi: 10.1370/afm.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adler AJ, Filippi V, Thomas SL, Ronsmans C. Quantifying the global burden of morbidity due to unsafe abortion: Magnitude in hospital-based studies and methodological issues. International Journal of Gynecology and Obstetrics. 118 doi: 10.1016/S0020-7292(12)60003-4. [DOI] [PubMed] [Google Scholar]; Int J Gynaecol Obstet. 2012 doi: 10.1016/S0020-7292(12)60003-4. [DOI] [Google Scholar]
- 24.Bartlett LA, Berg CJ, Shulman HB, et al. Risk factors for legal induced abortion-related mortality in the United States. Obstet Gynecol. 2004;103(4):729–737. doi: 10.1097/01.AOG.0000116260.81570.60. [DOI] [PubMed] [Google Scholar]
- 25.Raymond EG, Grossman D, Weaver MA, Toti S, Winikoff B. Mortality of induced abortion, other outpatient surgical procedures and common activities in the United States. Contraception. 2014;90(5):476–479. doi: 10.1016/j.contraception.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Abortion Care Guideline. 2022. [Accessed June 27, 2022]. https://apps.who.int/iris/handle/10665/349316 . [PubMed]
- 27.National Abortion Federation. 2020 Clinical Policy Guidelines for Abortion Care. 2020. [Accessed June 27, 2022]. pp. 1–68. www.prochoice.org .
- 28.Robson SC, Kelly T, Howel D, et al. Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS) Health Technol Assess (Rockv) 2009;13(53):1–124. doi: 10.3310/hta13530. [DOI] [PubMed] [Google Scholar]
- 29.Grossman D, Grindlay K, Buchacker T, Lane K, Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol. 2011;118(2):296–303. doi: 10.1097/AOG.0b013e318224d110. [DOI] [PubMed] [Google Scholar]
- 30.Kerns J, Steinauer J. Management of postabortion hemorrhage Contraception. Contraception. 2013;87:331–342. doi: 10.1016/j.contraception.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 31.Rahangdale L. Infectious complications of pregnancy termination. Clin Obstet Gynecol. 2009;52(2):198–204. doi: 10.1097/GRF.0b013e3181a2b6dd. [DOI] [PubMed] [Google Scholar]
- 32.Eschenbach DA. Treating spontaneous and induced septic abortions. Obstet Gynecol. 2015;125(5):1042–1048. doi: 10.1097/AOG.0000000000000795. [DOI] [PubMed] [Google Scholar]
- 33.Yonke N, Leeman LM. First-trimester surgical abortion technique. Obstet Gynecol Clin North Am. 2013;40(4):647–670. doi: 10.1016/j.ogc.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 34.Chan YF, Ho PC, Ma HK. Blood loss in termination of early pregnancy by vacuum aspiration and by combination of mifepristone and gemeprost. Contraception. 1993;47(1):85–95. doi: 10.1016/0010-7824(93)90111-J. [DOI] [PubMed] [Google Scholar]
- 35.White K, Carroll E, Grossman D. Complications from first-trimester aspiration abortion: a systematic review of the literature. Contraception. 2015;92(5):422–438. doi: 10.1016/j.contraception.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 36.Creinin MD, Grossman DA. Medical management of first-trimester abortion. Contraception. 2014;89(3):148–161. doi: 10.1016/j.contraception.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Bryant AG, Regan E, Stuart G. An overview of medical abortion for clinical practice. Obstet Gynecol Surv. 2014;69(1):39–45. doi: 10.1097/OGX.0000000000000017. [DOI] [PubMed] [Google Scholar]
- 38.Wu YM, Gomez-Alzugaray M, Haukkamaa M, et al. Comparison of two doses of mifepristone in combination with misoprostol for early medical abortion: A randomised trial. BJOG An Int J Obstet Gynaecol. 2000;107(4):524–530. doi: 10.1111/j.1471-0528.2000.tb13273.x. [DOI] [PubMed] [Google Scholar]
- 39.Christin-Maitre S, Bouchard P, Spitz IM. Medical termination of pregnancy. In: Wood AJJ, editor. N Engl J Med. 13. Vol. 342. 2000. pp. 946–956. [DOI] [PubMed] [Google Scholar]
- 40.Hertzen H, Honkanen H, Piaggio G, et al. WHO multinational study of three misoprostol regimens after mifepristone for early medical abortion. I: Efficacy. BJOG An Int J Obstet Gynaecol. 2003;110(9):808–818. doi: 10.1111/j.1471-0528.2003.02430.x. [DOI] [PubMed] [Google Scholar]
- 41.Honkanen H, Piaggio G, Von Hertzen H, et al. WHO multinational study of three misoprostol regimens after mifepristone for early medical abortion. II: Side effects and women’s perceptions. BJOG An Int J Obstet Gynaecol. 2004;111(7):715–725. doi: 10.1111/j.1471-0528.2004.00153.x. [DOI] [PubMed] [Google Scholar]
- 42.Davis AR, Hendlish SK, Westhoff C, et al. Bleeding patterns after misoprostol vs surgical treatment of early pregnancy failure: results from a randomized trial. Am J Obstet Gynecol. 2007;196(1):31.e1–31.e7. doi: 10.1016/j.ajog.2006.07.053. [DOI] [PubMed] [Google Scholar]
- 43.Trinder J, Brocklehurst P, Porter R, Read M, Vyas S, Smith L. Management of miscarriage: Expectant, medical, or surgical? Results of randomised controlled trial (miscarriage treatment (MIST) trial) Br Med J. 2006;332(7552):1235–1238. doi: 10.1136/bmj.38828.593125.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kruse B, Poppema S, Creinin MD, Paul M. Management of side effects and complications in medical abortion. Am J Obstet Gynecol. 2000;183(2 Suppl):S65–S75. doi: 10.1067/MOB.2000.107946. [DOI] [PubMed] [Google Scholar]
- 45.Orlowski MH, Soares WE, Kerrigan KL, Zerden ML. Management of Postabortion Complications for the Emergency Medicine Clinician. Ann Emerg Med. 2021;77(2):221–232. doi: 10.1016/j.annemergmed.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 46.Co. GDS and. Cytotec® (misoprostol) Package Insert
- 47.Novartis. Methergine ® (methylergonovine maleate) Package insert
- 48.Pfizer. Hemabate ® carboprost tromethamine injection, package insert
- 49.WOMAN Trial Collaborators H. Roberts I, Fawole B, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet (London, England) 2017;389(10084):2105–2116. doi: 10.1016/S0140-6736(17)30638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vegas G, Illescas T, Munoz M. Selective pelvic arterial embolizationin the managemetn of obstetric hemorrhage. Eur J Obstet Gynecol Reprod Bio. 2006 Jul;127(1):68–72. doi: 10.1016/j.ejogrb.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 51.Steinauer JE, Diedrich JT, Wilson MW, Darney PD, Vargas JE, Drey EA. Uterine artery embolization in postabortion hemorrhage. Obstet Gynecol. 2008;111(4):881–889. doi: 10.1097/AOG.0B013E3181685780. [DOI] [PubMed] [Google Scholar]
- 52.Gonsalves M, Belli A. The role of interventional radiology in obstetric hemorrhage. Cardiovasc Intervent Radiol. 2010;33(5):887–895. doi: 10.1007/s00270-010-9864-4. [DOI] [PubMed] [Google Scholar]
- 53.Rooks J, Cates W., Jr Abortion methods: morbidity, costs and emotional impact. 3. Emotional impact of D&E vs. instillation - PubMed. [Accessed June 27, 2022];Fam Plann Perspect. 1977 9(6):277–277. https://pubmed.ncbi.nlm.nih.gov/923758/ [PubMed] [Google Scholar]
- 54.Cui R, Li M, Lu J, Bai H, Zhang Z. Management strategies for patients with placenta accreta spectrum disorders who underwent pregnancy termination in the second trimester: a retrospective study. BMC Pregnancy Childbirth. 2018;18(1) doi: 10.1186/S12884-018-1935-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wolman I, Altman E, Faith G, et al. Combined clinical and ultrasonographic work-up for the diagnosis of retained products of conception. Fertil Steril. 2009;92(3):1162–1164. doi: 10.1016/J.FERTNSTERT.2009.01.087. [DOI] [PubMed] [Google Scholar]
- 56.Dayananda I, Maurer R, Fortin J, Goldberg AB. Medical abortion follow-up with serum human chorionic gonadotropin compared with ultrasonography: a randomized controlled trial. Obstet Gynecol. 2013;121(3):607–613. doi: 10.1097/AOG.0B013E3182839FDA. [DOI] [PubMed] [Google Scholar]
- 57.Cowett AA, Cohen LS, Lichtenberg ES, Stika CS. Ultrasound evaluation of the endometrium after medical termination of pregnancy. Obstet Gynecol. 2004;103(5 Pt 1):871–875. doi: 10.1097/01.AOG.0000124782.69622.48. [DOI] [PubMed] [Google Scholar]
- 58.McEwing RL, Anderson NG, Meates JBA, Allen RB, Phillipson GTM, Wells JE. Sonographic appearances of the endometrium after termination of pregnancy in asymptomatic versus symptomatic women. J Ultrasound Med. 2009;28(5):579–586. doi: 10.7863/JUM.2009.28.5.579. [DOI] [PubMed] [Google Scholar]
- 59.Ben-Ami I, Schneider D, Maymon R, Vaknin Z, Herman A, Halperin R. Sonographic versus clinical evaluation as predictors of residual trophoblastic tissue. Hum Reprod. 2005;20(4):1107–1111. doi: 10.1093/HUMREP/DEH689. [DOI] [PubMed] [Google Scholar]
- 60.Abbasi S, Jamal A, Eslamian L, Marsousi V. Role of clinical and ultrasound findings in the diagnosis of retained products of conception. Ultrasound Obstet Gynecol. 2008;32(5):704–707. doi: 10.1002/uog.5391. [DOI] [PubMed] [Google Scholar]
- 61.Sawyer E, Ofuasia E, Ofili-Yebovi D, Helmy S, Gonzalez J, Jurkovic D. The value of measuring endometrial thickness and volume on transvaginal ultrasound scan for the diagnosis of incomplete miscarriage. Ultrasound Obstet Gynecol. 2007;29(2):205–209. doi: 10.1002/UOG.3914. [DOI] [PubMed] [Google Scholar]
- 62.Van Den Bosch T, Daemen A, Van Schoubroeck D, Pochet N, De Moor B, Timmerman D. Occurrence and outcome of residual trophoblastic tissue: a prospective study. J Ultrasound Med. 2008;27(3):357–361. doi: 10.7863/JUM.2008.27.3.357. [DOI] [PubMed] [Google Scholar]
- 63.Alcázar JL. Transvaginal ultrasonography combined with color velocity imaging and pulsed Doppler to detect residual trophoblastic tissue. Ultrasound Obstet Gynecol. 1998;11(1):54–58. doi: 10.1046/J.1469-0705.1998.11010054.X. [DOI] [PubMed] [Google Scholar]
- 64.Center for Disease Control. Ectopic pregnancy--United States, 1988–1989. [Accessed June 27, 2022];MMWR Morb Mortal Wkly Rep. 1992 41(32):591–594. https://pubmed.ncbi.nlm.nih.gov/1640927/ [PubMed] [Google Scholar]
- 65.Ulmann A, Silvestre L, Chemama L, et al. Medical termination of early pregnancy with mifepristone (RU 486) followed by a prostaglandin analogue. Study in 16,369 women. Acta Obstet Gynecol Scand. 1992;71(4):278–283. doi: 10.3109/00016349209021052. [DOI] [PubMed] [Google Scholar]
- 66.Edwards J, Carson SA. New technologies permit safe abortion at less than six weeks’ gestation and provide timely detection of ectopic gestation. Am J Obstet Gynecol. 1997;176(5):1101–1106. doi: 10.1016/S0002-9378(97)70410-1. [DOI] [PubMed] [Google Scholar]
- 67.Shannon C, Brothers LP, Philip NM, Winikoff B. Ectopic pregnancy and medical abortion. Obstet Gynecol. 2004;104(1):161–167. doi: 10.1097/01.AOG.0000130839.61098.12. [DOI] [PubMed] [Google Scholar]
- 68.Pontius E, Vieth JT. Complications in Early Pregnancy. Emerg Med Clin North Am. 2019;37(2):219–237. doi: 10.1016/J.EMC.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 69.Taran FA, Kagan KO, Hübner M, Hoopmann M, Wallwiener D, Brucker S. The Diagnosis and Treatment of Ectopic Pregnancy. Dtsch Arztebl Int. 2015;112(41):693–704. doi: 10.3238/ARZTEBL.2015.0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hendriks E, Rosenberg R, Prine L. Ectopic Pregnancy: Diagnosis and Management. [Accessed June 27, 2022];Am Fam Physician. 2020 101(10):599–606. https://pubmed.ncbi.nlm.nih.gov/32412215/ [PubMed] [Google Scholar]
- 71.Robertson JJ, Long B, Koyfman A. Emergency Medicine Myths: Ectopic Pregnancy Evaluation, Risk Factors, and Presentation. J Emerg Med. 2017;53(6):819–828. doi: 10.1016/J.JEMERMED.2017.08.074. [DOI] [PubMed] [Google Scholar]
- 72.Gentile GP, Siegler AM. Inadvertent intestinal biopsy during laparoscopy and hysteroscopy: a report of two cases. Fertil Steril. 1981;36(3):402–404. doi: 10.1016/S0015-0282(16)45746-8. [DOI] [PubMed] [Google Scholar]
- 73.Sullivan B, Kenney P, Seibel M. Hysteroscopic resection of fibroid with thermal injury to sigmoid. [Accessed June 27, 2022];Obs Gynecol. 1992 80(3 pt 2):546–547. https://pubmed.ncbi.nlm.nih.gov/1495733/ [PubMed] [Google Scholar]
- 74.Hefler L, Lemach A, Seebacher V, Polterauer S, Tempfer C, Reinthaller A. The intraoperative complication rate of nonobstetric dilation and curettage. Obstet Gynecol. 2009;113(6):1268–1271. doi: 10.1097/AOG.0B013E3181A66F91. [DOI] [PubMed] [Google Scholar]
- 75.Darney PD, Sweet RL. Routine intraoperative ultrasonography for second trimester abortion reduces incidence of uterine perforation. J Ultrasound Med. 1989;8(2):71–75. doi: 10.7863/jum.1989.8.2.71. [DOI] [PubMed] [Google Scholar]
- 76.Aydeniz B, Gruber IV, Schauf B, Kurek R, Meyer A, Wallwiener D. A multicenter survey of complications associated with 21,676 operative hysteroscopies. Eur J Obstet Gynecol Reprod Biol. 2002;104(2):160–164. doi: 10.1016/S0301-2115(02)00106-9. [DOI] [PubMed] [Google Scholar]
- 77.Agostini A, Cravello L, Bretelle F, Shojai R, Roger V, Blanc B. Risk of uterine perforation during hysteroscopic surgery. J Am Assoc Gynecol Laparosc. 2002;9(3):264–267. doi: 10.1016/S1074-3804(05)60401-X. [DOI] [PubMed] [Google Scholar]
- 78.Jansen FW, Vredevoogd CB, Van Ulzen K, Hermans J, Trimbos JB, Trimbos-Kemper TCM. Complications of hysteroscopy: a prospective, multicenter study. Obstet Gynecol. 2000;96(2):266–270. doi: 10.1016/S0029-7844(00)00865-6. [DOI] [PubMed] [Google Scholar]
- 79.Kaali SG, Szigetvari IA, Bartfai GS. The frequency and management of uterine perforations during first-trimester abortions. Am J Obstet Gynecol. 1989;161(2):406–408. doi: 10.1016/0002-9378(89)90532-2. [DOI] [PubMed] [Google Scholar]
- 80.Chen L, Lai S, Lee W, Leon N. Uterine perforation during elective first trimester abortions: a 13-year review. [Accessed June 27, 2022];Singapore Med J. 1995 36(1):63–67. https://pubmed.ncbi.nlm.nih.gov/7570139/ [PubMed] [Google Scholar]
- 81.Goyal V. Uterine rupture in second-trimester misoprostol-induced abortion after cesarean delivery: a systematic review. Obstet Gynecol. 2009;113(5):1117–1123. doi: 10.1097/AOG.0B013E31819DBFE2. [DOI] [PubMed] [Google Scholar]
- 82.Bhole S, Harris ME, Sistrom CL, Shifrin RY, Mulvihill MS, Moawad NS. Retained products of conception through a perforated uterine wall following elective abortion: a unique case report. Emerg Radiol. 2012;19(5):477–481. doi: 10.1007/S10140-012-1040-5. [DOI] [PubMed] [Google Scholar]
- 83.Chang HM, Shen CJ, Lin CY, Tsai EM. Uterine perforation and bowel incarceration following surgical abortion during the first trimester. Taiwan J Obstet Gynecol. 2008;47(4):448–450. doi: 10.1016/S1028-4559(09)60016-4. [DOI] [PubMed] [Google Scholar]
- 84.Istre O. Managing bleeding, fluid absorption and uterine perforation at hysteroscopy. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):619–629. doi: 10.1016/J.BPOBGYN.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 85.Tong S, Jeflfares J, Lopes R, Vollenhoven B. Delayed presentation of uterine perforation and haemorrhagic shock 10 days after surgical termination of pregnancy. Aust N Z J Obstet Gynaecol. 2001;41(3):335–336. doi: 10.1111/J.1479-828X.2001.TB01241.X. [DOI] [PubMed] [Google Scholar]
- 86.Shulman SG, Bell CL, Hampf FE. Uterine perforation and small bowel incarceration: sonographic and surgical findings. Emerg Radiol. 2006;13(1):43–45. doi: 10.1007/S10140-006-0499-3. [DOI] [PubMed] [Google Scholar]
- 87.Dignac A, Novellas S, Fournol M, Caramella T, Bafghi A, Chevallier P. Incarceration of the appendix complicating a uterine perforation following surgical abortion: CT aspects. Emerg Radiol. 2008;15(4):267–269. doi: 10.1007/S10140-007-0679-9. [DOI] [PubMed] [Google Scholar]
- 88.Coughlin LM, Sparks DA, Chase DM, Smith J. Incarcerated small bowel associated with elective abortion uterine perforation. J Emerg Med. 2013;44(3) doi: 10.1016/J.JEMERMED.2012.02.071. [DOI] [PubMed] [Google Scholar]
- 89.Derr C, Henry M. Bedside ultrasound in the diagnosis of uterine rupture following surgical abortion. Emerg Radiol. 2013;20(2):165–167. doi: 10.1007/S10140-012-1069-5. [DOI] [PubMed] [Google Scholar]
- 90.Del Gaizo AJ, Lall C, Allen BC, Leyendecker JR. From esophagus to rectum: a comprehensive review of alimentary tract perforations at computed tomography. Abdom Imaging. 2014;39(4):802–823. doi: 10.1007/S00261-014-0110-4. [DOI] [PubMed] [Google Scholar]
- 91.Singh JP, Steward MJ, Booth TC, Mukhtar H, Murray D. Evolution of imaging for abdominal perforation. Ann R Coll Surg Engl. 2010;92(3):182. doi: 10.1308/003588410X12664192075251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pouli S, Kozana A, Papakitsou I, Daskalogiannaki M, Raissaki M. Gastrointestinal perforation: clinical and MDCT clues for identification of aetiology. Insights Imaging. 2020;11(1) doi: 10.1186/S13244-019-0823-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.West AB. The pathology of diverticulitis. J Clin Gastroenterol. 2008;42(10):1137–1138. doi: 10.1097/MCG.0b013e3181862a9f. [DOI] [PubMed] [Google Scholar]
- 94.Lichtenberg ES. Complications of osmotic dilators. Obstet Gynecol Surv. 2004;59(7):528–536. doi: 10.1097/00006254-200407000-00022. [DOI] [PubMed] [Google Scholar]
- 95.Lachman E, Czernobilsky B, Ben-David M, Vlodavsky E, Lifschitz-Mercer B, Mammet Y. Prolonged retention of laminaria fragments: a rare complication of induced abortion. Obstet Gynecol. 2004;103(5 Pt 2):1128–1130. doi: 10.1097/01.AOG.0000125150.64300.DD. [DOI] [PubMed] [Google Scholar]
- 96.Nilsson W, Mikhael S, Kaplan J. Chronic Pelvic Pain and Infertility Resulting from Unrecognized Retained Laminaria. Case Rep Obstet Gynecol. 2017;2017:1–3. doi: 10.1155/2017/6345712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bernstein SN, Cudemus-Deseda GA, Ortiz VE, Goodman A, Jassar AS. Case 33-2019: A 35-Year-Old Woman with Cardiopulmonary Arrest during Cesarean Section. N Engl J Med. 2019;381(17):1664–1673. doi: 10.1056/NEJMCPC1904046. [DOI] [PubMed] [Google Scholar]
- 98.Benson MD. Amniotic fluid embolism mortality rate. J Obstet Gynaecol Res. 2017;43(11):1714–1718. doi: 10.1111/jog.13445. [DOI] [PubMed] [Google Scholar]
- 99.Fong A, Chau CT, Pan D, Ogunyemi DA. Amniotic fluid embolism: antepartum, intrapartum and demographic factors. J Matern Fetal Neonatal Med. 2015;28(7):793–798. doi: 10.3109/14767058.2014.932766. [DOI] [PubMed] [Google Scholar]
- 100.Kramer MS, Rouleau J, Baskett TF, Joseph K. Amniotic-fluid embolism and medical induction of labour: a retrospective, population-based cohort study. Lancet (London, England) 2006;368(9545):1444–1448. doi: 10.1016/S0140-6736(06)69607-4. [DOI] [PubMed] [Google Scholar]
- 101.Crissman HP, Loder C, Pancaro C, Bell J. Case report of amniotic fluid embolism coagulopathy following abortion; Use of viscoelastic point-of-care analysis. BMC Pregnancy Childbirth. 2020;20(1):1–7. doi: 10.1186/S12884-019-2680-1/FIGURES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Panda S, Das A, Sharma N, Das R, vinayak Jante D. Amniotic Fluid Embolism After First-Trimester Abortion. Cureus. 2022;14(4) doi: 10.7759/CUREUS.24490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fekhkhar K, Rachet B, Gillet R, et al. Amniotic fluid embolism during curettage for a pregnancy arrest. Case report. [Accessed June 28, 2022];Ann Fr Anesth Reanim. 2009 28(9):795–798. doi: 10.1016/j.annfar.2009.06.022. https://www.academia.edu/23616918/Embolie_amniotique_lors_d_un_curetage_pour_une_grossesse_arrêtée_À_propos_d_un_cas . [DOI] [PubMed] [Google Scholar]
- 104.Rudra A, Chatterjee S, Sengupta S, Nandi B, Mitra J. Amniotic fluid embolism. Indian J Crit Care Med. 2009;13(3):129. doi: 10.4103/0972-5229.58537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ray BK, Vallejo MC, Creinin MD, et al. Amniotic fluid embolism with second trimester pregnancy termination: a case report. Can J Anesth. 2004;51(2):139–144. doi: 10.1007/BF03018773. 512. [DOI] [PubMed] [Google Scholar]
- 106.Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-Related Mortality in the United States, 2011–2013. Obstet Gynecol. 2017;130(2):366–373. doi: 10.1097/AOG.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zane S, Creanga AA, Berg CJ, et al. Abortion-Related Mortality in the United States: 1998–2010. Obstet Gynecol. 2015;126(2):258–265. doi: 10.1097/AOG.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Clark SL, Romero R, Dildy GA, et al. Proposed diagnostic criteria for the case definition of amniotic fluid embolism in research studies. Am J Obstet Gynecol. 2016;215(4):408–412. doi: 10.1016/J.AJOG.2016.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moore J, Baldisseri MR. Amniotic fluid embolism. Crit Care Med. 2005;33(10 Suppl) doi: 10.1097/01.CCM.0000183158.71311.28. [DOI] [PubMed] [Google Scholar]
- 110.Kaur K, Bhardwaj M, Kumar P, Singhal S, Singh T, Hooda S. Amniotic fluid embolism. J Anaesthesiol Clin Pharmacol. 2016;32(2):153–159. doi: 10.4103/0970-9185.173356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Creel-Bulos C, Hassani B, Stentz MJ, et al. Extracorporeal Membrane Oxygenation for Amniotic Fluid Embolism-Induced Cardiac Arrest in the First Trimester of Pregnancy: A Case Report. Crit care Explor. 2020;2(7):e0162. doi: 10.1097/CCE.0000000000000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Adachi M, Adachi T, Fujita T, Hyuga S, Onishi Y, Okutomi T. Venoarterial extracorporeal membrane oxygenation as an early treatment for amniotic fluid embolism with cardiac arrest: A case report. J Obstet Gynaecol Res. 2021;47(9):3374–3378. doi: 10.1111/JOG.14880. [DOI] [PubMed] [Google Scholar]
- 113.Aissi James S, Klein T, Lebreton G, et al. Amniotic fluid embolism rescued by venoarterial extracorporeal membrane oxygenation. Crit Care. 2022;26(1) doi: 10.1186/s13054-022-03969-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Austin J, Ford MD, Rouse A, Hanna E. Acute intravaginal misoprostol toxicity with fetal demise. J Emerg Med. 1997;15(1):61–64. doi: 10.1016/S0736-4679(96)00257-0. [DOI] [PubMed] [Google Scholar]
- 115.Bentov Y, Sheiner E, Katz M. Misoprostol overdose during the first trimester of pregnancy. Eur J Obstet Gynecol Reprod Biol. 2004;115(1):108–109. doi: 10.1016/J.EJOGRB.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 116.Barros JG, Reis I, Graça LM. Acute misoprostol toxicity during the first trimester of pregnancy. Int J Gynaecol Obstet. 2011;113(2):157–158. doi: 10.1016/J.IJGO.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 117.Randall Bond G, Van Zee A. Overdosage of misoprostol in pregnancy. Am J Obstet Gynecol. 1994;171(2):561–562. doi: 10.1016/0002-9378(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 118.Graber DJ, Meier KH. Acute misoprostol toxicity. Ann Emerg Med. 1991;20(5):549–551. doi: 10.1016/S0196-0644(05)81614-2. [DOI] [PubMed] [Google Scholar]
- 119.Gottlieb M, Long B, Koyfman A. The Evaluation and Management of Toxic Shock Syndrome in the Emergency Department: A Review of the Literature. J Emerg Med. 2018;54(6):807–814. doi: 10.1016/J.JEMERMED.2017.12.048. [DOI] [PubMed] [Google Scholar]
- 120.Nikolic O, Nikolic MB, Dar Spasic A, Otero-Garcia MM, Stojanovic S. Systematic radiological approach to uteroovarian pathologies. Br J Radiol. 2019;92(1099) doi: 10.1259/BJR.20180439/SUPPL_FILE/BJR.20180439.SUPPL-01.DOCX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Scarvelis D, Malcolm I. Embolization of a huge tricuspid valve bacterial vegetation. J Am Soc Echocardiogr. 2002;15(2):185–187. doi: 10.1067/MJE.2002.118173. [DOI] [PubMed] [Google Scholar]
- 122.Andresen K, Balf D, Marcu CB. Images in cardiology: Massive pulmonary embolism in a patient with Streptococcus agalactiae tricuspid valve endocarditis. Heart. 2005;91(3):279. doi: 10.1136/hrt.2004.038828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Reardon DC. The abortion and mental health controversy: A comprehensive literature review of common ground agreements, disagreements, actionable recommendations, and research opportunities. SAGE open Med. 2018;6 doi: 10.1177/2050312118807624. 205031211880762. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


