Abstract
Background
In the Republic of Korea, a trauma care system was not created until 2012, at which point regional trauma centers (RTCs) were established nationwide. In accordance with the national emergency care system and legislation, regional and local emergency medical centers (EMCs) also treat patients presenting with trauma. The aim of the present study was to assess whether treatment in RTCs is truly associated with better patient outcomes than that in EMCs by means of propensity score-matched comparisons and to identify populations that would benefit from treatment in RTCs.
Methods
This study analyzed the data of patients with consecutive emergency visits between January 1, 2018, and December 31, 2018, collected in the National Emergency Department Information System registry. Data from RTCs, designated regional EMCs, or local EMCs were included; data from smaller emergency departments were excluded because, in Korea, dedicated RTCs are established only in hospitals with regional or local EMCs. Propensity scores for treatment in RTCs or EMCs were estimated by logistic regression using linear terms. Mortality rates in RTCs and EMCs were compared between the matched samples.
Results
The in-hospital mortality rates in the matched cases treated in RTCs and EMCs were 1.4% and 1.6%, respectively. The odds ratio for in-hospital mortality in RTCs over EMCs was 0.984 (95% confidence interval: 0.813–1.191). Among the subgroups evaluated, the subgroup of patients with injuries involving the chest or lower limbs showed a significant difference in the in-hospital mortality rate.
Conclusion
There was no significant difference in the overall severity-adjusted mortality rate between patients treated in RTCs and EMCs. Treatment in an RTC might benefit those with injuries involving the chest or lower limbs.
1. Background
Trauma is a major health problem worldwide, and injuries account for 8% of all deaths globally [1]. In many industrialized countries, including the US, designated trauma centers are crucial in providing care to injured victims [2]. However, in the Republic of Korea, it was not until 2012 that a trauma care system was created and trauma centers were established nationwide [3, 4]. As of 2021, 15 dedicated regional trauma centers (RTCs) have been officially operating. In accordance with the national emergency care system and legislation, regional and local emergency medical centers (EMCs) also treat patients presenting with trauma [4, 5].
There have been efforts to evaluate the performance of trauma systems in Korea by measuring the preventable trauma death rate (PTDR) [4, 6, 7]. The PTDR is generally defined as the proportion of all deaths judged to have been preventable if optimal care had been delivered [8]. The most recent study published in 2019 reported that RTCs had lower PTDRs than non-RTCs, such as EMCs [4]. If the quality of trauma care is truly inadequate, as claimed by PTDR studied to date, patients with major trauma should exclusively be transported to fully equipped trauma centers [9]. However, the capacity of RTCs in Korea is far from sufficient to cover the entire volume of patients with major trauma. Moreover, it has been reported that an exclusive trauma system is costly and not an effective model, even in developed countries [9]. In addition, the PTDR has inherent limitations in that it relies on subjective panel reviews, and reliability between different panel assessments may vary [10]. A comparison of PTDRs between studies conducted in different locations or different periods is known to be difficult and unreliable because the methodology of assessing and terminology for defining preventability is not standardized [8]. Moreover, the review panels in the PTDR study mostly comprised of specialists working in RTCs; therefore, the results may have been subject to a bias in the judgment of preventability [4].
The aim of the present study is to assess whether RTCs are associated with truly better outcomes by means of propensity score-matched comparisons and to identify populations that would benefit from treatment in RTCs rather than in EMCs.
2. Methods
2.1. Study Setting
The study investigated the difference in treatment results represented by in-hospital mortality of those treated in the RTCs compared with those treated in EMCs. RTCs are treatment facilities that include emergency treatment areas, intensive care units, wards, operating theatres, and radiology services dedicated to the care of trauma victims [3, 6]. Dedicated personnel for those facilities is required and receive government financial support [3, 4]. A general surgeon, thoracic surgeon, neurosurgeon, and the orthopedic surgeon must be assigned to the trauma team [4]. On the other hand, EMCs are designated to care for patients with generic emergency problems, including medical emergencies and poisonings, as well as injuries. EMCs are mainly staffed by emergency physicians, and surgeons usually participate in treatment as consultants. The operation of EMCs is less independent from the main hospital compared with RTCs.
2.2. Study Population
The study analyzed data from the National Emergency Department Information System (NEDIS) of the Republic of Korea, which is a nationwide database managed by the National Emergency Medical Center of Korea [11]. The NEDIS includes clinical and administrative data of patients who visited emergency departments (EDs) throughout the country; the government monitors these data and provides feedback to the hospitals regarding the quality of data entered into the database. The data are available to researchers upon request, and all identifying information is anonymized.
2.3. Inclusion and Exclusion Criteria
The study analyzed the data of patients with consecutive emergency visits between January 1, 2018, and December 31, 2018, in the NEDIS registry (reference number: N20190320311).
Trauma cases were defined as those for which the mechanism of injury was either a traffic accident, fall, strike by a person or object, firearm injury, cut or piercing injury, machine-induced injury, or other injuries, including assault.
Data from RTCs, designated regional emergency medical centers, or local emergency medical centers were included, while data from smaller EDs were excluded because dedicated RTCs are established in only hospitals with regional or local EMCs in Korea. At the end of 2018, thirteen RTCs around the country were operational, and the numbers of regional emergency medical centers and local emergency medical centers were 36 and 118, respectively.
Patients who were referred from other hospitals or outpatient departments, who were experiencing cardiac arrest at the time of arrival, and who were transferred from the emergency department as the final disposition were excluded. Children aged less than 15 years were excluded because normal ranges for vital signs are different from those of adults, and therefore, the National Early Warning Score used for the propensity score calculation is incompatible with children [12]. Patients with missing data regarding possible confounding variables used for propensity score calculation were also excluded (Figure 1).
Figure 1.
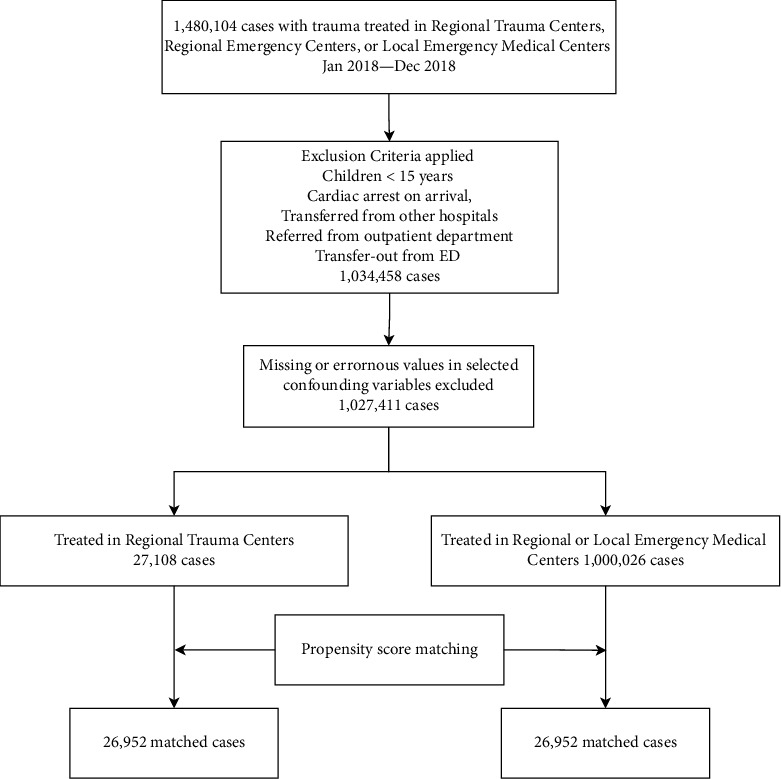
Flow diagram presenting the study population and cases matched for comparison.
2.4. Derivation of Survival Risk Ratios (SRRs) for Primary Diagnosis
A separate dataset of trauma cases treated in the emergency medical centers registered in the NEDIS between January 1, 2017, and December 31, 2017, was used for the derivation of SRRs for primary diagnosis as a representation of the diagnosis-based injury severity. The same exclusion criteria for the comparison of hospital mortality were applied, except for missing values with explanatory variables.
Primary diagnosis at the time of disposition from the ED, coded in the International Classification of Diseases, Revision 10 (ICD-10), was compressed into the first three digits. Cases were grouped by the primary diagnosis codes, and the SRR of each group was calculated as the number of survivors in the number of total cases in the group. The concept of SRR and the methodology was adopted from the studies regarding the International Classification of Disease-based Injury Severity Score (ICISS) [13–15].
2.5. Propensity Score Calculation and Matching
We considered injury mechanism; insurance status; intent; mode of transport; alert, voice, pain, and unresponsive (AVPU) scale score; the Korean Triage and Acuity Scale (KTAS) classification; anatomic area of injury; and vital signs on arrival, including systolic blood pressure, heart rate, respiratory rate, body temperature; and SRR of the primary diagnosis at the time of ED disposition, in the analysis of in-hospital mortality between those treated in RTCs and EMCs. Propensity scores for treatment in RTCs or EMCs were estimated by logistic regression using linear terms. Anatomic areas of injury were coded as dichotomous variables and categorized as head, neck, chest, abdomen-pelvis, upper limbs, and lower limbs according to the ICD-10, and patients with multiple injuries had multiple corresponding variables coded as “true.” ICD-10 codes between S00 and S99 were used to determine injury locations, and injury locations in cases without any of the aforementioned codes were classified as “unspecified.” Initial vital signs were scored according to the scheme used in the National Early Warning Score before being incorporated into the matching process to ensure linear correlation [12, 16]. Other parameters, including KTAS classification, were treated as categorical variables.
To create matched pairs, the nearest neighbor matching algorithm without replacement was used, with a caliper width of 0.01 standard deviation of the logit of the propensity score [17].
2.6. Comparison of Matched Mortality between the RTC and EMC Groups
Multivariate logistic regression analysis was applied in the matched samples to assess the effect of treatment in RTCs vs. EMCs on in-hospital mortality. Covariables used in the calculation of propensity scores were incorporated into the regression model to control small residual imbalances between the groups and thereby further enhance robustness [18, 19]. The odds ratios for in-hospital mortality treated in the RTCs over EMCs are presented with corresponding 95% confidence intervals and P values. A P value of less than 0.05 was considered statistically significant. Propensity score matching and comparison analyses were repeated in subgroups defined by injury severity represented by the primary diagnosis, which involved anatomic locations of injury and initial systolic blood pressure.
2.7. Statistical Software Used for Analysis
R version 4.1.3 (R Foundation for Statistical Computing, Vienna, Austria, 2022) was used for the statistical analyses. The package “MatchIt” was used for propensity score calculation and matching. The package “moonBook” was used for cross-tabulation, t-tests, and chi-square tests [20, 21].
2.8. Ethical Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki. The present study protocol was reviewed and approved by the Institutional Review Board of Dong-A University Hospital. Informed consent was waived by the Institutional Review Board of Dong-A University Hospital due to the retrospective nature of the study. (Approval No. DAUHIRB-EXP-21-065).
3. Results
3.1. Characteristics of the Study Subjects
A total of 2,963,362 patients presented to RTCs or EMCs during the study period and their data were extracted from the database. After applying the exclusion criteria, 23,215 patients in the RTC group and 700,809 patients in the EMC group were included in the analysis (Figure 1). Only 0.7% of cases that met the inclusion criteria were excluded because of missing data. The general characteristics of the study population are summarized in Table 1. The crude mortality rate in trauma victims treated in RTCs was 1.7%, while that in those treated in EMCs was 0.2%.
Table 1.
General characteristics of the study population and the propensity score-matched samples. Continuous variables were compared using the independent t-test, and categorical variables were compared using the chi-square test.
| Original study population | P value | Matched samples | P value | |||
|---|---|---|---|---|---|---|
| RTC (N = 27108) | EMC (N = 1000026) | RTC (N = 26694) | EMC (N = 26694) | |||
| Male sex | 17382 (64.1) | 566882 (56.7) | <0.001 | 17060 (63.9) | 15838 (59.3) | <0.001 |
| Age | 46.7 ± 19.1 | 46.3 ± 18.8 | 0.001 | 46.6 ± 19.1 | 46.8 ± 19.5 | 0.280 |
| Insurance type | <0.001 | 0.001 | ||||
| National health | 16520 (60.9) | 738396 (73.8) | 16468 (61.7) | 16789 (62.9) | ||
| Automobile | 6917 (25.5) | 168181 (16.8) | 6728 (25.2) | 6487 (24.3) | ||
| Occupational hazard | 548 (2.0) | 5960 (0.6) | 492 (1.8) | 521 (2.0) | ||
| Health aid type 1 | 821 (3.0) | 32408 (3.2) | 817 (3.1) | 860 (3.2) | ||
| Health aid type 2 | 248 (0.9) | 8922 (0.9) | 246 (0.9) | 275 (1.0) | ||
| Others | 46159 (4.6) | 2054 (7.6) | 1943 (7.3) | 1762 (6.6) | ||
| Mechanism | <0.001 | <0.001 | ||||
| Traffic car | 4487 (16.6) | 127319 (12.7) | 4424 (16.6) | 4071 (15.3) | ||
| Traffic bicycle | 864 (3.2) | 19894 (2.0) | 846 (3.2) | 909 (3.4) | ||
| Traffic motorcycle | 1626 (6.0) | 28134 (2.8) | 1555 (5.8) | 1543 (5.8) | ||
| Traffic others | 1845 (6.8) | 33091 (3.3) | 1745 (6.5) | 1683 (6.3) | ||
| Fall from heights | 2526 (9.3) | 51973 (5.2) | 2401 (9.0) | 2400 (9.0) | ||
| Fall from level | 5062 (18.7) | 201653 (20.2) | 5059 (19.0) | 5324 (19.9) | ||
| Struck by person or object | 5177 (19.1) | 179780 (18.0) | 5159 (19.3) | 5297 (19.8) | ||
| Firearm, cut, or pierce | 3776 (13.9) | 176449 (17.6) | 3766 (14.1) | 3693 (13.8) | ||
| Machine | 392 (1.4) | 14974 (1.5) | 386 (1.4) | 359 (1.3) | ||
| Others | 1353 (5.0) | 166759 (16.7) | 1353 (5.1) | 1415 (5.3) | ||
| Intent | <0.001 | <0.001 | ||||
| Accidental-unintentional | 25108 (92.6) | 926081 (92.6) | 24728 (92.6) | 24794 (92.9) | ||
| Intentional or self-harm | 511 (1.9) | 9032 (0.9) | 495 (1.9) | 557 (2.1) | ||
| Violence or assault | 1186 (4.4) | 46437 (4.6) | 287 (1.1) | 160 (0.6) | ||
| Others | 303 (1.1) | 18476 (1.8) | 1184 (4.4) | 1183 (4.4) | ||
| Mode of transport | <0.001 | 0.044 | ||||
| Ambulance | 13394 (49.4) | 289841 (29.0) | 12988 (48.7) | 12754 (47.8) | ||
| Others | 13714 (50.6) | 710185 (71.0) | 13706 (51.3) | 13940 (52.2) | ||
| Respiratory rate (min−1) | 19.2 ± 2.6 | 19.2 ± 2.2 | 0.268 | 19.1 ± 2.5 | 19.4 ± 3.2 | <0.000 |
| Pulse oxygen saturation (%) | 97.3 ± 4.0 | 97.9 ± 3.9 | <0.001 | 97.4 ± 3.7 | 97.6 ± 4.2 | 0.001 |
| Body temperature (°C) | 36.6 ± 0.5 | 36.5 ± 0.6 | <0.001 | 36.6 ± 0.6 | 36.6 ± 0.5 | 0.000 |
| Systolic blood pressure (mmHg) | 135.0 ± 24.0 | 134.8 ± 21.6 | 0.085 | 135.2 ± 23.7 | 135.5 ± 24.7 | 0.134 |
| Heart rate (min−1) | 85.3 ± 15.5 | 82.8 ± 13.6 | <0.001 | 85.0 ± 15.2 | 84.9 ± 15.6 | 0.395 |
| Responsiveness | <0.001 | 0.173 | ||||
| Alert | 24940 (92.0%) | 988403 (98.8%) | 24835 (93.0) | 24716 (92.6) | ||
| Response to voice | 1176 (4.3%) | 7826 (0.8%) | 1021 (3.8) | 1059 (4.0) | ||
| Response to pain | 789 (2.9%) | 3261 (0.3%) | 660 (2.5) | 733 (2.7) | ||
| Unresponsive | 203 (0.7%) | 536 (0.1%) | 178 (0.7) | 186 (0.7) | ||
| SRR of primary diagnosis | 0.99 ± 0.02 | 1.00 ± 0.01 | <0.001 | 0.99 ± 0.02 | 0.99 ± 0.02 | 0.041 |
| KTAS | <0.001 | <0.001 | ||||
| 1 | 517 (1.9) | 1064 (0.1) | 416 (1.0) | 430 (1.6) | ||
| 2 | 3684 (13.6) | 15387 (1.5) | 3372 (12.6) | 3527 (13.2) | ||
| 3 | 5160 (19.0) | 154128 (15.4) | 5159 (19.3) | 4622 (17.3) | ||
| 4 | 14459 (53.3) | 669423 (66.9) | 14459 (54.2) | 14830 (55.6) | ||
| 5 | 3288 (12.1) | 160024 (16.0) | 3288 (12.3) | 3285 (12.3) | ||
| Anatomic locations of injury | ||||||
| Head injury | 12874 (47.5) | 311749 (31.2) | <0.001 | 12528 (46.9) | 12707 (47.6) | 0.123 |
| Neck injury | 2532 (9.3) | 80550 (8.1) | <0.001 | 2478 (9.3) | 2043 (7.7) | <0.001 |
| Chest | 4341 (16.0) | 68075 (6.8) | <0.001 | 4030 (15.1) | 3614 (13.5) | <0.001 |
| Abdomen or pelvis | 3834 (14.1) | 100413 (10.0) | <0.001 | 3630 (13.6) | 3122 (11.7) | <0.001 |
| Upper limb | 6548 (24.2) | 273027 (27.3) | <0.001 | 6426 (24.1) | 6171 (23.1) | 0.010 |
| Lower limb | 5311 (19.6) | 213899 (21.4) | <0.001 | 5213 (19.5) | 4870 (18.2) | <0.001 |
| Unspecified | 3108 (11.5) | 174816 (17.5) | <0.001 | 3105 (11.6) | 3283 (12.3) | 0.018 |
| Number of involved anatomic locations of injury | 1.3 ± 1.0 | 1.0 ± 0.8 | <0.001 | 1.3 ± 1.0 | 1.2 ± 0.9 | <0.001 |
| Disposition from the ED | <0.001 | <0.001 | ||||
| Admission to ICU | 3830 (14.1) | 10462 (1.0) | 3471 (13.0) | 1819 (6.8) | ||
| Admission to ward | 4304 (15.9) | 4304 (15.9) | 4268 (16.0) | 3561 (13.3) | ||
| Admission to other units | 0 (0.0) | 22 (0.0) | 0 (0.0) | 1 (0.0) | ||
| Discharge | 18864 (69.6) | 872682 (87.3) | 18859 (70.7) | 21107 (79.1) | ||
| Hopeless discharge | 1 (0.0) | 24 (0.0) | 1 (0.0) | 3 (0.0) | ||
| Death | 31 (0.1) | 253 (0.0) | 17 (0.1) | 100 (0.4) | ||
| Others | 70 (0.3) | 3536 (0.4) | 70 (0.3) | 102 (0.4) | ||
RTC: regional trauma center; EMC: emergency medical center; SRR: survival risk ratio; KTAS: Korean Triage and Acuity Scale.
3.2. Propensity Score Matching
Propensity score matching resulted in 26,694 matched pairs, which included 99.4% of the original population treated in the RTCs and included in the matched sample group. Visual inspection of propensity score histograms revealed adequate overlapping propensity scores (Figure 2(a)), and the standard mean differences in each covariate were between −0.028 and 0.068 (Figure 2(b)). Absolute values of standardized mean differences below 0.1 to 0.25 are considered to represent an adequate balance. [18, 22] The general characteristics of the matched samples are summarized in Table 1.
Figure 2.
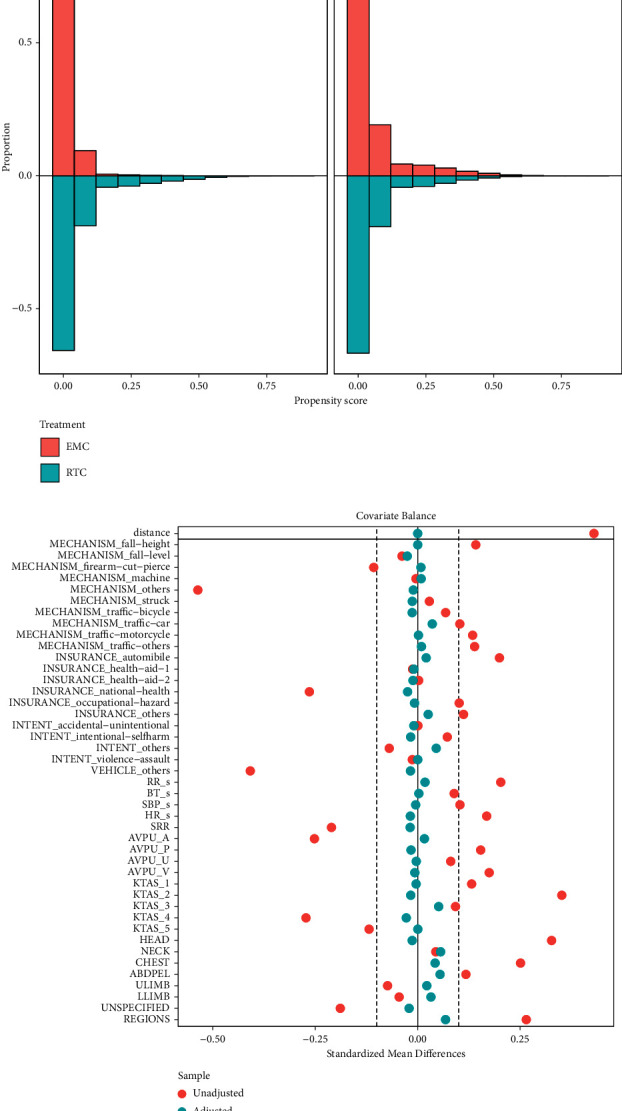
Graphs presenting balance statistics of the propensity matching. (a) Mirrored histogram showing the propensity score distribution in the original population and matched samples of trauma patients treated in regional trauma centers and emergency medical centers. (b) The Love plot shows changes in the standardized mean difference before (red) and after (blue) matching. EMC: emergency medical center; RTC: regional trauma center; RR: respiratory rate; BT: body temperature; SBP: systolic blood pressure; HR: heart rate; SRR: survival risk ratio of the primary diagnosis; AVPU: consciousness according to alert, verbal, painful, and unresponsive scale; KTAS: Korean Triage and Acuity Scale; ULIMB: upper limb; LLIMB: lower limb.
3.3. Primary Outcome
The in-hospital mortality rates in the matched patients treated in RTCs and EMCs were 1.4% and 1.6%, respectively. The difference was not statistically significant by multivariate logistic regression analysis (P = 0.870). The odds ratio for in-hospital mortality in RTCs over EMCs was 0.984 (95% CI; confidence interval: 0.813–1.191) (Figure 3).
Figure 3.
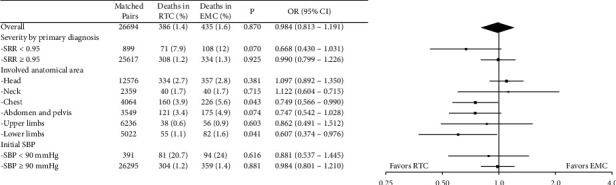
A Forest plot comparing the in-hospital mortality of matched cases treated in the regional trauma centers (RTC) and the emergency centers. An odds ratio below 1.0 indicates a more favorable result in the RTC. RTC: regional trauma center; EMC: emergency medical center; OR: odds ratio; SRR: survival risk ratio.
3.4. Subgroup Analysis
Propensity score matching was repeated for subgroups, and matched in-hospital mortality rates in the subgroups are summarized in Figure 3. Among the subgroups evaluated, the subgroup with injuries involving the chest or lower limbs showed a significant difference in the in-hospital mortality rate. Subgroups with more severe primary diagnoses or involving the abdomen or pelvis favored treatment in RTCs over EMCs, although a statistical significance could not be obtained.
4. Discussion
The study found that there was no significant difference in the overall mortality rate between the RTC and EMC groups when demographics and severity were matched. The crude mortality rate in trauma victims treated in RTCs was higher than that in those treated in EMCs; however, this result is suspected to be due to differences in the severity of trauma in patients treated in RTCs and EMCs because prehospital personnel are encouraged to transport severely injured patients to RTCs whenever possible. To objectively compare treatment results, scoring systems, such as the trauma and injury severity score (TRISS), have been developed, and the difference between actual mortality and predicted mortality based on the trauma score is represented by W or standardized W (Ws) statistics [23–25]. However, the TRISS requires that injuries be described in the Abbreviated Injury Scale (AIS) lexicon, which is an expensive step and applied in only a small number of hospitals, including RTCs, in Korea. [15] Because a score-based comparison of mortality between the RTC and EMC groups was not feasible, in-hospital mortality was compared between the propensity score-matched pairs. There was no significant difference between the two groups in in-hospital mortality after adjustment for trauma severity.
The PTDR is a concept used to compare the performance of trauma centers or to promote quality improvement within a trauma center [3, 26]. In Korea, the PTDR has been used as an indicator of trauma system performance at the national level since 2001; the PTDR is substantially higher than those in other developed countries, prompting the plan for trauma system improvement focused on the establishment of RTCs [6, 7, 27]. A recent study reported that non-RTC EMCs had higher PTDRs than RTCs (33.9% vs. 21.9%) and emphasized that trauma patients should urgently be transferred to RTCs [4]. However, there are concerns regarding the reliability of the PTDR. The definition of preventability has not been standardized and differs among studies [8, 28, 29]. Although the World Health Organization (WHO) recommends the utilization of the injury severity score (ISS) and the calculation of the probability of survival in the panel review process, not every study that employed the PTDR utilized objective estimates of survival in determining preventability [8, 10, 30]. Additionally, the possibility of bias in favor of treatment in RTCs cannot entirely be eliminated when review panels comprise people who work in RTCs and review processes are not blind, even though the panels include multidisciplinary experts [3, 4, 31].
Although the WHO recommends preventable death panel review as an essential part of the quality improvement process in a trauma system or an organization, the purpose of the multidisciplinary panel review is to identify potential areas of improvement for future patient care and not to compare a system or organization against national or international norms [10, 32]. An important caveat of PTDR in comparing performance is that PTDR only considers death cases and ignores the number of survivors. Montmany et al. compared the quality of care at a typical American trauma center and an equivalent European referral center in Spain [33]. Although the overall death rate was lower and ISS was higher in the Spanish center, higher PTDR was reported in the Spanish center (14.3%) than in the US trauma center. (7.7%) Among methods of comparing the performance of trauma systems, including PTDR, registry-based studies, and population-based studies, population-based studies are considered to provide the strongest evidence regarding the effect of trauma systems and trauma centers on patient outcomes [34].
Previous studies on the PTDR in Korea have emphasized that severely injured patients should be directly transferred to RTCs [4, 9]. However, it is impossible to transport every trauma victim to an RTC, considering that the number of RTCs in Korea was only 15 in 2022, and their capacity is limited. Moreover, there is substantial evidence that an inclusive trauma system in which hospitals other than RTCs or level I trauma centers participate in trauma care would improve inpatient survival [35–37].
For an inclusive trauma system to operate effectively, patients who would most likely benefit from treatment in an RTC should be identified. Therefore, subgroup analysis was performed, and we found that the in-hospital mortality rates due to injuries involving the chest, abdomen, pelvis, or lower extremities were significantly different between the RTC and EMC groups. The major difference between RTCs and EMCs is the presence of dedicated trauma teams and facilities dedicated to victims of major trauma, which enables resuscitative thoracotomy and laparotomy within a very short time from patient arrival and contributes to better survival in patients with abdominal and pelvic injuries [4]. Additionally, the ability to rapidly initiate the massive transfusion protocol and the early availability of angioembolization would have contributed in better results with those injuries in which hemorrhage is the major mechanism of death. However, initial stabilization by emergency physicians and subsequent definitive treatment by surgeons in EMCs also resulted in favorable outcomes in patients with traumatic injuries to the head and neck. Therefore, it could be suggested that when designing an inclusive trauma system, those with the possibility of severe hemorrhage would have the highest priority for transfer to an RTC, while others, especially those with injuries to the head and neck, could be triaged to EMCs according to injury severity.
Although vital signs, injury mechanisms, primary diagnoses, and anatomic locations of injuries were considered during the propensity score matching process, specific descriptions of injuries and detailed diagnoses could not be taken into consideration. The study intended to compare treatment results between RTCs and EMCs at the national level, but formal trauma scores, such as the TRISS, were not available in the national database. Instead, we reflected the severity of injury represented by the SRR of their primary diagnosis, a concept adopted from the ICD-based Injury Severity Score (ICISS) [15]. The employment of full-scale ICISS was limited because it would require a larger dataset and more thorough validation of the scoring system. However, the approach applied in the study enabled the objective comparison of in-hospital mortality at the national level, unlike previous research that utilized the PTDR. Moreover, the missing data rate was only 0.7%, and 99.4% of RTC cases in the original population could find an appropriate match in the control population. Therefore, the issues regarding selection bias would not be a significant concern.
5. Conclusion
There was no significant difference in the overall severity-adjusted mortality rate between the RTC and EMC groups. Treatment in an RTC might benefit those with injuries involving the chest or lower extremities, while other patients could be successfully managed in EMCs without compromising safety.
Acknowledgments
The study was supported by the Dong-A University Research Fund.
Abbreviations
- RTC:
Regional trauma center
- EMC:
Emergency medical center
- PTDR:
Preventable trauma death rate
- NEDIS:
National Emergency Department Information System
- ED:
Emergency department
- AVPU:
Alert, voice, pain, unresponsive (AVPU) scale score
- KTAS:
The Korean Triage and Acuity Scale
- TRISS:
Trauma Injury Severity Score
- WHO:
World Health Organization
- ISS:
Injury Severity Score
- ICISS:
International Classification Of Disease-Based Injury Severity Score.
Data Availability
The data that support the findings of this study are available from the National Emergency Medical Center of the Republic of Korea. Interested researchers can contact the department maintaining the database via mail (bigdata@nmc.or.kr).
Ethical Approval
The present study protocol was reviewed and approved by the Institutional Review Board of Dong-A University Hospital.
Consent
Informed consent was waived by the Institutional Review Board of Dong-A University Hospital due to the retrospective nature of the study. (Approval No. DAUHIRB-EXP-21-065).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Conceptualization was done by Lee SW. Methodology was performed by Jeong J and Kim SJ. Validation was done by Kim WY and Kang H. Formal analysis was done by Jeong J and Yuri Choi Y. Data curation was done by Han KS and Hong ES. Choi Y and Jeong J wrote the original draft. Lee SW, Kim WY, Kang H, Kim SJ, Han KS, and Hong ES reviewed the manuscript.
References
- 1. Injuries and Violence World Health Organization . 2021. https://www.who.int/news-room/fact-sheets/detail/injuries-and-violence . [Google Scholar]
- 2.Schubert F. D., Gabbe L. J., Bjurlin M. A., Renson A. Differences in trauma mortality between ACS-verified and state-designated trauma centers in the US. Injury . 2019;50(1):186–191. doi: 10.1016/j.injury.2018.09.038. [DOI] [PubMed] [Google Scholar]
- 3.Huh Y., Kwon J., Moon J., et al. An evaluation of the effect of performance improvement and patient safety program implemented in a new regional trauma center of Korea. Journal of Korean Medical Science . 2021;36(22) doi: 10.3346/jkms.2021.36.e149.e149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jung K., Kim I., Park S. K., et al. Preventable trauma death rate after establishing a national trauma system in Korea. Journal of Korean Medical Science . 2019;34(8):p. e65. doi: 10.3346/jkms.2019.34.e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang S. O., Lee C. C., Kim T. M., Singer A. J. The current status of the emergency medical system in Korea. The American Journal of Emergency Medicine . 2007;25(7):846–848. doi: 10.1016/j.ajem.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 6.Yoon H. D. Background and progress of regional trauma center development. Journal of the Korean Medical Association . 2016;59(12):p. 919. doi: 10.5124/jkma.2016.59.12.919. [DOI] [Google Scholar]
- 7.Kim Y., Jung K. Y., Cho K. H. Preventable trauma deaths rates and management errors in emergency medical system in Korea. Journal of The Korean Society of Emergency Medicine . 2006;17:385–394. [Google Scholar]
- 8.Oliver G. J., Walter D. P. A call for consensus on methodology and terminology to improve comparability in the study of preventable prehospital trauma deaths: a systematic literature review. Academic Emergency Medicine . 2016;23(4):503–510. doi: 10.1111/acem.12932. [DOI] [PubMed] [Google Scholar]
- 9.Paydar S., Ghahramani Z., Bolandparvaz S., et al. Exclusive versus inclusive trauma system model in high volume trauma regions. Bulletin of Emergency and Trauma . 2018;6(4):269–270. doi: 10.29252/beat-060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mock C., Juillard C., Brundage S., Goosen J. Guidelines for Trauma Quality Improvement Programmes . Geneva, Switzerland: WHO Press; 2009. [Google Scholar]
- 11.Kim J. S., Seo D. W., Kim Y. J., et al. Prolonged length of stay in the emergency department and increased risk of in-hospital cardiac arrest: a nationwide population-based study in South Korea, 2016-2017. Journal of Clinical Medicine . 2020;9(7):p. 2284. doi: 10.3390/jcm9072284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prytherch D. R., Smith G. B., Schmidt P. E., Featherstone P. I. ViEWS—towards a national early warning score for detecting adult inpatient deterioration. Resuscitation . 2010;81(8):932–937. doi: 10.1016/j.resuscitation.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Wong S. S. N., Leung G. K. K. Injury severity score (ISS) vs. ICD-derived injury severity score (ICISS) in a patient population treated in a designated Hong Kong trauma centre. McGill Journal of Medicine . 2020;11(1):9–13. doi: 10.26443/mjm.v11i1.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim Y., Jung K. Y., Kim C. Y., Kim Y. I., Shin Y. Validation of the international classification of diseases 10th edition-based injury severity score (ICISS) The Journal of Trauma, Injury, Infection, and Critical Care . 2000;48(2):280–285. doi: 10.1097/00005373-200002000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Osler T., Rutledge R., Deis J., Bedrick E. ICISS: an international classification of disease-9 based injury severity score. The Journal of Trauma, Injury, Infection, and Critical Care . 1996;41(3):380–388. doi: 10.1097/00005373-199609000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Jones M. NEWSDIG: the national early warning score development and implementation group. Clinical Medicine . 2012;12(6):501–503. doi: 10.7861/clinmedicine.12-6-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Austin P. C. A comparison of 12 algorithms for matching on the propensity score. Statistics in Medicine . 2014;33(6):1057–1069. doi: 10.1002/sim.6004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benedetto U., Head S. J., Angelini G. D., Blackstone E. H. Statistical primer: propensity score matching and its alternatives. European Journal of Cardio-Thoracic Surgery . 2018;53(6):1112–1117. doi: 10.1093/ejcts/ezy167. [DOI] [PubMed] [Google Scholar]
- 19.Zhao Q. Y., Luo J. C., Su Y., Zhang Y. J., Tu G. W., Luo Z. Propensity score matching with R: conventional methods and new features. Annals of Translational Medicine . 2021;9:p. 812. doi: 10.21037/atm-20-3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moon K. W. R Statistics and Graphs for Medical Papers . Seoul, Republic of Korea: Hannarae; 2015. [Google Scholar]
- 21.Daniel E. H., Kosuke I., Gary K., Elizabeth A. S. MatchIt: nonparametric preprocessing for parametric causal inference. Journal of Statistical Software . 2011;42:1–28. [Google Scholar]
- 22.Garrido M. M., Kelley A. S., Paris J., et al. Methods for constructing and assessing propensity scores. Health Services Research . 2014;49(5):1701–1720. doi: 10.1111/1475-6773.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hollis S., Yates D. W., Woodford M., Foster P. Standardized comparison of performance indicators in trauma: a new approach to case-mix variation. The Journal of Trauma, Injury, Infection, and Critical Care . 1995;38(5):763–766. doi: 10.1097/00005373-199505000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Jeong J., Lee S. W., Kim W. Y., Han K. S., Kim S. J., Kang H. Development and validation of a scoring system for mortality prediction and application of standardized W statistics to assess the performance of emergency departments. BMC Emergency Medicine . 2021;21(1):p. 71. doi: 10.1186/s12873-021-00466-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim O. H., Roh Y. I., Kim H. I., et al. Reduced mortality in severely injured patients using hospital-based helicopter emergency medical services in interhospital transport. Journal of Korean Medicine Science . 2017;32(7):1187–1194. doi: 10.3346/jkms.2017.32.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koh E. Y., Oyeniyi B. T., Fox E. E., et al. Trends in potentially preventable trauma deaths between 2005-2006 and 2012-2013. The American Journal of Surgery . 2019;218(3):501–506. doi: 10.1016/j.amjsurg.2018.12.022. [DOI] [PubMed] [Google Scholar]
- 27.Jung K. Y., Kim J. S., Kim Y. Problems in trauma care and preventable deaths. Journal of The Korean Society of Emergency Medicine . 2001;12:45–56. [Google Scholar]
- 28.MacKenzie E. J. Review of evidence regarding trauma system effectiveness resulting from panel studies. The Journal of Trauma, Injury, Infection, and Critical Care . 1999;47:S34–S41. doi: 10.1097/00005373-199909001-00008. [DOI] [PubMed] [Google Scholar]
- 29.Hakkenbrak N. A. G., Mikdad S. Y., Zuidema W. P. Preventable death in trauma: a systematic review on definition and classification. Injury . 2021 doi: 10.1016/j.injury.2021.07.040. [DOI] [PubMed] [Google Scholar]
- 30.Moon S., Lee S. H., Ryoo H. W., et al. Preventable trauma death rate in Daegu, South Korea. Clinical and Experimental Emergency Medicine . 2015;2(4):236–243. doi: 10.15441/ceem.15.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwon J., Lee J. H., Hwang K., et al. Systematic preventable trauma death rate survey to establish the region-based inclusive trauma system in a representative province of Korea. Journal of Korean Medical Science . 2020;35(50) doi: 10.3346/jkms.2020.35.e417.e417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mock C., Lormand J. D., Goosen J., Joshipura M. Guidelines for Essential Trauma Care . Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 33.Montmany S., Pascual J. L., Kim P. K., et al. American vs. European trauma centers: a comparison of preventable deaths. Cirugía Española . 2017;95(8):457–464. doi: 10.1016/j.cireng.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 34.Chiara O., Cimbanassi S., Pitidis A., Vesconi S. Preventable trauma deaths: from panel review to population based-studies. World Journal of Emergency Surgery: WJES . 2006;1:p. 12. doi: 10.1186/1749-7922-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKee J. L., Roberts D. J., van Wijngaarden-Stephens M. H., et al. The right treatment at the right time in the right place: a population-based, before-and-after study of outcomes associated with implementation of an all-inclusive trauma system in a large Canadian province. Annals of Surgery . 2015;261(3):558–564. doi: 10.1097/sla.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 36.Vanni A. J., Hotaling J., Hamlat C., Jurkovich G. J., Voelzke B. B. Do inclusive trauma systems improve outcomes after renal trauma? Journal of Trauma and Acute Care Surgery . 2012;72(2):385–389. doi: 10.1097/ta.0b013e3182411c67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moore L., Champion H., Tardif P. A., et al. Impact of trauma system structure on injury outcomes: a systematic review and meta-analysis. World Journal of Surgery . 2018;42(5):1327–1339. doi: 10.1007/s00268-017-4292-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the National Emergency Medical Center of the Republic of Korea. Interested researchers can contact the department maintaining the database via mail (bigdata@nmc.or.kr).


