Abstract
Sarcopenia, an age-associated skeletal muscle disorder characterized by muscle loss, is associated with disability in elderly populations. This literature review summarizes the impact of protein intake and supplementation on the indicators of severe sarcopenia—muscle mass, muscle strength, and physical function in community-dwelling older adults. We performed a literature search on PubMed, EMBASE, and MedLine, and included studies that evaluated the effects of protein intake with or without exercise intervention and on sarcopenia in community-dwelling older adults. Information regarding study participants, protein intervention, and sarcopenia-related outcomes were collected. Protein supplementation with or without exercise positively improves muscle mass, and aspects of muscle strength and physical function in sarcopenic and pre-frail older adults, while it elicited inconclusive effects in healthy populations. Greater dietary animal-based and soy-based protein diets can improve muscle mass in older adults. In conclusion, protein supplementation can improve muscle mass and reduce the risk of sarcopenia in sarcopenia and pre-frail older adults, while future studies should continue to investigate the effects of protein supplementation on indicators of sarcopenia in healthy older adults.
Keywords: sarcopenia, community-dwelling, older adults, dietary protein intake
INTRODUCTION
Sarcopenia is characterized by age-associated, progressive loss of muscle mass and physical function.(1) The European Working Group on Sarcopenia in Older People and the International Working group on Sarcopenia define severe sarcopenia as having lower skeletal muscle mass, muscle mass, and physical strength.(1) Previous research has demonstrated a higher prevalence of sarcopenia in older adults, due to decreasing hormonal activation, inadequate physical activity and nutrition, and lower neuromuscular junctional activity.(2–4) In fact, older adults over the age of 80 may lose up to 50% of their muscle mass.(2,3) Sarcopenia also acts as a significant determinant of disability: it increases the risk of falls, fractures, and mobility disorders, and is also correlated with higher risks of cognitive impairment and cardiometabolic comorbidities.(5,6)
There are no currently approved medications for sarcopenia treatment.(7) Instead, non-pharmacological therapies are often associated with the attenuation of muscle loss and improvements in muscle size and strength in older adults.(8) As reduced exercise capacity and higher prevalence of malnutrition is linked with older adults, an increasing number of studies report the impact of nutritional improvement and exercise intervention on sarcopenia, with the primary focus on protein supplementation with or without resistance exercise training.(8,9) From the current literature, multiple forms of protein intake interventions, with or without exercise intervention, are evaluated for their effects to attenuate muscle loss in the elderly population, including amino supplementation, whey protein intake, and an increase in an animal and protein-rich diet.(9) Therefore, this review aims to evaluate and provide a summary of evidence of dietary protein intake and protein supplementation and its effects on sarcopenia and the preservation of muscle mass, strength, and function in the community-dwelling elderly population.
METHODOLOGY AND SEARCH STRATEGY
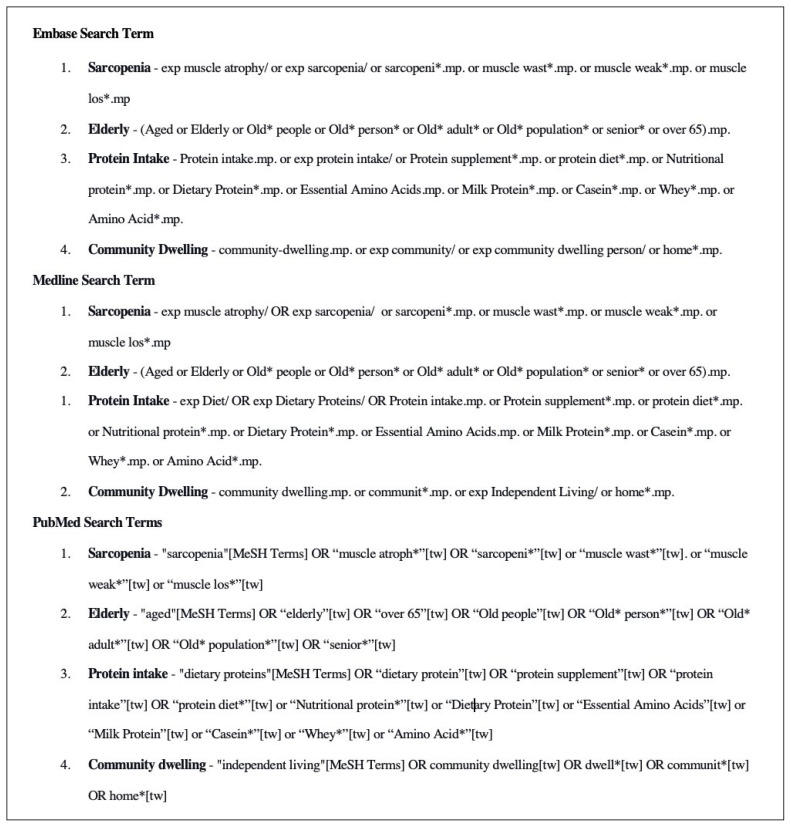
For this literature review, we performed searches on the impact of protein supplementation in community-dwelling older adults within PubMed, EMBASE, and MEDLINE databases from 1975 to 2020. Please see Figure 1 for the search terms.
FIGURE 1.
Search terms for literature review assessing the effects of dietary protein intake on saropenia in community-dwelling older adults
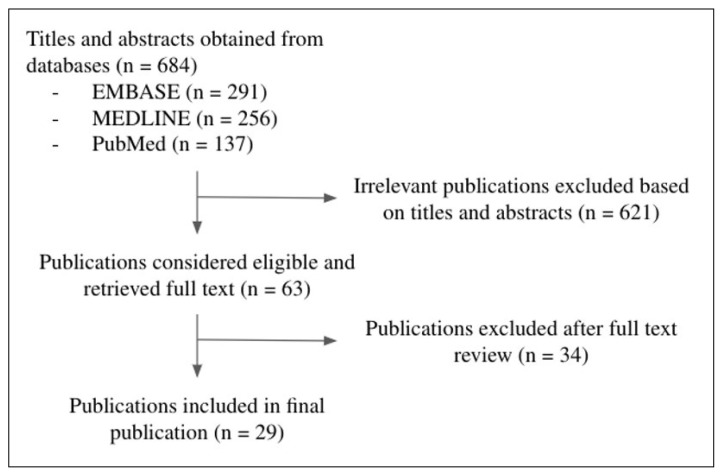
The titles and abstracts of the studies selected were screened. We included studies that evaluated the effects of increased dietary protein or any form of protein supplement, with or without other interventions, in improving the metrics of severe sarcopenia. Conference abstracts and studies that did not provide data on muscle mass, strength, or physical performance were excluded. Please see Figure 2 for the literature search flowchart.
FIGURE 2.
Literature search flowchart for review assessing the effects of dietary protein intake on saropenia in community-dwelling older adults
After study selection, we extracted the following data: patient population, sample size, intervention, and sarcopenia-related outcomes (muscle mass, strength, and physical performance). Specifically, muscle mass was reported as total and appendicular lean mass, skeletal muscle index, or cross-sectional muscle area. Muscle strength was assessed based on parameters such as handgrip strength and knee extension strength. Physical performance was reported either as a Short Physical Performance Battery (SPPB) (balance, chair stand, and gait speed) or other tests including stair climb and timed-up-and-go.
RESULTS
Overall, our literature search yielded 29 studies including 19 randomized control trials, six prospective cohort studies, and four cross-sectional studies. The study populations of the 29 studies were heterogeneous, ranging from healthy, sarcopenic, pre-frail, obese, and diabetic participants. The major categories of interventions and variables assessed include amino acid and whey protein supplementation alone, nutritional supplementation combined with exercise intervention or electromyostimulation, and dietary protein supplement/dietary pattern assessment.
Protein/Amino Acid Supplementation
Six studies assessed the effect of unimodal protein supplementation on indicators of sarcopenia in community-dwelling older adults (Table 1). Three studies evaluated the effect of amino acid supplementation on muscle mass, muscle strength, and physical function. Solerte et al. assessed the effect of daily amino acid supplementation in sarcopenic older adults and found significant improvements in whole-body, arm, and leg lean mass, to the average values found in age-appropriate non-sarcopenic healthy controls after 16 months.(10) Similarly, Peng et al. discovered that 12 weeks of daily amino acid supplementation significantly improves mid-thigh cross-sectional area in pre-frail older adults compared to control participants, with no effects in handgrip strength and SPPB.(11) Lastly, a randomized controlled trial by Ellis et al. found that 16 weeks of amino acid supplementation can significantly improve total lean body mass and timed stair climb in healthy community-dwelling elderly participants compared to the control intervention.(12) However, they found no significant differences in quadriceps muscle volume or other physical functional tests, including gait speed and timed up-and-go test.(12)
TABLE 1.
Studies with unimodal protein/amino acid supplementation
| Studies | Study Type | Population | Intervention / Independent Variables | Outcomes |
|---|---|---|---|---|
| Solerte et al. 200810 | RCT (cross-over study) | 41 elderly Italian sarcopenic older adults, aged 66–84 | 16 months Group A (n=19): 4 months of amino acid supplement (8g - leucine, lysine, isoleucine, and valine), 4 months of isocaloric placebo, followed by 8 months of amino acid supplement Group B (n=22): 4 months of isocaloric placebo, followed by 4 months of amino acid supplement, followed by 8 months of amino acid of amino acid supplement |
Both groups of sarcopenic participants experienced a significant increase in whole-body lean mass, arm, and leg lean mass after 8 and 16 months of intervention (p<.001). Participants reached the average values found in age-matched non-sarcopenic healthy controls at the end of the 16 months. |
| Peng et al. 202111 | RCT | 62 pre-frail Taiwanese older persons aged 65–80 | 12 weeks Group A (n=33): 6g of HMB (β-hydroxy-β-methylbutyrate) daily Group B (n=29) - Professional nutritional counselling |
Group A had significantly higher in mid-thigh cross-sectional area MRI (149.10 ± 272.29 vs. −22.90 ± 309.09 mm2, p =.045) No significant improvements in muscle strength (handgrip strength) and physical function (SPPB, gait speed) |
| Ellis et al. 201912 | RCT | 31 US ambulatory, community-dwelling older adult aged 65 yrs and older | 6 months Group A (n=15): Two daily doses of the supplement provided a total of 3 g HMB, 14 g L-arginine, and 14 g L-glutamine in the experimental group Group B (n=16): calorically similar placebo |
Group A had significantly greater total lean body mass (52.9 ± 11.9 vs. 48.4 ± 11.4 kg, p = .036) and timed stair climb (4.61 ± 0.80 s vs. 4.86 ± 1.66, p = .016). No significant differences in quadriceps muscle volume or other physical functional tests including gait speed and timed up-and-go test. |
| Kang et al. 202013 | RCT | 111 healthy community-dwelling adults aged 50–80 from South Korea | 12 weeks Group A (n= 54): Protein mixture powder - [protein 20 g (casein 50%+ whey 40%+ soy 10%, total leucine 3000 mg), vitamin D 800 IU(20 g), calcium 300 mg, fat 1.1 g, carbohydrate 2.5 g), twice daily Group B (n=57): exercise brochure |
Total lean body mass percentage (lean body mass / body weight) was only significantly increased in Group A in the 50–64 age group, but not in older adults aged over 65. No significant differences in appendicular skeletal muscle, muscle strength (grip strength or femoral muscle strength), or physical function (SPPB) |
| Chanet et al. 201714 | RCT | 24 healthy French older adults aged >65 yr with a BMI (in kg/m2) between 20 and 30 | 6 weeks Group A (n=12): vitamin D and leucine-enriched whey protein drink (20 g whey protein, 3 g leucine, 9 g carbohydrates, 3 g fat, and 800 IU cholecalciferol) Group B (n=12): isocaloric placebo before breakfast |
Participants in Group A had significantly higher appendicular and leg lean mass compared to group B (Estimated difference (ED): 0.37 kg; 95% CI: 0.03 – 0.72 kg; p = .035 and ED: 0.30 kg; 95% CI: 0.03, 0.57 kg; p = .034). No significant between-group differences in body weight, total lean body mass, arm lean mass, handgrip strength, and SPPB. |
| Zhu et al. 201515 | RCT | 196 healthy Australian women aged 70–80 years old | 2 years Group A (n=101): 250 mL skim milk–based high-protein supplement drink, consisting of 30 g of whey protein, 600 mg of calcium, and 3.2 kJ/mL Group B (n=95): placebo only (2.1 g of protein, 600 mg of Ca, 3.2 kJ/mL) |
No significant differences in muscle mass (appendicular skeletal muscle mass, upper/lower limb cross-sectional muscle area), muscle strength (handgrip and knee extension/flexion), and physical function (timed up-and-go test) between groups |
Three studies evaluated the effect of whey protein supplementation on muscle mass, muscle strength, and physical function. Through a randomized controlled trial, Kang et al. reported that 20 g of protein supplementation for 12 weeks only significantly improved total lean mass in healthy adults aged 50–64, but had no effects on muscle mass in participants >65 years old.(13) Furthermore, protein supplementation did not significantly improve muscle strength (grip strength or femoral muscle strength) or the SPPB.(13) On the other hand, Chanet et al. found that daily leucine-enriched whey protein medical nutrition drink can significantly improve higher appendicular and leg lean mass in healthy older adults.(14) However, there were no important between-group differences in total lean body mass, handgrip strength, and SPPB outcomes.(14) Lastly, Zhu et al. reported that two years of whey protein supplementation did not result in significant differences in muscle mass (appendicular skeletal muscle mass, upper/lower limb cross-sectional muscle area), muscle strength (handgrip and knee extension/flexion), and physical function (timed up and go test) in healthy older adults compared with isocaloric placebo intervention.(15)
The results suggest that amino acid supplementation effectively improves multiple aspects of muscle mass, including total-body, arm, and leg lean mass, in sarcopenic and pre-frail older adults over 3 to 16 months. However, amino acid supplementation had no significant effects on muscle strength and most aspects of physical function. In comparison, there are mixed findings regarding the effect of whey protein supplementation on muscle mass in community-dwelling elderly. However, whey protein alone is unlikely to induce any positive benefits in muscle strength and physical function in the healthy elderly population.
Nutritional Supplementation with Exercise and Other Interventions
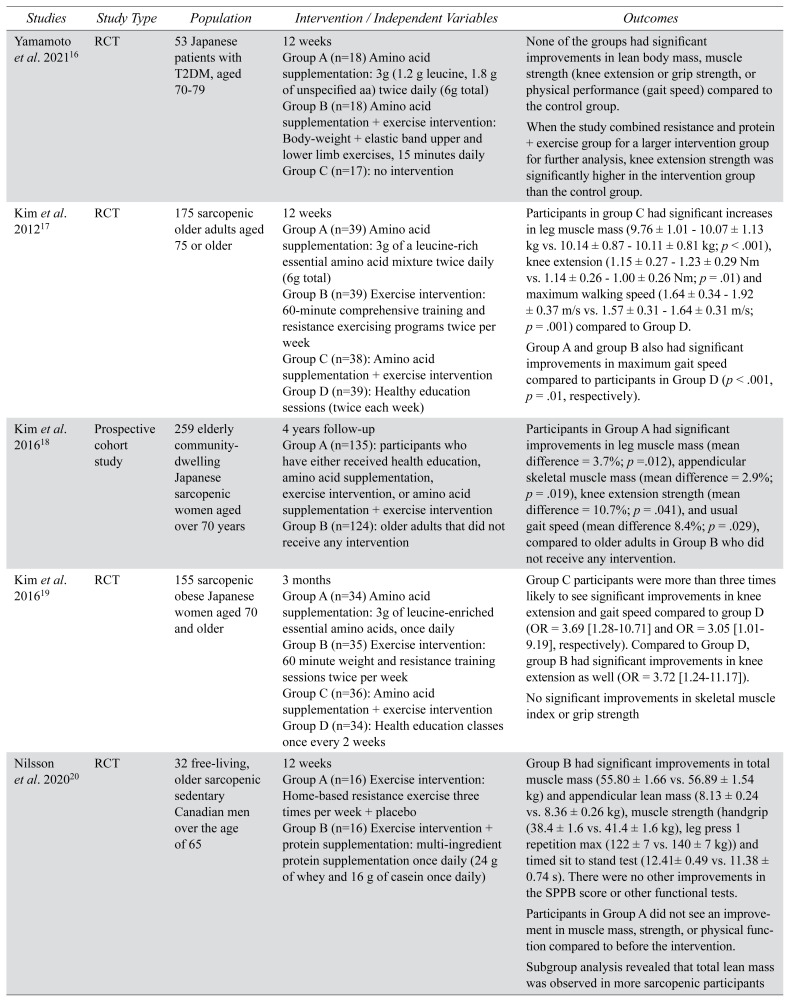
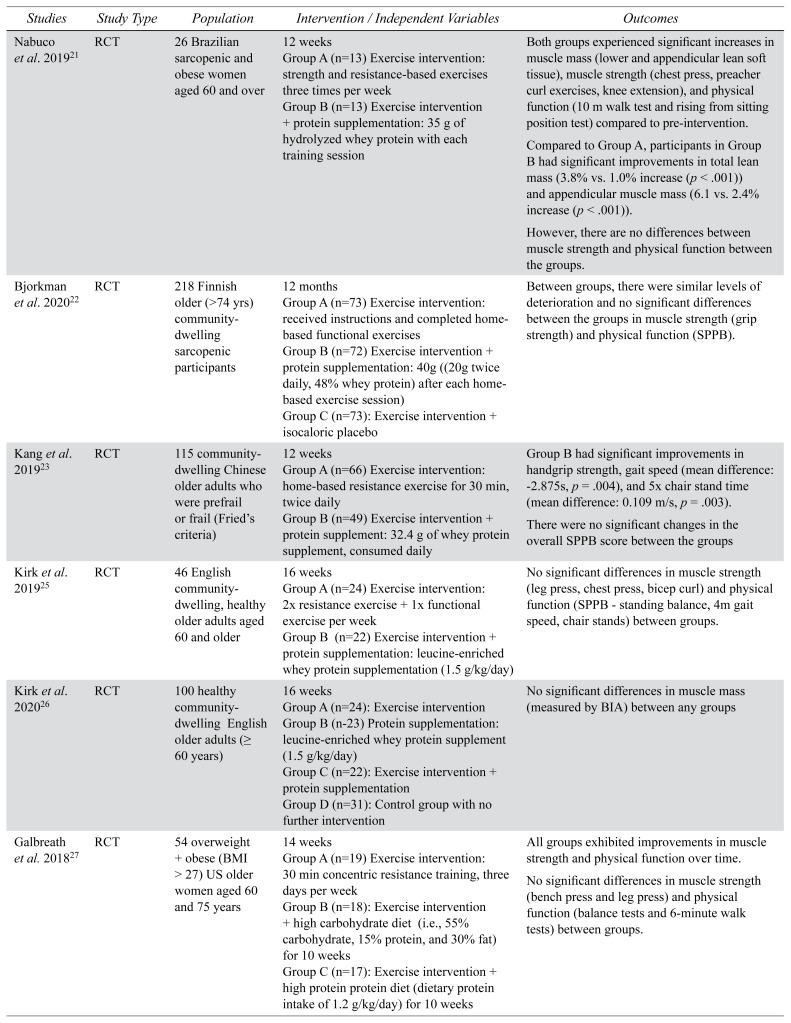
Overall, we identified 12 studies that evaluated the combined effects of nutritional supplementation and exercise or electromyostimulation intervention on various aspects of sarcopenia (Table 2). Exercise intervention in studies often included resistance exercises, such as biceps curl, chest press, and knee extension.
TABLE 2.
Studies with protein/amino acid supplementation and exercise intervention or electromyostimulation
| Studies | Study Type | Population | Intervention / Independent Variables | Outcomes |
|---|---|---|---|---|
| Yamamoto et al. 202116 | RCT | 53 Japanese patients with T2DM, aged 70–79 | 12 weeks Group A (n=18) Amino acid supplementation: 3g (1.2 g leucine, 1.8 g of unspecified aa) twice daily (6g total) Group B (n=18) Amino acid supplementation + exercise intervention: Body-weight + elastic band upper and lower limb exercises, 15 minutes daily Group C (n=17): no intervention |
None of the groups had significant improvements in lean body mass, muscle strength (knee extension or grip strength, or physical performance (gait speed) compared to the control group. When the study combined resistance and protein + exercise group for a larger intervention group for further analysis, knee extension strength was significantly higher in the intervention group than the control group. |
| Kim et al. 201217 | RCT | 175 sarcopenic older adults aged 75 or older | 12 weeks Group A (n=39) Amino acid supplementation: 3g of a leucine-rich essential amino acid mixture twice daily (6g total) Group B (n=39) Exercise intervention: 60-minute comprehensive training and resistance exercising programs twice per week Group C (n=38): Amino acid supplementation + exercise intervention Group D (n=39): Healthy education sessions (twice each week) |
Participants in group C had significant increases in leg muscle mass (9.76 ± 1.01 – 10.07 ± 1.13 kg vs. 10.14 ± 0.87 – 10.11 ± 0.81 kg; p < .001), knee extension (1.15 ± 0.27 – 1.23 ± 0.29 Nm vs. 1.14 ± 0.26 – 1.00 ± 0.26 Nm; p = .01) and maximum walking speed (1.64 ± 0.34 – 1.92 ± 0.37 m/s vs. 1.57 ± 0.31 – 1.64 ± 0.31 m/s; p = .001) compared to Group D. Group A and group B also had significant improvements in maximum gait speed compared to participants in Group D (p < .001, p = .01, respectively). |
| Kim et al. 201618 | Prospective cohort study | 259 elderly community-dwelling Japanese sarcopenic women aged over 70 years | 4 years follow-up Group A (n=135): participants who have either received health education, amino acid supplementation, exercise intervention, or amino acid supplementation + exercise intervention Group B (n=124): older adults that did not receive any intervention |
Participants in Group A had significant improvements in leg muscle mass (mean difference = 3.7%; p =.012), appendicular skeletal muscle mass (mean difference = 2.9%; p = .019), knee extension strength (mean difference = 10.7%; p = .041), and usual gait speed (mean difference 8.4%; p = .029), compared to older adults in Group B who did not receive any intervention. |
| Kim et al. 201619 | RCT | 155 sarcopenic obese Japanese women aged 70 and older | 3 months Group A (n=34) Amino acid supplementation: 3g of leucine-enriched essential amino acids, once daily Group B (n=35) Exercise intervention: 60 minute weight and resistance training sessions twice per week Group C (n=36): Amino acid supplementation + exercise intervention Group D (n=34): Health education classes once every 2 weeks |
Group C participants were more than three times likely to see significant improvements in knee extension and gait speed compared to group D (OR = 3.69 [1.28–10.71] and OR = 3.05 [1.01–9.19], respectively). Compared to Group D, group B had significant improvements in knee extension as well (OR = 3.72 [1.24–11.17]). No significant improvements in skeletal muscle index or grip strength |
| Nilsson et al. 202020 | RCT | 32 free-living, older sarcopenic sedentary Canadian men over the age of 65 | 12 weeks Group A (n=16) Exercise intervention: Home-based resistance exercise three times per week + placebo Group B (n=16) Exercise intervention + protein supplementation: multi-ingredient protein supplementation once daily (24 g of whey and 16 g of casein once daily) |
Group B had significant improvements in total muscle mass (55.80 ± 1.66 vs. 56.89 ± 1.54 kg) and appendicular lean mass (8.13 ± 0.24 vs. 8.36 ± 0.26 kg), muscle strength (handgrip (38.4 ± 1.6 vs. 41.4 ± 1.6 kg), leg press 1 repetition max (122 ± 7 vs. 140 ± 7 kg)) and timed sit to stand test (12.41± 0.49 vs. 11.38 ± 0.74 s). There were no other improvements in the SPPB score or other functional tests. Participants in Group A did not see an improvement in muscle mass, strength, or physical function compared to before the intervention. Subgroup analysis revealed that total lean mass was observed in more sarcopenic participants |
| Nabuco et al. 201921 | RCT | 26 Brazilian sarcopenic and obese women aged 60 and over | 12 weeks Group A (n=13) Exercise intervention: strength and resistance-based exercises three times per week Group B (n=13) Exercise intervention + protein supplementation: 35 g of hydrolyzed whey protein with each training session |
Both groups experienced significant increases in muscle mass (lower and appendicular lean soft tissue), muscle strength (chest press, preacher curl exercises, knee extension), and physical function (10 m walk test and rising from sitting position test) compared to pre-intervention. Compared to Group A, participants in Group B had significant improvements in total lean mass (3.8% vs. 1.0% increase (p < .001)) and appendicular muscle mass (6.1 vs. 2.4% increase (p < .001)). However, there are no differences between muscle strength and physical function between the groups. |
| Bjorkman et al. 202022 | RCT | 218 Finnish older (>74 yrs) community-dwelling sarcopenic participants | 12 months Group A (n=73) Exercise intervention: received instructions and completed home-based functional exercises Group B (n=72) Exercise intervention + protein supplementation: 40g ((20g twice daily, 48% whey protein) after each home-based exercise session) Group C (n=73): Exercise intervention + isocaloric placebo |
Between groups, there were similar levels of deterioration and no significant differences between the groups in muscle strength (grip strength) and physical function (SPPB). |
| Kang et al. 201923 | RCT | 115 community-dwelling Chinese older adults who were prefrail or frail (Fried’s criteria) | 12 weeks Group A (n=66) Exercise intervention: home-based resistance exercise for 30 min, twice daily Group B (n=49) Exercise intervention + protein supplement: 32.4 g of whey protein supplement, consumed daily |
Group B had significant improvements in handgrip strength, gait speed (mean difference: −2.875s, p = .004), and 5× chair stand time (mean difference: 0.109 m/s, p = .003). There were no significant changes in the overall SPPB score between the groups |
| Kirk et al. 201925 | RCT | 46 English community-dwelling, healthy older adults aged 60 and older | 16 weeks Group A (n=24) Exercise intervention: 2× resistance exercise + 1× functional exercise per week Group B (n=22) Exercise intervention + protein supplementation: leucine-enriched whey protein supplementation (1.5 g/kg/day) |
No significant differences in muscle strength (leg press, chest press, bicep curl) and physical function (SPPB - standing balance, 4m gait speed, chair stands) between groups. |
| Kirk et al. 202026 | RCT | 100 healthy community-dwelling English older adults (≥ 60 years) | 16 weeks Group A (n=24): Exercise intervention Group B (n-23) Protein supplementation: leucine-enriched whey protein supplement (1.5 g/kg/day) Group C (n=22): Exercise intervention + protein supplementation Group D (n=31): Control group with no further intervention |
No significant differences in muscle mass (measured by BIA) between any groups |
| Galbreath et al. 201827 | RCT | 54 overweight + obese (BMI > 27) US older women aged 60 and 75 years | 14 weeks Group A (n=19) Exercise intervention: 30 min concentric resistance training, three days per week Group B (n=18): Exercise intervention + high carbohydrate diet (i.e., 55% carbohydrate, 15% protein, and 30% fat) for 10 weeks Group C (n=17): Exercise intervention + high protein protein diet (dietary protein intake of 1.2 g/kg/day) for 10 weeks |
All groups exhibited improvements in muscle strength and physical function over time. No significant differences in muscle strength (bench press and leg press) and physical function (balance tests and 6-minute walk tests) between groups. |
| Mori & Tokuda 201828 | RCT | 75 healthy community-dwelling Japanese women aged 65–80 years | 24 weeks Group A (n=25) Protein Supplement: 25 g of protein supplement daily (22.3 g of whey protein, 1225 mg of valine, 2975 mg of leucine and 1175 mg of isoleucine) Group B (n=25) Exercise intervention: Resistance and functional exercises, twice per week Group C (n=25): Exercise intervention + protein supplementation |
Group C participants had more significant improvements in lower limb muscle mass (p =.038), skeletal muscle index (p = .007), and knee extension strength (p =.005) compared to Group B participants. Group C participants also significantly improved more in upper limb muscle mass (p = .029), lower limb muscle mass (p < .001), skeletal muscle index (p < .001), grip strength (p = .014), and gait speed (p < .001) compared to Group A participants |
| Kemmler et al. 201829 | RCT | 48 sarcopenic community-dwelling obese male older adults aged 70 and over | 16 weeks Group A (n=34) Whole-body electromyostimulation + protein supplementation: 30 min of electromyostimulation per week and whey protein supplementation (1.8g/kg/day) per day Group B (n=33): No further intervention |
Group A participants had significant improvements in muscle mass (fat-free (8.47 ± 10.37 vs. 1.77 ± 10.9 cm3; p=.033) and appendicular muscle mass (0.45 ± 0.53 vs. − 0.01 ± 0.47 cm3; p< .001)), leg press strength (189 ± 129 vs. 33 ± 132; p< .001), and gait speed (0.035 ± 0.046 vs. − 0.006 ± .039; p< .001) compared to Group B participants |
Four studies explored the role of amino acid supplementation and exercise intervention in improving muscle mass, muscle strength, and physical function. Yamamoto et al. randomized type II diabetic older adults into three groups: the amino acid + exercise intervention group, the exercise intervention group, and the control group. The study reported no significant differences in lean body mass, knee extension or grip strength, or gait speed between all groups post-intervention.(16) In contrast, Kim et al. found that sarcopenic older adults who received exercise and amino acid supplementation for 12 weeks significantly improved in leg muscle mass, knee extension, and maximum walking speed compared to the health education control group.(17) Furthermore, in a four-year follow-up study, they also compared the effects of all interventions (exercise + amino acid supplementation and either intervention alone) against sarcopenic older adults who were originally excluded from the study. The participants who received any one of the interventions had significant improvements in leg muscle mass, appendicular skeletal muscle mass, knee extension strength, and gait speed, compared to non-participating sarcopenic older adults.(18) Lastly, another randomized control trial reported that sarcopenic and obese older adults who received amino acid supplementation and resistance exercise intervention were over three times as likely to see improvements in knee extension strength and usual gait speed compared to the home education control group.(19) However, the study reported no significant differences in skeletal muscle index or grip strength between groups.(19)
In comparison, eight studies reported whey protein supplementation and exercise intervention and their effects on muscle mass, muscle strength, and physical function. Nilsson et al. conducted a randomized controlled trial in sarcopenic older men. The study found that participants who received both the protein supplementation and exercise intervention for 12 weeks had significant improvements in total muscle mass and appendicular lean mass, muscle strength (handgrip strength and leg press), and timed sit-to-stand test compared to pre-intervention.(20) There were no significant improvements in other functional tests or the overall SPPB score.(20) Similarly, Nabuco et al. reported that sarcopenic obese older women who received 12 weeks of both protein and exercise interventions had significant improvements in lower and appendicular lean soft tissue, muscle strength (chest press, preacher curl exercises, knee extension), and physical function (10-m walk and chair stand test) post-intervention.(21) Muscle mass was also significantly greater in the exercise and protein intervention group compared to the exercise intervention-only group.(21) In comparison, a Finnish study on community-dwelling sarcopenic older adults found that 12 months of protein supplementation in addition to home-based exercises resulted in no significant differences in grip strength and the SPPB compared to the exercise-only group.(22) However, the study reported poor compliance (45% compliance) throughout the intervention period.(22) Lastly, Kang et al. enrolled community-dwelling pre-frail or frail participants based on Fried’s criteria.(23,24) The study reported that participants who received both whey protein and exercise intervention for 12 weeks had significantly greater handgrip strength, gait speed, and five times longer chair stand time compared to those from the exercise-only group.(23)
Four studies evaluated the effects of exercise + protein interventions in healthy older adults. Kirk et al. reported that 16 weeks of whey protein supplementation in addition to resistance exercises did not significantly improve muscle strength (leg press, chest press, bicep curl) and physical function (SPPB) compared to exercise intervention alone.(25) Their follow-up study, recruiting more healthy older adults also found that protein supplementation and exercise intervention had no significant impact on muscle mass.(26) However, this study also cited a lack of compliance, with only 43% of participants completing the allocated intervention regimen.(26) Similarly, Galbreath et al. also reported that dietary protein intake and resistance exercise intervention on sarcopenia in overweight and obese older women did not significantly improve in muscle strength and physical function compared to isocaloric controls.(27) In contrast, Mori and Tokuda recruited healthy Japanese older women and randomized the participants into the resistance intervention + whey protein supplementation group, exercise-only, and protein-only groups.(28) After 24 weeks of intervention, the exercise + protein group had significant improvements in lower limb muscle mass, skeletal muscle index, and knee extension strength compared to the exercise-only group.(27) Exercise + protein group also had more significant improvements in upper limb muscle mass, grip strength, and gait speed, compared to the protein-only group.(27) Together, these results indicate that whey protein supplement + resistance exercise can improve aspects of sarcopenia more than either intervention alone.(27)
Lastly, Kemmler et al. evaluated the effects of protein supplementation and whole-body electromyostimulation (WB-EMS), an intervention using electric current to stimulate muscle growth, on sarcopenia in obese older males.(29) After 16 weeks of WB-EMS and whey protein supplementation, the intervention group significantly improved in fat-free and appendicular muscle mass, leg press strength, and gait speed compared to the control group.(29)
These findings demonstrate that amino acid supplementation and exercise intervention over three months significantly improved muscle mass, muscle strength, and physical function, particularly in sarcopenic older adults. Similarly, in sarcopenic and pre-frail older adults, most studies indicate that 12 weeks of whey protein supplementation combined with exercise intervention can improve muscle mass, muscle strength, and physical function compared to pre-intervention. However, when comparing protein + exercise intervention to exercise intervention alone, there are discrepancies in the improvements in muscle mass and strength, with generally fewer between-group differences in physical function. In healthy or non-sarcopenic older adults, there are incongruencies regarding the effects of whey protein supplementation and exercise on muscle mass, strength, and physical function. Lastly, whey protein supplementation combined with electromyostimulation can effectively improve parameters of sarcopenia in older adults.
Dietary Protein Intake
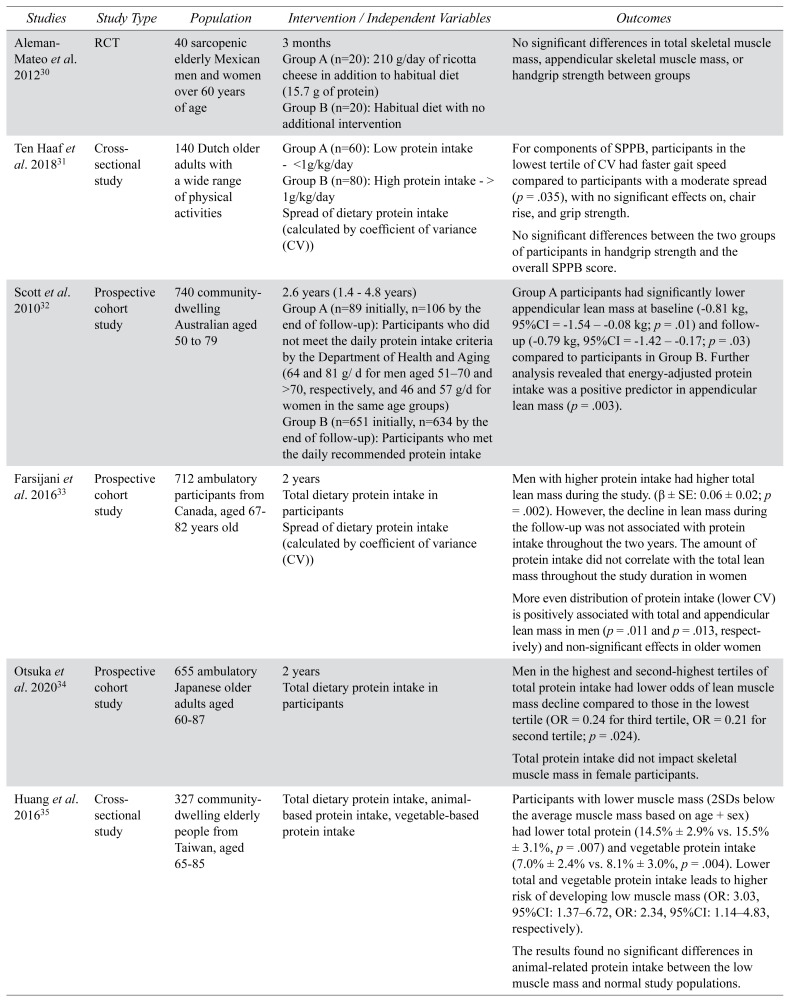
Quantity and Distribution of Protein Intake
Overall, five studies assessed the quantity of protein intake and its impact on aspects of sarcopenia in older adults (Table 3). One randomized trial evaluated the effects of daily ricotta cheese supplementation in sarcopenic older adults and found no significant differences in total muscle mass or handgrip strength between the intervention and control groups.(30) In comparison, in their cross-sectional study, Ten Haaf et al. reported that older adults with > 1 g/kg/day protein intake did not have significant improvements in handgrip strength and the SPPB score compared to participants with lower protein intake.(31) In contrast, in a prospective cohort study, Scott et al. assessed the effects of dietary protein intake on sarcopenia in healthy older adults, using cutoffs for protein intake based on the Australian Department of Health and Aging (64 and 81 g/day for men aged 51–70 and >70, respectively, and 46 and 57 g/day for women in the same age groups). The study found that participants who did not meet the recommended levels were associated with significantly lower appendicular lean mass at baseline and follow-up.(32)
TABLE 3.
Studies assessing dietary protein intake
| Studies | Study Type | Population | Intervention / Independent Variables | Outcomes |
|---|---|---|---|---|
| Aleman-Mateo et al. 201230 | RCT | 40 sarcopenic elderly Mexican men and women over 60 years of age | 3 months Group A (n=20): 210 g/day of ricotta cheese in addition to habitual diet (15.7 g of protein) Group B (n=20): Habitual diet with no additional intervention |
No significant differences in total skeletal muscle mass, appendicular skeletal muscle mass, or handgrip strength between groups |
| Ten Haaf et al. 201831 | Cross-sectional study | 140 Dutch older adults with a wide range of physical activities | Group A (n=60): Low protein intake - <1g/kg/day Group B (n=80): High protein intake - > 1g/kg/day Spread of dietary protein intake (calculated by coefficient of variance (CV)) |
For components of SPPB, participants in the lowest tertile of CV had faster gait speed compared to participants with a moderate spread (p = .035), with no significant effects on, chair rise, and grip strength. No significant differences between the two groups of participants in handgrip strength and the overall SPPB score. |
| Scott et al. 201032 | Prospective cohort study | 740 community-dwelling Australian aged 50 to 79 | 2.6 years (1.4 – 4.8 years) Group A (n=89 initially, n=106 by the end of follow-up): Participants who did not meet the daily protein intake criteria by the Department of Health and Aging (64 and 81 g/ d for men aged 51–70 and >70, respectively, and 46 and 57 g/d for women in the same age groups) Group B (n=651 initially, n=634 by the end of follow-up): Participants who met the daily recommended protein intake |
Group A participants had significantly lower appendicular lean mass at baseline (−0.81 kg, 95%CI = −1.54 – −0.08 kg; p = .01) and follow-up (−0.79 kg, 95%CI = −1.42 – −0.17; p = .03) compared to participants in Group B. Further analysis revealed that energy-adjusted protein intake was a positive predictor in appendicular lean mass (p = .003). |
| Farsijani et al. 201633 | Prospective cohort study | 712 ambulatory participants from Canada, aged 67–82 years old | 2 years Total dietary protein intake in participants Spread of dietary protein intake (calculated by coefficient of variance (CV)) |
Men with higher protein intake had higher total lean mass during the study. (β ± SE: 0.06 ± 0.02; p = .002). However, the decline in lean mass during the follow-up was not associated with protein intake throughout the two years. The amount of protein intake did not correlate with the total lean mass throughout the study duration in women More even distribution of protein intake (lower CV) is positively associated with total and appendicular lean mass in men (p = .011 and p = .013, respectively) and non-significant effects in older women |
| Otsuka et al. 202034 | Prospective cohort study | 655 ambulatory Japanese older adults aged 60–87 | 2 years Total dietary protein intake in participants |
Men in the highest and second-highest tertiles of total protein intake had lower odds of lean muscle mass decline compared to those in the lowest tertile (OR = 0.24 for third tertile, OR = 0.21 for second tertile; p = .024). Total protein intake did not impact skeletal muscle mass in female participants. |
| Huang et al. 201635 | Cross-sectional study | 327 community-dwelling elderly people from Taiwan, aged 65–85 | Total dietary protein intake, animal-based protein intake, vegetable-based protein intake | Participants with lower muscle mass (2SDs below the average muscle mass based on age + sex) had lower total protein (14.5% ± 2.9% vs. 15.5% ± 3.1%, p = .007) and vegetable protein intake (7.0% ± 2.4% vs. 8.1% ± 3.0%, p = .004). Lower total and vegetable protein intake leads to higher risk of developing low muscle mass (OR: 3.03, 95%CI: 1.37–6.72, OR: 2.34, 95%CI: 1.14–4.83, respectively). The results found no significant differences in animal-related protein intake between the low muscle mass and normal study populations. |
| Chan et al. 201436 | Prospective cohort study | 2726 Chinese community-dwelling older people aged 65 and older in Hong Kong | 4 years Total dietary protein intake, animal-based protein intake, vegetable-based protein intake |
Participants in the highest quartile (>0.72 g/kg/day) of plant-based protein intake lost significantly less appendicular skeletal mass over a 4-year period than those in the lowest quartile (mean loss ± SE: 0.270 ± 0.029 vs. 0.349 ± 0.030 kg, p=.025). Plant-based protein intake had no effects on physical function. No significant associations between the total and animal-based proteins and muscle mass or physical function. |
| Houston et al. 200837 | Prospective cohort study | 2066 healthy US older adults aged 70–80 | 3 years Total dietary protein intake, animal-based protein intake, vegetable-based protein intake |
Total and animal-based protein intake was significantly associated with increased total lean mass (SE: 8.76 (3.00), p = .004) and appendicular lean mass (SE: 5.31 (1.64), p = .001). Participants in the highest quintile of total protein intake lost considerably less lean mass (43% less) and appendicular lean mass (39% less) over 3 years compared to those in the lowest quintile of protein intake (intake (x ± SE: 0.501 ± 0.106 kg compared with 0.883 ± 0.104 kg for lean mass; 0.400 ± 0.058 kg compared with 0.661 ± 0.057 kg for appendicular lean mass; p < .01). Vegetable protein intake was not associated with improvements in total and appendicular lean mass |
| Li et al. 202038 | Cross-sectional study | 861 Chinese community-dwelling older adults | 3 Dietary patterns 1) Dietary Pattern 1 (DP1) “Cereals–tubers–animal oils” pattern (high carbohydrate diet) 2) Dietary Pattern 2 (DP2) “mushrooms–fruits–milk” pattern (also including relative high amounts of legume, fish, and seafood) 3) Dietary Pattern 3 (DP3) “animal foods” pattern |
The highest quartile intake of DP2 had the lowest prevalence rate of sarcopenia and negative association with sarcopenia (OR = 0.33, 95% CI = 0.14~0.77, p = .009). Lastly, significant correlations were observed between the DP2 score andgrip strength (r = 0.07, p value = .044), gait speed (r = 0.09, p value = .009), and skeletal muscle index (r = 0.11, p value = .002) Other dietary patterns did not exhibit any significant associations with sarcopenia |
| Hashemi et al. 201539 | Cross-sectional study | 296 community-dwelling older adults (> 55 yr old) living in Iran | 3 Dietary patterns 1) Mediterranean: higher consumption of olive oil, vegetables, tomatoes, whole grains, nuts, fish, fresh and dried fruits 2) Western: higher consumption of tea, soy, desserts, sugars, and fast foods 3) Mixed: higher consumption of meats, legumes, potatoes, and refined grains |
Subjects in the highest tertile of the Mediterranean dietary pattern had a lower odds ratio for sarcopenia than those in the lowest tertile (OR = 0.42; 95% CI = 0.18–0.97; p = .04). Adherence to western or mixed dietary patterns did not affect the odds of sarcopenia. |
Unlike previous studies with recommended protein intake levels, Farsijani et al. conducted a prospective cohort study to assess the correlation between protein intake and muscle mass in ambulatory older adults.(33) The study found that older men with higher protein intake had higher total lean mass at baseline and follow-up.(33) However, the overall decline in lean mass during the follow-up was not associated with lower protein intake throughout the two years. There was no correlation between dietary protein intake and total lean mass in female participants.(33) Similarly, in a prospective study with ambulatory older adults, Otsuka et al. also reported that greater total protein intake led to lower odds of lean muscle mass decline in men, with no association reported in older women.(34)
The current literature demonstrates that there are inconclusive findings regarding the exact amount of dietary protein intake required to positively impact muscle mass, strength, and physical function in the elderly population. However, there is a general trend that increased dietary protein intake is associated with greater muscle mass in older men. However, similar trends were not observed in older women.
Type of Dietary Protein and Dietary Protein Patterns
Three studies specifically evaluated the impact of an animal-based vs. plant-based protein diet on muscle mass (Table 3). A Taiwanese study reported that total and vegetable protein intake were significantly lower in healthy older adults with lower muscle mass, with participants with the lowest quartiles of intake having higher risks of developing low muscle mass compared to those in the highest quartile.(35) The study found no significant differences in animal-related protein intake between older adults with different muscle masses.(35) Similarly, another cross-sectional study found that Chinese participants in the highest quartile of vegetable protein intake lost significantly less appendicular skeletal mass over a four-year period than those in the lowest quartile of relative vegetable protein intake, with no effects on physical function.(36) Again, there were no significant associations between animal-based protein intake and muscle mass or physical function.(36) Compared to the two previous studies, a US study reported that animal protein intake was significantly associated with increased total and appendicular lean mass in older adults.(37) Participants in the highest quintile of total protein intake lost considerably less lean mass over three years compared to those in the lowest quintile of protein intake.(37)
Two studies also evaluated specific dietary patterns and their association with sarcopenia in older adults (Table 3). A cross-sectional study by Li et al. found that participants with the “mushroom-fruits-milk” diet (which also had a higher intake of legume and seafood) had the lowest prevalence rate of developing sarcopenia. In addition, the study reported significant associations between this type of diet and skeletal muscle index, grip strength, and gait speed.(38) Another cross-sectional study divided the participants’ diet based on three food groups: Mediterranean (olive oil, vegetables, whole grains, and fish), Western (tea, soy, fast foods, desserts, and sugars), and Mixed (animal proteins, legumes, potatoes, and refined grains).(39) The study found that participants in the highest tertile of the Mediterranean dietary pattern had lower odds of developing sarcopenia than those in the lowest tertile, and other patterns were not associated with sarcopenia.(39)
Overall, there are conflicting results when comparing the effects of plant-based protein vs. animal-based protein on muscle mass. Studies with an Asian population found that plant-based protein intake was associated with greater muscle mass, while animal-based protein intake was positively associated with muscle mass in American older adults. However, like previous studies, increased overall protein intake is generally negatively associated with lower muscle mass and developing sarcopenia in older adults. On the other hand, there is a wide distribution of dietary food groups and dietary patterns that may increase muscle mass. To summarize, a balanced diet consisting of fruits, vegetables, milk products, legumes, and seafood is positively associated with improved muscle mass and lower odds of sarcopenia development in older adults.
DISCUSSION
This literature review assessed the findings from studies on the impact of protein supplementation and dietary protein intake on various aspects of sarcopenia in community-dwelling older adults, including muscle mass, muscle strength, and physical function.
Nutritional Intervention Alone
In general, we found that both amino acid and protein supplementation alone can improve muscle mass in pre-frail and sarcopenic community-dwelling older adults. In comparison, there were inconsistent findings between studies regarding the effects of nutritional supplementation on muscle mass in healthy older adults. However, protein or amino acid intervention alone was unlikely to elicit any benefits in muscle strength and physical function in healthy older adults.
Our study findings are consistent with previous literature, which shows that increased amino acids or protein supplementation could increase muscle protein synthesis and improve muscle mass, particularly in frail older adults.(40,41) In comparison, a previous systematic review that evaluated protein supplementation in healthy older adults has concluded that protein supplementation alone is unlikely to elicit positive effects in improving muscle strength and physical function.(42) In sarcopenic and pre-frail older adults, poor nutrition and chronic inflammatory conditions often cause attenuated protein metabolism and muscle synthesis, leading to more significant muscle loss.(43) Furthermore, pre-existing sarcopenia and pre-frailty further reduces physical activity in older adults, therefore further increasing the rate of muscle loss.(44,45) Therefore, protein supplementation may improve muscle mass in older adults with considerable muscle loss and less anabolic muscle gain.
Nutritional Supplementation and Exercise Intervention
Our literature review found that exercise intervention combined with amino acid or protein supplementation effectively improves muscle mass, muscle strength, and physical function in sarcopenic older adults compared to pre-intervention in sarcopenic and pre-frail older adults. In comparison, in healthy older adults, protein supplementation and exercise intervention elicited mixed results in muscle mass, muscle strength, and physical function.
In general, previous studies have shown that physical exercise can improve cardiorespiratory function, bone and muscle health, and reduce the risk of immobility in older adults.(46,47) In particular, resistance-based exercises can prevent muscle wasting and improve muscle strength, while effectively reducing frailty and enhancing mobility in older adults.(48) In line with our study findings, an earlier systematic review assessing the effects of nutritional supplementation and exercise intervention found that the combined interventions can positively impact lean muscle mass, knee extension strength, and gait speed compared to pre-intervention in sarcopenic older adults.(48) However, in healthy older adults, the effect of exercise intervention and protein supplementation on sarcopenia is limited, with previous literature reporting inconclusive results when assessing the effects of combined interventions on muscle mass, strength, and physical function.(42,49,50) These findings may be due to differences in baseline protein intake, activity level, and adherence to the exercise and protein interventions.
Dietary Protein Intake
From studies within this literature review, there were inconclusive findings regarding the exact amount of dietary protein intake required to positively impact muscle mass, strength, and physical function in the elderly population. However, we found that overall increased levels of dietary protein intake is associated with greater muscle mass and lower odds of developing sarcopenia, particularly in older men. The National Academy of Science and the WHO established a Recommended Dietary Allowance of 0.8g/kg/day in older adults.(51,52) Nevertheless, recent reviews have suggested that higher levels of protein intake ranging from 1.0–1.5 g/kg/day may be more effective in preventing muscle loss in older adults.(53,54)
On the other hand, our literature review found mixed results when comparing vegetable-based proteins versus animal-based proteins and their effects on sarcopenia. Two studies with Asian participants found that plant-based proteins are more likely to improve muscle mass in older adults.(35,36) In contrast, one US study reported that animal-based protein intake is associated with increased muscle mass in older participants.(37) Previous research has revealed that animal-based protein contains higher levels of essential amino acids and is more easily digestible compared to plant-based proteins, leading to increased muscle protein synthesis and anabolism.(54) However, in studies with Asian participants, the most commonly ingestible vegetable-based proteins were soy products, which also have high essential amino acid profiles (with high levels of leucine) and near-equivalent protein digestibility compared to animal sources.(54) Consistent with our findings, a previous review also revealed when taken in adequate amounts, both animal-based and plant-based proteins can enhance and maintain muscle mass in aging populations, despite the differences in their anabolic properties.(55) Likewise, for dietary patterns, this review found that the Mediterranean diet, which consists of high amounts of fish protein and nuts, is associated with a lower risk of developing sarcopenia in older adults.(39) Many other studies have also cited the protective effects of the Mediterranean diet against muscle loss and frailty in the aging population.(56,57)
There are several limitations associated with this literature review. Firstly, we only conducted the literature search and only included studies from EMBASE, MEDLINE, and PubMed. We may have excluded literature in other languages or from other databases. Furthermore, the study participants’ baseline characteristics are not uniform. In particular, baseline dietary nutrition and physical activity were not assessed in several studies, making it difficult to draw conclusions based on the differences in the participant population. Lastly, the intervention and results are very heterogeneous in this study. Studies included varying protein supplementation amounts and exercise intervention durations, and they also measured outcomes in muscle mass, strength, and physical function differently. The variability in methods and outcomes can limit the comparability of the conclusions generated from the study findings.
CONCLUSION
In conclusion, in community-dwelling older adults, protein and amino acid supplementation can improve muscle mass in sarcopenia and pre-frail older adults, with variable effects in muscle strength and physical function. Furthermore, protein supplementation combined with exercise can further improve muscle mass, muscle strength, and physical function in the same group, with potentially additional beneficial effects than either intervention alone. However, there were inconclusive findings regarding the effects of protein supplementation with or without exercise intervention on muscle mass, muscle strength, and physical function in healthy older adults. Regarding dietary protein intake, higher protein intake and more spread protein intake distribution are associated with a lower risk of developing sarcopenia. Lastly, a higher intake of both animal-based and plant-based soy proteins can reduce the risk of sarcopenia. Future studies should continue to assess the impact of protein intake in community-dwelling older adults, with a particular focus on participant adherence and similar rates of baseline protein intake and physical activity, to generate a more comprehensive conclusion regarding the impact of protein and exercise interventions in healthy older adults. Furthermore, more standardized protein supplementation and exercise regimens can be implemented to improve comparability between studies and identify patterns in the future.
ACKNOWLEDGEMENTS
Not applicable.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood the Canadian Geriatrics Journal’s policy on conflicts of interest disclosure and declare there are none.
FUNDING
This research did not receive external funding.
REFERENCES
- 1.Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019 Jan 1;48(1):16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilkinson DJ, Piasecki M, Atherton PJ. The age-related loss of skeletal muscle mass and function: measurement and physiology of muscle fibre atrophy and muscle fibre loss in humans. Ageing Res Rev. 2018 Nov 1;47:123–32. doi: 10.1016/j.arr.2018.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012 Nov;24(6):623–27. doi: 10.1097/BOR.0b013e328358d59b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McIntire KL, Hoffman AR. The endocrine system and sarcopenia: potential therapeutic benefits. Curr Aging Sci. 2011 Dec 1;4(3):298–305. doi: 10.2174/1874609811104030298. [DOI] [PubMed] [Google Scholar]
- 5.Schaap LA, van Schoor NM, Lips P, Visser M. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the Longitudinal Aging Study Amsterdam. J Gerontol Series A. 2017 Aug 10;73(9):1199–1204. doi: 10.1093/gerona/glx245. [DOI] [PubMed] [Google Scholar]
- 6.Bahat G, Ilhan B. Sarcopenia and the cardiometabolic syndrome: a narrative review. Eur Geriatr Med. 2016 Jun 1;7(3):220–23. doi: 10.1016/j.eurger.2015.12.012. [DOI] [Google Scholar]
- 7.Kwak JY, Kwon KS. Pharmacological interventions for treatment of sarcopenia: current status of drug development for sarcopenia. Ann Geriatr Med Res. 2019 Sep;23(3):98–104. doi: 10.4235/agmr.19.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martone AM, Marzetti E, Calvani R, et al. Exercise and protein intake: a synergistic approach against sarcopenia. Biomed Res Int. 2017 Mar 21;2017:2672435. doi: 10.1155/2017/2672435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yanai H. Nutrition for sarcopenia. J Clin Med Res. 2015 Dec;7(12):926–31. doi: 10.14740/jocmr2361w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solerte S, Gazzaruso C, Bonacasa R, et al. Nutritional supplements with oral amino acid mixtures increases whole-body lean mass and insulin sensitivity in elderly subjects with sarcopenia. Am J Cardiol. 2008 Jun 2;101(11):S69–S77. doi: 10.1016/j.amjcard.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Peng L, Cheng Y, Yu P, Lee W, Lin M, Chen L. Oral nutritional supplement with xxbhydroxy-β-methylbutyrate (HMB) improves nutrition, physical performance and ameliorates intramuscular adiposity in pre-frail older adults: a randomized controlled trial. J Nutr Health Aging. 2021 Jun;25(6):767–73. doi: 10.1007/s12603-021-1621-7. [DOI] [PubMed] [Google Scholar]
- 12.Ellis A, Hunter G, Goss A, Gower B. Oral supplementation with Beta-Hydroxy-Beta-Methylbutyrate, arginine, and glutamine improves lean body mass in healthy older adults. J Diet Suppl. 2019 May 4;16(3):281–93. doi: 10.1080/19390211.2018.1454568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang Y, Kim N, Choi Y, et al. Leucine-enriched protein supplementation increases lean body mass in healthy Korean adults aged 50 years and older: a randomized, double-blind, placebo-controlled trial. Nutrients. 2020 Jun;12(6):1816. doi: 10.3390/nu12061816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chanet A, Verlaan S, Salles J, et al. Supplementing breakfast with a Vitamin D and leucine–enriched whey protein medical nutrition drink enhances postprandial muscle protein synthesis and muscle mass in healthy older men. J Nutr. 2017 Dec 1;147(12):2262–71. doi: 10.3945/jn.117.252510. [DOI] [PubMed] [Google Scholar]
- 15.Zhu K, Kerr D, Meng X, et al. Two-year whey protein supplementation did not enhance muscle mass and physical function in well-nourished healthy older postmenopausal women. J Nutr. 2015 Nov 1;145(11):2520–26. doi: 10.3945/jn.115.218297. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto Y, Nagai Y, Kawanabe S, et al. Effects of resistance training using elastic bands on muscle strength with or without a leucine supplement for 48 weeks in elderly patients with type 2 diabetes. Endocr J. 2021;68(3):291–98. doi: 10.1507/endocrj.EJ20-0550. [DOI] [PubMed] [Google Scholar]
- 17.Kim HK, Suzuki T, Saito K, et al. Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc. 2012 Jan;60(1):16–23. doi: 10.1111/j.1532-5415.2011.03776.x. [DOI] [PubMed] [Google Scholar]
- 18.Kim H, Suzuki T, Saito K, Kojima N, Hosoi E, Yoshida H. Long-term effects of exercise and amino acid supplementation on muscle mass, physical function and falls in community-dwelling elderly Japanese sarcopenic women: a 4-year follow-up study. Geriatr Gerontol Int. 2016 Feb;16(2):175–81. doi: 10.1111/ggi.12448. [DOI] [PubMed] [Google Scholar]
- 19.Kim H, Kim M, Kojima N, et al. Exercise and nutritional supplementation on community-dwelling elderly Japanese women with sarcopenic obesity: a randomized controlled trial. J Am Med Dir Assoc. 2016 Nov 1;17(11):1011–19. doi: 10.1016/j.jamda.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Nilsson MI, Mikhail A, Lan L, et al. A five-ingredient nutritional supplement and home-based resistance exercise improve lean mass and strength in free-living elderly. Nutrients. 2020 Aug 10;12(8):2391. doi: 10.3390/nu12082391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nabuco HC, Tomeleri CM, Fernandes RR, et al. Effect of whey protein supplementation combined with resistance training on body composition, muscular strength, functional capacity, and plasma-metabolism biomarkers in older women with sarcopenic obesity: a randomized, double-blind, placebo-controlled trial. Clin Nutr ESPEN. 2019 Aug 1;32:88–95. doi: 10.1016/j.clnesp.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Björkman MP, Suominen MH, Kautiainen H, et al. Effect of protein supplementation on physical performance in older people with sarcopenia—a randomized controlled trial. J Am Med Dir Assoc. 2020;21(2):226–232. doi: 10.1016/j.jamda.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Kang L, Gao Y, Liu X, et al. Effects of whey protein nutritional supplement on muscle function among community-dwelling frail older people: a multicenter study in China. Arch Gerontol Geriatr. 2019 Jul 1;83:7–12. doi: 10.1016/j.archger.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.M146. [DOI] [PubMed] [Google Scholar]
- 25.Kirk B, Mooney K, Amirabdollahian F, Khaiyat O. Exercise and dietary-protein as a countermeasure to skeletal muscle weakness: Liverpool Hope University–Sarcopenia Aging Trial (LHU-SAT) Front Physiol. 2019;445 doi: 10.3389/fphys.2019.00445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirk B, Mooney K, Cousins R, et al. Effects of exercise and whey protein on muscle mass, fat mass, myoelectrical muscle fatigue and health-related quality of life in older adults: a secondary analysis of the Liverpool Hope University–Sarcopenia Ageing Trial (LHU-SAT) Eur J Appl Physiol. 2020 Feb;120(2):493–503. doi: 10.1007/s00421-019-04293-5. [DOI] [PubMed] [Google Scholar]
- 27.Galbreath M, Campbell B, LaBounty P, et al. Effects of adherence to a higher protein diet on weight loss, markers of health, and functional capacity in older women participating in a resistance-based exercise program. Nutrients. 2018 Aug 11;10(8):1070. doi: 10.3390/nu10081070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mori H, Tokuda Y. Effect of whey protein supplementation after resistance exercise on the muscle mass and physical function of healthy older women: a randomized controlled trial. Geriatr Gerontol Int. 2018 Sep;18(9):1398–1404. doi: 10.1111/ggi.13499. [DOI] [PubMed] [Google Scholar]
- 29.Kemmler W, Grimm A, Bebenek M, Kohl M, von Stengel S. Effects of combined whole-body electromyostimulation and protein supplementation on local and overall muscle/fat distribution in older men with sarcopenic obesity: the Randomized Controlled Franconia Sarcopenic Obesity (FranSO) Study. Calcified Tissue Int. 2018 Sep;103(3):266–77. doi: 10.1007/s00223-018-0424-2. [DOI] [PubMed] [Google Scholar]
- 30.Alemán-Mateo H, Macías L, Esparza-Romero J, Astiazaran-García H, Blancas AL. Physiological effects beyond the significant gain in muscle mass in sarcopenic elderly men: evidence from a randomized clinical trial using a protein-rich food. Clin Interv Aging. 2012;7:225–34. doi: 10.2147/CIA.S32356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ten Haaf DS, van Dongen EJ, Nuijten MA, Eijsvogels TM, de Groot LC, Hopman MT. Protein intake and distribution in relation to physical functioning and quality of life in community-dwelling elderly people: acknowledging the role of physical activity. Nutrients. 2018 Apr 19;10(4):506. doi: 10.3390/nu10040506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scott D, Blizzard L, Fell J, Giles G, Jones G. Associations between dietary nutrient intake and muscle mass and strength in community-dwelling older adults: the Tasmanian Older Adult Cohort study. J Am Geriatr Soc. 2010 Nov;58(11):2129–34. doi: 10.1111/j.1532-5415.2010.03147.x. [DOI] [PubMed] [Google Scholar]
- 33.Farsijani S, Morais JA, Payette H, et al. Relation between mealtime distribution of protein intake and lean mass loss in free-living older adults of the NuAge study. Am J Clin Nutr. 2016 Sep;104(3):694–703. doi: 10.3945/ajcn.116.130716. [DOI] [PubMed] [Google Scholar]
- 34.Otsuka R, Kato Y, Tange C, et al. Protein intake per day and at each daily meal and skeletal muscle mass declines among older community dwellers in Japan. Public Health Nutr. 2020 Apr;23(6):1090–97. doi: 10.1017/S1368980019002921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang RY, Yang KC, Chang HH, Lee LT, Lu CW, Huang KC. The association between total protein and vegetable protein intake and low muscle mass among the community-dwelling elderly population in northern Taiwan. Nutrients. 2016 Jun 17;8(6):373. doi: 10.3390/nu8060373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chan R, Leung J, Wo J, Kwok T. Associations of dietary protein intake on subsequent decline in muscle mass and physical functions over four years in ambulant older Chinese people. J Nutr Health Aging. 2014 Feb;18(2):171–77. doi: 10.1007/s12603-013-0379-y. [DOI] [PubMed] [Google Scholar]
- 37.Houston DK, Nicklas BJ, Ding J, et al. Health ABC Study. Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2008 Jan 1;87(1):150–55. doi: 10.1093/ajcn/87.1.150. [DOI] [PubMed] [Google Scholar]
- 38.Li C, Kang B, Zhang T, et al. Dietary pattern and dietary energy from fat associated with sarcopenia in community-dwelling older Chinese People: a cross-sectional study in three regions of China. Nutrients. 2020 Nov 30;12(12):3689. doi: 10.3390/nu12123689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hashemi R, Motlagh AD, Heshmat R, et al. Diet and its relationship to sarcopenia in community dwelling Iranian elderly: a cross sectional study. Nutrition. 2015 Jan 1;31(1):97–104. doi: 10.1016/j.nut.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 40.Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012 Apr 1;11(2):278–96. doi: 10.1016/j.arr.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 41.Rondanelli M, Faliva M, Monteferrario F, et al. Novel insights on nutrient management of sarcopenia in elderly. Biomed Res Int. 2015;2015:524948. doi: 10.1155/2015/524948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ten Haaf DS, Nuijten MA, Maessen MF, Horstman AM, Eijsvogels TM, Hopman MT. Effects of protein supplementation on lean body mass, muscle strength, and physical performance in nonfrail community-dwelling older adults: a systematic review and meta-analysis. Am J Clin Nutr. 2018 Nov 1;108(5):1043–59. doi: 10.1093/ajcn/nqy192. [DOI] [PubMed] [Google Scholar]
- 43.Degens H. The role of systemic inflammation in age-related muscle weakness and wasting. Scand J Med Sci Sports. 2010 Feb;20(1):28–38. doi: 10.1111/j.1600-0838.2009.01018.x. [DOI] [PubMed] [Google Scholar]
- 44.Hairi NN, Cumming RG, Naganathan V, et al. Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitation and physical disability: the Concord Health and Ageing in Men Project. J Am Geriatr Soc. 2010 Nov;58(11):2055–62. doi: 10.1111/j.1532-5415.2010.03145.x. [DOI] [PubMed] [Google Scholar]
- 45.Mijnarends DM, Koster A, Schols JM, et al. Physical activity and incidence of sarcopenia: the population-based AGES-Reykjavik Study. Age Ageing. 2016 May 17;45(5):614–20. doi: 10.1093/ageing/afw090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:835–45. doi: 10.2147/CIA.S132940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taylor D. Physical activity is medicine for older adults. Postgrad Med J. 2014 Jan 1;90(1059):26–32. doi: 10.1136/postgradmedj-2012-131366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoo SZ, No MH, Heo JW, et al. Role of exercise in age-related sarcopenia. J Exerc Rehabil. 2018 Aug;14(4):551–58. doi: 10.12965/jer.1836268.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Finger D, Goltz FR, Umpierre D, Meyer E, Rosa LH, Schneider CD. Effects of protein supplementation in older adults undergoing resistance training: a systematic review and meta-analysis. Sports Med. 2015 Feb;45(2):245–55. doi: 10.1007/s40279-014-0269-4. [DOI] [PubMed] [Google Scholar]
- 50.Gomes-Neto M, da Silva T, Carvalho VO. Whey protein supplementation in association with resistance training on additional muscle strength gain in older adults: a meta-analysis. Sci Sports. 2017 Sep 1;32(4):214–20. doi: 10.1016/j.scispo.2017.03.008. [DOI] [Google Scholar]
- 51.Moore DR. Keeping older muscle “young” through dietary protein and physical activity. Adv Nutr. 2014 Sep;5(5):599–607. doi: 10.3945/an.113.005405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Trumbo P, Schlicker S, Yates AA, Poos M Food and Nutrition Board of the Institute of Medicine, The National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002 Nov;102(11):1621–30. doi: 10.1016/S0002-8223(02)90346-9. [DOI] [PubMed] [Google Scholar]
- 53.Beasley JM, Shikany JM, Thomson CA. The role of dietary protein intake in the prevention of sarcopenia of aging. Nutr Clin Pract. 2013 Dec;28(6):684–90. doi: 10.1177/0884533613507607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Putra C, Konow N, Gage M, York CG, Mangano KM. Protein source and muscle health in older adults: a literature review. Nutrients. 2021 Feb 26;13(3):743. doi: 10.3390/nu13030743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Berrazaga I, Micard V, Gueugneau M, Walrand S. The Role of the anabolic properties of plant- versus animal-based protein sources in supporting muscle mass maintenance: a critical review. Nutrients. 2019 Aug 7;11(8):1825. doi: 10.3390/nu11081825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Granic A, Sayer AA, Robinson SM. Dietary patterns, skeletal muscle health, and sarcopenia in older adults. Nutrients. 2019 Mar 30;11(4):745. doi: 10.3390/nu11040745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McClure R, Villani A. Mediterranean Diet attenuates risk of frailty and sarcopenia: new insights and future directions. JCSM Clin Rep. 2017 Jul;2(2):1–17. doi: 10.17987/jcsm-cr.v2i2.45. [DOI] [Google Scholar]