Abstract
Background
A decline in routine vaccination was reported by some countries early in the COVID-19 pandemic. In the context of the pandemic, determinants of routine childhood vaccination may have changed. Changes over time in parents’ perceptions of routine vaccines and intentions for their children during the pandemic have not been fully explored. Understanding changes provides opportunities to promote routine childhood vaccines and address factors that may compromise parents’ acceptance.
Methods
We conducted longitudinal analysis of two sequential national surveys during the pandemic (Dec 2020 and Oct/Nov 2021) to assess changes over time in Canadian parents’ perceptions of routine childhood vaccines, intentions to vaccinate, access for their children ≤ 17 years, and differences among sociodemographic characteristics. McNemar-Bowker tests were used to determine changes in parents’ responses collected at two time points.
Results
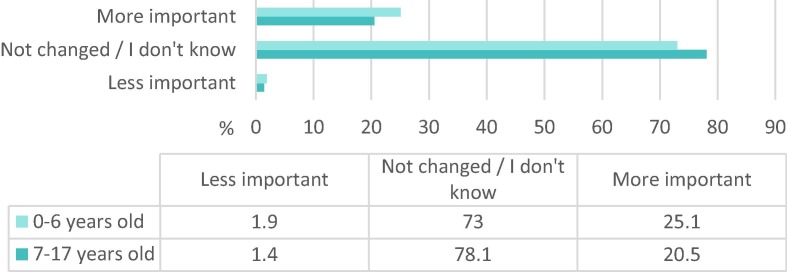
Of the 650 parents in the sample, 25.1% with a child ≤ 6 years and 20.5% with a child 7–17 years perceived that routine childhood vaccines were more important because of the pandemic. Between the two time points, parents’ confidence in the safety (72.8% to 80.2%, p <.001) and effectiveness (81.7% to 85.2%, p =.007) of routine vaccines increased, parents were more engaged in vaccine decision-making (73.4% to 79.8%, p =.006), and everyday stress preventing vaccination decreased (78.8% to 68.5%, p <.001). Acceptance of routine vaccines increased (82.9% to 86.5%, p =.021), but more parents were undecided about influenza vaccination (12.6% to 20.3%, p =.002). Compared to parents with 1 child, those with 2 children reported increased vaccination acceptance (82.6% to 87.4%, p =.024).
Interpretation
Under the spotlight of COVID-19, parents’ confidence in routine vaccines, engagement in decision-making, and vaccination acceptance increased. Vaccination providers should support parents’ decision-making as they navigate routine childhood vaccine uncertainties. Differences in parents’ acceptance of routine and influenza vaccines for their children highlight the need for targeted communication strategies for specific vaccines.
Keywords: Vaccine, Immunization, Child, Parents, COVID-19, Pandemic, Routine
1. Introduction
SARS-CoV-2 has raised global awareness of the importance of infectious disease prevention, highlighting vaccine innovation and its critical role in the transition from pandemic to endemic [1]. The focus on COVID-19 vaccination raises questions about whether the pandemic has influenced perceptions towards existing routine childhood vaccines and parents’ intentions to vaccinate. Prior to the pandemic, significant research focused on vaccine hesitancy as a key determinant of low routine childhood vaccination uptake [2], [3], [4], [5]. As posed by Harrison and Wu [6], “Will COVID-19 fix the problem of vaccine hesitancy?”.
A stark decline in routine childhood vaccination was reported by many countries during the first waves of the pandemic (i.e., 2020 and 2021) [7], [8], [9], [10], [11], [12], [13], while others experienced an increase in uptake [14]. In 2019 before the COVID-19 pandemic, 78% of 2-year-old children in Canada had received all recommended doses of pertussis-containing vaccine [15], with a notable decline in coverage reported in some provinces at the start of the pandemic (i.e., March-July 2020) [16], [17]. Declines were often attributed to stay-at-home orders, school closures, constraints on health resources and services (i.e., access to personal protective equipment, facility closures), and parents’ fear of COVID-19 transmission when accessing vaccine services [7], [16], [17], [18], [19]. Regional [20], national [21], [22], and international [23], [24] immunization regulatory bodies provided urgent recommendations outlining the importance of continued vaccination services during the pandemic, fearing infectious disease outbreaks in at-risk populations [25], [26]. Although routine vaccination rates trended towards pre-pandemic levels by January 2021, many regions reported time-delays in recommended coverage targets specific to the vaccine and age of the child [16], [17], [18], [19], [27]. These studies focus on administrative data and compare routine vaccination rates early in the pandemic to pre-pandemic levels. Few studies [28], [29] have explored changes over time during the pandemic, in parents’ perceptions of routine vaccines and their intentions to vaccinate their children.
The determinants of routine childhood vaccination may have changed within the context of the COVID-19 pandemic. Exploring these changes may present a timely opportunity for health officials and policy makers to identify areas to improve vaccination for a potentially captive audience. Therefore, this longitudinal study explores a national sample of parents’ perceptions of routine childhood vaccines, intentions to vaccinate, and access to routine vaccines for their child(ren) ≤ 17 years at two time points during the pandemic, and whether changes in vaccine acceptance vary by sociodemographic characteristics.
2. Methods
2.1. Study design and participants
We conducted two cross-sectional national online surveys with respondents selected from a panel of > 400,000 Canadians from a well-established national polling firm [30]. Initial data collection occurred December 10–24 2020 just as the first COVID-19 vaccine, BNT162b2 (Pfizer-BioNTech), was approved by Health Canada, with prioritized administration for adults most at risk for COVID-19 disease (i.e., long term care residents and healthcare workers) [31]. COVID-19 vaccines were readily available for those ≥ 12 years during the second data collection period (Oct 14 - Nov 12, 2021), however COVID-19 vaccination had not yet been approved for children aged 5–11 years [32]. The overall sample for each survey (Survey 1, Dec 2020, N = 5028; Survey 2, Oct/Nov 2021, N = 6,026) was representative for population size in all provinces, and by sex and age, based on data from the latest Census [33]. Respondents were adults who had access to the internet and were proficient in reading English or French. To ensure rigor and validity [34], respondents had unique URLs and 15% of respondents were contacted by telephone for identity verification.
We purposively sampled minimum quotas of targeted populations. This included a quota of respondents who identified as being a primary caregiver to one or more children ≤ 17 years of age in their home. For longitudinal analysis, parents from 10 Canadian provinces who responded to both surveys were included in this study (N = 650). Two age groups were assessed: children 0–6 years and 7–17 years old. Consistent with other studies [35], [36], if parents had multiple children within an age group, they were asked to respond for their youngest child in that group. We estimated the minimal sample size of the target parent population to be 402, based on the maximum variability possible in the outcome variable in the population (i.e., a proportion of 0.50), with a margin of error of +/- 5% and 95% confidence intervals (CI).
Each of the approximately 75-question online surveys took an average of 19 minutes to complete. The survey instrument was developed by drawing from a previous survey of Canadians’ acceptance of routine childhood vaccines [35], previously validated questions about perceptions of vaccination (i.e., 5C’s psychological antecedents of vaccination) [37], areas of focus for our policy partners (including the National Advisory Committee on Immunization Secretariat), and the expertise of our national team of immunization researchers and policy advisors. The draft questionnaires were reviewed by public health experts, pre-tested with team members, and pilot tested with members of the public and revised accordingly. This study received approval from the Health Research Ethics Board at the University of Alberta.
2.2. Measures
Our primary focus was the proportion and direction of difference between each variable at two points during the pandemic to assess for changes in parents’ perceptions and intentions over time. Variables were based on determinants of routine vaccination and included parents’ confidence in the safety, necessity, and effectiveness of routine vaccines, vaccination as a collective action to prevent the spread of disease, vaccination decision-making, competing priorities that prevent vaccination, mandated vaccination, routine childhood and influenza vaccination intention and receipt before and during the pandemic, and a direct question that asked how the pandemic had changed the way that parents think about routine vaccines. Sociodemographic variables included: province, age, level of education, employment status, annual household income, gender, relationship status, number and ages of children, self-identified ethnicity, citizenship, new to Canada in the past 5 years, and languages most often spoken at home. Survey questions are provided in the Appendix (Table A1).
2.3. Statistical analysis
We calculated descriptive statistics (i.e., frequencies and percentages) for variables at each data collection time point. Respondents’ paired data from survey 1 and survey 2 were analyzed using the McNemar-Bowker test with a significance level of 0.05 and 95% CIs to assess differences in participants’ responses to the same survey question at two time points during the pandemic. Sociodemographic factors from survey 2 were analyzed to reflect the most recent demographic data, including stratification by key characteristics. Post hoc tests were used to correct for multiple comparisons and stratum (i.e., Bonferroni's correction and Stuart–Maxwell test marginal homogeneity in a square table with more than two columns/rows). No data were missing due to the online survey completion requirements. We analyzed data using SPSS version 26.0 (IBM, Chicago, IL, USA).
3. Results
3.1. Sociodemographic characteristics of parent sample
The sample of parents who answered both surveys (N = 650) was proportionately representative of the national population by self-identified ethnicity, language spoken most often at home, citizenship, marital status of parents, and number of children [38]. As seen in Table 1 , 65.4% of parents were from the provinces of Ontario and Quebec, followed by Alberta and British Columbia (21.4%), and 77.2% were between the ages of 30–49. Over half of parents had a university degree (59.5%), an annual household income ≥ $80,000 (56.6%), and 74.2% were employed full-time. Over half of respondents identified as a woman (55.4%), 86.5% were married or in a common-law relationship. Half of parents had 1 child (50.9%), with the remaining parents having 2 or more children (49.1%). One-third of parents (32.6%) had only preschool-aged children (0–6 years), 52.2% only had school-aged children (7–17 years), and 15.2% had children in both age categories. Two-thirds of parents self-identified as White (62.3%), were a Canadian citizen by birth (68.8%), and spoke English most often at home (61.1%). Thirty-seven percent of parents self-identified as a Racialized minority and 8.2% of parents were new to Canada within the past 5 years.
Table 1.
Sociodemographic characteristics of parents of children ≤ 17 years old (N = 650).
| Characteristicsa | Category | n (%) |
|---|---|---|
| Province of residence | British Columbia | 68 (10.5) |
| Alberta | 71 (10.9) | |
| Saskatchewan and Manitoba | 47 (7.2) | |
| Ontario | 241 (37.1) | |
| Quebec | 184 (28.3) | |
| Atlantic provincesb | 39 (6.0) | |
| Age | 15–29 years | 46 (7.1) |
| 30–39 years | 231 (35.5) | |
| 40–49 years | 271 (41.7) | |
| 50–59 years | 96 (14.8) | |
| ≥ 60 years | 6 (0.9) | |
| Highest level of education | High school or less | 61 (9.4) |
| Non-university certificate or diploma (college/apprenticeship) | 196 (30.2) | |
| University degree/Bachelor’s or more than a Bachelor’s | 387 (59.5) | |
| Prefer not to answer | 6 (0.9) | |
| Employment status | Full-time (≥37 h per week) | 482 (74.2) |
| Part-time (<37 h per week) | 73 (11.2) | |
| Unemployed | 77 (11.8) | |
| Prefer not to answer | 18 (2.8) | |
| Annual household income | < $40,000 | 58 (8.9) |
| $40,000–79,000 | 170 (26.2) | |
| ≥ $80,000 | 368 (56.6) | |
| Prefer not to answer | 54 (8.3) | |
| Gender | Woman | 360 (55.4) |
| Man | 288 (44.3) | |
| Gender minority | 2 (0.3) | |
| Relationship status | Not married | 85 (13.1) |
| Married/common-law | 562 (86.5) | |
| Prefer not to answer | 3 (0.5) | |
| Number of children in household (0–17 years old) | 1 child | 331 (50.9) |
| 2 children | 247 (38.0) | |
| 3 or more children | 72 (11.1) | |
| Parents with a preschool and/or schoolaged child(ren) | Preschool aged child(ren) (0–6 years old) only | 212 (32.6) |
| School aged child(ren) (7–17 years old) only | 339 (52.2) | |
| Preschool and school-aged children (0–6 & 7–17 years) | 99 (15.2) | |
| Ethnic or cultural origin | White | 405 (62.3) |
| Racialized minorityc | 207 (31.8) | |
| Indigenousd | 34 (5.2) | |
| Prefer not to answer | 4 (0.6) | |
| Citizenship | Canadian citizen by birth | 447 (68.8) |
| Canadian citizen by immigration | 135 (20.8) | |
| Permanent residente | 55 (8.7) | |
| Temporary residentf | 12 (1.9) | |
| Prefer not to answer | 1 (0.2) | |
| New to Canada within the last 5 years | Yes | 53 (8.2) |
| No | 597 (91.8) | |
| Language spoken most often at home | English | 397 (61.1) |
| French | 162 (24.9) | |
| Other languages | 91 (14.0) |
Sociodemographic characteristics provided from survey 2; data collection October/November 2021.
Atlantic provinces include Prince Edward Island, Nova Scotia, New Brunswick, and Newfoundland and Labrador.
Racialized minority groups including Black, Latin/Central American, Arabic/West Asian/North African, East Asian, South Asian, and any respondents who selected one of these groups and White.
Indigenous respondents are individuals who self-identified as First Nations, Métis, or Inuk.
Permanent resident refers to a landed immigrant.
Temporary resident includes non-permanent residents, such as those in Canada on a work or study visa.
4. Parents’ perceptions of routine vaccination during the COVID-19 pandemic
Fig. 1 shows that 25.1% of parents with a child aged 0–6 years and 20.5% of parents with a child aged 7–17 years reported in survey 2 (Oct/Nov 2021) that they perceived routine childhood vaccines as being more important because of the COVID-19 pandemic.
Fig. 1.
How the pandemic has changed parents’ perceptions of routine childhood vaccines, as reported in survey 2. Note: variable data collection occurred only during survey 2, therefore change over time is not reported.
As seen in Table 2 , there were statistically significant increases over time in parents’ confidence in routine vaccines (72.8% to 80.2%, p <.001), agreement that they weigh the benefits and risks of vaccination to make the best decision possible (73.4% to 79.8%, p =.006), and that routine vaccines are effective (81.7% to 85.2%, p =.007). Parents increasingly disagreed that everyday stress would prevent them from getting a routine vaccine over time (68.5% to 78.8%, p <.001). There was an increase over time in parents’ acceptance of routine childhood vaccines during the pandemic (82.9% to 86.5%, p =.021), and a decrease in parents who reported no intent/no receipt of routine childhood vaccines (12.5% to 8.3%, p =.021). Finally, parents were increasingly undecided about vaccinating their children against influenza (12.6% to 20.3%, p =.002).
Table 2.
Changes in parents’ responses at two time points during the pandemic.
| Variable | Category | Survey 1 Dec 2020 n (%) |
Survey 2 Oct/Nov 2021 n (%) |
McNemar Bowker p-value |
|---|---|---|---|---|
| Parents’ perceptions of routine vaccines | ||||
| How has the pandemic changed the way you think about routine vaccines in general?a | Routine vaccines are more important | 149 (22.9) | 176 (27.1) | p =.166 |
| The pandemic has not changed how I think about routine vaccines | 480 (73.8) | 459 (70.6) | ||
| Routine vaccines are less important | 21 (3.2) | 15 (2.3) | ||
| I am completely confident that routine vaccines are safea | Agree, more likely to vaccinate | 473 (72.8) | 521 (80.2) |
p <.001 |
| Neutral | 112 (17.2) | 78 (12.0) | ||
| Disagree, less likely to vaccinate | 65 (10.0) | 51 (7.8) | ||
| Routine vaccination is necessary because vaccine-preventable diseases are commona | Agree, more likely to vaccinate | 476 (73.2) | 457 (70.3) | p =.268 |
| Neutral | 98 (15.1) | 97 (14.9) | ||
| Disagree, less likely to vaccinate | 76 (11.7) | 96 (14.8) | ||
| Vaccination is a collective action to prevent the spread of diseasea | Agree, more likely to vaccinate | 550 (84.6) | 559 (86.0) | p =.698 |
| Neutral | 64 (9.8) | 55 (8.5) | ||
| Disagree, less likely to vaccinate | 36 (5.5) | 36 (5.5) | ||
| When I think about getting vaccinated, I weigh the benefits and risks to make the best decision possiblea | Agree, more likely to vaccinate | 477 (73.4) | 519 (79.8) |
p =.006 |
| Neutral | 110 (16.9) | 94 (14.5) | ||
| Disagree, less likely to vaccinate | 63 (9.7) | 37 (5.7) | ||
| Everyday stress (such as competing priorities or many demands on my time) prevents me from getting vaccinateda | Disagree, more likely to vaccinate | 445 (68.5) | 512 (78.8) |
p <.001 |
| Neutral | 130 (20.0) | 68 (10.5) | ||
| Agree, less likely to vaccinate | 75 (11.8) | 70 (10.8) | ||
| Vaccines are effectivea | Agree | 531 (81.7) | 554 (85.2) |
p =.007 |
| Neutral | 90 (13.8) | 57 (8.8) | ||
| Disagree | 29 (4.5) | 39 (6.0) | ||
| It should be mandatory for children to get the recommended childhood vaccines | Agree | 456 (70.2) | 445 (68.5) | p =.207 |
| Neutral | 106 (16.3) | 109 (16.8) | ||
| Disagree | 88 (13.5) | 96 (14.8) | ||
| Routine childhood and influenza vaccine acceptance | ||||
| Parents’ routine childhood vaccination intent/receipt for their children during the COVID-19 pandemic | Intent/receipt | 539 (82.9) | 562 (86.5) |
p =.021 |
| No intent/no receipt | 81 (12.5) | 54 (8.3) | ||
| I don’t know | 30 (4.6) | 34 (5.2) | ||
| Child’s reported receipt of seasonal influenza vaccinebc | Received | 279 (42.9) | 252 (38.8) | p =.087 |
| Not received | 349 (53.7) | 367 (56.5) | ||
| Not eligible | 11 (1.7) | 19 (2.9) | ||
| I don’t remember | 11 (1.7) | 12 (1.8) | ||
| Parents’ influenza vaccination intent for their childrenc, d |
Intent to vaccinate | 296 (45.5) | 277 (42.6) |
p =.002 |
| Undecided | 82 (12.6) | 132 (20.3) | ||
| No intent to vaccinate | 256 (39.4) | 221 (34.0) | ||
| Not eligible | 16 (2.5) | 20 (3.1) | ||
Parents responded in reference to routine vaccines in general, not specific to routine childhood vaccines.
Parents reported children’s receipt of seasonal influenza vaccine for the 2019–2020 influenza season in survey 1, and for the 2020–2021 influenza season in survey 2.
Influenza vaccination is not publicly funded for healthy children in some Canadian provinces.
Parents reported intention to vaccinate their child against influenza for the 2020–2021 influenza season in survey 1, and the 2021–2022 influenza season in survey 2.
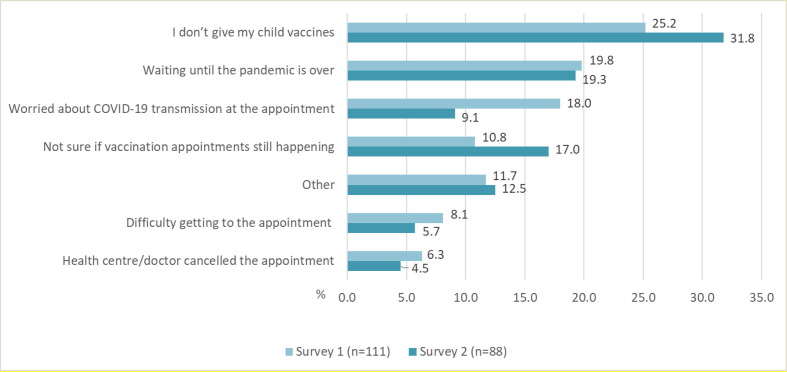
Of the 111 parents in survey 1 who were uncertain or would not accept routine childhood vaccination during the pandemic, 19.8% reported that they were waiting for the pandemic to be over and 18.0% were worried about COVID-19 transmission at the appointment (Fig. 2 ). Of the 88 parents in survey 2 who were uncertain or would not accept routine childhood vaccination during the pandemic, parents were less concerned about COVID-19 transmission at the appointment (9.1%), were waiting for the pandemic to be over (19.3%), or were not sure if appointments were happening (17.0%).
Fig. 2.
Parents’ reasons for not accepting routine childhood vaccines during the pandemic, among parents who indicated they were uncertain or declining routine vaccines.
Table 3 shows parents’ acceptance of routine childhood vaccines stratified by sociodemographic characteristics. Compared to other provinces, those from Ontario reported an increase over time in vaccine acceptance for their children during the pandemic (80.4% to 87.1%, p =.007) and a decrease in no intent/no receipt (15.4% to 7.5%, p =.007). Parents with 2 children reported an increase over time in routine vaccine acceptance for their children (82.6% to 87.4%, p =.024), and a decrease in no intent/no receipt (11.3% to 6.1%, p =.024), compared to parents with 1 child. No other sociodemographic factors were significant (see Appendix Table A2).
Table 3.
Routine childhood vaccine acceptance during the pandemic stratified by sociodemographic characteristics.
| Variable | Category | Survey 1 n (%) | Survey 2 n (%) | McNemar p-value |
|
|---|---|---|---|---|---|
| Language | English (n = 397) |
Intent/receipt | 327 (82.4) | 343 (86.4) | p =.15 |
| No intent/no receipt | 51 (12.8) | 35 (8.8) | |||
| I don't know | 19 (4.8) | 19 (4.8) | |||
| French (n = 162) |
Intent/receipt | 136 (84) | 138 (85.2) | p =.103 |
|
| No intent/no receipt | 18 (11.1) | 10 (6.2) | |||
| I don’t know | 8 (4.9) | 14 (8.6) | |||
| Other (n = 91) |
Intent/receipt | 76 (83.5) | 81 (89.0) | p =.429 |
|
| No intent/no receipt | 12 (13.2) | 9 (9.9) | |||
| I don’t know | 3 (3.3) | 1 (1.1) | |||
| Province | British Columbia and Prairiesa (n = 186) |
Intent/receipt | 155 (83.3) | 161 (86.6) | p =.559 |
| No intent/no receipt | 20 (10.8) | 18 (9.7) | |||
| I don’t know | 11 (5.9) | 7 (3.8) | |||
| Ontario (n = 241) |
Intent/receipt | 194 (80.5) | 210 (87.1) |
p =.007 |
|
| No intent/no receipt | 37 (15.4) | 18 (7.5) | |||
| I don’t know | 10 (4.1) | 13 (5.4) | |||
| Quebec (n = 184) |
Intent/receipt | 155 (84.2) | 159 (86.4) | p =.053 |
|
| No intent/no receipt | 21 (11.4) | 12 (6.5) | |||
| I don’t know | 8 (4.3) | 13 (7.1) | |||
| Atlantic (n = 39) |
Intent/receipt | 35 (89.7) | 32 (82.1) | p =.407 |
|
| No intent/no receipt | 3 (7.7) | 6 (15.4) | |||
| I don’t know | 1 (2.6) | 1 (2.6) | |||
| Number of Children | 1 child (n = 331) |
Intent/receipt | 278 (84.0) | 285 (86.1) | p =.488 |
| No intent/no receipt | 42 (12.7) | 32 (9.7) | |||
| I don’t know | 11 (3.3) | 14 (4.2) | |||
| 2 children (n = 247) |
Intent/receipt | 204 (82.6) | 216 (87.4) |
p =.024 |
|
| No intent/no receipt | 28 (11.3) | 15 (6.1) | |||
| I don’t know | 15 (6.1) | 16 (6.5) | |||
| ≥ 3 children (n = 72) |
Intent/receipt | 57 (79.2) | 61 (84.7) | p =.611 |
|
| No intent/no receipt | 11 (15.3) | 7 (9.7) | |||
| I don’t know | 4 (5.6) | 4 (5.6) | |||
Prairie provinces include Alberta, Saskatchewan, and Manitoba (collapsed due to sample size).
Table 4 shows parents’ reported vaccination status of their children before the pandemic, in comparison with parents’ vaccine acceptance for their children at two points during the pandemic. Compared to children’s pre-pandemic vaccination status, parents of children aged 0–6 and 7–17 years reported a decrease in routine vaccine acceptance at the time of survey 1 (93.5% to 85.5% and 92% to 80.9% respectively). Parents reported a slight increase in routine vaccine acceptance for survey 2 (89.7% and 84.9% respectively). However, these results are not significant, as CIs overlap.
Table 4.
Parents’ acceptance of routine childhood vaccines before and during the pandemic.
| Variable | Category | Survey 1 Pre-pandemica receipt % (CI), n |
Survey 1 Dec 2020 intent/receipt % (CI), n |
Survey 2 Oct/Nov 2021 intent/receipt % (CI), n |
|---|---|---|---|---|
| Parents of preschool-aged children (0–6 years) routine childhood vaccination intent/receipt (survey 1 N = 388; survey 2 N = 311)b |
Intent/receipt | 93.5 (87.4–97.1), 316 |
85.5 (77.6–91.4), 289 |
89.7 (82.6–94.5), 279 |
| No intent/no receipt | 5.3 (2.1–11), 18 |
12.4 (7.0–19.9), 42 |
7.7 (3.7–14.1), 24 |
|
| I don’t know | 1.2 (0.2–4.9), 4 |
2.1 (0.5–6.4), 7 |
2.6 (0.7–7.2), 8 |
|
| Parents of school-aged children (7–17 years) routine childhood vaccination intent/receipt (survey 1 N = 423; survey 2 N = 438)b |
Intent/receipt | 92.0 (85.5–96.1), 389 |
80.9 (72.4–87.7), 342 |
84.9 (76.9–90.9), 372 |
| No intent/no receipt | 5.7 (2.4–11.6), 24 |
13.9 (8.2–21.7), 59 |
10.0 (5.3–17.0), 44 |
|
| I don’t know | 2.4 (0.6–6.9), 10 |
5.2 (2.1–10.9), 22 |
5.0 (1.9–10.6), 22 |
|
| Parents of children aged 0–17 years routine childhood vaccination intent/receiptc (N = 650) | Intent/receipt | 92.3 (85.9–96.3), 600 |
82.9 (74.6–89.3), 539 |
86.5 (78.8–92.1), 562 |
| No intent/no receipt | 5.8 (2.4–11.7), 38 |
12.5 (7.1–20.0), 81 |
8.3 (4.1–14.9), 54 |
|
| I don’t know | 1.8 (0.3–5.9), 12 |
4.6 (1.7–10.1), 30 |
5.2 (2.1–10.9), 34 |
Pre-pandemic routine childhood vaccination status reported by parents in Survey 1, Dec 20, 2020.
Differences in survey 1 and survey 2 N is due to children changing age groups between data collection points.
Variable for parents with children 0–6 years and 7–17 years old combined. Responses of parents who had a child in each age group (0–6 years and 7–17 years old), and who answered both “received” and “not received” was coded as “I don’t know.”
5. Discussion
5.1. Changes in parents’ perceptions of routine childhood vaccines
In October/November 2021 during the second wave of the COVID-19 pandemic [i.e., when the Delta variant (B.1.617.2) was prominent and prior to the Omicron variant (B.1.1.529)], almost 25% of parents in our study reported that they perceived routine childhood vaccination as being more important as a result of the COVID-19 pandemic. We found an increase over time in parents’ perceived importance of routine vaccines in general (e.g., childhood and adult routine vaccines) and significant increases in parents’ reported confidence in their safety and effectiveness. Findings suggest that the COVID-19 pandemic has positively influenced Canadian parents’ perceptions about the importance of routine vaccines in preventing infectious diseases. Conversely, a study from the United States [29] found an increase in parents' routine childhood vaccine hesitancy and risk perception, and unchanged confidence in routine vaccines during the pandemic (September 2020 - February 2021). However, this was a regional study (N = 252) and measures of perceived risk and confidence in routine vaccines focused on trustworthiness in government and health systems [4], [29]. Therefore, differences in population characteristics, government policy, and vaccine delivery may account for discrepancies.
Parents in our study reported an increase over time in weighing the benefits and risks of routine vaccines when engaging in decision-making. It is possible that the global attention on the benefits, risks, and efficiency of COVID-19 vaccines in conjunction with parents’ ongoing (over a long period of time) active engagement in COVID-19 vaccine decision-making for their children, may have translated into active engagement in routine vaccine decision-making. Research has shown that trusting relationships with health care providers supports parents’ confidence and acceptance of routine vaccines when deciding whether to vaccinate their children [4], [18]. Our results demonstrate that under the spotlight of the pandemic, parents are actively weighing the benefits and risks of routine vaccines. Therefore, a critical opportunity exists for frontline care providers to support parents’ decision-making as they navigate vaccination uncertainties.
Over time more parents agreed that everyday stress would not prevent access to routine vaccines, suggesting that everyday stressors were perceived less as a barrier to accessing vaccines as the pandemic progressed. Along with increased perceptions of the importance, safety, and effectiveness of routine vaccines, parents in our study may have been more motivated to actively overcome perceived barriers to accessing routine vaccines. It is noteworthy that parents in Canada were less likely to encounter barriers to accessing routine childhood vaccines later in the pandemic due to the resumption of preschool-aged and school-based vaccination programs [39], [40].
5.2. Changes in parents’ acceptance of routine and influenza vaccines
We found a significant increase over time in parents' acceptance of routine vaccines for their children during the pandemic. Results may be explained in-part by parents’ perceptions that routine childhood vaccines were more important, safe, and effective. It is also noteworthy that parents’ lower acceptance reported in December 2020 may be reflective of stay-at-home measures [7], [16], school and vaccination service disruptions [40], initial absence of COVID-19 vaccines (i.e., Pfizer-BioNTech was approved in Canada December 9, 2020) [41], and fear of COVID-19 transmission at vaccination appointments [8], [12], [18]. Accordingly, our results suggest that parents were more concerned about COVID-19 transmission at vaccination appointments in December 2020 than they were in October/November 2021, when COVID-19 vaccines were widely accepted and available for persons aged 12 year and older within Canada [42]. Furthermore, parents in our study reported high routine childhood vaccination receipt before the pandemic, with a marked decrease in routine childhood vaccine acceptance in December 2020, and subsequent increasing acceptance in October/November 2021. Results are consistent with other Canadian [17], [19], [27] and international [9], [10] studies that found a significant decrease in routine childhood vaccination rates early in the pandemic, compared to before the pandemic, with a gradual recovery in vaccination rates as the pandemic progressed. Data collection in our study occurred prior to the more contagious COVID-19 Omicron variant (B.1.1.529), which may have further affected parents’ perceptions and acceptance of routine childhood vaccines.
A pan-Canadian environmental scan [40] from our research team reported disruptions to routine childhood vaccination services in all provinces. Of particular interest are differences in the recovery of vaccination rates between provinces, which are likely influenced by differences in vaccine service delivery. Studies conducted in provinces whose preschool-aged and infant vaccinations are primarily administered by nurses in community health centres reported a return to pre-pandemic vaccination rates by May/June 2020 [17], [27]. In Ontario, preschool-aged and infant routine vaccines are primarily administered by family physicians and pediatricians, therefore were directly impacted by the suspension of in-person appointments [19], [43]. Accordingly, studies found continued delays in the recovery of routine vaccination rates and coverage as late as Nov/Dec 2020 [16], [19], [44], [45]. Parents from Ontario in our study also reported the lowest routine vaccination acceptance in December 2020, compared to other provinces, with the highest increase in acceptance October/November 2021. Results suggest that routine childhood vaccination delivery methods in Ontario were more negatively impacted by public health measures to prevent the spread of COVID-19 than other provinces. In 2020, the World Health Organization's list of 13 global health threats for the next decade included delivering health during crises and stopping infectious diseases [46]. Thus, it is critical that the delivery of routine childhood vaccines is safeguarded through tailored strategies that ensure accessibility and inclusion [18], [26].
Finally, over time parents were increasingly undecided about whether to vaccinate their children against influenza. Similar to our study, Sokol and Grummon [47] found that the COVID-19 pandemic may exacerbate polarity between routine childhood and influenza vaccination, with a marked decrease in parents' influenza vaccination intentions for their children. Childhood influenza vaccination is typically lower than that of routine vaccines [48], [49], with parents reporting concerns with its necessity and effectiveness compared to routine childhood vaccines [5]. In the context of the COVID-19 pandemic, determinants of influenza vaccination in children are poorly understood. Considering the low prevalence of influenza disease during the pandemic, it is possible that parents prioritized COVID-19 and routine vaccines over influenza vaccine for their children.
5.3. Strengths and limitations
We collected novel information from a nationally representative sample of parents at two critical time points during the pandemic, just as the first COVID-19 vaccine was approved for persons ≥ 18 years in Canada, and before their approval in those aged 5–11 years. Our study captured how parents’ perceptions and intentions about routine childhood vaccines were influenced by the COVID-19 pandemic, and how these factors changed overtime. However, our sample was selected from a pre-existing panel of individuals, so even though representative by province, age, and sex, respondents may have characteristics and responses different from the general Canadian population. Data were self-reported, therefore some variables (i.e., children’s pre-pandemic routine vaccination status) may be affected by recall and desirability bias. Finally, parents’ routine vaccination intentions and receipt of vaccines for their children were collected as one variable in our survey. Intentions to vaccinate may not translate into future receipt of vaccines, therefore further research is needed to understand whether differences in parents’ perceptions and intentions for their children have influenced the behavior of routine vaccine uptake.
6. Conclusion
Routine vaccination is an effective public health intervention that prevents the transmission of infectious diseases. The COVID-19 pandemic has highlighted the importance of vaccination in the prevention of COVID-19 disease, which consequently has highlighted the importance of routine vaccines. Our study demonstrates that the pandemic has positively influenced parents’ confidence in and acceptance of routine vaccines for their children. As the pandemic progressed, parents were increasingly engaged in vaccine decision-making and motivated to overcome barriers to access vaccines. Therefore, within the spotlight of the COVID-19 pandemic, a unique opportunity exists for vaccine service providers to support parents’ decision-making as they navigate routine vaccine uncertainties. Differences in parents’ acceptance of routine and influenza vaccines for their children highlight the need for targeted communication strategies for specific vaccines.
Authors’ Statement: All authors attest that they meet the ICMJE criteria for authorship.
Funding: This work was funded by the Canadian Institutes of Health Research.
Contributors:
RH was involved in conceptualization, investigation, formal analysis, interpretation of findings, writing (original draft, review, and editing).
SM, SS, JO, ED were involved in conceptualization, interpretation of findings, writing (review and editing).
SM provided supervision and funding acquisition.
All authors approved the final version.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research is part of a larger project conducted by the COVImm study team. We express thanks to Applied Immunization (AImm) Research Program team member Ali Assi, who provided administration support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.11.052.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The data that has been used is confidential.
References
- 1.Alshrari A.S., Hudu S.A., Imran M., Asdaq S.M.B., Ali A.M., Rabbani S.I. Innovations and development of Covid-19 vaccines: A patent review. J Infect Public Health. 2022;15(1):123–131. doi: 10.1016/j.jiph.2021.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang E., Baras Y., Buttenheim A.M. “Everybody just wants to do what’s best for their child”: Understanding how pro-vaccine parents can support a culture of vaccine hesitancy. Vaccine. 2015;33(48):6703–6709. doi: 10.1016/j.vaccine.2015.10.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gowda C., Dempsey A.F. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1755–1762. doi: 10.4161/hv.25085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gust D.A., Darling N., Kennedy A., Schwartz B. Parents with doubts about vaccines: Which vaccines and reasons why. Pediatrics. 2008 Oct;122(4):718–725. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- 5.Kempe A., Saville A.W., Albertin C., Zimet G., Breck A., Helmkamp L., et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics. 2020 Jul 1;146(1):e20193852. doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrison E.A., Wu J.W. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. 2020;35(4):325–330. doi: 10.1007/s10654-020-00634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abu-rish E.Y., Bustanji Y., Abusal K. Nationwide Routine Childhood Vaccination Coverage During the COVID-19 Pandemic in Jordan: Current Situation, Reasons, and Predictors of Vaccination. Int J Clin Pract (Esher) 2022;2022:7918604. doi: 10.1155/2022/7918604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adamu A.A., Jalo R.I., Habonimana D., Wiysonge C.S. COVID-19 and routine childhood immunization in Africa: Leveraging systems thinking and implementation science to improve immunization system performance. Int J Infect Dis. 2020;98:161–165. doi: 10.1016/j.ijid.2020.06.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDonald H., Tessier E., White J.M., Woodruff M., Knowles C., Bates C., et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro surveillance: bulletin européen sur les maladies transmissibles. 2020;25(19):7–12. doi: 10.2807/1560-7917.ES.2020.25.19.2000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moura C., Truche P., Sousa Salgado L., Meireles T., Santana V., Buda A., et al. The impact of COVID-19 on routine pediatric vaccination delivery in Brazil. Vaccine. 2022;40(15):2292–2298. doi: 10.1016/j.vaccine.2022.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ota M.O.C., Badur S., Romano-Mazzotti L., Friedland L.R. Impact of COVID-19 pandemic on routine immunization. Ann Med (Helsinki) 2021;53(1):2286–2297. doi: 10.1080/07853890.2021.2009128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shapiro G.K., Gottfredson N., Leask J., Wiley K., Ganter-Restrepo F.E., Jones S.P., et al. COVID-19 and missed or delayed vaccination in 26 middle- and high-income countries: An observational survey. Vaccine. 2022;40(6):945–952. doi: 10.1016/j.vaccine.2021.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma M., Singh S., Sharma L., Dwiwedi M., Agarwal D., Gupta G., et al. Magnitude and causes of routine immunization disruptions during COVID-19 pandemic in developing countries. J Family Med Prim Care. 2021;10(11):3991–3997. doi: 10.4103/jfmpc.jfmpc_1102_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McQuaid F., Mulholland R., Sangpang Rai Y., Agrawal U., Bedford H., Cameron J.C., et al. Uptake of infant and preschool immunisations in Scotland and England during the COVID-19 pandemic: An observational study of routinely collected data. PLoS Med. 2022;19(2):e1003916. doi: 10.1371/journal.pmed.1003916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Government of Canada. Highlights from the 2019 childhood National Immunization Coverage Survey (cNICS) [Internet]. Ottawa: Public Health Agency of Canada; 2022 Feb 7 [cited 2022 Nov 7]. Available from: https://www.canada.ca/en/public-health/services/publications/vaccines-immunization/2019-highlights-childhood-national-immunization-coverage-survey.html.
- 16.Ji C., Piché-Renaud P.P., Apajee J., Stephenson E., Forte M., Friedman J.N., et al. Impact of the COVID-19 pandemic on routine immunization coverage in children under 2 years old in Ontario, Canada: A retrospective cohort study. Vaccine. 2022;40(12):1790–1798. doi: 10.1016/j.vaccine.2022.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDonald S.E., Paudel Y.R., Kiely M., Rafferty E., Sadarangani M., Robinson J.L., et al. Impact of the COVID-19 pandemic on vaccine coverage for early childhood vaccines in Alberta, Canada: a population-based retrospective cohort study. BMJ. 2022;12(1):e055968. doi: 10.1136/bmjopen-2021-055968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chanchlani N., Buchanan F., Gill P.J. Addressing the indirect effects of COVID-19 on the health of children and young people. Can Med Assoc J. 2020;192(32):E921–E927. doi: 10.1503/cmaj.201008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dong A., Meaney C., Sandhu G., De Oliveira N., Singh S., Morson N., et al. Routine childhood vaccination rates in an academic family health team before and during the first wave of the COVID-19 pandemic: a pre-post analysis of a retrospective chart review. Can Med Assoc J. 2022;10(1):E43–E49. doi: 10.9778/cmajo.20210084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.BC Centre for Disease Control. Continuity, prioritization and safe delivery of immunization services during COVID-19 response [Internet]. BC Ministry of Health; 2021 Oct 15 [cited 2022 Apr 25]. Available from: http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Epid/CD%20Manual/Chapter%202%20-%20Imms/Continuity_of_Immunization_Services_During_COVID-19.pdf.
- 21.National Advisory Committee on Immunization (NACI). Interim guidance on continuity of immunization programs during the COVID-19 pandemic [Internet]. Ottawa: Government of Canada; 2020 May 13 [cited 2022 Apr 25]. Available from: https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/interim-guidance-immunization-programs-during-covid-19-pandemic.html.
- 22.Canadian Paediatric Society. Stick to immunization schedule during the COVID-19 pandemic, pediatricians urge [Internet]. Ottawa: Canadian Paediatric Society; 2020 Apr 30 [cited 2022 Apr 25]. Available from: https://cps.ca/media/stick-to-immunization-schedule-during-the-covid-19-pandemic.
- 23.World Health Organization. WHO/UNICEF joint statement - Maintaining routine immunization services vital during the COVID-19 pandemic [Internet]. Geneva: World Health Organization; 2020 Apr 20 [cited April 25, 2022]. Available from: https://www.euro.who.int/en/media-centre/sections/statements/2020/whounicef-joint-statement-maintaining-routine-immunization-services-vital-during-the-covid-19-pandemic.
- 24.World Health Organization. Guidance on routine immunization services during the COVID-19 pandemic [Internet]. Geneva: World Health Organization; 2020 Mar 20 [cited 2022 April 25]. Available from: https://apps.who.int/iris/bitstream/handle/10665/334123/WHO-EURO-2020-1059-40805-55114-eng.pdf.
- 25.Klein J.D., Koletzko B., El-Shabrawi M.H., Hadjipanayis A., Thacker N., Bhutta Z. Promoting and supporting children’s health and healthcare during COVID-19–International Paediatric Association Position Statement. Arch Dis Child. 2020 Jul 1;105(7):620–624. doi: 10.1136/archdischild-2020-319370. [DOI] [PubMed] [Google Scholar]
- 26.MacDonald N.E., Comeau J.L., Dubé È., Bucci L.M. COVID-19 and missed routine immunizations: designing for effective catch-up in Canada. Can J Public Health. 2020;111(4):469–472. doi: 10.17269/s41997-020-00385-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiely M., Mansour T., Brousseau N., Rafferty E., Paudel Y.R., Sadarangani M., et al. COVID-19 pandemic impact on childhood vaccination coverage in Quebec. Canada Hum Vaccin Immunother. 2022;18(1):2007707–2007708. doi: 10.1080/21645515.2021.2007707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell S., Clarke R., Paterson P., Mounier-Jack S. Parents’ and guardians’ views and experiences of accessing routine childhood vaccinations during the coronavirus (COVID-19) pandemic: A mixed methods study in England. PLoS One. 2020;15(12):e0244049–e. doi: 10.1371/journal.pone.0244049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He K., Mack W.J., Neely M., Lewis L., Anand V. Parental Perspectives on Immunizations: Impact of the COVID-19 Pandemic on Childhood Vaccine Hesitancy. J Community Health. 2021;47(1):39–52. doi: 10.1007/s10900-021-01017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leger360.com [Internet]. Montreal: Leger Marketing Inc; c2022 [cited 2022 Feb 14]. Available from: https://leger360.com/.
- 31.Government of Canada. Statement from the Chief Public Health Officer of Canada on December 9, 2020 [Internet]. Ottawa: Public Health Agency of Canada; 2020 Dec 9 [cited 2022 June 8]. Available from: https://www.canada.ca/en/public-health/news/2020/12/statement-from-the-chief-public-health-officer-of-canada-on-december-9-2020.html.
- 32.Government of Canada. National Advisory Committee on Immunization (NACI) statement: Recommendation on the use of the Pfizer-BioNTech COVID-19 vaccine (10 mcg) in children 5 to 11 years of age [Internet]. Ottawa: Government of Canada; 2021 Nov 25 [cited 2022 June 8]. Available from: https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines/pfizer-biontech-10-mcg-children-5-11-years-age.html.
- 33.Statistics Canada. Data products, 2016 Census [Internet]. Ottawa: Government of Canada; 2016 [updated 2021 Feb 8; cited 2021 Dec 12]. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/index-eng.cfm.
- 34.Eysenbach G. Improving the quality of web surveys: The checklist for reporting results of Internet e-surveys (CHERRIES) J Med Internet Res. 2004;6(3):12–16. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dubé E., Gagnon D., Ouakki M., Bettinger J.A., Witteman H.O., MacDonald S., et al. Measuring vaccine acceptance among Canadian parents: A survey of the Canadian Immunization Research Network. Vaccine. 2018;36(4):545–552. doi: 10.1016/j.vaccine.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 36.Frew P.M., Fisher A.K., Basket M.M., Chung Y., Schamel J., Weiner J.L., et al. Changes in childhood immunization decisions in the United States: Results from 2012 & 2014 National Parental Surveys. Vaccine. 2016;34(46):5689–5696. doi: 10.1016/j.vaccine.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Boehm R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12):e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Statistics Canada. Census Profile. 2021 Census of Population. Statistics Catalogue no. 98-316-X2021001. Ottawa: Government of Canada: 2022Oct 26 [cited 2022 Nov 7]. Available from: https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/index.cfm?Lang=E.
- 39.Statistics Canada. School closures and COVID-19: Interactive tool [Internet]. Ottawa: Government of Canada; 2021May 3 [cited 2022 May 13]. Available from: https://www150.statcan.gc.ca/n1/pub/71-607-x/71-607-x2021009-eng.htm.
- 40.Sell H., Assi A., Driedger S.M., Dubé È., Gagneur A., Meyer S.B., et al. Continuity of routine immunization programs in Canada during the COVID-19 pandemic. Vaccine. 2021;39(39):5532–5537. doi: 10.1016/j.vaccine.2021.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Government of Canada. Health Canada authorizes first COVID-19 vaccine [Internet]. Ottawa: Government of Canada; 2020 Dec 9 [cited 2022 May 5]. Available from: https://www.canada.ca/en/health-canada/news/2020/12/health-canada-authorizes-first-covid-19-vaccine.html.
- 42.Government of Canada. Archive: COVID-19 vaccination in Canada. Table 2: Cumulative percent and number of people who have received a COVID-19 vaccine in Canada by age group and vaccination status, Nov 6, 2021 [Internet]. Ottawa: Government of Canada; 2021 [cited 2022 May 3]. Available from: https://health-infobase.canada.ca/covid-19/vaccination-coverage/archive/2021-11-15/index.html.
- 43.Canadian Institute for Health Information (CIHI). COVID-19’s impact on physician services [Internet]. CIHI; 2021 Dec 9 [cited 2022 May 13]. Available from: https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/physician-services.
- 44.Piché-Renaud P.P., Ji C., Farrar D.S., Friedman J.N., Science M., Kitai I., et al. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario. Canada Vaccine. 2021;39(31):4373–4382. doi: 10.1016/j.vaccine.2021.05.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee D.I.D., Vanderhout S., Aglipay M., Birken C.S., Morris S.K., Piche-Renaud P.P., et al. Delay in childhood vaccinations during the COVID-19 pandemic. Can J Public Health. 2022;113(1):126–134. doi: 10.17269/s41997-021-00601-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization. Urgent health challenges for the next decade [Internet]. Geneva: World Health Organization; 2020 Jan 13 [cited 2022 May 13]. Available from: https://www.who.int/news-room/photo-story/photo-story-detail/urgent-health-challenges-for-the-next-decade.
- 47.Sokol R.L., Grummon A.H. COVID-19 and Parent Intention to Vaccinate Their Children Against Influenza. Pediatrics. 2020 Dec;146(6) doi: 10.1542/peds.2020-022871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li Z., Doan Q., Dobson S. Determinants of influenza immunization uptake in Canadian youths. Vaccine. 2010;28(19):3462–3466. doi: 10.1016/j.vaccine.2010.02.068. [DOI] [PubMed] [Google Scholar]
- 49.Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.L. Barriers of Influenza Vaccination Intention and Behavior - A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS One. 2017;12(1):e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.