Abstract
Background
Fecal microbiota transplantation (FMT) is an emerging therapy for diseases associated with intestinal flora imbalance that has attracted increasing attention in recent years. This study aims to provide an overview of research trends in the field, and act as a reference point for future scientific research by analyzing the state of current research, identifying hotspots, and potential frontiers of FMT.
Methods
Articles relating to FMT that were published between the years 2012 and 2021 were retrieved from the Web of Science Core Collection. Bibliometric analysis was performed using Microsoft Excel and CiteSpace.
Results
A total of 2,403 English language articles relating to FMT research were published over the last ten years. Most of this research was carried out in the United States of America, with Harvard Medical school being the most productive institution. Much of the research was published in the PLoS One journal. Alexander Khoruts was identified as a prominent, productive researcher in the field. Keyword analysis revealed that research hot spots included gut microbiota, Clostridium difficile infection (CDI), and diseases. Burst detection indicated that future research frontiers include clinical practice guidelines and strategies.
Conclusion
Our analysis explored hot spots and emerging trends in the FMT field. Indications for use of FMT extended from digestive system diseases to other systemic diseases. Additionally, areas such as risk assessment and control, along with application methods were also a focus of current research. Moreover, research relating to optimization of clinical practice has excellent prospects.
Keywords: fecal microbiota transplantation, gut microbiota, bibliometric, CiteSpace, clostridium difficile infection
Introduction
Fecal microbiota transplantation (FMT) is a method for treating intestinal and extra-intestinal diseases. FMT can be used to reconstitute the intestinal microbial community in recipients by transplanting the functional flora in the feces of healthy donors into the gastrointestinal tract of patients (Gupta and Khanna, 2017; Wang et al., 2019b). Historical records revealed that feces treatment occurred in China as early as the fourth century AD. In 1958, Eiseman published his first paper on the use of FMT therapy to treat pseudomembranous colitis (Eiseman et al., 1958). Studies have shown that FMT has a definite therapeutic effect on several gastrointestinal diseases including recurrent Clostridium difficile (C. difficile) infection (CDI) (Cammarota et al., 2017), ulcerative colitis, and Crohn’s disease (Holleran et al., 2018). Moreover, FMT has also been shown to be beneficial in multiple system diseases including cancer (Chen et al., 2019), obesity (Aron-Wisnewsky et al., 2019), and hepatic encephalopathy (Karakan, 2017). In recent years, the field of FMT has enjoyed rapid development with the progress of the human microbiome project (Turnbaugh et al., 2007), the establishment of stool banks (Kragsnaes et al., 2020), and the improvement of transplantation techniques and specifications (Khoruts et al., 2019; Ossorio and Zhou, 2019).
Gut microbiota dysbiosis is involved in the pathology of many diseases (Guarner and Malagelada, 2003; Schmidt et al., 2018). The intestinal flora participates in metabolism and plays a vital role in the host’s immune, nutritional and digestive functions (Ananthakrishnan et al., 2019; Gomaa, 2020; Zhou et al., 2020). Short-term interventions often fail to alter the composition of the flora (Dostal Webster et al., 2019) as the intestinal community is quite resistant to change. In contrast, FMT has significant advantages in establishing healthy microbial systems. FMT reconstructs the intestinal microbial community by means of transplantation and colonization, increasing the number of beneficial bacteria and rebuilding the patient’s homeostatic environment (Suez et al., 2018). FMT was written into the guidelines for the diagnosis, treatment, and prevention of CDI in 2013 (Surawicz et al., 2013). In 2019, the international conference on FMT reached consensuses on stool banking and the implementation rules for fecal transplantation (Cammarota et al., 2019).
As the field of FMT has developed rapidly and shows great potential in treating various diseases, we carried out a bibliometric analysis of relevant articles published between 2012 and 2021. The bibliometric method allows quantitative and qualitative analyses of specific topics and articles to evaluate academic productivity and trends. CiteSpace is a network analysis and visualization software developed by Chaomei Chen based on the JAVA platform (Chen and Chen, 2005). It can identify relationships between scientific articles and explore emerging trends and theme changes over time. This study explored annual trends of publications, countries/regions of high productivity, institutions and authors, core journals, co-cited references, current status and future directions of research.
Materials and methods
Data source and search strategy
The literature retrieval was conducted on March 24th, 2022, using the Web of Science Core Collection. The search formula used was “((((((((TS=(fecal microbiota transplantation)) OR TS=(faecal microbiota transplantation)) OR TS=(fecal microbiota transfer)) OR TS=(faecal microbiota transfer)) OR TS=(fecal microbiota transplant)) OR TS=(faecal microbiota transplant)) AND PY=(2012-2021)) AND DT=(Article)) AND LA=(English).” We placed restrictions on the publication date (2012-01-01 to 2021-12-31) and the language (English). Inclusion was limited to original research articles. Other literature types such as review articles, meeting summaries, and editorial materials were excluded. Ultimately, we identified 2,403 eligible records ( Supplementary Figure 1 ). Search records were downloaded and exported to CiteSpace software for subsequent analysis.
The journal impact factor (IF) and quartile were obtained from Journal Citation Reports 2021. The IF is determined by the number of citations and total articles in the last two years (Garfield, 2006) and reflects the journal’s influence.
Data analysis
Microsoft Excel 2016 was used for basic calculations and plotting of annual trends of publications and citations. Publications and citations were represented by bar and line charts. The trend test was performed using polynomial curve fitting.
CiteSpace (5.8. R 3 64-bit) was used for bibliometric and visual analysis. The visual map consists of nodes and links. In the network, the nodes were used to represent the countries, institutions, authors, references, etc. Meanwhile, the size and frequency of the node were in direct proportion. The different colors of nodes correspond to different periods. The connection link between nodes indicates the relationship between them, and the thickness of the connection line indicates the strength of the association. The number of nodes and connections from the network are represented by N and E, respectively. Betweenness centrality was used to measure the centrality of the vertices of the shortest path in a network. It indicated the importance of a node and the relationship between neighboring nodes. Nodes with a betweenness centrality greater than 0.1 were usually marked with purple circles and were considered turning points or key points in the field.
Results
Temporal trends of publications and citations
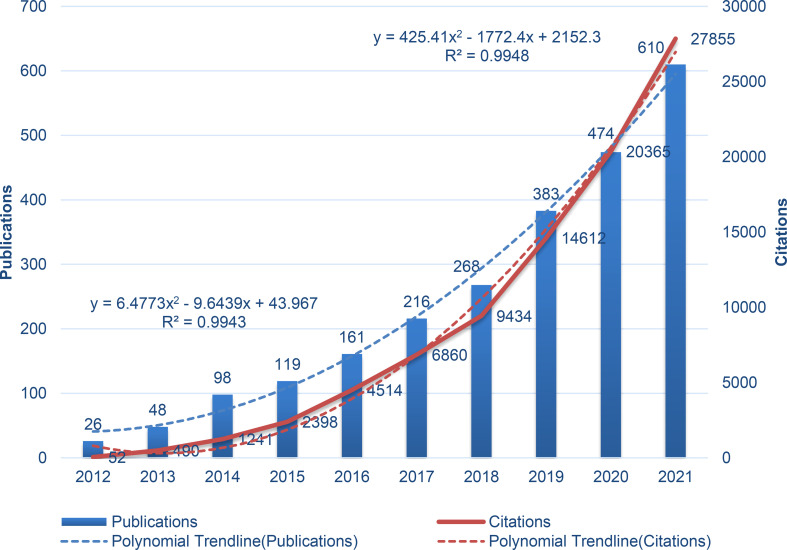
This study included 2,403 English articles related to FMT. A total of 42,796 articles were cited, with a total citation number of 92,290, and an average citation number of 38.41 times. The H-index was 134.
The number of FMT publications trended upwards over the period from 2012 to 2021, especially after 2018 ( Figure 1 ). In total, 1,467 articles were published from 2019 to 2021, accounting for 61.05% of the total publications over the 10 years. Over the past decade, citations have increased dramatically, especially from 2018 to 2021. The polynomial fitting curve showed significant correlations between publications, citations, and year (R2 = 0.9943, R2 = 0.9948). The above results demonstrate that FMT research has received increasing attention in recent years. It is expected that the number of related articles and citations will enter a sustained growth stage in the future.
Figure 1.
Annual trends in FMT research publications and citations.
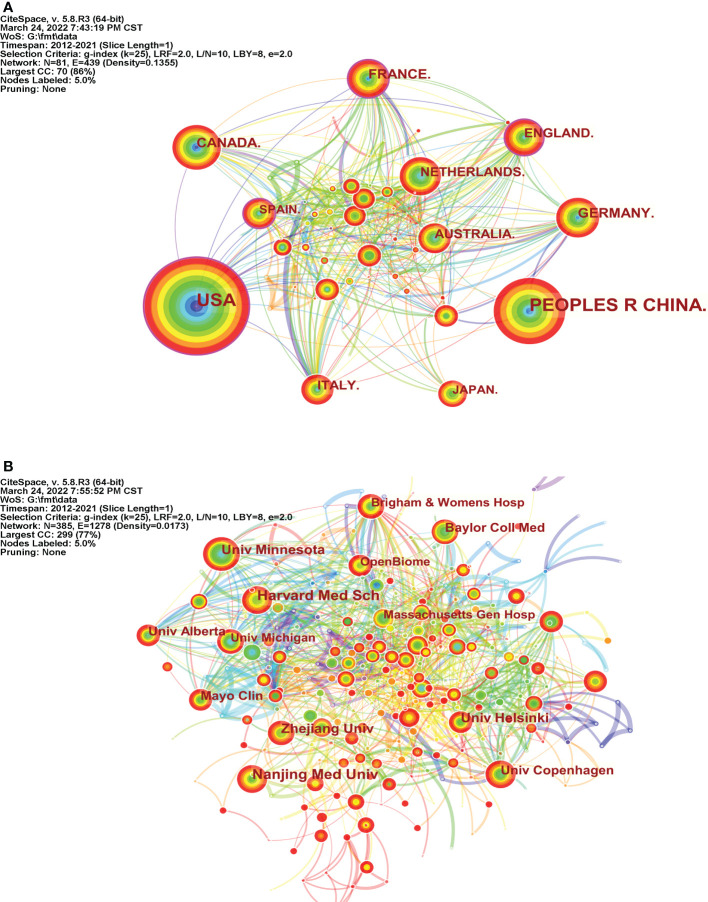
Countries and institutions analysis
Scholars in 81 countries published research articles ( Figure 2A ). The top 10 countries are listed in Table 1 . The United States of America (USA) was the leading country for publications, followed by the People’s Republic of China, Canada, France, and Germany. The top five countries in terms of centrality were France (0.20), England (0.17), the USA (0.16), Spain (0.15), and Germany (0.10), indicating that these countries are more influential and cooperative in FMT research.
Figure 2.
Countries and Institutions Analysis. (A) Map of countries performing FMT-related research (N=81, E=439); (B) Map of institutes performing FMT-related research (N=385, E=1278).
Table 1.
The most productive countries and institutions in FMT research.
| Rank | Count | Centrality | Country | Rank | Count | Centrality | Institution |
|---|---|---|---|---|---|---|---|
| 1 | 914 | 0.16 | USA | 1 | 59 | 0.01 | Harvard Medical School |
| 2 | 682 | 0 | China | 2 | 57 | 0 | Nanjing Medical University |
| 3 | 146 | 0.05 | Canada | 3 | 52 | 0.03 | Zhejiang University |
| 4 | 146 | 0.2 | France | 4 | 49 | 0.09 | University of Minnesota |
| 5 | 130 | 0.1 | Germany | 5 | 43 | 0.02 | University of Helsinki |
| 6 | 117 | 0.17 | England | 6 | 40 | 0.07 | University of Copenhagen |
| 7 | 110 | 0.05 | Italy | 7 | 39 | 0.03 | Baylor College of Medicine |
| 8 | 103 | 0.04 | Netherlands | 8 | 35 | 0.04 | Mayo Clinic |
| 9 | 97 | 0.08 | Australia | 9 | 35 | 0.03 | University of Alberta |
| 10 | 87 | 0.02 | Japan | 10 | 33 | 0.03 | University of Michigan |
A total of 385 institutions were enrolled in the FMT study ( Figure 2B ). Five of the top 10 most productive institutions are located in the USA ( Table 1 ): Harvard University, University of Minnesota, Baylor College of Medicine, Mayo Clinic, and University of Michigan, indicating that American scientific research institutions are heavily involved in the FMT research field. Notably, OpenBiome contributed 33 articles as a non-profit organization (stool bank) dedicated to collecting, screening, and transporting fecal samples (Cammarota et al., 2019).
The extensive network of cooperation between these countries and institutions indicates the importance of international collaboration in FMT research. Although China has an advantage in the number of publications, disparities still persist in global communication and collaboration compared with developed countries.
Journal and author analysis
In total, 728 journals were identified as publishing FMT-related articles, and Table 2 shows the top 10 academic journals. More than 50 articles were published in each of PLoS One, Scientific Reports, Frontiers in Microbiology, and Gut Microbes. The mean IF of top 10 journals were 14.192 and the highest IF was 33.883 (Gastroenterology). Among these top 10 journals, the fields of gastroenterology & hepatology, and microbiology were represented by five and two journals, respectively, further illustrating that the digestive system is an important area of focus for FMT research. In addition, all the listed journals were distributed in Q1 or Q2, indicating that the above journals had strong academic influences on FMT research.
Table 2.
Journals with the most published FMT-related articles.
| Rank | Count | Journal | IF1 | Quartile in Category |
|---|---|---|---|---|
| 1 | 65 | PLoS One | 3.752 | Q2 |
| 2 | 65 | Scientific Reports | 4.996 | Q2 |
| 3 | 54 | Frontiers in Microbiology | 6.064 | Q1 |
| 4 | 54 | Gut Microbes | 9.434 | Q1 |
| 5 | 53 | Microbiome | 16.837 | Q1 |
| 6 | 42 | Gut | 31.793 | Q1 |
| 7 | 38 | Gastroenterology | 33.883 | Q1 |
| 8 | 36 | World Journal of Gastroenterology | 5.374 | Q2 |
| 9 | 33 | Clinical Infectious Diseases | 20.999 | Q1 |
| 10 | 27 | Frontiers in Immunology | 8.786 | Q1 |
1Data from the 2021 edition of Journal Citation Reports.
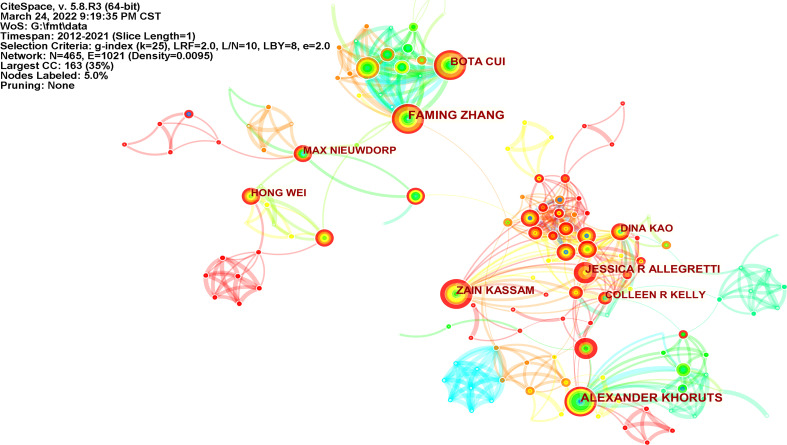
There were 465 authors who published articles related to FMT ( Figure 3 ). Among the top 10 most productive authors in Table 3 , Alexander Khoruts, a gastroenterologist at the University of Minnesota, has published 39 articles. Faming Zhang, who is known as the “first man of FMT in China” and is based at Nanjing Medical University, had a centrality of 0.11. Faming Zhang and Bota Cui cooperated closely together to improve the practices of FMT (Zhang et al., 2020).
Figure 3.
Map of authors performing FMT-related research (N=465, E=1021).
Table 3.
Top 10 productive authors of FMT-related research articles.
| Rank | Count | Centrality | Year | Authors |
|---|---|---|---|---|
| 1 | 39 | 0.05 | 2012 | Alexander Khoruts |
| 2 | 35 | 0.11 | 2015 | Faming Zhang |
| 3 | 29 | 0 | 2015 | Bota Cui |
| 4 | 29 | 0.01 | 2017 | Zain Kassam |
| 5 | 27 | 0 | 2014 | Jessica R Allegretti |
| 6 | 24 | 0.05 | 2014 | Dina Kao |
| 7 | 23 | 0.02 | 2018 | Hong Wei |
| 8 | 22 | 0.02 | 2014 | Colleen R Kelly |
| 9 | 22 | 0.03 | 2015 | Max Nieuwdorp |
| 10 | 21 | 0 | 2016 | Ting Zhang |
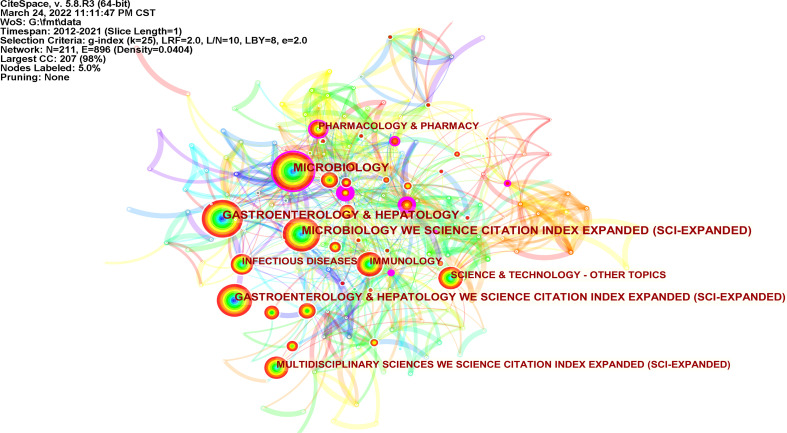
Category analysis
According to the category analysis of Web of Science, FMT research mainly focuses on microbiology, gastroenterology, hepatology, and immunology ( Figure 4 ). Social Science Citation Index (SSCI) (0.43), Biochemistry & Molecular Biology (0.3), and Conference Procedures Citation Index-Science (CPCI-S) (0.23) had relatively high concentricity.
Figure 4.
Map of categories related to FMT (N=211, E=896).
Keyword analysis
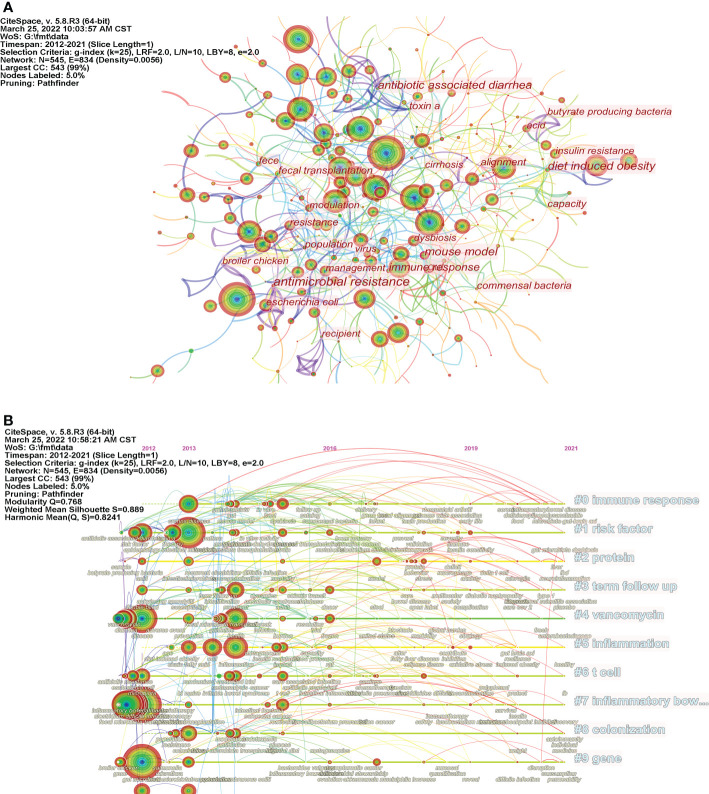
The keyword co-occurrence visualization map consists of 545 nodes and 1,954 links ( Figure 5A ). The top 5 keywords according to their frequency of occurrence were “gut microbiota,” “fecal microbiota transplantation,” “clostridium difficile infection,” “disease” and “infectious bowel disease”, indicating that the damage to the gastrointestinal tract caused by CDI and other inflammatory diseases were hot topics in FMT research. According to the centrality, the top five keywords are “antimicrobial resistance” (0.19), “mouse model” (0.18), “gut” (0.15), “immune response” (0.15), and “diet” (0.14). This indicates that FMT has a potential role in counteracting the side effects of certain drugs and lifestyles, and relevant animal experiments have been widely conducted ( Table 4 ). In addition, we conducted clustering analysis on co-occurring keywords. The top 10 clusters with the most significant number of keywords are shown in Table 4 . The immune response (cluster #0) is the largest cluster, and is considered as one of the main therapeutic of FMT (Frisbee and Petri, 2020). The alteration of host immune responses by FMT has been demonstrated in multiple studies (Jang et al., 2021; Spencer et al., 2021). Furthermore, disruption of the intestinal microbiota by antibiotic therapy (Gregory et al., 2021; Tomkovich et al., 2021) was the primary risk factor for CDI (cluster #1 risk factor). Meanwhile, other risk factors for FMT, such as early clinical recurrence of inflammatory bowel disease, have also received attention (Zhao et al., 2021).
Figure 5.
Analysis of keywords. (A) Map of keywords related to FMT (N=545, E=834); (B) The timeline visualization map of keywords related to FMT.
Table 4.
Top 10 keywords and clusters related to FMT research.
| Rank | Count | Centrality | Year | Keywords | ClusterID | Size | Label (LLR) |
|---|---|---|---|---|---|---|---|
| 1 | 667 | 0.01 | 2012 | gut microbiota | #0 | 48 | immune response |
| 2 | 540 | 0.02 | 2012 | fecal microbiota transplantation | #1 | 43 | risk factor |
| 3 | 320 | 0.01 | 2013 | intestinal microbiota | #2 | 39 | protein |
| 4 | 306 | 0.04 | 2012 | clostridium difficile infection | #3 | 37 | term follow up |
| 5 | 271 | 0.01 | 2012 | disease | #4 | 34 | vancomycin |
| 6 | 265 | 0.02 | 2012 | inflammatory bowel disease | #5 | 32 | inflammation |
| 7 | 231 | 0.03 | 2012 | ulcerative coliti | #6 | 31 | t cell |
| 8 | 200 | 0.01 | 2014 | inflammation | #7 | 29 | inflammatory bowel disease |
| 9 | 189 | 0.04 | 2012 | diversity | #8 | 27 | colonization |
| 10 | 189 | 0.02 | 2012 | clostridium difficile | #9 | 27 | gut microbiota |
The timeline view was used to demonstrate the changing trends of different clusters over time ( Figure 5B ). The first 10 clusters are shown in Table 4 . “Immune response,” “risk factor,” and “protein” are the clusters that contain the most keywords, while clusters such as “immune response,” “infrared,” and “colonization” appear relatively late. Additionally, people are increasingly concerned about the safety and efficacy of FMT due to the increased development of fecal transplantation technology and the deepening of relevant research.
Burst keyword detection can reveal the dynamic changes in hot spots and research frontiers over time. Table 5 shows the 30 keywords with the strongest citation bursts in the past decade. From 2012 to 2015, the main focus was on the treatment of diarrhea and C. difficile-associated diarrhea using bacterial therapy. The roles of FMT in other intestinal and metabolic diseases such as ulcerative colitis, Crohn’s disease, and obesity were explored from 2015 to 2017. In recent years, due to the promotion of FMT application, researchers have paid more attention to clinical practice guidelines and treatment strategies. This indicates that the current research is more committed to solving the practical problems in the implementation of FMT.
Table 5.
Top 30 Keywords related to FMT with the strongest citation bursts.
| Keywords | Year | Strength | Begin | End | 2012 - 2021 |
|---|---|---|---|---|---|
| bacteriotherapy | 2012 | 20.05 | 2012 | 2017 |

|
| clostridium difficile | 2012 | 18.94 | 2012 | 2016 |

|
| diarrhea | 2012 | 12.55 | 2012 | 2015 |

|
| flora | 2012 | 11.3 | 2012 | 2015 |

|
| coliti | 2012 | 6.34 | 2012 | 2014 |

|
| epidemiology | 2012 | 5.57 | 2012 | 2016 |

|
| antibiotic associated diarrhea | 2012 | 4.33 | 2012 | 2017 |

|
| enterocoliti | 2012 | 3.97 | 2012 | 2013 |

|
| double blind | 2012 | 3.3 | 2012 | 2014 |

|
| crohns disease | 2012 | 12.91 | 2013 | 2017 |

|
| therapy | 2012 | 8.79 | 2013 | 2015 |

|
| recurrent clostridium difficile | 2012 | 4.68 | 2013 | 2018 |

|
| microbiota transplantation | 2012 | 4.28 | 2013 | 2016 |

|
| inflammatory bowel disease | 2012 | 4 | 2013 | 2015 |

|
| toxin a | 2012 | 3.8 | 2013 | 2018 |

|
| randomized controlled trial | 2012 | 6.9 | 2014 | 2018 |

|
| pattern | 2012 | 4.17 | 2014 | 2016 |

|
| term follow up | 2012 | 4.05 | 2014 | 2018 |

|
| immune system | 2012 | 5.3 | 2015 | 2017 |

|
| intestinal microbiome | 2012 | 3.77 | 2015 | 2016 |

|
| diet induced obesity | 2012 | 3.32 | 2015 | 2017 |

|
| ulcerative coliti | 2012 | 4.19 | 2016 | 2017 |

|
| randomized clinical trial | 2012 | 4.18 | 2016 | 2017 |

|
| stem cell transplantation | 2012 | 3.79 | 2016 | 2018 |

|
| sequence | 2012 | 4.14 | 2017 | 2018 |

|
| united states | 2012 | 3.78 | 2017 | 2018 |

|
| innate immunity | 2012 | 3.78 | 2017 | 2018 |

|
| carriage | 2012 | 3.73 | 2017 | 2019 |

|
| clinical practice guideline | 2012 | 4 | 2019 | 2021 |

|
| strategy | 2012 | 3.66 | 2019 | 2021 |

|
Analysis of cited authors and co-cited references
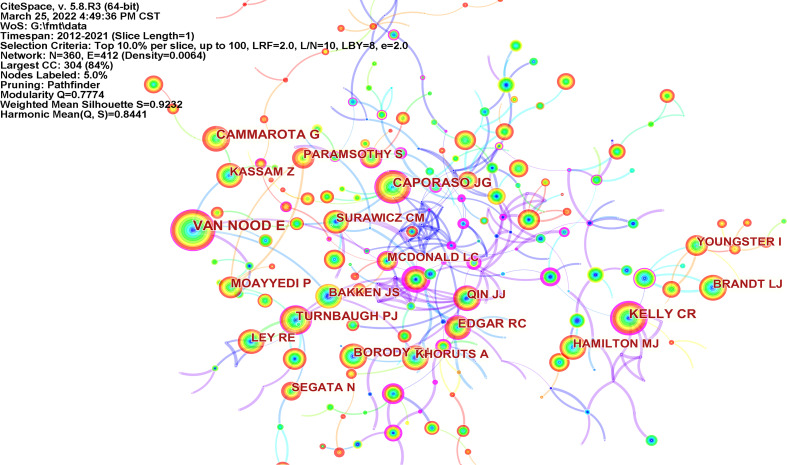
As shown in Figure 6 and Table 6 , the authors with the most citations were Van Nood E, Caporaso JG, and Cammarota G. The most central authors were Sekirov I (0.58), Damman CJ (0.53), and De Leon LM (0.49). Van Nood, from the Academic Medical Center in Amsterdam, the Netherlands, systematically reviewed the treatment of recurrent CDI with donor feces as early as 2009 (Van Nood et al., 2009).
Figure 6.
Map of cited authors performing FMT-related research (N=360, E=412).
Table 6.
Top 10 cited authors related to FMT research.
| Rank | Count | Centrality | Year | Cited authors |
|---|---|---|---|---|
| 1 | 543 | 0.11 | 2012 | Van Nood E |
| 2 | 363 | 0.12 | 2012 | Caporaso JG |
| 3 | 356 | 0.03 | 2015 | Cammarota G |
| 4 | 344 | 0.21 | 2012 | Kelly CR |
| 5 | 310 | 0.1 | 2012 | Turnbaugh PJ |
| 6 | 276 | 0.08 | 2015 | Moayyedi P |
| 7 | 262 | 0.15 | 2013 | Edgar RC |
| 8 | 245 | 0 | 2012 | Borody TJ |
| 9 | 242 | 0 | 2012 | Hamilton MJ |
| 10 | 235 | 0.05 | 2013 | Kassam Z |
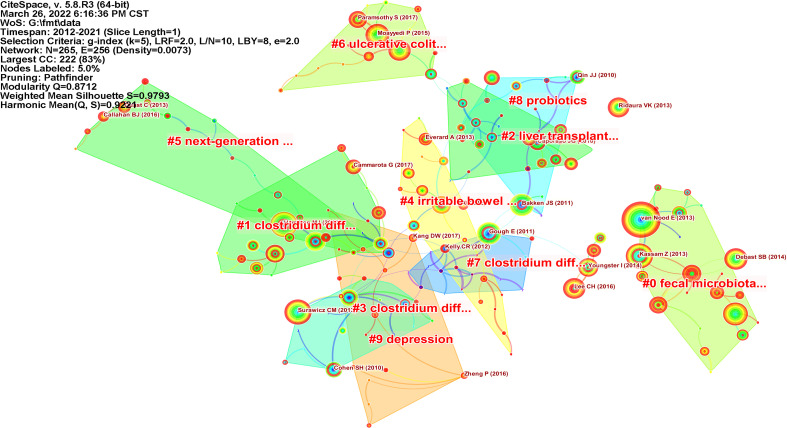
The visualization map of co-cited references is shown in Figure 7 , and the top 10 most frequently cited articles are shown in Table 7 . These citations are mainly focused on the technology of FMT, the application of FMT in a variety of intestinal diseases (randomized controlled trials), and expert consensus and guidelines. Van Nood and colleagues validated the feasibility of duodenal infusion of donor feces for the treatment of recurrent CDI diarrhea in a randomized controlled trial (Van Nood et al., 2013), which was published in the New England Journal of Medicine. This study demonstrated the advantages of FMT over antibiotic intervention. The article with the highest centrality (0.7) was reported by Vrieze and colleagues in 2012. It demonstrated that the transplantation of intestinal microflora from lean human donors could improve insulin sensitivity in recipients (Vrieze et al., 2012), and further cemented the potential role of FMT in obesity treatment. The most frequently cited articles were from PLoS One, Nature, Gastroenterology, Gut, and the New England Journal of Medicine.
Figure 7.
Map of co-cited references related to FMT (N=265, E=256).
Table 7.
Top 10 cited references related to FMT research.
| Rank | Count | Centrality | Year | Article title | Author | Journal |
|---|---|---|---|---|---|---|
| 1 | 523 | 0.07 | 2013 | Duodenal infusion of donor feces for recurrent Clostridium difficile | van Nood E | New Engl J Med |
| 2 | 223 | 0.04 | 2015 | Fecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in a Randomized Controlled Trial | Moayyedi P | Gastroenterology |
| 3 | 188 | 0.01 | 2013 | Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections | Surawicz CM | Am J Gastroenterol |
| 4 | 186 | 0.38 | 2013 | Fecal microbiota transplantation for Clostridium difficile infection: systematic review and meta-analysis | Kassam Z | Am J Gastroenterol |
| 5 | 165 | 0 | 2017 | Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial | Paramsothy S | Lancet |
| 6 | 164 | 0.04 | 2012 | Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection | Hamilton MJ | Am J Gastroenterol |
| 7 | 159 | 0.22 | 2011 | Treating Clostridium difficile infection with fecal microbiota transplantation | Bakken JS | Clin Gastroenterol H |
| 8 | 159 | 0.01 | 2017 | European consensus conference on faecal microbiota transplantation in clinical practice | Cammarota G | Gut |
| 9 | 158 | 0.03 | 2015 | Burden of Clostridium difficile infection in the United States | Lessa FC | New Engl J Med |
| 10 | 154 | 0.59 | 2011 | Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection | Gough E | Clin Infect Dis |
Clustering analysis was performed on the co-cited references ( Figure 7 ), and the top 10 clusters were identified ( Table 8 ). The development of sequencing technologies and the deepening of research on the composition and function of intestinal microorganisms, has led to an expansion in the scope of FMT research. Liver transplantation (cluster #2) and irritable bowel syndrome (cluster #4) had 19 and 18 co-cited references, respectively. Additionally, the therapeutic effect of FMT on psychological diseases such as depression has attracted extensive attention.
Table 8.
Top 10 clusters of cited references related to FMT research.
| ClusterID | Size | Sihouette | Year | Label (LLR) |
|---|---|---|---|---|
| #0 | 23 | 1 | 2015 | fecal microbiota transplant |
| #1 | 20 | 0.986 | 2014 | clostridium difficile infection |
| #2 | 19 | 1 | 2011 | liver transplantation |
| #3 | 19 | 0.958 | 2011 | clostridium difficile |
| #4 | 18 | 0.931 | 2016 | irritable bowel syndrome |
| #5 | 18 | 1 | 2012 | next-generation sequencing |
| #6 | 16 | 1 | 2016 | ulcerative colitis |
| #7 | 16 | 0.99 | 2010 | clostridium difficile |
| #8 | 14 | 0.944 | 2009 | probiotics |
| #9 | 14 | 1 | 2016 | depression |
Discussion
This study represents the first bibliometric and visual analysis of FMT research over the past 10 years. We used CiteSpace to perform a bibliometric analysis on FMT studies that were carried out between 2012 and 2021, and the current status and future trends of FMT research were identified through the analysis of the distribution of countries, institutions, journals and authors, as well as core keywords and references. As research interest into the effects of intestinal microorganisms has increased, FMT has attracted continuous and increasing attention as a potential therapeutic intervention. Our data shows that publications and citations related to FMT increase yearly, and it has become a hot research topic. The USA contributed the most significant number of publications, becoming one of the main driving forces in FMT research. American institutions have extensive resources in universities, medical institutions, and social organizations. European and American countries have the highest degree of centralization. They occupy a dominant position, demonstrating that they have advantages in international exchanges and cooperation. FMT research is also showing strong momentum in China. In recent years, Nanjing Medical University has committed to the standardization of FMT (Cui et al., 2015; Zhang et al., 2018). The Medical College of Zhejiang University has focused on the use of animal models of FMT to verify the role of specific bacteria in disease processes (Li et al., 2017; Bian et al., 2019). These institutions have published a large amount of literature, which will provide valuable scientific evidence and practical guidance for FMT moving forward.
Alexander Khoruts was identified as the most productive author. He was also the lead author of the clinical therapeutic guidelines for CDI, a study that was cited more than 500 times (Bakken et al., 2011). His research revealed that the mechanism of FMT is related to the restoration of normal intestinal microbial community structure and function (Khoruts and Sadowsky, 2016; Khoruts et al., 2021). In addition, he also investigated the use of FMT in treating liver cirrhosis, autism, and other diseases (Kang et al., 2017; Cheng et al., 2021). Faming Zhang published 35 articles on FMT studies. The development of the intelligent fecal bacteria isolation system, and the technology of washing microbiota transplantation, were led by his team. These technologies improve the safety of FMT and reduce the probability of adverse events (Zhang et al., 2020). This study was published in Protein & Cell and featured on the cover, pushing FMT into a new development stage. Additionally, the widely cited study carried out by Van Noude and colleagues demonstrating significant advantages of infusion of donor feces for treatment of recurrent CDI over traditional vancomycin therapy (Van Nood et al., 2013), also pushed the field forward. These authors have a strong presence in FMT research and have contributed to the exploration of safety, efficacy, and operability.
C. difficile is a gram-positive anaerobic bacteria (Chen et al., 2021), which can cause gastrointestinal infections (Zhou et al., 2021). C. difficile was first discovered in 1935 as normal flora in the intestines of newborn babies (Hopkins and Wilson, 2018). Use of antibiotics can cause C. difficile proliferation, which in turn leads to refractory diseases such as severe diarrhea, pseudomembranous colitis, and intestinal obstruction. However, antibiotic treatment seems to be ineffective against CDI, and may even cause antibiotic resistance (Spigaglia et al., 2018). An article in Lancet reported the first case of FMT for CDI treatment in 1983 (Schwan et al., 1983), which pioneered a new approach to non-antibiotic therapy. To date, FMT remains the recommended treatment for patients with severe and fulminant CDI according to ACG clinical guidelines (Kelly et al., 2021). From 2012 to 2021, the number of articles with the keywords of Clostridium difficile infection and Clostridium difficile was 306 and 189, respectively. We believe that the treatment of CDI remains the main direction of clinical and basic research on FMT.
Keywords are considered to reflect high-frequency hot spots in a particular field (Lin et al., 2022). We also conducted a comprehensive analysis of the co-cited references and categories, and summarized the research hot spots as follows: 1) Inflammatory bowel disease and CDI (Cammarota et al., 2017), principally including ulcerative colitis (Costello et al., 2019; Matsuoka, 2021), and Crohn’s disease (Bak et al., 2017; Sokol et al., 2020), also including constipation (Ge et al., 2017; Zhang et al., 2021), and diarrhea (Dai et al., 2019); 2) Complementary and alternative treatment of several metabolic diseases, such as obesity (Allegretti et al., 2020; Yu et al., 2020), type 2 diabetes (Wang et al., 2019a), metabolic syndrome (Mocanu et al., 2021); 3) Adjuvant tumor immunotherapy, mainly to reduce drug toxicity and modulate the immune response (Chang et al., 2020; Baruch et al., 2021); 4) Developmental disorders and psychological diseases, mainly related to the treatment of children’s autism (Kang et al., 2019) and the relief of symptoms of depression and anxiety (Kilinçarslan and Evrensel, 2020; Rao et al., 2021); 5) Transplantation mode and action mechanisms, such as in vitro sorting of transplanted microorganisms (Zhang et al., 2020), and short-chain fatty acid and bile acid metabolism (Seekatz et al., 2018); 6) Potential indications and risk assessment (Lagier and Raoult, 2016; Gupta et al., 2021), and the utilization of standardized fecal sample banks (Kragsnaes et al., 2020).
Emerging trends can be identified through the analysis of burst keywords (Chen et al., 2014). Burst keywords at a specific time often mean that research in related fields has attracted attention. Based on the burst keywords in recent years, we believe that the establishment and improvement of clinical guidelines for FMT will become an academic trend. This will help clarify the indications, reduce potential risks, and develop optimum treatment strategies. Although extensive clinical studies have proved the safety of FMT (Goloshchapov et al., 2019; Saha et al., 2021), a small number of patients undergoing FMT may suffer from adverse reactions such as abdominal pain, diarrhea (Michailidis et al., 2021), recurrent infection, and even death (Ser et al., 2021). Clinical guidelines are the evidence base for medical practice (Kondylakis et al., 2020), and therefore, are important for guiding research and promotion of FMT (Haifer et al., 2020), operating procedures (Cammarota et al., 2019), and administration routes (Ross and Reveles, 2020; Halaweish et al., 2022). At the policy and legislative levels, there is a need for both a flexible regulatory framework to promote the application and research, and traceability of fecal donors to ensure patient safety (Vyas et al., 2015; Cammarota et al., 2019). Additionally, ethical issues raised by fecal donation also need to be addressed (Grigoryan et al., 2020; Hollingshead et al., 2021).
In this study, we used CiteSpace to reveal the cutting-edge hot spots and dynamic changes in the FMT research field over the past decade. Our study found that FMT can improve the intestinal microenvironment and has prominent advantages in the treatment of many diseases. However, the large-scale application of FMT also faces safety, legal, and regulatory challenges. Furthermore, there are some limitations to this study. Firstly, all articles were retrieved from the Web of Science Core Collection only. Secondly, search strategies are not guaranteed to cover all FMT-related articles. Thirdly, due to the dynamic database updates and the rapid development of FMT research, our study cannot include all of the latest findings.
Conclusion
From 2012 to 2021, publications and citations relating to FMT research increased year by year. The USA has played a leading role in the field, with Harvard Medical School and Alexander Khoruts being the most prolific institutions and authors, respectively. A few key studies have pushed FMT into the spotlight, including the widely cited and influential study from Noude and colleagues titled “Duodenal infusion of donor feces for recurrent Clostridium difficile”. In recent years, the research of Chinese scholars has advanced at a rapid pace. Research hotspots and trends mainly involve the treatment of digestive system and other system diseases, with a particular focus on CDI and ulcerative colitis. In addition, new indications, new technologies, and new norms of FMT are also focuses of research. Overall, this study reports the advances in the field over the past 10 years from multiple dimensions through visual analysis of FMT research, paving the way for the follow-up research.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.
Author contributions
Conceptualization: LZ and MY; methodology: FZ and PY; software: YC; formal analysis: JW; data curation: LZ; writing—original draft preparation: FZ and PY; writing—review and editing: RW and BL; visualization: FZ, PY and YC; supervision: MY; project administration: LZ; funding acquisition: LZ. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by the National Natural Science Foundation of China (grant number: 81973730).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2022.1057492/full#supplementary-material
Flowchart of retrieval process.
Abbreviations
FMT, fecal microbiota transplantation; CDI, Clostridium difficile infection; C. difficile, Clostridium difficile; IF, impact factor.
References
- Allegretti J. R., Kassam Z., Mullish B. H., Chiang A., Carrellas M., Hurtado J., et al. (2020). Effects of fecal microbiota transplantation with oral capsules in obese patients. Clin. Gastroenterol. Hepatol. 18, 855–863.e2. doi: 10.1016/j.cgh.2019.07.006 [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan A. N., Singal A. G., Chang L. (2019). The gut microbiome and digestive health - a new frontier. Clin. Gastroenterol. Hepatol. 17, 215–217. doi: 10.1016/j.cgh.2018.10.040 [DOI] [PubMed] [Google Scholar]
- Aron-Wisnewsky J., Clément K., Nieuwdorp M. (2019). Fecal microbiota transplantation: A future therapeutic option for Obesity/Diabetes? Curr. Diabetes Rep. 19, 51. doi: 10.1007/s11892-019-1180-z [DOI] [PubMed] [Google Scholar]
- Bak S. H., Choi H. H., Lee J., Kim M. H., Lee Y. H., Kim J. S., et al. (2017). Fecal microbiota transplantation for refractory crohn's disease. Intest. Res. 15, 244–248. doi: 10.5217/ir.2017.15.2.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakken J. S., Borody T., Brandt L. J., Brill J. V., Demarco D. C., Franzos M. A., et al. (2011). Treating clostridium difficile infection with fecal microbiota transplantation. Clin. Gastroenterol. Hepatol. 9, 1044–1049. doi: 10.1016/j.cgh.2011.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baruch E. N., Youngster I., Ben-Betzalel G., Ortenberg R., Lahat A., Katz L., et al. (2021). Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371, 602–609. doi: 10.1126/science.abb5920 [DOI] [PubMed] [Google Scholar]
- Bian X., Wu W., Yang L., Lv L., Wang Q., Li Y., et al. (2019). Administration of akkermansia muciniphila ameliorates dextran sulfate sodium-induced ulcerative colitis in mice. Front. Microbiol. 10. doi: 10.3389/fmicb.2019.02259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cammarota G., Ianiro G., Kelly C. R., Mullish B. H., Allegretti J. R., Kassam Z., et al. (2019). International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut 68, 2111–2121. doi: 10.1136/gutjnl-2019-319548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cammarota G., Ianiro G., Tilg H., Rajilić-Stojanović M., Kump P., Satokari R., et al. (2017). European Consensus conference on faecal microbiota transplantation in clinical practice. Gut 66, 569–580. doi: 10.1136/gutjnl-2016-313017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C. W., Lee H. C., Li L. H., Chiang Chiau J. S., Wang T. E., Chuang W. H., et al. (2020). Fecal microbiota transplantation prevents intestinal injury, upregulation of toll-like receptors, and 5-Fluorouracil/Oxaliplatin-Induced toxicity in colorectal cancer. Int. J. Mol. Sci. 21 (2), 386. doi: 10.3390/ijms21020386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Chen Y. (2005). Searching for clinical evidence in CiteSpace. AMIA Annu. Symp. Proc. 2005, 121–125. [PMC free article] [PubMed] [Google Scholar]
- Chen C., Dubin R., Kim M. C. (2014). Orphan drugs and rare diseases: a scientometric review, (2000 – 2014). Expert Opin. Orphan Drugs 2, 709–724. doi: 10.1517/21678707.2014.920251 [DOI] [Google Scholar]
- Cheng Y. W., Alhaffar D., Saha S., Khanna S., Bohm M., Phelps E., et al. (2021). Fecal microbiota transplantation is safe and effective in patients with clostridioides difficile infection and cirrhosis. Clin. Gastroenterol. Hepatol. 19, 1627–1634. doi: 10.1016/j.cgh.2020.06.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D., Wu J., Jin D., Wang B., Cao H. (2019). Fecal microbiota transplantation in cancer management: Current status and perspectives. Int. J. Cancer 145, 2021–2031. doi: 10.1002/ijc.32003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P., Zeng J., Liu Z., Thaker H., Wang S., Tian S., et al. (2021). Structural basis for CSPG4 as a receptor for TcdB and a therapeutic target in clostridioides difficile infection. Nat. Commun. 12, 3748. doi: 10.1038/s41467-021-23878-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello S. P., Hughes P. A., Waters O., Bryant R. V., Vincent A. D., Blatchford P., et al. (2019). Effect of fecal microbiota transplantation on 8-week remission in patients with ulcerative colitis: A randomized clinical trial. Jama 321, 156–164. doi: 10.1001/jama.2018.20046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui B., Feng Q., Wang H., Wang M., Peng Z., Li P., et al. (2015). Fecal microbiota transplantation through mid-gut for refractory crohn's disease: safety, feasibility, and efficacy trial results. J. Gastroenterol. Hepatol. 30, 51–58. doi: 10.1111/jgh.12727 [DOI] [PubMed] [Google Scholar]
- Dai M., Liu Y., Chen W., Buch H., Shan Y., Chang L., et al. (2019). Rescue fecal microbiota transplantation for antibiotic-associated diarrhea in critically ill patients. Crit. Care 23, 324. doi: 10.1186/s13054-019-2604-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dostal Webster A., Staley C., Hamilton M. J., Huang M., Fryxell K., Erickson R., et al. (2019). Influence of short-term changes in dietary sulfur on the relative abundances of intestinal sulfate-reducing bacteria. Gut Microbes 10, 447–457. doi: 10.1080/19490976.2018.1559682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiseman B., Silen W., Bascom G. S., Kauvar A. J. (1958). Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery 44, 854–859. [PubMed] [Google Scholar]
- Frisbee A. L., Petri W. A., Jr. (2020). Considering the immune system during fecal microbiota transplantation for clostridioides difficile infection. Trends Mol. Med. 26, 496–507. doi: 10.1016/j.molmed.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield E. (2006). The history and meaning of the journal impact factor. Jama 295, 90–93. doi: 10.1001/jama.295.1.90 [DOI] [PubMed] [Google Scholar]
- Ge X., Zhao W., Ding C., Tian H., Xu L., Wang H., et al. (2017). Potential role of fecal microbiota from patients with slow transit constipation in the regulation of gastrointestinal motility. Sci. Rep. 7, 441. doi: 10.1038/s41598-017-00612-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goloshchapov O. V., Olekhnovich E. I., Sidorenko S. V., Moiseev I. S., Kucher M. A., Fedorov D. E., et al. (2019). Long-term impact of fecal transplantation in healthy volunteers. BMC Microbiol. 19, 312. doi: 10.1186/s12866-019-1689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomaa E. Z. (2020). Human gut microbiota/microbiome in health and diseases: a review. Antonie Van Leeuwenhoek 113, 2019–2040. doi: 10.1007/s10482-020-01474-7 [DOI] [PubMed] [Google Scholar]
- Gregory A. L., Pensinger D. A., Hryckowian A. J. (2021). A short chain fatty acid-centric view of clostridioides difficile pathogenesis. PloS Pathog. 17, e1009959. doi: 10.1371/journal.ppat.1009959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigoryan Z., Shen M. J., Twardus S. W., Beuttler M. M., Chen L. A., Bateman-House A. (2020). Fecal microbiota transplantation: Uses, questions, and ethics. Med. Microecol. 6, 100027. doi: 10.1016/j.medmic.2020.100027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarner F., Malagelada J. R. (2003). Gut flora in health and disease. Lancet 361, 512–519. doi: 10.1016/s0140-6736(03)12489-0 [DOI] [PubMed] [Google Scholar]
- Gupta A., Khanna S. (2017). Fecal microbiota transplantation. Jama 318, 102. doi: 10.1001/jama.2017.6466 [DOI] [PubMed] [Google Scholar]
- Gupta S., Mullish B. H., Allegretti J. R. (2021). Fecal microbiota transplantation: The evolving risk landscape. Am. J. Gastroenterol. 116, 647–656. doi: 10.14309/ajg.0000000000001075 [DOI] [PubMed] [Google Scholar]
- Haifer C., Kelly C. R., Paramsothy S., Andresen D., Papanicolas L. E., Mckew G. L., et al. (2020). Australian Consensus statements for the regulation, production and use of faecal microbiota transplantation in clinical practice. Gut 69, 801–810. doi: 10.1136/gutjnl-2019-320260 [DOI] [PubMed] [Google Scholar]
- Halaweish H. F., Boatman S., Staley C. (2022). Encapsulated fecal microbiota transplantation: Development, efficacy, and clinical application. Front. Cell Infect. Microbiol. 12. doi: 10.3389/fcimb.2022.826114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holleran G., Scaldaferri F., Ianiro G., Lopetuso L., Mc Namara D., Mele M. C., et al. (2018). Fecal microbiota transplantation for the treatment of patients with ulcerative colitis and other gastrointestinal conditions beyond clostridium difficile infection: an update. Drugs Today (Barc) 54, 123–136. doi: 10.1358/dot.2018.54.2.2760765 [DOI] [PubMed] [Google Scholar]
- Hollingshead C., Ciricillo J., Kammeyer J. (2021). Ethical implications of the fecal microbiota transplantation: Disclosure of a false-positive HIV test. Case Rep. Infect. Dis. 2021, 6696542. doi: 10.1155/2021/6696542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins R. J., Wilson R. B. (2018). Treatment of recurrent clostridium difficile colitis: a narrative review. Gastroenterol. Rep. (Oxf) 6, 21–28. doi: 10.1093/gastro/gox041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang H. M., Kim J. K., Joo M. K., Shin Y. J., Lee C. K., Kim H. J., et al. (2021). Transplantation of fecal microbiota from patients with inflammatory bowel disease and depression alters immune response and behavior in recipient mice. Sci. Rep. 11, 20406. doi: 10.1038/s41598-021-00088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang D. W., Adams J. B., Coleman D. M., Pollard E. L., Maldonado J., Mcdonough-Means S., et al. (2019). Long-term benefit of microbiota transfer therapy on autism symptoms and gut microbiota. Sci. Rep. 9, 5821. doi: 10.1038/s41598-019-42183-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang D. W., Adams J. B., Gregory A. C., Borody T., Chittick L., Fasano A., et al. (2017). Microbiota transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome 5, 10. doi: 10.1186/s40168-016-0225-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakan T. (2017). Fecal microbiota transplantation for treating recurrent hepatic encephalopathy: Ready for clinical application? Turk J. Gastroenterol. 28, 425–426. doi: 10.5152/tjg.2017.18817 [DOI] [PubMed] [Google Scholar]
- Kelly C. R., Fischer M., Allegretti J. R., Laplante K., Stewart D. B., Limketkai B. N., et al. (2021). ACG clinical guidelines: Prevention, diagnosis, and treatment of clostridioides difficile infections. Am. J. Gastroenterol. 116, 1124–1147. doi: 10.14309/ajg.0000000000001278 [DOI] [PubMed] [Google Scholar]
- Khoruts A., Hoffmann D. E., Palumbo F. B. (2019). The impact of regulatory policies on the future of fecal microbiota transplantation. J. Law Med. Ethics 47, 482–504. doi: 10.1177/1073110519897726 [DOI] [PubMed] [Google Scholar]
- Khoruts A., Sadowsky M. J. (2016). Understanding the mechanisms of faecal microbiota transplantation. Nat. Rev. Gastroenterol. Hepatol. 13, 508–516. doi: 10.1038/nrgastro.2016.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoruts A., Staley C., Sadowsky M. J. (2021). Faecal microbiota transplantation for clostridioides difficile: mechanisms and pharmacology. Nat. Rev. Gastroenterol. Hepatol. 18, 67–80. doi: 10.1038/s41575-020-0350-4 [DOI] [PubMed] [Google Scholar]
- Kilinçarslan S., Evrensel A. (2020). The effect of fecal microbiota transplantation on psychiatric symptoms among patients with inflammatory bowel disease: an experimental study. Actas Esp Psiquiatr. 48, 1–7. [PubMed] [Google Scholar]
- Kondylakis H., Axenie C., Kiran Bastola D., Katehakis D. G., Kouroubali A., Kurz D., et al. (2020). Status and recommendations of technological and data-driven innovations in cancer care: Focus group study. J. Med. Internet Res. 22, e22034. doi: 10.2196/22034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kragsnaes M. S., Nilsson A. C., Kjeldsen J., Holt H. M., Rasmussen K. F., Georgsen J., et al. (2020). How do I establish a stool bank for fecal microbiota transplantation within the blood- and tissue transplant service? Transfusion 60, 1135–1141. doi: 10.1111/trf.15816 [DOI] [PubMed] [Google Scholar]
- Lagier J. C., Raoult D. (2016). [Fecal microbiota transplantation: Indications and perspectives]. Med. Sci. (Paris) 32, 991–997. doi: 10.1051/medsci/20163211015 [DOI] [PubMed] [Google Scholar]
- Lin X., Zhou R., Liang D., Xia L., Zeng L., Chen X. (2022). The role of microbiota in autism spectrum disorder: A bibliometric analysis based on original articles. Front. Psychiatry 13. doi: 10.3389/fpsyt.2022.976827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Zhao F., Wang Y., Chen J., Tao J., Tian G., et al. (2017). Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome 5, 14. doi: 10.1186/s40168-016-0222-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuoka K. (2021). Fecal microbiota transplantation for ulcerative colitis. Immunol. Med. 44, 30–34. doi: 10.1080/25785826.2020.1792040 [DOI] [PubMed] [Google Scholar]
- Michailidis L., Currier A. C., Le M., Flomenhoft D. R. (2021). Adverse events of fecal microbiota transplantation: a meta-analysis of high-quality studies. Ann. Gastroenterol. 34, 802–814. doi: 10.20524/aog.2021.0655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocanu V., Zhang Z., Deehan E. C., Kao D. H., Hotte N., Karmali S., et al. (2021). Fecal microbial transplantation and fiber supplementation in patients with severe obesity and metabolic syndrome: a randomized double-blind, placebo-controlled phase 2 trial. Nat. Med. 27, 1272–1279. doi: 10.1038/s41591-021-01399-2 [DOI] [PubMed] [Google Scholar]
- Ossorio P. N., Zhou Y. (2019). Regulating stool for microbiota transplantation. Gut Microbes 10, 105–108. doi: 10.1080/19490976.2018.1502537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao J., Qiao Y., Xie R., Lin L., Jiang J., Wang C., et al. (2021). Fecal microbiota transplantation ameliorates stress-induced depression-like behaviors associated with the inhibition of glial and NLRP3 inflammasome in rat brain. J. Psychiatr. Res. 137, 147–157. doi: 10.1016/j.jpsychires.2021.02.057 [DOI] [PubMed] [Google Scholar]
- Ross C. N., Reveles K. R. (2020). Feasibility of fecal microbiota transplantation via oral gavage to safely alter gut microbiome composition in marmosets. Am. J. Primatol. 82, e23196. doi: 10.1002/ajp.23196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S., Mara K., Pardi D. S., Khanna S. (2021). Long-term safety of fecal microbiota transplantation for recurrent clostridioides difficile infection. Gastroenterology 160, 1961–1969.e3. doi: 10.1053/j.gastro.2021.01.010 [DOI] [PubMed] [Google Scholar]
- Schmidt T. S. B., Raes J., Bork P. (2018). The human gut microbiome: From association to modulation. Cell 172, 1198–1215. doi: 10.1016/j.cell.2018.02.044 [DOI] [PubMed] [Google Scholar]
- Schwan A., Sjölin S., Trottestam U., Aronsson B. (1983). Relapsing clostridium difficile enterocolitis cured by rectal infusion of homologous faeces. Lancet 2, 845. doi: 10.1016/s0140-6736(83)90753-5 [DOI] [PubMed] [Google Scholar]
- Seekatz A. M., Theriot C. M., Rao K., Chang Y. M., Freeman A. E., Kao J. Y., et al. (2018). Restoration of short chain fatty acid and bile acid metabolism following fecal microbiota transplantation in patients with recurrent clostridium difficile infection. Anaerobe 53, 64–73. doi: 10.1016/j.anaerobe.2018.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ser H. L., Letchumanan V., Goh B. H., Wong S. H., Lee L. H. (2021). The use of fecal microbiome transplant in treating human diseases: Too early for poop? Front. Microbiol. 12. doi: 10.3389/fmicb.2021.519836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol H., Landman C., Seksik P., Berard L., Montil M., Nion-Larmurier I., et al. (2020). Fecal microbiota transplantation to maintain remission in crohn's disease: a pilot randomized controlled study. Microbiome 8, 12. doi: 10.1186/s40168-020-0792-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer C. N., Mcquade J. L., Gopalakrishnan V., Mcculloch J. A., Vetizou M., Cogdill A. P., et al. (2021). Dietary fiber and probiotics influence the gut microbiome and melanoma immunotherapy response. Science 374, 1632–1640. doi: 10.1126/science.aaz7015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spigaglia P., Mastrantonio P., Barbanti F. (2018). Antibiotic resistances of clostridium difficile. Adv. Exp. Med. Biol. 1050, 137–159. doi: 10.1007/978-3-319-72799-8_9 [DOI] [PubMed] [Google Scholar]
- Suez J., Zmora N., Zilberman-Schapira G., Mor U., Dori-Bachash M., Bashiardes S., et al. (2018). Post-antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by autologous FMT. Cell 174, 1406–1423.e16. doi: 10.1016/j.cell.2018.08.047 [DOI] [PubMed] [Google Scholar]
- Surawicz C. M., Brandt L. J., Binion D. G., Ananthakrishnan A. N., Curry S. R., Gilligan P. H., et al. (2013). Guidelines for diagnosis, treatment, and prevention of clostridium difficile infections. Am. J. Gastroenterol. 108, 478–498. doi: 10.1038/ajg.2013.4 [DOI] [PubMed] [Google Scholar]
- Tomkovich S., Taylor A., King J., Colovas J., Bishop L., Mcbride K., et al. (2021). An osmotic laxative renders mice susceptible to prolonged clostridioides difficile colonization and hinders clearance. mSphere 6, e0062921. doi: 10.1128/mSphere.00629-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh P. J., Ley R. E., Hamady M., Fraser-Liggett C. M., Knight R., Gordon J. I. (2007). The human microbiome project. Nature 449, 804–810. doi: 10.1038/nature06244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Nood E., Speelman P., Kuijper E. J., Keller J. J. (2009). Struggling with recurrent clostridium difficile infections: Is donor faeces the solution? Euro Surveill. 14 (34), 19316. doi: 10.2807/ese.14.34.19316-en [DOI] [PubMed] [Google Scholar]
- Van Nood E., Vrieze A., Nieuwdorp M., Fuentes S., Zoetendal E. G., De Vos W. M., et al. (2013). Duodenal infusion of donor feces for recurrent clostridium difficile. N Engl. J. Med. 368, 407–415. doi: 10.1056/NEJMoa1205037 [DOI] [PubMed] [Google Scholar]
- Vrieze A., Van Nood E., Holleman F., Salojärvi J., Kootte R. S., Bartelsman J. F., et al. (2012). Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143, 913–6.e7. doi: 10.1053/j.gastro.2012.06.031 [DOI] [PubMed] [Google Scholar]
- Vyas D., Aekka A., Vyas A. (2015). Fecal transplant policy and legislation. World J. Gastroenterol. 21, 6–11. doi: 10.3748/wjg.v21.i1.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. W., Kuo C. H., Kuo F. C., Wang Y. K., Hsu W. H., Yu F. J., et al. (2019. b). Fecal microbiota transplantation: Review and update. J. Formos Med. Assoc. 118 (Suppl 1), S23–s31. doi: 10.1016/j.jfma.2018.08.011 [DOI] [PubMed] [Google Scholar]
- Wang H., Lu Y., Yan Y., Tian S., Zheng D., Leng D., et al. (2019. a). Promising treatment for type 2 diabetes: Fecal microbiota transplantation reverses insulin resistance and impaired islets. Front. Cell Infect. Microbiol. 9. doi: 10.3389/fcimb.2019.00455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu E. W., Gao L., Stastka P., Cheney M. C., Mahabamunuge J., Torres Soto M., et al. (2020). Fecal microbiota transplantation for the improvement of metabolism in obesity: The FMT-TRIM double-blind placebo-controlled pilot trial. PloS Med. 17, e1003051. doi: 10.1371/journal.pmed.1003051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang F., Cui B., He X., Nie Y., Wu K., Fan D. (2018). Microbiota transplantation: concept, methodology and strategy for its modernization. Protein Cell 9, 462–473. doi: 10.1007/s13238-018-0541-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Li N., Chen Q., Qin H. (2021). Fecal microbiota transplantation modulates the gut flora favoring patients with functional constipation. Front. Microbiol. 12. doi: 10.3389/fmicb.2021.700718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T., Lu G., Zhao Z., Liu Y., Shen Q., Li P., et al. (2020). Washed microbiota transplantation vs. manual fecal microbiota transplantation: clinical findings, animal studies and in vitro screening. Protein Cell 11, 251–266. doi: 10.1007/s13238-019-00684-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao D., Ye C., Zhang S., Lv X., Yang B. (2021). Analysis of risk factors for early clinical recurrence of inflammatory bowel disease after fecal microbiota transplantation. Am. J. Transl. Res. 13, 12875–12886. [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Horton J. R., Blumenthal R. M., Zhang X., Cheng X. (2021). Clostridioides difficile specific DNA adenine methyltransferase CamA squeezes and flips adenine out of DNA helix. Nat. Commun. 12, 3436. doi: 10.1038/s41467-021-23693-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou B., Yuan Y., Zhang S., Guo C., Li X., Li G., et al. (2020). Intestinal flora and disease mutually shape the regional immune system in the intestinal tract. Front. Immunol. 11. doi: 10.3389/fimmu.2020.00575 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flowchart of retrieval process.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding author.