Abstract
Objectives
The aim of this study was to understand the effects of the COVID-19 pandemic on paediatric cardiac services in critical access centres in low-income and middle-income countries.
Design
A mixed-methods approach was used.
Setting
Critical access sites that participate in the International Quality Improvement Collaborative (IQIC) for congenital heart disease (CHD) were identified.
Participants
Eight IQIC sites in low-income and middle-income countries agreed to participate.
Outcome measures
Differences in volume and casemix before and during the pandemic were identified, and semistructured interviews were conducted with programme representatives and analysed by two individuals using NVivo software. The qualitative component of this study contributed to a better understanding of the centres’ experiences and to identify themes that were common across centres.
Results
In aggregate, among the seven critical access sites that reported data in both 2019 and 2020, there was a 20% reduction in case volume, though the reduction varied among programmes. Qualitative analysis identified a universal impact for all programmes related to Access to Care/Clinical Services, Financial Stability and Professional/Personal Issues for healthcare providers.
Conclusions
Our study identified and quantified a significant impact of the COVID-19 pandemic on critical access to CHD surgery in low-income and middle-income countries, as well as a significant adverse impact on both the skilled workforce needed to treat CHD and on the institutions in which care is delivered. These findings suggest that the COVID-19 pandemic has been a major threat to access to care for children with CHD in resource-constrained environments and that this effect may be long-lasting beyond the global emergency. Efforts are needed to preserve vulnerable CHD programmes even during unprecedented pandemic situations.
Keywords: COVID-19, Public health, Congenital heart disease, Paediatric cardiology, HEALTH SERVICES ADMINISTRATION & MANAGEMENT
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The data were analysed using conventional content analysis using NVivo V.12 qualitative software.
The research team employed methods to add rigour to the process of data collection and analysis to enhance credibility, transferability, dependability and confirmability of findings.
Small sample size with only eight International Quality Improvement Collaborative (IQIC) sites participating.
With open-ended questions and probes, there is room for different interpretations of questions and answers among the interviewees.
The use of telemedicine at the participating sites is not captured in the IQIC database.
Introduction
Prior to COVID-19, children with congenital heart disease (CHD) were already struggling to access cardiovascular surgical care in low-income and middle-income countries (LMICs), such as in Guatemala and sub-Saharan Africa.1–4 These vulnerable paediatric cardiac facilities are burdened with shortages of staff, ventilators, intensive care unit (ICU) beds and operating rooms, as well as the postponement of non-emergency operations, all exacerbated by the pandemic.5 6 A study conducted to assess the impact of COVID-19 on paediatric cardiac services in India found a 73% and 74.5% reduction in cardiac surgeries and outpatient visits, respectively, across 24 paediatric cardiac centres in 2020 compared with 2019.7 The impact of the pandemic on paediatric cardiac centres in other LMICs has not been explored.
While there is great concern and uncertainty for patients whose procedures are delayed, there is also growing concern for the future of congenital heart surgery programmes. In countries with only one centre performing congenital heart surgery, lockdowns and closures can negatively impact the sustainability of vulnerable programmes. The purpose of this study was to understand the effects of the COVID-19 pandemic on paediatric cardiac services in critical access centres in LMICs. The study included evaluation of the quantitative change in the volume of cases performed and by thematic analysis through qualitative inquiry among selected sites participating in the International Quality Improvement Collaborative (IQIC) for CHD: Improving Care in LMICs.8
Methods
Design
Through a mixed-methods approach, this study conducted a retrospective review of the IQIC database and semi-structured interviews with a group of eight IQIC sites. Programmes that partook in this study were selected based on their status as a critical access centre in addition to their participation in the IQIC. For the purposes of this study, a critical access centre is defined as being the sole paediatric cardiac programme within a country or region. Among the IQIC sites, 10 were identified as critical access centres, and 8 agreed to participate in this study. Interviews took place between December 2020 and April 2021. The medical personnel interviewed at each site all worked within a paediatric cardiac programme. An author reflexivity statement has been included to acknowledge the role of each author and the codevelopment of this research (online supplemental appendix A).
bmjopen-2022-065031supp001.pdf (52.1KB, pdf)
Quantitative data collection and analysis
After reviewing global information about the pandemic for the 10 critical access IQIC sites, the time frame of data collection was selected to be March–November 2019 compared with March–November 2020. For the eight sites that agreed to participate, a retrospective review of the IQIC database was conducted to identify the number of surgeries performed and the age distribution and types of procedures in March–November 2019 and March–November 2020. The method for IQIC data collection has been previously reported.8 Types of surgery were placed into risk groups according to the Risk Adjustment for Congenital Heart Surgery (RACHS-1) method.9 The number, age distribution and RACHS-1 risk categories for each centre and in aggregate were compared for March–November 2019 vs March–November 2020 using Fisher’s exact test. The quantitative data assisted in planning the qualitative data collection and analysis.
Qualitative data collection and analysis
Once the invited IQIC site contact confirmed interest, they signed an informed consent document. Each IQIC site participated in one virtual (using the Zoom platform) interview lasting no more than 1 hour that took place at a mutually convenient time in December 2020 through April 2021. The first author (CD) and coinvestigator (BZ) used a semistructured interview guide to facilitate each interview (online supplemental appendix B). Each Zoom interview was recorded and transcribed verbatim. The first author relistened to the interview while reading the transcript to ensure accuracy.
bmjopen-2022-065031supp002.pdf (51.9KB, pdf)
Following confirmation of the written transcript, the data were analysed using conventional content analysis using NVivo V.12 qualitative software. The process consisted of reading and rereading the data to understand fully the participants’ words and intent. During the reading of the data, the coding process began. The first codes are codes that emerge directly from the data and are chosen because of emphasis, repetition, significance or clarity of statement. These codes were continuously reviewed, added and/or removed as new insights and ways of understanding the data set emerged.
Initially, each transcript was coded using this approach. Each investigator (CD and BZ) independently analysed the interviews focusing on similarities and differences among the eight sites. The researchers then met to discuss and compare their findings. After all codes were identified, codes were sorted and grouped into categories according to shared concepts to reduce the overall number. During the iterative coding process, data were continually reviewed and revised.
The research team employed methods to add rigour to the process of data collection and analysis to enhance credibility, transferability, dependability and confirmability of findings.
To enhance credibility, prolonged engagement, peer debriefing and member checking were employed. Prolonged engagement occurred by interviewing members from each IQIC programme for a full hour. This provided time to understand the context and ensure that data collection was comprehensive. Prolonged engagement also fosters the development of a trusting relationship with the participants, which facilitates sharing information of a sensitive nature. In addition, members of the investigative team have interacted with each of the IQIC teams for several years in improving and supporting care for children with CHD, adding to a trusting relationship.
Detailed quotes from participants were used to substantiate data analysis and coding decisions. The quotes assisted a reader in confirming the accuracy of the researchers’ interpretation to further enhance credibility. Peer debriefing took place as interviews progressed to ensure that the research data analysis remained true to the participant’s words. After analysis, we randomly selected four programmes to complete member checking and recontacted the IQIC teams who were interviewed to confirm interpretations using their individual interview quotes. Information regarding the researcher, population studied, sampling and coding decisions is detailed in this report to assess the transferability of the study findings.
Dependability was achieved through an inquiry audit of the process by JC, thus attesting and certifying that the process was acceptable, professional, legal and ethical. Confirmability was achieved through a confirmability audit by JC, which examined the product (data), findings, interpretations and recommendations attesting that the findings are supported by the data.
The intent of this descriptive study using mixed methods is to understand the impact of the COVID-19 pandemic on critical access centres in a select group of countries. For the qualitative assessment of this relatively homogeneous group, it was believed that saturation of information would be obtained after interviews 5–6 and interviews 7 and 8 were conducted to serve as confirmatory to the findings. The limited number of centres did not provide power beyond the description for the quantitative assessment.
Patient and public involvement
Patients were not involved in this research.
Results
A total of eight programmes participated in our study (table 1). Out of the eight interviews, four were conducted in December 2020, two were conducted in January 2021 and two were conducted in April 2021. Six programmes were in a general hospital, one programme was part of a paediatric hospital and one programme was a cardiac unit not a part of a general or paediatric hospital. The participants all provide paediatric cardiac care and included paediatric cardiologists, a paediatrician, a paediatric cardiology resident, a head of cardiac services, a consultant cardiothoracic surgeon, a chief of congenital cardiac surgery and a director of a paediatric cardiac unit.
Table 1.
The eight critical access centres that participated in this study
| Critical access Centre | Location | First reported COVID-19 case |
| Mother and Child Health Institute of Serbia | Belgrade, Serbia | 06 March 2020 |
| French Medical Institute for Children (FMIC) | Kabul, Afghanistan | 24 February 20 |
| National Heart Hospital | Sofia, Bulgaria | 08 March 2020 |
| Windhoek Central Hospital Cardiac Unit | Windhoek, Namibia | 14 March 2020 |
| Unidad de Cirugia Cardiovascular de Guatemala | Guatemala City, Guatemala | 13 March 2020 |
| Uganda Heart Institute | Kampala, Uganda | 21 March 2020 |
| JoAnn McGowan Pediatric Cardiac Surgery Center | Tbilisi, Georgia | 26 February 2020 |
| Jakaya Kikwete Cardiac Institute | Dar Es Salaam, Tanzania | 16 March 2020 |
Quantitative results
For the quantitative data, seven of the eight sites were analysed, as one of the sites had to be excluded due to missing data (table 2). In aggregate, there were 20% fewer cases conducted in 2020 compared with 2019 among the seven sites (figure 1). All showed reductions in case volume except for one site, which experienced an increase in cases from March–November 2019 to March–November 2020. The greatest reduction in case volume between 2019 and 2020 was 40%.
Table 2.
Age category, RACHS-1 and volume of cases on seven sites in 2019 vs 2020 (March–November)
| 2019 | 2020 | P value | |
| (n=776) | (n=571) | ||
| Age category | 0.26 | ||
| ≤30 days | 101 (13%) | 67 (11%) | |
| 31 days to <1 year | 210 (27%) | 196 (31%) | |
| 1 to 17 years | 395 (51%) | 306 (49%) | |
| ≥18 years | 70 (9%) | 59 (9%) |
| (n=686) | (n=548) | ||
| RACHS-1 risk category | 0.28 | ||
| 1 | 190 (28%) | 124 (23%) | |
| 2 | 311 (45%) | 260 (47%) | |
| 3 | 145 (21%) | 132 (24%) | |
| 4 | 31 (5%) | 27 (5%) | |
| 5–6 | 9 (1%) | 5 (1%) | |
| Volume of cases | n=776 | n=628 |
Figure 1.
Volume of cases among the seven sites, March–November (2019 vs 2020).
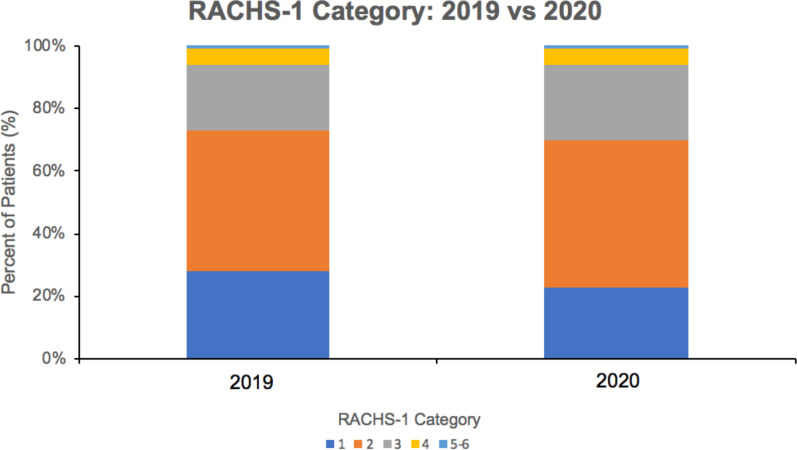
The data was analysed based on the level of severity of CHD through looking at the age category and RACHS-1 risk category. Among the seven sites, there was no difference in the distribution of RACHS-1 risk categories among the cases completed in 2019 compared with 2020 (figure 2). Similarly, the proportion of each age group remained similar between 2019 and 2020 (figure 3).
Figure 2.
RACHS-1 category, March–November (2019 vs 2020).
Figure 3.
Age category, March–November (2019 vs 2020).
Qualitative results
From the interviews and coding analysis, three themes were identified (table 3): (1) access to care and clinical services, (2) financial impact and (3) professional and personal impact.
Table 3.
Interview themes identified across the eight critical access centres
| Theme | Summary of description | Quotes | Translation in practice |
| Access to care/clinical Services | Access to care/clinical services impacted all programmes. This included hospital, city and/or countrywide lockdowns which restricted travel between/within countries. In addition to these restrictions, services were reduced as hospitals were only allowed to perform emergent cases. Access to care was further reduced with staff being reassigned to support COVID facilities and/or having to take medical leave. The decreased access has led to excess burden in these critical access centres as waiting lists increase. |
Lockdown/Restricted Travel “And then there was a dramatic decrease in outpatient cardiology appointments, because there was no transportation and cities were locked down so parents just could not take [their] baby to the doctor” Reduction in Services “Since exactly March this year, we had to close lots of services and actually support services for [patients] as well as cardiac surgery. So unfortunately, our activities reduced nearly to 50%.” Changes in Team Composition “We've had staff taking leave because of exposure or because of coming down with COVID, both doctors and nurses. I cannot tell you the magnitude to which it has affected us, but it has slowed down the ICU, especially in the last 1 month of operations of the ICU.” Waiting Lists “Our waiting lists are definitely too long. Sitting with 250 patients and that is both simple and complex heart disease and they are born every day. The burden is so huge. Unfortunately, this year we've only been able to cut on about 50 or so, which is pretty unfortunate.” |
Have transport systems in place to get patients to the hospital (ie, minivans to pick up patients) (Guatemala) Establish online services to continue supporting patients if in-person activities are reduced Ensure staff have safety equipment to protect themselves from exposure (ie, masks, hand sanitiser,) Grow the number of health personnel and hospitals to help alleviate the burden of patients with CHD |
| Financial Impact | There were large financial impacts to hospitals/programmes and staff. In hospitals, money and supplies were reallocated to support COVID-19 facilities resulting in budget cuts to some programmes. Additionally, reduction in services resulted in financial loss for many of the centres. For staff, the economic impacts on the hospital resulted in some staff not receiving pay. |
Financial Impact to Hospitals/Programs “Financially, it’s my biggest concern because of course before the pandemic our budgets were still to be decided for the year. By the pandemic, of course, money had to be redirected to COVID functions, building new facilities and equipping, as well as creating extra workforce to work in those areas. So, our economy, it was already kind of crippling and now with the COVID, so much was invested into fighting or trying to alleviate the COVID burden. And as a result, a lot of departments are going to suffer from budget deficiencies.” Financial Impact to Staff “We were nearly bankrupt. We had to close lots of services. I remember nearly 70% of the staff were on forced leave and unpaid leave or annual leave from the hospital because we even couldn't pay the salaries of the hospital” |
Implement an emergency relief fund to mitigate hospital bankruptcy Increase governmental support to help with retention of experienced staff |
| Professional/personal Impact | In a professional setting, not having many surgical cases and/or restrictions made it hard for medical professionals to advance in their profession. Additionally, many trainings and visiting team programmes were cancelled as a result of COVID-19. On a personal level, there was great variability seen among the interviewees. Most were impacted with not being able to see family and feeling emotionally exhausted or stressed. |
Professional Impact “The visiting teams were not coming and the visiting teams when they come it’s not only providing services but also training the local teams, so we miss the training platform of the visiting team, but also they're coming with consumables and some of the consumables are helping the local team to continue with surgery when they're not here.” Personal Impact “This year I think it’s better, yes, but yeah it was last year was a lot of stress in this matter, personally, because well, I had to take care of not only my family, but I had to take care of this big family of UNICAR, so yeah. Was a lot of stress.” |
Holding trainings, meetings and conferences through online platforms to allow for professional development Provide resources to staff to help with their mental well-being |
CHD, congenital heart disease; ICU, intensive care unit.
Access to care and clinical services
Limitations in access to care and clinical services impacted all programmes. Regional lockdowns restricted travel between and within countries, making it difficult for patients to receive care. The restrictions specifically reduced outpatient services as ‘there was no public transportation so parents could not take their baby to the doctor.’ Country-wide lockdowns further impacted these critical access centres that provide care for other countries as ‘complex patients who needed to go outside [the country] for their corrections could not go because the borders were closed.’ Additionally, compromised transportation made it difficult to access goods as some sites rely on ‘transportation [of goods] through airline cargoes [which] was closed for nearly 3 months’ which resulted in ‘consumables not coming on time.’
In addition to these restrictions, all hospitals reduced services to only emergent cases to support capacity for COVID-19 hospitalisations. Reduction in outpatient services ranged between sites from 25% to 70%. Reduction in the volume of surgeries performed was also notable among sites. For instance, ‘usually [there is] between 60 to 90 newborns every year that [one site] has to operate on with critical heart disease. However, last year [they] only did 22 [operations], so that means 70 patients probably died at home and never went to the hospital.’ Delays in surgical procedures were also evident from COVID-19 safety measures. If a child within the ICU was COVID-19 positive, ‘[they] could not admit anybody else into the ICU so for a period of about 2 weeks, [they] could not operate because [they] had to fumigate the entire [ICU].’
Additionally, changes in team composition affected access to care as some staff was reassigned to provide additional support to COVID-19 dedicated facilities and/or had to take medical leave because of contracting COVID-19. One participant stated, ‘60% to 65% of [their] staff contracted COVID-19, and the experienced staff from [the] ICU, especially from the cardiac ICU, were transferred to the [COVID-19 ICU].”
The restrictions and reduction in services increased the number of patients on waitlists. The burden is large with ‘nearly 2800 patients’ on waiting lists in one hospital, which ‘is still growing and has been growing over the years.’ Especially with lost operating time, ‘the waiting list(s) will only get worse’ in many of these programmes.
Financial impact
There were large financial impacts on hospitals, programmes and staff. In hospitals, money and supplies were reallocated to support COVID-19 facilities resulting in budget cuts to some programmes. With funds being redirected to ‘build new [COVID-19] facilities and equipping them, a lot of departments are going to suffer budget deficiencies.’ Furthermore, hospital closures and reduced procedures meant that minimal funds were coming in. The significant reduction in services that many of these centres saw equate to ‘very serious financial losses.’ In addition to reduced services impacting budgets, COVID-19 introduced new costs to programmes that many were not prepared for. Testing patients for COVID-19 ‘is costly with the cheapest [test] costing between US$50–US$60,’ which for LMICs is a significant expense. With it being ‘more expensive to take care of patients during the pandemic,’ the financial impact on the future of these hospitals is concerning.
For staff, the economic impacts on the hospital resulted in some staff not receiving pay. As the hospitals were under financial stress, ‘some of the staff [was] sent on forced leave and unpaid leave as [the hospital] could not afford to pay their salaries.’ This resulted in many experienced staff members leaving hospitals to work in other healthcare settings.
Professional and personal impact
In a professional setting, not having many surgical cases and/or restrictions made it hard for medical professionals to advance in their profession. With exam cancellations, ‘they could not take on residents’ as some hospitals had expected. Additionally, many trainings and visiting team programmes were cancelled because of COVID-19. Plans shifted as programmes ‘could not do what [they] had originally planned to do, which included trainings and exchange programmes, and people coming to visit.’ Many of these hospitals ‘depend on visiting teams, so when the visiting team was not coming, [they] could not do a lot of surgeries.’
The personal impact varied greatly among the interviewees. Most were impacted by not being able to see family and feeling emotionally exhausted or stressed. There is this fear ‘that you can transmit something to the most important people in your life.’ COVID-19 and their hospital’s experience ‘was really quite emotionally tasking’ and ‘a lot of stress because [they] had to take care of not only [their] family, but [they] had to take care of this big family of [their hospital].’
Discussion
The WHO has published several operational guidance documents on maintaining essential health services during the COVID-19 pandemic and conducted global surveys to describe the extent of disruptions to essential health services caused by the COVID-19 pandemic.10 11 While these documents include ‘critical facility-based therapies’ for chronic diseases, they do not mention paediatric cardiac surgery or surgical services, except some very specific emergencies, which we think is an omission. The eight paediatric congenital heart surgery programmes that were interviewed are all critical access centres, providing all or a significant part of all paediatric cardiac care in the country. The presence of these programmes in their respective regions is essential as they provide all or nearly all the care for CHD. Advancements in CHD care have largely benefitted high-income countries (HICs), while of the more than 1 300 000 babies born with CHD annually, 90% live in areas with little to no care.12 We believe, as Dearani et al, that cardiac surgery is an essential life-saving procedure, and if it were to be reduced, children would die.13 Thus, if critical access hospitals are forced to shut down, even temporarily, waiting lists will grow, and the number of patients at risk of dying increases as more patients are in need than are able to be treated. While these sites were all hit by COVID-19 at varying timeframes with different degrees in severity, their programmes were all impacted by the pandemic, whether due to closures, regional lockdowns or the development of new COVID-19 facilities.
The Global Surgery study in 2015 estimated that only 12% of the world’s specialist surgical and anaesthesia workforce practice in the poorest parts of the world.14 Yet, a third of the world population lives there, accounting for most of the global surgical burden. Thus, hospitals in low-resource settings are at a higher risk of substantial disruptions to health services due to the coronavirus. In our study, one of the most prominent effects the pandemic had on these critical access sites was the disruption and reduction of services. All eight sites experienced suspended elective operations in their facilities and were only allowed to perform complex or emergency surgeries. By the time the interviews were conducted in December 2020 and January 2021, some sites noted initial recoveries from the first wave of the pandemic, however, the two sites interviewed in April 2021 discussed the situation worsening with the resurgence of cases. Our results were similar to that of another paediatric cardiac study conducted in India which found that there was a 66% reduction in hospitalisations and cardiac surgeries as a result of COVID-19.7 Severe reductions in services in already resource-constrained settings may have serious impact over the coming years within these regions. Follow-up interviews should be conducted with these critical access centres to determine whether their programmes were able to fully recover.
With the regional and international lockdowns, transportation was compromised within each country. As a critical access centre, the country and often neighbouring regions rely on these hospitals to provide paediatric cardiac care. However, with borders being closed to mitigate COVID-19 transmission across countries, patients outside the region may struggle to access care. A study conducted at a Kenyan Referral Hospital for mental healthcare delivery demonstrated challenges in transportation as the limited ability to move made it more difficult for patients who had to travel long distances to receive care.15 Additionally, many of these critical access programmes do not have access to telemedicine to connect providers to patients through video. While some hospitals communicate with other facilities through telehealth, communication with patients occurs over the phone or in person. Telemedicine does have its limitations as it cannot impact complex cases that need surgical care. Still, it could be beneficial for consultation on elective cases that do not require immediate operations. Extended waiting times can transform an elective case into an urgent or potentially inoperable case.
Another major concern brought up by these hospitals were their finances. LMICs are facing serious financial challenges as it is estimated to cost around US$52 billion per month to support healthcare systems in response to COVID-19.16 Our study revealed that many of the programmes interviewed were impacted by budget cuts as hospitals were unable to cover the salaries of their staff. This could negatively impact the future of their hospital as experienced medical staff are forced to take unpaid leave and seek outside employment. In paediatric cardiac care, retaining trained staff members is essential to sustaining the normal function of a critical access centre. Studies suggest that protecting surgical personnel should be a priority in LMICs.17 It is a time extensive process to train paediatric cardiac specialists, and well-trained personnel are hard to find within LMICs where human resources are already extremely limited. The future of these resource-limited programmes is concerning, and further studies should be conducted to better understand the financial burdens created by COVID-19.
In LMICs, task sharing is common practice among healthcare workers who are often reorganised and expected to work in alternative roles due to staff shortages or changes in team composition.18 In this study, our findings supported this as many staff who contracted COVID-19 were forced to stay home, resulting in the reallocation of medical personnel. Given their LMIC critical access centre status, additional reductions in staff can be a major concern when staff shortages are the norm. However, the reduction of surgical volumes in the hospital lessened the burden of staff members when some healthcare workers had to be sent home.
The staff of the interviewed programmes is at greater risk of contracting the virus due to their increased risk of exposure when working in a hospital setting. Healthcare workers are even suspected to be at an increased risk of developing mental health problems such as depression, anxiety, or insomnia due to the stressful nature of their work environment.19 Most of the interviewees expressed a feeling of fear about contracting the virus and the possibility of infecting the people they love. Fortunately, much of their perspective has changed with the introduction of vaccines. Additionally, given their expertise in providing intensive care to critically ill patients, many staff members in these paediatric cardiac critical access programmes were assigned to help in COVID-19 dedicated facilities. This not only took away key personnel from their paediatric cardiac service but also became emotionally taxing and worrisome as they were uncertain of their own health. In programmes that are affected by budget cuts, there is an added fear of healthcare workers losing their jobs and their incomes during a time of economic uncertainty. Workers in essential access programmes must function in work environments that are demanding, exhausting and oftentimes unsafe due to shortages of medical equipment. These individuals are also isolated from family members for extended periods, which many interviewees had stated is very difficult. More research should be conducted on how COVID-19 has emotionally impacted medical staff in LMICs and ways to mitigate the stressful environments in which they work.
This research highlights the necessity of protecting the health of these critical access centres that were already constrained in supplies, personnel and access prior to the pandemic. While we admire the resiliency of the leadership at these critical access centres, all of which eventually opened back up, we recognise that these programmes and the patients with CHD they serve are vulnerable. Because of this, there is a need to not only advocate for the care of CHD children but also to preserve the programmes that serve them. As the COVID-19 pandemic is still ongoing and pandemics will reoccur, there are some potential solutions we recommend to help these centres prevent similar issues in the future. To address access of care, having transport systems in place and telehealth services can ensure patients are able to receive timely care. Guatemala noted their successful use of vans to pick up patients to guarantee accessibility of care. To mitigate the financial impact, there should be increased governmental support to help with the retention of experienced staff and to implement emergency relief funds. To target the professional and personal impact, trainings and conferences can be conducted on online platforms to promote professional development and hospitals resources should be provided to staff to support their mental well-being. The development of these paediatric critical access centres is difficult, and thus, it is in our best interest to protect these programmes to ensure their sustainability in their regions.
Limitations
A limitation of this study was that it relied largely on the qualitative data gathered from the interviews. With open-ended questions and probes, there is room for different interpretations of questions and answers among the interviewees. While we believe we reached saturation in our thematic analysis based on eight interviews, we cannot be certain that additional themes would not have been identified if more interviews were conducted or if findings are transferable to other LMICs or non-critical access sites. Additionally, the role of telemedicine was not adequately explored among the participating sites. While the use of telemedicine for surgical care has been emerging in LMICs and has been shown to streamline the follow-up care of CHD patients, this data is not captured withing the IQIC database.20 21 Another limitation was the small sample size for quantitative analysis and that there was variation in the timing of the impact of the pandemic on various programmes, which only compared data between March and November in 2019 vs 2020. Further studies should be conducted regarding the effects of COVID-19 on paediatric cardiac critical access centres at later time periods. Last, our dataset only included information on children who underwent surgery, not those who needed surgery but were delayed or deferred. An analysis of the impact of the COVID-19 pandemic on children who could not seek care should be explored as this could direct future research and policy.
Conclusion
Through the combined effects of shortages in staff, equipment and money, LMICs deal with greater burdens on their already resource-limited healthcare systems compared with HICs. There is an added burden for these paediatric cardiac critical access centres who are expected to treat and care for a larger population of individuals within a country. Our study shows that care for children with CHD has been threatened during the pandemic as closures of programmes and lockdowns cause delays in treatment, affect the well-being of highly skilled clinical staff capable of treating CHD, and jeapordize financial stability of the institutions providing care. Even prior to the pandemic, waiting lists were very long, and the pandemic has only increased the likelihood of greater mortality and disability. It is crucial for these programmes to continue operations to mitigate the burden of waiting lists and reduce mortality for children with CHD. This study should prompt governments and policymakers to consider the longer-term impact of pandemic measures in the future, especially public health measures to slow the spread of COVID-19 and ensure access to care through exemption policies, protection of specialised staff, and government financial assistance to help services recover quickly.22 If, because of the pandemic, such critical access centres close permanently, this will inevitably affect the survival of every child with CHD in their catchment region or country indefinitely, adding unnecessarily to the impact of the pandemic.
Supplementary Material
Acknowledgments
We would like to thank Kaitlin Doherty-Schmeck for her help in facilitating this project.
Footnotes
Twitter: @bzheleva
Contributors: KJ and BZ developed the concept; KJ, JC BZ and CD created the study design and methodology; CD and BZ conducted the interviews; KG conducted the data analysis; CD, JC and BZ drafted the manuscript; KJ is responsible for the overall content as the guarantor; all authors provided data, reviewed results or reviewed the manuscript, and approved the final version of the manuscript; BB, NB, GC, IC, NM, MO, DP, FS and TS were interviewed and contributed to the final version of the manuscript.
Funding: CD received the Harvard College Research Program award from the Monadnock Fund for Undergraduate Research.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Boston Children’s Hospital; IRB-P00037462. Participants gave informed consent to participate in the study before taking part.
References
- 1.Nguyen N, Jacobs JP, Dearani JA, et al. Survey of nongovernmental organizations providing pediatric cardiovascular care in low- and middle-income countries. World J Pediatr Congenit Heart Surg 2014;5:248–55. 10.1177/2150135113514458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Musa NL, Hjortdal V, Zheleva B, et al. The global burden of paediatric heart disease. Cardiol Young 2017;27:S3–8. 10.1017/S1047951117002530 [DOI] [PubMed] [Google Scholar]
- 3.Larrazabal LA, Jenkins KJ, Gauvreau K, et al. Improvement in congenital heart surgery in a developing country: the Guatemalan experience. Circulation 2007;116:1882–7. 10.1161/CIRCULATIONAHA.107.695403 [DOI] [PubMed] [Google Scholar]
- 4.Zimmerman M, Sable C. Congenital heart disease in low-and-middle-income countries: focus on sub-Saharan Africa. Am J Med Genet C Semin Med Genet 2020;184:36–46. 10.1002/ajmg.c.31769 [DOI] [PubMed] [Google Scholar]
- 5.Stephens EH, Dearani JA, Guleserian KJ, et al. COVID-19: crisis management in congenital heart surgery. World J Pediatr Congenit Heart Surg 2020;11:395–400. 10.1177/2150135120931398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Protopapas EM, Rito ML, Vida VL, et al. Early impact of the COVID-19 pandemic on congenital heart surgery programs across the world: assessment by a global Multi-Societal Consortium. World J Pediatr Congenit Heart Surg 2020;11:689–96. 10.1177/2150135120949462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choubey M, Ramakrishnan S, Sachdeva S, et al. Impact of COVID-19 pandemic on pediatric cardiac services in India. Ann Pediatr Cardiol 2021;14:260–8. 10.4103/apc.apc_133_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jenkins KJ, Castañeda AR, Cherian KM, et al. Reducing mortality and infections after congenital heart surgery in the developing world. Pediatrics 2014;134:e1422–30. 10.1542/peds.2014-0356 [DOI] [PubMed] [Google Scholar]
- 9.Jenkins KJ. Risk adjustment for congenital heart surgery: the RACHS-1 method. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2004;7:180–4. 10.1053/j.pcsu.2004.02.009 [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. (NO. WHO/2019-nCoV/essential_health_services/2020.2). Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 [Accessed 16 Mar 2022].
- 11.World Health Organization . Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 22 April 2021(No. WHO/2019-nCoV/EHS_continuity/survey/2021.1). Available: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 [Accessed 16 Mar 2022].
- 12.Tchervenkov CI, Jacobs JP, Bernier P-L, et al. The improvement of care for paediatric and congenital cardiac disease across the World: a challenge for the world Society for pediatric and congenital heart surgery. Cardiol Young 2008;18 Suppl 2:63–9. 10.1017/S1047951108002801 [DOI] [PubMed] [Google Scholar]
- 13.Dearani JA, Stephens EH, Guleserian KJ, et al. COVID-19: FAQs-congenital heart surgery recovery and defining a "New Normal". World J Pediatr Congenit Heart Surg 2020;11:548–56. 10.1177/2150135120934741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386:569–624. 10.1016/S0140-6736(15)60160-X [DOI] [PubMed] [Google Scholar]
- 15.Kwobah E, Jaguga F, Robert K, et al. Efforts and challenges to ensure continuity of mental healthcare service delivery in a low resource settings during COVID-19 pandemic-a case of a Kenyan referral hospital. Front Psychiatry 2020;11:588216. 10.3389/fpsyt.2020.588216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaye AD, Okeagu CN, Pham AD, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol 2021;35:293–306. 10.1016/j.bpa.2020.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma X, Vervoort D, Reddy CL, et al. Emergency and essential surgical healthcare services during COVID-19 in low- and middle-income countries: a perspective. Int J Surg 2020;79:43–6. 10.1016/j.ijsu.2020.05.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ullrich S, Cheung M, Namugga M, et al. Navigating the COVID-19 pandemic: lessons from global surgery. Ann Surg 2020;272:e216–8. 10.1097/SLA.0000000000004115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khanal P, Devkota N, Dahal M, et al. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health 2020;16:89. 10.1186/s12992-020-00621-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Owolabi EO, Mac Quene T, Louw J, et al. Telemedicine in surgical care in low- and middle-income countries: a scoping review. World J Surg 2022;46:1855–69. 10.1007/s00268-022-06549-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sachdeva S, Saxena A, Shakya S. Changing pattern of congenital heart disease care during COVID-19 pandemic [published correction appears in Indian J Pediatr. 2022 Jan;89(1):105]. Indian J Pediatr 2021;88:899–904. 10.1007/s12098-021-03702-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020;8:e901–8. 10.1016/S2214-109X(20)30229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065031supp001.pdf (52.1KB, pdf)
bmjopen-2022-065031supp002.pdf (51.9KB, pdf)
Data Availability Statement
No data are available.