Abstract
Objectives
The study aimed to determine how eHealth was adopted in pharmaceutical care (PC), the outcome reported and the contextual factors.
Design
Systematic literature review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Data sources
Literature was searched in six databases including PubMed, Scopus, Medline, Web of Science, Science Direct and China National Knowledge Infrastructure.
Eligibility criteria
Studies which reported the usage experiences of eHealth in any aspects of PC by pharmacists during the COVID-19 pandemic, written in English or Chinese, and published in peer-reviewed journals between December 2019 and March 2022 were included. Opinion articles, conference abstracts, correspondence, letters and editorials were excluded.
Data extraction and synthesis
The literature search was completed on 15 April 2022. Two researchers independently conducted the literature search and extracted the data into an Excel table informed by the logic model with the key components of goals, input, activities, output and contextual factors.
Results
Forty-three studies were included in this review. During the COVID-19 pandemic, hospital pharmacists, community pharmacists and specialist pharmacists in 17 countries continued to educate, consult, monitor and manage the patients and the general public via phone calls, videoconferences, mobile applications, social media, websites and/or enhanced interoperability of electronic medical records. Assuring the continuity of pharmacy care, reduced need for hospital visits, and improved work accuracy and efficiency were the benefits of eHealth mostly reported. Contextual factors affecting the adoption of eHealth were multifaceted, prompting supporting actions at the levels of government, hospital/pharmacy, pharmacists and patients.
Conclusion
This study revealed the wide adoption of eHealth in PC during the pandemic and the emerging evidence for its importance. Proper adoption of eHealth will help reshape the mode of pharmacy services to ensure continuity, quality and efficiency of care amid the challenges of the pandemic.
PROSPERO registration number
CRD42022299812.
Keywords: COVID-19, PUBLIC HEALTH, Telemedicine
STRENGTHS AND LIMITATIONS OF THIS STUDY
This review analysed literature on adopting eHealth in pharmaceutical care (PC) during COVID-19 pandemic written in either English or Chinese identified from six databases.
The study complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to address the research question developed using the population, intervention, comparison, outcome and time frame framework.
The use of a logic model to guide data extraction and analysis helped to depict an overall landscape of all the factors relevant to the research question in a structured approach.
Our search strategy might not have allowed the capture of all experiences of eHealth in PC if the pharmacist’s role was embedded in an interprofessional programme.
Introduction
Being an integral part of the health system, pharmaceutical system is charged with an important goal of ensuring the equitable access to pharmaceutical products and their quality use based on scientifically sound evidence and supported by pharmaceutical care (PC).1 PC is defined as ‘the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life’.2 By providing PC, pharmacists help to reduce drug-related problems, assuring rational drug use, supporting clinical management and promoting healthy lifestyles.3 4
Since the onset of the COVID-19 pandemic, the delivery of PC has been inevitably disrupted by major public health measures, compromising the provision of medicines and care. Nevertheless, pharmacists are expected not only to ensure the continuity of care but also to adapt PC to the new needs during the challenging time.5 As such, eHealth has been increasingly adopted to support PC to overcome geographic barriers and enhance health outcome.6
According to the WHO, eHealth is defined as ‘the cost-effective and secure use of information and communication technology (ICT) through online in support of health and health-related fields, including healthcare services, health surveillance, health literature, and health education, knowledge, and research’.7 Reportedly, integrating eHealth into PC is beneficial to patient self-management and drug adherence, clinical disease management and health promotion.3 8–10 During the COVID-19 pandemic, as a result of public health measures resulting in reduced accessibility to hospitals or pharmacies, the traditional mode of in-person care delivery would no longer suffix. eHealth has, thus, been widely considered as an instrument for setting up a more innovative, efficient and resilient PC service model.11
The research interest in examining the interface between PC and eHealth has been growing. Some studies focused on evaluating particular PC-eHealth programmes. Spanakis et al evaluated a personalised eHealth platform that addressed key features of PC and found that eHealth could be used as a tool to allow pharmacists provide personalised PC services to optimise pharmacotherapy.12 Other studies might focus on the application of PC-eHealth in the management of particular diseases. The study by Jeminiwa et al demonstrated the effectiveness of eHealth in improving adherence to inhaled corticosteroids among patients with persistent asthma.13 Kilova et al addressed the prospects for ICT in providing OC and how eHealth related technologies had aided in the promotion of patient care during the outbreak of the epidemic.14 15 Another review by Iftinan et al primarily explored the eHealth services which could be used as an immediate alternative to PC for chronically ll patients during an epidemic.16
At present, while most of the current research focused on how eHealth might benefit the continuous access to essential pharmacy services in the absence of in-person interactions between pharmacists and their patients, there is little systematic research about the ‘know-how’ of integrating eHealth services and tools in PC to perform certain interventions or achieve predefined outcomes amid the challenges of the COVID-19 pandemic. Considering the potential benefits of applying eHealth in maintaining pharmaceutical services, empowering patients to improve compliance and adherence, reducing the risks of drug-related problems (eg, adverse drug reactions or drug interactions) and supporting pharmacovigilance amid the challenges of the COVID-19 pandemic,17–19 this review aims to determine how eHealth was adopted in PC, the outcome reported and the contextual factors identified. The study findings are expected to be useful for informing the optimisation of eHealth in PC whenever needed in future public health events.
Methods
Study design
This systematic literature review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.17 The use of the PRISMA 2020 statement for guidance was to transparently report why the review was done, what the authors did, and what had been found during the course of identifying, selecting, appraising and synthesising studies.17 The review protocol had been registered in The International prospective register of systematic reviews (PROSPERO) with the reference number: CRD42022299812 (available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022299812). A combination of 6 databases were used to optimise the yield of relevant research and the databases (including PubMed, Scopus, Medline, Web of Science, Science Direct and China National Knowledge Infrastructure (CNKI)) were selected because they specialised in scholarly literature related to health and medical topics. The literature search was completed on 15 April 2022.
Search strategy
The research question ‘How did pharmacists employ eHealth during the COVID-19 pandemic for the provision of care to their patients?’ was developed using the population, intervention, comparison, outcome and time frame (PICOT) framework.18 In the PICOT framework, the population referred to pharmacists, either practised alone or as a member of an interprofessional team and regardless of their work setting; the intervention referred to adopting eHealth for the purpose of tele-education, tele-consultation, tele-monitoring, tele-case-management, tele-mentoring); the comparison is not applicable; the outcome referred to the impact of the care on people cared by pharmacists via eHealth; and the time frame was the period of COVID-19 pandemic.
Considering the three major concepts “pharmaceutical care”, “eHealth” and “COVID-19 pandemic” that constituted the research question of this review, their Medical Subject Headings terms as well as the corresponding keywords and phrases identified in related literature were used to formulate a comprehensive search strategy. Terms within “pharmaceutical care”, “eHealth” and “COVID-19 pandemic” were combined with OR, and this results from each concept were combined with AND. A detailed description of the search strategies for each chosen database is provided in online supplemental file 1. In addition, the reference lists and citations of included articles were examined to identify further papers for inclusion.
bmjopen-2022-066246supp003.pdf (198KB, pdf)
Eligibility criteria
Studies which reported the use of eHealth in any aspects of PC during the COVID-19 pandemic, published between December 2019 (when cases of COVID-19 infection were first reported) and March 2022, written in English or Chinese, and published in peer-reviewed journals were included. The study types were limited to descriptive studies, prospective observational studies, retrospective cohort studies, retrospective chart reviews, cross-sectional surveys and qualitative studies. Studies which reported about the use of eHealth to support the use of medicines during the COVID-19 pandemic by healthcare professionals other than pharmacists were not considered. In addition, opinion articles, conference abstracts, correspondence, letters and editorials were excluded.
Study selection, data extraction and presentation
All members in the research team responsible for literature screening which included two Master students (ZFC and PKT) and two senior researchers (HH and COLU) were fluent in both English and Chinese. Two of the authors (ZFC and PKT) independently conducted the literature search and applied the inclusion and exclusion criteria. After the removal of duplication, citations were screened for inclusion by title first, and the remaining papers were then screened by abstracts (ZFC and PKT). After initial screening, the full text of studies were screened (ZFC and PKT) with guidance from one of the senior researchers (COLU) who randomly selected and checked a percentage of the included and excluded articles to ensure the eligibility of the included papers and the appropriateness of the excluded papers. Any differences were discussed and resolved among ZFC, PKT, HH and COLU by consensus.
On confirmation of the included studies, the reference lists were first examined to identify any further papers for inclusion (ZFC and PT). This was followed by data extraction, in which the required data from each included study was extracted and input into a pre-designed Excel table (ZFC and PKT). In addition to the characteristics of the included studies (such as first author, year of publication, study type, study location, study aim, targets of eHealth pharmacy service and types of pharmacists involved), the design of the Excel table was also informed by the types of eHealth involved and the logic model featuring the key components of goals, input, activities, output and contextual factors.19
For the purpose of this study within the context of the logic model, ‘input’ referred to the eHealth tools involved and the support from different stakeholders such as the government, pharmacist professional organisations, hospital, pharmacy and pharmacist; ‘activities’ referred to services provided by pharmacists with eHealth; ‘output’ and ‘outcome’ referred to the impact of the services pharmacists provided with eHealth on the people they cared for. Any divergences during the data extraction process were resolved through discussion among ZFC and PKT, and subject to agreement by HH and COLU and final confirmation by all authors. Narrative synthesis was undertaken to summarise and report the findings.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
Study characteristics
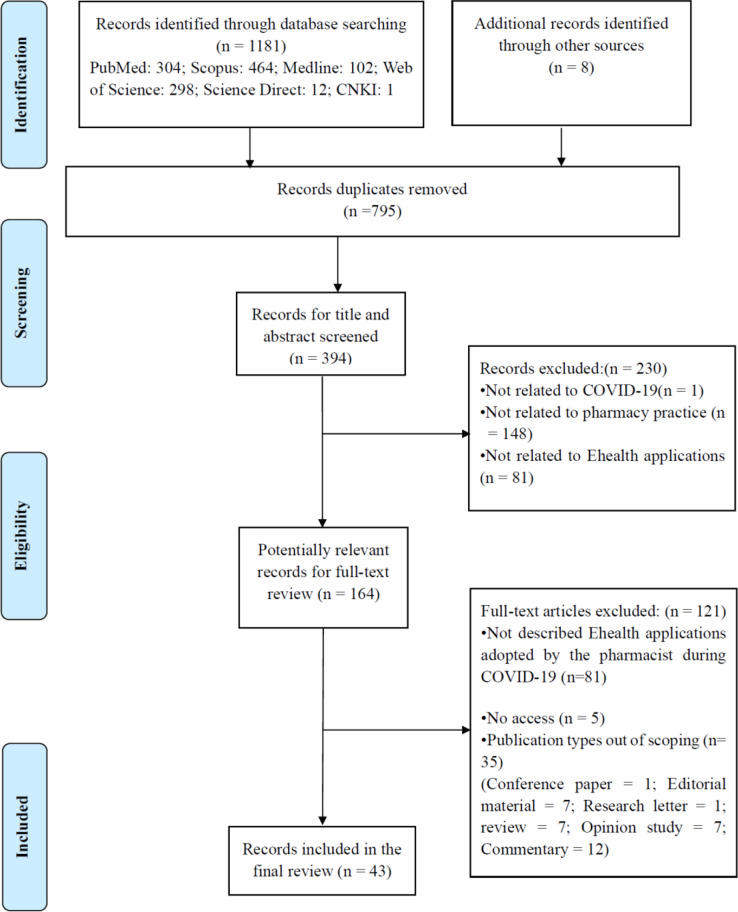
As shown in figure 1, 1,189 articles were retrieved initially. After removing duplicates (n=795), and screening by the title and abstract (n=230) and full text (n=121), 43 articles were included in this review.20–62 Among the included studies were 25 observational studies (including 13 cross-sectional studies,36–39 43–48 54 59 60 5 case series,34 35 49–51 5 retrospective study,40 41 52 53 55 1 prospective study61 and 1 interview study42 and 18 descriptive studies.20–33 56–58 62 The general characteristics of the included studies are summarised in online supplemental table 1. The majority of the studies reported about the use of eHealth by hospital pharmacists,20 21 23 25 29–31 33–35 37–41 43 46–49 52–55 58 59 61 followed by community pharmacists.28 35 45 46 50 51 54 60 62 Patients with chronic diseases27 31 32 34 37 39 40 43 44 48 52 54 57 60–62 were the primary targets populations of PC-eHealth interventions, followed by patients with COVID-1926 34 42 46 49–51 58 and patients with cancer.27 31 37 40
Figure 1.
PRISMA flow chart of literature search and selection of publications. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
bmjopen-2022-066246supp001.pdf (86.3KB, pdf)
Purposes of adopting eHealth in PC during the COVID-19 pandemic
The purpose of adopting eHealth, the eHealth tools used, the interventions provided by pharmacists with eHealth and the intervention output are illustrated in online supplemental table 2. Considering the lack of official definition or categorisation framework of eHealth applied to PC, the purposes of adopting eHealth in this study were informed by the current literature8 63–65 and thus categorised into: (1) tele-education (educating patients about how to take medicines and adverse drug effects, n=17)20 22 24 25 29 31–33 37–39 42 47 48 56 57 62; (2) tele-consultation (addressing patients’ enquiries about drug-related problems, n=28)20 21 23 25–28 30–33 35–38 44 45 49–51 53 56–62; (3) tele-monitoring (monitor the patients’ use of medications in real time, n=27)20 21 23 25–27 29–33 35 36 38 39 41 44–46 48–51 53–55 57; (4) tele-case-management (continuously manage the patient’s medication regimen according to the patient’s conditions, n=30)22 23 26 27 29 30 32–34 37–42 44 46 48–54 56–61 and (5) tele-mentoring (the use of eHealth by other healthcare workers to seek advice from pharmacists, n=19).21 25 28 30 31 33 34 38–40 42–44 47 48 53 57 59 62 It is noteworthy that all but five studies22 24 46 52 56 reported the use of eHealth for multiple purposes.
bmjopen-2022-066246supp002.pdf (129.7KB, pdf)
Interventions provided by pharmacists with eHealth
The services provided at the interface of PC-eHealth were multifaceted and could be categorised into one of nine interventions, as shown in table 1. Apart from the core components of PC such as (1) consultation, (2) medication order evaluation and dispensing, (3) patient monitoring for adverse drug events, (4) comprehensive follow-up and continuous assessment, (5) medication review and management, and (6) medication education, pharmacists had reportedly extended their services towards caring for patients’ mental well-being (intervention 7), facilitating collaboration with the healthcare team with information sharing (intervention 8) and public health measures (intervention 9) during the pandemic. In comparison, community pharmacists were more inclined to use eHealth in providing emotional support to their patients and the public to ease their anxiety about the pandemic development, while hospital pharmacists used eHealth to carry out various PC interventions.
Table 1.
Interventions provided by pharmacists at the interface of PC-eHealth during the COVID-19 pandemic
| Interventions | Description |
| Core components of PC | |
| (1) Consultation | Address patients’ enquires related to medications as well as the COVID-19 pandemic20 21 25–30 33 35–38 43–45 48 50 51 55–60 62 |
| (2) Medication order evaluation and dispensing | Evaluate, process and dispense electronic prescriptions22 25 26 30 32 33 37 40–42 49–51 53 57 59 62 |
| (3) Patient monitoring for adverse drug events | Monitor the drug reaction of patient after taking the medication20 23 26 29 36 40 46 48 55 57 62 |
| (4) Comprehensive follow-up and continuous assessment | Conduct follow-up physical and psychological assessments of the patients20 26 27 29 36 39 41 52 53 55 60 61 |
| (5) Medication review and management | Conduct individualised review and management of medications for patients with20 27–30 32 34 35 37 39 41 42 47–51 53 54 57 61 62 |
| (6) Medication education | Offer instructions about the administration of medications20 28 30 34 35 37 39 40 43–45 48 49 54 57 58 62 |
| Extended components of PC during the COVID-19 pandemic | |
| (7) Emotional support | Provide support to patients to alleviate their concerns about their diseases23 35 48 62 |
| (8) COVID-19 information sharing | Sharing of information about the patients or their medications with other members of the healthcare team22 24 27 31 35 37 39 42 45 47 48 53 58 60 |
| (9) Infectious disease surveillance | Detect any signs of possible infection with COVID-19 among patients while delivering pharmacy services remotely25 60 |
PC, pharmaceutical care.
Tool(s) involved in the PC-eHealth service models
Phone calls alone in the form of a hotline or as a combination with videoconference, social media and television, mobile applications, websites and/or wearable devices were mostly employed to enable PC-eHealth service mode in the included studies.20 23 25 27 32 35 36 39–43 45 49 50 55–57 59–62
Videoconference was often used to allow face-to-face interactions and observations of body language and facial expressions between the pharmacists and the patients.23 25 29 31–35 39 40 42 45–47 50 51 57 59 Social media (eg, Twitter)24 and Facebook,34 online networking services (eg, Doximity),33 41 53 mobile applications (eg, WeChat),26 38 44 58 Skype,29 Facetime,29 PetalMD,34 Cisco Jabber 12.6,33 Google voice,41 53 WhatsApp,49 61 short messages services,49 59 Signal53 and others,35 46 48 56 and wearable devices25 had also been integrated into the PC-eHealth service models. Other communication means such as television,24 email,30 34 41 fax30 and radio48 58 were also employed.
Some studies reported about the website monitoring applications developed by hospitals or pharmacies in response to the societal and patient needs during the pandemic. Examples were the SPHCC Patient Care (an online platform formed by six licensed internet hospitals allowing pharmacists continue to care for patients with COVID-19 online),26 the CCSS (a website monitoring application formed by a primary healthcare centre network for assuring medication supply),28 the Cloud SYSUCC (a website monitoring application developed by a university cancer centre to enable pharmacists continuously manage cancer patients),37 the VigiLanz (a clinical surveillance platform supported pharmacists to readily communicate with other healthcare providers and participate in daily patient care routine),25 the Virtual–Venipuncture INR (an IT support that allowed pharmacists monitor the INR of patients receiving anticoagulants during the pandemic)52 and several others.30 35 36 44 50 58 61 A number of PC-eHealth service models was also pertained with an integration of the electronic medical record (EMR) system.21 22 30 31 37 42 47 57
Other input relevant to establishing PC-eHealth service model
To aid in the establishment and development of PC using eHealth throughout the epidemic, key input at the levels of government, hospital and pharmacies, pharmacist professional organisations and pharmacists has been identified.
At the government level, legislation that defines the services of PC-eHealth and the liability for such services, safeguards data protection and promotes database interoperability was commonly discussed in the included studies.31 50 57 59 61 Initiatives to upgrade remote information technology and outpatient clinic systems might be launched by the government.33 35 Continuous supervision and evaluation of PC-eHealth interventions by the government had been suggested,28 57 which might require a special department or taskforce to lead and faciliate the adoption and implementation of eHealth in PC and other healthcare services alike.50 61 It was also important for the government to provide reliable and up-to-date information about the COVID-19 pandemic to be disseminated via the PC-eHealth platform.50
For the hospitals or pharmacies, efficient and appropriate communication mechanisms were considered the utmost important to control the spread of the pandemic, which was why many of them had established networks across different healthcare settings and developed their own eHealth applications.26 37 55 Hospitals and pharmacies not only developed new eHealth systems on their own, but also promoted the use of the systems to other hospitals or pharmacies through training, empowering their interconnections to optimise their patient coverage.22 54 Staff had been asked to sign codes of conduct to protect patient confidentialiaty.33
Pharmacist professional organisations were expected to define PC-eHealth services,41 47 offer advice to pharmacists about making eHealth plans and provide guidelines for PC-eHealth service provision,25 43 52 53 62 and support pharmacists with funding47 and human resources44 to establish the PC-eHealth infrastructure. At the pharmacist level, communication and collaboration among pharmacists from different sectors to care for complicated patients,20 29 34 self-motivation to learn about the PC-eHealth guidelines,25 training and supervision by more experienced pharmacists,29 38 60 participation in the eHealth multidisciplinary working group43 and closer collaboration with other healthcare providers and other key stakeholders51 were considered important factors.
Output of PC-eHealth interventions
The impact of adoption eHealth in PC during the pandemic was mainly in reducing the need for physical contact or visits to the hospital/clinic for minimising the risks of infection and transmission20 21 25 26 28 30 32 33 38 43 45 48 52–54 58 60 62 as well as allowing the continuous monitoring of the patients in the absence of in-person interactions.21 23 26 27 29–31 39–43 45–47 49 51 56 57 Some studies reported an improvement in the efficiency of PC due to the use of eHealth25 34 38 44 50 57 58 61 and patient satisfaction about the PC-eHealth services they received was also reported.28 29 32 36 37 44 46 54 59 Other benefits of adopting eHealth in PC during the pandemic included the dissemination of reliable information,24 reduced abuse of over-the-counter medicines,35 facilitating transition of care between hospitals22 and communications within the healthcare team and with patients and caregivers.25 However, there was one study that reported a negative impact on the quality of PC after eHealth was integrated.55
Contextual factors affecting the adoption of eHealth in PC during the pandemic
Contextual factors affecting the adoption of eHealth in PC during the COVID-19 pandemic had been described in terms of challenges and enablers in the included studies. Challenges might arise at the levels of pharmacists, government, patients and eHealth tool suppliers. For pharmacists, the shift from face-to-face towards eHealth service model resulting in long working hours had inevitably created conflicts between personal and professional lives.34 Other issues such as unfamiliarity with the eHealth systems,22 27 limitations of assessments due to a lack of in-person interactions32 35 62 or eye contact,31 difficulty in obtaining consent from the patients to receive PC-eHealth service,31 33 lack of control over the entire PC-eHealth process28 62 were also discussed. Some pharmacists just did not have the motivation to adopt eHealth.34 56
For government, evaluation of PC-eHealth services in order to inform a reasonable remuneration system41 47 56 and development of a robust legal framework, policies and procedures to guide the use of eHealth in PC lagged behind.47 56 From the perspectives of the healthcare institutes, whether it be hospital or community pharmacies, a lack of electronic patient records,50 51 a lack of funding to set up a teleworking envirnoment45 and a lack of communication infrastructure readily in place for timely scaling up during the pandemic34 were cited as the biggest challenges.
Patients’ digital health literacy30 31 31 45 48 56 57 and cultural acceptance31 36 37 might vary, and unfamiliarity with new PC-eHealth systems might collectively discourage them from taking up PC-eHealth services. Moreover, a lack of access to high-tech devices36 and a lack of willingness to accept eHealth services31 48 57 might also be a barrier to patients’ acceptance of PC-eHealth services. For some patients who had already receiving PC-eHealth interventions, a lack of adherence to the services could negatively impact on the outcome of eHealth service model.28
For the PC-eHealth tool suppliers, some of the biggest challenges experienced during the COVID-19 pandemic included the unstable network connectivity,21 49 inadequate interoperability of systems provided by different providers,21 a lack of standardised platform and technical support within and across the care settings,33 errors in digital systems,43 cybersecurity considerations27 42 and the lack of complete patient data for sharing.22
To support the adoption of eHealth in PC for better management of patients during the pandemic, several enablers had been suggested. These included new forms of supervision to regulate and standardise pharmacists’ interventions provided through PC-eHealth model,33 34 37 strategies for appropriate resource assessment and allocation, workflow modification and infrastructure maintenance,23 44 55 56 follow-up evaluation of the performance and reliability of the pharmacists,34 continuous and stable IT support,22 58 and research to develop the evidence about the effectiveness and societal implications of PC-eHealth during pandemic.46 54
Discussion
Significant use of eHealth in PC during the COVID-19 pandemic
This review revealed that it was common for pharmacists to adopt eHealth to ensure the continuity of PC amid the threat of COVID-19 pandemic and the challenges pertained with public health measures. This is in alignment with the overall development trend in PC for different care settings.8 During the pandemic, the most commonly reported purposes of using eHealth in PC were tele-case-management, tele-consultation and tele-monitoring, often with the use of phone calls in combination with videoconference, social media and television, mobile applications, websites and/or wearable devices. Specific to the needs during the pandemic, PC-eHealth was often employed to provide emotional support and to dissimilate pandemic-related information. The benefits of adopting eHealth, as reported in previous public health incidents,66 were widely recognised and mostly observed in terms of reduced need for physical contact, continuity of care and improved PC efficiency. However, due to the lack of face-to-face interactions, pharmacists may not be able to accurately evaluate the complete situation of patients, especially to those who were not very proficient in using information technology. As such, the effectiveness of the pharmacy service provided via eHealth might be affected.
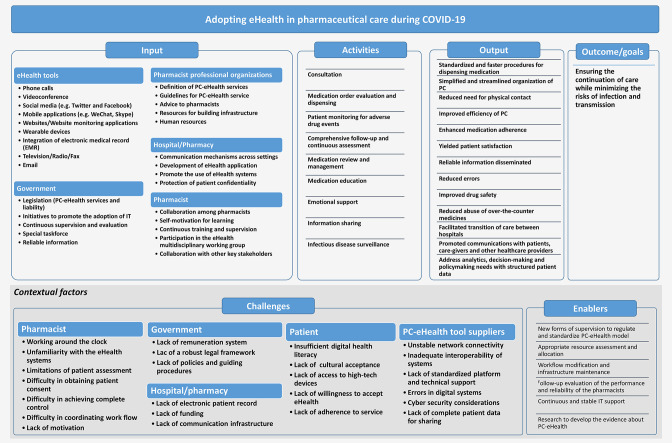
The logic model to guide the planning of eHealth adoption in PC
Integrating eHealth into PC was suggested as early as 20 years ago.67 Since then, many studies had been carried out to investigate different PC-eHealth practice models designed for different patient groups.68–71 However, up to date, the integration of eHealth into PC has not been generalised nor standardised, and a systematic approach to advancing the quality and coverage of PC with eHealth is still lacking. The COVID-19 pandemic has disturbed the traditional mode of healthcare delivery which has expectedly accelerated the uptake and scaling-up of eHealth.72 However, as far as PC is concerned, the attempts made so far are rather extemporaneous as evident by the vast variety of tools, purposes of care and interventions identified in this study.
In order to systematically and graphically present the blueprint of ‘know-how’, a logic model of establishing PC-eHealth during a pandemic has been built based on the study findings, detailing the goals to be achieved, the input and activities taken place, the output produced and the contextual factors involved (figure 2). This may serve as a framework for guiding and reinforcing the adoption of eHealth in PC to meet the challenges of COVID-19 pandemic or other public health incident alike.
Figure 2.
The logic model of adopting eHealth in pharmaceutical care during the COVID-19 pandemic. PC, pharmaceutical care.
The effectiveness of adopting eHealth in PC
Numerous studies have demonstrated the value of eHealth in healthcare services including PC. The effectiveness of eHealth adoption can be reflected in two aspects. On the one hand, the increase in the number of users receiving PC via eHealth. For example, Reardon et al showed that 1.5% of 2036 initial patient appointments were conducted virtually via eHealth prior to the pandemic. This increased to 64% for follow-up appointments in 2019, indicating that an increasing number of patients rely on the PC delivered via eHealth.34 Ibrahim et al also reported that the proportions of COVID-19 cases (either probable and confirmed) who received pharmaceutical services were 31.90% vs 11.74% and 6.07% versus 0.36%, respectively, in pharmacies with remote services (test group) versus pharmacies without remote services (control group).50
On the other hand, the effectiveness of eHealth adoption may also be assessed by comparing pharmacy services in hospitals and community pharmacies with and without eHealth. When providing pharmacy services through eHealth during the epidemic, patients can use relevant eHealth tools to book pharmacist services in advance, and can receive online pharmacy services at any location. Standard and faster dispensing procedures can be realised with the help of advanced technology, which may largely simplify the entire process of PC provision for patients to achieve higher efficiency of the entire pharmacy service process.16 39
With eHealth, electronic transaction and storage of patient information could help pharmacists to prevent mistakes in dispensing which would have happened with paper-based procedures, to help improve medication adherence, and to support analysis and decision making about medication availability with easily accessible and structured data. Using community pharmacies as an example, the rate of potential OTC abuse across pharmacies with and without eHealth services was 5.8% vs 7.7% and potential OTC misuse across pharmacies with and without eHealth services was 13.7% vs 16.6%.39
The significance of eHealth to PC in the healthcare system
The accessibility to pharmacies and the perceived affordability positions pharmacists at the first line of contact within the healthcare system especially during a pandemic.73 The emphasis placed on patient-centre service has further driven the new paradigm of pharmacy practice and accelerated the adoption of eHealth for the expansion of pharmacists’ professional role in pharmaceutical services. This implies a shift of focus towards the delivery of longitudinal value-added services for the patients as well as the closer collaboration with other healthcare professionals with higher level of data sharing. Besides, the use of ‘smart’ technological solutions in the medicine dispensing process could relieve pharmacists' workload, leaving more free time for pharmacists to assume other components of pharmacy practice, allowing the accomplishment of more professional and advanced PC services.74 Such transition, when properly executed, is considered extremely valuable for the patients, other healthcare professionals and even the health systems in terms of not only improvement in health services quality and in patient health related outcomes, but also greater efficiency and economic savings.75–77
The heterogeneity of eHealth tools used in PC
The heterogeneity of eHealth tools employed in the PC-eHealth during the COVID-19 pandemic are associated with both benefits and concerns for both the patients and the pharmacists. Prior to the pandemic, the utilisation of telemedicine was mainly to allow pharmacists to extend the reach of their interventions in chronic disease management and telephone was the most common communication method.8 With the additional use of videoconference, mobile applications, website application, social media and wearable devices as reported in this study, real-time interactions and data collection is now possible to achieve more personalised PC support.78 Nevertheless, the capacity to operate different eHealth tools could be challenging to some patients.79 and the hybrid mode of service provision would easily overwhelm a lot of pharmacists.80
Furthermore, the vast amount of personalised data generated from multiple sources and shared dynamically entails a new level of concerns over privacy and cybersecurity.81 In the absence of a legal or regulatory framework, the practice of PC via different eHealth tools might lead to ethical and legal issues and subject pharmacists to liability consequences should any adverse events happen to the patients.82 A lack of standardised design of PC-eHealth pose great challenges to scaling up and interoperability, preventing a timely and thorough transformation of service mode whenever needed.83 This is especially relevant during a pandemic when immediate actions are called for and healthcare resource allocation is particularly uncertain. To this end, it would be the priority of action for the regulatory bodies and pharmacist professional organisations to provide clear guidance on how to appropriately adopt eHealth in PC.
Adopting eHealth in PC in the context of the health system
In order to better develop and promote the measures to provide pharmacy services through eHealth during the epidemic, the government can try to take the lead in incorporating eHealth to support the role of pharmacists in public health measures. One of the essential criteria was for pharmacists and patients to acquire the necessary skills and to come to term the benefits of adopting eHealth. According to the technology acceptance model, an information systems theory that describes the acceptance and usage of a new technology from the users’ perspective, there are two major factors affecting users’ decision about when and how to use it: perceived usefulness and perceived ease-of-use.84 In other words, if a person believes that using a particular new technology would enhance the performance of some sort, and the new technology is easy to use, he/she will have the positive attitude and intention to use the new technology. As such, training and evidence-based use of eHealth in improving PC for pharmacists and public education about basic skills of information technology and benefits of eHealth are important for achieving high proficiency and wide acceptance of eHealth in PC.
In addition, resources are needed to ‘upgrade’ the healthcare system infrastructure to integrate eHealth into day-to-day practice. Equipment, internet access, information technology systems and process, sustainable engagement and initiative, competent staff and a well-designed, close-loop evaluation mechanism should be in place to form the basic infrastructure for eHealth in PC.85 A lack of an appropriate infrastructure might affect the quality of PC leading to more harm than benefits to the patients.86 In the context of a business operation such as community pharmacies, cost is one other key factors when adopting eHealth. The investment to achieve the readiness of the infrastructure can be expensive considering the costs of both hardware and software. While the focus on leveraging the advantage of any existing ICT infrastructure should be prioritised, it is also necessary to monitor and manage the costs over time.87
Moving forward
For the efficiency use of healthcare resources particularly in the context of a pandemic, eHealth adoption and implementation in PC requires adequate planning and continuous evaluation of cost-effectiveness.88 A more balanced research approach to investigate the pros and cons when adopting eHealth in PC is also warranted to better inform actions that support wider use of eHealth in PC as well as other areas of healthcare services. Indeed, any eHealth interventions in PC should be viewed a catalyst for change in the overall healthcare sector and should be adequately planned, piloted and progressively scaled up to ensure the expected deliverables. Other preparation should be carried out simultaneously. As eHealth continues to transform PC, strategies to help patients and pharmacists enhance digital literacy and build the knowledge of technology should take place to improve engagement and receptivity towards technological integration.89
For the PC-eHealth currently in operation, more efforts should be made to quantify the clinical and economic benefits for the patients or the public, and the long-term outcomes.75 76 In order to secure resources to support PC-eHealth, a fine balance needs to be established between evidence-based integration of e-Health and constructive experimentation of PC.90 Synthesising the evidence is important for informing the future directions and implications for policy and practice.
Limitations of this review
It is possible that our search strategy did not capture all examples of PC-eHealth experiences during the pandemic if they were embedded as part of an inter-professional programme, depending on how pharmacists were referenced in the text of available publications. The logic model developed in this study provided an overall landscape of all the factors relevant to the adoption of eHealth in PC during the pandemic but was not able to establish any causal chains among the components. Future research is warranted to confirm the interretionship among each factor in order to better future planning, monitoring and evaluation.
Conclusion
This study revealed the wide adoption of eHealth in PC during the pandemic and the emerging evidence for its importance. As the momentum of adopting eHealth in PC yielded during the COVID-19 pandemic will continue to drive further innovative development, an orchestrated, transdisciplinary approach adapted to different local contexts is needed to achieve the benefits of PC-eHealth. Future research should be directed to substantiate the assessment of eHealth in reshaping the mode of pharmacy service in terms of not only the continuity, but also the quality and efficiency of care amid the challenges of any pandemic.
Supplementary Material
Footnotes
Twitter: @acavaco
Correction notice: This article has been corrected since it first published. Author name 'Afonso Cavaco' has been updated.
Contributors: ZFC: conceptualisation, methodology, validation, investigation, writing—original draft. PKT: validation, writing—review and editing. HH: conceptualisation, methodology, review and editing. AC: review and editing. LZ: review and Editing. SLL: review and editing. COLU: conceptualisation, methodology, validation, writing—review and editing, supervision, project administration, the guarantor.
Funding: This research was financed by the University of Macau (SRG2021-00007-ICMS), and did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Berenguer B, La Casa C, de la Matta MJ, et al. Pharmaceutical care: past, present and future. Curr Pharm Des 2004;10:3931–46. 10.2174/1381612043382521 [DOI] [PubMed] [Google Scholar]
- 2.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:533–43. 10.1093/ajhp/47.3.533 [DOI] [PubMed] [Google Scholar]
- 3.Pande S, Hiller JE, Nkansah N, et al. The effect of pharmacist-provided non-dispensing services on patient outcomes, health service utilisation and costs in low- and middle-income countries. Cochrane Database Syst Rev 2013:Cd010398. 10.1002/14651858.CD010398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilke D, Schiek S, Bertsche T, et al. Verwendung von Routinedaten Der gesetzlichen Krankenkasse in einer Pilotstudie Zur evaluation pharmazeutischer Interventionen Im Krankenhaus. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen 2017;121:21–8. 10.1016/j.zefq.2017.03.004 [DOI] [PubMed] [Google Scholar]
- 5.Ghibu S, Juncan AM, Rus LL. The Particularities of pharmaceutical care in improving public health service during the COVID-19 pandemic. Int J Environ Res Public Health 2021:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . Telemedicine – opportunities and developments in member states. Report on the second global survey on eHealth 2010;2. [Google Scholar]
- 7.World Health Organization . 58th World health assembly. Geneva, Switzerland: World Health Organization, 2005. [Google Scholar]
- 8.Niznik JD, He H, Kane-Gill SL. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: a systematic review. Res Social Adm Pharm 2018;14:707–17. 10.1016/j.sapharm.2017.10.011 [DOI] [PubMed] [Google Scholar]
- 9.Littauer SL, Dixon DL, Mishra VK, et al. Pharmacists providing care in the outpatient setting through telemedicine models: a narrative review. Pharm Pract 2017;15:1134. 10.18549/PharmPract.2017.04.1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nkansah N, Mostovetsky O, Yu C, et al. Effect of outpatient pharmacists' non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev 2010:Cd000336. 10.1002/14651858.CD000336.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.George PP, Molina JAD, Cheah J, et al. The evolving role of the community pharmacist in chronic disease management - a literature review. Ann Acad Med Singap 2010;39:861–7. [PubMed] [Google Scholar]
- 12.Spanakis M, Sfakianakis S, Kallergis G, et al. PharmActa: personalized pharmaceutical care eHealth platform for patients and pharmacists. J Biomed Inform 2019;100:103336. 10.1016/j.jbi.2019.103336 [DOI] [PubMed] [Google Scholar]
- 13.Jeminiwa R, Hohmann L, Qian J, et al. Impact of eHealth on medication adherence among patients with asthma: a systematic review and meta-analysis. Respir Med 2019;149:59–68. 10.1016/j.rmed.2019.02.011 [DOI] [PubMed] [Google Scholar]
- 14.Kilova K, Mihaylova A, Peikova L. Opportunities of information communication technologies for providing pharmaceutical care in the COVID-19 pandemic. Pharmacia 2021;68:9–14. 10.3897/pharmacia.68.e56987 [DOI] [Google Scholar]
- 15.Kow CS, Hasan SS. Pharmacist-patient communication amid COVID-19 pandemic: a review of available options and potential impact. British Journal of Pharmacy 2021;6. 10.5920/bjpharm.836 [DOI] [Google Scholar]
- 16.Iftinan GN, Wathoni N, Lestari K. Telepharmacy: a potential alternative approach for diabetic patients during the COVID-19 pandemic. J Multidiscip Healthc 2021;14:2261-2273. 10.2147/JMDH.S325645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fandino W. Formulating a good research question: pearls and pitfalls. Indian J Anaesth 2019;63:611–6. 10.4103/ija.IJA_198_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moltó-Puigmartí C, Vonk R, van Ommeren G, et al. A logic model for pharmaceutical care. J Health Serv Res Policy 2018;23:148–57. 10.1177/1355819618768343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdallah I, Eltahir A, Fernyhough L, et al. The experience of Hamad General Hospital collaborative anticoagulation clinic in Qatar during the COVID-19 pandemic. J Thromb Thrombolysis 2021;52:1–7. 10.1007/s11239-020-02276-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allison A, Shahan J, Goodner J, et al. Providing essential clinical pharmacy services during a pandemic: virtual video rounding and precepting. Am J Health Syst Pharm 2021;78:1556–8. 10.1093/ajhp/zxab208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cashman H, Mayson E, Kliman D. An integrated electronic health record facilitates a safer and more efficient rural outreach haematology service. Internal Medicine Journal 2020. [DOI] [PubMed] [Google Scholar]
- 23.Do T, Luon S, Boothe K. Advancing ambulatory pharmacy practice through a crisis: Objectives and strategies used in an ambulatory care action team’s response to the COVID-19 pandemic. Am J Health Syst Pharm 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goff DA, Ashiru-Oredope D, Cairns KA, et al. Global contributions of pharmacists during the COVID-19 pandemic. J Am Coll Clin Pharm 2020;3:1480–92. 10.1002/jac5.1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kjerengtroen S, Wilde SM, Fontaine GV, et al. COVID-19 preparedness: clinical pharmacy services remote staffing in a quaternary, level I trauma and comprehensive stroke center. Am J Health Syst Pharm 2020;77:1250–6. 10.1093/ajhp/zxaa132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liao Y, Ma C, Lau AH, et al. Role of pharmacists during the COVID-19 pandemic in China-Shanghai experiences. J Am Coll Clin Pharm 2020;3:997–1002. 10.1002/jac5.1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marchese M, Heintzman A, Pasetka M, et al. Development of a process map for the delivery of virtual clinical pharmacy services at Odette cancer centre during the COVID-19 pandemic. J Oncol Pharm Pract 2021;27:650–7. 10.1177/1078155221991202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Margusino-Framiñán L, Illarro-Uranga A, Lorenzo-Lorenzo K. Pharmaceutical care to hospital outpatients during the COVID-19 pandemic. Telepharmacy, Farm Hosp 2020;44:61–5. [DOI] [PubMed] [Google Scholar]
- 29.Mohammad I, Berlie HD, Lipari M, et al. Ambulatory care practice in the COVID-19 era: redesigning clinical services and experiential learning. J Am Coll Clin Pharm 2020;3:1129–37. 10.1002/jac5.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reardon J, Yuen J, Lim T, et al. Provision of virtual outpatient care during the COVID-19 pandemic and beyond: enabling factors and experiences from the Ubc pharmacists clinic. Innov Pharm 2020;11. doi: 10.24926/iip.v11i4.3432. [Epub ahead of print: 28 10 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Segal EM, Alwan L, Pitney C, et al. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am J Health Syst Pharm 2020;77:1403–8. 10.1093/ajhp/zxaa184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warda N, Rotolo SM. Virtual medication tours with a pharmacist as part of a cystic fibrosis telehealth visit. J Am Pharm Assoc 2021;61:e119–25. 10.1016/j.japh.2021.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yerram P, Thackray J, Modelevsky LR, et al. Outpatient clinical pharmacy practice in the face of COVID-19 at a cancer center in New York City. J Oncol Pharm Pract 2021;27:389–94. 10.1177/1078155220987625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adam J-P, Khazaka M, Charikhi F, et al. Management of human resources of a pharmacy department during the COVID-19 pandemic: Take-aways from the first wave. Res Social Adm Pharm 2021;17:1990–6. 10.1016/j.sapharm.2020.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al Mazrouei N, Ibrahim RM, Al Meslamani AZ, et al. Virtual pharmacist interventions on abuse of over-the-counter medications during COVID-19 versus traditional pharmacist interventions. J Am Pharm Assoc 2021;61:331–9. 10.1016/j.japh.2021.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alhmoud EN, Abd El Samad OB, Elewa H, et al. Drive-up Inr testing and phone-based consultations service during COVID-19 pandemic in a pharmacist-lead anticoagulation clinic in Qatar: monitoring, clinical, resource utilization, and patient- oriented outcomes. J Am Coll Clin Pharm. In Press 2021;4:1117–25. 10.1002/jac5.1469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen Z-J, Liang W-T, Liu Q, et al. Use of a remote oncology pharmacy service platform for patients with cancer during the COVID-19 pandemic: implementation and user acceptance evaluation. J Med Internet Res 2021;23:e24619. 10.2196/24619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li H, Zheng S, Liu F, et al. Fighting against COVID-19: innovative strategies for clinical pharmacists. Res Social Adm Pharm 2021;17:1813–8. 10.1016/j.sapharm.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livet M, Levitt JM, Lee A, et al. The pharmacist as a public health resource: expanding telepharmacy services to address social determinants of health during the COVID-19 pandemic. Explor Res Clin Soc Pharm 2021;2:100032. 10.1016/j.rcsop.2021.100032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown S-A, Patel S, Rayan D, et al. A virtual-hybrid approach to launching a cardio-oncology clinic during a pandemic. Cardiooncology 2021;7:2. 10.1186/s40959-020-00088-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park L, Kim JH, Waldman G, et al. Impact analysis of virtual ambulatory transplant pharmacists during COVID-19. J Am Coll Clin Pharm 2021;4:978–87. 10.1002/jac5.1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Falconer N, Monaghan C, Snoswell CL. The pharmacist informatician: providing an innovative model of care during the COVID-19 crisis. Int J Pharm Pract 2021;29:152–6. 10.1093/ijpp/riaa017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gona OJ, Madhan R, Shambu SK. Assessment of clinical pharmacists' assistance for patients with established cardiovascular diseases during the COVID-19 pandemic: insights from southern India. Front Cardiovasc Med 2020;7:599807. 10.3389/fcvm.2020.599807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li H, Zheng S, Li D, et al. The establishment and practice of pharmacy care service based on Internet social media: telemedicine in response to the COVID-19 pandemic. Front Pharmacol 2021;12:707442. 10.3389/fphar.2021.707442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koster ES, Philbert D, Bouvy ML. Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Res Social Adm Pharm 2021;17:2002–4. 10.1016/j.sapharm.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Muflih SM, Al-Azzam S, Abuhammad S, et al. Pharmacists' experience, competence and perception of telepharmacy technology in response to COVID-19. Int J Clin Pract 2021;75:e14209. 10.1111/ijcp.14209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tortajada-Goitia B, Morillo-Verdugo R, Margusino-Framiñán L, et al. Survey on the situation of telepharmacy as applied to the outpatient care in hospital pharmacy departments in Spain during the COVID-19 pandemic. Farm Hosp 2020;44:135–40. 10.7399/fh.11527 [DOI] [PubMed] [Google Scholar]
- 48.Wang D, Liu Y, Zeng F, et al. Evaluation of the role and usefulness of clinical pharmacists at the Fangcang Hospital during COVID-19 outbreak. Int J Clin Pract 2021;75:e14271. 10.1111/ijcp.14271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al Meslamani AZ, Kassem AB, El-Bassiouny NA, et al. An emergency plan for management of COVID-19 patients in rural areas. Int J Clin Pract 2021;75:e14563. 10.1111/ijcp.14563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ibrahim OM, Ibrahim RM, Z Al Meslamani A, et al. Role of telepharmacy in pharmacist counselling to coronavirus disease 2019 patients and medication dispensing errors. J Telemed Telecare 2020;71:1357633X2096434. 10.1177/1357633X20964347 [DOI] [PubMed] [Google Scholar]
- 51.Mohamed Ibrahim O, Ibrahim RM, Abdel-Qader DH, et al. Evaluation of Telepharmacy services in light of COVID-19. Telemed J E Health 2021;27:649–56. 10.1089/tmj.2020.0283 [DOI] [PubMed] [Google Scholar]
- 52.Cope R, Fischetti B, Eladghm N. Outpatient management of chronic warfarin therapy at a pharmacist-run anticoagulation clinic during the COVID-19 pandemic. J Thromb Thrombolysis 2021:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sorbera M, Fischetti B, Khaimova R, et al. Evaluation of virologic suppression rates during the COVID-19 pandemic with outpatient interdisciplinary HIV care. J Am Coll Clin Pharm 2021;4:964–8. 10.1002/jac5.1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peláez Bejarano A, Villar Santos P, Robustillo-Cortés MdeLA, et al. Implementation of a novel home delivery service during pandemic. Eur J Hosp Pharm 2021;28:e120–3. 10.1136/ejhpharm-2020-002500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McNamara A, Zhao M, Lee S-Y. Evaluating the primary care clinical pharmacist visit transition to telehealth during the COVID-19 pandemic by comparing medication related problems from telehealth visits and in-person visits. J Am Coll Clin Pharm 2021;4:914–23. 10.1002/jac5.1487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alhraiwil NJ, Al-Aqeel S, AlFaleh AF, et al. Impact of COVID-19 on the 937 telephone medical consultation service in Saudi Arabia. Int J Telemed Appl 2022;2022:1–6. 10.1155/2022/4181322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mohiuddin SI, Thorakkattil SA, Abushoumi F, et al. Implementation of pharmacist-led tele medication management clinic in ambulatory care settings: a patient-centered care model in COVID-19 era. Explor Res Clin Soc Pharm 2021;4:100083. 10.1016/j.rcsop.2021.100083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li Z, Gan L, Zheng H, et al. Innovative strategies and efforts of clinical pharmacy services during and after COVID-19 epidemic: experience from Shanghai children's Hospital. Risk Manag Healthc Policy 2021;14:4759–64. 10.2147/RMHP.S324937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grosman-Dziewiszek P, Wiatrak B, Jęśkowiak I. Patients' habits and the role of pharmacists and telemedicine as elements of a modern health care system during the COVID-19 pandemic. J Clin Med 2021:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Itani R, Khojah HMJ, Jaffal F, et al. Provision of pharmaceutical care to suspected high-risk COVID-19 patients through telehealth: a nationwide simulated patient study. BMC Health Serv Res 2021;21:997. 10.1186/s12913-021-07014-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Al Ammari M, AlThiab K, AlJohani M, et al. Tele-pharmacy anticoagulation clinic during COVID-19 pandemic: patient outcomes. Front Pharmacol 2021;12:652482. 10.3389/fphar.2021.652482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kovačević M, Ćulafić M, Vezmar Kovačević S, et al. Telepharmacy service experience during the COVID-19 pandemic in the Republic of Srpska, Bosnia and Herzegovina. Health Soc Care Community 2022;30:e1639-e1650. 10.1111/hsc.13590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee SWH, Chan CKY, Chua SS, et al. Comparative effectiveness of telemedicine strategies on type 2 diabetes management: a systematic review and network meta-analysis. Sci Rep 2017;7:12680. 10.1038/s41598-017-12987-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chongmelaxme B, Lee S, Dhippayom T, et al. The Effects of Telemedicine on Asthma Control and Patients’ Quality of Life in Adults: A Systematic Review and Meta-analysis. J Allergy Clin Immunol 2019;7:e111:199–216. 10.1016/j.jaip.2018.07.015 [DOI] [PubMed] [Google Scholar]
- 65.Shafiee Hanjani L, Caffery LJ, Freeman CR, et al. A scoping review of the use and impact of telehealth medication reviews. Res Social Adm Pharm 2020;16:1140–53. 10.1016/j.sapharm.2019.12.014 [DOI] [PubMed] [Google Scholar]
- 66.Ohannessian R. Telemedicine: potential applications in epidemic situations. European Research in Telemedicine / La Recherche Européenne en Télémédecine 2015;4:95–8. 10.1016/j.eurtel.2015.08.002 [DOI] [Google Scholar]
- 67.Bynum A, Hopkins D, Thomas A, et al. The effect of telepharmacy counseling on metered-dose inhaler technique among adolescents with asthma in rural Arkansas. Telemed J E Health 2001;7:207–17. 10.1089/153056201316970902 [DOI] [PubMed] [Google Scholar]
- 68.Witt DM, Humphries TL. A retrospective evaluation of the management of excessive anticoagulation in an established clinical pharmacy anticoagulation service compared to traditional care. J Thromb Thrombolysis 2003;15:113–8. 10.1023/B:THRO.0000003325.62542.43 [DOI] [PubMed] [Google Scholar]
- 69.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA 2008;299:2857–67. 10.1001/jama.299.24.2857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Salvo MC, Brooks AM. Glycemic control and preventive care measures of indigent diabetes patients within a pharmacist-managed insulin titration program vs standard care. Ann Pharmacother 2012;46:29–34. 10.1345/aph.1Q512 [DOI] [PubMed] [Google Scholar]
- 71.Kimber MB, Peterson GM. Telepharmacy-Enabling technology to provide quality pharmacy services in rural and remote communities. Journal of Pharmacy Practice and Research 2006;36:128–33. 10.1002/j.2055-2335.2006.tb00588.x [DOI] [Google Scholar]
- 72.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020;6:e18810. 10.2196/18810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ung COL. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019-nCoV outbreak. Res Social Adm Pharm 2020;16:583–6. 10.1016/j.sapharm.2020.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mooranian A, Emmerton L, Hattingh L. The introduction of the National e-health record into Australian community pharmacy practice: pharmacists' perceptions. Int J Pharm Pract 2013;21:405–12. 10.1111/ijpp.12034 [DOI] [PubMed] [Google Scholar]
- 75.Poudel A, Nissen LM. Telepharmacy: a pharmacist's perspective on the clinical benefits and challenges. Integr Pharm Res Pract 2016;5:75–82. 10.2147/IPRP.S101685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hyder MA, Razzak J. Telemedicine in the United States: an introduction for students and residents. J Med Internet Res 2020;22:e20839. 10.2196/20839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chisholm-Burns MA, Graff Zivin JS, Lee JK, et al. Economic effects of pharmacists on health outcomes in the United States: a systematic review. Am J Health Syst Pharm 2010;67:1624–34. 10.2146/ajhp100077 [DOI] [PubMed] [Google Scholar]
- 78.Alonso SG, de la Torre Díez I, Zapiraín BG. Predictive, personalized, preventive and participatory (4P) medicine applied to telemedicine and eHealth in the literature. J Med Syst 2019;43:1–10. 10.1007/s10916-019-1279-4 [DOI] [PubMed] [Google Scholar]
- 79.Negrini S, Donzelli S, Negrini A, et al. Feasibility and acceptability of telemedicine to substitute outpatient rehabilitation services in the COVID-19 emergency in Italy: an observational everyday clinical-life study. Arch Phys Med Rehabil 2020;101:2027–32. 10.1016/j.apmr.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Al‐Jazairi A, Hijazi H, Samarkandi H, et al. What is the ideal clinical pharmacy practice model? A satisfaction comparative study. J Am Coll Clin Pharm 2021;4:441–9. 10.1002/jac5.1396 [DOI] [Google Scholar]
- 81.Baretić M, Protrka N. Healthcare information technology: fast and accurate information access vs. Cyber-Security. Int J E-Serv Mob Appl 2021;13:77–87. [Google Scholar]
- 82.Solimini R, Busardò FP, Gibelli F, et al. Ethical and legal challenges of telemedicine in the era of the COVID-19 pandemic. Medicina 2021;57:1314. 10.3390/medicina57121314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hendy J, Reeves BC, Fulop N, et al. Challenges to implementing the National programme for information technology (NPfIT): a qualitative study. BMJ 2005;331:331–6. 10.1136/bmj.331.7512.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Holden RJ, Karsh B-T. The technology acceptance model: its past and its future in health care. J Biomed Inform 2010;43:159–72. 10.1016/j.jbi.2009.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Luxon L. Infrastructure - the key to healthcare improvement. Future Hosp J 2015;2:4–7. 10.7861/futurehosp.15.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Alotaibi YK, Federico F. The impact of health information technology on patient safety. Saudi Med J 2017;38:1173–80. 10.15537/smj.2017.12.20631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Myers MB. Telemedicine: an emerging health care technology. Health Care Manag 2003;22:219–23. [DOI] [PubMed] [Google Scholar]
- 88.Oberjé EJM, de Kinderen RJA, Evers SMAA, et al. Cost effectiveness of medication adherence-enhancing interventions: a systematic review of trial-based economic evaluations. Pharmacoeconomics 2013;31:1155–68. 10.1007/s40273-013-0108-8 [DOI] [PubMed] [Google Scholar]
- 89.Mohammadyari S, Singh H. Understanding the effect of e-learning on individual performance: the role of digital literacy. Comput Educ 2015;82:11–25. 10.1016/j.compedu.2014.10.025 [DOI] [Google Scholar]
- 90.Car J, Tan WS, Huang Z, et al. eHealth in the future of medications management: personalisation, monitoring and adherence. BMC Med 2017;15:1–9. 10.1186/s12916-017-0838-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-066246supp003.pdf (198KB, pdf)
bmjopen-2022-066246supp001.pdf (86.3KB, pdf)
bmjopen-2022-066246supp002.pdf (129.7KB, pdf)
Data Availability Statement
No data are available.