Abstract
Purpose
To evaluate protective factors that help individuals overcome adverse health outcomes associated with childhood trauma in an urban environment.
Methods
This retrospective cohort study included adults born between 1970 and 1995 who grew up in the former Cabrini-Green Homes, a low-income, Chicago public housing development. Participants completed surveys asking about general health, smoking, and mental health status. Surveys included questions related to neighborhood and family support, community safety, and childhood youth program participation. Simple regression models were performed to compare childhood exposure of adverse and protective factors to adult health outcomes. Multivariable logistic regression models were constructed to adjust for age, sex, and educational attainment.
Results
334 former residents completed the survey, and only those that reported an adversity score ≥ 2 were included in the analysis (n = 248). For those individuals who reported that their families cared for them as children, they described feeling hopeful about the future (OR 2.77, 95% CI, 1.28-6.00, aOR 2.63, 95% CI, 1.21–5.75) and reported decreased smoking rates as adults (OR 0.30, 95% CI, 0.14–0.66, aOR 0.35, 95% CI, 0.16–0.78). Better self-reported adult health status was associated with residents who believed the neighborhood looked out for one another (OR 2.31, 95% CI, 1.21–4.42, aOR 2.01, 95% CI, 1.02–3.95).
Conclusion
These findings suggest that a caring family and neighborhood connectedness are protective in mitigating childhood adversity. Devoting resources to strengthen families and communities is a promising strategy to promote healthier adult behaviors.
Keywords: Adverse childhood experiences; Childhood trauma; Resilience; Protective factors, neighborhood; Race
Introduction
Both positive and negative childhood experiences impact future life outcomes and opportunities. In the early 1990s, a landmark study performed by Kaiser Health Plan and the Centers for Diseases Control and Prevention (CDC) demonstrated a strong association between adverse childhood experiences (ACEs) and poor health outcomes in adulthood (Felitti, 1998). Future studies expanded upon this research to demonstrate that adversity in childhood is common, interrelated, and demonstrates a graded dose-response on negative health and well-being outcomes Dong et al., 2004; Felitti et al., 1998; Hughes et al., 2017; Merrick et al., 2019).
Data from the Behavioral Risk Factor Surveillance Survey (BRFSS), a national survey of demographics, behaviors, and health indicators, demonstrate that nearly half of children experience at least one adverse childhood experience and more than 10% of children report three or more (Sacks & Murphey, 2018). Further, these traumatic experiences disproportionately affect children of color, socioeconomically disadvantaged children, and those residing in unsafe neighborhoods (Merrick et al., 2018; Sacks & Murphey, 2018). Racial and ethnic minority youth are at increased risk for poor health compared to their White counterparts, even after adjusting for other social determinants such as socioeconomic status (Mehta et al., 2013). Nationally, one in three Black non-Hispanic children have experienced two to eight ACEs, compared to only one in five White non-Hispanic children (CDC, 2009). Black youth living in urban settings are particularly impacted by failing school systems, community violence, and the justice system (Mersky et al., 2013; Slopen et al., 2016).
While the prevalence of adverse childhood experiences is alarming, not all of these children grow up to develop poor health outcomes. Many researchers credit the development of resilience, the context-specific ability to respond to real or perceived stress while avoiding the negative health trajectories (Davydov et al., 2010; Luthar et al., 2000; Masten, 2014). Individual, family, and community factors all contribute to the development of resilience (Bethell et al., 2014; Lee et al., 2012). Specifically, safe, stable, and nurturing relationships have a protective and moderating effect on adverse experiences (Mercy & Saul, 2009; Schofield et al., 2013). The Search Institute developed a list of “40 Developmental Assets” and demonstrated associations between the number of assets and both positive and negative outcomes (Bleck & Debate, 2016). These include internal assets described as beliefs, values, and skills needed to engage with others and external assets, relationships, activities, and structures that create positive environments (Search Institute, 2007). As resilience research has developed so too has the idea that the resilience of an individual over the course of development is dynamic and depends on the function of complex adaptive systems that are continually interacting and transforming (Masten, 2014; Schoon, 2012).
Similar, to racial disparities in adverse childhood experiences, a 2019 study by Liu et al. found that White youth endorsed fewer adverse experiences and reported greater access to protective factors compared to their Black and Latinx counterparts. There remains a great need to identify the protective factors that help members of ethnically diverse communities overcome adversity. The goal of this study was to further elucidate protective factors in Black youth growing up in an urban environment. This knowledge will aid in the development of targeted programs and policy promoting positive childhood experiences.
Methods
Study Setting
This retrospective cohort study included adults born between 1970 and 1995 who grew up in or near the former Cabrini-Green (CG) Homes, a low-income, Chicago public housing development. Beginning in 1942 until 2011, Cabrini-Green Homes housed generations of low-income families until the last high rise was torn down as part of the Chicago Housing Authority’s Plan for Transformation (Austen, 2018). In 1990, Cabrini Green census data indicated that 95% of residents were Black and 75% of families lived below the federal poverty level (U.S. Census Bureau, 1990). Nearly 70% of adults did not have a high school or GED diploma. Cabrini Green youth were at high risk for intergenerational poverty and low educational attainment (Marciniak, 1986). Given these difficult social and economic conditions, the children living in the Cabrini Green neighborhood were at an increased risk of traumatic childhood experiences (Anda et al., 2010; Crouch et al., 2000; Giano et al., 2020; Walsh et al., 2019).
Study Sample and Design
Participants were recruited through Facebook groups, word of mouth, and prior involvement in a youth program. Subjects completed a phone or electronic survey, which included validated measures assessing childhood adversity and a variety of self-reported adult health measures from other previously validated questions. This survey was conducted as part of a larger study assessing the long-term effects of participation in the Cabrini-Green Youth Program. Participants were compensated $50 for completion of the survey. Data collection for both groups by trained research assistants occurred between October 2018 and April 2019. This project was deemed exempt by Ann & Robert H. Lurie Children’s Hospital of Chicago’s Institutional Review Board.
Measures
Demographic measures of race, age, sex, and educational attainment were assessed using questions from the Behavioral Risk Factor Surveillance System (BRFSS; Table 1). The BRFSS is the largest ongoing health survey in the world and has proved useful in defining the prevalence of health behaviors and other determinants of health in the United States.
Table 1.
Socio-Demographic Characteristics
| Measure | n = 248 | % |
|---|---|---|
| Adversity Score ≥ 2 | 248 | 100 |
| Race | ||
| Black | 248 | 100 |
| Current Age (years) | ||
| Mean (SD) | 36.3 (6.6) | |
| Sex | ||
| Female | 162 | 65.3 |
| Male | 86 | 34.7 |
| Educational Attainment | ||
| < Highschool/GED | 20 | 8.1 |
| Highschool/ GED | 72 | 29.0 |
| >Highschool/GED | 156 | 62.9 |
Childhood adversity was assessed with measures from the Philadelphia Urban Ace Survey, which expanded the ACE questions from the initial CDC-Kaiser study to better understand the impact of community-level adversities in urban areas (Cronholm et al., 2015). This modified ACE questionnaire was found to be useful and validated in assessing adversity in traditionally marginalized communities (Cronholm et al., 2015). A composite adversity score was calculated for each participant using a total of six questions (Table 2). Responses were dichotomized for analysis. Participants with ≥ 2 were considered to have a high adversity score as was used previously (Bethell et al., 2014). Only those individuals with ≥ 2 were included for analysis as the goal was to evaluate differences between individuals who reported high adversity scores.
Table 2.
Childhood Adversity Survey Questions
| Adversity Questions |
|---|
| 1. Did you feel safe in your neighborhood? |
| 2. How often, if ever, did you see or hear someone being beaten up, stabbed, or shot in real life? |
| 3. How often, if ever, did you see or hear a parent, step-parent, or another adult who was helping to raise you being yelled at, screamed at, sworn at, insulted, or humiliated? |
| 4. How often, if ever, did you see or hear a parent, step-parent, or another adult who was helping to raise you being hit or kicked hard that caused injury? |
| 5. During your first 18 years of life, how often did a parent, step-parent, or another adult living in your home hit you so hard that you had marks or were injured? |
| 6. During your first 18 years of life, how often did a parent, step-parent, or another adult living in your home act in a way that made you afraid that you would be physically hurt? |
* All questions from the Philadelphia Urban ACE Survey
The main health metrics for this study were assessed by previously validated survey questions. Self-reported health status was assessed by asking the respondent to rate their overall heath on a scale from one to five (CDC, 2017). Current smoking status was assessed from the National Health and Nutrition Examination Survey (NHANES) - smoking and Tobacco use 2017–2018 question (SMQ.040). Participants current mental health status was assessed through questions asking about hopefulness for the future from the Center for Epidemiological Studies Short Depression Scale (CESD 10) and their ability to cope with stress from the Perceived Stress Scale (Cohen et al., 1983).
Protective factors were assessed using three survey questions. Survey participants were asked if they thought their family cared about them when times were hard using a question from the Resilience Research Center (Jefferies et al., 2018). They were asked if they felt the people in their neighborhood looked out for each other and could be trusted (BRFSS), and whether they participated in a childhood youth program. Responses were dichotomized for analysis.
Statistical Analysis
319 people were surveyed and only participants that reported an adversity score ≥ 2 were included in the analysis (n = 248). Descriptive statistics summarized demographic and survey variables of interest. Simple regression models were performed to compare childhood exposure of adverse and protective factors to the adult health outcomes of interest: their general health status, including smoking status, and mental health, including hopefulness for the future and ability to cope with stress. Multivariable logistic regression models were constructed to adjust for age, sex, and educational attainment. All statistical analysis was performed in the statistical software R version 4.0.0 (R Core Team, 2020), under an alpha level of 0.05.
Results
Demographic Measures
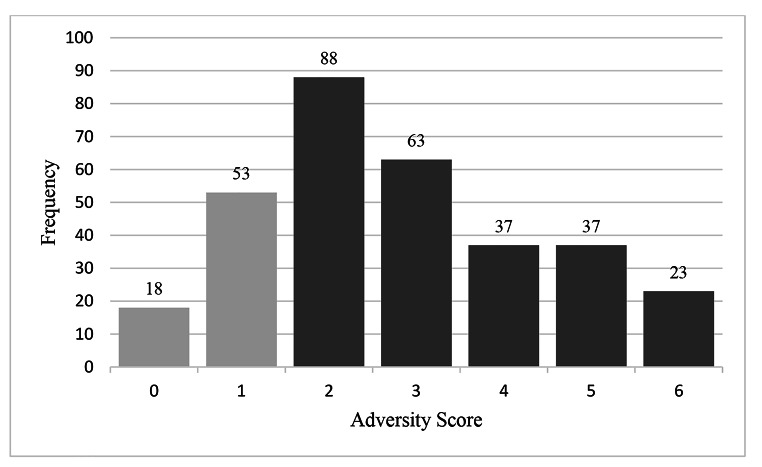
A distribution of the adversity score was examined and former residents that reported an adversity score ≥ 2 were included in the analysis (n = 248; Fig. 1). Demographic measures were assessed (Table 1). The average age of respondents was 36.3 years old (SD +/- 6.6 y). All participants primarily identified as Black and there were more women than men in the study (65.3% vs. 34.7%). Over 90% (91.9%) of participants had a high school GED or more. The majority of participants rated their health as excellent or very good (79.8%), were non-smokers (74.6%), felt hopeful about the future (60.5%), and felt like they could cope with stress (53.2%). The childhood support variables demonstrated that 87.5% felt like their family cared about them, 50.0% felt people in their neighborhood looked out for one another most of the time, and 56.9% of adults included for analysis had participated in the Cabrini Green youth mentoring program (CGYP; Table 3).
Fig. 1.
Adversity Score Distribution (Total surveyed = 319, only those with ≥ 2 included in analysis, n = 248)
Table 3.
Adult Health Outcomes, and Childhood Protective Factors Survey Results
| Survey Result | Number of people (n = 248) | % |
|---|---|---|
| Health Status | ||
| Excellent/Very Good/Good | 198 | 79.8% |
| Fair/Poor | 50 | 20.2% |
| Smoking Status | ||
| Yes | 63 | 25.4% |
| No | 185 | 74.6% |
| Affect | ||
| Felt hopeful | 150 | 60.5% |
| Not hopeful | 98 | 39.5% |
| Stress | ||
| Could Cope | 132 | 53.2% |
| No Cope | 116 | 46.8% |
| Childhood Support | ||
| Participation in Youth Program (Yes) | 141 | 56.9% |
| Family cared about you (Yes) | 217 | 87.5% |
| People in neighborhood looked out for each other (All/most of the time) | 124 | 50.0% |
Bivariate Analysis
Decreased smoking rates as an adult were observed for those who reported their families cared for them as children (OR 0.30, 95% CI, 0.14–0.66, aOR 0.35, 95% CI, 0.16–0.78; Table 4). Similarly, participants who felt like their family cared for them reported feeling more hopeful about the future (OR 2.77, 95% CI, 1.28-6.00, aOR 2.63, 95% CI, 1.21–5.75; Table 4). Additionally, former residents who believed that people looked out for each other in the neighborhood demonstrated more than a two-fold increase odds of having a self-reported adult health status of good or excellent health (OR 2.31, 95% CI, 1.21–4.42, aOR 2.01, 95% CI, 1.02–3.95; Table 4).
Table 4.
Childhood Protective Factors and Adult Health Outcomes
|
Childhood Protective Factor
Adult Health Outcome |
Odds ratio (95% CI) | Adjusted Odds ratio (95% CI)* |
|---|---|---|
| Family caring about you in childhood | ||
| Hopeful about future (Most or all of the time) | 2.77 (1.28-6.00)** | 2.63 (1.21–5.75)** |
| Current smoking status (not at all) | 0.30 (0.14–0.66)** | 0.35 (0.16–0.78)** |
| Neighborhood looking out for you | ||
| Current self-reported health status (good/very good/ excellent health) | 2.31 (1.21–4.42)** | 2.01 (1.02–3.95)** |
* Multivariable logistic regression was adjusted for age, sex, and educational attainment
** Statistically significant under p < .03
Discussion
Findings from this study suggest that a caring family and neighborhood connectedness are protective in mitigating the negative health outcomes associated with childhood adversity. Participants in this study grew up in a poor, segregated neighborhood with high rates of community violence. In a previous study surveying seven-to-13-year-old children living in Cabrini-Green Homes in the 1990’s, children reported that 42% had already seen someone shot and 37% had seen someone stabbed (Sheehan et al., 1997). These statistics are alarming and highlight the need to identify protective factors that could mitigate the effects of this trauma (Sheehan et al., 2021).
The Wisconsin Behavioral Risk Factor Survey (BRFS), a large national survey, expanded in 2014 to include questions related youth resilience and positive childhood experiences (Wisconsin Department of Health Services, 2015; Silva, 2014). Similar to our current study, results from the BRFS indicated that feeling like your family stood by you during hard times and having someone to talk with about difficult feelings led to the development of resilience (Sege et al., 2017). Another national study found that for children exposed to adverse childhood experiences, the strongest protective factor for positive academic success was having a parent sharing ideas and talking to their child about topics that mattered (Robles et al., 2019). Further, Bethell et al. demonstrated that similar to the cumulative effects of multiple ACEs, positive childhood experiences also demonstrate a dose-response association with adult mental and relational health (2019).
In a recent review, Duh-Leong et al. discussed the value of a social support system for children (2021). They described the importance of social capital, the benefits a child receives from social relationships at family and community levels, and explained that through social relationships, children exposed to adversity can achieve healthy outcomes and even thrive (Duh-Leong et al., 2021). Collectively, this research demonstrates that programs and resources should focus on strengthening family relationships and building community partnerships to increase social support for children.
This current study is not without its limitations. First, this is a retrospective cohort study and cannot confirm causal effect. It is further limited by the potential selection bias of participants. Participants were recruited through Facebook groups, word of mouth, and prior involvement in a youth group, which may not be representative of the entire Cabrini-Green Community. These participants who accessed the survey may represent a more affluent group than the population as a whole and may have looked more favorably on their circumstances and neighborhood growing up and their current health status. Unfortunately, it was challenging to locate individuals 25 years later from a neighborhood that no longer exists, leading to a small sample size. This study was also a subset of a larger one examining the effects of a youth development program for youth in the Cabrini Green Neighborhood and the questions used for this study were limited to the initial survey.
Further, multivariable analyses were difficult to perform due to an already small sample size of the study. Future efforts could work on expanding the sample size by surveying adults who grew up in government housing similar to Cabrini Green, such as the Henry Horner Homes on the West Side of Chicago and the Robert Taylor Homes and Stateway Gardens on the South Side of Chicago. Lastly, the average age of those surveyed was 36.3 years old and most participants rated their current health as very good/excellent. Participants may be too young for the adverse health outcome to have occurred and these results may continue to change as the population ages. Current smoking status, however, may be indicative of future health outcomes.
Conclusions
These findings suggest that a caring family and neighborhood connectedness are protective in mitigating the long-term health effects of childhood adversity in urban environments. Promoting these protective factors may be one path forward towards reducing existing health disparities. Resources should be devoted to help strengthen families and their communities.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of Interest
KS is a co-founder of the Chicago Youth Programs. She did not participate in the analysis of the data. All other authors have no conflict of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. American Journal of Preventive Medicine. 2010;39(1):93–98. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- Austen, B. (2018). High-Risers: Cabrini-Green and the Fate of American Public Housing. HarperCollins Publishers
- Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Affairs (Project Hope) 2014;33(12):2106–2115. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive Childhood Experiences and Adult Mental and Relational Health in a Statewide Sample. JAMA Pediatrics. 2019;173(11):e193007. doi: 10.1001/jamapediatrics.2019.3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleck J, Debate R. Long-Term Association Between Developmental Assets and Health Behaviors. Health Education & Behavior. 2016;43(5):543–551. doi: 10.1177/1090198115606915. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Adverse childhood experiences reported by adults—five states. MMWR Morb Mortal Wkly Rep. 2009;59(49):1609–1613. [PubMed] [Google Scholar]
- Center for Disease Control and Prevention [CDC] Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2017. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Fein JA. Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventive Medicine. 2015;49(3):354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. Journal of Community Psychology. 2000;28(6):625–641. doi: 10.1002/1520-6629(200011)28:6<625::AID-JCOP6>3.0.CO;2-R. [DOI] [Google Scholar]
- Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clinical Psychology Review. 2010;30(5):479–495. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Duh-Leong C, Dreyer BP, Huang TT, Katzow M, Gross RS, Fierman AH, Tomopoulos S, Di Caprio C, Yin HS. Social Capital as a Positive Social Determinant of Health: A Narrative Review. Academic Pediatrics. 2021;21(4):594–599. doi: 10.1016/j.acap.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Giano, Z., Wheeler, D. L., & Hubach, R. D. (2020). The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health, 20(1), 10.1186/s12889-020-09411-z [DOI] [PMC free article] [PubMed]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet. Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Jefferies P, McGarrigle L, Ungar M. The CYRM-R: A Rasch-validated revision of the Child and Youth Resilience Measure. Journal of Evidence-Informed Social Work. 2018 doi: 10.1080/23761407.2018.1548403. [DOI] [PubMed] [Google Scholar]
- Lee, T. Y., Cheung, C. K., & Kwong, W. M. (2012). Resilience as a Positive Youth Development Construct: A Conceptual Review. The Scientific World Journal, 1–9. 10.1100/2012/390450 [DOI] [PMC free article] [PubMed]
- Liu SR, Kia-Keating M, Nylund-Gibson K, Barnett ML. Co-Occurring Youth Profiles of Adverse Childhood Experiences and Protective Factors: Associations with Health, Resilience, and Racial Disparities. American Journal of Community Psychology. 2020;65(1–2):173–186. doi: 10.1002/ajcp.12387. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Development. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marciniak, E. (1986). Reclaiming the Inner City: Chicago’s Near North revitalization Confronts Cabrini-Green. Inst of Urban Life
- Masten AS. Global Perspectives on Resilience in Children and Youth. Child Development. 2014;85(1):6–20. doi: 10.1111/cdev.12205. [DOI] [PubMed] [Google Scholar]
- Mehta NK, Lee H, Ylitalo KR. Child health in the United States: Recent trends in racial/ethnic disparities. Social Science & Medicine. 2013;95:6–15. doi: 10.1016/j.socscimed.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of Adverse Childhood Experiences From the 2011–2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatrics. 2018;172(11):1038. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercy JA, Saul J. Creating a healthier future through early interventions for children. JAMA. 2009;301(21):2262–2264. doi: 10.1001/jama.2009.803. [DOI] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Journal of Child Abuse and Neglect. 2013;37:917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles A, Gjelsvik A, Hirway P, Vivier PM, High P. Adverse Childhood Experiences and Protective Factors With School Engagement. Pediatrics. 2019;144(2):e20182945. doi: 10.1542/peds.2018-2945. [DOI] [PubMed] [Google Scholar]
- Sacks, V., & Murphey, D. (2018). The prevalence of adverse childhood experiences, nationally, by state, and by race or ethnicity
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. The Journal of Adolescent Health: Society for Adolescent Medicine. 2013;53(4 Suppl):S32–S38. doi: 10.1016/j.jadohealth.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoon, I. (2012). The Social Ecology of Resilience. Temporal and Contextual Dimensions to Individual Positive Development: A Developmental–Contextual Systems Model of Resilience (pp. 143–156). 10.1007/978-1-4614-0586-3_13
- Search Institute (2007). 40 Developmental assets for adolescents. https://www.search-institute.org
- Sege, R., Bethell, C., Linkenbach, J., Jones, J., Klika, B., & Pecora, P. J. (2017). Balancing adverse childhood experiences with HOPE: New insights into the role of positive experience on child and family development. https://cssp.org/resource/balancing-aces-with-hope-final
- Sheehan K, DiCara JA, LeBailly S, Christoffel KK. Children’s exposure to violence in an urban setting. Archives of Pediatrics & Adolescent Medicine. 1997;151(5):502–504. doi: 10.1001/archpedi.1997.02170420072012. [DOI] [PubMed] [Google Scholar]
- Sheehan K, Bhatti PK, Yousuf S, Rosenow W, Roehler DR, Hazekamp C, Orbuch R, Bartell T, Quinlan K, DiCara J. Long-term Effects of a Community-based Positive Youth Development Program for African American Youth Living in Cabrini Green: Health, Education, and Financial Well-being in Adulthood. BMC Public Health. 2022;22(1):593. doi: 10.1186/s12889-022-13016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva NM. The Behavioral Risk Factor Surveillance System. International Journal of Aging and Human and Development. 2014;79(4):336–338. doi: 10.1177/0091415015574184. [DOI] [PubMed] [Google Scholar]
- Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, Williams DR. Racial disparities in child adversity in the US: Interactions with family immigration history and income. American Journal of Preventive Medicine. 2016;50(1):47–56. doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- Walsh D, Mccartney G, Smith M, Armour G. Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): a systematic review. Journal of Epidemiology and Community Health. 2019;73(12):1087–1093. doi: 10.1136/jech-2019-212738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisconsin Department of Health Services/Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. [Google Scholar]
- U.S (Census Bureau; Census 1990). https://www.census.gov