Abstract
Protective factors such as safe, stable, nurturing relationships and environments can prevent the long-term effects of adverse childhood experiences (ACEs). Recently, policymakers and practitioners have sought to better understand environmental level influences on exposure to ACEs, given the crucial role of social determinants of health in alleviating racial health inequities. Thus, this study seeks to understand how ACEs can be mitigated through neighborhood-level factors; it examines the relationships among ACEs, safe and supportive neighborhoods, and overall health status by race/ethnicity using a national data sample. Data were obtained from 30,530 households with children who participated in the 2018 National Survey for Children’s Health, a nationally representative survey. Using multivariable logistic regression, safe and supportive neighborhoods were assessed as potential moderators of the association between ACEs and overall health status by race/ethnicity. Two separate models were run for each moderator, controlling for sex, age, and gender of the child. The presence of a safe neighborhood weakened the association between ACEs and overall health status. This was demonstrated by lower odds of experiencing poor health. The presence of a supportive neighborhood showed a similar pattern. However, these patterns varied when disaggregating the data by race/ethnicity. This study underscores the importance of community-level prevention and intervention efforts to mitigate the health effects of ACEs. Public health efforts seeking to prevent poor health outcomes should consider the socio-environmental influences on health behaviors across the lifespan and continue to address the varying needs of historically disadvantaged populations.
Keywords: Adverse childhood experiences, Children’s health, Social cohesion, Protective factors
Background
Adverse Childhood Experiences (ACEs) include abuse (physical, emotional, sexual), neglect (physical, emotional), and household dysfunction (mental illness in the household, incarcerated relative, mother treated violently, substance abuse in the household, parental divorce or parental separation) (Felitti et al., 2019). ACEs expose developing brains to stress, which hinders cognitive development (Anda et al., 2006) and results in a wide range of physical health difficulties, mental health difficulties, and poor health behaviors during childhood, adolescence, and adulthood (Felitti et al., 2019; Flaherty et al., 2013; Lanier et al., 2018). The more ACEs an individual experiences, the more likely they are to experience health-related difficulties and early mortality (Brown et al., 2009; Crouch et al., 2018b; Felitti et al., 2019). Positive, supportive youth-adult relationships positively impact children’s health and may reduce the negative health and well-being impacts of ACEs as early as adolescence, which is a critical period for brain development, and is often the time that risk behavior engagement occurs (Srivastav et al., 2020c). Evidence suggests that individuals who found that growing up with an adult “who made them feel safe and protected” reduced the likelihood of poor health outcomes, even among individuals who experienced four or more ACEs (Crouch et al., 2018a). Safe, stable, nurturing relationships (SSNRs) can occur between children and their parents or between children and other supportive adults, across early childhood to late adolescence, has been shown to mitigate the negative health and social impacts of experiencing trauma (Srivastav et al., 2020c) and maltreatment (Schofield et al., 2013).
As ACEs have continued to receive widespread attention and recognition in public health as a root cause of many risk behaviors, chronic health conditions, and poor social outcomes, the measures of ACEs, focus largely on individual experiences (e.g., abuse, neglect, and household dysfunction) have been critiqued because they ignore the role of cultural and social context that may play a role in exposure to such experiences. For example, Ellis and Dietz (2017) have developed a new framework to address ACEs which recognizes that ACEs are experiences caused by adverse community environments which are created by inequities such as structural racism (Ellis & Dietz, 2017). Community advocates have called to amend the original “ACE pyramid,” which conceptualized ACEs as a root cause of disease and mortality to include the role of structural, systemic, and historical trauma as the foundation for exposure to ACEs (Bruner, 2017; Dhaliwal, 2016). This is supported by emerging evidence that suggests that the traditional ACEs may not fully capture the lived experiences of children of color, who are more likely to be exposed to traumatic environments compared to their white counterparts due to systemic inequities (Bruner, 2017; Cronholm et al., 2015; Srivastav et al., 2020c). As the role of the life course, specifically early childhood (Williams & Cooper, 2019a, b), is increasingly recognized as a crucial approach to race equity, there has been a call to better understand the role of systemic and environmental influences in exposure to ACEs to better understand ways to alleviate health disparities for associated health consequences.
Neighborhoods are a key example of such systemic and environmental influences, also known as structural determinants of health. Neighborhoods profoundly influence child health. Children who live in safe neighborhoods may have better outcomes related to behavior (Edwards & Bromfield, 2009), development, and physical health (Christian et al., 2015; Fan & Chen, 2012), including complex and intersecting childhood health conditions (Jackson et al., 2019). Community development efforts may positively influence a range of health care outcomes (Chisolm et al., 2020). However, the health impacts of community development efforts “generally have not been considered or evaluated” (Jutte et al., 2015). Because children experience their neighborhoods indirectly through their caregivers (To et al., 2001), parental factors may have a greater influence over child well-being than neighborhood factors (Kenney, 2012). Although socioeconomic status and neighborhoods are often intertwined, neighborhood factors impact child health beyond family income levels, specifically through racial residential segregation, a form of structural racism (Kersten et al., 2018). Structural racism refers to influential socio-ecological levels in which racism exists, including systems, social forces, institutions, ideologies, and processes that can adversely affect individuals of color (Gee & Ford, 2011). Racial residential segregation is considered a major form of structural racism in the U.S. Though institutional racial segregation became illegal in 1968 during the Civil Rights Era, residential segregation for Blacks continues to be high across the U.S. today (Abramovitz & Smith, 2021; Williams & Collins, 2001; Williams & Cooper, 2019b).
There is a need to better understand how neighborhood safety may mitigate the association between ACEs and physical health to advance racial health equity for children and families. While there has been promising research demonstrating safe neighborhoods may partially mitigate the association between ACEs and well-being, little is known about how neighborhood contexts influence the health outcomes associated with ACEs and how this may differ between racial/ethnic groups, given historical and structural inequities that exist in the U.S. To fill in this knowledge gap, our study aims to better understand how ACEs can be mitigated through neighborhood-level factors using a large population-level dataset. Our study is guided by the socio-ecological model, which posits that Adverse Childhood Experiences occur in connection with complex, interrelated systems (Ungar, 2012).
Methods
Data were obtained from the 2018 National Survey of Children’s Health (n = 30,530; weighted n = 73,433,138). The survey was completed by an adult in the household with knowledge of both the child’s health and their healthcare. Those missing or with non-Hispanic multi-racial/other race/ethnicity were excluded (n = 2,407). Then, the number of ACEs a participant reported was collapsed into a binary “no ACEs” or “at least one ACE.”
Examining ACE exposure this way is consistent with previous research (Merrick et al., 2020; Srivastav et al., 2020a) and the original ACE study. (Felitti et al., 1998) The examination of ACEs as a binary variable also considers the original study’s pivotal findings: ACEs are highly interrelated (Crouch et al., 2017; Dong et al., 2004), the toxic stress from any type of ACE is approximately the same. (Felitti et al., 1998) and exposure to even one can increase the risk of poor outcomes in adulthood. (Felitti, 2009) Finally, assessing ACEs as a dichotomous variable recognizes limitations identified by the original ACE study—many studies prior focused on single exposures and single health outcomes; they did not consider that experiences in childhood are not static. (Anda et al., 1999; Felitti et al., 1998; Srivastav et al., 2020a).
ACE exposure was defined as at least one of the following: hard to cover basics on family’s income (‘somewhat often’ or ‘very often’); parents divorced/separated (‘yes’); parent or guardian died (‘yes’); parent or guardian incarcerated (‘yes’); witnessed physical violence (‘yes’); victim/witness of neighborhood violence (‘yes’); lived with anyone mentally ill (‘yes’); lived with anyone alcohol/drug problem (‘yes’); treated or judged unfairly due to race/ethnicity (‘yes’). The final analytic sample (Fig. 1) included 10,475 responses, which represents 38,828,788 children with at least one ACE when the survey weights are accounted for.
Fig. 1.
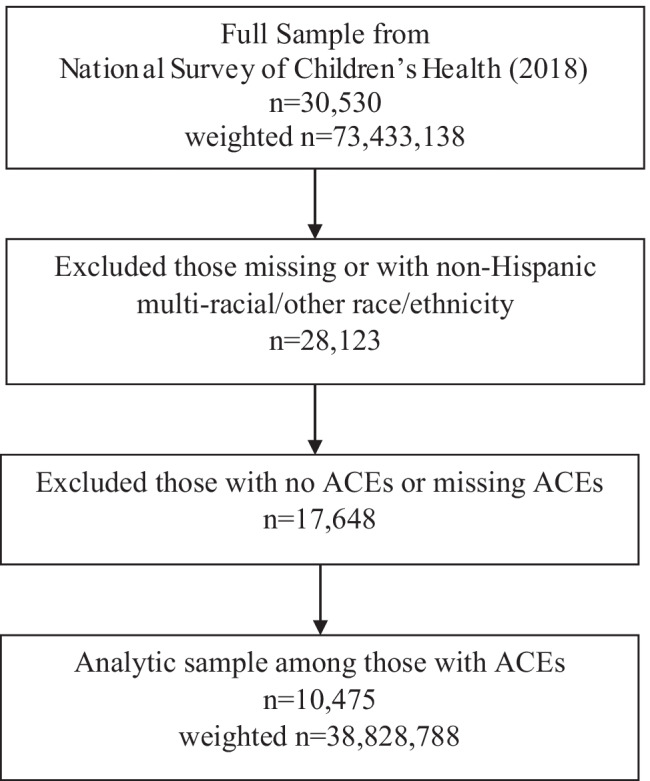
CONSORT diagram of analytics sample among those with at least one ACE
Consistent with previous studies, safe neighborhoods and supportive neighborhoods were examined as separate constructs. (Borrell et al., 2016) A child was considered living in a supportive neighborhood when a respondent answered “definitely agree” to at least one and “somewhat agree” or “definitely agree” to the remainder among the following: “people in this neighborhood help each other out”; “we watch out for each other's children in this neighborhood”; “when we encounter difficulties, we know where to go for help in our community.” A child was considered to live in a safe neighborhood if they answered “definitely agree,” to the prompt, “this child is safe in our neighborhood.” The outcome of interest was whether the child’s overall health status was poor (i.e., not excellent or very good).
The control variables included: child’s age group, household poverty level, and parents’ combined health status. Child’s age group was categorized as: 0–3; 4–7; 8–11; 12–14; 15–17, and child’s gender was grouped as male and female. Household poverty level was categorized as: <100% of the federal poverty level (FPL); 100- <200% FPL; 200- <400% FPL; and 400% + FPL. Combined parent health status was defined using mother and father reported health status. Parent health status was defined as “excellent/very good” if both parents reported excellent or very good health, or, in the case of a single-parent household, the primary caregiver reported excellent or very good health. Conversely, combined parent health status was defined as “not excellent/very good” if either parent reported not excellent or very good health. Further, we stratified our analysis by child’s race/ethnicity. Child’s race/ethnicity was categorized as: Hispanic or non-Hispanic Asian, Black, or white.
To account for the complex sampling design, analyses were done in SAS 9.4 using survey analysis procedures. Bivariate analyses of ACE status, ACE components, and neighborhood variables were done by race/ethnicity. We conducted bivariate analyses of demographic variables and potential confounders by ACE status. Finally, we conducted bivariate analyses of demographic variables and potential confounders by neighborhood variables.
Finally, we conducted multivariable modeling to assess the association between neighborhood-level factors and self-reported poor health. We restricted our population to those with at least one ACE. Multivariable logistic regression models were done to obtain the odds of having poor health among those living in a safe neighborhood compared to those living in an unsafe neighborhood, and among those live in a supportive neighborhood compared to those living in an unsupportive neighborhood. Adjusted odds ratios and their relevant 95% confidence intervals (CIs) were obtained. Models were adjusted for child’s age group and household poverty status. We stratified each model by the child’s race/ethnicity.
Results
Approximately 40.7% (95% CI: 39.4–41.9) of children in the.S.U.S. have at least one ACE. Non-Hispanic Black children had a significantly higher prevalence (55.4%; 95% CI: 51.6–59.1) of at least one ACE than their counterparts of any other race/ethnicity. The most prevalent ACE was parent/guardian divorce (23.4%; 95% CI: 22.4–24.5), and the next prevalent was hard to cover basics on family’s income (15.1%; 95% CI: 14.1–16.1; Table 1). This was true across all race/ethnicity groups.
Table 1.
Components of ACEs and supportive or safe neighborhood for overall sample by race/ethnicity (2018 NSCH)
| Overall | Hispanic | non-Hispanic white | non-Hispanic Black | non-Hispanic Asian | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||||||
| Components of ACEs | 40.7 | 39.4 | 41.9 | 43.1 | 39.7 | 46.4 | 37.5 | 36.3 | 38.7 | 55.4 | 51.6 | 59.1 | 22.1 | 17.7 | 26.4 |
| At least one ACE | 40.7 | 39.4 | 41.9 | 43.1 | 39.7 | 46.4 | 37.5 | 36.3 | 38.7 | 55.4 | 51.6 | 59.1 | 22.1 | 17.7 | 26.4 |
| Hard to cover basics on family's income | 15.1 | 14.1 | 16.1 | 18.0 | 15.3 | 20.7 | 13.3 | 12.3 | 14.2 | 19.3 | 16.3 | 22.3 | 7.2 | 4.2 | 10.2 |
| Parent or Guardian Divorced | 23.4 | 22.4 | 24.5 | 24.1 | 21.2 | 26.9 | 22.4 | 21.4 | 23.4 | 31.2 | 27.9 | 34.6 | 9.5 | 6.2 | 12.9 |
| Parent or Guardian Died | 3.2 | 2.7 | 3.6 | 3.2 | 2.0 | 4.4 | 2.6 | 2.2 | 3.0 | 5.4 | 3.9 | 6.9 | 2.9 | 1.5 | 4.3 |
| Parent or Guardian Time in Jail | 7.4 | 6.7 | 8.1 | 7.9 | 6.0 | 9.8 | 6.4 | 5.7 | 7.0 | 12.5 | 10.2 | 14.8 | 1.4 | 0.4 | 2.4 |
| Adults Slap, Hit, Kick, Punch Others in Home | 5.4 | 4.8 | 6.0 | 5.9 | 4.2 | 7.5 | 4.8 | 4.2 | 5.3 | 8.0 | 6.0 | 9.9 | 2.5 | 0.6 | 4.3 |
| Victim/witness of Violence in Neighborhood | 4.0 | 3.4 | 4.6 | 5.2 | 3.5 | 6.9 | 2.9 | 2.5 | 3.3 | 7.0 | 5.2 | 8.8 | 0.9 | 0.3 | 1.5 |
| Lived with Mentally Ill | 7.3 | 6.7 | 7.9 | 5.2 | 4.0 | 6.5 | 8.9 | 8.2 | 9.6 | 7.4 | 5.5 | 9.2 | 0.9 | 0.3 | 1.4 |
| Lived with Person with Alcohol/Drug Problem | 7.9 | 7.3 | 8.5 | 6.9 | 5.3 | 8.4 | 9.4 | 8.7 | 10.1 | 6.3 | 4.6 | 7.9 | 1.9 | 0.0 | 4.3 |
| Treated or judged unfairly due to race/ethnicity | 3.6 | 3.1 | 4.0 | 4.6 | 3.5 | 5.8 | 1.3 | 0.9 | 1.7 | 9.7 | 7.8 | 11.6 | 5.6 | 2.8 | 8.4 |
| Components of Outcomes of Interest | |||||||||||||||
| Supportive neighborhood | 56.3 | 55.0 | 57.6 | 49.6 | 46.2 | 53.0 | 62.9 | 61.7 | 64.2 | 45.1 | 41.5 | 48.7 | 50.5 | 45.4 | 55.7 |
| People in this neighborhood help each other out (definitely agree) | 37.1 | 35.9 | 38.3 | 28.6 | 25.5 | 31.7 | 44.0 | 42.8 | 45.2 | 26.1 | 22.9 | 29.2 | 37.9 | 33.0 | 42.7 |
| We watch out for each other's children in this neighborhood (definitely agree) | 45.3 | 44.1 | 46.6 | 40.3 | 37.0 | 43.6 | 51.0 | 49.8 | 52.2 | 33.9 | 30.5 | 37.3 | 42.1 | 37.1 | 47.1 |
| When we encounter difficulties, we know where to go for help in our community (definitely agree) | 49.6 | 48.4 | 50.9 | 44.3 | 41.0 | 47.7 | 54.3 | 53.1 | 55.5 | 44.3 | 40.5 | 48.0 | 42.1 | 37.2 | 47.1 |
| This child is safe in our neighborhood (definitely agree) | 65.4 | 64.1 | 66.6 | 58.1 | 54.7 | 61.4 | 71.2 | 70.1 | 72.4 | 57.0 | 53.3 | 60.7 | 64.3 | 59.2 | 69.3 |
Approximately 56.3% (95% CI: 55.0–57.6) of children lived in a supportive neighborhood, and 65.4% (95% CI: 64.1–66.6) lived in a safe neighborhood. Non-Hispanic Black (45.1%; 95% CI: 41.5–48.7), Hispanic (49.6%; 95% CI: 46.2–53.0), and non-Hispanic Asian (50.5%; 95% CI: 45.4–55.7) had a significantly lower prevalence of living in a supportive neighborhood than non-Hispanic white children (62.9%; 95% CI: 61.7–64.2). Similarly, Non-Hispanic Black (57.0%; 95% CI: 53.3–60.7), Hispanic (58.1%; 95% CI: 54.7–61.4), and non-Hispanic Asian (64.3%; 95% CI: 59.2–69.3) had a significantly lower prevalence of living in a safe neighborhood than non-Hispanic white children (71.2%; 95% CI: 70.1–72.4; Table 1).
Overall, children with at least one ACE had a significantly higher prevalence of poor health and had a significantly higher proportion who identified as non-Hispanic Black, as an adolescent (ages 12–17), as living in a household <200% FPL, and as living in a household where the highest adult educational attainment was less than a high school diploma, compared to those with no ACEs (Table 2). Children with at least one ACE who lived in an unsafe neighborhood had a significantly higher prevalence of poor health and had a significantly higher proportion who identified as non-Hispanic Black or Hispanic and living in a household <200% FPL, compared to those with at least one ACE who lived in a safe neighborhood (Table 3). Children with at least one ACE who lived in an unsupportive neighborhood had a significantly higher prevalence of poor health and a significantly higher proportion who identified as non-Hispanic Black children and living in a household <200% FPL, compared to those with at least one ACE who lived in a supportive neighborhood (Table 3).
Table 2.
Bivariate analyses: demographic distribution by adverse childhood experience (ACE). Sample excluding those missing or non-Hispanic multi-racial/other race/ethnicity (2018 National Survey of Children’s Health; n = 28,123)
| Overall | No ACEs | At Least One ACE | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| weighted n | % | 95% CI | weighted n | % | 95% CI | weighted n | % | 95% CI | ||||
| Poor health | 6,719,935 | 9.8 | 9.0 | 10.6 | 2,325,194 | 6.0 | 5.2 | 6.9 | 3,994,123 | 15.0 | 13.5 | 16.6 |
| Race/ethnicity | ||||||||||||
| Hispanic | 18,530,886 | 26.9 | 25.6 | 28.2 | 9,924,175 | 25.6 | 23.8 | 27.4 | 7,503,460 | 28.2 | 26.0 | 30.4 |
| non-Hispanic white | 37,089,273 | 53.8 | 52.6 | 55.0 | 22,408,257 | 57.7 | 56.0 | 59.4 | 13,457,389 | 50.5 | 48.5 | 52.6 |
| non-Hispanic Black | 9,818,353 | 14.2 | 13.3 | 15.2 | 3,999,360 | 10.3 | 9.2 | 11.4 | 4,958,220 | 18.6 | 17.0 | 20.3 |
| non-Hispanic Asian | 3,488,274 | 5.1 | 4.6 | 5.5 | 2,496,996 | 6.4 | 5.7 | 7.2 | 707,311 | 2.7 | 2.1 | 3.2 |
| Age group | ||||||||||||
| 0–3 | 14,597,013 | 21.2 | 20.1 | 22.2 | 10,458,923 | 26.9 | 25.5 | 28.4 | 3,401,583 | 12.8 | 11.3 | 14.3 |
| 4–7 | 14,731,959 | 21.4 | 20.3 | 22.4 | 8,861,955 | 22.8 | 21.5 | 24.1 | 5,146,020 | 19.3 | 17.6 | 21.1 |
| 8–11 | 15,844,232 | 23.0 | 22.0 | 24.0 | 8,402,585 | 21.6 | 20.3 | 23.0 | 6,539,744 | 24.6 | 22.9 | 26.2 |
| 12–14 | 11,892,132 | 17.3 | 16.3 | 18.2 | 5,887,015 | 15.2 | 13.9 | 16.4 | 5,286,087 | 19.9 | 18.3 | 21.4 |
| 15–17 | 11,861,449 | 17.2 | 16.3 | 18.1 | 5,218,310 | 13.4 | 12.5 | 14.4 | 6,252,946 | 23.5 | 21.8 | 25.2 |
| Household poverty level | ||||||||||||
| <100% FPL | 13,627,438 | 19.8 | 18.6 | 20.9 | 5,591,380 | 14.4 | 13.0 | 15.8 | 7,136,116 | 26.8 | 24.8 | 28.8 |
| 100-<200% FPL | 15,147,730 | 22.0 | 20.8 | 23.1 | 6,937,470 | 17.9 | 16.4 | 19.3 | 7,426,678 | 27.9 | 25.9 | 29.8 |
| 200-<400% FPL | 18,560,212 | 26.9 | 25.9 | 27.9 | 10,744,615 | 27.7 | 26.3 | 29.0 | 6,976,361 | 26.2 | 24.6 | 27.8 |
| 400%+ FPL | 21,591,406 | 31.3 | 30.3 | 32.4 | 15,555,323 | 40.1 | 38.6 | 41.5 | 5,087,226 | 19.1 | 17.7 | 20.5 |
| Highest education of adults in household | ||||||||||||
| Less than high school | 7,019,158 | 10.2 | 9.0 | 11.4 | 3,515,665 | 9.1 | 7.6 | 10.5 | 2,994,734 | 11.2 | 9.2 | 13.3 |
| High school or GED | 13,348,041 | 19.4 | 18.3 | 20.4 | 5,621,129 | 14.5 | 13.2 | 15.8 | 7,040,439 | 26.4 | 24.5 | 28.4 |
| Some college or technical school | 14,996,006 | 21.8 | 20.8 | 22.7 | 6,923,132 | 17.8 | 16.6 | 19.1 | 7,219,267 | 27.1 | 25.5 | 28.7 |
| College degree or higher | 33,563,581 | 48.7 | 47.5 | 49.9 | 22,768,861 | 58.6 | 56.9 | 60.3 | 9,371,939 | 35.2 | 33.4 | 37.0 |
Table 3.
Bivariate analyses: demographic distribution of outcomes of interest (among those with at least one ACE; 2018 National Survey of Children's Health; n = 10,200)
| Neighborhood Safety | Neighborhood Support | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Safe | Not Safe | Supportive | Not Supportive | |||||||||||||
| weighted n | % | 95% CI | weighted n | % | 95% CI | weighted n | % | 95% CI | weighted n | % | 95% CI | |||||
| Poor health | 1,706,247 | 11.3 | 9.8 | 12.8 | 2,268,368 | 20.1 | 17.1 | 23.0 | 1,398,132 | 11.5 | 9.8 | 13.2 | 2,541,871 | 18.2 | 15.7 | 20.6 |
| Race/ethnicity | ||||||||||||||||
| Hispanic | 3,747,728 | 24.8 | 22.1 | 27.4 | 3,711,341 | 32.7 | 29.1 | 36.4 | 3,054,789 | 25.1 | 22.0 | 28.1 | 4,372,662 | 31.2 | 28.0 | 34.3 |
| non-Hispanic white | 8,526,866 | 56.4 | 53.8 | 59.0 | 4,846,138 | 42.7 | 39.6 | 45.9 | 6,976,115 | 57.2 | 54.3 | 60.2 | 6,325,293 | 45.1 | 42.3 | 47.8 |
| non-Hispanic Black | 2,491,258 | 16.5 | 14.4 | 18.5 | 2,442,633 | 21.5 | 18.9 | 24.2 | 1,883,476 | 15.5 | 13.4 | 17.5 | 2,922,719 | 20.8 | 18.5 | 23.1 |
| non-Hispanic Asian | 351,849 | 2.3 | 1.8 | 2.9 | 340,053 | 3.0 | 1.9 | 4.1 | 271,773 | 2.2 | 1.6 | 2.8 | 416,701 | 3.0 | 2.0 | 3.9 |
| Age group | ||||||||||||||||
| 0–3 | 1,961,622 | 13.0 | 10.9 | 15.1 | 1,429,787 | 12.6 | 10.4 | 14.8 | 1,419,791 | 11.7 | 9.5 | 13.8 | 1,863,524 | 13.3 | 11.3 | 15.2 |
| 4–7 | 2,538,880 | 16.8 | 15.0 | 18.6 | 2,566,265 | 22.6 | 19.4 | 25.9 | 2,076,479 | 17.0 | 15.0 | 19.1 | 2,976,889 | 21.2 | 18.5 | 23.9 |
| 8–11 | 3,680,582 | 24.3 | 22.3 | 26.4 | 2,831,952 | 25.0 | 22.2 | 27.8 | 3,251,931 | 26.7 | 24.2 | 29.1 | 3,242,524 | 23.1 | 20.7 | 25.4 |
| 12–14 | 3,152,395 | 20.9 | 18.9 | 22.8 | 2,117,716 | 18.7 | 16.3 | 21.0 | 2,541,528 | 20.9 | 18.6 | 23.1 | 2,701,260 | 19.2 | 17.2 | 21.3 |
| 15–17 | 3,784,222 | 25.0 | 22.9 | 27.2 | 2,394,446 | 21.1 | 18.2 | 24.0 | 2,896,424 | 23.8 | 21.3 | 26.2 | 3,253,178 | 23.2 | 20.7 | 25.6 |
| Household poverty level | ||||||||||||||||
| <100% FPL | 3,455,848 | 22.9 | 20.5 | 25.2 | 3,654,094 | 32.2 | 28.8 | 35.6 | 2,721,048 | 22.3 | 19.6 | 25.0 | 4,307,517 | 30.7 | 27.8 | 33.6 |
| 100-<200% FPL | 3,771,319 | 24.9 | 22.6 | 27.2 | 3,572,299 | 31.5 | 28.2 | 34.8 | 2,958,984 | 24.3 | 21.8 | 26.7 | 4,254,412 | 30.3 | 27.5 | 33.1 |
| 200-<400% FPL | 4,289,150 | 28.4 | 26.3 | 30.5 | 2,642,475 | 23.3 | 20.8 | 25.8 | 3,494,488 | 28.7 | 26.3 | 31.1 | 3,429,745 | 24.4 | 22.3 | 26.6 |
| 400% + FPL | 3,601,384 | 23.8 | 21.9 | 25.8 | 1,471,298 | 13.0 | 11.0 | 14.9 | 3,011,634 | 24.7 | 22.4 | 27.0 | 2,045,700 | 14.6 | 12.9 | 16.3 |
Overall, among children with at least one ACE, those living in a safe neighborhood had 42% lower (95% CI: 27–54) odds of poor health than those living in an unsafe neighborhood after adjustment. Among children with at least one ACE, those living in a supportive neighborhood had 34% lower (95% CI: 16–48) odds of poor than those living in an unsupportive neighborhood after adjustment (Table 4).
Table 4.
Adjusted odds ratio (aOR) and associated 95% confidence interval (CI) of poor health by neighborhood safe/supportive status—stratfied by race/ethnicity—only among those exposed to at least one ACE
| Overall | Hispanic | Non-Hispanic white | Non-Hispanic Black | Non-Hispanic Asian | |
|---|---|---|---|---|---|
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Neighborhood Safety | |||||
| Safe | 0.58 (0.46, 0.73) | 0.55 (0.33, 0.92) | 0.48 (0.37, 0.63) | 0.90 (0.56, 1.43) | 0.66 (0.19, 2.38) |
| Not safe | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| Neighborhood Support | |||||
| Supportive | 0.66 (0.53, 0.84) | 0.58 (0.33, 1.01) | 0.66 (0.50, 0.87) | 0.91 (0.57, 1.46) | 0.72 (0.24, 2.12) |
| Not supportive | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
Among non-Hispanic white children exposed to at least one ACE, those living in a safe neighborhood had 52% lower (95% CI: 37–63) odds of poor health than those living in an unsafe neighborhood after adjustment. The same pattern was true for supportive neighborhoods. Among non-Hispanic white children experiencing ACEs, those living in a supportive neighborhood had 34% lower (95% CI: 13–50) odds of poor health than those living in an unsafe neighborhood after adjustment (Table 4).
Among Hispanic children exposed to at least one ACE, those living in a safe neighborhood had 45% lower (95% CI: 8–67) odds of poor health than those living in an unsafe neighborhood after adjustment. No other significant differences were detected for the various race/ethnicity groups (Table 4).
Discussion
This study investigated whether the presence of a safe neighborhood or supportive neighborhood was associated with poor health among children who have experienced at least one ACE. As hypothesized, we found that children who have experienced at least one ACEs have a significantly lower prevalence of living in a safe or supportive neighborhood compared to children with no ACEs. Children with at least one ACE who lived in a safe or supportive neighborhood faced lower odds of experiencing poor health compared to their counterparts. These findings underscore previous research that suggests that ACEs are a social determinant of health; that is, they are affected by and can affect socio-environmental and structural factors that promote or deter engagement in healthy behaviors, leading to poor health outcomes. This also reinforces the importance of investing in community resilience, or the ability for communities to adapt, recover and thrive, even in the face of adversity. Prevention and intervention efforts should continue to ensure their approaches are rooted in community-level factors that dismantle systemic inequities. These can include promoting social supports, building social cohesion, ensuring equitable investment in communities, developing healthy community design and infrastructure, increasing access to healthy food, providing affordable housing, and ensuring all families are able to meet their basic needs through livable wages (Turner & Rawlings, 2009).
When examining these patterns by race/ethnicity, however, we found differing relationships. Although we found that Black and Hispanic children are more likely to live in unsafe and unsupportive neighborhoods compared to their white counterparts, the moderating effects of a safe and supportive neighborhood were only present for Hispanic children exposed to at least one ACE. Interestingly, the odds of poor health increased for Black children when they reported at least one ACE and living in a safe and/or supportive neighborhood compared to those who did not live in a safe and supportive neighborhood but reported at least one ACE. Some studies have suggested that racially diverse neighborhoods may have lower levels of trust, altruism, or community cohesion compared to homogenous neighborhoods (Dinesen et al., 2020; Putnam, 2007). These studies suggest that often, a solution to providing access and opportunity to Black families is not through investing in their neighborhoods but rather moving them into wealthier, all White neighborhoods, which may increase exposure to discrimination and stress (Turner & Rawlings, 2009). This is also consistent with research that shows that the negative effects of racial residential segregation are largely seen in urban areas as opposed to rural areas, which are comprised of a striking percentage of Black families (Dinesen et al., 2020). This may also support why the moderating effects of a safe and supportive neighborhood were present for Hispanic children, as they are more likely to live in urban settings that are impacted by racial residential segregation and concentrated disadvantage (Turner et al., 2016).
It should also be noted that there were no significant differences between safe and supportive neighborhoods and health status for non-Hispanic Asian children with at least one ACE. We suggest that these results be interpreted with caution, given the methodological concerns around the Asian American category. Specifically, this category is comprised of several racial/ethnic categories, and studies have found that some of the largest racial, health, and economic disparities exist within groups that comprise this category (Holland & Palaniappan, 2012). Additionally, there is some research to show that Asian Americans are more likely to live in ethnic enclaves (West Coast Poverty Center, 2010), which can be protective against the effects of community and systemic inequities that have been linked to ACEs (Srivastav et al., 2020a).
Ultimately, the impact of structural racism, whether through racial residential segregation or lack of access to opportunities and resources for children and families of color living in ethnic enclaves, likely plays a role in children of color’s disproportionate impact of ACEs and its associated consequences. Overall, these findings have important implications for focusing on systemic and community-level factors in the prevention of ACEs, specifically how place-based contexts can mitigate the effects of these traumatic experiences. This is also consistent with the field of research around ACEs moving towards a strengths-based approach through the concept of positive childhood experiences, which recognizes that early life experiences are fluid; children who have experienced ACEs may also have experienced several positive childhood experiences (Bethell et al., 2019; Srivastav et al., 2020b).
This study is the first to examine the relationship between ACEs, safe and supportive neighborhoods, and health status by race/ethnicity using a nationally representative sample of children. It provides innovative evidence that addresses existing gaps in knowledge about how the effects of a safe and supportive neighborhood in childhood may or may not mitigate the long-term effects of ACEs across racial groups. We recognize, however, that this study has some limitations. This data is self-reported by caregivers of the children. Caregivers may over-report socially desirable factors such as their children’s not being exposed to ACEs, living in a safe and supportive neighborhood, or having good health. In addition, our primary outcome measure was self-reported overall health, which can be a subjective assessment. Furthermore, there are varying approaches to constructing the ACE variable, with some studies using a continuous variable instead of a dichotomous variable, as used within this study. We believe that presenting/assessing the relationship by ACE type goes back to the limitations identified by the original ACE study—many public health studies focus on single exposures and single outcomes, which do not take into account that experiences in childhood are not static and the reality that the same type of trauma can have differing effects on different individuals (Srivastav et al., 2020a). Future research could, however, could focus on the accumulation of multiple ACEs to further examine these relationships.
Finally, the questions used to ask about a safe and supportive neighborhood have not yet been validated. There may also be other neighborhood factors that can provide a more precise understanding of a safe and supportive neighborhood that are not included in the NSCH, including but not limited to crime rate data, observations of neighborhood conditions, and ratings of neighborhood climate by a sample of residents. Future research should compare the self-reported measures of safe and supportive neighborhoods by caregivers to other validated measures.
In conclusion, this study provides unique and timely insight on whether protective factors at a community level, namely, a safe or supportive neighborhood, can buffer the effects of ACEs on health. The data show that while in the overall population, a safe or supportive neighborhood may be protective against the effect of ACEs on health, its effects may differ by race/ethnicity, likely due to the complex ways in which structural racism influences neighborhood contexts. Ensuring that all children live in safe and supportive neighborhoods should still be considered a solution for preventing the long-term consequences of ACEs, although this study highlights that there may be slightly different approaches to building resilience within these neighborhoods for different communities of color. Thus, as the field looks to address ACEs as a root cause of health disparities, it must consider multi-level approaches that not only provide safe and supportive neighborhoods for all children but address the socioeconomic and systemic inequities that contribute to racial health disparities among children.
Declarations
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abramovitz M, Smith RJ. The Persistence of Residential Segregation by Race, 1940 to 2010: The Role of Federal Housing Policy. Families in Society. 2021;102(1):5–32. doi: 10.1177/1044389420923469. [DOI] [Google Scholar]
- Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, Giovino GA. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell CD, Gombojav N, Whitaker RC. Family resilience and connection promote flourishing among US, children even amid adversity. Health Affairs (project Hope) 2019;38(5):729–737. doi: 10.1377/hlthaff.2018.05425. [DOI] [PubMed] [Google Scholar]
- Borrell, L. N., Graham, L., & Joseph, S. P. (2016). Associations of neighborhood safety and neighborhood support with overweight and obesity in US children and adolescents. Ethnicity & Disease, 26(4), 469–476. 10.18865/ed.26.4.469 [DOI] [PMC free article] [PubMed]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, Giles WH. Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine. 2009;37(5):389–396. doi: 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Bruner C. ACE, place, race, and poverty: Building hope for children. Academic Pediatrics. 2017;17(7, Supplement):S123–S129. doi: 10.1016/j.acap.2017.05.009. [DOI] [PubMed] [Google Scholar]
- Chisolm DJ, Jones C, Root ED, Dolce M, Kelleher KJ. A community development program and reduction in high-cost health care use. Pediatrics. 2020;146(2):e20194053. doi: 10.1542/peds.2019-4053. [DOI] [PubMed] [Google Scholar]
- Christian H, Zubrick SR, Foster S, Giles-Corti B, Bull F, Wood L, Knuiman M, Brinkman S, Houghton S, Boruff B. The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health & Place. 2015;33:25–36. doi: 10.1016/j.healthplace.2015.01.005. [DOI] [PubMed] [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Pachter LM, Fein JA. Adverse childhood experiences: Expanding the concept of adversity. American Journal of Preventive Medicine. 2015;49(3):354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Crouch E, Radcliff E, Strompolis M, Srivastav A. Safe, stable, and nurtured: Protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs) Journal of Child & Adolescent Trauma. 2018;12(2):165–173. doi: 10.1007/s40653-018-0217-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouch E, Strompolis M, Bennett KJ, Morse M, Radcliff E. Assessing the interrelatedness of multiple types of adverse childhood experiences and odds for poor health in South Carolina adults. Child Abuse & Neglect. 2017;65:204–211. doi: 10.1016/j.chiabu.2017.02.007. [DOI] [PubMed] [Google Scholar]
- Crouch E, Strompolis M, Radcliff E, Srivastav A. Examining exposure to adverse childhood experiences and later outcomes of poor physical and mental health among South Carolina adults. Children and Youth Services Review. 2018;84:193–197. doi: 10.1016/j.childyouth.2017.11.031. [DOI] [Google Scholar]
- Dhaliwal, K. (2016). Rejected. Reflected. Altered: Racing ACEs revisited [Brief]. Berkeley Media Studies Group. http://www.bmsg.org/wp-content/uploads/2016/10/racing_aces_memo_october2016.pdf. Accessed 12 July 2020
- Dinesen PT, Schaeffer M, Sønderskov KM. Ethnic diversity and social trust: A narrative and meta-analytical review. Annual Review of Political Science. 2020;23(1):441–465. doi: 10.1146/annurev-polisci-052918-020708. [DOI] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Edwards B, Bromfield LM. Neighborhood influences on young children’s conduct problems and pro-social behavior: Evidence from an Australian national sample. Environment and Child Well-Being. 2009;31(3):317–324. doi: 10.1016/j.childyouth.2008.08.005. [DOI] [Google Scholar]
- Ellis WR, Dietz WH. a new framework for addressing adverse childhood and community experiences: The building community resilience model. Academic Pediatrics. 2017;17(7S):S86–S93. doi: 10.1016/j.acap.2016.12.011. [DOI] [PubMed] [Google Scholar]
- Fan Y, Chen Q. Family functioning as a mediator between neighborhood conditions and children’s health: Evidence from a national survey in the United States. Social Science & Medicine (1982) 2012;74(12):1939–1947. doi: 10.1016/j.socscimed.2012.01.039. [DOI] [PubMed] [Google Scholar]
- Felitti VJ. Adverse childhood experiences and adult health. Academic Pediatrics. 2009;9(3):131–132. doi: 10.1016/j.acap.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Reprint of: relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 2019;56(6):774–786. doi: 10.1016/j.amepre.2019.04.001. [DOI] [PubMed] [Google Scholar]
- Flaherty EG, Thompson R, Dubowitz H, Harvey EM, English DJ, Proctor LJ, Runyan DK. Adverse childhood experiences and child health in early adolescence. JAMA Pediatrics. 2013;167(7):622–629. doi: 10.1001/jamapediatrics.2013.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Ford CL. Structural racism and health inequities. Du Bois Review : Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland AT, Palaniappan LP. Problems with the collection and interpretation of Asian-American health data: Omission, aggregation, and extrapolation. Annals of Epidemiology. 2012;22(6):397–405. doi: 10.1016/j.annepidem.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson DB, Posick C, Vaughn MG. New evidence of the nexus between neighborhood violence, perceptions of danger, and child health. Health Affairs. 2019;38(5):746–754. doi: 10.1377/hlthaff.2018.05127. [DOI] [PubMed] [Google Scholar]
- Jutte DP, Miller JL, Erickson DJ. Neighborhood adversity, child health, and the role for community development. Pediatrics. 2015;135(Suppl 2):S48–57. doi: 10.1542/peds.2014-3549F. [DOI] [PubMed] [Google Scholar]
- Kenney MK. Child, family, and neighborhood associations with parent and peer interactive play during early childhood. Maternal and Child Health Journal. 2012;16(Suppl 1):S88–101. doi: 10.1007/s10995-012-0998-7. [DOI] [PubMed] [Google Scholar]
- Kersten EE, Adler NE, Gottlieb L, Jutte DP, Robinson S, Roundfield K, LeWinn KZ. Neighborhood child opportunity and individual-level pediatric acute care use and diagnoses. Pediatrics. 2018 doi: 10.1542/peds.2017-2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier P, Maguire-Jack K, Lombardi B, Frey J, Rose RA. Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal. 2018;22(3):288–297. doi: 10.1007/s10995-017-2365-1. [DOI] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Haegerich TM, Simon T. Adverse childhood experiences increase risk for prescription opioid misuse. The Journal of Primary Prevention. 2020;41(2):139–152. doi: 10.1007/s10935-020-00578-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam RD. E pluribus unum: Diversity and community in the twenty-first century the 2006 Johan Skytte Prize Lecture. Scandinavian Political Studies. 2007;30(2):137–174. doi: 10.1111/j.1467-9477.2007.00176.x. [DOI] [Google Scholar]
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: A meta-analysis. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine. 2013;53(4 Suppl):S32–38. doi: 10.1016/j.jadohealth.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastav A, Richard CL, Kipp C, Strompolis M, White K. Racial/ethnic disparities in health care access are associated with adverse childhood experiences. Journal of Racial and Ethnic Health Disparities. 2020;7(6):1225–1233. doi: 10.1007/s40615-020-00747-1. [DOI] [PubMed] [Google Scholar]
- Srivastav A, Spencer M, Thrasher JF, Strompolis M, Crouch E, Davis RE. Addressing health and well-being through state policy: Understanding barriers and opportunities for policy-making to prevent adverse childhood experiences (ACEs) in South Carolina. American Journal of Health Promotion : AJHP. 2020;34(2):189–197. doi: 10.1177/0890117119878068. [DOI] [PubMed] [Google Scholar]
- Srivastav A, Strompolis M, Kipp C, Richard CL, Thrasher JF. Moderating the effects of adverse childhood experiences to address inequities in tobacco-related risk behaviors. Health Promotion Practice. 2020;21(1_suppl):139S–147S. doi: 10.1177/1524839919882383. [DOI] [PubMed] [Google Scholar]
- To T, Cadarette SM, Liu Y. Biological, social, and environmental correlates of preschool development. Child: Care, Health and Development. 2001;27(2):187–200. doi: 10.1046/j.1365-2214.2001.00182.x. [DOI] [PubMed] [Google Scholar]
- Turner, K., Wildsmith, E., Guzman, L., & Alvira-Hammond, M. (2016). The changing geography of hispanic children and families. National research center on hispanic children & families. https://www.hispanicresearchcenter.org/research-resources/the-changing-geography-of-hispanic-children-and-families/. Accessed 12 July 2020
- Turner, M., & Rawlings, L. (2009). Promoting neighborhodd diversity: Benefits, barriers, and strategies. Urban Institute. https://www.urban.org/sites/default/files/publication/30631/411955-Promoting-Neighborhood-Diversity-Benefits-Barriers-and-Strategies.PDF. Accessed 12 July 2020
- Ungar, M. (Ed.). (2012). The social ecology of resilience: A handbook of theory and practice. The Social Ecology of Resilience: A Handbook of Theory and Practice., xv, 463–xv, 463. 10.1007/978-1-4614-0586-3
- West Coast Poverty Center. (2010). Dialogues on Research and Policy: Ethnic Residential Clustering and Health in West Coast States. University of Washington. https://depts.washington.edu/wcpc/sites/default/files/wcpc/documents/dialogues/DIALOGUE%20No.%202.Ethnic%20Enclaves.webFN_.pdf. Accessed 12 July 2020
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports (washington: d.c.: 1974) 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Cooper LA. Reducing racial inequities in health: Using what we already know to take action. International Journal of Environmental Research and Public Health. 2019 doi: 10.3390/ijerph16040606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Cooper LA. Reducing racial inequities in health: Using what we already know to take action. International Journal of Environmental Research and Public Health. 2019;16(4):606. doi: 10.3390/ijerph16040606. [DOI] [PMC free article] [PubMed] [Google Scholar]


