Abstract
Two cases of pyogenic granulomas in burned skin were presented, a 17‐month‐old boy and a 7‐year‐old girl, being given oral propranolol and topical timolol. Both cases showed lesions improvement with no adverse effects, suggesting that beta‐blocker therapy may have a positive impact on the treatment of pyogenic granuloma after burns.
Keywords: beta‐blocker, burn, hemangioma, oral beta‐blocker, post‐burn hemangioma, post‐burn pyogenic granuloma, propranolol, pyogenic granuloma, therapy, timolol, topical beta‐blocker, treatment
Pyogenic granuloma (PG) is an uncommon complication of burned skin; most treatments are supportive or invasive. In our study, using beta‐blockers, oral and topical form, to treat post‐burn PG as a type of hemangioma were effective and safe.

What's already known about this topic?
Pyogenic granuloma or lobular capillary hemangioma is a benign vascular tumor of the skin that is common in adolescents and may be a complication of a burn. Invasive treatments for cutaneous hemangiomas such as laser, curettage, and minor surgery can lead to adverse effects such as ulceration and scarring that are uncomfortable and distress patients.
What does this study add?
Beta‐blockers affecting on cutaneous hemangiomas in oral and topical forms (oral propranolol and topical timolol in this study) could be consider as an effective treatment for post‐burn pyogenic granulomas without particular complications.
1. INTRODUCTION
A pyogenic granuloma (PG) or lobular capillary hemangioma is a benign vascular proliferation of the skin and mucous membranes. PG is a hyperproliferative vascular response to trauma, skin irritation, hormonal factors, viral pathogens, and growth factors that can develop on normal skin and cause tissue hypoxia and angiogenesis. 1 Pyogenic granuloma after a burn or scalded pyogenic granuloma is a variant of hemangioma that manifests within 2 to 4 weeks after a burn injury. As a result of the burn, intense and rapid vascularization of the skin and mucosa occurs, resulting in hemangioma‐like tissue. 2 Thermal, radiation, chemical, or electrical contact irritates the skin and causes burns of varying degrees, depending on the depth and severity of penetration. 3
Several treatment options are available for PG, including surgical removal, curettage and cauterization, laser, and topical imiquimod; however, these treatments are invasive and may be associated with pain, scarring, as well as other local side effects. 4 , 5 One of the treatments that may have fewer side effects for hemangiomas is beta‐blocker therapy. In addition, beta‐blockers have been shown to be an effective treatment for small PG, especially in children. 6 In this study, we describe two cases with second‐degree burns resulting hemangiomas. Both cases were treated with oral propranolol and topical timolol without any adverse effects.
2. CASES PRESENTATION AND TREATMENT METHODS
2.1. Case 1
A 17‐month‐old healthy boy was referred to the emergency department of Sina Hospital with a second‐degree burn from boiling water in the area behind the ears, anterior and posterior to the right elbow, and anterior to the left shoulder (18% burn). The child was admitted to the burn ward and underwent fluid therapy with normal saline, intravenous ampicillin, and dressing. It was discharged after 5 days in good general condition with a wound dressing. One month later, the child and his mother presented to the outpatient department of Sina Hospital with multiple eruptive red lesions on the periphery of the burn sites behind the left ear and on the right elbow (Figure 1A–C). The child had no history of congenital etiology. Initially, the child was treated with oral amoxicillin and a mupirocin dressing, which was not effective. On physical examination, we found numerous asymptomatic angiomatous papulonodular lesions with crusted surface on a hyperpigmented background. The lesion behind the left ear and the lesion at the elbow were 2 and 1 cm in size, respectively (Figure 1A,B). Based on the biopsy performed, a possible diagnosis of post‐burn pyogenic granuloma was made, propranolol was administered 5 mg orally twice a day and then the dosage was increased to 10 and15 mg every 3 days. In addition, 0.5% timolol drop was administered twice a day during oral propranolol administration. The child's blood pressure and heart rate were closely monitored within 2 h from the start of medication and were normal. 7 After 9 days, physical examination showed that the lesions had dramatically decreased (Figure 1D), so the treatments were discontinued.
FIGURE 1.

(A–C): Multiple post‐burn pyogenic granulomas specially behind the left ear and on the right elbow. (D): Significant improvement after a 9‐day treatment with oral propranolol and topical timolol.
2.2. Case 2
A 7‐year‐old healthy girl suffered a burn from boiling water on her face and was referred to the skin clinic at Sina Hospital. The second‐degree burn involved the left side of the face. Three weeks later, the mother brought the child with a swollen face and a 2‐cm lesion (Figure 2A,B). Examination of the lesion revealed a red, oozing plaque with a crusty surface that bled easily. The patient received 15 mg of oral propranolol (under supervision) and 0.5% topical timolol drop, both of them twice a day. At the first administration, the patient's blood pressure and heart rate were monitored for 2 h in the clinic, 7 which were normal and medication was continued as an outpatient. Three days later, the patient was referred again, the propranolol dose was increased to 20 mg twice a day, and the patient's blood pressure and heart rate continued to be monitored. After 2 weeks of treatment, the lesion had significantly regressed (Figure 2C), and only an atrophic scar remained after 6 months of follow‐up (Figure 2D).
FIGURE 2.
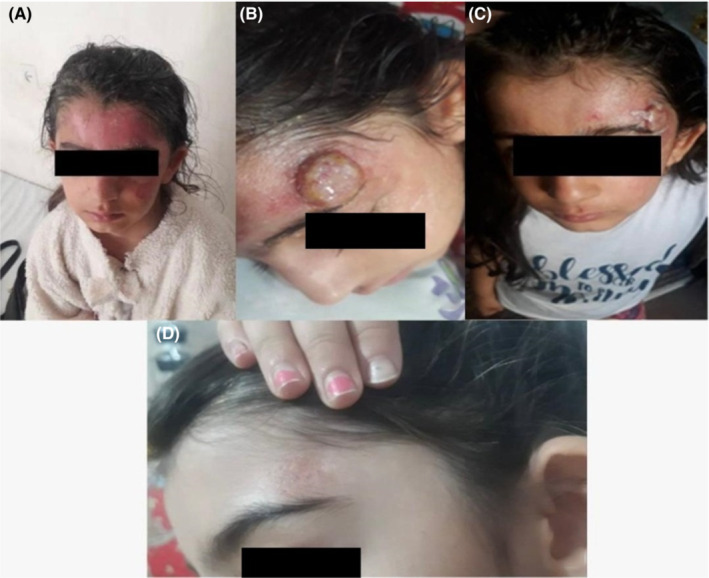
(A, B): A red, oozing pyogenic granuloma on the burned skin. (C): A dramatic reduction of the lesion after 2 weeks of treatment. (D): The lesion after treating with beta‐blockers and a 6‐month follow‐up.
3. DISCUSSION
This study described two cases that occurred after trauma to the skin from a burn. Both cases were treated with oral propranolol and topical timolol, which resulted in significant improvement.
The PG‐like or hemangioma‐like lesions after a burn can be triggered by hypoxia of the skin but can also occur in other situations such as chronic trauma or hormonal disorders. 8 Lesions may bleed and cause psychological distress to patients, especially lesions on the face; therefore, treatment of these benign tumors is a high priority. Various treatments for cutaneous hemangiomas (which are described in Table 1) may be invasive or have various adverse effects such as ulceration or scarring. Surgery is a common treatment, but it is invasive and may cause distress or pain, scarring, and, in some cases, nonresponse or recurrence. 9
TABLE 1.
Case reports and case series of post‐burn pyogenic granuloma based on a literature review
| Reference | Article type | Age/sex | Causing agent | Degree of burn | Latency (days) | Location | Effective treatment |
|---|---|---|---|---|---|---|---|
| De kaminsky et al. (1978) 17 | Case report | 15 months/Female | Boiling milk | Second | 7 | Arm, trunk, face | Electrocoagulation |
|
Momeni AZet al. (1995) 18 |
Case series (N = 3) | 1.5 years/Male | Boiling milk | Second | 14 | Trunk | Healed spontaneously after a period of 3 weeks. |
| 5 years/Female | Boiling milk | Second | 14 | Back, abdomen, high | Two of the lesions were electrocoagulated and the remainder healed spontaneously in 3 weeks | ||
| 35 years/Female | Boiling milk | Second | Nil | Face | Healed spontaneously after 4 weeks | ||
| Ceyhan et al. (1997) 19 | Case report | 18 months/Female | Boiling milk | Second | 15 | Arm, trunk, face | Excision |
| Aliagaoglu et al. (2006) 20 | Case report | 5 years/Female | Unknown | Second | 15 | Arm | Total excision and primary closure. |
| Bozkurt M, et al. (2006) 21 | Case report | 2 years/Male | Boiling milk | Second | 10 | Forearm | Excision |
| Liao et al. (2006) 22 | Case series (N = 2) | 41 years/Male | Scaling burn | Second | 10 | Forehead, cheek, lower jaw, forearm | Infusion of cefazolinum and topical application of mupirocin |
| 19 years/Male | Boiling water | Second | 9 | Back, face, upper limbs | Oral minocycline and topical application resulted in complete clearance | ||
| Diallo et al. (2006) 23 | Case series (N = 3) | 8 months/Male | Thermal burn | Second | 7–14 | Face, limbs | Self‐healing |
| 13 months/Male | Thermal burn | Second | 7–14 | Face, limbs | Self‐healing | ||
| 13 years/Male | Thermal burn | Second | 7–14 | Face, limbs | Self‐healing | ||
| Ceyhan AM et al. (2007) 24 | Case report | 17 months/Male | Boiling water | Second | 14 | Arm | Oral erythromycin, 40 mg/kg four times daily, was given for 8 weeks. The lesions clearly improved after 12 weeks of the treatment. |
| Ozbayoglu et al. (2011) 25 | Case report | 8 years/Male | Flame | Second | 21 | Trunk | Excision |
| Shirol et al. (2012) 26 | Case report | 42 years/Female | Unknown | Second | 30 | Chin | Surgical excision with split‐thickness skin graft |
| Durgun et al. (2013) 27 | Case series (N = 2) | 2 years/Female | Unknown | Second | 15 | Face, neck | Excised and fixed with a full thickness skin graft |
| 7 years/Male | Boiling water | Second | 14 | Forearm | Excised and primarily sutured | ||
| Netchiporouk et al. (2014) 28 | Case report | 17 years/Male | Lightning injury | Second and third | 14 | Face, chest, limbs | Surgical excision |
| Dastgheib et al. (2016) 29 | Case report | 12 months/Male | Boiling milk | Second | 14 | Lower limbs | Lost patient |
| Zhao et al. (2015) 30 | Case series (N = 5) | 4 years/Male | Scaling | Second | Nil | Face, neck | Conservative |
| 15 months/Male | Scaling | Second | Nil | Arm, hand | Conservative | ||
| 3 years/Male | Scaling | Second | Nil | Arms | Conservative | ||
| 26 months/Female | Scaling | Second | Nil | Back, buttocks | Conservative | ||
| 2 years/Female | Scaling | Second | Nil | Hand | Conservative | ||
| Xu et al. (2016) 31 | Case report | 4 years/Female | Boiling soup | Second | 13 | Arm | Sodium fusidic ointment and compound Huangbo solution (Chinese herbal medicine) were applied topically twice daily for 4 weeks |
| Khalifa E et al. (2017) 13 | Case series (N = 6) | 9 months/Male | Boiling tea | Second | 10 | Abdomen | Lost patient |
| 10 months/Male | Boiling tea | Second | 12 | Foot | Oral propranolol at a dose of 5 mg twice daily for 2 weeks | ||
| 25 years/Female | Thermaldermabration | Nil | Nil | Cheek | Supportive therapy like topical and systemic ointment within 2 weeks. | ||
| 3 years/Male | Boiling tea | Second | Nil | Lower limb | Propranolol therapy for 2 weeks | ||
| 7 years/Female | Boiling tea | Second | Nil | Lower limbs | Lost patient | ||
| 2.5 years/Male | Boiling soup | Second | 10 | Abdomen, lower limb | Oral propranolol 10 mg with topical potassium permanganate solution given but lost follow‐up. | ||
| Ashk Torab et al. (2018) 32 | Case report | 15 months/Female | Boiling water | Second | 10 | Trunk | Conservative (herbal treatment) |
| Staggers JR et al. (2019) 33 | Case report | 29 years/Male | Unknown | Nil | 14 | Finger | Silver nitrate therapy was ineffective, though surgical excision resulted in complete resolution of the mass. |
| Rosa‐Mangeret F et al. (2020) 34 | Case report | premature neonate/Female | Transcutaneous CO2 | First | 24 | Thigh | Topical beta‐blocker (Timolol gel) |
| Krieger Y et al. (2020) 35 | Case report | 17 months/Male | Boiling water | Second | 21 | Forearm and arm | Excision and skin grafting |
| Iraji, et al. (2020) 36 | Case report | 30 years/Female | Oil | Third | 28 | Forearm | The excision of the lesions followed by electrosurgery of the base |
| Keshavarzi A et al. (2021) 37 | Case report | 49 years/Female | Boiling water | Nil | 14 | Hand | Full thickness skin excision and debridement and skin graft |
| Sharquie KE et al. (2022) 38 | Case series (N = 34) | mean age: 17.6 years and median age: 3.5 years/16 Female, 18 Male | Boiling liquids, Fire flame | Second‐ and combined second‐ and third‐degree | 7–14 | Scalp in two cases, trunk in six cases, upper limbs in eight cases, and lower limbs in 15 cases | Nil |
In this study, we found that we can treat hemangiomas in children with a series of oral and topical beta‐blockers, which appear to be an attractive option for disease management and maybe effective in treating wounds, ulcers, and proliferative vascular lesions based on their physiopathology and with a few side effects. In addition, recent studies have reported that beta‐blocker therapy has a significant effect on wound healing and infantile hemangioma. 10 , 11
PG Lesions similar to infantile hemangioma have been discovered to express beta‐adrenergic receptors. 12 Some studies have used oral and topical beta‐blockers such as propranolol, timolol, and betaxolol to treat PG, which are described in Table 1. In a study by Khalifa E et al., oral propranolol was used for 2 weeks to treat post‐burn pyogenic granulomas of two cases, which proved successful. 13
Consensus guidelines exist for initiating and monitoring treatment with propranolol but are extremely variable. 7 The mechanism of action of beta‐blockers, particularly propranolol and timolol, is not fully understood. However, inhibition of angiogenesis, blockade of beta‐2‐adrenergic vasodilator nerves of the skin, and induction of apoptosis of capillary endothelial cells have been proposed as mechanisms. 14 , 15 , 16 Contraindications to oral propranolol for burn hemangioma are similar to those for infantile hemangioma and include the following: cardiogenic shock, sinus bradycardia, hypotension, greater than first‐degree heart block, heart failure, bronchial asthma, and hypersensitivity to propranolol. 7
We also reviewed 23 studies that included 71 cases of post‐burn PG (Table 1). More than 60 patients from previous studies suggest that the lesion is more likely to develop in children, so it logically needs to be approached more conservatively with noninvasive, effective, and safe treatments, making beta‐blockers a good choice, and current ones are particularly interesting in this regard.
4. CONCLUSION
Beta‐blockers in systemic and local forms could be consider as an effective treatment options for scalded PG, and with minimal complications, they may replace invasive procedures such as surgical excision in the future.
AUTHOR CONTRIBUTIONS
ZE and AG designed the research, wrote and edited the paper, and edited the manuscript. ZM, AAK, EB, and AGZ identified and treated the cases. ZE, AD and AG supervised the study, and wrote the manuscript. All authors have read and approved the content of the article.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
CONSENT
Written informed consent was obtained from the patients' legal guardians to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
The authors would like to express their gratitude to the staff of Sina Hospital, and Rasool Akram Medical Complex Clinical Research Development Center (RCRDC) and Mrs Farahnaz Nikkhah for their technical and editorial assistance.
Ebrahimi Z, Mahdi Z, Khairi AA, et al. Oral propranolol and topical timolol in the treatment of post‐burn pyogenic granuloma: Two cases and a review of the literature. Clin Case Rep. 2022;10:e06538. doi: 10.1002/ccr3.6538
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Supekar BB, Wankhade VH, Chopkar AD, Singh RP, Bhat D. Multiple erythematous nodules: an intriguing entity. Indian Dermatol Online J. 2021;12(1):142‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Harris M, Desai R, Chuang TY, Hood AF, Mirowski GW. Lobular capillary hemangiomas: an epidemiologic report, with emphasis on cutaneous lesions. J Am Acad Dermatol. 2000;42(6):1012‐1016. [PubMed] [Google Scholar]
- 3. Ball RL, Keyloun JW, Brummel‐Ziedins K, et al. Burn‐induced coagulopathies: a comprehensive review. Shock. 2020;54(2):154‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee J, Sinno H, Tahiri Y, Gilardino MS. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011;64(9):1216‐1220. [DOI] [PubMed] [Google Scholar]
- 5. Giblin AV, Clover AJP, Athanassopoulos A, Budny PG. Pyogenic granuloma–the quest for optimum treatment: audit of treatment of 408 cases. J Plast Reconstr Aesthet Surg. 2007;60(9):1030‐1035. [DOI] [PubMed] [Google Scholar]
- 6. Kim JH, Lam JM. Paediatrics: how to manage infantile haemangioma. Drugs Context. 2021;10:2020‐12‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Drolet BA, Frommelt PC, Chamlin SL, et al. Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics. 2013;131(1):128‐140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arany Z, Foo SY, Ma Y, et al. HIF‐independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC‐1α. Nature. 2008;451(7181):1008‐1012. [DOI] [PubMed] [Google Scholar]
- 9. Dinehart SM, Kincannon J, Geronemus R. Hemangiomas: evaluation and treatment. Dermatol Surg. 2001;27(5):475‐485. [DOI] [PubMed] [Google Scholar]
- 10. Goodarzi A, Mozafarpoor S, Dodangeh M, Seirafianpour F, Shahverdi MH. The role of topical timolol in wound healing and the treatment of vascular lesions: a narrative review. Dermatol Ther. 2021;34(2):e14847. [DOI] [PubMed] [Google Scholar]
- 11. Ghassemi M, Shahverdi MH, Behrangi E, Hosseini‐Baharanchi FS, Goodarzi A. Efficacy and safety of topical timolol 0.5% plus saline 0.9% versus each one alone in acne scar trichloroacetic acid‐CROSS therapy: a blinded randomized controlled trial. Dermatol Ther. 2022;35(4):e15341. [DOI] [PubMed] [Google Scholar]
- 12. Chen Y, Bai N, Bi JH, et al. Propranolol inhibits the proliferation, migration and tube formation of hemangioma cells through HIF‐1α dependent mechanisms. Braz J Med Biol Res. 2017;50:e6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharquie KE, Noaimi AA, Radhi SK. Burn Hemangioma (BH) (scalded pyogenic granuloma) versus infantile hemangioma: report of six cases of bh and its effective therapy with oral propranolol. J Cosmetics Dermatol Sci Appl. 2017;7(3):229‐244. [Google Scholar]
- 14. Storch C, Hoeger P. Propranolol for infantile haemangiomas: insights into the molecular mechanisms of action. Br J Dermatol. 2010;163(2):269‐274. [DOI] [PubMed] [Google Scholar]
- 15. Prabha N, Chhabra N, Arora R. Beta‐blockers in dermatology. Indian J Dermatol Venereol Leprol. 2017;83(3):399. [DOI] [PubMed] [Google Scholar]
- 16. Solman L, Glover M, Beattie PE, et al. Oral propranolol in the treatment of proliferating infantile haemangiomas: British Society for Paediatric Dermatology consensus guidelines. Br J Dermatol. 2018;179(3):582‐589. [DOI] [PubMed] [Google Scholar]
- 17. de Kaminsky AR, Otero AC, Kaminsky CA, Shaw M, Formentini E. Multiple disseminated pyogenic granuloma. Br J Dermatol. 1978;98(4):461‐464. [DOI] [PubMed] [Google Scholar]
- 18. Momeni AZ, Enshaieh S, Sodifi M, Aminjawaheri M. Multiple giant disseminated pyogenic granuloma in three patients burned by boiling milk. Int J Dermatol. 1995;34(10):707‐710. [DOI] [PubMed] [Google Scholar]
- 19. Ceyhan M, Erdem G, Kotiloḡlu E, et al. Pyogenic granuloma with multiple dissemination in a burn lesion. Pediatr Dermatol. 1997;14(3):213‐215. [DOI] [PubMed] [Google Scholar]
- 20. Aliağaoğlu C, Bakan V, Atasoy M, Toker S. Pyogenic granuloma with multiple and satellite involvement after a burn in a 5‐year‐old child. J Dermatol. 2006;33(2):150‐152. [DOI] [PubMed] [Google Scholar]
- 21. Bozkurt M, Külahç Y, Zor F, Aşkar İ. Multiple giant disseminated pyogenic granuloma in a burn lesion. J Burn Care Res. 2006;27(2):247‐249. [DOI] [PubMed] [Google Scholar]
- 22. Liao W‐J, Fan PS, Fu M, Gao TW, Liu YF, Ikeda S. Clinicopathological and ultrastructural study of multiple lobular capillary hemangioma after scalding. Dermatology. 2006;213(1):34‐36. [DOI] [PubMed] [Google Scholar]
- 23. Diallo M, Niang S, Kane A, Dieng M, Ndiaye B. Pyogenic granulomas with multiple satellites spontaneously resolved. Nouvelles Dermatologiques. 2006;25(10):701. [Google Scholar]
- 24. Ceyhan AM, Basak PY, Akkaya VB, Yildirim M, Kapucuoglu N. A case of multiple, eruptive pyogenic granuloma developed on a region of the burned skin: can erythromycin be a treatment option? J Burn Care Res. 2007;28(5):754‐757. [DOI] [PubMed] [Google Scholar]
- 25. Ozbayoglu AC, Aksungur E, Senem A. Pyogenic granuloma developed in a healed flame burn area and review of the literature: case report. Turkish J Plastic Surg. 2011;19(1):27‐29. [Google Scholar]
- 26. Shirol S, Nimbaragi G, Choukimath SM, Yenni VV. Lobular capillary hemangioma in a post‐burn scar. Eur J Plast Surg. 2013;36(5):323‐326. [Google Scholar]
- 27. Durgun M, Selçuk CT, Ozalp B, Aydinol M, Alabalik U. Multiple disseminated pyogenic granuloma after second degree scald burn: a rare two case. Int J Burns Trauma. 2013;3(2):125‐129. [PMC free article] [PubMed] [Google Scholar]
- 28. Netchiporouk E, Moreau L, Ramirez LP, et al. Eruptive disseminated pyogenic granulomas following lightning injury. Dermatology. 2015;230(3):199‐203. [DOI] [PubMed] [Google Scholar]
- 29. Dastgheib L, Maghami Z, Aslani FS. Infantile multiple large pyogenic granuloma on burned skin. Case report and review of literature. An Bras Dermatol. 2016;91:212‐214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zhao H, Zhao H, Zhang C, Fu X. Multiple pyogenic granulomas after burns: response to conservative treatment in five children. Pediatr Dermatol. 2015;32(4):e175‐e176. [DOI] [PubMed] [Google Scholar]
- 31. Xu Y, Li H, Wang ZX, Yang S. Multiple eruptive pyogenic granulomas occurring in a region of scalded skin. Pediatr Dermatol. 2016;33(1):e27‐e28. [DOI] [PubMed] [Google Scholar]
- 32. Ashk Torab T, Tahereh A, Camelia R. Disseminated pyogenic granuloma without surgical intervention: a case report. Adv Nursing Patient Care Int J. 2018;1(1):180004. [Google Scholar]
- 33. Staggers JR, Pearson JM, Chaudhari NM. Capillary hemangioma of the finger in an adult after a burn: a unique case mimicking pyogenic granuloma. J Orthopaedic Case Rep. 2019;9(1):3‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rosa‐Mangeret F, Calza AM, Pfister RE, Barcos‐Munoz F. Post‐burn infantile hemangioma in an extremely premature neonate. Biomed Hub. 2020;5(2):1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Krieger Y, Weiss E, Horev A, Melamed R, Shoham Y. Multiple large pyogenic granulomas overlying a burn: case report and literature review. J Clin Cosmet Dermatol. 2020;4(3). doi: 10.16966/2576-2826.155 [DOI] [Google Scholar]
- 36. Iraji F, Jelvan M, Ganjei Z, Rajabi P. Multiple disseminated pyogenic granuloma post–oil burning—review literature. Clin Case Rep. 2021;9(1):169‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Keshavarzi A, Dahmardehei M, Emami A, Ghadimi T, Bouzari B. Management of pyogenic granulomas following burn wounds. World J Plastic Surg. 2021;10(3):117‐120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sharquie KE, al‐Dhalimi MA, Kawen AA, Dhaher SA. Burn hemangioma: a new variant of hemangioma. Dermatology. 2022;238(4):1‐6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


