Abstract
Introduction
Children with long-term physical health conditions (pLTCs) are at increased risk of mental health conditions but less is known about time trends in the mental health of this group of children.
Methods
We used data from three comparable, population-based surveys of children conducted in 1999, 2004, and 2017. We examined whether the proportion of children aged 5–15 years old with comorbid mental health conditions (measured using the multi-informant Development and Well-being Assessment tool) and pLTCs (measured using parental report) in England increased from 1999 to 2017 using linear regression analysis.
Results
Our analysis used data from 8662 (1999), 6401 (2004) and 6219 (2017) children, respectively. The proportion of children with comorbid pLTCs and psychiatric disorders was 0.050 (95% CI = 0.045, 0.055) in 1999, 0.054 (95% CI = 0.049, 0.060) in 2004, and 0.059 (95% CI = 0.053, 0.065) in 2017. The linear regression model revealed a non-significant effect of time on the proportion of children with comorbid pLTCs and psychiatric disorders from 1999 to 2017 (B = 0.0004785; SE = 0.0001256; p = 0.163).
Conclusion
The estimated prevalence of school-aged children with comorbid pLTCs and mental health conditions in England remained stable since 1999, highlighting the need to prioritize mental health resources for children with physical health comorbidities.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00787-022-02112-5.
Keywords: Trends, Long-term physical health conditions, Mental health conditions, Comorbitidy
Introduction
Globally, there is an increased focus on the importance of children and young people’s (CYP) mental health [1]; however, less is known about the mental health of CYP with long-term physical health conditions (pLTCs) over time. Research indicates that the risk of having a mental health disorder is two–four times greater in children with pLTCs as compared to their physically healthier counterparts [2]. Untreated mental health conditions in pediatric patients are linked with suboptimal disease management [3], negative health outcomes [4, 5], increased hospitalization stay, and costs compared to peers without a mental health comorbidity [6, 7]. Therefore, there is an urgent need to estimate and respond to the mental health needs of young patients with mental health disturbances.
Studies of clinical samples reflect only those who are in contact with services and whose mental health condition has been detected. An understanding of the level of comorbid pLTCs and poor mental health in all CYP using robust, population-based data is essential for health care provision planning and commissioning, as well as development of health policy. However, no population-based studies have investigated time trends in comorbid pLTCs and mental health conditions in CYP. We aimed to examine whether the proportion of CYP with comorbid mental health conditions and pLTCs in England increased from 1999 to 2017 using population-based, national surveys.
Methods
Participants
We used data from the British Child and Adolescent Mental Health Surveys and the Mental Health of Children and Young People in England Survey. These are cross-sectional, population-based surveys of CYP conducted in 1999, 2004, and 2017. The 1999 (age 5–15 years; Great Britain) and 2004 (age 5–16 years; Great Britain) samples were drawn from the Child Benefit Register. The 2017 sample (age 2–19 years; England) was drawn from the NHS Patient Register, as Child Benefit was no longer universal. A detailed description of all three surveys is reported elsewhere [8]. The 1999 and 2004 data are publicly available via the UK Data Service (references 4227 and 5269, respectively), and the 2017 data were accessed via NHS Digital’s Data Access Request Service (DARS, reference DARS-NIC-424336-T7K7T-v0.6). The original surveys were approved by Research Ethics Committees [9, 10], while the University of Cambridge Ethics Committee does not require applications for secondary data analysis. Informed consent was obtained from legal guardians (for children < 11 years old) and from adolescent participants.
In all three surveys, data were collected from parents (94% from the biological mothers), children (aged ≥ 11 years), and teachers (the family nominated the teacher who knew the child best). Parents and CYP were interviewed face-to-face by trained lay interviewers using computer-assisted interviews, with self-reported questionnaires completed for sensitive topics. Teachers responded to a mailed questionnaire. To increase the comparability between the three surveys, we included children from England only (excluded n = 2514) aged 5–15 years old (excluded n = 3502). Participants with incomplete data on study measures were also excluded (n = 234).
Measures
Mental health conditions were measured using the validated Development and Well-being Assessment [11], a standardized diagnostic tool that combines highly structured and semi-structured questions about psychiatric disorders, based on the International Classification of Diseases-10 (ICD-10) criteria [12]. The DAWBA incorporated information from parents (via interview), CYP (via interview), and teachers (via questionnaire). Computer-generated predictions of disorders were produced and reviewed by trained clinicians (including co-authors TF and TND) who assigned diagnoses based on ICD-10 criteria [12]. The DAWBA covered the following: (emotional disorders [separation anxiety disorder, specific phobia, social phobia, panic disorder, agoraphobia, post-traumatic stress disorder, obsessive compulsive disorder, generalized anxiety disorder, other anxiety disorder, depressive episode, other depressive episode], hyperactivity disorders [hyperkinetic disorder, other hyperactivity disorder], conduct disorders [oppositional defiant disorder, conduct disorder confined to family, unsocialized conduct disorder, socialized conduct disorder, other conduct disorder], less common psychiatric disorders [autistic spectrum disorder, tic disorder, eating disorder, selective mutism, psychosis]).
pLTCs were assessed using parent report on whether the child has any of the following conditions at the time of assessment (yes/no): asthma, eczema, hayfever, epilepsy, cerebral palsy, muscle disease, coordination problems, heart problems, food allergy, kidney/urinary tract problems, a condition present since birth (e.g., club foot or cleft palate), deformities, spina bifida, cystic fibrosis, blood disorders, missing limb(s), diabetes, cancer, vision problems, hearing problems. This selection was based on the consensus definition of chronic health conditions in childhood [13] and discussion with our Study Steering Committee.
Statistical analysis
We estimated the population prevalence of CYP with comorbid pLTCs and mental health conditions in 1999, 2004, and 2017. We also estimated the population prevalence of children without identified pLTCs or mental health conditions (healthy group), with pLTCs but no mental health conditions, and with mental health conditions but no pLTCs at the three time points. Prevalence analyses used survey weighting (provided by the three national surveys) to account for selection and non-response bias [8]. Not all teachers responded to the mailed questionnaire [14]; For the 2017 survey, weighting does not fully adjust for the teacher report sub-sample. Nevertheless, applying the teacher adjustment factor, provided for the group of children with mental health conditions [14], had minimal impact relative to our estimated 95% Confidence Interval (CI). Given that the teacher adjustment factor is provided for children with mental health conditions and it is not broken down for our sub-groups (children with pLTCs only, children with mental health conditions only, children with comorbid pLTCs and mental health conditions, healthy children), by applying this factor would not give correct estimates.
In the sub-group of children with comorbid pLTCs and mental health conditions, we undertook linear regression analysis to test for a linear trend in survey weighted prevalence across the three surveys (the trend analysis was weighted by the standard errors for each survey to account for uncertainty in the estimates). In sensitivity analyses, we examined whether there were significant changes in the proportion of children with comorbidities by including the whole Great Britain sample (the 1999 and 2004 surveys included children from Scotland and Wales, while the 2017 survey only sampled from England). Analyses were carried out in STATA 17.0 and R programming language.
Results
Our analysis used data from 8,662 (1999), 6,401 (2004) and 6,219 (2017) CYP from England. The proportion of children with comorbid pLTCs and mental health conditions was 0.050 (95% CI = 0.045, 0.055) in 1999, 0.054 (95% CI = 0.049, 0.060) in 2004, and 0.059 (95% CI = 0.053, 0.065) in 2017. Figure 1 illustrates the weighted prevalence estimates of CYP in the four study groups at the three time points. Prevalence estimates indicated an increase in the proportion of CYP with neither pLTCs or mental health conditions, and a corresponding decrease in the proportion of CYP with pLTCs. Additionally, we showed an increase in the proportion of CYP with mental health conditions and in those with comorbid pLTCs and mental health conditions from 1999 to 2017. Weighted prevalence estimates and 95% CIs for the four study groups are reported in supplementary Table 1.
Fig. 1.
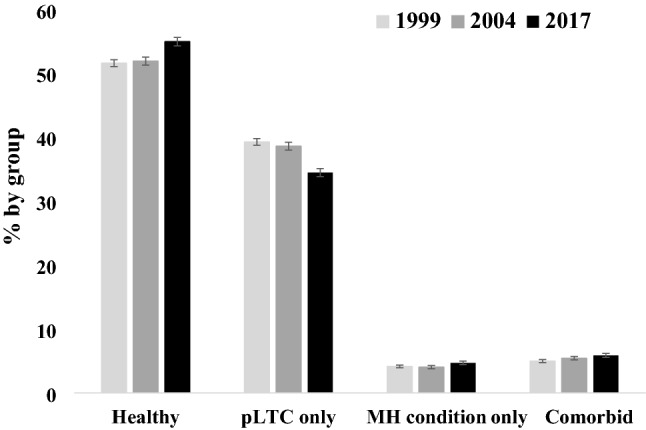
Weighted prevalence estimates of long-term physical health conditions and mental health conditions in children and young people aged 5–15 years in England in 1999 (N = 8662), 2004 (N = 6401), and 2017 (N = 6219) by group. Error bars represent standard errors. MH = mental health; pLTC = long-term physical health condition
The linear regression model revealed a non-significant effect of time on the proportion of CYP with comorbid pLTCs and mental health conditions from 1999 to 2017 [B = 0.0004785; SE = 0.0001256; p = 0.163 (Fig. 2)]. Repeating the analyses including the whole Great Britain sample (see supplementary Table 2 for the weighted prevalence estimates) showed a significant increase in the proportion of CYP with comorbid conditions from 1999 to 2017 (B = 0.0006; SE = 0.00000312; p = 0.003).
Fig. 2.
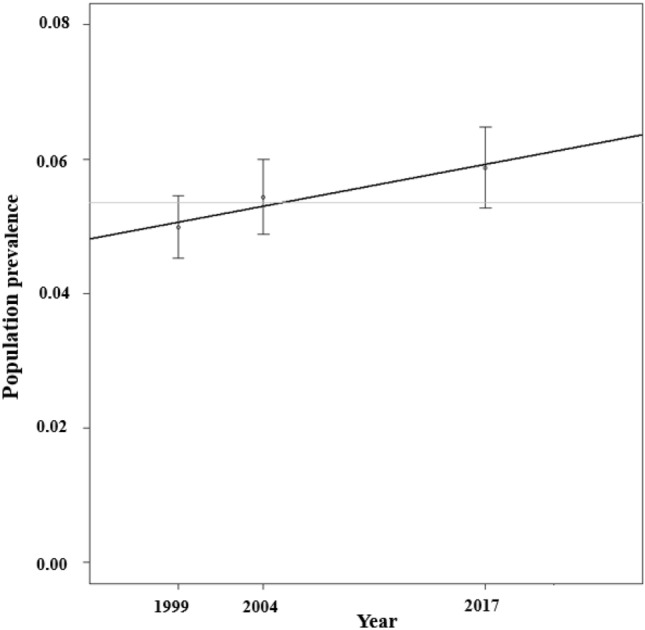
Prevalence estimates of comorbid long-term physical health conditions and mental health conditions in children and young people aged 5–15 years in England from 1999 to 2017
Discussion
To our knowledge, this is the first population-based study to investigate changes in the proportion of CYP with comorbid pLTCs and mental health conditions. Despite the falling prevalence rate of pLTCs, we detected an upward trend (albeit not significant) in comorbid pLTCs and mental health conditions between 1999 and 2017, which is expected given that previous studies suggested a deterioration in the mental health of CYP in the UK during this time [15–17]. We would predict that these rates may well have worsened since 2017, given the effects of Covid-19 pandemic on the mental and physical [18] health of school-aged children [19, 20]. When the analyses were broadened to include CYP from Great Britain, a significant upward trend in the proportion of CYP with comorbid conditions was observed, which may suggest a lower prevalence of comorbid pLTCs and mental health conditions in Scotland and Wales compared to England. We could not directly test this hypothesis as the 2017 survey did not recruit Scottish or Welsh participants. It is also possible that the smaller sample size in England-only analyses reduced the power to detect a change, particularly as so few participants were identified with comorbidities at each time point. Nevertheless, together these findings suggest that CYP with mental health problems have seen no improvements in health over time comparable to the reduction in pLTCs; hence, health disparities are widening. Future studies using larger samples should explore which specific mental health conditions are the most common in CYP with pLTCs, as well as investigate mediators of the presence of comorbid conditions.
Our findings emphasize the need for more effective strategies to identify and support CYP with poor mental health. Combined with the reduction in pLTCs, our study suggests that CYP with physical health needs access support more effectively than CYP with mental health needs; we have yet to obtain ‘parity of esteem’. To halve the number of children with persistent mental health problems, which is the first of the shared goals as stated by the Department of Health and Social Care [21], the identification of problems is required. Even though CYP with poor physical health are in regular contact with primary and secondary health care, which provides opportunities for the identification of symptoms, mental health conditions are often missed [22]. We recently found that CYP with comorbid pLTCs and mental health conditions are more often in contact with primary health care and pediatricians for their mental health than specialist mental health services [Under review]. However, pediatricians only identify a quarter of all cases with a possible psychiatric disorder [22]. Timely delivery of treatment is also critical to prevent mental health conditions from becoming entrenched, yet children waited for a mean of 2 months pre-pandemic for specialist mental health assessment, with many children still not accepted onto waiting lists [23]. This is double the UK government’s 4-week target [24], suggesting that services are overstretched and under-resourced. Improving practitioners’ specific knowledge on childhood mental health conditions as well as introducing routine mental health screening in primary and secondary health care settings could be beneficial [25]. Brief and/or low-intensity (< 6 sessions) psychological interventions based on cognitive behavioral principles [26] have demonstrated the potential to benefit young people with [27] and without [28, 29] a pLTC. These interventions could be delivered at drop-in centers [30], which could be in primary or secondary health care, or at schools [31], to increase access to evidence-based therapy for CYP and their families.
Our analysis benefits from three robust and comparable single-phase, population-based surveys with rigorous mental health assessment using the same measure in each survey. Many previous surveys have used self-/parent report of mental health conditions [32] instead of a multi-informant standardized diagnostic assessment. If a standardized diagnostic assessment is used, surveys often use a two-phase approach with a simple screen initially administered [33], rather than the detailed, one-phase approach in those analyzed here (where each participant had the diagnostic assessment). The survey data we analyzed covered both children and adolescents whereas other similar studies have involved either children only [34] or adolescents only [35]. However, the lengthy gap between 2004 and 2017 assessments may have masked interim time trends. Given the design of the survey, it was not possible to collect objective medical data; thus, pLTCs were parent reported and we lack data on disease severity. Given the likely impact of the COVID-19 pandemic and resulting restrictions, a more recent survey to assess the current level of needs is essential, and we would argue that our estimate is necessarily an underestimate.
In conclusion, the proportion of CYP with comorbid pLTCs and mental health conditions in England remained stable since 1999, highlighting the need to prioritize mental health resources for CYP with physical health comorbidities as they are a particularly vulnerable group.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the Young Persons Advisory Group based at the Great Ormond Street Hospital for providing input to the study from a patient’s point of view. We thank Dr Birgit Westphal, Professor Elena Garralda, Dr Nancy Bostock, and Professor Russell Viner for providing input to the study from an expert’s point of view.
Author contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by LP and TN-D. The first draft of the manuscript was written by LP and all authors commented on previous versions. All authors read and approved the final manuscript.
Funding
This research was funded by the Beryl Alexander Charity. Professor Tamsin Ford is funded by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Dr Tamsin Newlove-Delgado is funded by an NIHR Advanced Fellowship (NIHR300056). Dr Sophie Bennett and Professor Roz Shafran are funded by the NIHR Great Ormond Street Hospital Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the National Health System, the NIHR or the Department of Health and Social Care.
Data availability
The 1999 and 2004 data are available via application to the UK Data Service (references 4227 and 5269, respectively). The 2017 data are available via NHS Digital’s Data Access Request Service (DARS, reference DARS-NIC-424336-T7K7T-v0.6).
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The original surveys were approved by Research Ethics Committees, while the University of Cambridge Ethics Committee does not require applications for secondary data analysis.
Consent to participate
Informed consent was obtained from legal guardians (for children < 11 years old) and from young participants.
References
- 1.Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. The Lancet. 2018;392:1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 2.Finning K, NeochoritiVarvarrigou I, Ford T, Panagi L, Ukoumunne OC. Mental health and school absenteeism in children with long-term physical conditions: a secondary analysis of the British child and adolescent mental health surveys 2004 and 2007. Child Care Health Dev. 2022;48:110–119. doi: 10.1111/cch.12910. [DOI] [PubMed] [Google Scholar]
- 3.Sildorf SM, Breinegaard N, Lindkvist EB, Tolstrup JS, Boisen KA, Teilmann GK, et al. Poor metabolic control in children and adolescents with type 1 diabetes and psychiatric comorbidity. Diabetes Care. 2018;41:2289–2296. doi: 10.2337/dc18-0609. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EK, Jones JE, Seidenberg M, Hermann BP. The relative impact of anxiety, depression, and clinical seizure features on health-related quality of life in epilepsy. Epilepsia. 2004;45:544–550. doi: 10.1111/j.0013-9580.2004.47003.x. [DOI] [PubMed] [Google Scholar]
- 5.Olusunmade M, Qadir T, Akyar S, Farid A, Aggarwal R. Incremental hospital utilization and mortality associated with co-morbid depression in pediatric hospitalizations. J Affect Disord. 2019;251:270–273. doi: 10.1016/j.jad.2019.03.073. [DOI] [PubMed] [Google Scholar]
- 6.Ansari H, Santiago-Jiménez M, Saab H, De Souza C, Szatmari P, Monga S. Association between comorbid psychiatric disorders and hospital resource use in physically Ill pediatric inpatients: a case-matched analysis. J Am Acad Child Adolesc Psychiatry. 2021;60:346–354. doi: 10.1016/j.jaac.2020.07.889. [DOI] [PubMed] [Google Scholar]
- 7.Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Psychiatric disorders and trends in resource use in pediatric hospitals. Pediatrics. 2016;138:e20160909. doi: 10.1542/peds.2016-0909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford T, Vizard T, Sadler K, McManus S, Goodman A, Merad S, et al. Data resource profile: mental health of children and young people (MHCYP) surveys. Int J Epidemiol. 2020;49:363–364g. doi: 10.1093/ije/dyz259. [DOI] [PubMed] [Google Scholar]
- 9.Green H, McGinnity Á, Meltzer H, Ford T, Goodman R. Mental health of children and young people in Great Britain, 2004. London: Palgrave Macmillan Basingstoke; 2005. [Google Scholar]
- 10.Vizard T, Sadler K, Ford T, Merad S, Brodie E, Forbes N, et al (2018) Mental Health of Children and Young People in England, 2017. Survey Design and Methods Report. https://dera.ioe.ac.uk/32622/11/MHCYP%202017%20Survey%20Design%20and%20Methods.pdf. Accessed 21 March 2022
- 11.Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–655. doi: 10.1111/j.1469-7610.2000.tb02345.x. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organizations (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization
- 13.Mokkink LB, Van der Lee JH, Grootenhuis MA, Offringa M, Heymans HS. Defining chronic diseases and health conditions in childhood (0–18 years of age): national consensus in the Netherlands. Eur J Pediatr. 2008;167:1441–1447. doi: 10.1007/s00431-008-0697-y. [DOI] [PubMed] [Google Scholar]
- 14.NHS Digital (2017) Mental Health of Children and Young People in England, 2017. Survey Design and Methods Report. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2017/2017. Accessed 27 October 2022
- 15.Pitchforth JM, Viner RM, Hargreaves DS. Trends in mental health and wellbeing among children and young people in the UK: a repeated cross-sectional study, 2000–14. The Lancet. 2016;388:S93. doi: 10.1016/S0140-6736(16)32329-7. [DOI] [Google Scholar]
- 16.McManus S, Gunnell D, Cooper C, Bebbington PE, Howard LM, Brugha T, et al. Prevalence of non-suicidal self-harm and service contact in England, 2000–14: repeated cross-sectional surveys of the general population. The Lancet Psychiatry. 2019;6:573–581. doi: 10.1016/S2215-0366(19)30188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sadler K, Vizard T, Ford T, Marchesell F, Pearce N, Mandalia D, et al (2018) Mental health of children and young people in England, 2017. Summary of key findings. https://dera.ioe.ac.uk/32622/1/MHCYP%202017%20Summary.pdf. Accessed 21 March 2022
- 18.Rahman AM, Chandrasekaran B. Estimating the impact of the pandemic on children's physical health: a scoping review. J Sch Health. 2021;91:936–947. doi: 10.1111/josh.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ford T, John A, Gunnell D. Mental health of children and young people during pandemic. BMJ. 2021;372:n765. doi: 10.1136/bmj.n765. [DOI] [PubMed] [Google Scholar]
- 20.Newlove-Delgado T, McManus S, Sadler K, Thandi S, Vizard T, Cartwright C, et al. Child mental health in England before and during the COVID-19 lockdown. The Lancet Psychiatry. 2021;8:353–354. doi: 10.1016/S2215-0366(20)30570-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wykes T, Bell A, Carr S, Coldham T, Gilbody S, Hotopf M, et al (2021) Shared goals for mental health research: What, why and when for the 2020s. J Ment Health:1–9. 10.1080/09638237.2021.1898552 [DOI] [PubMed]
- 22.Glazebrook C, Hollis C, Heussler H, Goodman R, Coates L. Detecting emotional and behavioural problems in paediatric clinics. Child Care Health Dev. 2003;29:141–149. doi: 10.1046/j.1365-2214.2003.00324.x. [DOI] [PubMed] [Google Scholar]
- 23.de Souza R (2022) Briefing on Children’s Mental Health Services – 2020/2021. https://www.childrenscommissioner.gov.uk/report/briefing-on-childrens-mental-health-services-2020-2021/. Accessed 21 March 2022
- 24.Whitney C-J, Hutchinson J (2020). Access to child and adolescent mental health services in 2019. 2020. https://dera.ioe.ac.uk/34811/1/Access-to-CAMHS-in-2019_EPI.pdf Accessed 21 March 2022
- 25.Ogundele MO. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World J Clin Pediatr. 2018;7:9–26. doi: 10.5409/wjcp.v7.i1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shafran R, Myles-Hooton P, Bennett S, Öst L-G. The concept and definition of low intensity cognitive behaviour therapy. Behav Res Ther. 2021;138:103803. doi: 10.1016/j.brat.2021.103803. [DOI] [PubMed] [Google Scholar]
- 27.Catanzano M, Bennett SD, Sanderson C, Patel M, Manzotti G, Kerry E, et al. Brief psychological interventions for psychiatric disorders in young people with long term physical health conditions: a systematic review and meta-analysis. J Psychosom Res. 2020;136:110187. doi: 10.1016/j.jpsychores.2020.110187. [DOI] [PubMed] [Google Scholar]
- 28.Edbrooke-Childs J, Calderon A, Wolpert M, Fonagy P (2015) Rapid Internal Audit. National Report. https://www.ucl.ac.uk/evidence-based-practice-unit/sites/evidence-based-practice-unit/files/pub_and_resources_project_reports_rapid_internal_audit_2015.pdf. Accessed 21 March 2022
- 29.Bennett SD, Cuijpers P, Ebert DD, McKenzie Smith M, Coughtrey AE, Heyman I, et al. Practitioner review: Unguided and guided self-help interventions for common mental health disorders in children and adolescents: a systematic review and meta-analysis. J Child Psychol Psychiatry. 2019;60:828–847. doi: 10.1111/jcpp.13010. [DOI] [PubMed] [Google Scholar]
- 30.Catanzano M, Bennett SD, Kerry E, Liang H, Heyman I, Coughtrey AE, et al. Evaluation of a mental health drop-in centre offering brief transdiagnostic psychological assessment and treatment for children and adolescents with long-term physical conditions and their families: a single-arm, open, non-randomised trial. Evid Based Ment Health. 2021;24:25–32. doi: 10.1136/ebmental-2020-300197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ludlow C, Hurn R, Lansdell S. A current review of the children and young people's improving access to psychological therapies (CYP IAPT) program: perspectives on developing an accessible workforce. Adolesc Health Med Ther. 2020;11:21–28. doi: 10.2147/AHMT.S196492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pitchforth J, Fahy K, Ford T, Wolpert M, Viner RM, Hargreaves DS. Mental health and well-being trends among children and young people in the UK, 1995–2014: analysis of repeated cross-sectional national health surveys. Psychol Med. 2019;49:1275–1285. doi: 10.1017/S0033291718001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry 56:370–393. doi: 10.1111/jcpp.12372 [DOI] [PubMed]
- 34.Sellers R, Maughan B, Pickles A, Thapar A, Collishaw S. Trends in parent- and teacher-rated emotional, conduct and ADHD problems and their impact in prepubertal children in Great Britain: 1999–2008. J Child Psychol Psychiatry. 2015;56:49–57. doi: 10.1111/jcpp.12273. [DOI] [PubMed] [Google Scholar]
- 35.Patalay P, Gage SH. Changes in millennial adolescent mental health and health-related behaviours over 10 years: a population cohort comparison study. Int J Epidemiol. 2019;48:1650–1564. doi: 10.1093/ije/dyz006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The 1999 and 2004 data are available via application to the UK Data Service (references 4227 and 5269, respectively). The 2017 data are available via NHS Digital’s Data Access Request Service (DARS, reference DARS-NIC-424336-T7K7T-v0.6).


