Abstract
Loneliness and social network size have been found to be predictors of mortality in older adults. The objective of this study was to investigate whether loneliness and small social network size are associated with an increased mortality risk and to review the evidence for either network size, or loneliness that constitutes the higher mortality risk. A systematic literature search was performed in PubMed, EMBASE and PsychInfo in January/February 2018 and March/April 2021. Studies that mentioned outcome data were included in the meta-analysis and coded using the Newcastle–Ottawa Quality Assessment Scale for Cohort Studies. The meta-analysis showed that both loneliness and small social network size are associated with mortality risk in older adults (Hazard Ratio 1.10 (95% Confidence Interval 1.06–1.14) for loneliness and 0.96 (95% Confidence Interval 0.93–0.99) for larger network size). Sensitivity analyses according to the Newcastle–Ottawa Quality Assessment Scale yielded varying results. Heterogeneity was large. In conclusion, both loneliness and small social network size in older adults are associated with increased mortality, although the effect size is small. Targeting subjective and objective aspects of older adults’ social contacts should be on the agenda of preventive as well as personalized medicine. In order to be able to compare the association between loneliness and network size and mortality, more studies are needed that include both these risk factors.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10433-022-00740-z.
Keywords: Loneliness, Social isolation, Social network, Mortality
Introduction
It has long been recognized that social relationships have an impact on health and mortality (House et al. 1988; Olsen et al. 1991; Penninx et al. 1997). Both subjective and objective aspects of social relationships are important in this respect. The subjective feeling of missing an intimate relationship or missing a wider social network is recognized as loneliness (Jong and Tilburg 2006). On the other hand, objective indicators of social relationships reflect a small social network size (O’Luanaigh and Lawlor 2008; Routasalo et al. 2004; Shankar et al. 2011; Steptoe et al. 2013), the absence of a spouse, low frequency of social contacts and lack of participation in social groups (Cacioppo et al. 2015). These objective indicators can be grouped under the term social isolation. Loneliness and social isolation are related, although the association has been found to be rather weak (Cornwell and Waite 2009).
Both subjective and objective aspects of social relationships have been argued to be important predictors of increased mortality in older adults, although results have been inconsistent. Whereas associations between loneliness and mortality have been found in some studies (Holwerda et al. 2012; Luo et al. 2012; Patterson and Veenstra 2010; Penninx et al. 1997; Perissinotto et al. 2012; Shiovitz-Ezra and Ayalon 2010), other studies concluded that mortality was not increased in lonely older adults (Holwerda et al. 2016; Steptoe et al. 2013). Associations between social isolation and mortality have also been found (House et al. 1988; Steptoe et al. 2013; Tanskanen and Anttilla 2016), with the effect size of the lack of social relationships on mortality being comparable to that of smoking, obesity and lack of exercise. However, one study concluded there was no significant association between social isolation and mortality (Cerhan and Wallace 1997).
The mechanisms underlying an association between both loneliness and social isolation and mortality are not clear. Possible explanations generally include two mechanisms: through the stress-buffering effects of social connections, or the direct biological effects of the stress of loneliness or lack of contacts (Holt-Lunstad et al. 2010; House et al. 1988). Potential biological mechanisms that have been studied include cognitive decline (Holwerda et al. 2014; Lara et al. 2019; Rafnsson et al. 2020), immune dysregulation (Jaremka et al. 2013, 2018; O’Luanaigh and Lawlor 2008), sleep disturbances (Cacioppo et al. 2002; O’Luanaigh and Lawlor 2008), increased food intake (Jaremka et al. 2018), endocrine dysregulation (Adam et al. 2006; Steptoe et al. 2004) and cardiovascular disease (Cacioppo et al. 2002; Hawkley et al. 2006, 2010; O’Luanaigh and Lawlor 2008; Steptoe et al. 2004). Examples of the stress-buffering effects of social connections are the promoting of adaptive behavior and the availability of instrumental support in case of stress (Holt-Lunstad et al. 2010; House et al. 1988).
To evaluate the associations between both loneliness and social isolation and mortality, systematic reviews and meta-analyses have been done (Holt-Lunstad et al. 2010, 2015; Rico-Uribe et al. 2018). These studies showed that both objective and subjective aspects of social relationships influence mortality in adults. However, many studies that were included in these meta-analyses used a ‘social network index’ (Berkman and Syme 1979), considering not only the number of social ties but also their relative importance. This index has been used by several authors (Kawachi et al. 1996; Schoenbach et al. 1986; Seeman et al. 1987). The problem with using an index is that it obscures which aspects are responsible for the outcome (Avlund et al. 1998). In contrast, our goal was to investigate whether studies that have focused on the association between social relations and mortality provide more evidence in this association for objective aspects or for subjective aspects of social relationships. This division into objective and subjective aspects is in agreement with most research into the effects on health and mortality of loneliness and social relationships, as most researchers focus either on the more objective quantitative measure of network size and diversity, reflecting reduced social network size and paucity of social contact (Shankar et al. 2011; Steptoe et al. 2013), or on the subjective psychological experience of loneliness (Hawkley & Cacioppo 2010; Routasalo et al. 2004; Shankar et al. 2011; Steptoe et al. 2004, 2013). In addition, many studies included in previous meta-analyses did not adjust for covariates. Moreover, because of the inconsistent outcomes of studies into the associations between mortality and both loneliness and social isolation in older adults, we were especially interested in a meta-analysis including studies in older adults only.
The distinction between objective and subjective aspects of social relationships and their associations with mortality in older adults are the main focus of the present study. The number of people in a person’s network can be seen as an indication of social isolation (Victor et al. 2000) and although some research revealed a stable total network size over a four-year period (Van Tilburg 1998), over longer periods of time this network size has been reported to decrease with age (Bowling et al. 1991; Broese van Groenou et al. 2013). Although living alone has been used as an operationalization of social isolation (Victor et al. 2000) and is one of the aspects of social isolation that is associated with increased mortality (Holt-Lunstad et al. 2015), we were especially interested in the question whether there is more evidence for objective aspects or for subjective aspects of social contacts in the association with mortality. Loneliness is often regarded as the subjective counterpart to the objective social isolation (Steptoe et al. 2013; Victor et al. 2000) and it has been reported to increase with age (Victor et al. 2000; Dykstra et al. 2005). Loneliness and depression are related but separate concepts that have strong reciprocal influences in middle-aged and older adults (Cacioppo et al. 2006; Holvast et al. 2015; Peerenboom et al. 2015), and depression has been found to be associated with increased mortality (Li et al. 2019; Wei et al. 2019). Therefore, the presence of depression is an important covariate in the association between loneliness and mortality.
Our main research questions are: 1. Are subjective (loneliness) and objective aspects (small social network size) associated with increased mortality in older adults? 2. Is there more evidence for subjective or for objective aspects of social relations in this association? 3. Do these associations remain when controlled for important covariates such as depression?
Method
Search strategy and selection criteria
To identify studies investigating the mortality effects of loneliness and/or social network size, we systematically searched PubMed in January/February 2018 and in March/April 2021 using the following search: (("Mortality"[Mesh:noexp] OR "mortality"[Subheading] OR mortalit*[tiab])) AND ((("Aged"[Mesh] OR elderly[tiab] OR older people*[tiab] OR older adult*[tiab] OR late-life[tiab] OR latelife[tiab] OR very old*[tiab] OR old patient*[tiab] OR old person*[tiab] OR aging[tiab] OR ageing[tiab] OR octagenarian*[tiab] OR octogenarian*[tiab] OR centenarian*[tiab] OR geriatri*[tiab] OR older patient*[tiab] OR old age*[tiab])) AND ("Loneliness"[Mesh] OR "Social Isolation"[Mesh] OR "Social Support"[Mesh] OR lonely[tiab] OR lonelines*[tiab] OR social isolation*[tiab] OR social contact*[tiab] OR social network*[tiab] OR social support*[tiab] OR psychosocial support system*[tiab])) and EMBASE and PsychInfo using the following search terms: aged, elderly, older people, older adult, older patient, late-life, very old, old patient, old person, old age, aging, ageing, octagenarian, octogenarian, centenarian, geriatric, geriatrics, geriatric patients, elder care; combined with loneliness, lonely, social isolation, social networks, social support, social contact, psychosocial support system, social interaction, social behavior, psychosocial factors, social participation, community network, care network, community health network; combined with mortality, death and dying.
When conceptualizing social isolation, several aspects deserve consideration. An important issue is what constitutes the ‘active ingredient’ (Cornwell and Waite 2009) of the lack of social relationships responsible for the association with morbidity and mortality. Different measures of a lack of social relationships have been proposed by different researchers, including living alone, having a small social network, low participation in social activities, low frequency of contacts, perceived lack of social support and feelings of loneliness (Cornwell and Waite 2009), and different aspects of social relationships can be taken into account, such as the existence and quantity of relationships, their formal structure and the actual content (House et al. 1988). To be clear about the ‘active ingredient’ and to oppose objective and subjective aspects of social relationships, we chose network size as the most readily measurable objective indicator of social isolation.
There was no preregistered protocol.
Study selection
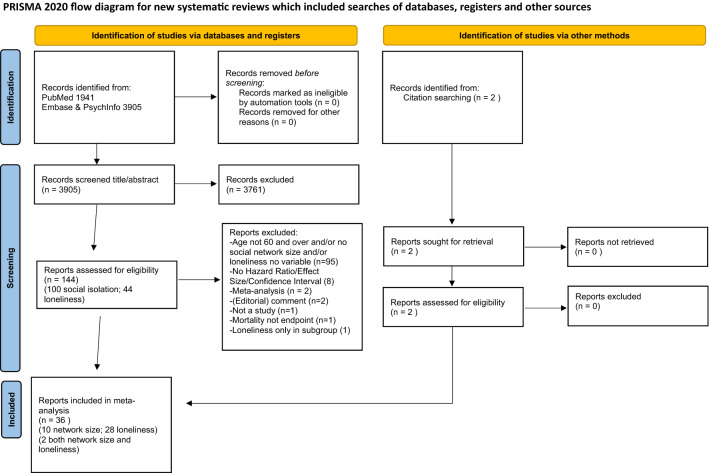
Figure 1 shows the flow diagram. Studies were included when they were original studies; in English, French, German or Dutch; had been published in peer reviewed journals; answered the following research question: ‘in older adults, is there an association between loneliness and/or social network size and mortality?’ The exclusion criteria were: age younger than 60 years at start of the study; case reports; systematic reviews and meta-analyses; no measure for loneliness or social network size; lack of information about covariates. In a first selection round, studies were identified with title/abstract using the above-mentioned criteria. This selection was done by two authors (NS and HC or NS and JD). When their opinion differed, a third author was consulted (TH). In the second round, abstracts were examined and if they were not informative enough about the study design, the method section of the full text was read. This was done by two authors (NS and TH or NS and JD). When their opinion differed, a third author (MS) was consulted. Differences in opinion mainly regarded the use of a social network size measure.
Fig. 1.
Flow diagram of the study selection
Data extraction
In the third round, articles were coded using the Newcastle–Ottawa Quality Assessment Scale for Cohort Studies (Wells et al. 2000) (NOS) (Table 1) to evaluate the quality of the studies by assessing potential bias. Each article was coded by the first author (NS) and another author (TH, MS or JD). When there was difference in opinion, a third author (HC) was consulted.
Table 1.
Newcastle–Ottawa Quality assessment scale criteria including attribution of points
| Criteria: | Points to be gained |
|---|---|
| Selection | |
| Representativeness | |
| Truly | 1 |
| Somewhat | 1 |
| Selected group | 0 |
| No description | 0 |
| Selection of non-exposed cohort | |
| Drawn from same community | 1 |
| Drawn from a different source | 0 |
| No description | 0 |
| Ascertainment of exposure | |
| Secure record | 1 |
| Structured interview | 1 |
| Written self-report | 0 |
| No description | 0 |
| Demonstration that outcome of interest not present at start | |
| Yes | 1 |
| No | 0 |
| Comparability | |
| Comparability of cohorts | |
| Study controls for most important factor | |
| Study controls for additional factors | 1 |
| Outcome | 1 |
| Assessment of outcome | |
| Independent blind assessment | 1 |
| Record linkage | 1 |
| Self-report | 0 |
| No description | 0 |
| Follow-up long enough? | |
| Yes | 1 |
| No | 0 |
|
Adequacy of follow-up 0 | |
| Complete follow-up | 1 |
| Small number lost/description provided | 1 |
| Higher number lost/no description | 0 |
| No statement | 0 |
When outcome data were mentioned we included the study in the meta-analysis. Data extraction was done by two authors (NS and TH). In case of studies including also younger adults, we contacted the authors and asked for data concerning only older adults. We extracted adjusted Hazard Ratios from all included studies. When no Hazard Ratio or Relative Risk was mentioned, we estimated the Hazard Ratio using p value, total events and numbers of participants in both groups of participants (Tierney et al. 2007) and calculated the 95% Confidence Interval using the standard error. From every study, the following data were recorded: country, study population, number of participants, age group studied, length of follow-up, Hazard Ratio/Odds Ratio, 95% Confidence Interval and covariates (Table 2).
Table 2.
Studies included in the meta-analysis
| Study | Country | Study name | Study population | Nr. of participants | Age | Assessment of loneliness/network size | Length of follow-up | OR/HR/ RH/RR | Result | Main covariates |
|---|---|---|---|---|---|---|---|---|---|---|
| Loneliness | ||||||||||
| Aguiar et al. (2020) | USA | Kuakini Honolulu Heart Program | Japanese-American men in Honolulu | 3186 | 71–93 | Single question | 28 yrs | HR | 1.29 | Age, cardiovascular risk factors, chronic diseases |
| Conde-Sala et al. (2020) | Europe | Survey of Health, Ageing and Retirement in Europe | 14 European countries | 35,604 | ≥ 60 | 3-item UCLA loneliness scale | 2 yrs | HR | 1.27 |
Age, gender, marital status, depressive symptoms, self-rated health, presence of diseases |
| Drageset et al. (2012) | Norway | – | Nursing home residents | 227 | ≥ 65 | Social Provisions Scale | 5 yrs | HR | 0.96 (attachment) | Gender, age, marital status, comorbidity, social integration, GDS-score |
| Ellwardt et al. (2015) | Netherlands | Longitudinal Aging Study Amsterdam | Nationally representative | 2462 | ≥ 60 | De Jong Gierveld loneliness scale | ≤ 20 yrs | HR | NS | Age, mental health, physical health |
| Elovainio et al. (2017) | UK | UK Biobank Study | Within sensible distance from assessment center | 178,769 | ˃ 60 | 2 questions | 8 yrs | HR | 1.44 | Age, gender, chronic disease |
| Holwerda et al. (2012) | Netherlands | Longitudinal Aging Study Amsterdam | Nationally representative | 2433 | ≥ 60 | De Jong Gierveld loneliness scale | 19 yrs | HR | NS | Age, gender, marital status, network size, depression, chronic diseases |
| Holwerda et al. (2016) | Netherlands | Amsterdam Study of the Elderly | Urban | 4004 | ≥ 60 | Single question | 10 yrs | HR |
1.30 (men) 1.04 (women) |
Age, social isolation, CVA, diabetes, depression, other diseases |
| Hoogendijk et al. (2020) | Netherlands | Longitudinal Aging Study Amsterdam | Nationally representative | 1427 | ≥ 65 | De Jong Gierveld loneliness scale | 22 yrs | HR | NS | Age, partner status, sex, depression score, social participation, chronic diseases |
| Iecovich et al. (2011) | Israel | Jerusalem Longitudinal Study | Nationally representative | 605 | 70–88 | Single question | 18 yrs | HR | NS | Gender, health, network type, morbidity, self-rated health (age cohort) |
| Julsing et al. (2016) | Netherlands | Zutphen Elderly Study | Small town men | 719 | 64–84 | De Jong Gierveld loneliness scale | 25 yrs | HR | NS (moderate) | Age, chronic disease |
| Jylha and Aro (1989) | Finland | – | Urban | 1060 | 60–89 | Single question | 6.5 yrs | RH | NS | Age, gender, baseline health status, social participation |
| Lara et al. (2020) | Spain | Collaborative Research on Ageing in Europe | Nationally representative | 4467 | ≥ 60 | 3-item UCLA loneliness scale | 6–7 yrs | HR | NS | Sex, age, depression, social activities |
| Luo and Waite (2014) | China | Chinese Longitudinal Healthy Longevity Survey | Nationally representative | 14,072 | ≥ 65 | Single question | 6 yrs | HR | 1.04 | Age, gender, self-assessed health, living arrangement social activities |
| Ng et al. (2021) | Singapore | Panel on Health and Ageing of Singaporean Elderly | Nationally representative | 4536 | ≥ 60 | 3-item UCLA loneliness scale | 6 yrs | HR | 1.40 (women) NS (men) | Age, gender, total number of morbidities, social network size, social engagement, living arrangements |
| Novak et al. (2020) | Sweden | Gothenburg H70 Birth Cohort Studies Collaborative | Urban | 512 | 70 | Single question | 12 yrs | HR | NS | Health, health-related behavioral factors, living alone, physical disease, depression |
| Olaya et al. (2017) | Spain | Research on Ageing in Europe | Nationally representative | 2113 | ≥ 60 | 3-item UCLA loneliness scale | 3 yrs | HR | NS | Age, gender, marital status, depression, social support, physical conditions |
| Olsen et al. (1991) | Denmark | – | Urban, experimental group | 1752 | 70–100 | Single question | ≤ 15 yrs | HR | NS | Age, gender, health indicators, social contacts |
| O’Suilleabhain et al. (2019) | Germany | Berlin Aging Study | Urban | 413 | 70–103 | UCLA 8 items | 16–19 yrs | HR | NS | Age, sex, marital status, depressive illness |
| Perissinotto et al. (2012) | USA | – | Nationally representative | 1604 | ˃ 60 | 3-item UCLA loneliness scale | 6 yrs | HR | 1.45 | Age, gender, marital status, living arrangement, depression, medical conditions |
| Schutter et al. (2020) | Netherlands | Netherlands Study on Depression in Older adults | Depressed and control group | 443 | ˃ 60 | De Jong Gierveld loneliness scale | 6 yrs | HR | NS | Age, sex, partner status, depression, chronic diseases |
| Steptoe et al. (2013) | England | English Longitudinal Study of Ageing | Nationally representative | 6500 | ≥ 60 | 3-item UCLA loneliness scale | 7–8 yrs | HR | NS |
Age, gender, marital status, general health, depression, CES-D rating, longstanding illness, social isolation |
| Stessman et al. (2014) | Israel | Jerusalem Longitudinal Cohort Study | Urban | 1566 | 70–90 | Single question | 7 yrs | HR | NS | Gender, marital status, self-rated health, age group, Depression |
| Sugisawa et al. (1994) | japan | – | Nationally representative | 2200 | ≥ 60 | Single question | 3 yrs | HR | NS | Gender, age, marital status, self-rated health, chronic diseases, social contacts, social participation |
| Tabue Teguo et al. (2016) | France | Personnes Agées Quid | Nationally representative | 3620 | ≥ 65 | Single question | ≤ 22 yrs | OR | NS | Age, gender, living alone, chronic diseases |
| Tanskanen et al. (2016) | Finland | Living Conditions Survey of 1994 | Nationally representative | 1731 | ≥ 60 | Single question | ≤ 17 yrs | HR | NS | Age, gender, self-reported health, social isolation |
| Tilvis et al. (2011) | Finland | – | Nationally representative | 3687 | ≥ 75 | Single question | < 5 yrs | HR | 1.17 | Age, gender, subjective health |
| Wang et al. (2020) | England | Cambridge City over-75 s Cohort | Urban | 665 | ≥ 75 | Single question | 10 yrs | HR | NS | Age, sex, marital status, chronic diseases, depression |
| Youm et al. (2021) | South Korea | Korean Social Life, Health and Aging Project | Rural | 679 | ≥ 60 | Single question | 8 yrs | HR | 1.31 | Sex, living with spouse, comorbidity, physical health, depression |
| Network size | ||||||||||
| Ali et al. (2018) | USA | Chicago Health and Aging Project | Urban | 6497 | ≥ 65 | Single question | 10 yrs | HR | 1.01 | Age, gender, marital status, medical conditions |
| Cerhan and Wallace (1997) | USA | Iowa 65 + Rural Health Study | Rural | 2575 | 65–102 | Single question | 8 yrs | HR |
NS (men) NS (women) |
Age, major illness, depressive symptoms, self- perceived health |
| De Brito et al. (2017) | Brazil | Health, Well-being and Aging Study | Nationally representative | 1413 | ≥ 60 | Single question | 4 yrs | HR | 0.67 | Age, gender, living arrangements, comorbidity, depressive symptoms |
| Ellwardt et al. (2015) | Netherlands | Longitudinal Aging Study Amsterdam | Nationally representative | 2462 | ≥ 60 | Single question | ≤ 20 yrs | HR | 0.99 | Age, mental health, physical health |
| Giles et al. (2005) | Australia | Australian Longitudinal Study of Aging | Nationally representative | 1477 | ≥ 70 | Combined networks (4) | 10 yrs | HR | 0.95 | Age, gender, comorbid conditions, self-rated health, CES-D score |
| McLaughlin et al. (2011) | Australia | Men, Women and Aging Project | Urban | 6877 | 69–87 | Duke Social Support Index | 5–10 yrs | RR | 0.89 | Age, marital status, chronic disease |
| Roth (2020) | USA | National Social Life, Health and Aging Project | Nationally representative | 2553 | ≥ 60 | Single question (core discussion network name generator) | 5–6 yrs | HR | 0.90 | Sex, age, marital status, depressive symptoms |
| Schutter et al. (2020) | Netherlands | Netherlands Study of Depression in Older Adults | Depressed and control group | 443 | ≥ 60 | Close Persons Questionnaire | 6 yrs | HR | NS | Age, sex, partner status, depression, chronic |
| Shye et al. (1995) | England | Kaiser Permanente Northwest Region | Members of Health Maintenance Organization group | 455 | ≥ 65 | Single question | 15 yrs | RH |
1.65 (men)1.61 (women) (small network) |
Age, gender, marital status, health |
| Vogt et al. (1992) | USA | Northwest Kaiser Permanente | Members of HMO group | 451 | ≥ 60 | 4 questions | 15 yrs | RH | 2.0 (small network) | Age, gender, baseline subjective health |
OR odds ratio, HR hazard ratio, RH relative hazard, RR relative risk
Statistical analysis
All studies mentioning Hazard Ratio or Relative Risk and a Confidence Interval, or offering enough data to estimate a Hazard Ratio, were included in the meta-analysis (Table 2). Separate analyses were done for loneliness and network size, using the random effects model. Additionally, we executed sensitivity analyses. Firstly, we examined the effect of depression on the association between mortality and loneliness/social network size by first including only studies with depression as a covariate, followed by including only studies without depression as a covariate. The same method was used for examining the effect of a social network variable in the association between mortality and loneliness. Similarly we examined whether differences in scores on items from the NOS influenced the meta-analysis outcome. This was assessed by grouping the studies according to NOS-scores. Additionally, heterogeneity was assessed using Cochran’s Q test at significance level of p ˂ 0.05 and quantified by the I2 statistic, with the following rough interpretation: a value of less than 40% indicating little heterogeneity, 30–60% indicating moderate heterogeneity, 50–90% substantial heterogeneity and 75–100% considerable heterogeneity (Deeks et al. 2008). The interpretation of the I2 statistic depends on several factors, such as the significance level and the magnitude of effects (Deeks et al. 2008). Additional sensitivity analyses were executed to examine possible causes of heterogeneity. Publication bias was assessed in funnel plots. We executed the meta-analysis using Comprehensive Meta-Analysis (CMA) software.
Results
Of 144 publications that initially fitted our inclusion criteria, 110 did not fit on closer examination (Fig. 1). The most frequent reason for non-inclusion was a different measure for social isolation. For example, authors used measures like frequency of contact, relationship quality, a ‘social index’ or ‘social integration index,’ living situation, social support measure, network type and marriage status. Another frequent reason for exclusion was that the age of included participants was younger than 60 years old and the authors could not provide additional analyses for participants aged 60 and over. Eight studies had to be excluded because they did not include quantitative results. Two studies were retrieved from citation searching, leading to a total of 36 studies.
Meta-analysis
Table 2 shows studies included in the meta-analysis. There was some overlap in studies: three publications were based on data from the Longitudinal Aging Study Amsterdam, two publications on data from the Collaborative Research on Ageing in Europe, two publications on data from the Jerusalem Longitudinal Cohort Study and two publications on data from the Kaiser Permanente Northwest study, although data were from different waves and/or different endpoints in time. Using the NOS, all included studies but five appeared to be of good quality; only the study by Drageset et al. (2012) was of fair quality due to the fact that the study investigated nursing home patients only and consequently the participants had a higher mortality risk, whereas the studies by Aguiar et al. (2020), Ng et al. (2021), O’Suilleabhain et al. (2019) and Youm et al. (2021) were of poor quality, due to missing information about assessment of outcome and about participants lost to follow-up (Table 3).
Table 3.
Points acquired in the assessment of quality for each study according to the Newcastle–Ottawa quality assessment scale criteria
| Study Loneliness |
Representativeness | Selection | Comparability On the basis of design or analysis |
Outcome | Total | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-exposed cohort | Ascertainment of exposure | Outcome of interest not present at start | Assessment of outcome | Follow-up long enough | Adequacy of follow-up | |||||||||||||
| Aguiar et al. (2020) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 7 | |||||||||
| Conde-Sala et al. (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Drageset et al. (2012) | 0 | 1 | 1 | 0 | 2 | 1 | 1 | 1 | 7 | |||||||||
| Ellwardt et al. 2015 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Elovainio et al. (2017) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Holwerda et al. (2016) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Holwerda et al. (2012) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| Hoogendijk et al. (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Iecovich et al. (2011) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Julsing et al. (2016) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| Jylha and Aro (1989) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Lara et al. (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Luo and Waite (2014) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Ng et al. (2021) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 7 | |||||||||
| Novak et al. (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Olaya et al. (2017) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Olsen et al. (1991) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| O’Suilleabhain et al. (2019) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 7 | |||||||||
| Perissinotto et al. (2012) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Schutter et al. (2020) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 8 | |||||||||
| Steptoe et al. (2013) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Stessman et al. (2014) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| Sugisawa et al. (1994) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Tabue Teguo et al. (2016) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 9 | |||||||||
| Tanskanen et al. (2016) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Tilvis et al. (2011) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Wang et al. (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Youm et al. (2021) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 0 | 7 | |||||||||
| Networksize | ||||||||||||||||||
| Ali et al. (2018) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Cerhan and Wallace et al. (1997) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| DeBrito et al. (2017) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Ellwardt et al. 2015 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 | |||||||||
| Giles et al. (2005) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| McLaughlin et al. (2011) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| Roth (2020) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
| Schutter et al. (2020) | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 1 | 8 | |||||||||
| Shye et al. (1995) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 | |||||||||
| Vogt et al. (1992) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 | |||||||||
Loneliness and mortality
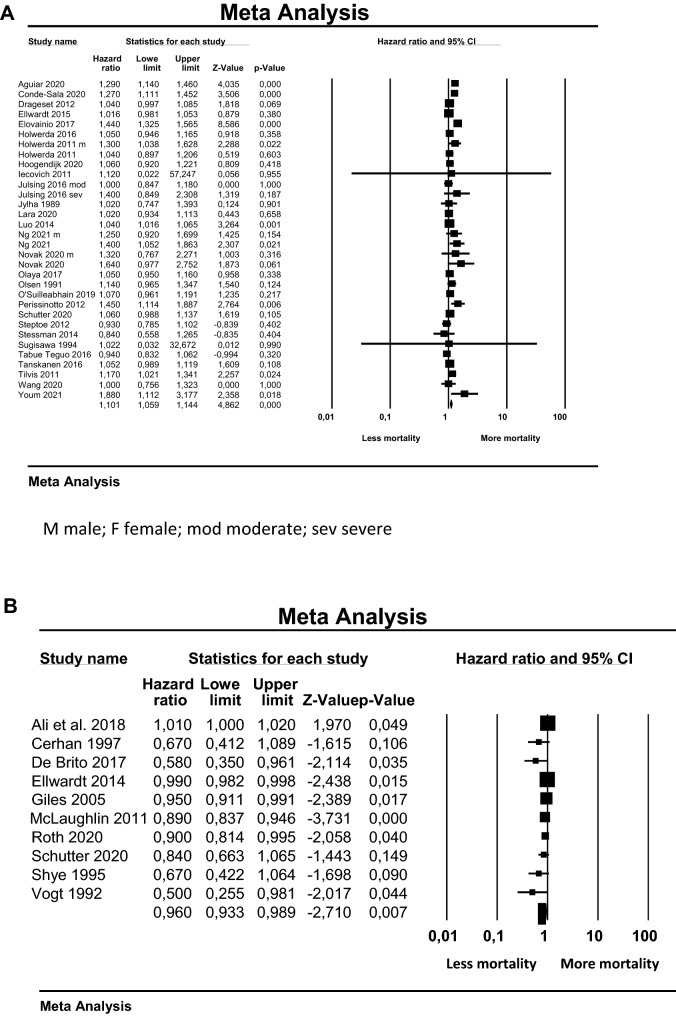
We included 28 studies investigating the association between loneliness and mortality. Three studies did not calculate Hazard Ratios but other effect sizes. Since they mentioned p value, total events and numbers of participants in both groups of participants, we were able to estimate a Hazard Ratio using the method described by Tierney et al. (2007) (See Supplement for the formulas used). In 18 studies (Table 2), loneliness was not associated with mortality after controlling for a number of covariates. All studies controlled for age and gender. All studies controlled for (self-assessed) physical health, (chronic) diseases, comorbidity and/or medical conditions. Of the 28 studies, 13 controlled for depression and/or depressive symptoms and 16 studies controlled for a ‘social contact’ variable. Figure 2A shows the forest plot: overall, it shows a small but significant positive association between loneliness and mortality. That the overall analysis shows a positive association could be due to the positive studies showing more robust results, as displayed in Fig. 2A.
Fig. 2.
Forest plots showing the results for studies studying the association between mortality and loneliness (A) and between mortality and network size (B)
Network size and mortality
We included ten studies investigating the association between network size and mortality (Table 2). All but two showed a lower mortality when the network was larger. All studies controlled for age and gender and (self-rated) physical health, comorbidity or chronic diseases. Seven studies controlled for depression diagnosis or depressive symptoms. None of the studies controlled for loneliness. Figure 2B shows the forest plot: it shows a small but significant negative association between network size and mortality, with a larger network showing a lower mortality risk.
Sensitivity analyses
Table 4 shows the results of the sensitivity analyses according to covariates and according to NOS-scores. The second and sixth columns show the number of loneliness and network size studies. When only studies that included depression as a covariate were grouped into the meta-analysis, the association with mortality did not change for loneliness: HR was 1.13, 95% CI 1.06–1.22 (original HR 1.10) and decreased for network size: HR was 0.88, 95% CI 0.80–0.97 (original HR 0.96). Introduction of a ‘social contact variable’ diminished the association between loneliness and mortality (HR 1.04).
Table 4.
Studies in Meta-Analysis According to covariates and Newcastle–Ottawa Quality Assessment Scale criteria
| Covariates | Loneliness | HR | 95%CI | Heterogeneity | Networksize | HR | 95%CI | Heterogeneity |
|---|---|---|---|---|---|---|---|---|
| Depression | ||||||||
| Covariate | 14 | 1.13 | 1.06,1.22 | I280, P < 0.001 | 6 | 0.88 | 0.80,0.97 | I245, P0.11 |
| Nocovariate | 14 | 1.06 | 1.02,1.11 | I247, P0.02 | 4 | 0.98 | 0.95,1.01 | I289, P < 0.001 |
| Socialcontactvariable | ||||||||
| Covariate | 16 | 1.04 | 1.02,1.06 | I20, P0.62 | ||||
| Nocovariate | 12 | 1.19 | 1.08,1.31 | I279, P < 0.001 | ||||
| NOS-criteria: Selection |
Loneliness | HR | 95%CI | Heterogeneity | Networksize | HR | 95%CI | Heterogeneity |
|---|---|---|---|---|---|---|---|---|
| Representativeness | ||||||||
| Truly | 16 | 1.11 | 1.0, 1.16 | I276, P < 0.001 | 5 | 0.98 | 0.95, 1.00 | I278, P < 0.001 |
| Somewhat | 8 | 3 | ||||||
| Selectedgroup | 4 | 1.04 | 1.00, 1.08 | I20, P0.44 | 2 | 0.85 | 0.70, 1.04 | I230, P0.23 |
| Nodescription | 0 | 0 | ||||||
| Outcome | ||||||||
| Follow-up long enough? | ||||||||
| Yes | 28 | 10 | ||||||
| No | 0 | 0 | ||||||
| < 5yrs | 3 | 1.13 | 1.06, 1.19 | I279, P < 0.001 | 1 | 0.92 | 0.86, 0.99 | I284, P < 0.001 |
| 5–10yrs | 14 | 6 | ||||||
| > 10yrs | 11 | 1.07 | 1.02, 1.12 | I248, P0.03 | 3 | 0.76 | 0.51, 1.15 | I270, P0.04 |
| Adequacy of follow-up | ||||||||
| Complete follow-up | 2 | 3 | ||||||
| Smallnumberlost/descriptionprovided | 13 | 1.11 | 1.05, 1.18 | I281, P < 0.001 | 2 | 0.89 | 0.80, 1.00 | I280, P < 0.001 |
| Higher number lost/no description | 9 | 3 | ||||||
| Nostatement | 4 | 1.09 | 1.03, 1.15 | I243, P0.04 | 2 | 0.95 | 0.89, 1.02 | I279, P0.001 |
HR hazard ratio
95% CI: 95% confidence interval
The first NOS-criterion is ‘representativeness of the exposed cohort.’ This refers to the degree in which the participants are representative of all older adults in the community. With regard to representativeness, the grouping of studies had different effects for loneliness and network size. The association between loneliness and mortality was stronger in the studies that used a more representative population. The association between network size and mortality diminished as a result of this grouping.
The next set of NOS-criteria we used in sensitivity analyses regards the duration and adequacy of follow-up. Grouping studies according to duration of follow-up had different effects for loneliness and social network size: the association between loneliness and mortality was stronger with a follow-up of ten years or less, whereas the association between network size and mortality was no longer significant and showed a wider Confidence Interval with a follow-up over 10 years (Table 4).
‘Adequacy of follow-up’ refers to the loss of follow-up of participants and the description of those lost to follow-up. Grouping studies according to this criterion had similar effects in studies with loneliness and studies with network size. The association between loneliness/network size and mortality was stronger when only studies with (near) complete follow-up were regarded.
Additional sensitivity analyses
Because there was some overlap in studies using data from the same group of participants, we repeated our analyses excluding overlapping studies. We only used the results from the most recent studies. The results show that this did not influence the Hazard Ratios: 1.12 (95% CI 1.06–1.17) for the loneliness studies and 0.96 (95% CI 0.94–0.99) for the network size studies. Heterogeneity was not influenced either (I2 statistic for the loneliness studies 76 and for the network size studies 81).
Heterogeneity
Statistical heterogeneity was large. Across the loneliness studies, the I2 statistic was 72, with a Cochran’s Q-test at ˂0.001. The same values applied to the network sizes studies: I2 = 81, and p ˂0.001. Grouping the studies according to covariates and according to NOS-criteria influenced heterogeneity. Network size studies that included depression as a covariate were statistically less heterogeneous. Loneliness studies were less statistically heterogeneous when they included a ‘social contact variable’ as a covariate (Table 4). Grouping the studies according to the NOS-criterion ‘representativeness’ resulted in a less statistically heterogeneous group for the studies that used a selected population, both in loneliness and in network size studies. Grouping studies according to follow-up duration had comparable effects on heterogeneity in loneliness and network size studies. Grouping according to ‘adequacy of follow-up’ however only had an effect on loneliness studies: with higher loss to follow-up, studies appeared to be less heterogeneous. We also investigated the effect of ‘outliers’: in the forest plot (Fig. 2A) showing the association between loneliness and mortality, two studies show very large Confidence Intervals. Removing these studies from the analysis did not diminish heterogeneity: I2 = 74, p ˂ 0.001, nor did it effect Hazard Ratio: 1.10, 95% CI 1.06–1.15. The same procedure was followed for investigating the effect of different sample sizes: removing smaller studies (˂ 1000 participants) did not diminish heterogeneity in the loneliness studies: I2 = 79, p ˂ 0.001, nor in the network size studies: I2 = 84, p ˂ 0.001. Additionally, we examined the effect of the assessment of loneliness on heterogeneity by including only studies that used a questionnaire. This diminished heterogeneity somewhat: I2 = 46, p = 0.03, while also diminishing the Hazard Ratio (1.06, 95% CI 1.02–1.10). Including only studies that assessed loneliness by asking a single question did not reduce heterogeneity: I2 = 81, p ˂ 0.00, with a Hazard Ratio of 1.14 (95% CI 1.05–1.24). We also examined the effect of excluding studies that were scored on the NOS as of ‘poor quality’. When these studies were excluded, heterogeneity did not diminish: I2 = 72, p ˂ 0.001, while the Hazard Ratio was 1.08 (95% CI 1.04–1.13).
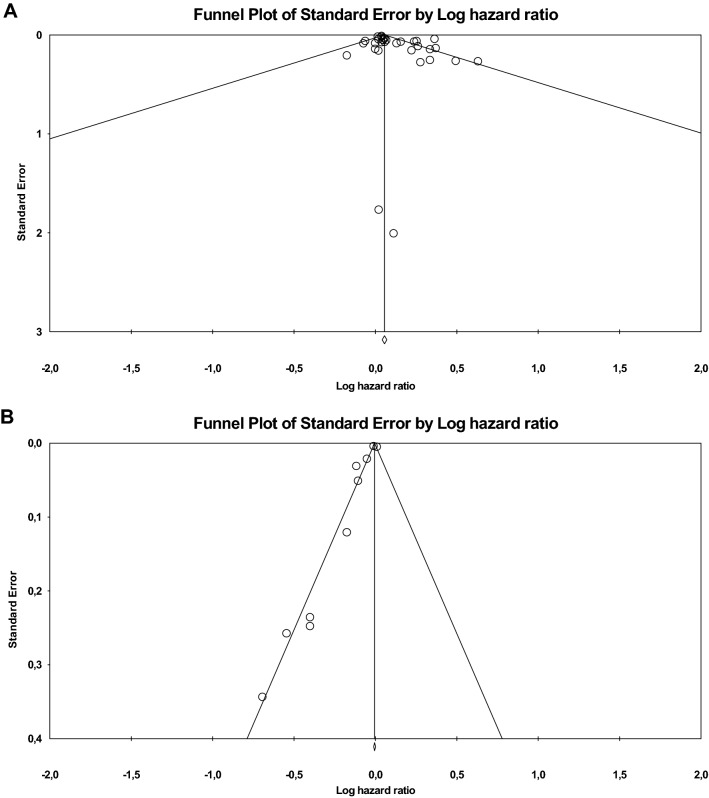
Publication bias
The funnel plots (Fig. 3) show a fairly symmetrical distribution of loneliness studies (A), but a one-sided distribution of network size studies (B). Therefore, publication of studies investigating the association between network size and mortality could be biased in the direction of showing a stronger association than actually present.
Fig. 3.
Funnel plots showing distribution of published loneliness studies (A) and network size studies (B)
Discussion
This meta-analysis was performed to investigate whether loneliness and social network size in older adults are associated with mortality and to accumulate evidence for either the subjective aspects or the objective aspects of missing social relationships to be more important in this association. Additionally, the role of important covariables such as depression was investigated.
In the present study, both loneliness and small network size show an association with mortality in older adults. These results are in line with previous meta-analyses investigating mortality effects of loneliness, social isolation and social relationships (Holt-Lunstad et al. 2010, 2015; Rico-Uribe et al. 2018). Compared with the present study, these meta-analyses showed larger effect sizes, varying from a Hazard Ratio of 1.22 (Rico-Uribe et al. 2018) to an Odds Ratio of 1.50 (Holt-Lunstad et al. 2010). In comparison, in a study by Katzmarzyk et al. (2003) the Relative Risk of all-cause mortality for elevated Body Mass Index was 1.23 (95% CI 1.18–1.29) and for physical activity 0.80 (95% CI 0.78–0.82).
In order to compare the associations with mortality of loneliness and social network size it is essential that studies investigating the associations between loneliness and mortality control for social network size and vice versa. Of the studies investigating the associations between loneliness and mortality that were included, more than half controlled for a social contact variable, although in only three studies this variable was the actual size of the social network. These studies still showed an association between loneliness and mortality (Table 4). Therefore, it can be concluded that loneliness in itself is associated with higher mortality, independent of the objective social situation. Unfortunately, the studies in this meta-analysis investigating the association between mortality and social network size did not control for feelings of loneliness. As a consequence, the effects of loneliness and social network size cannot be compared directly. Only two studies investigated both loneliness and social network size (Ellwardt et al. 2015; Schutter et al. 2020). One of these studies concluded that social network size was associated with mortality, but loneliness was not (Ellwardt et al. 2015); the other study concluded that neither was associated with mortality (Schutter et al. 2020).
With respect to covariables, we investigated the role of depression. Studies in the present meta-analysis that included depression as a covariate still showed a significant association with mortality. In accordance with our results, sensitivity analyses in the meta-analysis by Rico-Uribe et al. (2018) showed that when only studies were included that used depression as a covariate, loneliness was still associated with higher mortality. These findings suggest that loneliness and small social network size might be risk factors for mortality in themselves, irrespective of depression.
Contrary to the present study, Holt-Lunstad et al. (2010; 2015) included unadjusted mortality risks and concluded that the number of covariates included was negatively associated with effect size (Holt-Lunstad et al. 2015). The difference in effect size between unadjusted Hazard Ratios and fully adjusted Hazard Ratios reached statistical significance (Holt-Lunstad et al. 2015). This could partly explain the smaller Hazard Ratios in the present meta-analysis, since we only included studies that adjusted for a number of relevant covariates. In addition, the three previous meta-analyses (Holt-Lunstad et al. 2010, 2015; Rico-Uribe et al. 2018) were done on studies including also younger participants. It is conceivable that the effects of loneliness and social network size on mortality are smaller in older versus younger people. This is illustrated by a number of studies in the present analysis that investigated the association between loneliness and mortality in older adults over the age of 70 years: 6 out of 8 studies did not find a significant association (Table 2). Furthermore, smaller associations between loneliness and mortality were found when only the studies that followed participants for more than 10 years were included in the meta-analysis (Table 4). Apparently, when people grow older, other factors can become more important. This is in accordance with the results in the meta-analyses by Holt-Lunstad et al. (2015). They included adults aged under 50 to over 80 years and concluded that the effects of loneliness and social isolation on mortality risk diminished with age. Similarly, Lara et al. (2020) analyzed different age groups and found that loneliness was associated with mortality in younger and middle-aged adults, but not in older adults. Unfortunately, the effect of age has not been examined in the study by Rico-Uribe et al. (2018).
The large statistical heterogeneity between the included studies obviously influences the external validity. We tried to explain heterogeneity by adding sensitivity analyses, but these did not provide a sufficient explanation. One of the aspects that could underlie this heterogeneity is the fact that the range of loneliness prevalence is large, especially in the studies that were published before 2018: this range is 6–43% (Standard Deviation (SD) 12.5), whereas in the studies published after 2017 this range is 23–36% (SD 5.2). Other aspects are the age of included participants (≥ 60 versus ≥ 70) and the representativeness of the study population: some studies included a nationally representative population, whereas other studies included only urban or only rural populations. These aspects comprise clinical heterogeneity, which compromises generalizability to broader populations. Other aspects of heterogeneity can be described as methodological heterogeneity, such as differences in follow-up or the introduction or omitting of covariables (Deeks et al. 2008). The grouping of studies according to covariates and NOS-criteria resulted in lower heterogeneity for some groups. For example, including only loneliness studies that included a social contact variable resulted in little heterogeneity (I2˂40), while diminishing but not annihilating the Hazard Ratio. Moderate heterogeneity was reached in the loneliness studies when depression was not included as a covariate, and in the network size studies when depression was included. Again, the Hazard Ratios were influenced but remained elevated. The finding that the Hazard Ratios remained significantly elevated in less heterogeneous groups of studies might signify that loneliness and social network size are associated with mortality, although other variables are of influence. Gender differences might also explain heterogeneity. However, since only three studies provided separate outcomes for men and women, we did not perform additional sensitivity analyses with gender. In their meta-analysis, Rico-Uribe et al. (2018) divided studies by gender and concluded that for both men and women, there was a significant association between loneliness and mortality, with a slightly higher Effect Size for men. A recent study by Lennartsson et al. (2021) examined gender differences in the association between mortality and both loneliness and social isolation. They concluded that there were small differences: the association between loneliness and mortality was stronger in men, whereas the association between social isolation and mortality was stronger in women. However, this is only partly comparable to the studies in our meta-analysis, since they did not use social network size as a measure for social isolation but a social isolation index. The three studies in our meta-analysis that analyzed men and women separately showed various outcomes (see Fig. 2A).
The results of this meta-analysis have implications for both clinical practice and public health. For clinicians working with older patients, inquiring after the existence of loneliness or social isolation should be as common as inquiring after smoking, alcohol use or physical exercise, since the effects on mortality of loneliness and social isolation can be as deadly (Holt-Lunstad et al. 2010; House et al. 1988). Additionally, addressing loneliness and social isolation should be on the agenda of public health institutions. Local and national initiatives to combat loneliness and social isolation should be supported by governments. The relevance of these measures has recently been emphasized by studies showing heightened loneliness and social isolation in older adults as a consequence of the COVID-19 pandemic (Cudjoe et al. 2020; Kotwal et al. 2020).
The strengths of our study are that this is the first meta-analysis that included only older adults and that the quality of most of the included studies is good, based on the NOS-scores. An additional strength is the performance of sensitivity analyses to try to unravel the effects of different variables on the associations of loneliness and social network size with mortality. It should also be mentioned that studies that did not control for covariates were excluded, leading to more comparable studies. Furthermore, we were able to execute a comprehensive systematic search, and studies were selected by independent authors. Since an association between loneliness/network size and mortality was found in studies using cohorts that were representative for older adults in the community, our results may be relevant for the general public and for public health. Finally, although only studies in English were included, we were able to include not only studies from the Western world, but also from Brazil, China, Japan, Singapore and South Korea.
There are some limitations to this study too. Firstly, heterogeneity was large and could only partly be accounted for by grouping studies according to covariates, NOS-criteria, sample size and method of measuring loneliness. Large heterogeneity compromises generalizability to a broader population. Secondly, as our study involved merely observational longitudinal studies, causality cannot be assessed. Thirdly, since loneliness and social network size were measured at only one time point in the studies included, variance and persistence of loneliness have not been taken into account. Finally, the funnel plot showed that there is a possible publication bias regarding studies on network size, since only positive studies were published.
Conclusion
In conclusion, this meta-analysis shows that both loneliness and a small social network are associated with a small mortality risk in older adults, which appears to decrease over time. This risk is not influenced by the presence of depression. Since both subjective and objective aspects of social contacts appear to be relevant, interventions should be aimed both at the subjective experience of social contacts as well as the expansion of the size of the network. In addition, as a consequence of the fact that we included mostly epidemiological studies, there are important implications for public health. Targeting subjective and objective aspects of older adults’ social contacts should be on the agenda of preventive as well as personalized medicine. Finally, in order to gather evidence for either the objective or the subjective lack of social contacts to pose the greater mortality risk, more comparative studies need to be done.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors’ contributions
NS was involved in conceptualization; NS, HC and JD helped in literature search; NS, TH, HC, MS and JD contributed to data curation; NS, TH, JP and JD were involved in formal analysis; NS helped in original draft; review and editing were performed by TH, HC, MS, JP and JD. Preparation of this manuscript was in accordance with PRISMA guidelines.
Funding
No funding was received for conducting this research.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare that are of relevance to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Natasja Schutter, Email: natasja.schutter@arkinouderen.nl.
Tjalling J. Holwerda, Email: tjalling.holwerda@puntp.nl
Hannie C. Comijs, Email: h.comijs@kpnmail.nl
Max L. Stek, Email: m.stek@ggzingeest.nl
Jaap Peen, Email: jaap.peen@arkin.nl.
Jack J. M. Dekker, Email: jack.dekker@arkin.nl
References
- Adam EK, Hawkley LC, Kudielka BM, et al. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. PNAS. 2006;45:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguiar SG, Chen R, Willcox B, Takenaka C, Okamoto L, Lorenzo P, Masaki K (2020) Loneliness and depressive symptoms and 28-year mortality in older Japanese-American men: the Kuakini Honolulu Heart Program. JAGS 68:S2
- Ali T, Nilsson CJ, Weuve J, Rajan KB, Mendes de Leon CF. Effects of social network diversity on mortality, cognition and physical function in the elderly: a longitudinal analysis of the Chicago Health and Aging Project (CHAP) J Epidemiol Commun Health. 2018;72:990–996. doi: 10.1136/jech-2017-210236. [DOI] [PubMed] [Google Scholar]
- Avlund K, Damsgaard MT, Holstein BE. Social relations and mortality. an eleven year follow-up study of 70-year-old men and women in Denmark. Soc Sci Med. 1998;47:635–643. doi: 10.1016/S0277-9536(98)00122-1. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Bowling A, Farquhar M, Browne P. Life satisfaction and associations with social network and support variables in three samples of elderly people. Int J Geriatr Psychiatr. 1991;6:549–566. doi: 10.1002/gps.930060803. [DOI] [Google Scholar]
- Broese van Groenou M, Hoogendijk EO, Van Tilburg TG. Continued and new personal relationships in later life: differential effects of health. J Ageing Health. 2013;25:274–295. doi: 10.1177/0898264312468033. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, et al. Loneliness and health: potential mechanisms. Psychosom Med. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66:733–767. doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerhan JR, Wallace RB. Change in social ties and subsequent mortality in rural elders. Epidemiology. 1997;8:475–481. doi: 10.1097/00001648-199709000-00001. [DOI] [PubMed] [Google Scholar]
- Conde-Sala JL, Garre-Olmo J, Calvó-Perxas L, Turró-Garriga O, Vilalta-Franch J, López-Pousa S. Causes, mortality rates and risk factors of death in community-dwelling Europeans aged 50 years and over: results from the survey of health, ageing and retirement in Europe 2013–2015. Archiv Gerontol Geriatr. 2020;89:104035. doi: 10.1016/j.archger.2020.104035. [DOI] [PubMed] [Google Scholar]
- Cornwell EY, Waite L. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudjoe TKM, Kotwal AA. “Social distancing” amid a crisis in social isolation and loneliness. JAGS. 2020;68:E27–E29. doi: 10.1111/jgs.16527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Brito TRP, Nunes DP, Corona LP, Da Silva AT, De Oliveira Duarte YA. Low supply of social support as risk factor for mortality in the older adults. Arch Gerontol Geriatr. 2017;73:77–81. doi: 10.1016/j.archger.2017.07.016. [DOI] [PubMed] [Google Scholar]
- Deeks JJ, Higgins JPT, Altman DG (2008) Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S. (Eds.), Cochrane Handbook for systematic reviews of interventions. West Sussex, England: The Cochrane Collaboration and John Wiley & Sons Ltd
- De Jong GJ, Van Tilburg TG. A 6-item scale for overall, emotional, and social loneliness: confirmatory tests on survey data. Res Aging. 2006;28:582–598. doi: 10.1177/0164027506289723. [DOI] [Google Scholar]
- Drageset J, Eide GE, Kirkevold M, Ranhoff AH. Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: a five year follow-up study. J Clin Nurs. 2012;22:106–114. doi: 10.1111/j.1365-2702.2012.04209.x. [DOI] [PubMed] [Google Scholar]
- Dykstra PA, Van Tilburg TG, De Jong GJ. Changes in older adult loneliness. results from a seven-year longitudinal study. Res Aging. 2005;27:725–747. doi: 10.1177/0164027505279712. [DOI] [Google Scholar]
- Ellwardt L, Van Tilburg TG, Aartsen M, Wittek R, Steverink N. Mortality risk in older adults: a twenty-year longitudinal study. PLoS ONE. 2015 doi: 10.1371/journal.pone.0116731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elovainio M, Hakulinen C, Pulkki-Raback L, Virtanen M, Josefsson K, Jokela M, Vahtera J, Kivimaki M. Contribution of risk factors to excess mortality in isolated and lonely individuals: an analysis of data from the UK Biobank cohort study. Lancet Publ Health. 2017 doi: 10.1016/S2468-2667(17)30075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles LC, Glonek GFV, Luszcz MA, Andrews GR. Effect of social networks on 10 year survival in very old Australians: the Australian longitudinal study of aging. J Epidemiol Commun Health. 2005;59:574–579. doi: 10.1136/jech.2004.025429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25:132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoogendijk EO, Smit AP, Van Dam C, Schuster NA, De Breij S, Holwerda TJ, Huisman M, Dent E, Andrew MK. Frailty combined with loneliness or social isolation: an elevated risk for mortality in later life. JAGS. 2020;68:2587–2593. doi: 10.1111/jgs.16716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Holvast F, Burger H, De Waal MMW, Van Marwijk HWJ, Comijs HC, Verhaak PFM. Loneliness is associated with poor prognosis in late-life depression: longitudinal analysis of the Netherlands study of depression in older persons. J Aff Disorders. 2015;185:1–7. doi: 10.1016/j.jad.2015.06.036. [DOI] [PubMed] [Google Scholar]
- Holwerda TJ, Beekman ATF, Deeg DJH, Stek ML, Van Tilburg TG, Visser PJ, Schmand B, Jonker C, Schoevers RA. Increased risk of mortality associated with social isolation in older men: only when feeling lonely? Results from the Amsterdam Study of the Elderly (AMSTEL) Psychol Med. 2012;42:843–853. doi: 10.1017/S0033291711001772. [DOI] [PubMed] [Google Scholar]
- Holwerda TJ, Deeg DJH, Beekman ATF, et al. Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL) J Neurol Neurosurg Psychiatr. 2014;85:135–142. doi: 10.1136/jnnp-2012-302755. [DOI] [PubMed] [Google Scholar]
- Holwerda TJ, Van Tilburg TG, Deeg DJH, et al. Impact of loneliness and depression on mortality: results from the longitudinal ageing study Amsterdam. Br J Psychiatr. 2016;209:127–134. doi: 10.1192/bjp.bp.115.168005. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Iecovich E, Jacobs JM, Stessman J. Loneliness, social networks, and mortality: 18 years of follow-up. Int J Aging Human Dev. 2011;72:243–263. doi: 10.2190/AG.72.3.e. [DOI] [PubMed] [Google Scholar]
- Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, Kiecolt-Glaser JK. Loneliness promotes inflammation during acute stress. Psychol Sci. 2013;24:1089–1097. doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Christopher PF, Peng J, Bennett JM, Glaser R, Malarkey WB, Kiecolt-Glaser JK (2018) Threats to belonging, immune function, and eating behavior: an examination of sex and gender differences. Curr Psychiatry Rep 20:71 [DOI] [PubMed]
- Julsing JE, Kromhout D, Geleijnse JM, Giltay EJ. Loneliness and all-cause, cardiovascular and non-cardiovascular mortality in older men: the Zutphen Elderly Study. Am J Geriatr Psychiatr. 2016;24:475–484. doi: 10.1016/j.jagp.2016.01.136. [DOI] [PubMed] [Google Scholar]
- Jylha M, Aro S. Social ties and survival among the elderly in Tampere, Finland. Int J Epidemiol. 1989;18:158–164. doi: 10.1093/ije/18.1.158. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Janssen I, Ardern CI. Physical inactivity, excess adiposity and premature mortality. Obes Rev. 2003;4:257–290. doi: 10.1046/j.1467-789X.2003.00120.x. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E, Stampfer MJ, Willett WC. A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. J Epidemiol Commun Health. 1996;50:245–251. doi: 10.1136/jech.50.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Holt-Lunstad J, Newmark RL, Cenzer I, Smith AK, Covinsky KE, Escueta DP, Lee JM, Perissinotto CM. Social isolation and loneliness among San Francisco Bay area older adults during the COVID-19 shelter-in-place orders. JAGS. 2020 doi: 10.1111/jgs.16865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara E, Caballero FF, Rico-Uribe LA, Olaya B, Haro JM, Ayuso-Mateos JL, Miret M. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiat. 2019;34:1613–1622. doi: 10.1002/gps.5174. [DOI] [PubMed] [Google Scholar]
- Lara E, Moreno-Agostino D, Martín-María N, Miret M, Rico-Uribe LA, Olaya B, Cabello M, Haro JM, Ayuso-Mateos JL. Exploring the effect of loneliness on all-cause mortality: Are there differences between older adults and younger and middle-aged adults? Soc Sci Med. 2020;258:113087. doi: 10.1016/j.socscimed.2020.113087. [DOI] [PubMed] [Google Scholar]
- Lennartsson C, Rehnberg J, Dahlberg L. The association between loneliness, social isolation and all-cause mortality in a nationally representative sample of older women and men. Aging Ment Health. 2021 doi: 10.1080/13607863.2021.1976723. [DOI] [PubMed] [Google Scholar]
- Li H, Qian F, Hou C, Li X, Gao Q, Luo Y, Tao L, Yang X, Wang W, Zheng D, Guo X. Longitudinal changes in depressive symptoms and risks of cardiovascular disease and all-cause mortality: a nationwide population-based cohort study. The J Gerontol: Ser A. 2019;75:2200–2206. doi: 10.1093/gerona/glz228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74:907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y, Waite LJ. Loneliness and mortality among older adults in China. J Gerontol B Psychol Sci Soc Sci. 2014;69:633–645. doi: 10.1093/geronb/gbu007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin D, Leung J, Dobson A. Social support and mortality: if you’re sick, friends can’t save you. JAGS. 2011;59:1984–1986. doi: 10.1111/j.1532-5415.2011.03610_16.x. [DOI] [PubMed] [Google Scholar]
- Ng TKS, Visaria A, Ma S, Chan AWM. Differential effects of loneliness and depression on mortality. JAMDA. 2021;22:474–478. doi: 10.1016/j.jamda.2020.11.018. [DOI] [PubMed] [Google Scholar]
- Novak M, Waern M, Johansson L, Zettergren A, Ryden L, Wetterberg H, Gudmundsson P, Skoog I. Cardiovascular and all-cause mortality attributable to loneliness in older Swedish men and women. BMC Geriatr. 2020;20:201. doi: 10.1186/s12877-020-01603-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaya B, Domènech-Abella J, Moneta MV, Lara E, Caballero FF, Rico-Uribe LA, Haro JM. All-cause mortality and multimorbidity in older adults: the role of social support and loneliness. Exp Gerontol. 2017;99:120–127. doi: 10.1016/j.exger.2017.10.001. [DOI] [PubMed] [Google Scholar]
- Olsen RB, Olsen J, Gunner-Svensson F, Waldstrom B. Social networks and longevity. A 14 year follow-up study among elderly in Denmark. Soc Sci Med. 1991;33:1189–1195. doi: 10.1016/0277-9536(91)90235-5. [DOI] [PubMed] [Google Scholar]
- O’Luanaigh CO, Lawlor BA. Loneliness and the health of older people. Int J Geriatr Psychiatr. 2008;23:1213–1221. doi: 10.1002/gps.2054. [DOI] [PubMed] [Google Scholar]
- O’Súilleabháin PS, Gallagher S, Steptoe A. Loneliness, living alone, and all-cause mortality: the role of emotional and social loneliness in the elderly during 19 years of follow-up. Psychosom Med. 2019;V81:521–526. doi: 10.1097/PSY.0000000000000710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson AC, Veenstra G. Loneliness and risk of mortality: a longitudinal investigation in Alameda County, California. Soc Sci Med. 2010;71:181–186. doi: 10.1016/j.socscimed.2010.03.024. [DOI] [PubMed] [Google Scholar]
- Peerenboom L, Collard RM, Naarding P, Comijs HC. The association between depression and emotional and social loneliness in older persons and the influence of social support, cognitive functioning and personality: a cross-sectional study. J Aff Disord. 2015;182:26–31. doi: 10.1016/j.jad.2015.04.033. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Van Tilburg TH, Kriegsman DMW, Deeg DJH, Boeke AJP, Van Eijk JThM. Effects of social support and personal coping resources on mortality in older age: the Longitudinal Aging Study Amsterdam. Am J Epidemiol. 1997;146:510–519. doi: 10.1093/oxfordjournals.aje.a009305. [DOI] [PubMed] [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafnsson SB, Orrell M, d’Orsi E, Hogervorst E, Steptoe A. Loneliness, social integration, and incident dementia over 6 years: prospective findings from the English Longitudinal Study of Ageing. The J Gerontol Ser b, Psychol Sci Soc Sci. 2020;75:114–124. doi: 10.1093/geronb/gbx087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, Miret M. Association of loneliness with all-cause mortality: a meta-analysis. PLoS ONE. 2018 doi: 10.1371/journal.pone.0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth AR. Personal networks and mortality in later life: racial and ethnic differences. J Public Health. 2020 doi: 10.1093/pubmed/fdaa135. [DOI] [PubMed] [Google Scholar]
- Routasalo PE, Savikko N, Tilvis RS, Strandberg TE, Pitkälä KH. Social contacts and their relationship to loneliness among aged people – a population-based study. Gerontology. 2004;52:181–187. doi: 10.1159/000091828. [DOI] [PubMed] [Google Scholar]
- Schoenbach VJ, Kaplan BH, Fredman L, Kleinbaum DG. Social ties and mortality in Evans County, Georgia. Am J Epidemiol. 1986;123:577–591. doi: 10.1093/oxfordjournals.aje.a114278. [DOI] [PubMed] [Google Scholar]
- Schutter N, Holwerda TJ, Comijs HC, Naarding P, Van HL, Dekker JM, Stek ML, Rhebergen D. Loneliness, social network size, and mortality in older adults and the role of cortisol. Aging Ment Health. 2020 doi: 10.1080/13607863.2020.1843001. [DOI] [PubMed] [Google Scholar]
- Seeman T, Kaplan GA, Knudsen L, Cohen R, Guralnik J. Social network ties and mortality among the elderly in the Alameda County Study. Am J Epidemiol. 1987;126:714–723. doi: 10.1093/oxfordjournals.aje.a114711. [DOI] [PubMed] [Google Scholar]
- Shankar A, McMunn A, Banks J, Steptoe A. Loneliness, social isolation and behavioral and biological health indicators in older adults. Health Psychol. 2011;30:377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- Shiovitz-Ezra S, Ayalon L. Situational versus chronic loneliness as risk factors for all-cause mortality. Int Psychogeriatr. 2010;22:455–462. doi: 10.1017/S1041610209991426. [DOI] [PubMed] [Google Scholar]
- Shye D, Mullooly JP, Freeborn DK, Pope CR. Gender differences in the relationship between social network support and mortality: a longitudinal study of an elderly cohort. Soc Sci Med. 1995;41:935–947. doi: 10.1016/0277-9536(94)00404-H. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and endocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. PNAS. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stessman J, Rottenberg Y, Shimshilashvili I, Ein-Mor E, Jacobs JM. Loneliness, health, and longevity. J Gerontol A Biol Sci Med Sci. 2014;69:744–750. doi: 10.1093/gerona/glt147. [DOI] [PubMed] [Google Scholar]
- Sugisawa H, Liang J, Liu X (1994) Social network, social support, and mortality among older people in Japan. J Gerontol Soc Sci 49:S3–S13 [DOI] [PubMed]
- Tabue Teguo M, Simo-Tabue N, Stoykova R, Meillon C, Cogne M, Amieva H, Dartigues J-F. Feelings of loneliness and living alone as predictors of mortality in the elderly: The PAQUID Study. Psychosom Med. 2016;V78:904–909. doi: 10.1097/PSY.0000000000000386. [DOI] [PubMed] [Google Scholar]
- Tanskanen J, Anttilla T. A prospective study of social isolation, loneliness, and mortality in Finland. Am J Pub Health. 2016;106:2042–2048. doi: 10.2105/AJPH.2016.303431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007 doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilvis RS, Laitala V, Routasalo PE, Pitkal KH. Suffering from loneliness indicates significant mortality risk of older people. J Aging Res. 2011 doi: 10.4061/2011/534781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Tilburg T (1998) Losing and gaining in old age: changes in personal network size and social support in a four-year longitudinal study. J Gerontol Soc Sci 53B:S313–S323 [DOI] [PubMed]
- Victor C, Scambler S, Bond J, Bowling A. Being alone in later life: loneliness, social isolation and living alone. Rev Clin Gerontol. 2000;10:407–417. doi: 10.1017/S0959259800104101. [DOI] [Google Scholar]
- Vogt TM, Mullooly JP, Ernst D, Pope CR, Hollis JF. Social networks as predictors of ischemic heart disease, cancer, stroke and hypertension: incidence, survival and mortality. J Clin Epidemiol. 1992;45:659–666. doi: 10.1016/0895-4356(92)90138-D. [DOI] [PubMed] [Google Scholar]
- Wang H, Leng Y, Zhao E, Fleming J, Brayne C, The CC75C Study Collaboration Mortality risk of loneliness in the oldest old over a 10-year follow-up. Aging Ment Health. 2020;25:35–40. doi: 10.1080/13607863.2018.1510897. [DOI] [PubMed] [Google Scholar]
- Wei J, Hou R, Zhang X, Xu H, Xie L, Chandrasekar EK, Ying M, Goodman M. The association of late-life depression with all-cause and cardiovascular mortality among community-dwelling older adults: systematic review and meta-analysis. Br J Psychiatr. 2019;215:449–455. doi: 10.1192/bjp.2019.74. [DOI] [PubMed] [Google Scholar]
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Tugwell P (2000) The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomised studies in meta-analyses. EBM Reviews: 3rd Symposium on Systematic Reviews: Beyond the Basics. 15p. Jul 3–5, Oxford, UK
- Youm Y, Baldina E, Baek J. All-cause mortality and three aspects of social relationships: an eight-year follow-up of older adults from one entire Korean village. Sci Rep. 2021;11:465. doi: 10.1038/s41598-020-80684-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.