Abstract
Background
Postnatal care (PNC) is critical for both the mother and the infant to treat delivery complications and provide the mother with important information on caring for herself and her baby. However, only 17% of women and 13% of newborns in Ethiopia received a postnatal checkup within the first two days of birth. This figure is significantly lower than the least developed countries. This study aimed to assess the coverage and associated factors of PNC service utilization in South Gondar Zone, Northwest Ethiopia.
Method
A community-based cross-sectional study was conducted from September 2020 to May 2021. The data were gathered using an interviewer-administered structured questionnaire. A total of 434 women who gave birth within 2 years of the study were included in the analysis. Bivariable and multivariable logistic regression model was used to identify factors associated with PNC service utilization.
Result
The prevalence of women who used PNC services was 36.4%. The study showed that antenatal care visit, husbands who have a secondary education, women with a secondary education, daily laborer women, husbands working for the government or non-profit sector, delivered in a health institution, nearby hospitals, travel by car to the nearest health facility were positively associated with PNC utilization. While, not having a cell phone, rural women and not having road access to a health facility, have not been receiving counseling were negatively associated with PNC utilization.
Conclusion
The coverage of PNC service utilization in the study area was extremely low. Therefore, government and health care departments should pay special attention to uneducated women, women in rural areas, and women who are unemployed, are not exposed to mass media, and do not have access to transportation to improve PNC service utilization. Furthermore, programs educating mothers on the benefits of antenatal checkups and safer places of childbirth should be considered to increase PNC service utilization.
Keywords: postnatal care, logistic regression, South Gondar, women, utilization
Background
Maternal mortality has been a major focus of public health programs. It is also used to determine the level of development, health, and socioeconomic position of a population. One of the Sustainable Development Goals (SDGs) aim is to reduce maternal mortality and improve maternal health (Lim et al., 2016; UNICEF, 2016).
In 2017, approximately 295 000 women died during and after pregnancy and childbirth. Most of these deaths (94%) occurred in developing countries and most could have been prevented. Sub-Saharan Africa and Southern Asia accounted for about 86% (254,000) of the estimated global maternal deaths. Sub-Saharan Africa alone accounted for nearly two-thirds (196,000) of maternal deaths, while Southern Asia accounted for nearly one-fifth (58,000) (UNICEF & WHO, 2015). In 2015, maternal mortality was 239 per 100,000 live births in developing countries, compared to 12 per 100,000 live births in developed countries (WHO, 2018). Ethiopia has one of the highest maternal death rates in the developing world. According to 2016 Ethiopian Demographic and Health Survey, maternal mortality is 412 deaths per 100,000 live births (EDHS). This indicates that Ethiopian women have a 1 in 243 chance of dying over their lifetime. This maternal death rate is much higher than the SDG of 70 maternal deaths per 100,000 live births (CSA, 2016; Tessema et al., 2017). About 75% of all maternal deaths are caused by severe bleeding (usually after childbirth), infections (usually after childbirth), high blood pressure during pregnancy (pre-eclampsia and eclampsia), delivery complications, and botched abortions. Preterm birth, asphyxia, and severe infections were responsible for two-thirds of all neonatal deaths, while hemorrhage and sepsis accounted for 27.1% and 10.7% of maternal mortality, respectively (Gebrehiwot et al., 2018; Say et al., 2014).
Postnatal care (PNC) use is one of the most essential and critical methods for reducing high mother mortality rates. However, Ethiopia is one of the countries with low PNC coverage and a large geographical (urban-rural) gap. As a result, the government of Ethiopia's major initiatives for achieving Universal Health Coverage includes exempted services or cost-sharing for high-priority programs (Health, 2015). PNC services are provided free of charge to village dwellers in Ethiopia, although only 17% of women obtained a postnatal check-up in the EDHS 2016 which is far from 26% of health facilities delivery. Only 18.4% of women received a postnatal checkup within the first two days of delivery in the Amhara region including this study area (CSA & ICF, 2012; Debie & Tesema, 2021).
Review of Literature
The use of PNC services has been attempted to be quantified by several researchers, who have identified some linked characteristics. Several studies have been conducted to investigate the utilization of PNC, as well as the factors that influence it. Several studies have linked it to maternal-related influencing factors such as age of women (Yoseph et al., 2021), educational level of the women (Ahinkorah et al., 2021), occupational status of women and husbands (Ahinkorah et al., 2021), wealth index (Ahinkorah et al., 2021), antenatal care (ANC) (Belachew et al., 2016), media exposure (Ahinkorah et al., 2021), place of delivery (Belachew et al., 2016; Limenih et al., 2016; Somefun & Ibisomi, 2016), wealth index (Mekonnen et al., 2021; Somefun & Ibisomi, 2016). In addition, the utilization of PNC can be affected by other factors, such as time taken to get the nearest health facility (Ndugga et al., 2020), planned and wanted pregnancy (Yoseph et al., 2021), health profession preferred by women, source of information about maternal care, duty service of maternal health care (Ahinkorah et al., 2021), number of living children (Debie & Tesema, 2021), cultural practices (Belachew et al., 2016; Miller et al., 2016), lack of counselling, transportation problem, distance from the health institutions (Hordofa et al., 2015; Mukonka et al., 2018; Somefun & Ibisomi, 2016). Different cultures and socio-economic status within a society have varied factors of PNC service utilization. However, the determinants of utilization of PNC services are not the same across different cultures and socioeconomic status within a society. Determinants of PNC service utilization differ from place to place. In order to improve mother and child health services, it is important to assess factors affecting PNC service utilization in different settings. Therefore, this study aimed to assess the coverage and identify associated factors of PNC service utilization in South Gondar Zone, Northwest Ethiopia.
Methods
Design
A community-based cross-sectional study design was conducted in South Gondar Zone, in the Amhara region of Northwest Ethiopia, from September 2020 to May 2021. Debre Tabor is the capital city of the South Gondar Zone and is located around 666 km from Addis Ababa, the capital city of Ethiopia, and 105 km away from Bahir Dar, the capital city of the Amhara region. According to the 2007 Central Statistical Agency Report, the population of South Gondar Zone is 2,051,738, of which 1,041,061 were men and 1,010,677 were women. South Gondar is bordered on the south by East Gojjam, on the southwest by West Gojjam and Bahir Dar, on the west by Lake Tana, on the north by North Gondar, on the northeast by Wag Hemra, on the east by North Wollo, and on the southeast by South Wollo; the Abbay River separates South Gondar from the two Gojjam Zones. Currently, the south Gondar zone had one referral hospital, seven district hospitals, and 94 health centers. In this zone, a total of 468,238 households were counted, resulting in an average of 4.38 people per household. Among 13 woredas in the South Gondar zone four districts/woredas were randomly selected (these randomly selected woredas are Debre Tabor town, Laye Gayint, Libokekem, and Fogera).
Research Questions
Is postnatal care utilization related to the maternal education?
Is postnatal care utilization related to the media exposure, and source of information?
Is the women, and their husbands occupation related to postnatal care utilization?
Is there a relationship between the postnatal care utilization of women's and presence of health facility in kebele?
Is the postnatal care utilization related to the transportation, and road accessibility to the nearest health facility?
Is planned pregnancy, and wanted pregnancy related to postnatal care utilization?
Sample
Prior to the actual data collection, the emphasis was placed on selecting the right sample size, which mostly depended on the study's objective, the available resources, and the precision required. The sample size was determined using a single population proportion formula with the assumption; 95% confidence interval, 4.7% margin of error, 10% estimated non-response rate, and taking 34.6% proportion of PNC utilization in East Gojjam Zone, Northwest Ethiopia (Zeleke et al., 2021) then, the required sample size was 434. The study's individuals were assessed using a multi-stage sampling method. To calculate the number of households in each selected kebele, the sample size was distributed proportionally (the smallest administrative unit in Ethiopia). Finally, using computer-generated random numbers in an Excel spreadsheet, simple random sampling was used to choose study participants by name from the sampling frame.
Inclusion Criteria and Exclusion Criteria
All women from 15 to 49 years of age who had given birth within the previous 10 months were eligible for the survey. Women admitted for most of their postnatal periods, women who gave birth more than 10 months ago, and women who had stillbirths were all excluded from the study.
Data Collection Tools and Methods
Data Collection Tool
This instrument was a self-administered survey questionnaire. A validated, pre-tested, and well-structured Amharic version questionnaire with closed-ended questions on PNC was used to collect data. To assure the quality of data, and to determine the reliability of research instruments, pilot study was conducted on 30 respondents who met the inclusion criteria but were not included in the current data set to ensure clarity and applicability of the tools. The researchers developed the questionnaire based on guidelines from the World Health Organization (WHO), and the Ethiopian Ministry of Health and by reviewing different types of literature. Content validity was tested by expert academic members and proved to be valid for use. The research instruments reliability was tested by pilot study and it was found to be reliable. The questionnaire was first written in English and then translated into Amharic to ensure that it was appropriate for approaching research participants, and then back to English by language experts to ensure consistency. The socio-demographic, accessibility, behavioral, and obstetric factors variables were all included in the questionnaire.
Data Collection
After approval from the Institutional Review Board of the higher institute in Debre tabor University, Ethiopia, this research was conducted. Before the data collection date, for ensuring data quality, one-day training was given to supervisors and data collectors on the study's goal, data gathering processes, data collection tools, respondents’ approach, data confidentiality, and respondents’ rights. Proper categorization and coding of the data, completeness, and consistency of the collected data were checked daily during data collection by the supervisor and principal investigators. Double entry and data cleaning were deliberating.
Study Variables
Dependent Variables
The outcome variable was the utilization of PNC services. The variable was developed using the WHO definition of PNC, which is described as seeking postnatal treatment for the mother within 6 weeks of delivery at a dispensary, health center, or hospital (government or private).
Independent Variables
The potential variables associated with PNC service utilization have been selected based on different works of literature (Akibu et al., 2018; Bwalya et al., 2017; Debie & Tesema, 2021; Mosiur Rahman et al., 2011; Seid & Ahmed, 2020; Zeleke et al., 2021). Age of women, religion, education level of women, occupation of women, education level of husband's, husband's occupation, family size, monthly income, own mobile telephone, the decision of maternal care service utilization, access to mass media, residence, and marital status were considered to be explanatory variables within the study.
Statistical Analysis
After data collection, each questionnaire was reviewed for completeness and consistency by principal investigators and supervisor. Data were cleaned, edited, coded, and entered by using SPSS version 25 and exported to R version 4.1.0 for further analysis. The data were analyzed using R statistical software. Categorical variables were summarized using frequencies, percentages, and a bar chart. Bivariate and multivariable binary logistic regression model was used to identify factors associated with PNC utilization. Variables that demonstrated statistical significance in bivariate analysis at a p-value of .20 were entered into multivariable logistic regression. To assess the strength of the associations, adjusted odds ratios (AOR) with 95% confidence intervals (CI) were estimated, and statistical significance was declared at a p-value of .05.
Ethical Clearance
Ethical approval for this study was obtained from Ethical Approval Committee of facility of natural and computational science, Debre Tabor University, Ethiopia. Written informed consent was obtained from each study participant before participation in the study after the objectives of the study were fully explained to them. Each participant signed and returned a written informed consent form. The confidentiality of participants was ensured and guaranteed, all identities have been replaced by codes and numbers in this research. The returned survey questionnaires were kept at the locked place for data security.
Results
Sample Characteristics
A total of 434 mothers participated in the study. The mean age of respondents was 33.63 years with a standard deviation of 7.19. About 188 (43.3%) of the respondents were in the age group of greater than 34 years. Most of the participants 390 (89.9%) were Orthodox and married. Regarding educational status, 194 (44.7%) mothers and 155 (35.7%) respondents’ husbands were unable to read and write. Regarding occupation, 157 (36.2%) mothers and 228 (52.5%) respondents’ husbands were a farmer. More than half, 252 (58.1%) of the respondents were rural residents (Table 1).
Table 1.
Socio-Demographic Characteristics of Respondents in South Gondar Zone.
| Variable | Categories | Frequency | Percentage |
|---|---|---|---|
| Age of respondents | <25 | 48 | 11.1 |
| 25–29 | 91 | 21.0 | |
| 30–34 | 107 | 24.7 | |
| >34 | 188 | 43.3 | |
| Respondent religion | Orthodox | 390 | 89.9 |
| Muslim | 37 | 8.5 | |
| Others | 7 | 1.6 | |
| Education level of respondent | Illiterate | 194 | 44.7 |
| Only read and write (no formal education) | 35 | 8.1 | |
| Primary educated (Grade1–8) | 85 | 19.6 | |
| Secondary school (Grade 9–12) | 49 | 11.3 | |
| Tertiary level | 71 | 16.4 | |
| Respondent occupation | Housewife | 152 | 35.0 |
| Farmer | 157 | 36.2 | |
| Governmental or non-governmental employed | 62 | 14.3 | |
| Merchant | 55 | 12.7 | |
| Daily Laborer | 8 | 1.8 | |
| Education level of husband's | Illiterate | 155 | 35.7 |
| Only read and write (no formal education) | 57 | 13.1 | |
| Primary educated (Grade1–8) | 75 | 17.3 | |
| Secondary school (Grade 9–12) | 60 | 13.8 | |
| Tertiary level | 87 | 20.0 | |
| Husband's occupation | Farmer | 228 | 52.5 |
| Governmental or non-governmental employed | 100 | 23.0 | |
| Merchant | 81 | 18.7 | |
| Daily Laborer | 25 | 5.8 | |
| Family size | 2–4 | 175 | 40.3 |
| 5–7 | 188 | 43.3 | |
| 8 and above | 71 | 16.4 | |
| Monthly income (in Birr) | < = 1000 | 63 | 14.5 |
| 1001–2500 | 124 | 28.6 | |
| 2501–5000 | 177 | 40.8 | |
| 5001 and above | 70 | 16.1 | |
| Owns mobile telephone | No | 209 | 48.2 |
| Yes | 225 | 51.8 | |
| Decision of maternal care service utilization | Husband | 14 | 3.2 |
| Wife | 90 | 20.7 | |
| Both | 330 | 76.0 | |
| Access to mass media | Exposed to mass media | 190 | 43.8 |
| Not exposed to mass media | 244 | 56.2 | |
| Residence | Urban | 182 | 41.9 |
| Rural | 252 | 58.1 | |
| Marital status | Married | 390 | 89.9 |
| Divorced | 24 | 5.5 | |
| Windowed | 14 | 3.2 | |
| Single | 6 | 1.4 |
Approximately three-fourths, 321 (74%) of participants had their first pregnancy after age 19 years. Most, 369 (85.0%) of pregnancies were wanted and planned. Above half of, 241 (55.5%) respondents had less than four living children while 193 (44.5%) reported having more than three living children. Around one-fourth, 197 (45.4%) of the respondents was their first pregnancy. About 79 (18.2%) of women had a history of abortion and 68 (15.7%) of the respondent had a history of neonatal death. Nearly half, 205 (47.2%) of the respondents were married between the age of 20–24 years (Table 2).
Table 2.
Obstetric Characteristics of Respondents in South Gondar Zone.
| Variable | Categories | Frequency | Percentage |
|---|---|---|---|
| Birth order | First | 81 | 18.7 |
| 2–3 | 156 | 35.9 | |
| 4 and above | 197 | 45.4 | |
| Counseling about maternal health care | No | 90 | 20.7 |
| Yes | 344 | 79.3 | |
| Size of child at birth | Small | 111 | 25.6 |
| Average | 240 | 55.3 | |
| Large | 83 | 19.1 | |
| Maternal health insurance | No | 162 | 37.3 |
| Yes | 272 | 62.7 | |
| Health Provider Behavior | Good | 364 | 83.9 |
| Poor | 70 | 16.1 | |
| Post delivery shelter | No | 42 | 9.7 |
| Yes | 392 | 90.3 | |
| Health facility in kebele | No | 61 | 14.1 |
| Yes | 373 | 85.9 | |
| Nearest health institution | Health center | 387 | 89.2 |
| Privet clinic | 14 | 3.2 | |
| Hospital | 33 | 7.6 | |
| Duty service of maternal health care | No | 172 | 39.6 |
| Yes | 262 | 60.4 | |
| Transportation | On foot | 293 | 67.5 |
| By car | 141 | 32.5 | |
| Number of living children | 1–3 | 241 | 55.5 |
| 4 and above | 193 | 44.5 | |
| Experienced child death | No | 325 | 74.9 |
| Yes | 109 | 25.1 | |
| Road accessibility to the HF | No | 235 | 54.1 |
| Yes | 199 | 45.9 | |
| Place of previous delivery | Home | 187 | 43.1 |
| Health institution | 247 | 56.9 | |
| Did you face any health problem in the last pregnancy? | No | 279 | 64.3 |
| Yes | 155 | 35.7 | |
| Planned pregnancy | No | 65 | 15.0 |
| Yes | 369 | 85.0 | |
| Wanted pregnancy | No | 65 | 15.0 |
| Yes | 369 | 85.0 | |
| Experienced death of neonate age less than seven day | No | 366 | 84.3 |
| Yes | 68 | 15.7 | |
| History of abortion | No | 355 | 81.8 |
| Yes | 79 | 18.2 | |
| Age at first pregnancy | <20 | 113 | 26.0 |
| > = 20 | 321 | 74.0 | |
| Age at first marriage | Less than 15 | 57 | 13.1 |
| 15–19 | 146 | 33.6 | |
| 20–24 | 205 | 47.2 | |
| > = 25 | 26 | 6.0 | |
| The time taken to get the nearest health facility | Below 1 h | 243 | 56.0 |
| 1–2 h | 162 | 37.3 | |
| Above 2 h | 29 | 6.7 |
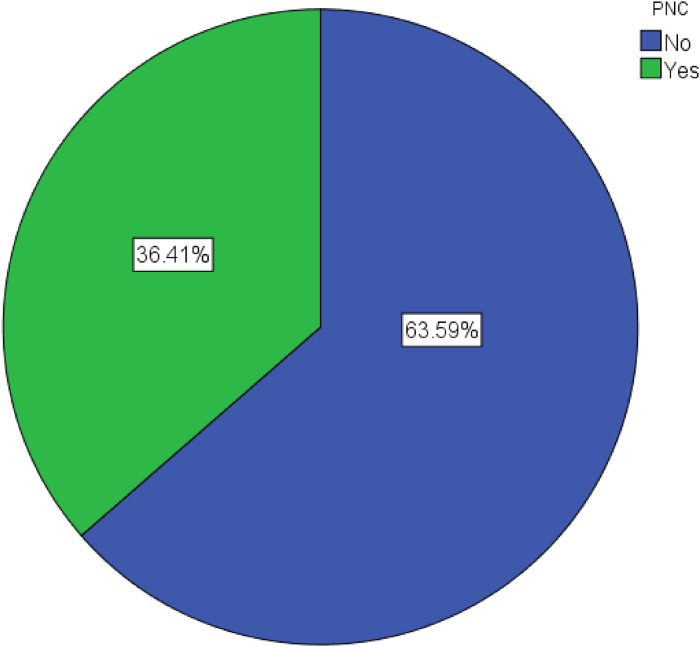
Prevalence of Postnatal Care Utilization
The prevalence of PNC in the south Gondar zone is shown in Figure 1. The percentage of women who used PNC services was 36.41%. Majority of women (63.59%) were not used PNC (Figure 1).
Figure 1.
The prevalence of PNC utilization in South Gonder Zone.
Factors Associated With Postnatal Care Utilization Among Reproductive-age Women
Table 3 summarizes the results of bivariate and multivariable binary logistic regression analysis. The study indicated that maternal education, maternal occupation, husbands education, husbands occupation, media exposure, time taken to get the nearest health facility, planned pregnancy, wanted pregnancy, health profession preferred by women, source of information about maternal care, media exposure, residence, duty service of maternal health care, number of living children, road accessibility to the nearest health facility, health provider behavior, presence of health facility in kebele, transportation, family size were significantly associated with PNC utilization.
Table 3.
Factors Associated With Postnatal Care Utilization in South Gondar Zone.
| Variables | Postnatal care (PNC) | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| No (%) | Yes (%) | |||
| Education level of women | ||||
| Illiterate | 161 (58.3) | 33 (20.9) | 1 | 1 |
| Only read and write (no formal education) | 18 (6.5) | 17 (10.8) | 4.608 (2.152, 9.866)* | 3.931 (1.757, 8.795)* |
| Primary educated (Grade 1–8) | 51 (18.5) | 34 (21.5) | 3.253 (1.833, 5.770)* | 3.490 (1.841, 6.616)* |
| Secondary school (Grade 9–12) | 16 (5.8) | 33 (20.9) | 10.062 (4.973,20.361)* | 9.967 (4.472, 13.212)* |
| Tertiary level | 30 (10.9) | 41 (25.9) | 6.668 (3.653, 12.170)* | 8.039 (3.156, 20.480)* |
| Respondent occupation | ||||
| Housewife | 78 (28.3) | 74 (46.8) | 1 | 1 |
| Farmer | 127 (46.0) | 30 (19.0) | 0.249 (0.150, 0.414)* | 0.536 (0.298, 0.965)* |
| Governmental or non-governmental employee | 28 (10.1) | 34 (21.5) | 1.280 (0.708, 2.315) | 0.510 (0.212, 1.229) |
| Merchant | 41 (14.9) | 14 (8.9) | 0.360 (0.181, 0.714)* | 0.306 (0.144, 0.648)* |
| Daily Laborer | 2 (0.7) | 6 (3.8) | 3.162 (0.619, 6.165) | 5.900 (1.064, 9.701)* |
| Education level of husband's | ||||
| Illiterate | 121 (43.8) | 34 (21.5) | 1 | 1 |
| Only read and write (no formal education) | 42 (15.2) | 15 (9.5) | 1.271 (0.630, 2.564) | 1.174 (0.575, 2.398) |
| Primary educated (Grade 1–8) | 53 (19.2) | 22 (13.9) | 1.477 (0.790, 2.763) | 1.113 (0.562, 2.201) |
| Secondary school (Grade 9–12) | 22 (8.0) | 38 (24.1) | 6.147 (3.214, 11.756)* | 4.082 (1.933, 8.622)* |
| Tertiary level | 38 (13.8) | 49 (31.0) | 4.589 (2.597, 8.110)* | 2.610 (1.100, 6.194)* |
| Husband's occupation | ||||
| Farmer | 175 (63.4) | 53 (33.5) | 1 | 1 |
| Governmental or none-governmental employee | 44 (15.9) | 56 (35.4) | 4.202 (2.548, 6.931)* | 4.297 (1.989, 9.281)* |
| Merchant | 46 (16.7) | 35 (22.2) | 2.512 (1.469, 4.296)* | 2.760 (1.138, 6.695)* |
| Daily laborer | 11 (4.0) | 14 (8.9) | 4.202 (1.801, 9.806)* | 2.831 (1.083, 7.400)* |
| Access to mass media | ||||
| Exposed to mass media | 89 (32.2) | 10 (63.9) | ||
| Not exposed to mass media | 187 (67.8) | 57 (36.1) | 0.269 (0.178, 0.405)* | 0.384 (0.244, 0.606)* |
| The time taken to get the nearest HF | ||||
| Below 1 h | 125 (45.3) | 118 (74.7) | 1 | 1 |
| 1–2 h | 126 (45.7) | 36 (22.8) | 0.303 (0.193, 0.474)* | 0.463 (0.282, 0.761)* |
| Above 2 h | 25 (9.1) | 4 (2.5) | 0.169 (0.057, 0.502)* | 0.256 (0.084, 0.778)* |
| Place of delivery | ||||
| Home | 116 (42.0) | 131 (82.9) | 1 | 1 |
| Health institution | 160 (58.0) | 27 (17.1) | 11.690 (5.268,25.939)* | 8.184 (3.616, 18.523)* |
| Antenatal care (ANC) visit | ||||
| No | 1 | 1 | ||
| Yes | 3.979 (2.545, 6.221)* | 2.573 (1.599, 4.141)* | ||
| Health profession preferred by women | ||||
| Yes | 41 (14.9) | 92 (58.2) | 1 | 1 |
| No | 235 (85.1) | 66 (41.8) | 0.125 (0.079,0.198)* | 0.131 (0.08, 0.213)* |
| Counseling about PNC | ||||
| Yes | 196 (71.0) | 148 (93.7) | 1 | 1 |
| No | 80 (29.0) | 10 (6.3) | 0.166 (0.083, 0.330)* | 0.145 (0.070, 0.300)* |
| Owns mobile telephone | ||||
| Yes | 105 (38.0) | 120 (75.9) | ||
| No | 171 (62.0) | 38 (24.1) | 0.194 (0.125, 0.301)* | 0.208 (0.132, 0.329)* |
| Residence | ||||
| Urban | 87 (31.5) | 95 (60.1) | 1 | 1 |
| Rural | 189 (68.5) | 63 (39.9) | 0.588 (0.367, 0.942)* | 0.584 (0.364, 0.936)* |
| Road accessibility to the HF | ||||
| Yes | 86 (31.2) | 113 (71.5) | 1 | 1 |
| No | 190 (68.8) | 45 (28.5) | 0.230 (0.143, 0.370)* | 0.227 (0.140, 0.366)* |
| Health facility in the kebele | ||||
| Yes | 230 (83.3) | 143 (90.5) | 1 | 1 |
| No | 46 (16.7) | 15 (9.5) | 0.524 (0.282, 0.974)* | 0.479 (0.253, 0.905)* |
| Nearest health institution | ||||
| Health center | 255 (92.4) | 132 (83.5) | ||
| Privet clinic | 9 (3.3) | 5 (3.2) | 1.073 (0.353, 3.267)* | 1.028 (0.336, 3.144)* |
| Hospital | 12 (4.3) | 21 (13.3) | 3.381 (1.613, 7.084)* | 3.650 (1.720, 7.747)* |
| Duty service of maternal health care | ||||
| Yes | 149 (54.0) | 113 (71.5) | 1 | 1 |
| No | 127 (46.0) | 45 (28.5) | 0.513 (0.335, 0.787)* | 0.467 (0.307, 0.710)* |
| Transportation to health facility | ||||
| On foot | 221 (80.1) | 72 (45.6) | ||
| By car | 55 (19.9) | 86 (54.4) | 4.799 (3.121, 7.381)* | 4.341 (2.794, 6.745)* |
| Family size | ||||
| 2–4 | 96 (34.8) | 79 (50.0) | 1 | 1 |
| 5–7 | 127 (46.0) | 61 (38.6) | 0.584 (0.381, 0.894)* | 0.570 (0.352, 0.925)* |
| 8 and above | 53 (19.2) | 18 (11.4) | 0.413 (0.224, 0.761)* | 0.407 (0.206, 0.803)* |
| Number of living child | ||||
| 1–3 | 131 (47.5) | 110 (69.6) | 1 | 1 |
| 4 and above | 145 (52.5) | 48 (30.4) | 0.394 (0.261, 0.596)* | 0.385 (0.204, 0.725)* |
ANC = antenatal care; AOR = adjusted odds ratio; COR = crude odds ratio; HF = health facility; PNC = postnatal care; 1 = reference category.
*Significance at 5% of level of significance.
Relative to women who had no ANC visits, those who had one or more ANC visits were 2.573 (AOR = 2.573; 95%CI: 1.599, 4.141) times more likely to use PNC services. Women with a husband with a secondary education were 4.082 (AOR = 4.082; 95%CI: 1.933, 8.622) times more likely to use PNC than women with an illiterate husband. In comparison to uneducated women, women who completed secondary school were 9.967 (AOR = 9.967; 95%CI: 4.472, 13.212) times more likely to use PNC. In comparison to housewife women, daily laborer women were 5.9 (AOR = 5.900; 95%CI: 1.064, 9.701) times more likely to use PNC services. Women whose husbands worked for the government or non-profit sector were 4.297 (AOR = 4.297; 95%CI: 1.989, 9.281) times more likely to use PNC services than women whose husbands worked as farmers. The odds of PNC service utilization were lower for women who had no media exposure than media users (AOR = 0.384; 95%CI: 0.244, 0.606). When compared to when it took less than 2 h to get to the nearest health institution, people who took more than 2 h were 74.4% (AOR = 0.256; 95%CI: 0.084, 0.778) less likely to use PNC services. When compared to women who were delivered at home, women who were delivered in a health institution were 8.184 (AOR = 8.184; 95%CI: 3.616, 18.523) times more likely to use PNC services. Women who did not choose a health profession for health care service were 86.9% less likely to use PNC services than women who did. When compared to women who own a cell phone, women who do not own a cell phone were 79.2% (AOR = 0.208; 95%CI: 0.132, 0.329) less likely to use PNC service. Rural women were 54.6% (AOR = 0.584; 95%CI: 0.364, 0.936) less likely to use PNC service than urban women. When compared to women who had road access to the health facility, women who do not have road access to the health facility were 77.3% (AOR = 0. 227; 95%CI: 0.140, 0.366) less likely to use PNC service. Women who had not been counseled about PNC during their ANC visits were 85.5% (AOR = 0.145; 95% CI: 0.070, 0.300) less likely to use PNC than mothers who had been counseled. The odds of using PNC services among women who go to the nearest health facility by car were 4.341 (AOR = 4.341; 95%CI: 2.794, 6.745) higher than those women who go on foot. Women who did not own a mobile phone were 0.208 (AOR = 0.208; 95% CI: 0.132, 0.329) times less likely to use PNC services than those who did. Women who did not have a health facility in their kebele had (AOR = 0.479; 95% CI: 0.253, 0.905) a lower likelihood of using PNC services than women who did. Women whose nearest health institution is a hospital were 3.650 (AOR = 3.650; 95% CI: 1.720, 7.747) times more likely to use PNC services than those women whose nearest health institution is a health center. Women with a household size of eight or more were 0.407 (AOR = 0.407; 95% CI: 0.206, 0.803) times less likely to use PNC services than women with a household size of four or less. Women with eight or more children were 0.385 (AOR = 0.385; 95% CI: 0.204, 0.725) times less likely to use PNC services than women with four or fewer children. Women whose husbands worked in government or non-government were 4.297 (AOR = 4.297; 95% CI: 1.989, 9.281) times more likely to use PNC services than women whose husbands were farmers (Table 3).
Discussion
In developing countries, PNC is one of the most effective strategies for improving maternal health outcomes. Accordingly, the purpose of this study was to look into the prevalence and predictors of PNC use among women aged 15–49 in the South Gondar Zone. The coverage of PNC service utilization was 36.4% in south Gondar Zone. This prevalence is lower than that recorded in Ugandan (50%) (Ndugga et al., 2020), Zambia (55% %) (Bwalya et al., 2017), Debre Birhan Town, North Ethiopia (83.3%) (Angore et al., 2018), Indonesia (78.4%) (Idris & Syafriyanti, 2021), rural Ghana (74%) (Appiah et al., 2021), and sub-Saharan Africa countries (52.48%) (Tessema et al., 2020). It is, however, higher than what was reported in East Gojjam Zone, Northwest Ethiopia (34.6%) (Zeleke et al., 2021), Northern Shoa, Ethiopia (28.4%) (Akibu et al., 2018), Tigray, Northern Ethiopia (8%) (Berhe et al., 2019), Ezha district of southern Ethiopia (23.9%) (Habte et al., 2021), and rural Myanmar (25.20%) (Mon et al., 2018). The observed difference could be caused by differences in healthcare infrastructure and socio-cultural differences between countries. The possible causes of these differences include a variety of complex factors such as policy variations against maternal health services, variability in the quality of care, and other factors such as circumstances, value, and understandings of PNC services.
ANC visit is one of the factors that influence the utilization of PNC services. In comparison to women who had no ANC visits, those who had one or more ANC visits were more likely to use PNC services. The finding is similar to study conducted in Bangladesh (Adane et al., 2020b), Halaba kulito town, Southern Ethiopia (Abebo & Tesfaye, 2018), Uganda (Ndugga et al., 2020), and Mwingi district, Kenya (Nzioki et al., 2015). This is due to the fact that mothers who utilize ANC services during pregnancy are more likely to engage with health workers, who can influence mothers’ decisions about whether or not to use PNC services. ANC visits, in particular, can improve mothers’ motivation to use sustainable maternal health care, such as giving birth with the help of health workers and using PNC services.
When compared to women who gave birth at home, those who gave birth at a health facility were more likely to use PNC services. The finding is similar to studies conducted in Ugandan (Ndugga et al., 2020), Halaba Kulito town, Southern Ethiopia (Abebo & Tesfaye, 2018), Ethiopia (Adane et al., 2020; Ayele et al., 2019), and Bangladesh (Adane et al., 2020b). This could be due to women who give birth in a health facility have a better chance of being informed, and educated about the different types, benefits, and options for PNC services, as well as the danger signals of postpartum depression.
Rural women were less likely to use the PNC service than urban women. This finding is supported by the studies conducted in Zimbabwe and Ethiopia (Adane et al., 2020; Muchabaiwa et al., 2012), and Swaziland and Uganda (Ndugga et al., 2020; Tsawe et al., 2015). The reason for this could be that urban women have better education, access to health care, and are more aware of the importance of PNC service utilization (Fenta et al., 2021).
The education level of women and husbands had positively associated with PNC services. Educated women were more likely to use PNC services than uneducated women. This is consistent with results from studies in Ethiopia (Adane et al., 2020), Bangladesh (Adane et al., 2020b), Nigeria (Igboanusi et al., 2019; Sydavong & Goto, 2019), Uganda (Ndugga et al., 2020), and Mwingi district, Kenya (Nzioki et al., 2015). This may be because education plays an important role in enhancing female autonomy and assisting women in developing greater confidence and capability in making health-related decisions for themselves. As a result, literate women seek out higher-quality health services and have a greater ability to use health-care inputs that result in better health outcomes. Women whose husbands were literate were more likely to use PNC than women whose husbands were illiterate. This finding was supported by the studies done in Ethiopia (Adane et al., 2020b), Bangladesh (Adane et al., 2020b), Nigeria (Igboanusi et al., 2019; Ononokpono et al., 2020). The potential explanation for this may be that educated husbands communicate better with their wives and are more willing to discuss the use of PNC services as well as other maternal health services (Adane et al., 2020b). This could also give their wives more independence (Tarekegn et al., 2014).
Women who had no exposure to the media were less likely to use PNC services than women who had exposure to the media. This finding was supported by the studies done in Ethiopia (Seid & Ahmed, 2020), Nigeria (Igboanusi et al., 2019; Ononokpono et al., 2020), and Uganda (Ndugga et al., 2020). The possible explanation for this result may be that women who had media exposure could have adequate information about maternal health care services. Women who have access to the media have been found to have more ANC visits, allowing them to learn about the benefits of PNC after birth (Seid & Ahmed, 2020).
In comparison to housewife women, Women who worked daily labor were more likely to use PNC services. This result was in line with the studies conducted in rural Ghana (Appiah et al., 2021), and Mwingi district, Kenya (Nzioki et al., 2015). Working mothers can boost their financial ability to benefit from health promotion and make independent decisions about whether or not to use health services (Izudi & Amongin, 2015). Furthermore, the status of women in working households has an impact on their decision to utilize health services: women who work independently are more likely to use health services than those who are reliant on their husbands or other family members (Fawole & Adeoye, 2015). Women whose husbands worked in government or non-government organizations were more likely to use PNC services than women whose husbands were farmers. This finding is in line with findings of studies in Mangochi district, Malawi (Sagawa et al., 2021).
Women who had not received PNC counseling were less likely to use PNC services than women who had. This finding is consistent with the studies conducted in Abi-Adi Town, Tigray, Ethiopia (Alemayeh et al., 2014) and Nepal (Neupane & Doku, 2013). This may be during the postnatal period, mothers who were counseled about the importance of PNC services and the risks associated with them will recognize the value and use PNC.
When compared to when it took less than 2 h to get to the nearest health institution, people who took more than 2 h were less likely to use PNC services. This finding is consistent with a study done in East Gojjam Zone, Northwest Ethiopia (34.6%) (Zeleke et al., 2021) and Uganda (Ndugga et al., 2020). Because of the physical difficulties of travel and the high costs of motorized transportation, postpartum women's willingness and ability to seek PNC is limited (Izudi et al., 2017). Women who lived far from the health facility had limited access to health care services after childbirth due to transportation issues and inconvenient geographical and seasonal conditions.
Strengths and Limitations of the Study
The primary data were used to conduct this study. It was more likely that the sampling strategy and study design would produce reliable estimates. It will be possible to address women who were unable to access medical institutions by using a community-based study design. However, using a community-based study design will help to address those mothers who were unable to visit health care facilities. However, because of the cross-sectional nature of the data, there may be a recall bias in the assessment of some variables, despite efforts to reduce recollection biases by informing local events. In addition, the cross-sectional nature of the study limits the capacity to draw any causal implications.
Implications for Practice
PNC is important for maximizing maternal and newborn health. Postnatal visit gives an opportunity for providers to facilitate healthy breastfeeding practices, screen for postpartum depression, and monitor the newborn's growth and overall health status. The postnatal period are a critical phase in the lives of mothers and newborn babies. In this study, the prevalence of postnatal utilization is extremely low. Discussing on the factors of PNC utilization of mothers is essential to ensure that the woman and her child birth have adequate care and to improve PNC utilization. In addition to this finding, Healthcare professionals, including midwives, need to enhance women's counseling regarding PNC utilization. Thus, programs such as training of healthcare providers and information dissemination through social media could break the barriers to PNC utilization. To halt women's’ negative beliefs toward PNC service, community mobilization, including arranging mothers’ conferences, needs to be reinforced. We are also hopeful that the current findings will help the government and other interested parties to address the service inaccessibility issues.
Conclusion
The coverage of PNC service utilization in the South Gondar Zone was extremely low. This study revealed that maternal education, maternal occupation, husbands education, husbands occupation, media exposure, time taken to get the nearest health facility, planned pregnancy, wanted pregnancy, health profession preferred by women, source of information about maternal care, residence, duty service of maternal health care, number of living children, road accessibility to the nearest health facility, health provider behavior, presence of health facility in kebele, transportation, family size were significantly associated with PNC utilization. This suggests that continuity of care has a favorable impact on the use of services. By providing information and instruction to married women, PNC should be strengthened by raising knowledge of its use. In order to encourage the use of PNC services, the concerned body should place a strong emphasis on women's empowerment and institutional delivery. The government and health care department should pay special attention to uneducated women, women who live in rural areas, are unemployed, are not exposed to mass media, and do not have access to transportation to improve PNC service utilization. Furthermore, programs educating mothers on the benefits of antenatal check-ups and safer places of childbirth should be considered to increase PNC service utilization.
Acknowledgment
First, we would like to thank Debre Tabor University, the College of Natural and Computational Sciences, Department of Statistics that allowed us to do research on this interesting area. Lastly, special thanks also go to the study participants, data collectors, and supervisors.
Footnotes
Author Contributions: All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Availability of Data and Materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval for this study was obtained from Ethical Approval Committee of facility of natural and computational science, Debre Tabor University, Ethiopia (Reference number: RCS/112/2020).
Funding: The authors received the following financial support for the research, authorship, and/or publication of this article: This study was done by the fund obtained from Debre Tabor University for the design and collection, analysis and interpretation of data. However, the funder has no specific role in the preparation of the manuscript.
Informed Consent: After the objectives of the study were fully explained to them written informed consent was obtained from each study participant before participation in the study.
ORCID iDs: Yikeber Abebaw Moyehodie https://orcid.org/0000-0001-9275-8705
Alebachew Taye Belay https://orcid.org/0000-0002-1102-9621
Mitiku Wale Muluneh https://orcid.org/0000-0002-2413-8026
References
- Abebo T. A., Tesfaye D. J. (2018). Postnatal care utilization and associated factors among women of reproductive age group in Halaba Kulito town, Southern Ethiopia. Archives of Public Health, 76(1), 1–10. 10.1186/s13690-017-0251-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adane B., Fisseha G., Walle G., Yalew M. (2020b). Factors associated with postnatal care utilization among postpartum women in Ethiopia: A multi-level analysis of the 2016 Ethiopia demographic and health survey. Archives of Public Health, 78(1), 1–10. 10.1186/s13690-020-00415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahinkorah B. O., Seidu A.-A., Budu E., Armah-Ansah E. K., Agbaglo E., Adu C., Yaya S. (2021). Individual, household, and community level factors associated with postnatal care utilization among childbearing women: A mixed effects multilevel analysis of the 2018 Mali demographic and health survey. International Journal, 5(1), 23–32. 10.21106/ijtmrph.318 [DOI] [Google Scholar]
- Akibu M., Tsegaye W., Megersa T., Nurgi S. (2018). Prevalence and determinants of complete postnatal care service utilization in northern Shoa, Ethiopia. Journal of Pregnancy, 2018: 1–7. 10.1155/2018/8625437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemayeh H., Assefa H., Adama Y. (2014). Prevalence and factors associated with post natal care utilization in Abi-Adi town, Tigray, Ethiopia: A cross sectional study. IJPBSF International Journal of Pharmaceutical and Biological Sciences Fundamentals, 8(01), 23–35. http://ijpbsf.com/journal%20data/IJPBSFNov2014_23_35_Huruy%20.pdf [Google Scholar]
- Angore B. N., Tufa E. G., Bisetegen F. S. (2018). Determinants of postnatal care utilization in urban community among women in Debre Birhan town, Northern Shewa, Ethiopia. Journal of Health, Population and Nutrition, 37(1), 1–9. 10.1186/s41043-018-0140-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appiah F., Salihu T., Fenteng J. O. D., Darteh A. O., Kannor P., Ayerakwah P. A., Ameyaw E. K. (2021). Postnatal care utilisation among women in rural Ghana: Analysis of 2014 Ghana demographic and health survey. BMC Pregnancy and Childbirth, 21(1), 1–9. 10.1186/s12884-020-03485-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayele B. G., Woldu M. A., Gebrehiwot H. W., Gebre-egziabher E. G., Gebretnsae H., Hadgu T., Medhanyie A. A. (2019). Magnitude and determinants for place of postnatal care utilization among mothers who delivered at home in Ethiopia: A multinomial analysis from the 2016 Ethiopian demographic health survey. Reproductive Health, 16(1), 162. 10.1186/s12978-019-0818-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belachew T., Taye A., Belachew T. (2016). Postnatal care service utilization and associated factors among mothers in Lemo Woreda, Ethiopia. Journal of Women’s Health Care, 5(3), 10.4172/2167-0420.1000318 [DOI] [Google Scholar]
- Berhe A., Bayray A., Berhe Y., Teklu A., Desta A., Araya T., Roosevelt L. (2019). Determinants of postnatal care utilization in Tigray, Northern Ethiopia: A community based cross-sectional study. PloS One, 14(8), e0221161. 10.1371/journal.pone.0221161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bwalya B. B., Mulenga M. C., Mulenga J. N. (2017). Factors associated with postnatal care for newborns in Zambia: Analysis of the 2013-14 Zambia demographic and health survey. BMC Pregnancy and Childbirth, 17(1), 1–13. 10.1186/s12884-017-1612-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CSA (2016). Ethiopia demographic and health survey. Central Statistical Agency. [Google Scholar]
- CSA, & ICF (2012). Central Statistical Agency [Ethiopia] and ICF International. 2012. Ethiopia Demographic and Health Survey 2011. Central Statistical Agency and ICF International. Ethiopia and Calverton: Ethiopia Demographic and Health Survey, 14. [Google Scholar]
- Debie A., Tesema G. A. (2021). Time to early initiation of postnatal care service utilization and its predictors among women who gave births in the last 2 years in Ethiopia: A shared frailty model. Archives of Public Health, 79(1), 1–11. 10.1186/s13690-021-00575-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawole O. I., Adeoye I. A. (2015). Women’s status within the household as a determinant of maternal health care use in Nigeria. African Health Sciences, 15(1), 217–225. 10.4314/ahs.v15i1.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenta S. M., Ayenew G., Getahun B. E. (2021). Magnitude of antenatal care service uptake and associated factors among pregnant women: Analysis of the 2016 Ethiopia demographic and health survey. BMJ Open, 11(4), e043904. 10.1136/bmjopen-2020-043904 [DOI] [Google Scholar]
- Gebrehiwot G., Medhanyie A. A., Gidey G., Abrha K. (2018). Postnatal care utilization among urban women in northern Ethiopia: Cross-sectional survey. BMC Women’s Health, 18(1), 1–10. 10.1186/s12905-018-0557-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habte A., Gebiremeskel F., Shewangizaw M., Dessu S., Glagn M. (2021). Uptake of complete postnatal care services and its determinants among rural women in Southern Ethiopia: Community-based cross-sectional study based on the current WHO recommendation. PloS One, 16(2), e0246243. 10.1371/journal.pone.0246243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health F. D. R. o. E. M. o. (2015). Health sector transformation plan (2015/16–2019/20). Federal Ministry of Health Addis Ababa. [Google Scholar]
- Hordofa M. A., Almaw S. S., Berhanu M. G., Lemiso H. B. (2015). Postnatal care service utilization and associated factors among women in Dembecha district. Northwest Ethiopia. Science Journal of Public Health, 3(5), 686–692. 10.11648/j.sjph.20150305.24 [DOI] [Google Scholar]
- Idris H., Syafriyanti W. (2021). Determinants of postnatal care service utilization in Indonesia: A secondary analysis using the Indonesian health and demographics survey. Makara Journal of Health Research, 25(1), 7. https://scholarhub.ui.ac.id/cgi/viewcontent.cgi?article=1260&context=mjhr [Google Scholar]
- Igboanusi C. J.-C., Sabitu K., Gobir N., Awawu Grace J. I. (2019). Factors affecting the utilization of postnatal care services in primary health care facilities in urban and rural settlements in Kaduna state, North-western Nigeria. American Journal of Public Health, 7, 111–117. http://pubs.sciepub.com/ajphr/7/3/4/index.html [Google Scholar]
- Izudi J., Akwang G. D., Amongin D. (2017). Early postnatal care use by postpartum mothers in Mundri east county, South Sudan. BMC Health Services Research, 17(1), 1–8. 10.1186/s12913-017-2402-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izudi J., Amongin D. (2015). Use of early postnatal care among postpartum women in Eastern Uganda. International Journal of Gynecology & Obstetrics, 129(2), 161–164. 10.1016/j.ijgo.2014.11.017 [DOI] [PubMed] [Google Scholar]
- Lim S. S., Allen K., Bhutta Z. A., Dandona L., Forouzanfar M. H., Fullman N., Holmberg M. (2016). Measuring the health-related sustainable development goals in 188 countries: A baseline analysis from the global burden of disease study 2015. The Lancet, 388(10053), 1813–1850. 10.1016/S0140-6736(16)31467-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limenih M. A., Endale Z. M., Dachew B. A. (2016). Postnatal care service utilization and associated factors among women who gave birth in the last 12 months prior to the study in Debre Markos town, northwestern Ethiopia: A community-based cross-sectional study. International Journal of Reproductive Medicine, 2016: 1–7. 10.1155/2016/7095352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekonnen T., Dune T., Perz J., Ogbo F. A. (2021). Postnatal care service utilisation in Ethiopia: Reflecting on 20 years of demographic and health survey data. International Journal of Environmental Research and Public Health, 18(1), 193. 10.3390/ijerph18010193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S., Abalos E., Chamillard M., Ciapponi A., Colaci D., Comandé D., Langer A. (2016). Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. The Lancet, 388(10056), 2176–2192. 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- Tsawe M., Moto A., Netshivhera T., Ralesego L., Nyathi C., Sathiya Susuman A. (2015). Factors influencing the use of maternal healthcare services and childhood immunization in Swaziland. International Journal for Equity in Health, 14(1), 32. 10.1186/s12939-015-0162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mon A. S., Phyu M. K., Thinkhamrop W., Thinkhamrop B. (2018). Utilization of full postnatal care services among rural Myanmar women and its determinants: A cross-sectional study. F1000Research, 7. https://doi: 10.12688/f1000research.15561.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosiur Rahman M., Haque S. E., Sarwar Zahan M. (2011). Factors affecting the utilisation of postpartum care among young mothers in Bangladesh. Health & Social Care in the Community, 19(2), 138–147. 10.1111/j.1365-2524.2010.00953 [DOI] [PubMed] [Google Scholar]
- Muchabaiwa L., Mazambani D., Chigusiwa L., Bindu S., Mudavanhu V. (2012). Determinants of maternal healthcare utilization in Zimbabwe. International Journal of Economic Sciences and Applied Research, 5(2), 145–162. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2155627 [Google Scholar]
- Mukonka P. S., Mukwato P. K., Kwaleyela C. N., Mweemba O., Maimbolwa M. (2018). Household factors associated with use of postnatal care services. African Journal of Midwifery and Women’s Health, 12(4), 189–193. 10.12968/ajmw.2018.12.4.189 [DOI] [Google Scholar]
- Ndugga P., Namiyonga N. K., Sebuwufu D. (2020). Determinants of early postnatal care attendance: Analysis of the 2016 Uganda demographic and health survey. BMC Pregnancy and Childbirth, 20(1), 1–14. 10.1186/s12884-020-02866-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neupane S., Doku D. (2013). Utilization of postnatal care among Nepalese women. Maternal and Child Health Journal, 17(10), 1922–1930. 10.1007/s10995-012-1218-1 [DOI] [PubMed] [Google Scholar]
- Nzioki J. M., Onyango R. O., Ombaka J. H. (2015). Socio-Demographic factors influencing maternal and child health service utilization in Mwingi; A rural SemiArid district in Kenya. American Journal of Public Health Research, 3(1), 21–30. 10.12691/ajphr-3-1-4 [DOI] [Google Scholar]
- Ononokpono D. N., Gayawan E., Adedini S. A. (2020). Regional variations in the use of postnatal care in Nigeria: A spatial analysis. Women & Health, 60(4), 440–455. 10.1080/03630242.2019.1643816 [DOI] [PubMed] [Google Scholar]
- Sagawa J., Kabagenyi A., Turyasingura G., Mwale S. E. (2021). Determinants of postnatal care service utilization among mothers of Mangochi district, Malawi: A community-based cross-sectional study. BMC Pregnancy and Childbirth, 21(1), 1–11. 10.1186/s12884-021-04061-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Say L., Chou D., Gemmill A., Tunçalp Ö, Moller A.-B., Daniels J., Alkema L. (2014). Global causes of maternal death: A WHO systematic analysis. The Lancet Global Health, 2(6), e323–e333. 10.1016/S2214-109X(14)70227-X [DOI] [PubMed] [Google Scholar]
- Seid A., Ahmed M. (2020). Determinants of postnatal checkup for newborns in Ethiopia: Further analysis of 2016 Ethiopia demographic and health survey. BMC Pregnancy and Childbirth, 20(1), 1–7. 10.1186/s12884-020-03468-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somefun O. D., Ibisomi L. (2016). Determinants of postnatal care non-utilization among women in Nigeria. BMC Research Notes, 9(1), 1–11. 10.1186/s13104-015-1823-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sydavong T., Goto D. (2019). Does community-based health insurance have potential impacts on direct and indirect outcomes? Evidence from rural villages, Savannakhet province, Lao people’s democratic republic. Journal of International Development and Cooperation, 25(1–2), 69–83. https://cir.nii.ac.jp/crid/1390572174812265344 [Google Scholar]
- Tarekegn S. M., Lieberman L. S., Giedraitis V. (2014). Determinants of maternal health service utilization in Ethiopia: Analysis of the 2011 Ethiopian demographic and health survey. BMC Pregnancy and Childbirth, 14(1), 1–13. 10.1186/1471-2393-14-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessema G. A., Laurence C. O., Melaku Y. A., Misganaw A., Woldie S. A., Hiruye A., Deribew A. (2017). Trends and causes of maternal mortality in Ethiopia during 1990–2013: Findings from the global burden of diseases study 2013. BMC Public Health, 17(1), 1–8. 10.1186/s12889-017-4071-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessema Z. T., Yazachew L., Tesema G. A., Teshale A. B. (2020). Determinants of postnatal care utilization in sub-Saharan Africa: A meta and multilevel analysis of data from 36 sub-Saharan countries. Italian Journal of Pediatrics, 46(1), 1–11. 10.1186/s13052-019-0764-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF W. a. (2016). Trends in maternal mortality: 1990 to 2015: Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division: executive summary.
- UNICEF, & WHO (2015). Trends in maternal mortality: 1990 to 2013: estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division: executive summary. World Health Organization. [Google Scholar]
- WHO (2018). Maternal mortality.
- Yoseph S., Dache A., Dona A. (2021). Prevalence of early postnatal-care service utilization and its associated factors among mothers in Hawassa Zuria district, Sidama regional state, Ethiopia: A cross-sectional study. Obstetrics and Gynecology International, 2021: 1–8. 10.1155/2021/5596110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeleke L. B., Wondie A. T., Tibebu M. A., Alemu A. A., Tessema M. T., Shita N. G., Khajehei M. (2021). Postnatal care service utilization and its determinants in East Gojjam Zone, Northwest Ethiopia: A mixed-method study. PloS One, 16(8), e0256176. 10.1371/journal.pone.0256176 [DOI] [PMC free article] [PubMed] [Google Scholar]