Abstract
BACKGROUND
Septic arthritis of the hand, which is the second most common after damage of the knee joint, remains one of the leading causes of temporary disability. An inflammation can cause dysfunction of the joint, and in the most severe cases, the need for amputation of the finger may arise. The results of their treatment today, especially from a functional point of view, cannot be considered satisfactory. Urgent surgical treatment is extremely important in septic arthritis of the hand, as it helps to prevent cartilage destruction and the development of osteomyelitis.
AIM
To explore the features of the course of septic arthritis of the hand as well as approaches to surgical treatment and its results, depending on the nature of the damage to the articular structures.
METHODS
The results of the treatment of 170 patients with septic arthritis of the hand, which were treated in the period of 2020-2021, were analyzed. Inflammation of the interphalangeal and metacarpophalangeal joints (MCP) of fingers 1, 2, and 3 was more often noted in 147 (81.6%) joints. The most common cause of arthritis was a penetrating injury as a result of household trauma (101, 59.4%), animal bite (30, 17.6%), and clenched fist injury (15, 8.8%). Septic arthritis with contiguous osteomyelitis was observed in 98 (54.4%) cases. Surgical treatment was completed with drainage and irrigation of the joint. Early mobilization was used to restore function. In patients with osteomyelitis, it was aimed at the formation of neoarthrosis. Arthrodesis was not applied. Long-term results of treatment were assessed in 142 (83.5%) patients within 1 mo to 12 mo after discharge from the hospital [the median was 7 mo (IQR: 4-9)].
RESULTS
The most commonly isolated organism was Staphylococcus aureus (35.3%). The median treatment delay in patients without osteomyelitis was 5 d (IQR: 4-7); for septic arthritis with contiguous osteomyelitis, it was 14 d (IQR: 5-21). Radiography for osteomyelitis within 2 wk was uninformative: 41.2% of diagnoses. A single surgical treatment was required in 138 (81.2%) patients, two treatments in 22 (12.9%), and three or more in 10 (5.9%). Total elimination of the infection was achieved in 163 (95.9%) patients. The best functional results of treatment were noted in patients without osteomyelitis. After septic arthritis, Total Active Motion (TAM) for the MCP was 96.2% (IQR: 85.1-98.0), for the proximal interphalangeal joint (PIP) 82.4% (IQR: 54.5-98.5), and for the distal interphalangeal joint (DIP) 69.4% (IQR: 65.4-74.1). In cases with osteomyelitis, it was possible to achieve the formation of neoarthrosis with TAM for MCP-64.2% (IQR: 45.3-90.1), for PIP-62.5% (IQR: 41.8-68.9), and for DIP-59.4% (IQR: 50-62.1). Additionally, the severity of pain during movements did not exceed 1 point.
CONCLUSION
The delay in treatment of patients with septic arthritis of the hand was accompanied by a high incidence of osteomyelitis, especially in the presence of diabetes mellitus. Urgent surgical treatment, along with continued irrigation of the joint and antibiotic therapy, made it possible to eliminate the infection, and early rehabilitation restored the range of motion. The best results were noted in patients without osteomyelitis. With the development of osteomyelitis, a complex of early rehabilitation measures also made it possible to partially restore the range of motion due to the formation of neoarthrosis, without resorting to arthrodesis.
Keywords: Septic arthritis, Osteomyelitis, Hand, Surgical treatment, Neoarthrosis
Core Tip: The timing of surgical treatment initiation is extremely important in septic arthritis of the hand. Prompt and timely surgical intervention can prevent the destruction of cartilage and the development of osteomyelitis. In the presence of osteomyelitis, surgical debridement followed by early rehabilitation aimed at developing neoarthrosis may be an alternative to traditional treatment using arthrodesis. This conception makes it possible to largely preserve the range of active motions in the affected joint.
INTRODUCTION
It is difficult to overestimate the importance of the hand as a unique anatomical and physiological formation. The hand is important not only from the point of view of aesthetics but is also often decisive in the performance of professional activities. Therefore, any disease or traumatic injury can cause irreparable damage[1,2]. Septic diseases of the hand are characterized by a high prevalence and remain one of the leading causes of temporary disability. Among the pathologies of the hand, septic arthritis of the metacarpophalangeal and interphalangeal joints is characterized by particular severity. An inflammation can cause dysfunction of the joint, and in the most severe cases, the need for amputation of the finger[1,3,4] may arise. The incidence of septic arthritis of the hand differs significantly by region and ranges from 2 to 12 cases per 100000 population per year[5]. Among septic arthritis, septic arthritis of the hand takes second place in prevalence (15%-20%) after lesions of the knee joint, and among hand infections it occurs in 5%-18% cases[3,6]. Pathogenesis, clinical manifestations, and approaches to the treatment of septic arthritis of the hand have quite significant differences from inflammation of large joints. The causes of their occurrence are most often the direct penetration of the infection as a result of traumatic injury or the spread of infection from the surrounding soft tissues during felon, tenosynovitis, etc. In the absence of timely and complete treatment, cartilage destruction and osteomyelitis will develop in a short time[7-9]. A diagnosis of septic arthritis of the hand is based on clinical data, as well as the results of instrumental and laboratory research. Such clinical manifestations as pain, edema, hyperemia, and limitation of range of motion (ROM) are typical but do not allow us to establish the stage of the inflammatory process, including cartilage destruction and osteomyelitis[10]. The most commonly used radiography is also uninformative in the early stages. All these substantiate the expediency of using computed tomography and magnetic resonance imaging, which have high diagnostic value[1,3,11]. The microbial landscape in septic arthritis of the hand is not well understood. The leading role of Staphylococcus aureus (S. aureus) in this pathology has been reported. At the same time, data regarding the frequency of isolation of methicillin-resistant S. aureus (MRSA) differ significantly (from 0% to 73%)[10,12-14].
Treatment of septic arthritis of the hand is based on a combination of surgical methods and antibiotic therapy[10,15,16]. A number of authors note that persistent inflammation after surgical debridement determines the need to perform repeated surgical intervention within 24-48 h[2,17,18]. Articular cartilage destruction and osteomyelitis are considered by most experts as indications for arthrodesis[4,10,17,19]. The possibility of neoarthrosis formation after resection of the destroyed joint is not considered. Some authors, characterizing their own observations, testify that arthrodesis was not performed in patients with osteochondral destruction. However, they do not report long-term functional results of the treatment [15].
The duration of antibiotic therapy remains a subject of discussion. A significant number of authors are supporters of long-term (at least 1 mo) administration of antibiotics[20-22]. However, in a study performed by Gjika et al[23], it was shown that a shorter 2-wk course of antibiotic therapy was as effective as a 4-wk course. The most important moment in the treatment of septic arthritis of the hand is the beginning of rehabilitation as a factor contributing to the restoration of movements and a decrease in joint stiffness. Some authors refer to supporters of early rehabilitation (1 d after surgery), while others consider it necessary to ensure peace for 7-14 d[5,16,18,24].
Thus, although septic arthritis of the hand is a common pathology, many questions regarding its etiology, pathogenesis, and treatment approaches remain insufficiently explored. There is still no answer to the question of whether there is a real alternative to arthrodesis in the presence of osteochondral destruction of the joint.
MATERIALS AND METHODS
Population
The results of the examination and treatment of 170 patients (180 joints) who were hospitalized with a diagnosis of septic arthritis of the hand from 2020 to 2021 were retrospectively analyzed. The average age of the patients was 49 years (IQR: 34-65). There were 116 men (68.2%) and 54 women (31.8%). Damage to the joints of the right hand was observed in 103 (60.6%) patients, and damage to the left hand was observed in 67 (39.4%). Most often, inflammation of the joints of 1, 2, and 3 fingers was diagnosed (detected: 147 (81.6%) joints). Septic arthritis of the metacarpophalangeal joint (MCP) was noted in 55 (30.6%) cases, proximal interphalangeal joint (PIP) in 54 (30%), distal interphalangeal joint (DIP) in 45 (25%), and interphalangeal joint of the first finger (IP of the thumb) in 26 (14.4%) (Figure 1).
Figure 1.

Distribution of 180 small joints involved in 170 episodes of septic arthritis.
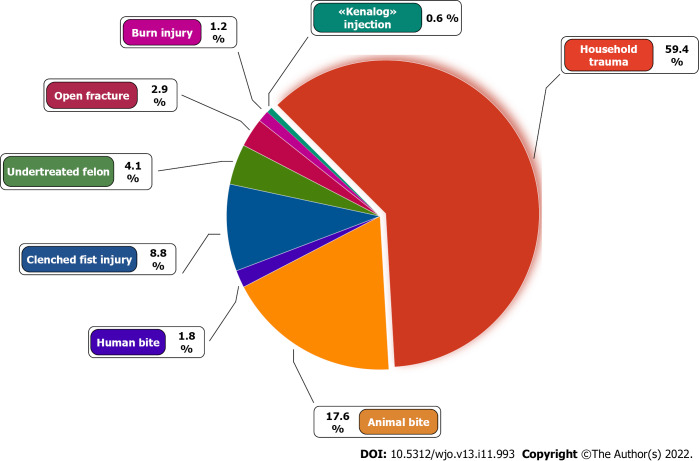
Exogenous infection was detected in 164 (96.5%) patients, and endogenous (the source of infection was not found) was detected in 6 (3.5%). Among the causes of septic arthritis, various types of household trauma were most often noted-101 (59.4%), animal bites-30 (17.6%), and clenched fist injury-15 (8.8%) (Figure 2).
Figure 2.
Causative factors of septic arthritis of the hand.
The nature of the clinical course of arthritis was assessed based on the duration of symptoms: Acute-less than 3 wk and chronic-3 wk or more[25]. An acute course was observed in 156 (91.8%) patients, and a chronic course was observed in 14 (8.2%).
While a specialized classification of septic arthritis of the hand needs further specification, the classification of septic arthritis of large joints worked out by Tan et al[26] is widely used in surgery. Isolated septic arthritis was noted in 11 (6.1%) cases, septic arthritis with soft-tissue extension but no osteomyelitis in 71 (39.4%), and septic arthritis with contiguous osteomyelitis in 98 (54.4%).
Among comorbidities, arterial hypertension was most often observed (36 patients; 21.2%), followed by diabetes mellitus (16 patients; 9.4%) and postinfarction cardiosclerosis (7 patients; 4.1%).
All patients underwent surgical treatment during the first day after hospitalization. It included the excision of all nonviable tissues (soft tissues, and in the case of osteomyelitis, both bone and cartilage structures) and ended with drainage and irrigation of the joint cavity. The drains were removed after the inflammation subsided, usually after 3-5 d. Persistent inflammation served as the basis for repeated surgical treatment within 24-48 h. Although the conventional surgical approach for septic arthritis with contiguous osteomyelitis is the need for arthrodesis (either primary or delayed), a different approach was used in these observations. The concept of the formation of neoarthrosis was fundamental, and was achieved through early mobilization, starting 5-7 d after the removal of the affected bone and cartilage structures.
Immobilization of the hand was carried out for 3-5 d using a developed design that allows axial extension of the affected finger (Figure 3). Subsequently, rehabilitation activities began.
Figure 3.
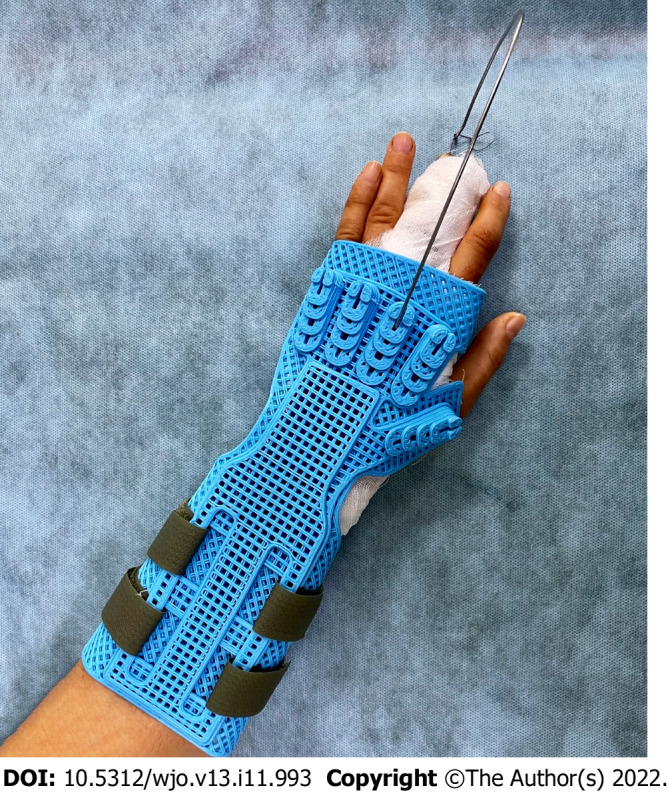
Immobilization of the hand using a developed design that allows axial extension of the affected finger.
Antibacterial therapy at the inpatient stage included intravenous administration of antibiotics such as amoxicillin/clavulanate, ceftriaxone, ciprofloxacin, and clindamycin. The results of microbiological research were taken into account. Patients who developed osteomyelitis after discharge continued to receive oral antibiotic therapy for 2 wk.
The long-term results of the performed treatment were evaluated in 142 (83.5%) patients within 1 mo to 12 mo after discharge from the hospital [the median was 7 mo (IQR: 4-9)]. The evaluation parameters included totalelimination of the infection as well as the volume of active movements of the affected joint (ROM). For this, the Total Active Motion (TAM) system was used. TAM is described by the American Society for Surgery of the Hand as the sum of active MCP, PIP, and DIP arc of motion in degrees of an individual digit. This calculation can then be compared to the TAM of the contralateral hand[27]. If necessary, control radiography or computed tomography was performed.
The severity of chronic pain during movement was assessed using a 10-cm visual analog scale (VAS), where 0 is no pain, and 10 cm is pain that is as bad as it could possibly be. In the analysis, centimeters were converted into points, where 1 cm equaled 1 point on the pain scale.
When examining patients, along with general clinical methods, radiography, computed tomography, microbiological examination with identification of microbial flora and determination of its sensitivity to antibiotics, as well as morphological examination of tissues removed during surgical treatment were used.
Statistical analysis
Statistical processing was carried out by methods of collecting and grouping factual material, calculating the median (Me) and IQR. The normality of the distribution was determined using the Shapiro-Wilk normality test. The significance of difference for nonparametric indicators was determined using the Mann-Whitney U test. Differences in indicators at P < 0.05 were considered significant. The study was reviewed by our biostatistic expert
RESULTS
Men predominated among the sick (68.2% vs 31.8% of women). The most common inflammation was MCP of the middle finger (15%), IP of the thumb (14.4%), PIP of the index finger (13.3%), and DIP of the index finger (11.7%). Septic arthritis of the MCP of the middle finger in all cases was the result of a clenched fist injury. At the same time, damage to the joint capsule and the extensor tendon of the finger was observed. Defects in the treatment of felon as a cause of septic arthritis DIP were identified in 7 (4.1%) patients.
The clinical course of septic arthritis in most patients (91.8%) was regarded as acute. However, local inflammation prevailed. An increase in body temperature was noted only in 55 (32.4%) patients; the median was 37.2 °C (IQR: 37.2-37.6). An increase in the number of leukocytes in the peripheral blood was observed in 82 (48.2%) patients; the median was 11.1 × 109/L (IQR: 10.2-13.6).
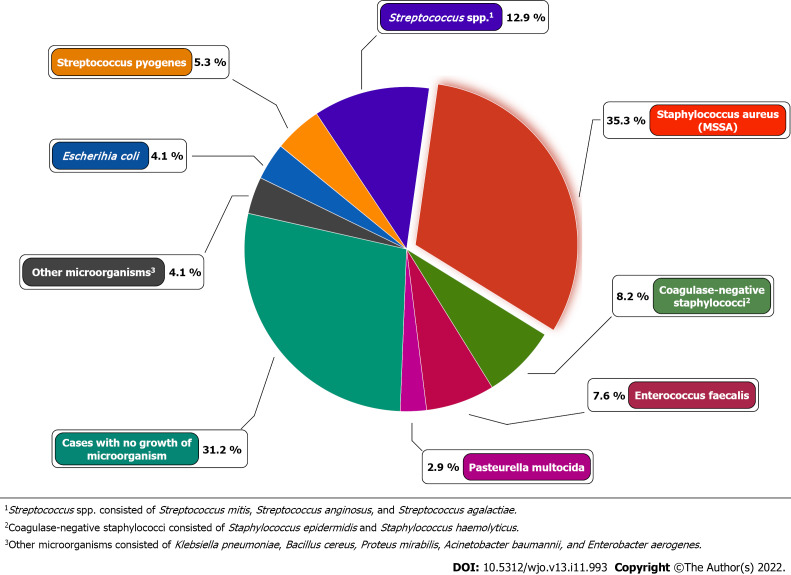
As a result of microbiological analysis, the bacterial flora was identified in 117 (68.8%) cases (Figure 4). In other plates the growth of microflora was absent. Among the isolated microorganisms, S. aureus was the most common (35.3%). A feature of the observations was that MRSA was not detected in any case. Monoinfection was noted in 98 (57.6%) cases, and polymicrobial infection was detected in 19 (11.2%).
Figure 4.
Microorganisms cultured from patients with septic arthritis of the hand.
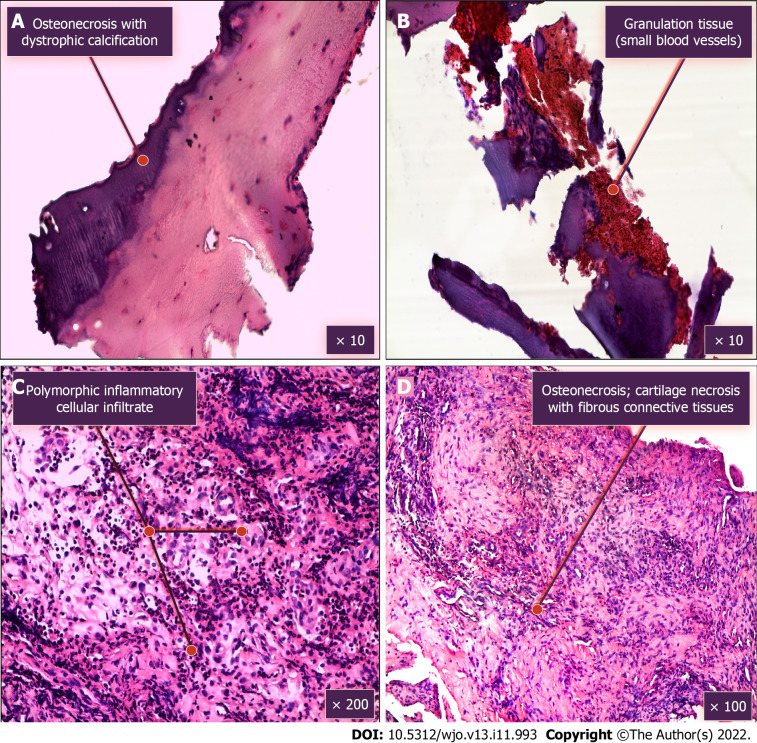
Another feature of the presented observations was a large number of cases of septic arthritis with contiguous osteomyelitis: 98 (54.4%) cases. To explain this fact, the duration of the delay in the start of treatment in various anatomical types of septic arthritis was analyzed. The median treatment delay in patients with septic arthritis without osteomyelitis was 5 d (IQR: 4-7). Septic arthritis with contiguous osteomyelitis was significantly longer and lasted for 14 d (IQR: 5-21). The diagnosis of osteomyelitis was confirmed by the results of intraoperative revision, morphological examination, and radiography (Figure 5). At the same time, radiographic data did not always make it possible to diagnose osteomyelitis in a timely manner. Among all cases with proven osteomyelitis (n = 98) with a treatment delay of up to 14 d (n = 51), it was detected on radiographs only in 21 (41.2%) cases. If the delay in treatment exceeded 14 d (n = 47), then radiographic signs of osteomyelitis were much more common and were reported in 39 (83%) cases. In 8 (17%) observations, even in these terms, radiographs did not allow a correct diagnosis.
Figure 5.
Morphological examination of tissues removed during surgical treatment (hematoxylin and eosin staining). A: Osteonecrosis with dystrophic calcification; B: Granulation tissue (small blood vessels); C: Polymorphic inflammatory cellular infiltrate; D: Osteonecrosis; cartilage necrosis with fibrous connective tissues.
The course of septic arthritis in patients with diabetes mellitus (n = 16) was characterized by particular severity. Fourteen (87.5%) of them developed osteomyelitis. The median treatment delay was 6 d (IQR: 4-28).
Surgical treatment has become a fundamental moment in the treatment of septic arthritis. A single surgical treatment was performed in 138 (81.2%) patients. The need for two surgical treatments was noted in 22 (12.9%) patients. Three or more treatments were required in 10 (5.9%) patients. Thus, repeated operations were performed in 32 (18.8%) patients. There was a certain relationship between the cause of septic arthritis and the need to perform repeated surgical treatment. The highest frequency of repeated surgical interventions was noted in patients with diabetes mellitus: 56.3%.
The duration of antibiotic therapy depended on the anatomical form of arthritis and the effectiveness of the treatment. In septic arthritis without osteomyelitis, the duration of antibiotic therapy averaged 7 d (IQR: 5-7). Septic arthritis with contiguous osteomyelitis was longer and lasted for 23 d (IQR: 21-25). This included inpatient and subsequent outpatient antibiotics.
In the majority of patients (163, 95.9%), it was possible to achieve elimination of infection and healing the wounds. However, 7 (4.1%) patients required rehospitalization for surgical treatment due to the ongoing septic process. Among them, there were 3 patients initially hospitalized with a diagnosis of septic arthritis of the hand without osteomyelitis and 4 with a diagnosis of septic arthritis with contiguous osteomyelitis.
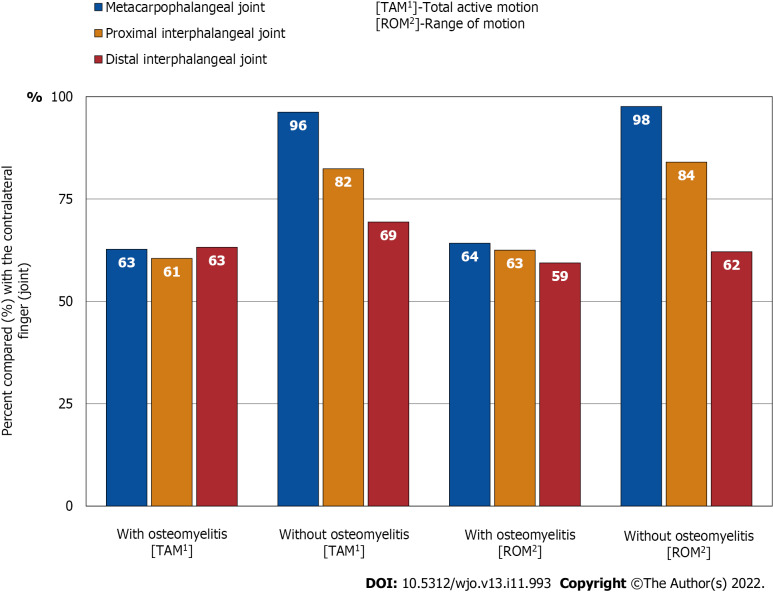
The best functional results were noted in the treatment of septic arthritis without osteomyelitis. The TAM assessment showed that the range of active movements of the finger was maximal after suffering septic arthritis of the MCP, and its median was 96.2% (IQR: 85.1-98.0) on the ROM of the contralateral finger. Slightly worse rates were reported for lesions of the proximal interphalangeal [median, 82.4% (IQR: 54.5-98.5)] and distal interphalangeal [median, 69.4% (IQR: 65.4-74.1)] joints. If we consider the recovery of ROM in a particular joint, then it was significantly better in the MCP [median, 97.6% (IQR: 84.6-100.0)] (P < 0.05). The worst indicators were characterized by the DIP [median, 62.1% (53.6-67.9)]. The median ROM of PIP was 84% (IQR: 68.2-98.5). The severity of pain during movement (according to the VAS scale) was minimal and did not exceed 1 point on a ten-point scale.
In cases of septic arthritis with contiguous osteomyelitis, the formation of neoarthrosis allowed only partial restoration of the range of active movements. The median TAM with MCP destruction was 62.7% (IQR: 48.1-87.5), with destruction of PIP was 60.5% (IQR: 51.8-71.8), and with DIP destruction was 63.2% (IQR: 61.5-71.7). The ROM in these joints was as follows: MCP-64.2% (IQR: 45.3-90.1), PIP-62.5% (41.8-68.9), and DIP-59.4% (50.0-62.1) (Figures 6-8). The severity of pain during movement was insignificant, although it was statistically significantly higher than pain in patients with septic arthritis without osteomyelitis. It was 0.86 points (IQR: 0.72-1.45) for MCP, 1.05 points (IQR: 0.71-1.55) for PIP, and 0.4 points (IQR: 0.3-0.55) for DIP (Table 1, Supplementary material).
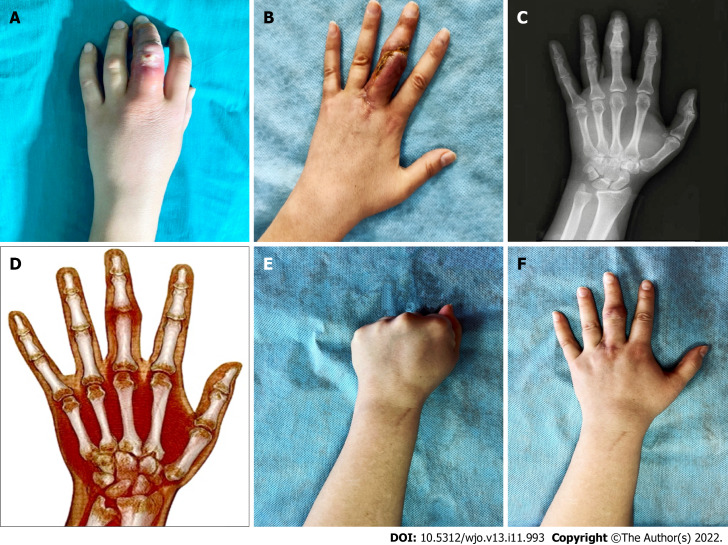
Figure 6.
Summary of total active motion and range of motion.
Figure 8.
Treatment of septic arthritis with osteomyelitis of the proximal interphalangeal joint, third finger (left hand). A: Clinical presentation at admission; B: Short-term outcomes after operative intervention; C: Preoperative radiography; D: 3D-reconstruction (CT) 4 mo after operative intervention; E and F: Long-term outcomes of the function recovery of the proximal interphalangeal joint.
Table 1.
Summary of total active motion and range of motion
|
Outcome
|
Patients without osteomyelitis, median (IQR)
|
Patients with osteomyelitis, median (IQR)
|
P
value
|
| TAM, % | |||
| MCP | 96.2 (85.1-98.0) | 62.7 (48.1-87.5) | 0.01072 |
| PIP | 82.4 (54.5-98.5) | 60.5 (51.8-71.8) | 0.00695 |
| DIP | 69.4 (65.4-74.1) | 63.2 (61.5-71.7) | 0.03662 |
| ROM, % | |||
| MCP | 97.6 (84.6-100.0) | 64.20 (45.30-95.05) | 0.03362 |
| PIP | 84.0 (68.2-98.5) | 62.5 (41.8-68.9) | 0.01017 |
| DIP | 62.1 (53.6-67.9) | 59.4 (50.0-62.1) | 0.00960 |
| Pain, VAS, cm | |||
| MCP | 0.40 (0.20-0.55) | 0.86 (0.72-1.45) | < 0.00100 |
| PIP | 0.98 (0.75-1.50) | 1.05 (0.71-1.55) | < 0.00100 |
| DIP | 0.20 (0.10-0.45) | 0.40 (0.30-0.55) | < 0.00100 |
The values are given as the median and IQR. TAM: Total active motion; ROM: Range of motion; MCP: Metacarpophalangeal joint; PIP: Proximal interphalangeal joint; DIP: Distal interphalangeal joint; VAS: Visual analogue scale.
Figure 7.

Outcomes of septic arthritis with osteomyelitis of the metacarpophalangeal joint, third finger (right hand). A: Preoperative radiography; B: 3D-reconstruction (CT) 5 mo after operative intervention; C and D: Long-term outcomes of the function recovery of the metacarpophalangeal joint.
DISCUSSION
The occurrence of septic arthritis of the hand, as a rule, was the result of a penetrating injury to the joint. The predominance of men with septic arthritis was explained by their frequent traumatization. The frequency of lesions of different joints of the hand was different. The most frequent involvement in the inflammatory process of MCP of the middle finger (15%), IP of the thumb (14.4%), and PIP (13.3%) and DIP (11.7%) of the index finger can be explained by the high frequency of damage. S. aureus has become a characteristic causative agent of joint infection. A feature of these observations was the fact that its polyantibiotic-resistant form, MRSA, was not isolated. The clinical course of septic arthritis of the hand in most cases was characterized as acute with a predominance of local inflammation.
Patients with septic arthritis with contiguous osteomyelitis were characterized by a significant delay in the start of treatment associated with late seeking medical help. The radiography performed during the first 14 d after the onset of the disease was uninformative, and must be taken into account in clinical practice. The course of septic arthritis of the hand in patients with diabetes mellitus was characterized by the greatest severity. This was evidenced by the high incidence of osteomyelitis in these patients (87.5%) with a relatively small delay in the start of treatment (the median was 6 d). Thus, timely treatment of septic arthritis of the hand is one of the most important factors in the prevention of osteomyelitis.
Surgical treatment, which ended with drainage and irrigation of the joint supplemented by antibiotic therapy, eliminated the inflammatory process. Some patients (18.8%) had a need for repeated surgical treatments. Most often, this concerned patients with diabetes mellitus, as well as victims of human and animal bites. In these cases, highly virulent microflora from the oral cavity entered the tissues.
Antibacterial therapy for septic arthritis without osteomyelitis was characterized by a short course (the median was 7 d), differing from the longer duration in osteomyelitis (the median was 23 d).
In 7 (4.1%) patients, after discharge from the hospital, a recurrence of the septic process was noted, which required readmission for surgical treatment. In 3 of them, septic arthritis with soft-tissue extension but no osteomyelitis was initially diagnosed, and signs of osteomyelitis were revealed during rehospitalization. Perhaps this situation was associated with an underestimation of objective data during the initial hospitalization, or with defects in subsequent outpatient treatment. Another 4 patients were initially diagnosed with osteomyelitis, and in all cases there was a severe lesion of the soft tissue of the finger. Of these, 2 patients had to undergo finger amputation as a result, including a patient with severe diabetes mellitus (Supplementary Table 1).
The key to success in restoring joint function was early rehabilitation. Arthrodesis was not used in patients with osteomyelitis after surgical debridement with removal of affected bone and cartilage structures. A complex of early rehabilitation measures contributed to the formation of neoarthrosis with a significant restoration of the volume of active movements. Painful arthrosis as one of the grounds for arthrodesis was not observed in any case. The functional results of the treatment of septic arthritis of the hand with osteomyelitis were slightly worse than those in cases without osteomyelitis. However, they also testified to the possibility of restoring more than 50% of the ROM in the joint without significant pain.
Contraindications to the start of early rehabilitation were related to patients who had damage to the flexor/extensor tendons that did not allow recovery of joint function. In these cases, arthrodesis was achieved using prolonged immobilization of the finger in a functionally advantageous position. Patients who violated the prescribed rehabilitation regime and systematically failed to follow the recommendations of a specialist were excluded from the research.
The main limitations are related to the fact that the research is retrospective. Not in all cases was it possible to estimate the extent of damage to paraarticular soft tissues, if any. Also, insufficient information was received on the condition of the flexor/extensor tendons of the finger, the presence and extent of their possible damage. And this is of fundamental importance in predicting the possibility of restoring the function, and choosing the nature and extent of rehabilitation measures. With an overall significant number of patients included in the research, the number of patients with concomitant diabetes mellitus is relatively small. Therefore, the data concerning this category of patients need to be clarified. A retrospective research also created significant difficulties in assessing the quality of rehabilitation after discharge of patients from the hospital. While rehabilitation, as you know, is the most important factor in restoring the function of the hand after septic arthritis.
CONCLUSION
To sum up, the duration of delay in treatment of patients significantly correlated with the incidence of osteomyelitis. In patients with diabetes mellitus, osteomyelitis developed much faster, which must be taken into account in clinical practice. Timely surgical treatment, along with continued irrigation of the joint and antibiotic therapy, made it possible to eliminate the infection, and early rehabilitation allowed restoring the ROM. The best results were noted in patients without osteomyelitis. With the development of osteomyelitis, a complex of early rehabilitation measures also made it possible to partially restore the ROM due to the formation of neoarthrosis, without resorting to arthrodesis.
ARTICLE HIGHLIGHTS
Research background
Septic arthritis of the hand, which is the second most common after damage of the knee joint, remains one of the leading causes of temporary disability. The results of their treatment today, especially from a functional point of view, cannot be considered satisfactory.
Research motivation
Dissatisfaction with the results of the treatment of septic arthritis of the hand, including a significant number of cases of joint stiffness and even amputations of the fingers, followed by the loss of the ability of patients to engage in their usual work activities, which is a severe psychological trauma, motivated us to find ways to solve this problem.
Research objectives
To explore the etiology and clinical course of septic arthritis of the hand; to analyze the timing of the development of osteomyelitis with a delay in the treatment of patients; and to compare approaches to surgical treatment and rehabilitation depending on the nature of the pathological process.
Research methods
The results of treatment of 170 patients with septic arthritis of the hand were retrospectively analyzed. The causes of the disease and the nature of the microbial flora were explored. The frequency of various forms of septic arthritis of the hand and approaches to surgical treatment were analyzed.
Research results
The most common pathogen was S. aureus. The form of septic arthritis was largely determined by the duration of treatment delay. In the presence of osteomyelitis, it was maximal. In patients with diabetes mellitus, osteomyelitis developed much earlier. Comprehensive treatment made it possible to eliminate the infection. Functional outcomes were better in patients without osteomyelitis. With the development of osteomyelitis, surgical debridement and early rehabilitation made it possible to partially restore the range of motion without resorting to arthrodesis.
Research conclusions
Timely surgical treatment of septic arthritis of the hand allows reducing the number of cases of osteomyelitis. Early rehabilitation is the key to success in restoring hand function after surgery. The development of osteochondral destruction does not exclude the possibility of partial restoration of function due to the formation of neoarthrosis.
Research perspectives
To optimize approaches to the surgical treatment of septic arthritis of the hand and postoperative rehabilitation, it is necessary to develop a specialized classification of this disease, taking into account the involvement in the pathological process of not only the elements of the joint, but also the paraarticular soft tissues and flexor/extensor tendons of the finger.
Footnotes
Institutional review board statement: The study was reviewed and approved by the I.M. Sechenov First Moscow State Medical University Institutional Review Board (Approval No. 03-22).
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: All the authors have no conflict of interest related to the manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 26, 2022
First decision: September 26, 2022
Article in press: October 27, 2022
Specialty type: Surgery
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chisthi MM, India; Sun Z, China S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
Contributor Information
Konstantin V Lipatov, General Surgery Department, Institute of Clinical Medicine named after N.V. Sklifosovsky, Sechenov First Moscow State Medical University (Sechenov University), Moscow 119021, Russia. lipatov_k_v@staff.sechenov.ru.
Arthur Asatryan, General Surgery Department, State Budgetary Institution “City Clinical Hospital named after S.S. Yudin of Moscow Healthcare Department”, Moscow 115142, Russia.
George Melkonyan, General Surgery Department, The Hospital for War Veterans N3, Moscow 129336, Russia.
Aleksandr D Kazantcev, General Surgery Department, Institute of Clinical Medicine named after N.V. Sklifosovsky, Sechenov First Moscow State Medical University (Sechenov University), Moscow 119021, Russia.
Ekaterina I Solov’eva, General Surgery Department, I.M. Sechenov First Moscow State Medical University, Moscow 119991, Russia.
Irina V Gorbacheva, General Surgery Department, I.M. Sechenov First Moscow State Medical University, Moscow 119991, Russia.
Alexander S Vorotyntsev, General Surgery Department, I.M. Sechenov First Moscow State Medical University, Moscow 119991, Russia.
Andrey Y Emelyanov, General Surgery Department, I.M. Sechenov First Moscow State Medical University, Moscow 119991, Russia.
Data sharing statement
The original anonymous dataset is available on request from the corresponding author at lipatov_k_v@staff.sechenov.ru.
References
- 1.McKay P, Formby PM, Dickens J, Gibson M. Osteomyelitis and septic arthritis of the hand and wrist. Curr Orthop Pract. 2010;21:542–550. [Google Scholar]
- 2.Meier R, Wirth T, Hahn F, Vögelin E, Sendi P. Pyogenic Arthritis of the Fingers and the Wrist: Can We Shorten Antimicrobial Treatment Duration? Open Forum Infect Dis. 2017;4:ofx058. doi: 10.1093/ofid/ofx058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sendi P, Kaempfen A, Uçkay I, Meier R. Bone and joint infections of the hand. Clin Microbiol Infect. 2020;26:848–856. doi: 10.1016/j.cmi.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Chenoweth B. Septic Joints: Finger and Wrist. Hand Clin. 2020;36:331–338. doi: 10.1016/j.hcl.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Lamou HJ, Kim S, Kuchenbuch C, Thelen S, Eisenschenk A, Hakimi M. Septic Arthritis of the Hand and Wrist. Handchir Mikrochir Plast Chir. 2021;53:290–295. doi: 10.1055/a-1512-0321. [DOI] [PubMed] [Google Scholar]
- 6.Angly B, Steiger R, Zimmerli W. Septic arthritis of finger joints. Handchir Mikrochir Plast Chir. 2007;39:118–123. doi: 10.1055/s-2007-965137. [DOI] [PubMed] [Google Scholar]
- 7.Nair R, Schweizer ML, Singh N. Septic Arthritis and Prosthetic Joint Infections in Older Adults. Infect Dis Clin North Am. 2017;31:715–729. doi: 10.1016/j.idc.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 8.Ross K, Mehr J, Carothers B, Greeley R, Benowitz I, McHugh L, Henry D, DiFedele L, Adler E, Naqvi S, Lifshitz E, Tan C, Montana B. Outbreak of Septic Arthritis Associated with Intra-Articular Injections at an Outpatient Practice - New Jersey, 2017. MMWR Morb Mortal Wkly Rep. 2017;66:777–779. doi: 10.15585/mmwr.mm6629a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sultana S, Dey R, Bishayi B. Dual neutralization of TNFR-2 and MMP-2 regulates the severity of S. aureus induced septic arthritis correlating alteration in the level of interferon gamma and interleukin-10 in terms of TNFR2 blocking. Immunol Res. 2018;66:97–119. doi: 10.1007/s12026-017-8979-y. [DOI] [PubMed] [Google Scholar]
- 10.Giuffre JL, Jacobson NA, Rizzo M, Shin AY. Pyarthrosis of the small joints of the hand resulting in arthrodesis or amputation. J Hand Surg Am. 2011;36:1273–1281. doi: 10.1016/j.jhsa.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 11.Barbieri RA, Freeland AE. Osteomyelitis of the hand. Hand Clin. 1998;14:589–603, ix. [PubMed] [Google Scholar]
- 12.Kowalski TJ, Thompson LA, Gundrum JD. Antimicrobial management of septic arthritis of the hand and wrist. Infection. 2014;42:379–384. doi: 10.1007/s15010-013-0566-0. [DOI] [PubMed] [Google Scholar]
- 13.Bach HG, Steffin B, Chhadia AM, Kovachevich R, Gonzalez MH. Community-associated methicillin-resistant Staphylococcus aureus hand infections in an urban setting. J Hand Surg Am. 2007;32:380–383. doi: 10.1016/j.jhsa.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Kistler JM, Thoder JJ, Ilyas AM. MRSA Incidence and Antibiotic Trends in Urban Hand Infections: A 10-Year Longitudinal Study. Hand (N Y) 2019;14:449–454. doi: 10.1177/1558944717750921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwak SH, Bae JY, Oh Y, Jang HS, Ahn TY, Lee SH. Primarily treated patients versus referred patients in the treatment of native septic arthritis of digits: a retrospective comparative study. BMC Musculoskelet Disord. 2020;21:780. doi: 10.1186/s12891-020-03770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung SR, Kang YC, McGrouther DA. Techniques for Continuous Irrigation of Septic Joints of the Hand. Tech Hand Up Extrem Surg. 2019;23:133–137. doi: 10.1097/BTH.0000000000000241. [DOI] [PubMed] [Google Scholar]
- 17.McBride S, Mowbray J, Caughey W, Wong E, Luey C, Siddiqui A, Alexander Z, Playle V, Askelund T, Hopkins C, Quek N, Ross K, Orec R, Mistry D, Coomarasamy C, Holland D. Epidemiology, Management, and Outcomes of Large and Small Native Joint Septic Arthritis in Adults. Clin Infect Dis. 2020;70:271–279. doi: 10.1093/cid/ciz265. [DOI] [PubMed] [Google Scholar]
- 18.Vorderwinkler KP, Mühldorfer M, Pillukat T, van Schoonhoven J. Treatment of bacterial infection in the interphalangeal joints of the hand. Oper Orthop Traumatol. 2011;23:192–203. doi: 10.1007/s00064-011-0024-z. [DOI] [PubMed] [Google Scholar]
- 19.Allieu Y, Chammas M, Hixson ML. External fixation for treatment of hand infections. Hand Clin. 1993;9:675–682. [PubMed] [Google Scholar]
- 20.Clerc O, Prod'hom G, Greub G, Zanetti G, Senn L. Adult native septic arthritis: a review of 10 years of experience and lessons for empirical antibiotic therapy. J Antimicrob Chemother. 2011;66:1168–1173. doi: 10.1093/jac/dkr047. [DOI] [PubMed] [Google Scholar]
- 21.Türker T, Capdarest-Arest N, Bertoch ST, Bakken EC, Hoover SE, Zou J. Hand infections: a retrospective analysis. PeerJ. 2014;2:e513. doi: 10.7717/peerj.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stengel D, Bauwens K, Sehouli J, Ekkernkamp A, Porzsolt F. Systematic review and meta-analysis of antibiotic therapy for bone and joint infections. Lancet Infect Dis. 2001;1:175–188. doi: 10.1016/S1473-3099(01)00094-9. [DOI] [PubMed] [Google Scholar]
- 23.Gjika E, Beaulieu JY, Vakalopoulos K, Gauthier M, Bouvet C, Gonzalez A, Morello V, Steiger C, Hirsiger S, Lipsky BA, Uçkay I. Two weeks versus four weeks of antibiotic therapy after surgical drainage for native joint bacterial arthritis: a prospective, randomised, non-inferiority trial. Ann Rheum Dis. 2019;78:1114–1121. doi: 10.1136/annrheumdis-2019-215116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sinha M, Jain S, Woods DA. Septic arthritis of the small joints of the hand. J Hand Surg Br. 2006;31:665–672. doi: 10.1016/j.jhsb.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 25.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR Infectious Diseases Society of America. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 26.Tan V, Pepe MD, Esterhai JL. Sepsis of the shoulder girdle. In: Disoders of the shoulder: diagnosis and management. Iannotti J, Williams GR, editors. Philadelphia, Baltimore, New York, London, Buenos Aires, Hong Kong, Sydney, Tokyo: Lippincott Williams and Wilkins, 1998: 951-976. [Google Scholar]
- 27.American Society for Surgery of the Hand. Clinical Assessment Committee Report. IL, United States: Rosemont, 1976. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original anonymous dataset is available on request from the corresponding author at lipatov_k_v@staff.sechenov.ru.