Abstract
Question
Effective prevention of suicide requires a comprehensive understanding of risk factors.
Study selection and analysis
Five databases were systematically searched to identify psychological autopsy studies (published up to February 2022) that reported on risk factors for suicide mortality among adults in the general population. Effect sizes were pooled as odds ratios (ORs) using random-effects models for each risk factor examined in at least three independent samples.
Findings
A total of 37 case–control studies from 23 countries were included, providing data on 40 risk factors in 5633 cases and 7101 controls. The magnitude of effect sizes varied substantially both between and within risk factor domains. Clinical factors had the strongest associations with suicide, including any mental disorder (OR=13.1, 95% CI 9.9 to 17.4) and a history of self-harm (OR=10.1, 95% CI 6.6 to 15.6). By comparison, effect sizes were smaller for other domains relating to sociodemographic status, family history, and adverse life events (OR range 2–5).
Conclusions
A wide range of predisposing and precipitating factors are associated with suicide among adults in the general population, but with clear differences in their relative strength.
PROSPERO registration number
CRD42021232878.
Keywords: Suicide & self-harm, Adult psychiatry
WHAT IS ALREADY KNOWN ON THIS TOPIC
Psychological autopsy provides one validated approach to determine factors that contribute to suicide. Previous reviews of this literature have focused on a selected number of risk factors.
WHAT THIS STUDY ADDS
We have synthesised a wide range of risk factors for suicide, which allows for a comparison of their relative risks. Sources of heterogeneity were examined by meta-regression and subgroup analyses.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Suicide prevention should combine public health approaches with interventions that target high-risk groups, including those with mental disorders, a history of self-harm, and recent adverse life events.
Background
Suicide is a global public health concern, accounting for over 700 000 deaths annually.1 Identifying factors associated with suicide can improve risk stratification and help target interventions for high-risk groups.2 One widely used approach to investigating suicide risk factors at the individual level is the psychological autopsy method,3 which involves collecting information about the person who has died by suicide through standardised interviews with proxy informants (such as family members) and, when available, examination of medical and coronial records. This retrospective approach aims to construct a comprehensive picture of the clinical and psychosocial circumstances that contributed to the suicide. In doing so, psychological autopsies allow for examination of a wider range of risk factors, and in more detail, than possible in register-based studies which rely on data that is routinely collected for administrative purposes.4 To our knowledge, five previous reviews have quantitatively summarised findings from psychological autopsy studies,5–9 but these have been limited in scope (primarily focusing on mental disorders) and samples (including selected populations such as psychiatric patients). The most recent meta-analysis, based on studies published up to 2016, only examined associations with mood and substance use disorders.9 Synthesising the full range of risk factors reported in the psychological autopsy literature by adopting a uniform analytical approach would allow for a direct comparison of their associations with suicide.
Objectives
We have conducted a systematic review and meta-analysis to provide an up-to-date and comprehensive synthesis of psychological autopsy studies comparing adults in the general population who died by suicide with those who did not. We aimed to improve the precision of effect sizes of previously identified risk factors, to delineate associations not examined in prior meta-analyses and to compare estimates across risk factor domains. Findings could assist clinicians to prioritise interventions based on modifiable risk factors and their relative strengths, researchers to consider evidence gaps and policy makers to target resources most effectively.
Study selection and analysis
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines10 (online supplemental table S1). The study protocol was pre-registered with PROSPERO.
ebmental-2022-300549supp001.pdf (307.2KB, pdf)
Search strategy
We systematically searched five electronic databases (PubMed, Global Health, Embase, Web of Science and PsycINFO) for psychological autopsy studies published from inception to 28 February 2022. Keywords were identical for all databases: (suicid*) AND (autops*). No language restrictions were set. Bibliographical searches were complemented by manual searches of reference lists of included studies and previous systematic reviews.5–9
Selection criteria
One researcher (AU) screened titles and abstracts of the retrieved articles for eligibility. Full-text publications were then screened with an additional reviewer (LF) and disagreements were resolved by consensus. Primary studies using the psychological autopsy method to examine risk factors for death by suicide in adults from the general population were eligible for inclusion. The following inclusion criteria were set: the psychological autopsy study (1) has a quantitative observational design, (2) includes predominantly adults aged 18–65 years, (3) is based on a general population sample, (4) includes suicide mortality as outcome and (5) provides data for a control group of general population individuals either living in the community (living control group) or who died from causes other than suicide (deceased control group). The inclusion of studies with controls who died by causes other than suicide is consistent with previous reviews of psychological autopsy studies.5–9 We excluded studies (1) with qualitative and case designs, (2) that examined self-harm or attempted suicide as outcome, (3) without proxy interviews available for all suicide cases, (4) with selected samples (eg, soldiers) or specific age groups (eg, exclusively adolescents or older adults) and (5) including a high-risk control group (eg, psychiatric patients). Studies excluded based on these sample criteria are listed in online supplemental table S2.
Data extraction
Data extraction was done independently by two authors (LF and AU) using a predetermined form listing relevant study characteristics (ie, publication year, country and sample size), sample details (ie, age, sex and type of control group) and risk factor estimates. Extraction sheets were cross-checked for consistency and discrepancies were resolved by discussion within the research team. When study characteristics were unclear, the authors of the respective primary papers were contacted. When multiple publications on the same or overlapping study population were available, information on risk factors was extracted from the investigation with the largest sample. Data were only extracted from overlapping publications when a new risk factor was reported. For example, a 2002 Chinese investigation analysed risk factors for suicide in 519 cases and 536 controls,11 for which an update was published in 2010 that covered an overlapping sample of 895 cases and 701 controls.12 In this case, we extracted data from the 2010 article (with the largest sample) and only included data from the 2002 investigation if an additional risk factor was reported. For brevity, one main reference is provided for each unique study (see online supplemental table S3 for a list of all included publications).
Data analysis
Crude ORs and their 95% CIs were extracted as reported or calculated from available prevalence data in the paper (eg, 2×2 contingency tables). The majority (78%) of studies also included adjusted estimates derived from multivariable models. As adjustments were inconsistent across studies, ranging from basic demographic characteristics to psychiatric diagnoses, we selected crude estimates for the main analysis in order to reduce heterogeneity due to non-comparability. In sensitivity analyses, however, we compared adjusted to crude effect sizes when reported in the same study.
Risk factors were categorised into four broad domains: sociodemographic, clinical, family history and adverse life events. Similar risk factors within a particular domain were grouped. For example, all alcohol-related exposures (eg, alcohol dependence, abuse and misuse) were coded as alcohol use disorder.6 A recent meta-analysis indicated that combining these variables into a single measure does not lead to a significant loss of information.9 All mental disorders were based on standardised diagnostic criteria. Additionally, adverse life events were grouped into three temporal categories: within the past month, 3 months and 6 months. In a secondary analysis, we estimated the crude prevalence of the strongest risk factors within an individual domain.
Risk of bias was assessed using the Newcastle-Ottawa Scale for case–control studies.13 Studies were rated on three criteria (ie, selection, comparability and exposure) with a total of eight items (eg, representativeness of the cases, comparability of cases and controls and ascertainment of exposure), resulting in an overall score between 0 and 9. A maximum score of 9 points indicates low risk of bias.
Meta-analyses were conducted using the metan command in Stata IC (V.13). To ensure accuracy and reliability of obtained estimates, meta-analysis was performed only for risk factors that were examined in at least three independent samples.14 For all analyses, a random-effects model (using the inverse-variance method) was generated to account for the anticipated heterogeneity between studies. Heterogeneity was estimated using the I² statistic, which specifies the percentage of variation in effect sizes underlying the different studies. Considerable heterogeneity across studies is indicated by an I² value of 75% and over.15 The degree to which methodological differences between studies moderated the associations between risk factors and suicide was investigated using univariate meta-regression models (using the metareg command). Meta-regression was considered for risk factors when there were 10 or more samples in the meta-analysis.15 Categorical variables examined in meta-regression were type of control group (living vs deceased), data source for control subjects (proxy informants vs controls themselves) and region (low/middle-income vs high-income). Risk of bias score (0–9), proportion of men in the sample (%) and sample size (n) were included as continuous covariates. We were not able to include mean age at death as a continuous covariate in meta-regression since a third (32%) of studies did not provide such information. The presence of publication bias was examined by visual inspection of funnel plots16 and by applying Egger’s test17 for variables examined in at least 10 independent samples.15
Post hoc, we conducted subgroup analyses by type of control group (living vs deceased) and sensitivity analyses excluding studies in which controls acted as their own informants.
Findings
Study characteristics
Our systematic search of the literature yielded 4284 unique records for screening, from which 231 full-text reports were examined for eligibility (online supplemental figure S1). A total of 37 studies reported in 97 publications met our inclusion criteria (table 1). This discrepancy between the number of studies and publications is partly explained by one Chinese investigation that resulted in more than 20 publications on the same sample (online supplemental table S3). Studies were conducted across 23 countries (21 [57%] in high-income countries) and published between 1994 and 2021. All included studies had a case–control design, with sample sizes ranging from 45 to 1596 (median=216, IQR=194–400). Collectively, studies included a total of 12 734 individuals, of which 7101 (56%) were controls and 5633 (44%) were suicide cases, with an average of 152 suicides per study. The mean age of the suicide group was 39.8 years (SD=10.9) and 71% were men. All but three (92%) studies included both men and women. Twenty-nine (78%; n=9194) studies recruited living community controls and eight (22%; n=3540) used a control group of people who died from causes other than suicide (mostly accidents and sudden deaths). In five (14%; n=2419) studies, information on the living control group was collected directly from (a portion of) the control subjects themselves, rather than by interviewing proxy informants.
Table 1.
Study characteristics
| Study | Country | Case group | Control group* | NOS | |||
| n | Age, M (range) | Men (%) | n | Type | |||
| Almasi et al (2009)e1 | Hungary | 194 | 43 (30–62) | 80.9 | 194 | Living† | 5 |
| Altindag et al (2005)e2 | Turkey | 26 | 24 (12–62) | 15.4 | 25 | Living | 9 |
| Anton-San-Martin et al (2013)e3 | Spain | 40 | 56 (19–90) | 67.5 | 80 | Living | 7 |
| Appleby et al (1999)e4 | England | 84 | 27 (13–34) | 81.0 | 64 | Living | 6 |
| Arafat et al (2021)e5‡ | Bangladesh | 100 | 26 (9–75) | 49.0 | 100 | Living | 7 |
| Beautrais (2001)e6‡ | New Zealand | 202 | 37 (14–88) | 77.7 | 984 | Living | 7 |
| Chachamovich et al (2015)e7 | Canada | 120 | 23 | 82.5 | 120 | Living | 4 |
| Chen et al (2006)e8‡ | China | 150 | 39 (15–59) | 64.0 | 150 | Living | 7 |
| Cheng et al (2000)e9‡ | Taiwan | 113 | NR | 61.5 | 226 | Living | 8 |
| de la Vega Sanchez et al (2020)e10 | Spain | 192 | 54 | 100 | 81 | Deceased | 4 |
| De Leo et al (2013)e11‡ | Australia | 261 | ≥35 | 75.1 | 182 | Deceased | 6 |
| Foster et al (1999)e12 | Ireland | 117 | 16–76 | 79.5 | 117 | Living | 7 |
| Gururaj et al (2004)e13 | India | 269 | 75% 16–49 | 64.3 | 269 | Living† | 7 |
| Jia et al (2014)e14‡ | China | 200 | 61 (11–93) | 57.5 | 200 | Living | 7 |
| Jollant et al (2014)e15 | Philippines | 15 | 15–64 | 73.3 | 30 | Living | 5 |
| Khan et al (2008)e16 | Pakistan | 100 | NR | 83.0 | 100 | Living | 7 |
| Kim et al (2003)e17‡ | Canada | 115 | 29 (18–65) | 100 | 82 | Living | 8 |
| Kodaka et al (2017)e18‡ | Japan | 102 | ≥20 | 69.6 | 334 | Living | 7 |
| Kolves et al (2006)e19‡ | Estonia | 427 | 48 | 80.3 | 427 | Living† | 7 |
| Kurihara et al (2009)e20 | Indonesia | 60 | 41 (13–87) | 63.3 | 120 | Living | 9 |
| Manoranjitham et al (2010)e21 | India | 100 | 42 | 59.0 | 100 | Living | 6 |
| Martiello et al (2019)e22 | Italy | 91 | ≥25 | 80.2 | 270 | Living | 7 |
| Morales & Martinez (2010)e23 | Colombia | 101 | 28 | 69.3 | 112 | Deceased | 7 |
| Nicolas et al (2016)e24‡ | Canada | 42 | 37 | 50.0 | 42 | Living | 5 |
| Overholser et al (2012)e25 | United States | 148 | 47 | 78.4 | 257 | Deceased | 4 |
| Owens et al (2003)e26 | England | 100 | ≥18 | 67.0 | 100 | Living | 6 |
| Page et al (2014)e27 | Australia | 84 | 18–34 | 84.5 | 250 | Living | 7 |
| Palacio et al (2007)e28‡ | Colombia | 108 | 29 (19–43) | 80.6 | 108 | Deceased | 6 |
| Politakis et al (2017)e29 | Slovenia | 90 | 49 | 70.0 | 90 | Living | 4 |
| Rasouli et al (2019)e30 | Iran | 40 | 39 (19–75) | 80.0 | 40 | Living† | 7 |
| Ross et al (2017)e31 | Australia | 126 | 25–44 | 100 | 68 | Deceased | 6 |
| Schneider et al (2006)e32‡ | Germany | 163 | 50 | 64.4 | 396 | Living† | 6 |
| Tong & Phillips (2010)e33‡ | China | 895 | 42 (12–94) | 50.7 | 701 | Deceased | 5 |
| Vijayakumar & Rajkumar (1999)e34 | India | 100 | ≥15 | 55.0 | 100 | Living | 7 |
| Zhang et al (2004)e35‡ | China | 66 | 46 | 72.7 | 66 | Living | 5 |
| Zhang et al 2010e36‡ | China | 392 | 27 (15–34) | 54.6 | 416 | Living | 7 |
| Zonda (2006)e37 | Hungary | 100 | 52 | 67.0 | 100 | Deceased | 7 |
Note. References are provided in online supplemental table S3.
*Matched with the case group for age and sex in all but five studies.e6,e10,e11,e25,e33
†Control subjects acted as their own informants.
‡Multiple publications for this study.
NOS, Newcastle-Ottawa Scale score; NR, not reported.
Quality assessment
Of a maximum of 9 points, the mean quality score of case–control studies was 6.4 (SD=1.3, range 4–9). Twenty-one (57%) studies had a score of 7 points or more, indicating low risk of bias (online supplemental table S4). Across studies, non-response was a key weakness. Many investigations with considerable differences in response rates (>10%) between cases and controls did not clarify reasons for this discrepancy and therefore scored conservatively for this domain.
Risk estimates
We identified 40 risk factors that were examined in at least three independent samples (table 2). For significant associations, pooled ORs ranged from 2.2 to 4.0 in the sociodemographic domain. The strongest risk factors identified were social isolation (OR=4.0, 95% CI 2.1 to 7.7), unemployment (OR=3.8, 95% CI 2.7 to 5.2) and low socioeconomic status (OR=2.8, 95% CI 1.8 to 4.2). Risk factors within the family history domain were a family history of mental disorder (OR=5.2, 95% CI 1.9 to 14.1), suicide (OR=3.7, 95% CI 2.3 to 5.7) and attempted suicide (OR=2.8, 95% CI 1.5 to 5.0).
Table 2.
Pooled estimates of risk factors for suicide, by domain
| Samples (k) | Cases (n) | Controls (n) | OR (95% CI) | z | I² | |
| Sociodemographic domain | ||||||
| Social isolation | 10 | 1549 | 1613 | 4.0 (2.1 to 7.7) | 4.2 | 95 |
| Unemployment | 25 | 4010 | 4439 | 3.8 (2.7 to 5.2) | 8.1 | 79 |
| Low socioeconomic status | 4 | 284 | 450 | 2.8 (1.8 to 4.2) | 4.9 | 0 |
| Low education | 19 | 3099 | 4474 | 2.7 (2.1 to 3.5) | 8.2 | 64 |
| Single/not married | 21 | 2773 | 3576 | 2.4 (1.8 to 3.2) | 6.4 | 74 |
| Low income | 6 | 1530 | 2317 | 2.4 (1.6 to 3.6) | 4.2 | 74 |
| Living alone | 15 | 2748 | 3014 | 2.3 (1.5 to 3.4) | 4.0 | 77 |
| Not religious | 12 | 1383 | 1550 | 2.2 (1.4 to 3.5) | 3.4 | 77 |
| Not having children | 6 | 1026 | 979 | 1.3 (0.9 to 1.8) | 1.4 | 61 |
| Family history domain | ||||||
| Mental disorder | 6 | 415 | 800 | 5.2 (1.9 to 14.1) | 3.2 | 82 |
| Suicide | 14 | 2018 | 2268 | 3.7 (2.3 to 5.7) | 5.7 | 73 |
| Suicide attempt | 7 | 1638 | 1789 | 2.8 (1.5 to 5.0) | 3.4 | 82 |
| Clinical domain | ||||||
| Any mental disorder | 28 | 4085 | 4368 | 13.1 (9.9 to 17.4) | 17.8 | 76 |
| Depression | 22 | 3432 | 3805 | 11.0 (7.3 to 16.5) | 11.5 | 77 |
| Schizophrenia spectrum disorder | 17 | 3056 | 4165 | 7.8 (4.5 to 13.5) | 7.4 | 63 |
| Bipolar disorder | 8 | 1220 | 1485 | 4.6 (2.1 to 10.1) | 3.8 | 33 |
| Substance use disorder | 21 | 3525 | 4621 | 3.7 (2.8 to 5.0) | 8.7 | 71 |
| Alcohol use disorder | 18 | 2777 | 4277 | 3.2 (2.3 to 4.4) | 6.5 | 71 |
| Drug use disorder | 6 | 1163 | 2098 | 3.0 (1.7 to 5.4) | 3.7 | 20 |
| Anxiety disorder | 17 | 2997 | 4199 | 2.5 (1.7 to 3.5) | 4.8 | 52 |
| Dysthymia | 6 | 964 | 1566 | 2.4 (1.4 to 4.1) | 3.2 | 36 |
| Any personality disorder (PD) | 13 | 1437 | 1634 | 6.8 (4.7 to 9.8) | 10.3 | 42 |
| Borderline PD | 7 | 754 | 1009 | 9.0 (5.6 to 14.4) | 9.0 | 0 |
| Paranoid PD | 5 | 519 | 807 | 6.2 (3.5 to 11.2) | 6.1 | 0 |
| Dependent PD | 4 | 393 | 739 | 6.1 (2.5 to 15.1) | 3.9 | 0 |
| Avoidant PD | 5 | 526 | 701 | 3.9 (1.4 to 11.1) | 2.5 | 69 |
| Antisocial PD | 5 | 515 | 715 | 3.4 (2.0 to 6.1) | 4.3 | 0 |
| Psychiatric treatment | 11 | 2171 | 2972 | 10.5 (7.4 to 14.9) | 13.1 | 41 |
| History of self-harm | 26 | 3466 | 4582 | 10.1 (6.6 to 15.6) | 10.5 | 77 |
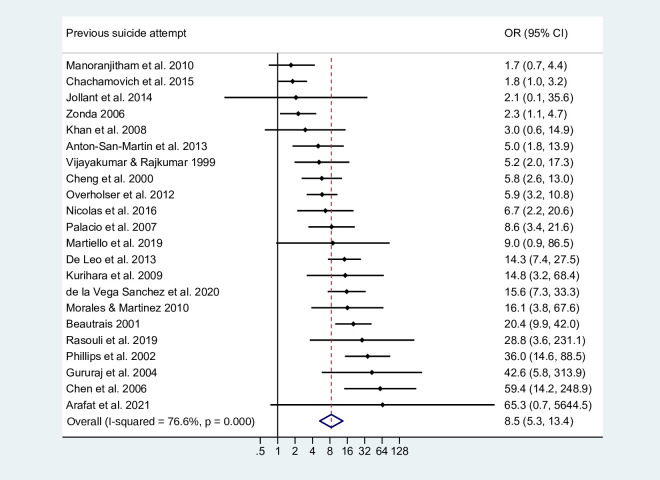
| Previous suicide attempt | 22 | 2971 | 4107 | 8.5 (5.3 to 13.4) | 9.1 | 77 |
| Smoking | 4 | 412 | 660 | 4.3 (2.3 to 7.9) | 4.6 | 67 |
| Physical illness | 16 | 2963 | 3253 | 2.9 (2.4 to 3.6) | 11.2 | 19 |
| Adverse life events | ||||||
| Relationship conflict | 10 | 1338 | 2318 | 5.0 (3.3 to 7.6) | 7.8 | 73 |
| Legal problems | 6 | 889 | 1769 | 4.8 (2.4 to 9.4) | 4.5 | 75 |
| Family-related conflict | 9 | 1154 | 1364 | 4.5 (2.0 to 10.3) | 3.6 | 92 |
| Abuse/victimisation | 6 | 823 | 803 | 3.5 (2.4 to 5.0) | 6.8 | 0 |
| Financial problems | 15 | 1805 | 2261 | 2.8 (2.0 to 4.0) | 5.9 | 65 |
| Early separation from parents | 4 | 344 | 676 | 2.7 (1.6 to 4.5) | 3.7 | 5 |
| Work/school-related conflict | 11 | 1614 | 2565 | 1.8 (1.1 to 2.8) | 2.5 | 84 |
| Bereavement | 7 | 889 | 1122 | 1.2 (0.5 to 3.1) | 0.4 | 86 |
| Timing of life events | ||||||
| Within past month | 7 | 1140 | 1136 | 10.4 (7.1 to 15.3) | 12.1 | 19 |
| Within past 6 months | 3 | 402 | 402 | 5.3 (1.8 to 15.9) | 3.0 | 91 |
| Within past 3 months | 4 | 613 | 613 | 2.9 (1.6 to 5.0) | 3.7 | 72 |
Within the clinical domain, a history of self-harm (OR=10.1, 95% CI 6.6 to 15.6) and a previous suicide attempt (OR=8.5, 95% CI 5.3 to 13.4; figure 1) were both strongly associated with suicide. We found strong associations for any mental disorder (OR=13.1, 95% CI 9.9 to 17.4) and any personality disorder (OR=6.8, 95% CI 4.7 to 9.8). By diagnosis, depression had the strongest association with suicide (OR=11.0, 95% CI 7.3 to 16.5), followed by borderline personality disorder (OR=9.0, 95% CI 5.6 to 14.4) and schizophrenia spectrum disorder (OR=7.8, 95% CI 4.5 to 13.5). Risk of suicide was comparable for alcohol use disorder (OR=3.2, 95% CI 2.3 to 4.4) and drug use disorder (OR=3.0, 95% CI 1.7 to 5.4).
Figure 1.
Previous suicide attempt as a risk factor for suicide. The dots and lines represent the ORs and corresponding 95% CIs from each primary study. The diamond denotes the pooled summary effect size and CI from random-effects meta-analysis. References are provided in online supplemental table S3.
For adverse life events, relationship conflict (OR=5.0, 95% CI 3.3 to 7.6), legal problems (OR=4.8, 95% CI 2.4 to 9.4) and family-related conflict (OR=4.5, 95% CI 2.0 to 10.3) had the strongest associations with suicide. By timing, adverse life events occurring within the previous month increased the risk of suicide 10-fold (OR=10.4, 95% CI 7.1 to 15.3).
The prevalence of the strongest risk factor within each domain is listed in online supplemental table S5—all of which were more than 40% in people who died by suicide. Seven in 10 (71.1%) cases had a mental disorder at the time of death compared with 22.2% of controls. In addition, a previous suicide attempt was documented for 28.5% of cases and 6.0% of controls.
Sensitivity analysis
Comparisons between crude and adjusted estimates are provided in online supplemental table S6 for 21 risk factors. Adjusted ORs were smaller than crude ORs for all but three factors examined, with an average reduction of 19% in risk estimates (ranging from +48% to −61%). The largest reductions were found in the clinical domain. For example, the crude OR for a history of self-harm (OR=18.1, 95% CI 13.2 to 24.6) was two times larger than its adjusted counterpart (aOR=9.1, 95% CI 6.0 to 13.7). Similar differences were found for any personality disorder (OR=10.7 vs aOR=4.2) and any mental disorder (OR=12.1 vs aOR=7.7). Differences between crude and adjusted estimates should, however, be interpreted with caution because many studies exclusively reported significant associations from the multivariable models, which likely results in biased comparisons between estimates.
Meta-regression
We examined six variables as possible sources of between-study heterogeneity in estimates for 21 risk factors where there were at least 10 samples (online supplemental table S7). Type of control group (living vs deceased) was significantly associated with heterogeneity for 7 (33%) out of all 21 risk factors studied: marital status, living alone, any mental disorder, schizophrenia spectrum disorder, substance use disorder, alcohol use disorder, and any personality disorder. We found that studies including a deceased control group reported smaller effect sizes for these risk factors compared with those including living controls. Furthermore, source of data for the control group (proxy informants vs control individuals themselves) explained some of the between-study heterogeneity only for schizophrenia spectrum disorder and a history of self-harm. Results indicate larger effect sizes for these two risk factors in studies where control subjects were interviewed directly (instead of proxy respondents). Income region was a moderator only for the association between depression and suicide, with a smaller effect observed in samples from high-income countries. No consistent associations for between-study heterogeneity were found for sample size, risk of bias and proportion of men.
Publication bias
We found evidence of publication bias for eight risk factors (online supplemental table S7). Egger’s test was significant for social isolation (p=0.001), unemployment (p=0.015), living alone (p=0.044), any mental disorder (p=0.009), depression (p=0.071), substance use disorder (p=0.006), any personality disorder (p=0.006) and financial problems (p=0.061). Funnel plots for these variables are shown in online supplemental figures S2–S9.
Conclusions and implications
In this systematic review and meta-analysis of 37 psychological autopsy studies comparing 5633 adults who died by suicide with 7101 controls, we have synthesised findings on a wide range of risk factors for suicide in the general population. Our work adds to the evidence base in three ways.
First, previous reviews of psychological autopsy studies5–9 have not captured the breadth of individual-level risk factors for suicide, and instead mainly focused on the contribution of mental disorders to suicide risk. In contrast, we meta-analysed effect sizes for a broader range of risk factors, which allows for comparison between risk factor domains. Specifically, across the 40 risk factors under study, the strongest associations with suicide were found in the clinical domain. The presence of any mental disorder was associated with more than a 10-fold increase in the odds of suicide, as was a history of self-harm. By comparison, effect sizes (ranging from 2 to 5) were smaller for other domains relating to sociodemographic factors, family history, and adverse life events. Absolute rates were also high, with 71% of suicide decedents reported to have a mental disorder at the time of death and 29% having previously attempted suicide.
Second, we found considerable variation in risk estimates within each domain. For example, although it is well known that having a mental disorder is a strong risk factor for suicide,2 there were clear differences between diagnoses in their relative strength. Effect sizes ranged from 2 for dysthymia and 3 for substance use disorders to 11 for depression. To our knowledge, we have for the first time quantified associations for individual personality disorders with suicide, with risk estimates in the range of 3 (antisocial personality disorder) to 9 (borderline personality disorder). In keeping, we also found such variation in effect sizes for adverse life events. Legal problems (such as contact with the criminal justice system) and interpersonal conflict had the strongest associations with suicide risk. The negative effect that exposure to stressful life events has on an individual’s overall functioning and life expectations may, at least in part, explain these findings.18 As expected, we found timing to be of significance, with adverse events occurring in the month before death being the most important. Other studies have found a dose–response relationship between the number of events experienced and the risk of suicide.18
Third, we have investigated possible explanations for the observed heterogeneity in risk estimates. Specifically, for a third of risk factors examined in meta-regression, significantly smaller effect sizes were observed in studies that included a control group of individuals who died from causes other than suicide, relative to studies with living controls. This finding was corroborated in post hoc subgroup analyses (online supplemental table S8). Comparing suicide cases with controls who have died by other external causes such as accidents may generate smaller or no differences between groups because of overlapping risk factors19 and because prematurely deceased controls may be at increased risk of suicide themselves.4 In addition, some deaths classified as accidents will include probable suicides,20 further reducing differences between cases and controls. This observation that heterogeneity is associated with study design underscores the need for a standardised approach to conducting psychological autopsies. We recommend that the optimal control group would be living individuals. Researchers need to consider, though, the implications of using living controls on the timing of risk factors, which may underestimate the effects of certain factors. To ensure comparability between groups, it has been recommended that information on living controls should equally be obtained by means of proxy-based interviews.21 In meta-regression analyses, however, we found that how data was collected for the control group (ie, whether proxy informants or controls themselves were interviewed) did not moderate the strength of associations for most risk factors. Post hoc sensitivity analyses confirmed this finding, showing no major change in the magnitude of estimates after removal of studies in which controls acted as their own informants (online supplemental table S9).
Strengths and limitations
Strengths of this review include the use of a quantitative synthesis and examination of a wide range of risk factors not limited to mental disorders. Several limitations should also be noted. First, the strength of the reported associations is likely to be overestimated as we did not account for confounding, and the risk factors examined are not independent from one another (eg, psychiatric comorbidity). In sensitivity analyses, we found that the majority of adjusted estimates were materially smaller than crude ones, with an average reduction of a fifth in effect sizes and up to half for clinical risk factors. However, because different studies used contrasting approaches to adjustment, which would make adjusted estimates difficult to compare, our main analysis focused on crude effect sizes. Future work should consider confounding more carefully, examine a fuller range of sociodemographic confounds when assessing clinical factors, and use consistent and replicable approaches. Second, we identified considerable heterogeneity for about one-third of all risk estimates. Although a high degree of heterogeneity can be expected in meta-analyses of observational studies,22 pooled effect sizes should be interpreted with caution, and ranges should be considered. This heterogeneity is likely caused by varying instruments used to assess risk factors. Third, we retained all eligible studies in our analyses irrespective of their methodological quality, which may have influenced the results—though there was little evidence to suggest that study quality was associated with heterogeneity in meta-regression. Fourth, we were unable to examine risk factors for men and women separately because most primary studies did not stratify analyses by sex; future work should investigate this. Fifth, our findings should not be generalised to adolescents and older adults as we only focused on working-age adults. Risk factors are known to vary by age groups2 and might have a different impact according to when they occur in someone’s life (eg, unemployment and physical illness).
In addition, there are several limitations inherent to the psychological autopsy approach,23–25 including issues relating to the choice (and selective non-response) of control subjects and the reliance on proxy reports—the latter being prone to recall bias and measurement error. While register-based studies may minimise such biases, they are more restricted in scope since many potential risk factors are not captured in routinely collected administrative records (eg, recent life events, social isolation, religious beliefs and self-harm not resulting in service contact). Although the method of psychological autopsy has been criticised for overestimating the contribution of mental disorders to suicide,25 risk estimates for diagnostic categories in the current review (in particular when limited to studies using living controls) were largely similar in magnitude to those reported in a recent meta-analysis of record linkage studies.22 In contrast, prospective cohort studies of suicide mortality in the general population—which allow for a more reliable measurement of exposures—tend to report more conservative risks for sociodemographic factors, adverse life events, family history of mental disorder, and depression.26–28 Among other reasons, effects might be smaller in prospective studies owing to long follow-up periods, whereas psychological autopsies focus on the time window close to death.9 Notwithstanding its limitations, the psychological autopsy method can complement other study designs to identify suicide risk factors, allow for triangulation of evidence, and may be the approach of choice in settings where population-based registers are not available or when prospective studies are not feasible.
Clinical implications
The main implication of this review is that suicide is associated with many factors across clinical, life events, family history, and sociodemographic domains—and within a particular domain, there are differential associations with suicide. Consistent with a stress-diathesis model,29 this underscores the need to understand suicide as the result of a cumulation of multiple risk factors,2 some of which are predisposing (such as sociodemographic background and family history) and some precipitating (such as incident diagnoses and life events). Consequently, suicide prevention should combine strategies aimed at a general reduction in population risk (eg, through means restriction) with interventions that focus on high-risk groups, such as people with severe mental illness or recently hospitalised for self-harm.30–32
Our findings underline the importance of both assessment and treatment of mental disorders in healthcare settings.33 Screening and assessment in itself will not improve outcomes, unless it leads to effective intervention.34 This approach differs from that in general population settings, where many people at elevated risk of suicide do not access healthcare services and links to effective interventions may not be possible or timely. Rather, high-risk groups should be a focus for prevention as they are likely to already be accessing healthcare services, such as individuals who have attempted suicide, especially if they have underlying mental disorders.35 Interventions to consider include psychosocial treatment following self-harm, particularly cognitive behavioural approaches, which can reduce risk of repetition.36 Brief interventions such as safety planning37 have also been found to prevent future suicidal behaviour. Another high-risk group with a treatment gap is people with depression, for whom effective pharmacological and psychosocial treatments are available38 and assessment of suicide risk can be improved by considering somatic39 and psychiatric40 comorbidities. Further, our findings highlight the need for assessment of suicide risk that incorporates multiple factors, and their interactions, in prediction models.41 Previous research found single factors, including self-harm, to be poor predictors of subsequent suicide.2
Conclusion
We found that a wide range of predisposing and precipitating risk factors are associated with suicide among adults in the general population, but to differing degrees. Our findings highlight a number of modifiable risk factors and suggest that suicide prevention should combine strategies aimed at a general reduction in population risk with interventions that focus on high-risk groups. As part of this, healthcare services at national, regional and local levels can review the extent and quality of clinical and psychosocial interventions to reduce suicide risk.
Footnotes
LF and RY contributed equally.
Contributors: SF and RY conceived and designed the study. LF and AU did the literature search, extracted the data, did the analyses, and, with SF, drafted the manuscript. All authors contributed to the interpretation of the findings and subsequent edits of the manuscript. SF and RY provided overall supervision to the project. SF is guarantor.
Funding: This study was funded by Wellcome Trust (202836/Z/16/Z).
Competing interests: There are no competing interests.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. WHO . Suicide worldwide in 2019: global health estimates. Geneva: World Health Organization, 2021. [Google Scholar]
- 2. Fazel S, Runeson B. Suicide. N Engl J Med 2020;382:266–74. 10.1056/NEJMra1902944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Conner KR, Beautrais AL, Brent DA, et al. The next generation of psychological autopsy studies. Suicide Life Threat Behav 2011;41:594–613. 10.1111/j.1943-278X.2011.00057.x [DOI] [PubMed] [Google Scholar]
- 4. Pirkis J, Nicholas A, Gunnell D. The case for case–control studies in the field of suicide prevention. Epidemiol Psychiatr Sci 2020;29:e62. 10.1017/S2045796019000581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cavanagh JTO, Carson AJ, Sharpe M, et al. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395–405. 10.1017/S0033291702006943 [DOI] [PubMed] [Google Scholar]
- 6. Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry 2004;4:37. 10.1186/1471-244X-4-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yoshimasu K, Kiyohara C, Miyashita K, et al. Suicidal risk factors and completed suicide: meta-analyses based on psychological autopsy studies. Environ Health Prev Med 2008;13:243–56. 10.1007/s12199-008-0037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cho S-E, Na K-S, Cho S-J, et al. Geographical and temporal variations in the prevalence of mental disorders in suicide: systematic review and meta-analysis. J Affect Disord 2016;190:704–13. 10.1016/j.jad.2015.11.008 [DOI] [PubMed] [Google Scholar]
- 9. Conner KR, Bridge JA, Davidson DJ, et al. Metaanalysis of mood and substance use disorders in proximal risk for suicide deaths. Suicide Life Threat Behav 2019;49:278–92. 10.1111/sltb.12422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Phillips MR, Yang G, Zhang Y, et al. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet 2002;360:1728–36. 10.1016/S0140-6736(02)11681-3 [DOI] [PubMed] [Google Scholar]
- 12. Tong Y, Phillips MR. Cohort-specific risk of suicide for different mental disorders in China. Br J Psychiatry 2010;196:467–73. 10.1192/bjp.bp.109.070409 [DOI] [PubMed] [Google Scholar]
- 13. Wells GA, Shea B, O'Connell D. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Health Research Institute, 2014. [Google Scholar]
- 14. Favril L, Yu R, Hawton K, et al. Risk factors for self-harm in prison: a systematic review and meta-analysis. Lancet Psychiatry 2020;7:682–91. 10.1016/S2215-0366(20)30190-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JPT, Thomas J, Chandler J. Cochrane Handbook for systematic reviews of interventions. 2nd ed. Chichester: John Wiley & Sons, 2019. [Google Scholar]
- 16. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56:455–63. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 17. Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fjeldsted R, Teasdale TW, Jensen M, et al. Suicide in relation to the experience of stressful life events: a population-based study. Arch Suicide Res 2017;21:544–55. 10.1080/13811118.2016.1259596 [DOI] [PubMed] [Google Scholar]
- 19. Neeleman J. A continuum of premature death. Meta-analysis of competing mortality in the psychosocially vulnerable. Int J Epidemiol 2001;30:154–62. 10.1093/ije/30.1.154 [DOI] [PubMed] [Google Scholar]
- 20. Gunnell D, Bennewith O, Simkin S, et al. Time trends in coroners' use of different verdicts for possible suicides and their impact on officially reported incidence of suicide in England: 1990-2005. Psychol Med 2013;43:1415–22. 10.1017/S0033291712002401 [DOI] [PubMed] [Google Scholar]
- 21. Isometsä ET. Psychological autopsy studies – a review. Eur Psychiatry 2001;16:379–85. 10.1016/S0924-9338(01)00594-6 [DOI] [PubMed] [Google Scholar]
- 22. Too LS, Spittal MJ, Bugeja L, et al. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J Affect Disord 2019;259:302–13. 10.1016/j.jad.2019.08.054 [DOI] [PubMed] [Google Scholar]
- 23. Hawton K, Appleby L, Platt S, et al. The psychological autopsy approach to studying suicide: a review of methodological issues. J Affect Disord 1998;50:269–76. 10.1016/s0165-0327(98)00033-0 [DOI] [PubMed] [Google Scholar]
- 24. Pouliot L, De Leo D. Critical issues in psychological autopsy studies. Suicide Life Threat Behav 2006;36:491–510. 10.1521/suli.2006.36.5.491 [DOI] [PubMed] [Google Scholar]
- 25. Hjelmeland H, Dieserud G, Dyregrov K, et al. Psychological autopsy studies as diagnostic tools: are they methodologically flawed? Death Stud 2012;36:605–26. 10.1080/07481187.2011.584015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yu R, Chen Y, Li L, et al. Factors associated with suicide risk among Chinese adults: a prospective cohort study of 0.5 million individuals. PLoS Med 2021;18:e1003545. 10.1371/journal.pmed.1003545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nie J, O'Neil A, Liao B, et al. Risk factors for completed suicide in the general population: a prospective cohort study of 242, 952 people. J Affect Disord 2021;282:707–11. 10.1016/j.jad.2020.12.132 [DOI] [PubMed] [Google Scholar]
- 28. Kleiman EM, Liu RT. Prospective prediction of suicide in a nationally representative sample: religious service attendance as a protective factor. Br J Psychiatry 2014;204:262–6. 10.1192/bjp.bp.113.128900 [DOI] [PubMed] [Google Scholar]
- 29. Mann JJ, Rizk MM. A brain-centric model of suicidal behavior. Am J Psychiatry 2020;177:902–16. 10.1176/appi.ajp.2020.20081224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mann JJ, Michel CA, Auerbach RP. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry 2021;178:611–24. 10.1176/appi.ajp.2020.20060864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hofstra E, van Nieuwenhuizen C, Bakker M, et al. Effectiveness of suicide prevention interventions: a systematic review and meta-analysis. Gen Hosp Psychiatry 2020;63:127–40. 10.1016/j.genhosppsych.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 32. Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry 2016;3:646–59. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 33. Bolton JM, Gunnell D, Turecki G. Suicide risk assessment and intervention in people with mental illness. BMJ 2015;351:h4978. 10.1136/bmj.h4978 [DOI] [PubMed] [Google Scholar]
- 34. Miller IW, Camargo CA, Arias SA, et al. Suicide prevention in an emergency department population. JAMA Psychiatry 2017;74:563–70. 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tidemalm D, Långström N, Lichtenstein P, et al. Risk of suicide after suicide attempt according to coexisting psychiatric disorder: Swedish cohort study with long term follow-up. BMJ 2008;337:a2205. 10.1136/bmj.a2205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Witt KG, Hetrick SE, Rajaram G. Psychosocial interventions for self-harm in adults. Cochrane Database Syst Rev 2021;4:CD013668. 10.1002/14651858.CD013668.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nuij C, van Ballegooijen W, de Beurs D, et al. Safety planning-type interventions for suicide prevention: meta-analysis. Br J Psychiatry 2021;219:419–26. 10.1192/bjp.2021.50 [DOI] [PubMed] [Google Scholar]
- 38. Malhi GS, Mann JJ. Depression. Lancet 2018;392:2299–312. 10.1016/S0140-6736(18)31948-2 [DOI] [PubMed] [Google Scholar]
- 39. Qin P, Hawton K, Mortensen PB, et al. Combined effects of physical illness and comorbid psychiatric disorder on risk of suicide in a national population study. Br J Psychiatry 2014;204:430–5. 10.1192/bjp.bp.113.128785 [DOI] [PubMed] [Google Scholar]
- 40. Hawton K, Casañas I Comabella C, Haw C, et al. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord 2013;147:17–28. 10.1016/j.jad.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 41. Fazel S, Wolf A, Larsson H, et al. The prediction of suicide in severe mental illness: development and validation of a clinical prediction rule (OXMIS). Transl Psychiatry 2019;9:98. 10.1038/s41398-019-0428-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ebmental-2022-300549supp001.pdf (307.2KB, pdf)
Data Availability Statement
Data are available upon reasonable request.