Abstract
Introduction
The coronavirus disease 2019 (COVID-19) pandemic enforced changes to healthcare services at a pace and extent not seen previously in the NHS. The Royal Devon and Exeter provides regional vascular surgery services. A consultant-led urgent ‘hot clinic’ was established, providing patients with ambulatory care. We aim to describe the service for critical limb ischaemia (CLI) before and during the COVID-19 pandemic, and evaluate this against recommended best practice.
Methods
Retrospective review of electronic databases and records of patients with CLI during a non-COVID vs COVID-19 period. Primary outcome measures were those established by guidance from the Vascular Society of Great Britain and Ireland.
Results
Non-COVID vs COVID-19: total patients n=97 vs 96, of which CLI patients n=29 vs 21. Median length of stay 15 vs 0 days (p<0.001); median time from referral to specialist review 0 vs 3 days (p<0.001); multidisciplinary team meeting (MDT) recorded 3% vs 29%; median time to intervention 6 vs 8 days; conservative management 52% vs 67%; endovascular 28% vs 10%; open surgery 21% vs 24%; 30-day survival 79% vs 76%.
Conclusion
COVID-19 imposed a major change to the service for patients with CLI with a focus on ambulatory care pathways for diagnosis and intervention. We observe a significant reduction in overall length of stay with no clinically significant change in time to consultant review, time to imaging, overall management strategy or outcomes. The results of this study show that patients with CLI can be managed safely and effectively on an ambulatory basis in accordance with established best practice.
Keywords: Ambulatory care, COVID, Critical limb ischaemia –Limb salvage, Outcomes
Introduction
The severe acute respiratory distress syndrome coronavirus-2 (SARS-CoV-2) reached the UK as part of a global health pandemic resulting in coronavirus disease 2019 (COVID-19) in early 2020. As part of measures to mitigate against this highly infectious and lethal disease, the UK Government announced a ‘lockdown’ on public life on 23 March 2020 with the aim of attenuating the rate of infection and the unprecedented surge of demand on healthcare services that had been seen in other parts of Europe.1 This was accompanied by guidance approved jointly by the four Surgical Royal Colleges of the UK and Ireland advising that the surgical workforce would require adaptation during the COVID-19 pandemic, and the priorities of care would be to maintain emergency surgery capability and protect the surgical workforce. This guidance advocated that plans must be dynamic and reactive, with surgeons needing to display flexibility, collaboration and leadership.2
With efforts concerted, emergency funding approved and normal bureaucracy waived, an intense period of innovation across the NHS ensued, with changes in the structure and delivery of services designed to permit an increase in the provision of intensive care beds.
The Royal Devon and Exeter Hospital provides a Vascular Surgery service as an arterial hub for East and South Devon. An emergency ‘on-call’ rota is normally staffed by six consultant surgeons with ‘24/7’ interventional radiology support. Traditional surgical working models of outpatient clinics, regular elective theatre lists and a weekly face-to-face multidisciplinary team meeting (MDT) were well established, with acute referrals coming via a surgical assessment unit into an inpatient bed. Local intensive care capacity was increased by utilising theatre space, resulting in a loss of usual vascular theatre availability. Due to the need for shielding, the number of consultant vascular surgeons was reduced to three. The service was therefore redesigned to have shielded consultants triaging existing referrals and taking new referrals before discussing urgent cases with the ‘on call’ consultant.
A major restructuring was the cancellation of all routine and elective outpatient work and the establishment of four urgent ‘hot clinic’ sessions per week, to which patients would be referred and seen on an urgent basis, with imaging and other investigations arranged in an ambulatory fashion. This was designed with support from the vascular laboratory providing same day duplex imaging. Urgent intervention could be scheduled as required. This type of service was not previously available in the region.
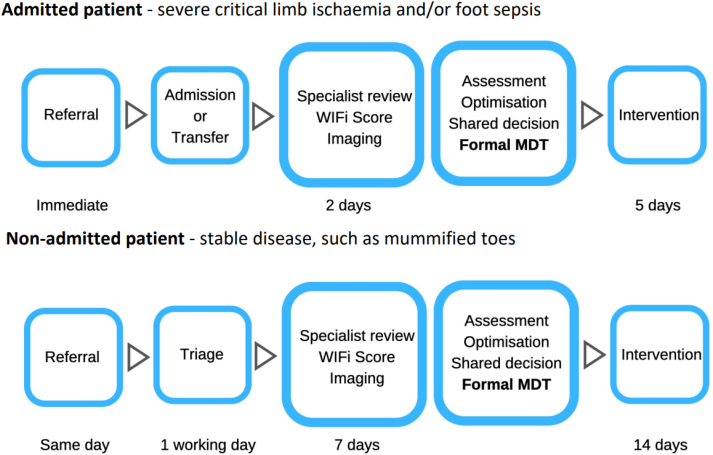
The Vascular Society of Great Britain and Ireland published guidance on best practice for peripheral arterial disease in April 2019, with the aim of reducing delays in care, standardising practice and improving outcomes across the UK.3 This guidance defines critical limb ischaemia (CLI) as ‘persistently recurring rest pain requiring analgesia for more than 2 weeks, OR ulceration, OR gangrene of the foot or toes’. Treatment should be MDT-led and delivered in an appropriate facility. Particular reference is made to timely management of these patients (Figure 1).
Figure 1 .
Pathways and timings for managing critical limb ischaemia3 CLI = Critical limb ischaemia; MDT = multidisciplinary team meeting
The aim of this work was to evaluate service provision for CLI in a period prior to the COVID-19 pandemic, compare this with the change in service during the COVID-19 pandemic and evaluate service provision against established guidance.
Methods
A retrospective review of an electronic referral database of admitted patients at our institution was conducted for a ‘non-COVID’ period between 23 March 2019 and 30 May 2019. This period was equivalent to the UK lockdown period in 2020. Patients admitted with a diagnosis of CLI or signs suggestive of it from referral were included. Data were collected from electronic admission and referral records, operation notes and radiology software on admission length of stay (LOS), time from referral to specialist review, time from specialist review to diagnostic imaging, record of formal MDT within 5 days, time to intervention, type of intervention (conservative, endovascular, open surgery) and 30-day outcome. Open surgery includes any open lower limb revascularisation procedure, including lower limb bypass or minor amputation. Endovascular management includes any percutaneous angiography-based procedure, which, in this institution, is performed in an interventional radiology suite.
The COVID-19 period was examined from 23 March 2020 to 30 May 2020 with retrospective review of the same electronic referral database, lists of patients seen in the ambulatory ‘hot clinic’ and telephone clinics. Data on the same parameters were collected.
Analysis was performed using R,4 with Mann–Whitney tests for comparing continuous data and Fisher's exact tests for categorical data.
Results
The results are summarised in Table 1.
Table 1 .
Demographics, management and outcomes for patients with diagnosis of CLI
| Variable | Non-COVID period (n=29) | COVID-19 period (n=21) |
|---|---|---|
| Age, mean (SD) | 78 (12) | 70 (12) |
| Gender, n (%) | ||
| Male | 16 (55) | 13 (62) |
| Female | 13 (45) | 8 (38) |
| Length of stay, median (IQR) | 15 (9–24) | 0 (0–6)* |
| Time from referral to Vascular review†, median (IQR) | 0 (0–1) | 3 (1–7)** |
| Time to imaging following review‡, median (IQR) | 1 (1–7) | 0 (0–2) |
| MDT recorded within 5 days, n (%) | 1 (3) | 6 (29) |
| Time to intervention§, median (IQR) | 6 (5–11) | 8 (2–16) |
| Management, n (%) | ||
| Conservative | 15 (52) | 14 (67) |
| Endovascular | 8 (28) | 2 (10) |
| Open surgery | 6 (21) | 5 (24) |
| 30 day outcome, n (%) | ||
| Alive | 23 (79) | 16 (76) |
| Alive with major amputation | 1 (4) | 3 (14) |
| Dead | 5 (17) | 2 (10) |
*p=<0.001; **p=0.02
†Based on 21 patients in COVID-19 period, 23 in Non-COVID period
‡Based on 14 patients in COVID-19 period, 25 in non-COVID period
§Based on 7 patients in COVID-19 period, 14 in non-COVID period
CLI = Critical limb ischaemia; COVID-19 = Coronavirus disease 2019; IQR = Interquartile range; MDT = multidisciplinary team meeting; SD = Standard deviation
Non-COVID period
During the non-COVID period, a total of 97 referrals were recorded on the electronic referral database, of which 29 patients had a diagnosis of CLI (30%). Of the CLI patients, the mean age was 78 years (standard deviation (SD) 12) and 55% were male. The median LOS was 15 days (interquartile range (IQR) 9–24). The median time to specialist review was 0 days (IQR 0–1). The median time from specialist review to imaging was 0 days (IQR 1–7). One of these patients had a documented MDT discussion (3%). The median time to intervention was 6 days (IQR 5–10). The management strategy for these patients was open surgery for 6 (21%), endovascular intervention for 8 (28%) and conservative management for 15 (52%). Outcomes at 30 days were 23 patients alive (79%), with 1 patient in this group having an above-knee amputation (4%) and 1 requiring admission to a nursing home (4%), and 5 deaths (17%).
COVID-19 period
During the COVID-19 period, the total number of recorded patients seen by the service was 96, with 21 cases of CLI (22%). This comprised a total of 16 referrals recorded on the electronic referral database with 3 patients seen with a diagnosis of CLI (21%). A total of 66 patients were seen in the ‘hot clinic’, with 18 cases of CLI (27%). An additional 14 patients were contacted in a telephone clinic, with 0 cases of CLI. The mean age was 70 years (SD 12) and 62% were male. The median LOS for patients in this period was 0 days (IQR 0–5). This was significantly lower than the non-COVID LOS (p<0.001).
The median time from referral to specialist review was 3 days (IQR 1–7) (p<0.001). The median time from specialist review to imaging was 0 days (IQR 0–2). Six of these patients had a documented MDT discussion (29%). The median time to intervention was 8 days (IQR 2–15). The management strategy for these patients was open surgery for 5 (24%), endovascular intervention for 2 (10%) and conservative management for 14 (67%). Outcomes at 30 days were 16 patients alive (76%), with three below-knee amputations in this group (14%), and 2 deaths (10%). There was little evidence of a difference in management strategy (p=0.3) or 30 day outcome (p=0.1) between the non-COVID and the COVID-19 group.
Discussion
The COVID-19 pandemic enforced significant changes in the way healthcare services were delivered in the UK. The focus on increasing intensive therapy unit (ITU) capacity and limiting exposure of patients and clinicians to COVID-19 meant that traditional models of routine elective surgical capacity and outpatient clinics were suspended indefinitely. The ensuing service innovation proceeded at a pace not previously seen in the NHS. The Royal Devon and Exeter Hospital established a consultant-led urgent ‘hot clinic’ four times per week where patients could be seen with relevant investigations and interventions organised on an ambulatory basis, rather than a traditional pathway of admission via the acute route, being taken into an inpatient bed to await review and subsequent management. This type of service has not previously existed in the region and has not been evaluated.
The results of this study show a significant reduction in LOS for patients with CLI during the COVID-19 period compared with the equivalent non-COVID period. The median time from referral to vascular review was significantly higher in the COVID-19 period compared with the non-COVID period. There was no significant change in time to imaging or time to intervention. A greater number of patients had a documented formal MDT discussion during the COVID-19 period than during the non-COVID period. Finally, there were no significant differences in the way patients were managed (conservative, endovascular, or open surgery) between each period and no significant differences in outcomes.
The overall findings of this study show that patients with CLI were managed safely and effectively through a ‘hot clinic’ in an ambulatory fashion and that those requiring admission for a revascularisation procedure had a shorter overall inpatient LOS. In this population, there was no delay in vascular imaging, and in fact two patients had undergone imaging with duplex ultrasound prior to their consultant review in the ‘hot clinic’. Similarly, there was no significant delay to intervention and a greater number of patients had their treatment led by a documented MDT discussion. This supports the idea of managing patients on an ambulatory basis.
Our change in Vascular Surgery service provision in response to COVID-19 to focus predominantly on urgent and emergency cases is reflected in international practice.5,6 The delivery of Emergency General Surgery has already undergone review and a restructured model of consultant-led triage and ambulatory clinical assessment is increasingly established with positive patient outcomes7–10 and improved financial efficiency.11 The same changes have not been made generally in Vascular Surgery although ambulatory endovascular strategies for CLI have been shown to be feasible,12,13 and one recent study examining the ‘hot clinic’ for CLI has shown comparable outcomes in treating CLI and significantly shorter LOS compared with emergency admission.14 These findings are corroborated by the results of our study.
There is evidence to suggest COVID-19 induces a hypercoaguable state,15 which is associated with disease severity and poor outcomes,16,17 although the clinical manifestation of this and its effects on existing vascular disease is poorly understood. A more global overview of the changes to Vascular Surgery services in response to COVID-19 is currently being undertaken.18
The Vascular Society of Great Britain and Ireland guidance on best practice for management of peripheral arterial disease recognises inconsistencies across the UK in the delivery of revascularisation services in terms of LOS, service provision and outcomes.3 The recommendations of this guidance are aligned with the Getting It Right First Time report for Vascular Surgery,19 and acknowledge that the standards set out are deliberately challenging and will require restructuring of services so that vascular networks develop processes to deliver urgent care. The restructuring of services at this centre during COVID-19 and the results of this study support this type of change as effective in providing safe and expedient care within the national time targets set out by the Vascular Society.3
It is worth commenting on the difference in time from referral to specialist vascular review (median non-COVID vs COVID-19 0 vs 3 days). This reflects the fact that, during the non-COVID period, the referrals recorded were seen via the acute surgical intake and reviewed by a senior vascular clinician on the same or the following day.
During the COVID-19 period, patients seen in the ‘hot clinic' were often referred from the community and booked into the next available clinic slot after discussion with a consultant vascular surgeon. The finite capacity of clinic slots explains the observed increase in time to specialist review. However, it should also be noted that the increase from 0 to 3 days is not clinically significant, and is within the 7 day target laid out in the best practice guidance.3 Similarly there was an increase in time from referral to intervention during the COVID-19 period of from 6 to 8 days. This is not clinically significant and is well within the 14-day target in best practice guidance.3
We acknowledge the limitations of this study as a retrospective review with small sample size. However, we have examined a common pathology seen by any UK Vascular Surgery service and assessed this against national guidance, making these findings generalisable. Further work should include re-evaluating this in a prospective manner at a future interval.
Conclusion
This study aimed to examine the effect of COVID-19 on the provision of service for CLI. The results show that by implementing a consultant-led ‘hot clinic’ and a focus on ambulatory service, patients can be managed safely in a timely manner according to established best practice with significant reduction in hospital LOS.
Funding
SB is supported by the National Institute for Health Research Applied Research Collaboration South West Peninsula. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
References
- 1.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020; 395: 1225–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Royal College of Surgeons of England. Guidance for surgeons working during the COVID-19 pandemic. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/(cited October 2022).
- 3.Vascular Society . https://www.vascularsociety.org.uk/_userfiles/pages/files/Newsletters/PAD%20QIF%20April%202019(1).pdf (cited October 2022).
- 4.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.r-project.org/ (cited October 2022). [Google Scholar]
- 5.Latz CA, Boitano LT, Png CYMet al. Early vascular surgery response to the COVID-19 pandemic: results of a nationwide survey. J Vasc Surg 2021; 73: 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valdivia AR, Sanus EA, Santos ÁDet al. Adapting vascular surgery practice to the current COVID-19 era at a tertiary academic center in Madrid. Ann Vasc Surg 2020; 67: 1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Navarro AP, Hardy EJ, Oakley Bet al. The front-line general surgery consultant as a new model of emergency care. Ann R Coll Surg Engl 2017; 99: 550–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Macano CA, Kirby GC, Lake Bet al. Surgical assessment clinic – One stop emergency out-patient clinic for rapid assessment, reduced admissions and improved acute surgical service: a quality improvement study. Ann Med Surg 2017; 23: 28–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnstone C, Harwood R, Gilliam Aet al. A clinical decisions unit improves emergency general surgery care delivery. Clin Gov 2015; 20: 191–198. [Google Scholar]
- 10.Kazem MA, Hopley C, Corless DJ. Reducing emergency admissions and length of stay by introducing emergency surgical ambulatory service. Ann Med Surg 2019; 43: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panagiotopoulou IG, Bennett JM, Tweedle EMet al. Enhancing the emergency general surgical service: an example of the aggregation of marginal gains. Ann R Coll Surg Engl 2019; 101: 479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hauguel A, Maurel B, Bague Net al. Management of ambulatory (day case) endovascular procedures for peripheral arterial disease. J Cardiovasc Surg (Torino) 2017; 58: 293–304. [DOI] [PubMed] [Google Scholar]
- 13.Maurel B, Paumier A, Jacobi Det al. Ambulatory percutaneous angioplasty in patients with claudication. Ann Vasc Surg 2011; 25: 191–196. [DOI] [PubMed] [Google Scholar]
- 14.Khan A, Hughes M, Ting Met al. A ‘hot clinic’ for cold limbs: the benefit of urgent clinics for patients with critical limb ischaemia. Ann R Coll Surg Engl 2020; 102: 412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Xiao M, Zhang Set al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020; 382: e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F, Yu T, Du Ret al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang N, Li D, Wang Xet al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020; 18: 844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.UK Vascular and endovascular research network. Cover study: COVID-19 vascular service study. http://vascular-research.net/projects/cover-study-covid-19-vascular-service-study/ (cited October 2022). [DOI] [PMC free article] [PubMed]
- 19.Getting It Right First Time. https://gettingitrightfirsttime.co.uk/wp-content/uploads/2018/02/GIRFT_Vascular_Surgery_Report-March_2018.pdf (cited October 2022).