Abstract
We report a rare complication involving a healthy 45-year-old male patient who underwent an emergency laparoscopic appendicectomy for acute perforated gangrenous appendicitis. The patient was catheterised pre- procedure and the ports were inserted under vision. Upon completion of the procedure, a 15 Fr Robinson drain was left in the pelvis and was fed through the suprapubic port hole. Postoperatively the patient developed worsening, generalised abdominal pain and high output from the drain. The patient was re-catheterised but the computed tomography (CT) cystogram did not show any injury to the bladder. The drain fluid creatinine was noted to be raised (>4,000), indicating that urine was leaking into the drain. Conventional cystogram confirmed a contrast leak from the dome around the drain. Flexible cystoscopy confirmed that the drain had transversed the vesicourachal diverticula. The drain was pulled back and converted to a suprapubic catheter with the patient subsequently being discharged. Vesicourachal diverticula is a rare and often asymptomatic anomaly. When undertaking laparoscopic surgery, precautions should be taken to prevent port site injury such as catheterising the patient to ensure the bladder is empty and inserting the ports under direct vision. It is safer to visualise muscle rather than peritoneum during port insertion. In this case, the bladder diverticula was noticed extraperitoneally. Though the indirect CT cystogram reported no injury, this was unreliable as the bladder was not distended which led to the subtle injury being missed. Traditional cystogram should be considered in cases with a negative CT cystogram and a strong suspicion of bladder injury.
Keywords: Vesicourachal diverticulum, Laparoscopic appendectomy, Bladder injury, Urachus, Cystogram
Introduction
The urachus is an embryological remnant of the allantois, a channel that is present before birth that runs from the bladder to the umbilicus, where urine drains. It usually closes around the 12th week of gestation and leaves behind a small fibrous cord named the median umbilical ligament.1 The urachus has no purpose after birth, therefore a patent urachus following delivery is an abnormality of fetal development. One such abnormality is a vesicourachal diverticulum, in which the urachus fails to close leading to a blind-ending tract. This is often asymptomatic or can present with a urinary tract infection. Vesicourachal diverticula account for roughly 5% of all urachal abnormalities.2
Minimally invasive procedures using laparoscopic techniques have revolutionised surgery by reducing postoperative pain, improving cosmesis, reducing inpatient stay and facilitating faster return to normal activity. However, there remain complications associated with laparoscopic surgery. Major vascular injury and bowel injuries, although uncommon, can be potentially life-threatening and usually occur during the initial access and insertion of ports.3 A study by Karthik et al4 found that of 570 patients undergoing a laparoscopic surgery, 17 (3%) developed complications related specifically to the port site, the most common being a port site infection (1.8%). Other complications include bleeding (0.7%) and port site metastasis (0.175%) following laparoscopic oncosurgery. Rarer complications included visceral injury and damage to blood vessels (0.14%),5 most commonly the left common iliac vein, the right common iliac artery and the left internal iliac artery. With regards to bladder injury, it is estimated to occur in 0.3%–0.5% of adult laparoscopic appendicectomies.6 The use of a suprapubic port is common in laparoscopic appendicectomies and is the most likely to cause a bladder injury.7
Case history
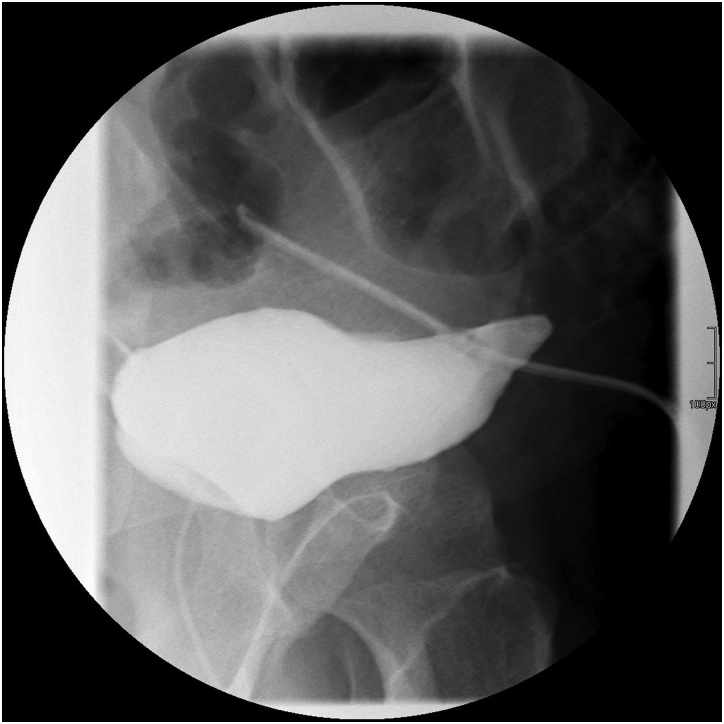
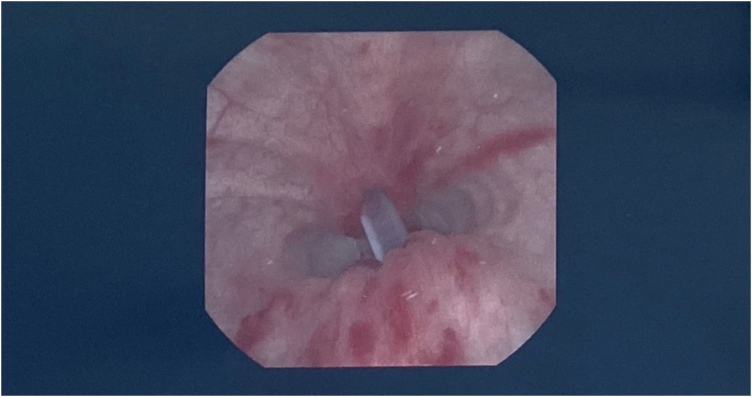
We report a rare complication involving a 45-year-old male patient, who was otherwise fit and healthy, who underwent an emergency laparoscopic appendicectomy for acute perforated gangrenous appendicitis. The patient was catheterised pre-procedure and the ports were inserted under vision. Following the procedure, a 15 Fr Robinson drain was left in the pelvis, which was fed through the suprapubic port hole. Postoperatively the patient developed worsening, generalised abdominal pain and high output from the drain. The patient was re-catheterised but the computed tomography (CT) cystogram did not show any injury to the bladder (Figure 1). The drain fluid creatinine was raised (>4,000), indicating that urine was leaking into the drain. Conventional cystogram confirmed a contrast leak from the dome around the drain (Figure 2). Flexible cystoscopy confirmed the drain had transversed the vesicourachal diverticula (Figure 3). The drain was pulled back and converted to a suprapubic catheter (SPC) with the patient subsequently being discharged.
Figure 1 .
The patient was re-catheterised but the computed tomography cystogram did not show any injury to the bladder
Figure 2 .
Conventional cystogram confirmed a contrast leak from the dome around the drain
Figure 3 .
Flexible cystoscopy confirmed the drain had transversed the vesicourachal diverticula
Discussion
During laparoscopic appendicectomies there are a few simple measures taken to prevent bladder injury. The first measure is to ensure that the patient has voided prior to induction of anaesthesia. Often, a catheter may be inserted to ensure the bladder remains empty intraoperatively with an in/out technique of catheterisation often being utilised safely.7
Another measure taken to prevent bladder injury during a laparoscopic appendicectomy is to insert the suprapubic port under direct vision, as extraperitoneal injuries are mostly caused during port placement. Bladder injuries may take a few days to present postoperatively, with symptoms including lower abdominal swelling, pain, oliguria, urinary leakage from wound sites and cystitis. In this case, there was an increased output from the abdominal drain left in the suprapubic port, which indicated that there may have been a bladder injury regardless of the fact the patient voided prior to the procedure and that the suprapubic port was inserted under direct vision. Small extraperitoneal injuries can be managed conservatively with catheterisation of the bladder along with broad-spectrum antibiotics. However, larger injuries with associated haematomas may require radiological drainage or exploration in theatre, with a washout and potential repair of the bladder needed if conservative management fails.8
Given the rarity of the case, the operating surgeons had to improvise when it came to management of the perforated bladder. In this situation, the patient was taken to theatre and given general anaesthetic. A flexible cystoscope was used to visualise the bladder, helping identify the drain traversing through the bladder. The drain was pulled back carefully, under direct visualisation, until the tip of the drain was in the bladder. A guidewire was then fed through the drain until it was inside the bladder and the drain was carefully removed. An SPC was railroaded into the bladder, over the guidewire through the suprapubic port hole. The guidewire was then removed, and the SPC balloon was hyperinflated with 20ml of saline to tamponade the other perforation in the bladder wall caused by the drain.
A repeat cystogram was carried out two weeks after discharge, showing no evidence of contrast extravasation from the bladder. The patient was then seen in the outpatient clinic where he underwent a successful trial without catheterisation, with a post void bladder scan showing only 57ml of residual volume. The SPC remained for another two weeks, and the patient was advised to leave the SPC clamped and to try to pass urine urethrally. Because he was able to pass urine urethrally with no difficulty, the SPC was removed. Following this, he had no urinary symptoms and the suprapubic wound healed well. This was a novel treatment approach for this rare complication. This complication was recognised in the immediate postoperative period and treatment was completed prior to discharge.
Conclusions
Vesicourachal diverticula is a rare and often asymptomatic anomaly. When undertaking laparoscopic surgery, precautions should be taken to prevent port site injury such as catheterising the patient to ensure the bladder is empty and inserting the ports under direct vision. It is safer to visualise muscle rather than peritoneum during port insertion. In this case the bladder diverticula was noticed extraperitoneally.
Although the indirect CT cystogram reported no injury, this was unreliable as the bladder was not distended, which led to the subtle injury being missed. Traditional cystogram should be considered in cases with a negative CT cystogram and a strong suspicion of bladder injury.
References
- 1.Cilento B, Bauer S, Retik Aet al. Urachal anomalies: defining the best diagnostic modality. Urology 1998; 52: 120–122. [DOI] [PubMed] [Google Scholar]
- 2.Schnyder P, Candardjis G. Vesicourachal diverticulum: CT diagnosis in two adults. Am. J. Roentgenol. 1981; 137: 1063–1065. [DOI] [PubMed] [Google Scholar]
- 3.Jansen F, Kapiteyn K, Trimbos-Kemper Tet al. Complications of laparoscopy. Obstet Gynecol Surv 1997; 52: 619–620. [DOI] [PubMed] [Google Scholar]
- 4.Augustine A, Pai M, Shibumon M, Karthik S. Analysis of laparoscopic port site complications: A descriptive study. J Minim Access Surg 2013; 9: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asfour V, Smythe E, Attia R. Vascular injury at laparoscopy: a guide to management. J Obstet Gynaecol 2018; 38: 598–606. [DOI] [PubMed] [Google Scholar]
- 6.Levy B, De Guara J, Willson Pet al. Bladder injuries in emergency/expedited laparoscopic surgery in the absence of previous surgery: a case series. Ann R Coll Surg Engl 2012; 94: e118–e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hotonu S, Gopal M. Bladder injury in a child during laparoscopic surgery. J Surg Case Rep 2019; 2019: rjz043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lad M, Duncan S, Patten D. Occult bladder injury after laparoscopic appendicectomy. Case Rep. 2013; 2013: bcr2013200430. [DOI] [PMC free article] [PubMed] [Google Scholar]