Abstract
Background:
Haemophilia and von Willebrand disease are the bleeding disorders most frequently encountered in the emergency department (ED), that are often the first point of contact for patients. Evidence suggests that management in the ED is currently suboptimal, mainly because the physicians have few opportunities to deal with this kind of patients.
Objectives:
We carried out a survey to investigate the management of patients with haemophilia A in Emergency Departments (EDs), and to understand the training needs of the involved physicians.
Methods:
Overall, in Piedmont Region there are 32 EDs, and considering that our survey was conducted on 21 physicians working in 23 Emergency Departments (EDs), this number is representative of the Region’s reality. The interviews were conducted through face-to-face meetings, including general aspects regarding the clinical characteristics and the management of patients, and self-evaluation of knowledge and interest in receiving information about the disease.
Results:
In 2019, 131 patients with haemophilia A were admitted (108 adults, 23 paediatric). The best-known and most widely available and used treatments were plasma derivatives, followed by first- and second-generation recombinant FVIII. More recent recombinant and bypassing agents were less known. Half of the interviewees considered their knowledge of bleeding disorders in general and haemophilia in particular to be “basic”, and only one third defined it as “good”; however, 86% expressed great interest in receiving information about the topic.
Conclusions:
The survey confirms the needs related to the clinical management of rare inherited clotting disorders in EDs. The physicians involved are keen to overcome this lack of knowledge, and proper initiatives should be implemented. (www.actabiomedica.it)
Keywords: haemophilia, emergency treatment, emergency doctors’ knowledge, emergency department care
Introduction
Despite being rare conditions, haemophilia and von Willebrand disease are the bleeding disorders most frequently encountered in the emergency department (ED) (1).
According to the 2018 National Registry on Congenital Coagulopathy, haemophilia A is the most common disease, with a total of 4,109 cases, followed by haemophilia B (882), von Willebrand disease (3,245) and by other clotting disorders (2,318) (2). In haemophilia A, the X-linked genetic defect causes a partial or total reduction in coagulation factor VIII activity and consequent hemorrhages: the clinical presentations can vary in severity, and can even be life-threatening (3-5). In the Piedmont region, 85 patients with severe haemophilia A were registered and included in the Istisan Report in 2019 (2). The actual overall number of patients is probably higher, if we include patients with less severe disease and that therefore are not included in the Therapeutic Plan.
For the severe forms, the clinical presentations of the disease can be present from birth and in any case from the early years of life; the more serious the disease, the earlier the symptoms are likely to occur, and they are usually observed when the child starts to move independently (3,4). Diagnosis and the consequent introduction of therapy must take place as early as possible, with infusions of factor VIII possibly before or at least soon after the first bleeding episode, in order to reduce joint bleeding and osteochondral damage and obtain better musculoskeletal outcomes (6-8).
When bleeding symptoms occur, emergency department physicians are often the first point of contact for patients, especially for those with mild disease. However, although the awareness of ED physicians regarding bleeding disorders is crucial, evidence suggests that management in the ED is currently suboptimal, mainly because these physicians have few opportunities to deal with this kind of patients (9-12).
This survey was carried out in 2019 to investigate the management of patients with haemophilia A in EDs in the Piedmont region, and to understand the training needs of the physicians involved.
The initiative was conducted in the EDs by exploring and quantifying patient flows, characterizing the management of hemophiliac patients, verifying the existence of internal protocols/guidelines for disease management and cooperation with Haemophilia Centers, focusing on the knowledge, availability and choice of therapeutic agents, and finally evaluating the physicians’ awareness of the disease and their willingness to improve their skills on the topic.
Methods
The survey was carried out between August and December 2019 in Piedmont. 23 Emergency Departments were involved, and 21 physicians (two of them each were working in two different units) were interviewed.
One specialist was interviewed at each ED. Physicians had to have been working in the ED for at least 2 years but no more than 25 years.
A 30-minute questionnaire was administered in face-to-face interviews.
The survey consisted of three sections (Figure 1). The first dealt with the general aspects of the management of patients with coagulation disorders, with a special focus on haemophilia A. In the second section, participants were invited to share the last 4 cases they had seen in the ED, and to provide details of the clinical characteristics and management of the patients. Lastly, in the third part, the physicians had to self-evaluate their awareness and knowledge of the disease, specifying their interest in receiving information and through what tool/initiatives.
Figure 1.
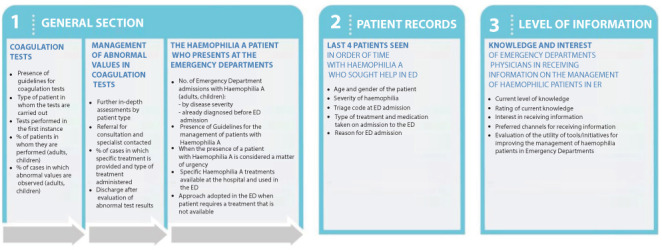
Structure of the three sections of the questionnaire
The general section regarded bleeding disorder management, and in particular investigated the presence of guidelines, the rate and types of patients undergoing coagulation tests, and the tests performed in first instance, physician choices in the case of abnormal test results (further in-depth investigations, referral for a specialist consultation), the type of treatment provided and the rate of administration. The following part focused on the profile of haemophilia A patients, and investigated, amongst other things, the number of adult or paediatric admissions with a previous or current diagnosis of haemophilia A, the existence of patient management guidelines, the proportion of patients considered medical emergencies, the percentages of referrals for a consultation at a specialized haemophilia center and/or with a hematologists, and finally the availability of specific treatments for haemophilia A.
Section two included questions about the last 4 hemophiliac patients whose clinical details the doctor was able to recall, recording their age and gender, reasons for admission to the ED, disease severity, and choice of treatment.
The third section focused on the level of awareness and knowledge regarding the management of hemophiliac patients, the physicians’ interest in receiving further information and the preferred channels/tools/initiatives for this purpose.
Results
Here we report the main data obtained by the survey.
Section 1: Characteristics of the sample and general section
The interviews were held in the EDs of a total of 23 facilities, and all the percentages reported refer to these 23 EDs. In 2 of the 23 units, the hospital had also a bleeding disorder center dedicated to haemophilia and coagulopathies (Figure 2).
Figure 2.
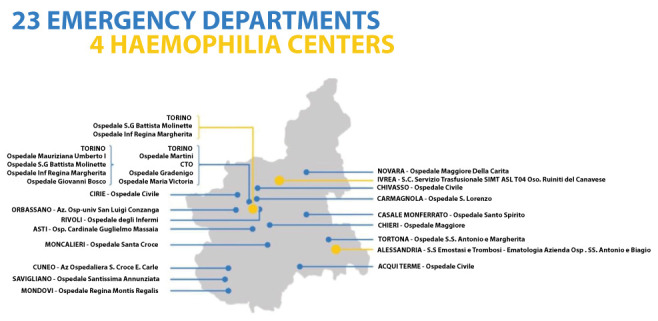
Geographic distribution of Emergency Departments involved in the survey and haemophilia centers in the Piedmont Region
Guidelines and/or protocols for first-level coagulation tests were present in 13 (55%) of the hospitals involved; in 23% of cases they were formalized and mandatory. Clotting tests were nevertheless assessed in 65% of adults and in 18% of paediatric patients: PT in 100% of cases, PTT/aPPT in 91%, and fibrinogen in 74%, whereas clotting factors were also analyzed in just 9% of cases. The diagnoses that urged the physicians to explore coagulation function were: known coagulopathy, thrombotic events, stroke, acute coronary syndrome, bleeding, actual or suspected hemarthrosis, surgical/traumatic emergency, and headache (in 87% of units). Abnormal values were detected in 18% of adults and 6% of children. In cases where abnormal values were observed (especially PT/aPTT), 74% of Emergency Departments carried out further in-depth analyses, and in 75% of these cases coagulation factors were also analyzed; the vast majority (87%) of physicians who conducted a more in-depth diagnostic work-up referred the patient for a consultation with a specialist, in most cases, a hematologist for adults and a pediatrician for children (at the same or another hospital).
The specific treatments administered to manage the bleeding disorders are shown in figure 3. The most commonly prescribed treatment was fresh frozen plasma (administered in 27% of adult cases and 19% of paediatric patients), followed by recombinant factor concentrates; however, factor concentrates combined (plasma-derived and recombinant) were administered in 41% of adults and 31% of paediatric patients, when a firm diagnosis had already been defined.
Figure 3.
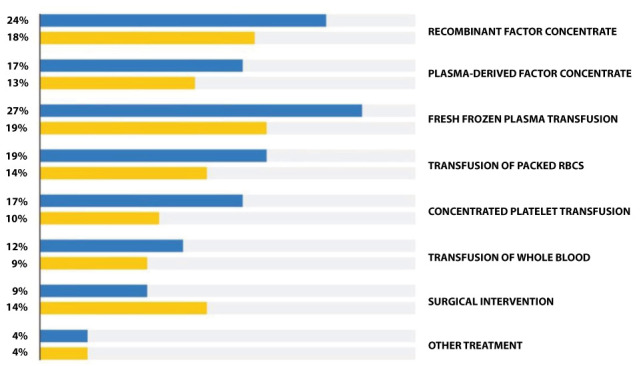
Treatments administered to manage clotting disorders. Some patient may receive more than one treatment. Blue = adult patients; Yellow = paediatric patients
Focus on Haemophilia A
In 2019, 131 patients with haemophilia A were admitted in 14 Emergency Departments, 108 adults and 23 paediatric patients.
Disease severity was mild in 42% of adults and 45% of children, moderate in 22% and 35%, and severe in 36% and 20%, respectively. All paediatric patients had already been diagnosed with haemophilia A, and just 5% of adults were diagnosed during or after admission to the ED.
During the triage phase, when a patient diagnosed with haemophilia A was admitted to one of the 23 EDs, a haemophilia center was contacted in 67% of cases for adult patients and in 57% of cases for children. In 52% of EDs, haemophilia was not considered a matter of urgency per se, unless it resulted in an emergency situation (actual or suspected bleeding). In 39% of cases, the disease was always considered a matter of urgency.
Another group of questions concerned the physicians’ knowledge of haemophilia treatments, their availability at the hospital and their use in the ED. The results clearly show that, as expected, plasma derivatives were the best known (74%), the most widely available (57%) and the most commonly used preparations (52%). Plasma derivatives were followed by the older recombinant factors (first- and second-generation agents). The less well-known and less commonly used preparations were those that were recently placed on the market (third- and fourth- generation agents) and bypassing agents.
More than a half the patients admitted to the 23 EDs received plasma derivatives, and the others received recombinant factor VIII. Other drugs used in the EDs were desmopressin (17%) and bypassing agents (4%), so some patients received more than one treatment.
64% of patients reported to the ED taking their normal medication, which was usually, but not always, administered (89% of cases) (Figure 4A). When a specific haemophilia treatment was not available at the Department, 43% of physicians contacted another hospital that provided the drug, 7% used another medicinal product, and 50% of centres never needed to (Figure 4B).
Figure 4.
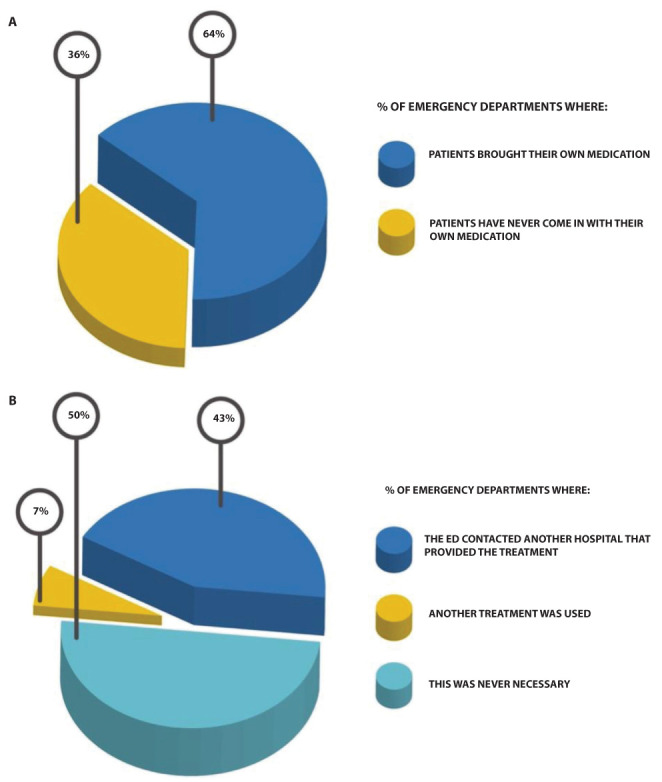
A) Percentage of EDs to which patients took their usual medication; B) Approach adopted by ED physicians when FVIII was not available at the department
Section 2: Hemophiliac patient records
In this part of the interview, each physician was asked to provide the anonymized records of the last 4 patients with haemophilia A he/she had seen in the ED, regardless of all other characteristics, e.g. type of urgency, whether they had already been diagnosed or were diagnosed during or following admission to the Emergency Departments. 13 records regarded other coagulopathies. As we had decided to focus on haemophilia A, just 12 records, all relating to male patients, were included in the analysis.
Patients reported to the ED for headache in 50% of cases, hemarthrosis in 25%, and other causes in 25% of cases (Fig. 5A). The tests carried out at admission to the ED are reported in figure 5B. All of the patients had already been diagnosed with haemophilia, and were on as needed treatment in 75% of cases, and prophylactic treatment in the remaining 25%. Disease was severe (FVIII <1%) in 17% of patients, moderate (FVIII 1-5%) in 33% and mild (FVIII 5-40%) in 50%.
Figure 5.
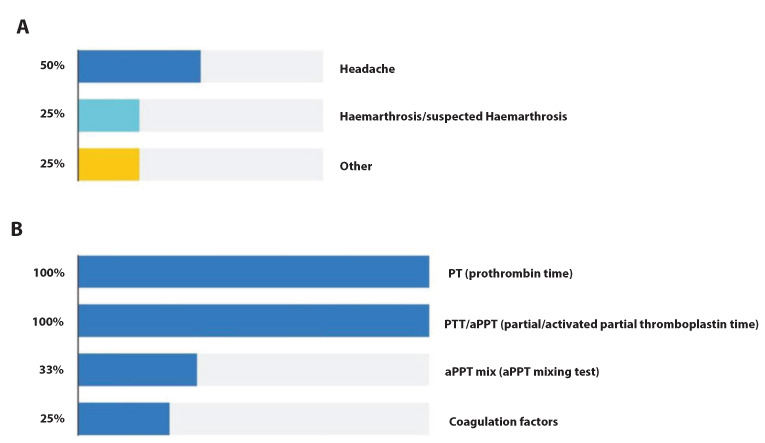
A) Reasons for admission to the ED; B) Coagulation tests carried out at admission to the Emergency Department
In 67% of cases a hematologist working at the same hospital was consulted. Haemophilia centers were contacted in 34% of cases (the center that usually treated the patient in 17% of them). No ED contacted a hematologist at another hospital.
During hospitalization in the ED, 10 patients received a specific treatment (plasma derivatives in the case of 5 patients, and two different octocog alfa preparations for a further 5 patients, all dispended by the hospital pharmacy), whereas 2 patients did not receive any treatment and underwent an observation period.
75% of patients were discharged directly from the ED, 17% needed a longer observation period, and in a minority of cases (8%) the patients required hospitalization in another department.
Section 3: Level of information and physicians’ educational needs
One of the main aims of the survey was to evaluate the physicians’ awareness and knowledge of the disease, as well as their desire to obtain more information.
52% of the physicians interviewed had never received any specific training in the management of hemophiliac patients in the ED. Half of them considered their knowledge of bleeding disorders and haemophilia in particular to be “basic”, and just one third rated it to be “good”. None of them considered it to be “Excellent” (Figure 6).
Figure 6.

Self-evaluation of knowledge of coagulopathy management by interviewed physicians.
However, 86% of participants showed a significant interest in receiving information on the management of severe hemorrhage in hemophiliac patients. When asked about the preferred tools/opportunities, most chose:
dedicated sessions during congresses or conferences
small workshops at the hospital or at the bleeding disorder hub center
on-line learning
Lastly, guidelines or at least hospital protocols and a regional integrated care pathway (Percorso diagnostico-terapeutico-assistenziale, PDTA) for the management of hemophiliac patients were identified as key needs.
Discussion
The survey highlighted the complexities of the management of patients with bleeding disorders and showed that, in some cases, even the proper identification of hemophiliac patients in the ED is a challenge. 26% of EDs only carry out first-instance tests (predominantly PT/PTT), which are not sufficient for a detailed diagnosis and adequate therapy. Moreover, certain practical problems, such as long test turnaround times, further complicate the situation. The number of admissions of hemophiliac patients is very low compared to other diagnoses, meaning that ED physicians do not have the opportunity to develop adequate experience of this disease.
In our experience, patients admitted to the emergency department have mild-moderate disease requiring on demand therapy, rather than patients with severe forms requiring chronic treatment. The mild forms, especially in the paediatric age, may not have already been diagnosed at the time of admission to the ED, or patients may not be used to reporting their condition (1,9).
A recent article has reported a survey conducted on 128 HCPs in USA and 98 in Germany working in in hemophilia non-specialized centers, regarding the barriers that hinder the timely treatment of haemophilia patients (13). Most of the HCPs involved in the urgent treatment of bleeding in haemophilia patients were EDs specialists (38%) in the USA and anesthesiologists (32%) and hematologists (30%) in Germany. The physician reported that they managed an average of five-six patients with haemophilia and inhibitors per year (13). Guidelines for the treatment of these patients were available in 26% of the centers in the USA and in 28% of the German ones.
The participants (especially those in EDs) agreed that a faster diagnosis, due to a better education/knowledge, would improve the outcomes of bleeds in patients with haemophilia and inhibitors (13).
Similarly to the USA-Germany report also in our experience the lack of guidelines and management protocols is indicated as one of the more crucial factors that does not facilitate the adoption of a consistent and shared clinical approach.
Barriers to fast treatment of bleeds in patients with haemophilia and inhibitors were identified in the lack of national or regional network of hemophilia treatment centers (HTCs) in the United States and Germany. These could be reduced by improving the availability of treatment guidelines, bypassing agents and HCP education/training.
As regards haemophilia A, many patients may receive complete coagulation test results (including FVIII and FIX) late and consequently may not receive a timely and proper treatment approach. In some cases, patient recognition may be impacted: indeed, the survey also included female patients, possibly due to a lack of knowledge regarding other rare coagulopathies (i.e. von Willebrand syndrome) (14).
It is also important to note that a very low number of EDs (just two out of twenty-three) were able to refer patients directly to a bleeding disorders center at the same hospital, which may have had an impact in timely and correct patient assessment, resulting in delayed diagnosis and, consequently, late treatment. In the de Moerloose survey, the referral to a specialized center occurred in 28% (USA) and 47% (Germany) of cases, but more often than in our records the patient is managed by a hematologist from the beginning (13).
In both surveys, however, it appears clear that ED physicians require better training on the management of patients with coagulopathies, including the formulation of a protocol for suspected or actual bleeding, indications of the tests to be administered, and confirmation of the diagnosis. Our case study, although very smaller than the de Moerloose casuistry, shows that the barriers to a timely and proper management of hemophilic patients are very similar.
These data confirm the importance of and the need for a higher level of awareness and knowledge amongst ED healthcare professionals, as well as a better-coordinated interaction between EDs and hematology specialists (15).
The interviews show that half of the physicians interviewed had not received specific training on these diseases, and rate their knowledge as “basic”; however, 86% of them stated they would be very interested to receive information on the topic. Lastly, the availability of formal guidelines or protocols emerged as a major need. However, our survey showed that, although not familiar with the disease, the majority of ED doctors was able to refer the patient to the most appropriate specialists and often to treat the patient early.
In 2001, Minhas et al. highlighted the importance of early identification of the disease, and in their study reported the age of the diagnosis to be 29.5 months (16). In recent years, the situation has improved, and other Authors have reported a far earlier median age of 7.7 months, with a wide range that varied in accordance with disease severity and family history (17). The need for better knowledge and awareness has also been highlighted by other Authors (18,19). Reasons for the delay in diagnosis include the fact that few clinicians have direct clinical experience of this condition and of coagulation disorders in general (9,16,20). Nevertheless, early recognition is key to avoiding unnecessary investigations and establishing correct treatment. The administration of FVIII to patients with haemophilia A reduces severe bleeding and is crucial, especially in young patients and children, for avoiding severe late complications (6, 10,12,15).
One interesting Italian study was conducted in 2010, involving eight haemophilia centers and 44 EDs in the Emilia-Romagna region, aimed at improving emergency care for patients with inherited bleeding disorders (PWIBD). The project included an educational program for ED staff and a dedicated website providing extensive information, proposing treatments, and sharing data from patients’ electronic clinical records (11).
The limit of our survey is that it is not a systematic extraction of data from patient records, rather interviewees were asked to recall the most recently visited patients. Nevertheless, in our opinion this paper may provide the rationale for implementing more structured and larger scale studies, and without a doubt highlights the need and possibility to organize professional development initiatives.
Conclusions
It can be concluded that this survey confirms the literature data regarding the considerable needs associated with the clinical management of inherited coagulopathies in EDs, which, nevertheless, remain crucial hubs for healthcare. There is a significant interest and willingness by the physicians involved to overcome their lack of knowledge, and appropriate initiatives could be implemented with a good chance of success.
Acknoledgements:
The Authors thanks IQVIATM that has carried out the present survey through face-to-face interviews to EDs physicians and performed all the statistical data analyses. The authors thanks also Maria Carla Marrè Brunenghi for editorial assistance. Special thanks go to the participating centers, listed below: Azienda Ospedaliera/Universitaria S. Luigi Gonzaga – Orbassano; Ospedale Mauriziano Umberto I – Torino; Ospedale Cardinale G. Massaia – Asti; Ospedale Civile – Ciriè; Ospedale Santissima Annunziata – Savigliano; Ospedale degli Infermi – Rivoli; Ospedale Civile – Chivasso; Ospedale S. G. Battista/Molinette – Torino; Ospedale Regina Montis Regalis – Mondovì; Ospedale Regina Margherita – Torino; Az. Ospedaliera S. Croce e Carle – Cuneo; Ospedale S. Giovanni Bosco- Torino; Ospedale Martini – Torino; Ospedale SS Antonio e Margherita – Tortona; Ospedale S. Spirito – Casale Monferrato; Ospedale Civile – Acqui Terme; CTO – Torino; Ospedale Maggiore della Carità – Novara; Ospedale Santa Croce – Moncalieri; Ospedale S. Lorenzo – Carmagnola; Ospedale Maggiore – Chieri; Ospedale Gradenigo – Torino; Ospedale Maria Vittoria - Torino
Statement of ethics:
This survey is comply with the guidelines for human studies and was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. IQVIA carried out this non-interventional retrospective survey, without collecting any sensitive data on patients, as such it was not necessary to obtain the consent of the Intercompany Ethics Committee A.O.U. City of Health and Science of Turin.
Funding:
The survey and the medical writing assistance service were sponsored by CSL Behring, Italy, which did not influence the results output/intervene in the definition of the results.
Conflict of interest:
AB received honoraria for speaker’s bureau and/or participation in Advisory Boards from Bayer, CSL Behring, Kedrion, Novo Nordisk, Roche, Sobi, Takeda. BP, IR, CD, FV, AV, CL declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Author contributions:
AB BP, IR, CD, FV, AV and CL contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
References
- Schwartz KR, Rubinstein M. Haemophilia And Von Willebrand Disease In Children: Emergency Department Evaluation And Management. Pediatr Emerg Med Pract. 2015;12:1–20. quiz 20–1. [PubMed] [Google Scholar]
- Abbonizio F, Biffoni R, Arcieri R, Giampaolo A Associazione Italiana Centri Emofilia (AICE) Istituto Superiore di Sanità - Registro Nazionale Coagulopatie Congenite. Rapporti ISTISAN 20/14. Rapporto 2019. 2021:iii, 53. [Google Scholar]
- CDC. Data & Statistics on Haemophilia (04.05.2022) https://www.cdc.gov/ncbddd/hemophilia/data.html#:~:text=In%20the%20United%20States%2C%20most,for%20those%20with%20severe%20hemophilia. [Google Scholar]
- National Haemophilia Foundation. Bleeding Disorders (22.02.2022) https://www.hemophilia.org/bleeding-disorders-a-z. [Google Scholar]
- Zimmerman B, Valentino LA. Haemophilia: in review. Pediatr Rev. 2013;34:289–94. doi: 10.1542/pir.34-7-289. [DOI] [PubMed] [Google Scholar]
- Dunn AL. Management and prevention of recurrent hemarthrosis in patients with haemophilia. Curr Opin Hematol. 2005;12:390–4. doi: 10.1097/01.moh.0000169285.66841.c8. [DOI] [PubMed] [Google Scholar]
- Page D. Comprehensive care for haemophilia and other inherited bleeding disorders. Transfus Apher Sci. 2019;58(5):565–8. doi: 10.1016/j.transci.2019.08.005. [DOI] [PubMed] [Google Scholar]
- Srivastava A, Santagostino E, Dougall A, et al. WFH Guidelines for the Management of Hemophilia. Haemophilia. (3rd edition) 2020;26(Suppl 6):1–158. doi: 10.1111/hae.14046. [DOI] [PubMed] [Google Scholar]
- Singleton T, Kruse-Jarres R, Leissinger C. Emergency department care for patients with haemophilia and von Willebrand disease. J Emerg Med. 2010;39:158–65. doi: 10.1016/j.jemermed.2007.12.024. [DOI] [PubMed] [Google Scholar]
- Zakieh A, Siddiqu AH. Emergency department utilization by haemophilia patients in United States Haemophilia. 2017;23:e188–e193. doi: 10.1111/hae.13187. [DOI] [PubMed] [Google Scholar]
- Tagliaferri A, Di Perna C, Biasoli C, et al. A Web Site to Improve Management of Patients with Inherited Bleeding Disorders in the Emergency Department: Results at 2 Years. Semin Thromb Hemost. 2016;42:589–98. doi: 10.1055/s-0036-1571312. [DOI] [PubMed] [Google Scholar]
- Lee A. Emergency management of patients with bleeding disorders: Practical points for the emergency physician. Transfus Apher Sci. 2019;58:553–62. doi: 10.1016/j.transci.2019.08.003. [DOI] [PubMed] [Google Scholar]
- Philippe de Moerloose P, Davis JA, El Fegoun SB, Habis R, Klamroth R. Barriers and challenges for the fast treatment of bleeds in the non-haemophilia treatment centre hospital setting. Haemophilia. 2020;00:1–9. doi: 10.1111/hae.13956. [DOI] [PubMed] [Google Scholar]
- Livesey K, Yealy DM, Li J, Moore CG, Ragni MV. Von Willebrand disease in the emergency department. Haemophilia. 2016;22:263–7. doi: 10.1111/hae.12841. [DOI] [PubMed] [Google Scholar]
- Tebo C, Gibson C, Mazer-Amirshahi M. Haemophilia and von Willebrand disease: a review of emergency department management. J Emerg Med. 2020;58:756–66. doi: 10.1016/j.jemermed.2020.02.019. [DOI] [PubMed] [Google Scholar]
- Minhas HL, Giangrande PL. Presentation of severe haemophilia—A role for accident and emergency doctors? Emerg Med J. 2001;18:246–9. doi: 10.1136/emj.18.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambost H, Gaboulaud V, Coatmélec B. What factors influence the age at diagnosis of haemophilia? Results of the French haemophilia cohort. J Pediatr. 2002;141:548–52. doi: 10.1067/mpd.2002.128115. [DOI] [PubMed] [Google Scholar]
- Mantik FJ, Gunawan S, Wowiling S. Knowledge about haemophilia among teachers of patients with haemophilia in Indonesia. Pediatr Hematol Oncol J. 2020;5:126–9. [Google Scholar]
- Peyvandi F, Lillicrap D, Mahlangu J, et al. Haemophilia gene therapy knowledge and perception: results of an international survey. Res Pract. Thromb Haemost. 2020;4:644–51. doi: 10.1002/rth2.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhajri H, Darwish M, Richhariya D, Almemari A. Approach to Patients with Bleeding Disorders in the Emergency Department. EC Emer Med Criti Care 3.1. 2019:20–8. [Google Scholar]


