Abstract
Background and aim:
Hallux rigidus represent a surgical challenge, with a multitude of possible surgical options, but with no ideal procedures. The propose of this paper was to review the actual knowledge on the operative techniques, paying particular attention to the evolution of interposition arthroplasties, as an alternative to arthrodesis and prosthesis in the advanced stages of the disease.
Methods:
A comprehensive literature PubMed search was performed, and the actual literature regarding hallux rigidus was overviewed. The operative and nonoperative options for HR were described. Studies on interposition arthroplasty were classified by publication year, summarizing the operative technique, results and complications.
Results:
Among the various techniques for interposition arthroplasty, the Modified Oblique Keller Interposition Arthtoplasty (MOKCIA) showed the lower complication rate. It does not sacrifice the insertion of the flexor halluces brevis, maintaining the stability, length and strength of the big toe.
Conclusions:
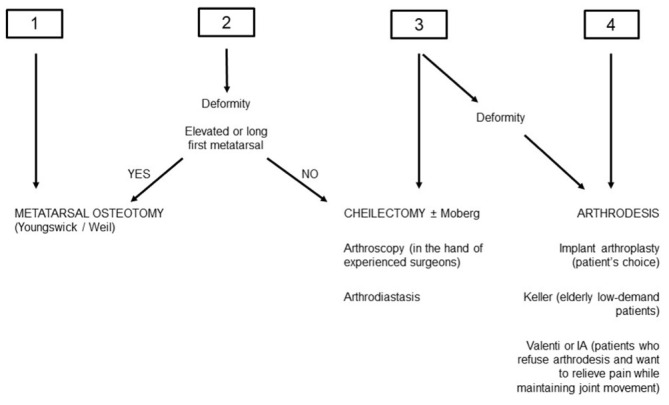
Although long-term randomized controlled trials are lacking for interposition arthroplasties, the reported results are comparable to the other alternatives for the treatment of end-stage hallux rigidus, making this technique a valid alternative also in the young active patient, without precluding other end-stage procedures in case of failure. Based on the current knowledge, a treatment algorithm was developed, according to the Coughlin classification. (www.actabiomedica.it)
Keywords: hallux rigidus, interposition, arthroplasty, treatment, algorithm
Introduction
Hallux rigidus (HR) is a common pathologic condition affecting the first metatarsophalangeal joint (FMTPJ), second in incidence only to hallux valgus, affecting 1 in 40 people over the age of 60 (1). Degenerative arthritis of the FMTPJ was initially reported by Davies-Colley in 1887 (2), although Cotterill first proposed the term hallux rigidus (3).
Hallux rigidus is defined as a painful and stiff arthritic joint, whereas hallux limitus is defined as functional pain and stiffness due to plantar fascia and flexor hallucis longus tendon (FHL) tightness, eventually associated with a long and elevated first metatarsal. Hallux limitus may progress to hallux rigidus, thus there may be overlapping of the two conditions (4).
In 1988 Hattrup and Johnson published the most common classification system used in the orthopedic literature (Table 1), based on radiographic findings (5). Lately Coughlin and Shurnas introduced a new classification method, including radiographic and clinical information (Table 2) (6).
Table 1.
1988 Hattrup and Johnson classification
| I | Preservation of joint space Mild osteophyte formation |
| II | Less than 50% joint space narrowing Moderate osteophyte formation Subchondral sclerosis |
| III | More than 50% loss of joint space Marked osteophyte formation ± subchondral cyst formation and loose bodies |
Table 2.
2003 Coughlin and Shurnas classification
| Grade | Dorsiflexion | X-rays | Clinical findings |
|---|---|---|---|
| 0 | 40-60° | Normal | No pain Only moderate stiffness |
| 1 | 30-40° | Dorsal osteophyte Minimal joint space narrowing Minimal periarticular sclerosis, minimal flattening of metatarsal head |
Mild intermittent pain evoked at maximum degrees of ROM Mild stiffness |
| 2 | 10-30° | Dorsal, lateral, and possibly medial osteophytes giving flattened appearance to metatarsal head No more than ¼ if dorsal joint space involved on lateral radiograph, mild-to-moderate joint-space narrowing and sclerosis, sesamoids not usually involved |
Moderate-to-severe pain and stiffness that may be constant Pain occurs just before maximum dorsiflexion and maximum plantar flexion on examination |
| 3 | < 10° | Same as in grade 2 but with substantial narrowing, possibly periarticular cystic changes, more than ¼ of dorsal joint space involved on lateral radiograph, sesamoids enlarged and/or cystic and/or irregular | Nearly constant pain and substantial stiffness at extremes of range of motion but not at mid-range |
| 4 | < 10° | Same as grade 3 | Same criteria as grade 3 but there is definite pain at mid-range of passive motion |
A review of 18 HR classification systems reported in literature found no reliability and scientific validity in most of the classifications. The authors concluded that the system proposed by Coughlin and Shurnas most closely approximates the gold standard (7).
The etiology of HR is not well understood, albeit demographic studies attempted to correlate with its incidence. A familiar history was present in about 66% of patients. Patients with a familiar history had bilateral involvement in 95% of cases. Unilateral cases were instead associated with a history of trauma in 78% of cases. Female sex represented 62-69% of cases. There was no clear correlation with flat foot, Achilles tendon contracture, hallux valgus, metatarsus adductus, long first metatarsal, first ray hypermobility, shoe wear or occupation. HR was associated with hallux valgus interphalangeus, but it was hypothesized that as the FMTPJ becomes more resistant to transverse plane deformity, this predisposes to hallux valgus interphalangeus as a consequence (8). DuVries hypothesized that a round or oval joint was less stable and thus more prone to hallux valgus, while a flat or chevron-shaped joint was more stable and prone to hallux rigidus (9).
Development of degenerative changes can also be secondary to repetitive stress or inflammatory or metabolic conditions such as gout, rheumatoid arthritis and seronegative arthropathies (10). Osteochondritis dissecans was also described as a possible cause (11).
Lambrinudi theorized that an elevated first metatarsal leads to excessive plantarflexion of the phalanx resulting in a flexion contracture of the joint (12). This hypothesis was confirmed by more recent studies, but reporting that the elevation of the first metatarsal has to be considered more as a consequence than a cause of HR, and more common in its final stages (8,13).
The mean age at onset of symptoms is 43 years (8). The classical finding is represented by the restricted and painful range of motion (ROM), particularly dorsiflexion. As the disease progresses, dorsal osteophytes may form, causing conflict with the shoe. High heels are usually not tolerated. Patients may complain about numbness along the medial border of the great toe as the osteophytes can compress on the dorsomedial cutaneous nerve. Bursitis or skin ulcerations can be found. Patients with HR may present gait pattern alterations, walking on the lateral aspect of the foot, attempting to reduce load on the FMTPJ (14).
As the disease progresses it is possible to observe a plantarflexion of the proximal phalanx with painful interphalangeal joint hyperextension as compensation of restricted FMTPJ dorsiflexion. Pain at the first metatarsal-cuneiform joint may also occur as a compensation of the restricted FMTPJ movement (15).
In milder forms of HR, pain usually occurs near the end of dorsiflexion, while midrange pain indicates more severe arthritis (4).
The present study was conceived as a narrative description of current knowledge on HR. The operative techniques have all been described, but particular attention has been paid to the evolution of interposition arthroplasties, which have often been described as a marginal procedure, but which nevertheless provide a valid alternative to arthrodesis and prosthesis in the advanced stages of the disease, without precluding the execution of other end-stage procedures in case of failure.
A comprehensive literature search using PubMed database has been performed, using various combinations of the keyword terms “hallux rigidus”, “hallux limitus”, “non-operative”, “conservative”, “surgery”, “treatment”, “osteotomy”, “arthodesis”, “fusion”, “replacement”, “arthroplasty”, “hemiarthroplasty”, “interposition”, “cheilectomy”, “arthroscopy”, “arthrodesis”, “arthrodiastasis”.
English language full-text articles were ordered, and citations from the selected papers were analyzed. Only articles published in peer-reviewed journals and authoritative books were included in this review. Relevant data were then extracted and collected to describe the actual operative and nonoperative options for HR. Finally, a simplified treatment algorithm has been described, based on the current knowledge.
Nonoperative Management
Nonoperative treatment for HR should always be attempted before surgery. Medical therapy by oral nonsteroidal anti-inflammatory drugs may reduce swelling and joint pain. However, they are often insufficient or transient (14).
Articular injections showed to provide pain relief particularly in patients with early stage HR. One study evaluating manipulation under anesthesia and intra-articular steroid injection, found out that most of the patients with low grade HR had benefited for about six months while one-third required surgery; mid-grade patients experienced pain relief for about three months with two-thirds requiring surgery; high grade patients had minimal benefit and all required surgery (16).
Rocker-bottom soles can reduce painful dorsiflexion by avoiding the foot and the shoe to bend. Shoes with high toe box can prevent direct contact with the dorsal osteophytes. It was demonstrated that 47% of patients responded to custom orthoses alone while another 10% responded to simple shoe modifications (11).
Physical therapy involves joint mobilization and manipulation to improve the ROM. Gaiting training, ice packs and rest reduce pain and inflammation. The use of physical therapies such as extracorporeal shockwave therapy, iontophoresis and ultrasound therapy were also proposed, but with little evidence (17).
Anyway, the literature agree that conservative management cannot stop the degenerative progression of the disease (18).
Operative Management
When conservative management fails, a variety of surgical options are available. Joint-sparing procedures are generally preferred in the early stages, while in cases of severe arthritis, joint-sacrificing procedures are indicated. The choice is based on the degree of HR, patient’s age, motivation, activity level and expectations. Different techniques have been proposed, but the optimal operative technique has yet to be defined.
Joint-sparing procedures
Cheilectomy
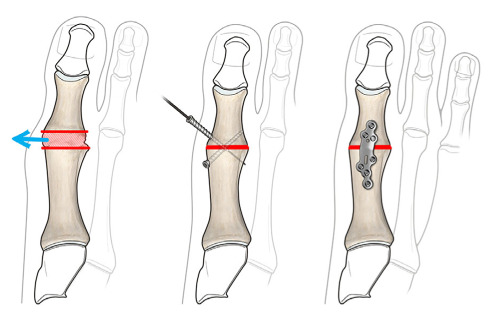
Cheilectomy is a joint-sparing technique popularized by Mann et al. in 1979 (19), involving the resection of 25-30% of the dorsal metatarsal head. In addition, intra-articular loose bodies and metatarsal or phalangeal osteophytes are removed, and the medial, lateral and plantar capsule is released. More than 30% of the dorsal metatarsal head removal is not advised to avoid joint instability and hallux weakening or deformity (Figure 1).
Figure 1.
Cheilectomy involves the resection of 25-30% of the dorsal metatarsal head and removal of osteophytes localized in the metatarsal head and proximal phalanx.
Despite overall good clinical outcomes, with low complication rate (0-3%) (20), cheilectomy does not prevent the progression of the disease and so it is rarely a definitive solution. Recurrence of a dorsal exostosis was found in up to 30% of patients, with arthritic progression. However further operative treatments are not compromised in case of failure (10).
The literature agrees that cheilectomy is indicated in case of end range pain localized on the dorsal exostosis, with minimal or no pain through the midrange of motion (6). Retrospective case series reported good results in early stages, with success rates ranging from 72% to 100%, but poorer results for advanced disease (11).
Phalangeal osteotomy
Bonney and Macnab first described a dorsal closing wedge osteotomy of the proximal phalanx in 1952. The procedure shifted the limited arc of FMTPJ motion dorsally and placed the hallux into more dorsiflexed position, allowing for improved function (Figure 2). Later Moberg published a small case series with satisfactory outcomes (21).
Figure 2.
Moberg osteotomy is a dorsal closing wedge osteotomy of the proximal phalanx.
Several investigators reported on the use of this osteotomy in conjunction with a cheilectomy, with better results than cheilectomy alone. The authors agree that a Moberg osteotomy should be supplemented if a 70° dorsiflexion cannot be achieved intraoperatively with cheilectomy alone (22).
A “peg-in-hole” osteotomy was then described by Regnauld in 1986 (23).
Metatarsal osteotomy
Many of these osteotomies were conceived to correct a long first metatarsal or a metatarsus primus elevatus, in the hypothesis that these are the causes of the disease in some cases. However, the exact role of both conditions as etiologic factors is controversial. Some studies found that a long first metatarsal was not more common in patients with HR than in the general population (24). They demonstrated that 94% of patients with HR has a normal amount of metatarsal elevation (8). The elevation of the first metatarsal was more common in the final stages of HR, and so it appeared more as a consequence than a cause of HR (13).
The rationale of metatarsal osteotomies is to obtain a longitudinal decompression of the joint by obtaining a metatarsal shortening with concomitant plantar translation, allowing the surrounding soft tissues (plantar fascia, long flexors and extensors, capsule) to relax. The stability of fixation is crucial to allow immediate active and passive motion exercises.
Watermann in 1927 was the first to report a distal dorsal closing wedge osteotomy of the first metatarsal. It was designed to relocate the viable plantar cartilage to a more dorsal location, allowing better dorsiflexion. The major disadvantage is that the osteotomy is relatively unstable due to the perpendicular orientation of the osteotomy, with difficult fixation. Moreover, it does not shorten the first metatarsal and it may exacerbate a metatarsus primus elevatus, and it does not relax the plantar fascia (25).
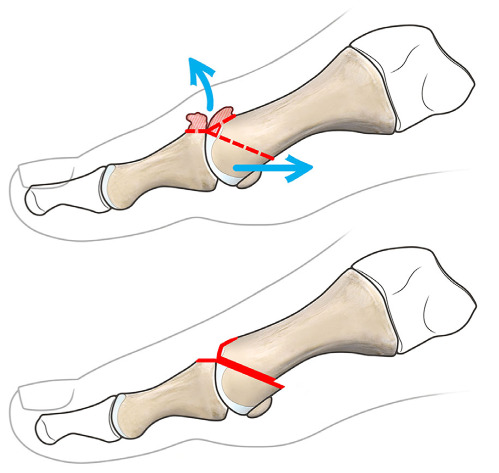
In 1982 Youngswick described a modification to the Austin (chevron-type) distal osteotomy. His modification consisted in making a second osteotomy parallel to the dorsal limb of the V-shaped osteotomy (Figure 3), to translate the metatarsal head plantarward and backward to decompress the joint (26). One of the advantages of this osteotomy is its stability, allowing early range of motion exercises.
Figure 3.
Youngswick is a modification of the Austin (chevron-type) distal osteotomy, with a second osteotomy parallel to the dorsal limb of the V-shaped osteotomy, to translate the metatarsal head plantarward and backward to decompress the joint. Osteophyte removal is also represented.
The authors started to use this technique in index plus forefeet, but the procedure was lately performed also in index minus forefeet with similar results. At present, the authors indicate this osteotomy without taking care of the metatarsal index, because shortening is compensated by plantarization (27).
The Reverdin Green osteotomy is a modification of the Youngswick procedure, with the excised bone block implanted in the plantar limb of the osteotomy to further translate the metatarsal head plantarwards. This procedure was abandoned due to the high rate of complications (28).
Distal oblique sliding osteotomy (Weil osteotomy) is a single, dorsal-distal to plantar-proximal osteotomy line, beginning just proximal to the articular surface and running parallel to the ground (Figure 4) (29).
Figure 4.
Distal oblique sliding (Weil) osteotomy is characterized by a single, dorsal-distal to plantar-proximal oriented osteotomy, translating the metatarsal head plantarward and backward to decompress the joint. Osteophyte removal is also represented.
Sagittal Z osteotomy is performed creating two parallel arms perpendicular to the long axis of the metatarsal bone, a lateral distal and a proximal medial arm, linked by a central arm running sagittally. The sagittal Z osteotomy aims at shortening and thereby decompressing the FMTPJ, while allowing plantarflexion. The advantage is represented by the wide contact area for bone healing, stability and low risk of bone necrosis (30).
Drago et al. described a double osteotomy consisting distally of a Watermann procedure, with associated a proximal plantar flexing osteotomy. The aim was to add the metatarsal plantarflexion, impossible to achieve with the distal osteotomy alone (31).
The sagittal V procedure is a V-shaped osteotomy of the metatarsal neck. The osteotomy is oriented in the sagittal plane, with apex distally (32).
One study tested the mechanical strength of three types of osteotomies, including Youngswick, sagittal V, and Weil, founding that the sagittal V osteotomy was significantly weaker and less stiff (33).
First metatarsal-cuneiform arthrodesis according to Lapidus addresses multiple issues of hallux limitus, specifically elevation and elongation. With a plantar wedge resection at the first metatarsal–cuneiform joint, the first metatarsal can be plantarflexed and shortened accordingly. Cheilectomy can be associated to increase dorsiflexion (34).
A recent review of the literature on metatarsal osteotomies has revealed an increase in dorsiflexion of 10.4°, with a clinical improvement of 39 points on the AOFAS scale, however with a satisfaction rate of only 73.3%, moreover with a high number of reoperations for hardware removal, lesser metatarsals osteotomies, Keller and treatment of infections and non-unions. The rate of post-operative metatarsalgia was 30.5%, so that the authors recommended caution with these procedures (35).
Arthrodiastasis
Arthodiastasis involves extra-articular distraction of the FMTPJ. This is based on the principle that offloading the articular surfaces can stimulate cartilage healing, with pain reduction and ROM improvement. Indications for arthrodiastasis of the FMTPJ include a congruent but painful and stiff joint, with moderate arthritic changes. The procedure involves the use of a hinged or a fixed mini external fixator to obtain distraction, and it can be associated with other periarticular procedures, such as a cheilectomy, microfractures, or metatarsal osteotomies (36).
The disadvantage of the procedure is the need to carry an external fixator for about two months.
Arthroscopy
This procedure was first described by Watanabe in 1972 (37). Ferkel then described the first systematic arthroscopy in 1996 (38).
It is mainly indicated for early grade HR with joint motion still preserved, for arthroscopic debridement and dorsal cheilectomy. Advantages include smaller incisions, reduced operative morbidity and rapid rehabilitation. In addition, joint visualization is possible, which allows for identification of concomitant pathologies. If visualization of the joint is limited, the dorsomedial portal can be extended to convert the procedure to an open cheilectomy. Arthroscopy of the FMTPJ is technically challenging and requires additional surgical training. Complications include iatrogenic cartilage injury, superficial or deep infection, wound dehiscence and sinus tract formation (39).
Joint-sacrificing procedures
Arthrodesis
Arthrodesis of the FMTPJ has been widely accepted as the gold-standard for severe HR, due to its safety and efficacy. It is indicated in young and active patients and as an end-stage procedure in recurrent cases (11,39). The rate of satisfaction with arthrodesis has been reported to be over 80% (40).
Reported complications were malunion, nonunion, interphalangeal arthritis, transfer metatarsalgia. The nonunion rate ranged from 2% to 10% in different studies, even in patients with appropriate fixation. Most of the patients with nonunion rated the result of the surgery as good (probably because of a fibrous union). Patients with osteoporosis and those with rheumatoid arthritis have higher nonunion rates (17,41,42).
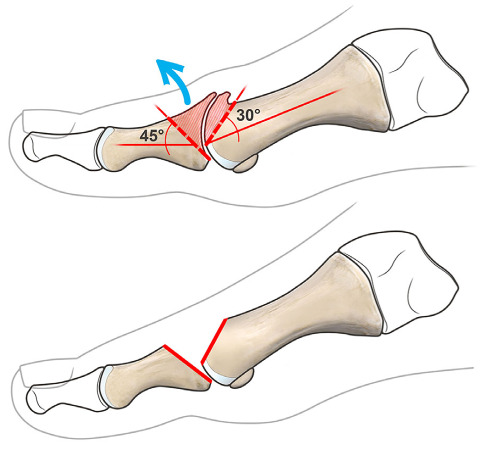
The procedure is typically performed as open surgery, although a percutaneous approach was described (43). The joint surfaces can be prepared either in flat or dome-cup pair configuration. The latter allows for easier intraoperative adjustability. Optimal position of the FMTPJ is 5°–15° of valgus and 10°–20° of dorsiflexion with neutral rotation (Figure 5) (44).
Figure 5.
Arthrodesis of the FMTPJ involves removing the articular cartilage to viable bone tissue in flat or dome-cup pair configuration. Optimal position of the FMTPJ is 5°–15° of valgus and 10°–20° of dorsiflexion with neutral rotation. Various fixation methods are feasible.
Multiple fixation techniques are accepted, such as plates, screws, wires and staples. The most stable technique was demonstrated to be the combination of an oblique lag screw and a dorsal plate. The weakest technique was dorsal plate alone with Kirschner wire fixation (45). One study compared the cost and results of two crossed screws and dorsal plating techniques. The two crossed screws represented a simple and less costly technique, with no statistically significant differences in time to fusion, revision surgery or hardware removal rate between the two techniques (46).
Prosthesis
FMTPJ prosthesis are joint-sacrificing procedures but, unlike arthrodesis, they save the joint movement. This is attractive for many patients who refuse arthrodesis, and the consequent loss of motion, for various functional requests, such as wearing high-heeled shoes and squatting for work or daily activities (47).
Despite the potential benefit of maintaining joint motion while relieving pain, multiple complications have been documented for prosthesis, including implant failure, soft tissue instability, joint stiffness, aseptic loosening, pathological wear, infection (48).
In one study, two years after surgery, 40% of patients operated by prosthesis would not undergo surgery again, compared with only 3% of patients operated by arthrodesis (49). In a recent systematic review of the literature (50) the post-operative AOFAS score was 75.6-90 points for arthrodesis and 72-95.3 points for total joint prosthesis. The improvement on the AOFAS scale was 43.8 points for arthrodesis and 37.7 points for prosthesis. Complication rate was 26.3% for prosthesis and 23.1% for arthrodesis, while the revision rate was 11% for prosthesis and only 3.9% for arthrodesis.
In high-degree HR, chronic stiffness and muscle disuse may limit the resumption of movement even after successful implantation of a prosthesis. This could explain why prosthesis provide limited ROM improvements (51).
To avoid the disadvantages of the total implant, hemiarthroplasties were also developed. Hemiarthroplasty consists of a unipolar implant designed to replace the articular surface of the metatarsal head or the proximal phalanx base. Hemiarthroplasty requires less bone resection and ensures maintenance of toe length. As a result, conversion to arthrodesis would be easier if a revision becomes necessary.
One study showed better mean postoperative AOFAS scores in patients undergoing hemiarthroplasty compared to total joint prosthesis patients, with better ROM improvement (52).
While the success and benefit of prosthesis have been documented in the literature, the reports of high complication rates, unpredictable results and poor survival have led orthopedic surgeons to become cautious with the use of prosthesis. Failure of both total prosthesis and hemiarthroplasty is very difficult to manage because of the significant bone loss. Additionally, the cost compared to arthrodesis is significantly higher.
Resection Arthroplasty
Keller resection arthroplasty was one of the pioneer procedures for the treatment of HR. It involves the resection of up to 50% of the base of the proximal phalanx, achieving joint decompression while increasing movement. However, the procedure may destabilize the FMTPJ leading to weakness, transfer metatarsalgia, excessive shortening of the toe, cock-up deformity. Nevertheless, it is a simple procedure that could be still recommended for low-demand and elderly patients (53).
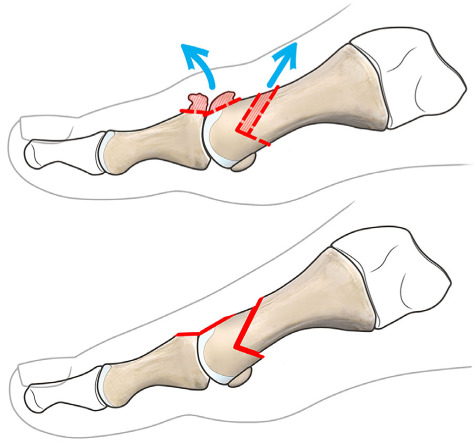
Due to the potential complications, multiple modifications of the Keller resection arthroplasty have been developed. These include a much more limited resection of the proximal phalanx and the addition of a cheilectomy. In 1987, Valente Valenti presented a personal communication describing an 80° sagittal plane “V” resection of the FMTPJ with preservation of the first ray length, and the plantar portion of the first proximal phalangeal base, so conserving the flexor hallucis brevis and the sesamoid function (Figure 6). Complications of the Valenti procedure were a progressive worsening of joint stiffness, but no sesamoiditis, deformities, metatarsalgia or hallux weakening were documented. Through this osteotomy, FMTPJ switches from the movement of two spheroids, to a “book” or a “hinge” movement, which opens and closes, obtaining a good dorsiflexion (54).
Figure 6.
Valenti resection arthroplasty is a “V” resection of the FMTPJ with preservation of the first ray length, the plantar portion of the first metatarsal head and first proximal phalangeal base, and so conserving the flexor hallucis brevis and the sesamoid function.
Some authors stated that this procedure is not indicated in patients with metatarsus primus elevatus, as it does not address the biomechanical etiology of the HR, but other recent studies indicate the opposite, reporting that elevatus was significantly reduced after Valenti procedure. This confirmed that metatarsus elevatus may be secondary to HR and not a cause of it (13).
Interposition Arthroplasty
Arthroplasties can be implemented with the addition of a spacer (joint capsule, extensor hallucis brevis, tendon autograft, tendon allograft, synthetic matrix). The aim of the modifications is maintaining or increase joint motion, stability and length, while adding a tissue that can be rehabited, so acting as a biological spacer between the two joint surfaces. Patients affected by moderate to severe HR but desiring to preserve FMTPJ movement may opt for interposition arthroplasty (IA) to avoid the movement restrictions of arthrodesis (55).
The studies were classified by publication year, and the results were summarized in Table 3. Simple technical reports were discussed in the historical overview, but excluded from the table.
Table 3.
Results from IA studies in the literature
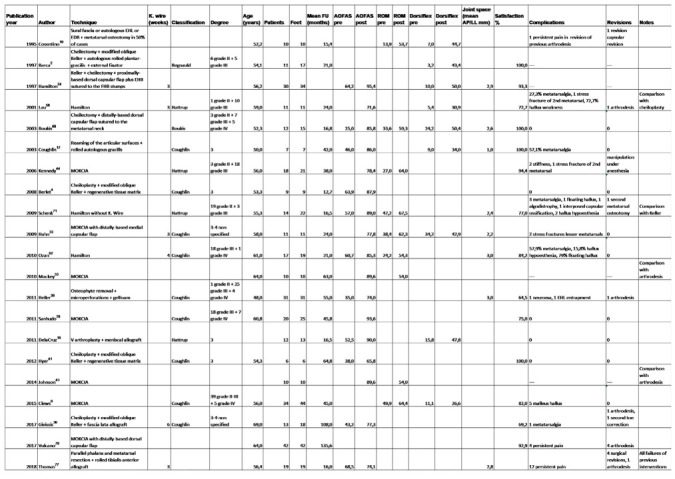
|
The first to describe this technique was Cosentino in 1995, who was inspired by hand surgeons, and in particular by thumb tenosuspension techniques. The author suggested covering the head of the first metatarsal with a graft from the extensor hallucis longus tendon (EHL), long or short extensors of the lesser fingers or sural fascia, sculpted in various ways, in association with eventual decompressive metatarsal osteotomy. He concluded that it was a good procedure to avoid end-stage interventions such as arthrodesis, Keller, implant arthroplasty, which however remained possible in case of failure (56).
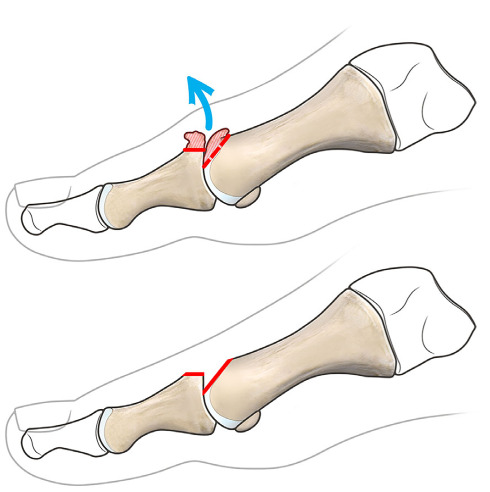
The milestone in the IA was the study by Hamilton et al., who in 1997 described an arthroplasty according to Keller in association with a cheilectomy, implemented by the interposition of a dorsal capsular flap with included the extensor hallucis brevis tendon (EHB), sutured to the stumps of the flexor halluces brevis (FHB). The EHB tendon was sectioned proximally to allow plantar extension and to prevent the flap from tension during gait (Figure 7). The author reported a satisfaction rate of 93% of patients, and recommended to select patients who had first and second metatarsals of approximately the same length (57).
Figure 7.
Hamilton arthroplasty involves a Keller resection of the proximal phalanx in association with a cheilectomy, implemented by the interposition of a dorsal capsular flap including the EHB, sutured to the stumps of the FHB. The EHB tendon is sectioned proximally to prevent the flap from tension during gait.
In the same year Barca et al. described a technique of cheilectomy associated with a modified oblique Keller osteotomy in order to preserve the plantar part of the proximal phalanx with the insertion of FHB. A rolled autologous plantar-gracilis graft was then interposed, and an external fixator was placed for the initial assisted mobilization exercises, maintaining alignment and toe length. This technique has taken over the concepts described by Valenti in 1997, with the addition of a tendon interposition (58).
In 2001 Lau et al. resumed the technique described by Hamilton, comparing it with a cheilectomy group with phalangeal osteotomy. They found post-operative metatarsalgia in 27% of the arthroplasty group, with one stress fracture of the second metatarsal, and hallux weakening in 72,7% of cases. They concluded that IA provides unsecured results, and should therefore be considered as a rescue procedure, while cheilectomy with associated phalangeal osteotomy provided a better load distribution on the forefoot and gave more reproducible results, albeit indicated in early arthritic degrees in the study (59).
The IA proposed by Hamilton was later studied by other authors, who found a rate of metatarsalgia of 21-58%, with floating hallux in 79% of cases (60,61). One of the aforementioned studies evaluated the differences in the outcomes between the Hamilton IA and the Keller arthroplasty. The study did not find any relevant difference between the two procedures (61).
In 2003 Coughlin et al. described a technique for preparation of the articular surfaces by reaming for subsequent positioning of a rolled gracilis tendon. The authors reported a high patient satisfaction rate, albeit with metatarsalgia in 57% of cases (62).
In the same 2003 Roukis described a cheilectomy associated with the interposition of a distal-based dorsal capsular flap, sutured plantarly to the metatarsal neck through transosseous points anchored dorsally to the metatarsal (63).
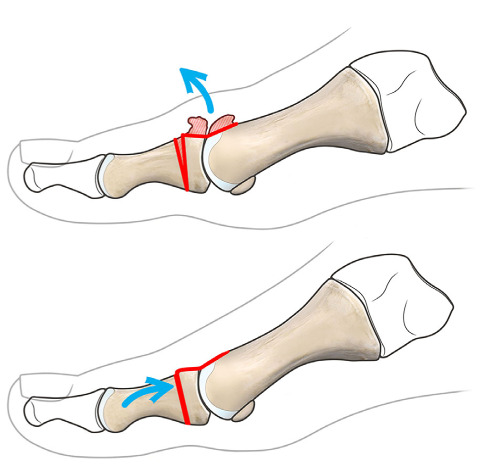
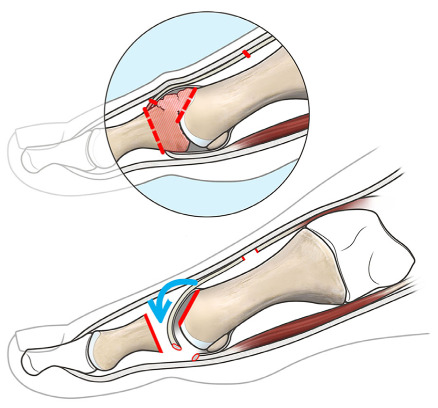
However, the description of the most accepted technique, which was called “modified oblique Keller procedure” was due to Mroczek et al. in 2003. This technique involved the creation of a cheilectomy associated with a modified Keller oblique osteotomy in order to preserve the plantar part of the proximal phalanx with the insertion of FHB, in the same way described by Barca in 1997. Nonetheless, a dorsal capsular flap was associated, with included the EHB tendon sectioned proximally. This flap was sutured to the plantar plate distal to the sesamoids (Figure 8) (64).
Figure 8.
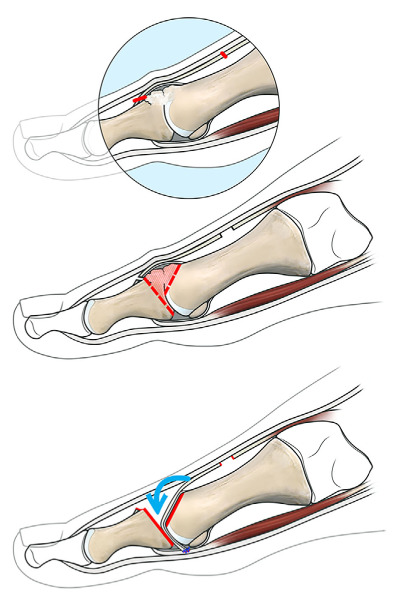
MOKCIA arthroplasty involves a cheilectomy associated with a modified Keller oblique osteotomy in order to preserve the plantar part of the proximal phalanx with the insertion of FHB. A dorsal capsular flap was interposed, with included the EHB tendon sectioned proximally. This flap was sutured to the plantar plate distal to the sesamoids.
The authors limited their description to a technical report. Nevertheless, this was the starting point for the subsequent evolution of the technique (65-67).
Among these it was Mackey in 2012 who first coined the initials MOKCIA to identify the Modified Oblique Keller Capsular Interposition Arthroplasty technique, with the use of a dorsal flap with proximal base (68).
Various authors studied this procedure describing a little number of complications such as recurrence of stiffness and stress fracture of the second metatarsal (69), or hallux malleus (65). This technique was recommended in severe HR, in the absence of deformities such as hallux valgus or varus, in patients who want to maintain range of motion while obtaining pain relief. Two studies compared the results obtained with MOKCIA technique and arthrodesis, demonstrating better clinical outcomes for the MOKCIA, which obtained a nearly normal pattern of plantar pressures during walking. In particular no difference was retrieved in plantar pressure under the second metatarsal head between arthroplasties and arthrodesis, but the arthrodesis groups did have a greater plantar pressure under the first metatarsal head (66,70).
The MOKCIA preserves the stability of the big toe while maintaining the plantar plate, being suitable for young or middle-aged patients with an active lifestyle, not precluding the possibility of subsequent arthrodesis. An interesting aspect is to avoid FMTPJ arthrodesis in patients with interphalangeal arthrosis of the big toe.
In 2008 Berlet et al. described a similar technique, but with the interposition of a regenerative tissue matrix membrane, consisting of collagen and extracellular protein matrices and created from human cadaver tissue (71,72).
In 2009 Hahn et al. described a variant of the modified Keller + cheilectomy technique, with medial access and interposition of a distally based medial capsular flap. These authors also described good results, even though with two cases of stress fracture of the second metatarsal out of the 11 cases included in the series (73).
In 2011 DelaCruz et al. described a V-shaped arthroplasty with interposition of allogeneic meniscus. The results described after an average follow-up of 16.5 months were encouraging, and the authors recommended the technique for advanced HR in patients who refuse arthrodesis and also in those with failure of previous surgery (74).
In 2011 Heller et al. described an osteophyte regularization technique with gelfoam interposition, obtaining a rate of patient satisfaction of 64.5% after an average follow-up of 55 months (75).
In 2017 Givissis et al. described a cheilectomy with associated modified Keller and fascia lata allograft interposition. The authors reported a 69.2% satisfaction rate after an average follow-up of 108 months (76).
In 2017 Vulcano et al. described a variant of MOKCIA, using a distally based dorsal capsular flap, and obtaining good or excellent results in 92.9% of cases after an average follow-up of 135.6 months (77).
In 2018 Thomas et al. described a technique of parallel resection of the metatarsal head and of the base of the proximal phalanx with the interposition of a rolled tibialis anterior tendon allograft. All operated patients were failures of previous interventions, and this technique was recommended as a rescue procedure (78).
In the years 2011 to 2017 our group adopted the arthroplasty technique described by Pisani G. et al., with regularization of the metatarsal head and interposition of a proximal-based medial capsular flap. We performed a case series of 20 cases, which could be the subject of a future study (79).
Discussion
HR is a challenging pathology for the surgeon, who must work out the best treatment based on the patient’s characteristics, extricating from a multitude of possible interventions and carefully relating them to the patient’s activity level and expectations (Table 4). Patients must be correctly informed that there is no ideal procedure, which is free from failures and complications.
Table 4.
Simplified treatment algorithm according to Coughlin and Shurnas classification
|
Given the unsecured results with surgical treatment, a nonoperative strategy should always be attempted before surgery.
Joint-sparing procedures must be considered for early stages HR. Decompression osteotomies are indicated in early stages and in the hallux limitus, because it is necessary to decompress a still functioning joint, releasing the soft tissues. An elevated and/or long first metatarsal should suggest this type of indication, even though it has been shown that decompressive osteotomies are not affected by the metatarsal formula (26). Youngswick and Weil osteotomies have proven to be stable enough to allow early mobilization (27,32).
In the middle degrees cheilectomy is indicated, especially in case of pain only at the end range of dorsiflexion (6). Phalangeal osteotomy according to Moberg is considered as an addition to cheilectomy in the case that it fails to achieve sufficient dorsiflexion alone (22). The field of application of arthroscopy overlaps with that of cheilectomy, which in fact can be performed arthroscopically.
Arthrodiastasis also ranks in the mid grades HR, but with uncertain results compared to long rest time, which is often unacceptable for active patients.
Joint-sacrificing procedures are indicated in advanced stages, particularly in case of mid-range pain. Among these, prosthesis showed limited survivorship with high complication rate, and this does not justify their cost, especially if compared with arthrodesis. The choice of arthroplasty depends more on the patient than on the surgeon: it is in fact intended for the patient with high-grade HR who refuses arthrodesis.
From the available literature the gold standard is still represented by arthrodesis, which provides the safest and most reproducible results, being the only one to achieve a grade B recommendation (39). The drawback of arthrodesis is the loss of motion which restricts shoe choice, and contributes to patient dissatisfaction, particularly in females.
Between these two techniques the Valenti procedure has shown excellent results with a low complication rate, without precluding end-stage procedures such as implant arthroplasties or arthrodesis in case of failure (54).
Keller arthroplasty is instead a quick and simple procedure that is reserved for elderly low-demand patients (53).
Implementing the arthoplasties with the interposition of a biologic spacer can provide an alternative to the end-stage procedures for young patients who want to preserve FMTPJ, without precluding end-stage procedures in case of failure. Among the IA, the MOKCIA technique showed lower complication rates than the other IA techniques. MOKCIA does not sacrifice the insertion of the FHB, maintaining the stability and strength of the big toe, and does not alter the toe length. Accordingly, most cases of post-operative metatarsalgia or floating hallux were described in relation to the Hamilton technique, which demonstrated results similar to the Keller arthroplasty (61).
Although long-term randomized controlled trials are lacking for MOKCIA, the reported results are comparable to the other alternatives for end-stage HR, providing better plantar load distribution than arthrodesis (65,69), and avoiding the drawbacks of implant arthroplasties. These findings make the MOKCIA technique a valid alternative for the treatment of HR also in the young active patient, as attractive as the most consolidated techniques to date (80).
In the case of deformities, the only suitable procedures are osteotomies for low degrees and arthrodesis for high degrees HR.
The limitation of the present study lies in its narrative nature, preferring a historical examination of the various techniques evolving over the years, rather than the systematic analysis of the results of interposition arthroplasties. The latter could be the goal of further studies.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Gould N, Schneider W, Ashikaga T. Epidemiological survey of foot problems in the continental United States: 1978-1979. Foot Ankle. 1980;1(1):8–10. doi: 10.1177/107110078000100104. [DOI] [PubMed] [Google Scholar]
- Davies-Colley M. Contraction of the metatarsophalangeal joint of the great toe. Br Med J. 1887;1:728. [Google Scholar]
- Cotterill JM. The pathology of hallux rigidus. Br Med J. 1903;2(2239):1400. doi: 10.1136/bmj.2.2239.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam A, Chan JJ, Surace MF, Vulcano E. Hallux rigidus: How do I approach it? World J Orthop. 2017;8(5):364–71. doi: 10.5312/wjo.v8.i5.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattrup SJ, Johnson KA. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res. 1988;226:182–91. [PubMed] [Google Scholar]
- Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85(11):2072–88. [PubMed] [Google Scholar]
- Beeson P, Phillips C, Corr S, Ribbans W. Classification systems for hallux rigidus: a review of the literature. Foot Ankle Int. 2008;29(4):407–14. doi: 10.3113/FAI.2008.0407. [DOI] [PubMed] [Google Scholar]
- Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731–43. doi: 10.1177/107110070302401002. [DOI] [PubMed] [Google Scholar]
- DuVries H. Static deformities. In: DuVries H, editor. Surgery of the Foot. St. Louis: Mosby; 1959. pp. 392–8. [Google Scholar]
- Perler AD, Nwosu V, Christie D, Higgins K. End-stage osteoarthritis of the great toe/hallux rigidus: a review of the alternatives to arthrodesis: implant versus osteotomies and arthroplasty techniques. Clin Podiatr Med Surg. 2013;30(3):351–95. doi: 10.1016/j.cpm.2013.04.011. [DOI] [PubMed] [Google Scholar]
- Migues A, Slullitel G. Joint-preserving procedure for moderate hallux rigidus. Foot Ankle Clin. 2012;17(3):459–71. doi: 10.1016/j.fcl.2012.06.006. [DOI] [PubMed] [Google Scholar]
- Lambrinudi C. Metatarsus Primus Elevatus. Proc R Soc Med. 1938;31(11):1273. doi: 10.1177/003591573803101103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez PJ, Grady JF, Lenz RC, Park SJ, Ruff JG. Metatarsus Primus Elevatus Resolution After First Metatarsophalangeal Joint Arthroplasty. J Am Podiatr Med Assoc. 2018;108(3):200–4. doi: 10.7547/16-176. [DOI] [PubMed] [Google Scholar]
- Deland JT, Williams BR. Surgical management of hallux rigidus. J Am Acad Orthop Surg. 2012;20(6):347–58. doi: 10.5435/JAAOS-20-06-347. [DOI] [PubMed] [Google Scholar]
- Feldman RS, Hutter J, Lapow L, Pour B. Cheilectomy and hallux rigidus. J Foot Surg. 1983;22(2):170–4. [PubMed] [Google Scholar]
- Solan MC, Calder JD, Bendall SP. Manipulation and injection for hallux rigidus. Is it worthwhile? J Bone Joint Surg Br. 2001;83(5):706–8. doi: 10.1302/0301-620x.83b5.11425. [DOI] [PubMed] [Google Scholar]
- Kunnasegaran R, Thevendran G. Hallux Rigidus: Nonoperative Treatment and Orthotics. Foot Ankle Clin. 2015;20(3):401–12. doi: 10.1016/j.fcl.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Caravelli S, Mosca M, Massimi S, et al. A comprehensive and narrative review of historical aspects and management of low-grade hallux rigidus: conservative and surgical possibilities. Musculoskelet Surg. 2018;102(3):201–11. doi: 10.1007/s12306-018-0530-3. [DOI] [PubMed] [Google Scholar]
- Mann RA, Coughlin MJ, DuVries HL. Hallux rigidus: A review of the literatureand a method of treatment. Clin Orthop Relat Res. 1979;142:57–63. [PubMed] [Google Scholar]
- Bussewitz BW, Dyment MM, Hyer CF. Intermediate-term results following first metatarsal cheilectomy. Foot Ankle Spec. 2013;6(3):191–5. doi: 10.1177/1938640013484793. [DOI] [PubMed] [Google Scholar]
- Moberg E. A simple operation for hallux rigidus. Clin Orthop Relat Res. 1979;142:55–6. [PubMed] [Google Scholar]
- Waizy H, Czardybon MA, Stukenborg-Colsman C, et al. Mid- and long-term results of the joint preserving therapy of hallux rigidus. Arch Orthop Trauma Surg. 2010;130(2):165–70. doi: 10.1007/s00402-009-0857-1. [DOI] [PubMed] [Google Scholar]
- Freeman BL, Hardy MA. Multiplanar phalangeal and metatarsal osteotomies for hallux rigidus. Clin Podiatr Med Surg. 2011;28(2):329–44. doi: 10.1016/j.cpm.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Horton GA, Park YW, Myerson MS. Role of metatarsus primus elevatus in the pathogenesis of hallux rigidus. Foot Ankle Int. 1999;20(12):777–80. doi: 10.1177/107110079902001204. [DOI] [PubMed] [Google Scholar]
- Galois L, Hemmer J, Ray V, Sirveaux F. Surgical options for hallux rigidus: state of the art and review of the literature. Eur J Orthop Surg Traumatol. 2020;30(1):57–65. doi: 10.1007/s00590-019-02528-x. [DOI] [PubMed] [Google Scholar]
- Youngswick FD. Modifications of the Austin bunionectomy for treatment of metatarsus primus elevatus associated with hallux limitus. J Foot Surg. 1982;21(2):114–6. [PubMed] [Google Scholar]
- Slullitel G, López V, Seletti M, Calvi JP, Bartolucci C, Pinton G. Joint Preserving Procedure for Moderate Hallux Rigidus: Does the Metatarsal Index Really Matter? J Foot Ankle Surg. 2016;55(6):1143–7. doi: 10.1053/j.jfas.2016.06.003. [DOI] [PubMed] [Google Scholar]
- Kilmartin TE. Phalangeal osteotomy versus first metatarsal decompression osteotomy for the surgical treatment of hallux rigidus: a prospective study of age-matched and condition-matched patients. J Foot Ankle Surg. 2005;44(1):2–12. doi: 10.1053/j.jfas.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Lundeen RO, Rose JM. Sliding oblique osteotomy for the treatment of hallux abducto valgus associated with functional hallux limitus. J Foot Ankle Surg. 2000;39(3):161–7. doi: 10.1016/s1067-2516(00)80017-4. [DOI] [PubMed] [Google Scholar]
- Viegas GV. Reconstruction of hallux limitus deformity using a first metatarsal sagittal-Z osteotomy. J Foot Ankle Surg. 1998;37(3):204–11. doi: 10.1016/s1067-2516(98)80112-9. [DOI] [PubMed] [Google Scholar]
- Drago JJ, Oloff L, Jacobs AM. A comprehensive review of hallux limitus. J Foot Surg. 1984;23(3):213–20. [PubMed] [Google Scholar]
- LaMar L, Deroy AR, Sinnot MT, Haut R, Squire M, Wertheimer S. Mechanical comparison of the Youngswick, sagittal V, and modified Weil osteotomies for hallux rigidus in a sawbone model. J Foot Ankle Surg. 2006;45(2):70–5. doi: 10.1053/j.jfas.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Blitz NM. The versatility of the Lapidus arthrodesis. Clin Podiatr Med Surg. 2009;26(3):427–41. doi: 10.1016/j.cpm.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Roukis TS. Clinical outcomes after isolated periarticular osteotomies of the first metatarsal for hallux rigidus: a systematic review. J Foot Ankle Surg. 2010;49(6):553–60. doi: 10.1053/j.jfas.2010.08.014. [DOI] [PubMed] [Google Scholar]
- Abraham JS, Hassani H, Lamm BM. Hinged external fixation distraction for treatment of first metatarsophalangeal joint arthritis. J Foot Ankle Surg. 2012;51(5):604–12. doi: 10.1053/j.jfas.2012.04.022. [DOI] [PubMed] [Google Scholar]
- Watanabe M. Selfoc-Arthroscope (Watanabe no. 24 arthroscope) Tokyo: Teishin Hospital; 1972. pp. 1–12. [Google Scholar]
- Ferkel RD. In: Great-toe arthroscopy. Arthroscopic Surgery: The Foot and Ankle. Ferkel RD, editor. Philadelphia: Lippincott-Raven; 1996. pp. 255–72. [Google Scholar]
- Nakajima K. Arthroscopy of the First Metatarsophalangeal Joint. J Foot Ankle Surg. 2018;57(2):357–363. doi: 10.1053/j.jfas.2017.10.003. [DOI] [PubMed] [Google Scholar]
- McNeil DS, Baumhauer JF, Glazebrook MA. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int. 2013;34(1):15–32. doi: 10.1177/1071100712460220. [DOI] [PubMed] [Google Scholar]
- Ellington JK, Jones CP, Cohen BE, Davis WH, Nickisch F, Anderson RB. Review of 107 hallux MTP joint arthrodesis using dome-shaped reamers and a stainless-steel dorsal plate. Foot Ankle Int. 2010;31(5):385–90. doi: 10.3113/FAI.2010.0385. [DOI] [PubMed] [Google Scholar]
- Doty J, Coughlin M, Hirose C, Kemp T. Hallux metatarsophalangeal joint arthrodesis with a hybrid locking plate and a plantar neutralization screw: a prospective study. Foot Ankle Int. 2013;34(11):1535–40. doi: 10.1177/1071100713494779. [DOI] [PubMed] [Google Scholar]
- Hunt KJ, Ellington JK, Anderson RB, Cohen BE, Davis WH, Jones CP. Locked versus nonlocked plate fixation for hallux MTP arthrodesis. Foot Ankle Int. 2011;32(7):704–9. doi: 10.3113/FAI.2011.0704. [DOI] [PubMed] [Google Scholar]
- Fanous RN, Ridgers S, Sott AH. Minimally invasive arthrodesis of the first metatarsophalangeal joint for hallux rigidus. Foot Ankle Surg. 2014;20(3):170–3. doi: 10.1016/j.fas.2014.03.004. [DOI] [PubMed] [Google Scholar]
- Ho B, Baumhauer J. Hallux rigidus. EFORT Open Rev. 2017;2(1):13–20. doi: 10.1302/2058-5241.2.160031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2003;24(4):332–7. doi: 10.1177/107110070302400405. [DOI] [PubMed] [Google Scholar]
- Hyer CF, Glover JP, Berlet GC, Lee TH. Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg. 2008;47(1):13–8. doi: 10.1053/j.jfas.2007.08.016. [DOI] [PubMed] [Google Scholar]
- Massimi S, Caravelli S, Fuiano M, Pungetti C, Mosca M, Zaffagnini S. Management of high-grade hallux rigidus: a narrative review of the literature. Musculoskelet Surg. 2020;104(3):237–43. doi: 10.1007/s12306-020-00646-y. [DOI] [PubMed] [Google Scholar]
- Horisberger M, Haeni D, Henninger HB, Valderrabano V, Barg A. Total Arthroplasty of the Metatarsophalangeal Joint of the Hallux. Foot Ankle Int. 2016;37(7):755–65. doi: 10.1177/1071100716637901. [DOI] [PubMed] [Google Scholar]
- Gibson JN, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int. 2005;26(9):680–90. doi: 10.1177/107110070502600904. [DOI] [PubMed] [Google Scholar]
- Stevens J, de Bot RTAL, Hermus JPS, van Rhijn LW, Witlox AM. Clinical Outcome Following Total Joint Replacement and Arthrodesis for Hallux Rigidus: A Systematic Review. JBJS Rev. 2017 Nov;5(11):e2. doi: 10.2106/JBJS.RVW.17.00032. [DOI] [PubMed] [Google Scholar]
- Stone OD, Ray R, Thomson CE, Gibson JN. Long-Term Follow-up of Arthrodesis vs Total Joint Arthroplasty for Hallux Rigidus. Foot Ankle Int. 2017;38(4):375–80. doi: 10.1177/1071100716682994. [DOI] [PubMed] [Google Scholar]
- Stibolt RD, Patel HA, Lehtonen EJ, et al. Hemiarthroplasty Versus Total Joint Arthroplasty for Hallux Rigidus: A Systematic Review and Meta-analysis. Foot Ankle Spec. 2019;12(2):181–93. doi: 10.1177/1938640018791017. [DOI] [PubMed] [Google Scholar]
- Schneider W, Kadnar G, Kranzl A, Knahr K. Long-term results following Keller resection arthroplasty for hallux rigidus. Foot Ankle Int. 2011;32(10):933–9. doi: 10.3113/FAI.2011.0933. [DOI] [PubMed] [Google Scholar]
- Colò G, Samaila EM, Magnan B, Felli L. Valenti resection arthroplasty for hallux rigidus: A systematic review. Foot Ankle Surg. 2020 Dec;26(8):838–44. doi: 10.1016/j.fas.2019.11.009. [DOI] [PubMed] [Google Scholar]
- Patel HA, Kalra R, Johnson JL, et al. Is interposition arthroplasty a viable option for treatment of moderate to severe hallux rigidus? - A systematic review and meta-analysis. Foot Ankle Surg. 2019;25(5):571–9. doi: 10.1016/j.fas.2018.07.006. [DOI] [PubMed] [Google Scholar]
- Cosentino GL. The Cosentino modification for tendon interpositional arthroplasty. J Foot Ankle Surg. 1995;34(5):501–8. doi: 10.1016/S1067-2516(09)80028-8. [DOI] [PubMed] [Google Scholar]
- Hamilton WG, O’Malley MJ, Thompson FM, Kovatis PE. Roger Mann Award 1995. Capsular interposition arthroplasty for severe hallux rigidus. Foot Ankle Int. 1997;18(2):68–70. doi: 10.1177/107110079701800204. [DOI] [PubMed] [Google Scholar]
- Barca F. Tendon arthroplasty of the first metatarsophalangeal joint in hallux rigidus: preliminary communication. Foot Ankle Int. 1997;18(4):222–8. doi: 10.1177/107110079701800407. [DOI] [PubMed] [Google Scholar]
- Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int. 2001;22(6):462–70. doi: 10.1177/107110070102200602. [DOI] [PubMed] [Google Scholar]
- Ozan F, Bora OA, Filiz MA, Kement Z. Interposition arthroplasty in the treatment of hallux rigidus. Acta Orthop Traumatol Turc. 2010;44(2):143–51. doi: 10.3944/AOTT.2010.2243. [DOI] [PubMed] [Google Scholar]
- Schenk S, Meizer R, Kramer R, Aigner N, Landsiedl F, Steinboeck G. Resection arthroplasty with and without capsular interposition for treatment of severe hallux rigidus. Int Orthop. 2009;33(1):145–50. doi: 10.1007/s00264-007-0457-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin MJ, Shurnas PJ. Soft-tissue arthroplasty for hallux rigidus. Foot Ankle Int. 2003;24(9):661–72. doi: 10.1177/107110070302400902. [DOI] [PubMed] [Google Scholar]
- Roukis TS, Landsman AS, Ringstrom JB, Kirschner P, Wuenschel M. Distally based capsule-periosteum interpositional arthroplasty for hallux rigidus. Indications, operative technique, and short-term follow-up. J Am Podiatr Med Assoc. 2003;93(5):349–66. doi: 10.7547/87507315-93-5-349. [DOI] [PubMed] [Google Scholar]
- Mroczek KJ, Miller SD. The modified oblique Keller procedure: a technique for dorsal approach interposition arthroplasty sparing the flexor tendons. Foot Ankle Int. 2003;24(7):521–2. doi: 10.1177/107110070302400702. [DOI] [PubMed] [Google Scholar]
- Clews CN, Kingsford AC, Samaras DJ. Autogenous capsular interpositional arthroplasty surgery for painful hallux rigidus: assessing changes in range of motion and postoperative foot health. J Foot Ankle Surg. 2015;54(1):29–36. doi: 10.1053/j.jfas.2014.09.004. [DOI] [PubMed] [Google Scholar]
- Mackey RB, Thomson AB, Kwon O, Mueller MJ, Johnson JE. The modified oblique keller capsular interpositional arthroplasty for hallux rigidus. J Bone Joint Surg Am. 2010;92(10):1938–46. doi: 10.2106/JBJS.I.00412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanhudo JA, Gomes JE, Rodrigo MK. Surgical treatment of advanced hallux rigidus by interpositional arthroplasty. Foot Ankle Int. 2011;32(4):400–6. doi: 10.3113/FAI.2011.0400. [DOI] [PubMed] [Google Scholar]
- Mackey RB, Johnson JE. Modified Oblique Keller Capsular Interposition Arthroplasty for Hallux Rigidus. JBJS Essent Surg Tech. 2012;2(1):e3. doi: 10.2106/JBJS.ST.K.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy JG, Chow FY, Dines J, Gardner M, Bohne WH. Outcomes after interposition arthroplasty for treatment of hallux rigidus. Clin Orthop Relat Res. 2006;445:210–5. doi: 10.1097/01.blo.0000201166.82690.23. [DOI] [PubMed] [Google Scholar]
- Johnson JE, McCormick JJ. Modified oblique Keller capsular interposition arthroplasty (MOKCIA) for treatment of late-stage hallux rigidus. Foot Ankle Int. 2014;35(4):415–22. doi: 10.1177/1071100714523590. [DOI] [PubMed] [Google Scholar]
- Berlet GC, Hyer CF, Lee TH, Philbin TM, Hartman JF, Wright ML. Interpositional arthroplasty of the first MTP joint using a regenerative tissue matrix for the treatment of advanced hallux rigidus. Foot Ankle Int. 2008;29(1):10–21. doi: 10.3113/FAI.2008.0010. [DOI] [PubMed] [Google Scholar]
- Hyer CF, Granata JD, Berlet GC, Lee TH. Interpositional arthroplasty of the first metatarsophalangeal joint using a regenerative tissue matrix for the treatment of advanced hallux rigidus: 5-year case series follow-up. Foot Ankle Spec. 2012;5(4):249–52. doi: 10.1177/1938640012443285. [DOI] [PubMed] [Google Scholar]
- Hahn MP, Gerhardt N, Thordarson DB. Medial capsular interpositional arthroplasty for severe hallux rigidus. Foot Ankle Int. 2009;30(6):494–9. doi: 10.3113/FAI.2009.0494. [DOI] [PubMed] [Google Scholar]
- DelaCruz EL, Johnson AR, Clair BL. First metatarsophalangeal joint interpositional arthroplasty using a meniscus allograft for the treatment of advanced hallux rigidus: surgical technique and short-term results. Foot Ankle Spec. 2011;4(3):157–64. doi: 10.1177/1938640011402821. [DOI] [PubMed] [Google Scholar]
- Heller E, Robinson D. Gelfoam first metatarsophalangeal replacement / interposition arthroplasty - a case series with functional outcomes. Foot (Edinb) 2011;21(3):119–23. doi: 10.1016/j.foot.2010.11.007. [DOI] [PubMed] [Google Scholar]
- Givissis PK, Symeonidis PD, Kitridis DM, Daskalakis DN, Christodoulou AG. Minimal resection interposition arthroplasty of the first metatarsophalangeal joint. Foot (Edinb) 2017;32:1–7. doi: 10.1016/j.foot.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Vulcano E, Chang AL, Solomon D, Myerson M. Long-Term Follow-up of Capsular Interposition Arthroplasty for Hallux Rigidus. Foot Ankle Int. 2018;39(1):1–5. doi: 10.1177/1071100717732124. [DOI] [PubMed] [Google Scholar]
- Thomas D, Thordarson D. Rolled Tendon Allograft Interposition Arthroplasty for Salvage Surgery of the Hallux Metatarsophalangeal Joint. Foot Ankle Int. 2018;39(4):458–62. doi: 10.1177/1071100717746609. [DOI] [PubMed] [Google Scholar]
- Pisani G. Alluce rigido. Trattato di chirurgia del piede. Torino: Minerva Medica; 2004. pp. 364–367. [Google Scholar]
- Galli MM, Hyer CF. Hallux rigidus: what lies beyond fusion, resectional arthroplasty, and implants. Clin Podiatr Med Surg. 2011;28(2):385–403. doi: 10.1016/j.cpm.2011.02.005. [DOI] [PubMed] [Google Scholar]


