Abstract
Pertussis is a highly contagious respiratory infection caused by Bordetella pertussis bacterium. The mainstay of treatment is macrolide antibiotics that reduce transmissibility, shorten the duration of symptoms and decrease mortality in infants. Recently, the macrolide resistance of B. pertussis has been reported globally but is especially widespread in mainland China. In this review, we aim to summarise the current understanding of the epidemiology, resistance mechanisms and clinical implications of B. pertussis macrolide resistance. Since the first appearance of macrolide-resistant B. pertussis in Arizona, USA, in 1994, only sporadic cases have been reported outside China. In certain parts of China, on the other hand, up to 70–100% of the recent clinical isolates have been found to be macrolide resistant. Reasons for macrolide resistance being centred upon China during the last decade can only be speculated on, but the dominant B. pertussis lineage is different between China and most of the high-income countries. It seems evident that efforts to increase awareness, guide molecular epidemiological surveillance and carry out systematic screening of B. pertussis positive samples for macrolide resistance should be implemented globally. In addition, practices to improve the clinical care of infants with pertussis caused by resistant strains should be studied vigorously.
Keywords: Bordetella pertussis, pertussis, whooping cough, macrolides, macrolide resistance, erythromycin, azithromycin, clarithromycin
1. Introduction
Pertussis, or whooping cough, is a highly contagious respiratory infection caused by Bordetella pertussis, a small Gram-negative rod bacterium. Despite extensive vaccinations, whooping cough is resurging in many countries including USA, UK and China [1]. The disease can manifest as a severe life-threatening illness, especially in unvaccinated young infants. A cornerstone of the clinical management of infants with recent onset of pertussis infection is, in addition to supportive care, antibiotic management by macrolide antibiotics. Macrolide treatment might ameliorate the disease when started early after infection onset, before the appearance of paroxysmal cough [2].
Macrolides (erythromycin (ERY), clarithromycin (CHL) and azithromycin (AZT)] are the first line antimicrobials used to treat pertussis patients. Several studies have shown their efficacy in vitro, and in clinical settings for clearance of B. pertussis [3,4,5,6].
The first B. pertussis strain with decreased sensitivity to macrolide antibiotics was detected in Arizona, USA in 1994 [7]. Since then, macrolide resistant B. pertussis has been detected in several countries, although it is rare. However, macrolide resistant B. pertussis has been increasingly reported in China during past decade, raising the concern of its potential transmission to other regions and countries. In this review, we aim to describe the epidemiological features, main resistance mechanism, issues with rapid diagnostics, and clinical implications of macrolide resistant B. pertussis. Search strategy: We searched PubMed and Google Scholar for articles published before 20 October 2022, by use of the terms: “pertussis” AND “macrolide” AND “resistance”, and reference lists of identified studies. Only articles written in English were included. Finally, only the most relevant papers for this review were citated.
2. Pertussis Diagnostics
Pertussis diagnostics can be divided into three main approaches: (1) culture, (2) nucleic acid detection (PCR) and (3) serology. Patient age, vaccination history and onset of the symptoms should be considered when choosing the correct diagnostic method [8]. Culture can be performed up to 2 weeks after the symptoms have appeared, before the bacteria is cleared by the immune defence. Specimen from freshly obtained nasopharyngeal (NP) samples should be cultured on Regan-Lowe (RL, charcoal) or Bordet-Gengou (BG, blood) agar containing cephalexin. Suspected B. pertussis specific colonies are further cultured on RL/BG agar (without cephalexin), and identified with e.g., slide agglutination test with specific anti-B. pertussis and anti-B. parapertussis sera or MALDI-TOF [8,9,10]. Specific nucleic acid identification (targeting IS481/ptxp) with PCR requires only a small amount of DNA for detection and identification of the bacterium and is therefore far more sensitive than culture. Furthermore, it can be used even three to four weeks after the onset of symptoms. Therefore, PCR-based approaches are more widely used than culture, especially with infants and small children. For school children and adults, serology is commonly used as there is less interference in antibodies induced from previous vaccinations and the only symptom may have been a prolonged cough (>3–4 weeks, culture nor PCR can be used). Serological diagnosis should be made based on the measurement of serum IgG antibodies against pertussis toxin [11]. Furthermore, laboratory confirmation of B. pertussis from clinical samples is needed before antimicrobial susceptibility testing (AST) is performed.
3. Epidemiology
The first macrolide resistant B. pertussis strain was identified in a 2-month-old infant from Yuma, Arizona, US in 1994 [7]. The isolate was highly resistant to erythromycin with a minimum inhibitory concentration (MIC) > 64 µg/mL. However, the origin of this isolate was not known. Breakpoints to detect antimicrobial resistance of clinical B. pertussis isolates were not standardized but the reported resistant strains had MICs of >256 µg/mL with erythromycin (ERY) and clarithromycin (CHL) by Etest method suggesting macrolide resistance. Concurrently, seven additional B. pertussis isolates from the same area were tested, but macrolide resistance was not detected in these cases. In a review of 47 B. pertussis isolates from children in Utah, US, in 1985–1997, one isolate from January 1997 was resistant against erythromycin [12].
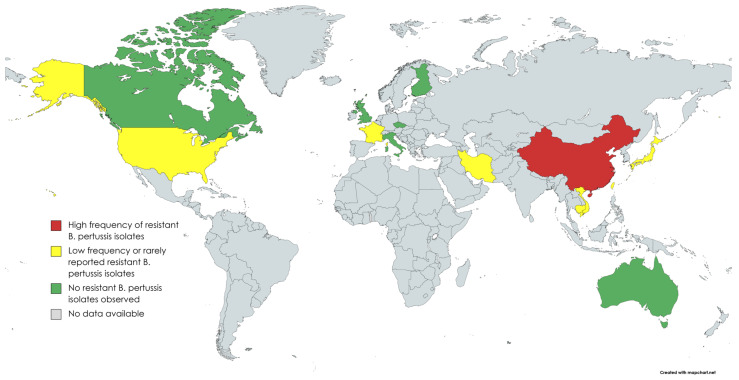
Since the first appearance of macrolide-resistant B. pertussis, macrolide susceptibility has been tested in thousands of cultured isolates all over the world (Table 1, Figure 1). In a study of 1030 isolates collected from various parts of the the US, five (0.5%) isolates were erythromycin resistant. Four out of five isolates were from Arizona (1994–1995) and one from Georgia (1995). All isolates initially showed the growth inhibition of B. pertussis by disc diffusion method, but after 5–7 days of incubation, novel bacterial colonies appeared on the plate inside the growth inhibition area, demonstrating heterogeneous phenotype [13]. In a review of 38 B. pertussis isolates from France in 2003, none of them were resistant to erythromycin [14]. However, nine years later in 2012, the first patient in Europe with macrolide-resistant B. pertussis was diagnosed in Lyon, France [15]. A three-week-old neonate with severe pertussis was treated repeatedly with macrolides before the detection of the resistant isolate. Of the three serial isolates from the patient, the first two were sensitive, but the third one turned to be resistant, suggesting that the B. pertussis isolate acquired the mutation leading to macrolide resistance during the macrolide treatment. Sporadic cases of macrolide-resistant B. pertussis isolates were also reported from Iran in 2009 [16].
Figure 1.
Countries where B. pertussis antimicrobial susceptibility studies have been performed (created with MapChart).
In Asia, studies from Cambodia, Japan, Taiwan and Vietnam have found some macrolide-resistant B. pertussis isolates that seem to be related to resistant strains in mainland China [17,18,19]. In northern Vietnam, of NP swab samples from 184 patients with pertussis diagnosed during 2016–2020, 24 (13.0%) were found to be resistant. In Japan, the first isolation of a macrolide-resistant strain was from a 2-month-old baby in 2018. The MICs of the isolate showed >256 µg/mL for ERY and CHL and >32 µg/mL for AZT. The complete genome sequence of the macrolide resistant B. pertussis strain from Japan has been published [20]. It confirms that the isolate has a homogeneous A2047G mutation in each of the three copies of its 23S rRNA gene and that it belongs to the genotype that is common in Chinese macrolide resistant B. pertussis isolates. The issue of macrolide-resistant B. pertussis is greater and reported in more detail in China than in anywhere else in the world. The first macrolide-resistant isolates from Shandong Province in China were reported in 2011 in two asymptomatic pupils [21]. No macrolide resistance has been detected in historical isolates in China from 2008 or earlier [22,23]. More recent reports show very high prevalence of macrolide resistance among B. pertussis isolates in different parts of China (Table 1).
Table 1.
Global frequencies of macrolide-resistant Bordetella pertussis.
| Country | Region/City | Year | Resistant Isolates Identified (Frequency %) |
Reference |
|---|---|---|---|---|
| Australia | New South Wales, Perth | 1971–2010 | 0/120 (0.0) | [24,25] |
| Cambodia | Whole country | 2017–2020 | 1/71 (1.4) | [19] |
| Canada | Ontario | 2011–2013 | 0/275 (0.0) | [26] |
| China | Xi’an | 2012–2020 | 274/299 (91.6) | [27,28,29,30,31] |
| Shandong | 2011 | 2/2 (100.0) | [21] | |
| Northern | 1970–2014 ** | 91/124 ** (91.9) | [22] | |
| Shanghai | 2016–2017 | 81/141 (57.5) | [32] | |
| Zhejiang | 2016–2020 | 271/381 (71.1) | [33,34,35] | |
| Beijing, Jinan, Nanjing, Shenzhen | 2014–2016 | 292/335 (87.2) | [36] | |
| Midwest | 2012–2015 | 163/167 (97.6) | [37] | |
| Whole country | 1950–2018 | 316/388 (81.4) | [23] | |
| Hunan | 2017–2018 | 27/55 (49.1) | [38] | |
| Shenzhen | 2015–2017 | 51/105 (48.6) | [39] | |
| Whole country | 2017–2019 | 265/311 (85.2) | [40] | |
| Czech republic | Whole country | 1967–2015 | 0/135 (0.0) | [41] |
| Finland | Whole country | 2006–2017 | 0/148 (0.0) | [42] |
| France | Bordeaux & Lyon | 2003 and 2012 | 1/41 (2.4) | [10,11] |
| Iran | Whole country | 2009–2010 | 2/11 (18.2) | [16,43] |
| Italy | Rome | 2012–2015 | 0/18 (0.0) | [44] |
| Japan | Whole country | 2017–2019 | 1/33 (3.0) | [17,19] |
| Taiwan | Whole country | 2003–2007 | 2/76 (2.6) | [19,23] |
| United Kingdom | Whole country | 2001–2009 | 0/582 (0.0) | [45] |
| United States | Colorado, Maryland, Oklahoma, Wisconsin | 1986 | 0/75 (0.0) | [46] |
| Arizona—Yuma County | 1994 | 1/1 (100.0) | [47] | |
| Utah | 1985–1997 | 1/47 (2.1) | [12] | |
| Northern California | 1998–1999 | 0/36 (0.0) | [48] | |
| Phoenix, Oakland *, San Diego | N/A *** | 1/48 (2.1) | [49] | |
| California, New York, Minnesota, Massachusetts, Illinois, Arizona, Georgia | 1994–2000 | 5/1030 **** (0.5) | [13] | |
| Minnesota | 1997–1999 | 1/8 (12.5) | [50] | |
| Vietnam | Hanoi, Ha Nam, Thai Binh | 2016–2020 | 24/184 (13.0) | [18,19] |
* Hill et al. included a control B. pertussis strain, resistant to macrolides. This strain has been isolated in Oakland but not officially published elsewhere. ** Divided into three time periods: 1970s, 2000–2008 and 2013–2014. All isolates (N = 25) collected in 1970–2008 were macrolide sensitive. *** N/A = Not available. **** Notified 5 to 7 days after incubation. Four from Arizona, one from Georgia.
Until recently, macrolide resistance in B. pertussis in China has been associated almost exclusively with the ptxP1 lineage of the bacterium [22,27,29,30,31,32,37]. However, a recent cross-sectional study describes two ptxP3 isolates from eastern China that had acquired the A2047G mutation in their 23S rRNA gene [40]. The ptxP3 lineage is currently the dominating B. pertussis circulating in most of the high-income countries that have switched to acellular pertussis vaccine in recent decades [51,52]. It has been hypothesized that the replacement of the whole-cell pertussis vaccine with co-purified acellular pertussis vaccine in the national immunization programme, the liberal use of macrolides in children with respiratory infections, and high population densities could have contributed to the effective spread of macrolide-resistant B. pertussis in China [53].
4. Mechanisms behind Macrolide Resistance in B. pertussis
Macrolide resistance can be caused by three distinct mechanisms. The most common mechanism, including for B. pertussis, is the A2047G single nucleotide polymorphism (SNP) in the 23S rRNA gene within the domain V [15,28,50]. This is equal to a SNP in position A2058G in E. coli and A2064G in M. pneumoniae [54,55]. The A2047G mutation affects the macrolide binding site in the 23S rRNA component of the 50S ribosomal subunit and prevents macrolides to inhibit the peptide elongation [50]. There are three copies of this gene in the B. pertussis genome. Bartkus et al. showed that the A2047G SNP can be found in one or more of the copies. They suggested that this mutation needs at least two copies for resistance [50]. However, many studies have shown that in most cases, all three copies are mutated among the macrolide-resistant B. pertussis strains [15,27,37].
The second possible cause is the acquisition of the ERY-resistant methylase (erm) gene, which leads to addition of methyl group in the 23S rRNA to block the ERY binding site [37,50]. However, B. pertussis do not possess this gene, which is also shown in a novel study in which 167 clinical isolates were screened to identify the possible inclusion of this gene. However, none of the strains carried such a gene [37]. So far, no studies have found this mechanism to be the cause of macrolide resistance in B. pertussis.
The third proposed mechanism is the expression of MexAB-OprM efflux pump (regulated by the mexAB-oprM operon), which helps the bacteria to regulate the uptake of macrolides. This mechanism excretes macrolide molecules out of the bacterial cell. The mechanism has been well-described and has been shown to cause resistance against many antimicrobial agents, including macrolides, in Pseudomonas aeruginosa [56]. Lately, Fong et al. described the expression of the mexAB-oprM operon within macrolide-resistant Bordetella parapertussis. Furthermore, they showed upregulation of the mexAB-oprM when B. parapertussis was grown in 256 mg/mL of ERY. As no other mechanism was found to cause the resistance, they speculated on the potential effect of this mechanism to cause the resistance. However, they also showed that this operon was not functional in B. pertussis due to deletions in mexA and oprM genes [57]. Whether there will be B. pertussis with functional mexAB-oprM operon remains to be seen.
There have only been two reports (Iran and China) where the A2047G SNP has not been the mechanism behind the macrolide resistance in B. pertussis [22,43]. However, these two studies did not perform erm gene or mexAB-oprM operon identification, and the reason for the resistance remains unknown. In the study by Mirzaei et al., the macrolide-resistant isolate was resistant to ERY/CHL but not to AZT [43]. Therefore, the presence of erm could be the cause of the resistance in these studies and would be the first one detected among macrolide-resistant B. pertussis.
5. Methods to Detect Macrolide Resistant B. pertussis
Antimicrobial susceptibility testing can be performed with cultured B. pertussis isolates or with B. pertussis-specific DNA. The first approaches to studying AST were performed by agar and broth dilution series, where plates and liquid medium were prepared with standardised antimicrobial agent concentrations [58,59]. Later, disk diffusion (DD) and MIC Etests were adapted, which made the testing less time consuming and simpler to carry out [12]. Eventually, the lack of cultures performed, and the possibility for the easy detection of SNPs, led to the DNA-based identification of macrolide-resistant B. pertussis [21,50,60]. Here, we briefly describe the AST methods used currently to identify macrolide-resistant B. pertussis.
5.1. Disk Diffusion and Minimum Inhibition Concentration Methods
To perform DD or MIC testing, a confirmed B. pertussis culture is needed. So far, there are no cut-offs for either of the previous methods recommended by EUCAST, and all determinations for sensitivity or resistance are based on notifications from clinical studies. For both DD and MIC testing, bacterial suspension equivalent to McFarland (McF) standard 0.5 is inoculated on selected culture plates. RL and BG agar plates are used in many studies with 0.5 McF [12,42,49,50]. In addition, Muller–Hinton agar supplemented with blood (HMB) have been used, although studies have shown that 8 McF is needed for confluent growth on this medium [42,45]. For DD testing, an antimicrobial agent disk (ERY, AZT, CHL, clindamycin (CLI)) is placed on the plate, and the disk diffusion zone is measured. Results from the studies performing DD vary, and different intervals have been used for plate read-outs. In general, the DD zone for ERY-susceptible strains varies between 37 and 60 mm, whereas for resistant strains, it is 6mm (reflecting the diagonal of the disk) [12,38,49,59,61]. The DD zone is also affected by the incubation time. Longer incubation leads mostly to an increase in the zone diameter [59]. In general, DD tests are no longer that widely used, and there has been criticism over the reliability of this testing method as the results are not reproducible, have low sensitivity and do not correlate with good clinical outcomes [8,38,62].
The MIC testing is more commonly performed than DD tests. After the Etest (slides with increasing antimicrobial agent concentrations) became available and were evaluated, they more or less replaced the plate dilution methods [49]. The method is simple to perform. After the addition of 0.5 McF B. pertussis suspension on a culture plate, an Etest slide is added in the middle of the plate. After 2–5 days, sensitivity to the selected antimicrobial agent can be interpreted as the point where bacterial growth is in touch with the test strip. Figure 2 shows antimicrobial susceptibility testing of B. pertussis to ERY (Etests for AZT similar to ERY) on RL charcoal agar with inoculation density equivalent to a 0.5 McFarland standard.
Figure 2.
Etest of B. pertussis on Regan–Lowe charcoal agar with inoculation density equivalent of 0.5 McFarland standard. (1) = erythromycin resistant B. pertussis and (2) = erythromycin sensitive B. pertussis.
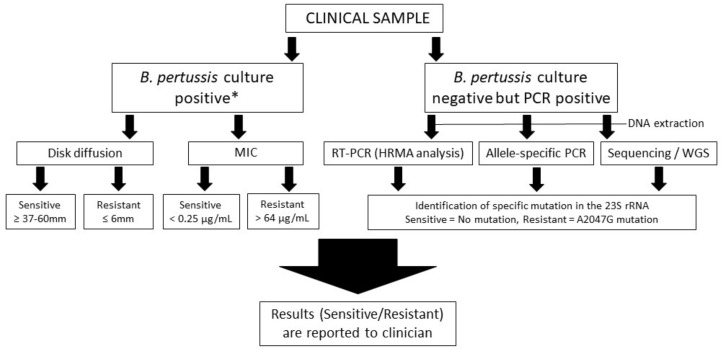
For B. pertussis, several studies have been performed for MICs against antimicrobials (ERY, AZT, CHL, CLI). These tests have been quite consistent with the findings. For sensitive strains, MIC has varied from <0.016 to 0.25 µg/mL, whereas nearly all resistant strains have MIC >256 µg/mL [28,31,32,38,42,63]. However, one study in Iran described an isolate that was resistant to ERY (128 µg/mL) and CHL (>256 µg/mL) but not to AZT (<0.06 µg/mL). Furthermore, the authors did not identify the A2047G mutation in this strain as previously described [43]. In addition, Hill et al. and Korgenski et al. described the first two identified macrolide-resistant B. pertussis in the USA (Arizona and California) to have an MIC of 64 µg/mL for ERY [12,49]. A flow chart of how to identify macrolide-resistant B. pertussis is presented in Figure 3. For B. pertussis culture-positive samples, the nucleic acid amplification indicated in the flow chart should be also used for rapid identification of possible A2047G mutation of 23S rRNA.
Figure 3.
A flow chart of sample processing to detect macrolide-resistant B. pertussis. * The A2047G mutation can also be detected from the culture-positive clinical samples by DNA extraction and following the procedure for B. pertussis culture-negative but PCR-positive scheme.
5.2. DNA-Based Identification of A2047G Mutation in the 23S rRNA
There are different approaches to detecting the A2047G mutation. One method is based on the amplification of a 521 bp fraction of the 23S rRNA gene by PCR and its cleavage with BbsI restriction enzyme. This results in two separate fragments (393 bp and 128 bp) for resistant isolates and one fragment (521 bp) for sensitive isolates when imaged on a gel [15,27,50]. Another option is the Sanger sequencing of the amplification product to detect the specific A2047G SNP [27,36,50]. However, short-read Sanger sequencing cannot differentiate the three copies of the 23S rRNA gene; long-read sequencing is needed to confirm the number of mutations in the three copies [57]. In addition, whole-genome sequencing (WGS) can be used, but so far, no studies are relying on this method as a sole approach to detecting macrolide-resistant B. pertussis. In 2015, Wang et al. introduced an allele-specific PCR to detect the A2047G SNP [60]. In this method, specific primers with small modifications are used to produce either one or two bands after amplification when imaged on a gel. Two bands mark resistance and one band susceptibility of the studied B. pertussis isolates. Zhang et al. published another approach based on qPCR high-resolution melting analysis (HRMA) [21]. In this method, the A2047G mutation is identified by the difference in the HRMA melting temperatures of the amplified PCR products. To enhance the HRMA difference, DNA samples were spiked with wild-type DNA. However, the method was only performed with extracted DNA from cultured B. pertussis, and its usability among DNA extracted from NP samples needs further evaluation. In general, the above-described methods are currently widely used, especially in China, where most of the macrolide-resistant B. pertussis isolates have appeared [28,40,53].
6. Conclusions and Perspective
Macrolide antibiotics are the mainstay of both the treatment and prevention of pertussis [2]. Traditionally, ERY has been the most-used macrolide to treat pertussis. It has been shown in a randomized controlled trial that 7 days of erythromycin is adequate to eradicate B. pertussis from the nasopharynx [64]. More recently, AZT has replaced ERY as the drug of choice for pertussis, due to being as effective, having higher compliance and causing fewer side effects [65]. Early macrolide treatment has shown to be associated with shorter durations of symptoms, shorter periods of being able to transmit and decreased mortality from pertussis in young infants [66,67,68,69]. Macrolides have been recommended as the first-line therapy for all age groups. The second-line treatment option is sulphamethoxazole/trimethoprim (SMZ-TMP), but because of the potentially severe side effects, it is not recommended for the treatment of the youngest infants <2 months of age.
The emergence of macrolide resistance has raised new questions regarding the optimal treatment of young infants with infection caused by macrolide-resistant B. pertussis. In vitro, several classes of antibiotics seem to be effective against B. pertussis, including SMZ-TMP, levofloxacin, ampicillin, 3rd-generation cephalosporins, gentamicin and piperacillin-tazobactam [17,34,38,40,46,63]. However, no data regarding clinical benefit of these antibiotics in infants with severe pertussis caused by a macrolide-resistant strain exist. Clinical treatment failure with macrolides in patients with pertussis caused by resistant strains has seldom been documented.
In two novel studies, piperacillin and cefoperazone-sulbactam were shown to be effective for killing B. pertussis both in vitro and in vivo, providing good options for alternative treatment in hospitalized infants if an isolate is identified to be macrolide resistant, although their suitability for young infants still needs to be better studied [34,35]. As stated in the study by Hua et al. [33], a controlled clinical trial including more pertussis patients to be treated with single piperacillin, cefoperazone or other antibiotics is scheduled in Zhejiang, China. The use of alternative therapy for pertussis other than macrolide in outpatients needs clinical studies.
For the future, it is also worth speculating how the use of co-purified acellular pertussis vaccines versus separately purified acellular pertussis vaccines and changes in the overall use of macrolide antibiotics and population density might affect the epidemiology of macrolide-resistant B. pertussis and whether these issues could be targeted to combat the spread of resistant strains. Novel vaccines, such as live attenuated nasal vaccine, that would produce more sterilizing mucosal immunity could also help to address the issue of antibiotic resistance in pertussis [70,71].
So far, the only mechanism identified to cause macrolide resistance has been a point mutation at position 2047 (A2047G) in domain V of the 23S rRNA gene of B. pertussis. Therefore, simple methods for the rapid identification of this mutation in clinical microbiology laboratories will provide important help for clinicians to use proper antimicrobials for (prophylactic) treatment of patients, especially young infants. These direct typing methods are even more crucial in the future because culture is less and less used for diagnosis of pertussis. The macrolide resistance of B. pertussis has not yet been of clinical concern outside mainland China. However, efforts to increase awareness, guide national/international surveillance and implement systematic screening of B. pertussis-positive samples are highly recommended. At the same time, practices for the best possible clinical care of infants with pertussis caused by resistant strains should be studied.
Author Contributions
All authors (L.I., A.-M.B., J.M. and Q.H.) contributed to the literature review process and writing the original draft preparation, review and editing. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was partly funded by InFLAMES Flagship Programme of the Academy of Finland (decision number: 337530), Tampere Tuberculosis Foundation (Grant number: 26005475) and The Foundation for Paediatric Research [LI]. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yeung K.H.T., Duclos P., Nelson E.A.S., Hutubessy R.C.W. An Update of the Global Burden of Pertussis in Children Younger than 5 Years: A Modelling Study. Lancet Infect. Dis. 2017;17:974–980. doi: 10.1016/S1473-3099(17)30390-0. [DOI] [PubMed] [Google Scholar]
- 2.Kimberlin D.W., Barnett E.D., Lynfield R., Sawyer M.H., editors. Red Book: 2021 Report of the Committee on Infectious Diseases. American Academy of Pediatrics (AAP); Itasca, IL, USA: 2021. Pertussis (Whooping Cough) pp. 578–589. [Google Scholar]
- 3.Bass J.W., Crast F.W., Kotheimer J.B., Mitchell I.A. Susceptibility of Bordetella Pertussis to Nine Antimicrobial Agents. Am. J. Dis. Child. 1969;117:276–280. doi: 10.1001/archpedi.1969.02100030278004. [DOI] [PubMed] [Google Scholar]
- 4.Hardy D.J., Hensey D.M., Beyer J.M., Vojtko C., McDonald E.J., Fernandes P.B. Comparative in Vitro Activities of New 14-, 15-, and 16-Membered Macrolides. Antimicrob. Agents Chemother. 1988;32:1710–1719. doi: 10.1128/AAC.32.11.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tiwari T., Murphy T.V., Moran J. Recommended Antimicrobial Agents for the Treatment and Postexposure Prophylaxis of Pertussis: 2005 CDC Guidelines. MMWR Recomm. Rep. 2005;54:1–16. [PubMed] [Google Scholar]
- 6.Carbonetti N.H. Bordetella Pertussis: New Concepts in Pathogenesis and Treatment. Curr. Opin. Infect. Dis. 2016;29:287–294. doi: 10.1097/QCO.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewis K., Saubolle M.A., Tenover F.C., Rudinsky M.F., Barbour S.D., Cherry J.D. Pertussis Caused by an Erythromycin-Resistant Strain of Bordetella Pertussis. Pediatr. Infect. Dis. J. 1995;14:388–391. doi: 10.1097/00006454-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Wirsing Von König C.H. Pertussis Diagnostics: Overview and Impact of Immunization. Expert Rev. Vaccines. 2014;13:1167–1174. doi: 10.1586/14760584.2014.950237. [DOI] [PubMed] [Google Scholar]
- 9.Zintgraff J., Irazu L., Lara C.S., Rodriguez M., Santos M. The Classical Bordetella Species and MALDI-TOF Technology: A Brief Experience. J. Med. Microbiol. 2018;67:1737–1742. doi: 10.1099/jmm.0.000860. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organisation (WHO) Laboratory Manual for the Diagnosis of Whooping Cough Caused by Bordetella Pertussis/Bordetella Parapertussis. Update 2014. World Health Organisation (WHO); Geneva, Switzerland: 2014. [Google Scholar]
- 11.Guiso N., Liese J., Plotkin S. The Global Pertussis Initiative: Meeting Report from the Fourth Regional Roundtable Meeting, France, April 14–15, 2010. Hum. Vaccin. 2011;7:481–488. doi: 10.4161/hv.7.4.14528. [DOI] [PubMed] [Google Scholar]
- 12.Korgenski E.K., Daly J.A. Surveillance and Detection of Erythromycin Resistance in Bordetella Pertussis Isolates Recovered from a Pediatric Population in the Intermountain West Region of the United States. J. Clin. Microbiol. 1997;35:2989–2991. doi: 10.1128/jcm.35.11.2989-2991.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson K.E., Cassiday P.K., Popovic T., Sanden G.N. Bordetella Pertussis Isolates with a Heterogeneous Phenotype for Erythromycin Resistance. J. Clin. Microbiol. 2002;40:2942–2944. doi: 10.1128/JCM.40.8.2942-2944.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bourgeois N., Ghnassia J.C., Doucet-Populaire F. In Vitro Activity of Fluoroquinolones against Erythromycin-Susceptible and -Resistant Bordetella Pertussis. J. Antimicrob. Chemother. 2003;51:742–743. doi: 10.1093/jac/dkg145. [DOI] [PubMed] [Google Scholar]
- 15.Guillot S., Descours G., Gillet Y., Etienne J., Floret D., Guiso N. Macrolide-Resistant Bordetella Pertussis Infection in Newborn Girl, France. Emerg. Infect. Dis. 2012;18:966. doi: 10.3201/eid1806.120091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahcheraghi F., Lotfi M.N., Nikbin V.S., Shooraj F., Azizian R., Parzadeh M., Torkaman M.R.A., Zahraei S.M. The First Macrolide-Resistant Bordetella Pertussis Strains Isolated From Iranian Patients. Jundishapur J. Microbiol. 2014;7:10880. doi: 10.5812/jjm.10880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamaguchi T., Kawasaki Y., Katsukawa C., Kawahara R., Kawatsu K. The First Report of Macrolide-Resistant Bordetella Pertussis Isolation in Japan. Jpn. J. Infect. Dis. 2020;73:361–362. doi: 10.7883/yoken.JJID.2019.421. [DOI] [PubMed] [Google Scholar]
- 18.Kamachi K., Duong H.T., Dang A.D., Do H.T., Koide K., Otsuka N., Shibayama K., Hoang H.T.T. Macrolide-Resistant Bordetella Pertussis, Vietnam, 2016−2017. Emerg. Infect. Dis. 2020;26:2511–2513. doi: 10.3201/eid2610.201035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koide K., Yao S., Chiang C., Thuy P.T.B., Nga D.T.T., Huong D.T., Dien T.M., Vichit O., Vutthikol Y., Sovannara S., et al. Genotyping and Macrolide-Resistant Mutation of Bordetella Pertussis in East and South-East Asia. J. Glob. Antimicrob. Resist. 2022;31:263–269. doi: 10.1016/j.jgar.2022.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koide K., Yamaguchi T., Katsukawa C., Otsuka N., Kenri T., Kamachi K. Complete Genome Sequence of a Macrolide-Resistant Bordetella Pertussis Isolated in Japan. Microbiol. Resour. Announc. 2022;11:e00718-22. doi: 10.1128/mra.00718-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Q., Li M., Wang L., Xin T., He Q. High-Resolution Melting Analysis for the Detection of Two Erythromycin-Resistant Bordetella Pertussis Strains Carried by Healthy Schoolchildren in China. Clin. Microbiol. Infect. 2013;19:E260–E262. doi: 10.1111/1469-0691.12161. [DOI] [PubMed] [Google Scholar]
- 22.Yang Y., Yao K., Ma X., Shi W., Yuan L., Yang Y. Variation in Bordetella Pertussis Susceptibility to Erythromycin and Virulence-Related Genotype Changes in China (1970–2014) PLoS ONE. 2015;10:e0138941. doi: 10.1371/journal.pone.0138941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yao K., Deng J., Ma X., Dai W., Chen Q., Zhou K., Ye J., Shi W., Wang H., Li D., et al. The Epidemic of Erythromycin-Resistant Bordetella Pertussis with Limited Genome Variation Associated with Pertussis Resurgence in China. Expert Rev. Vaccines. 2020;19:1093–1099. doi: 10.1080/14760584.2020.1831916. [DOI] [PubMed] [Google Scholar]
- 24.Sintchenko V., Brown M., Gilbert G.L. Is Bordetella Pertussis Susceptibility to Erythromycin Changing? MIC Trends among Australian Isolates 1971–2006. J. Antimicrob. Chemother. 2007;60:1178–1179. doi: 10.1093/jac/dkm343. [DOI] [PubMed] [Google Scholar]
- 25.Dorji D., Graham R.M., Richmond P., Keil A., Mukkur T.K. Biofilm Forming Potential and Antimicrobial Susceptibility of Newly Emerged Western Australian Bordetella Pertussis Clinical Isolates. Biofouling. 2016;32:1141–1152. doi: 10.1080/08927014.2016.1232715. [DOI] [PubMed] [Google Scholar]
- 26.Marchand-Austin A., Memari N., Patel S.N., Tang P., Deeks S.L., Jamieson F.B., Crowcroft N.S., Farrell D.J. Surveillance of Antimicrobial Resistance in Contemporary Clinical Isolates of Bordetella Pertussis in Ontario, Canada. Int. J. Antimicrob. Agents. 2014;44:82–84. doi: 10.1016/j.ijantimicag.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Wang Z., Li Y., Hou T., Liu X., Liu Y., Yu T., Chen Z., Gao Y., Li H., He Q. Appearance of Macrolide-Resistant Bordetella Pertussis Strains in China. Antimicrob. Agents Chemother. 2013;57:5193–5194. doi: 10.1128/AAC.01081-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Z., Cui Z., Li Y., Hou T., Liu X., Xi Y., Liu Y., Li H., He Q. High Prevalence of Erythromycin-Resistant Bordetella Pertussis in Xi’an, China. Clin. Microbiol. Infect. 2014;20:O825–O830. doi: 10.1111/1469-0691.12671. [DOI] [PubMed] [Google Scholar]
- 29.Wang Z., Luan Y., Du Q., Shu C., Peng X., Wei H., Hou T., Liu Y., Liu X., Li Y. The Global Prevalence PtxP3 Lineage of Bordetella Pertussis Was Rare in Young Children with the Co-Purified APV Vaccination: A 5 Years Retrospective Study. BMC Infect. Dis. 2020;20:615. doi: 10.1186/s12879-020-05332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu X., Wang Z., Zhang J., Li F., Luan Y., Li H., Li Y., He Q. Pertussis Outbreak in a Primary School in China: Infection and Transmission of the Macrolide-Resistant Bordetella Pertussis. Pediatr. Infect. Dis. J. 2018;37:E145–E148. doi: 10.1097/INF.0000000000001814. [DOI] [PubMed] [Google Scholar]
- 31.Zhang J., Zhang D., Wang X., Wei X., Li H. Macrolide Susceptibility and Molecular Characteristics of Bordetella Pertussis. J. Int. Med. Res. 2022;50:03000605221078782. doi: 10.1177/03000605221078782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fu P., Wang C., Tian H., Kang Z., Zeng M. Bordetella Pertussis Infection in Infants and Young Children in Shanghai, China, 2016-2017: Clinical Features, Genotype Variations of Antigenic Genes and Macrolides Resistance. Pediatr. Infect. Dis. J. 2019;38:370–376. doi: 10.1097/INF.0000000000002160. [DOI] [PubMed] [Google Scholar]
- 33.Hua C.Z., Wang H.J., Zhang Z., Tao X.F., Li J.P., Mi Y.M., Tang L.F., Chen Z.M. In Vitro Activity and Clinical Efficacy of Macrolides, Cefoperazone-Sulbactam and Piperacillin/Piperacillin-Tazobactam against Bordetella Pertussis and the Clinical Manifestations in Pertussis Patients Due to These Isolates: A Single-Centre Study in Zheji. J. Glob. Antimicrob. Resist. 2019;18:47–51. doi: 10.1016/j.jgar.2019.01.029. [DOI] [PubMed] [Google Scholar]
- 34.Mi Y.M., Hua C.Z., Fang C., Liu J.J., Xie Y.P., Lin L.N., Wang G.L. Effect of Macrolides and β-Lactams on Clearance of Bordetella Pertussis in the Nasopharynx in Children with Whooping Cough. Pediatr. Infect. Dis. J. 2021;40:87–90. doi: 10.1097/INF.0000000000002911. [DOI] [PubMed] [Google Scholar]
- 35.Lin L.-N., Zhou J.-S., Hua C.-Z., Bai G.-N., Mi Y.-M., Zhou M.-M. Epidemiological and Clinical Characteristics of Pertussis in Children and Their Close Contacts in Households: A Cross-Sectional Survey in Zhejiang Province, China. Front. Pediatr. 2022;10:1442. doi: 10.3389/fped.2022.976796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li L., Deng J., Ma X., Zhou K., Meng Q., Yuan L., Shi W., Wang Q., Li Y., Yao K. High Prevalence of Macrolide-Resistant Bordetella Pertussis and PtxP1 Genotype, Mainland China, 2014–2016. Emerg. Infect. Dis. 2019;25:2205–2214. doi: 10.3201/eid2512.181836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu Z., Wang Z., Luan Y., Li Y., Liu X., Peng X., Octavia S., Payne M., Lan R. Genomic Epidemiology of Erythromycin-Resistant Bordetella Pertussis in China. Emerg. Microbes Infect. 2019;8:461–470. doi: 10.1080/22221751.2019.1587315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin X.J., Zou J., Yao K., Li L., Zhong L. Analysis of Antibiotic Sensitivity and Resistance Genes of Bordetella Pertussis in Chinese Children. Medicine. 2021;100:e24090. doi: 10.1097/MD.0000000000024090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tian S., Hu N., Lou J., Chen K., Kang X., Xiang Z., Chen H., Wang D., Liu N., Liu D., et al. Characteristics of COVID-19 Infection in Beijing. J. Infect. 2020;80:401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu X., Du Q., Li D., Yuan L., Meng Q., Fu Z., Xu H., Yao K., Zhao R. A Cross-Sectional Study Revealing the Emergence of Erythromycin-Resistant Bordetella Pertussis Carrying PtxP3 Alleles in China. Front. Microbiol. 2022;13:2504. doi: 10.3389/fmicb.2022.901617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jakubů V., Zavadilová J., Fabiánová K., Urbášková P. Trends in the Minimum Inhibitory Concentrations of Erythromycin, Clarithromycin, Azithromycin, Ciprofloxacin, and Trimethoprim/Sulfamethoxazole for Strains of Bordetella Pertussis Isolated in the Czech Republic in 1967–2015. Cent. Eur. J. Public Health. 2017;25:282–286. doi: 10.21101/cejph.a4948. [DOI] [PubMed] [Google Scholar]
- 42.Lönnqvist E., Barkoff A.M., Mertsola J., He Q. Antimicrobial Susceptibility Testing of Finnish Bordetella Pertussis Isolates Collected during 2006–2017. J. Glob. Antimicrob. Resist. 2018;14:12–16. doi: 10.1016/j.jgar.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 43.Mirzaei B., Bameri Z., Babaei R., Shahcheraghi F. Isolation of High Level Macrolide Resistant Bordetella Pertussis without Transition Mutation at Domain V in Iran. Jundishapur J. Microbiol. 2015;8:18190. doi: 10.5812/jjm.8(5)2015.18190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stefanelli P., Buttinelli G., Vacca P., Tozzi A.E., Midulla F., Carsetti R., Fedele G., Villani A., Concato C., Carannante A., et al. Severe Pertussis Infection in Infants Less than 6 Months of Age: Clinical Manifestations and Molecular Characterization. Hum. Vaccines Immunother. 2017;13:1073–1077. doi: 10.1080/21645515.2016.1276139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fry N.K., Duncan J., Vaghji L., George R.C., Harrison T.G. Antimicrobial Susceptibility Testing of Historical and Recent Clinical Isolates of Bordetella Pertussis in the United Kingdom Using the Etest Method. Eur. J. Clin. Microbiol. Infect. Dis. 2010;29:1183–1185. doi: 10.1007/s10096-010-0976-1. [DOI] [PubMed] [Google Scholar]
- 46.Kurzynski T.A., Boehm D.M., Rott-Petri J.A., Schell R.F., Allison P.E. Antimicrobial Susceptibilities of Bordetella Species Isolated in a Multicenter Pertussis Surveillance Project. Antimicrob. Agents Chemother. 1988;32:137–140. doi: 10.1128/AAC.32.1.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (CDC) Erythromycin-Resistant Bordetella Pertussis—Yuma County, Arizona, May–October 1994. MMWR Morb. Mortal. Wkly. Rep. 1994;43:807–810. [PubMed] [Google Scholar]
- 48.Gordon K.A., Fusco J., Biedenbach D.J., Pfaller M.A., Jones R.N. Antimicrobial Susceptibility Testing of Clinical Isolates of Bordetella Pertussis from Northern California: Report from the SENTRY Antimicrobial Surveillance Program. Antimicrob. Agents Chemother. 2001;45:3599–3600. doi: 10.1128/AAC.45.12.3599-3600.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hill B.C., Baker C.N., Tenover F.C. A Simplified Method for Testing Bordetella Pertussisfor Resistance to Erythromycin and Other Antimicrobial Agents. J. Clin. Microbiol. 2000;38:1151–1155. doi: 10.1128/JCM.38.3.1151-1155.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bartkus J.M., Juni B.A., Ehresmann K., Miller C.A., Sanden G.N., Cassiday P.K., Saubolle M., Lee B., Long J., Harrison A.R., et al. Identification of a Mutation Associated with Erythromycin Resistance in Bordetella Pertussis: Implications for Surveillance of Antimicrobial Resistance. J. Clin. Microbiol. 2003;41:1167–1172. doi: 10.1128/JCM.41.3.1167-1172.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barkoff A.M., Mertsola J., Pierard D., Dalby T., Hoegh S.V., Guillot S., Stefanelli P., Van Gent M., Berbers G., Vestrheim D.F., et al. Surveillance of Circulating Bordetella Pertussis Strains in Europe during 1998 to 2015. J. Clin. Microbiol. 2018;56:e01998-17. doi: 10.1128/JCM.01998-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bowden K.E., Williams M.M., Cassiday P.K., Milton A., Pawloski L., Harrison M., Martin S.W., Meyer S., Qin X., DeBolt C., et al. Molecular Epidemiology of the Pertussis Epidemic in Washington State in 2012. J. Clin. Microbiol. 2014;52:3549–3557. doi: 10.1128/JCM.01189-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feng Y., Chiu C.H., Heininger U., Hozbor D.F., Tan T.Q., von König C.H.W. Emerging Macrolide Resistance in Bordetella Pertussis in Mainland China: Findings and Warning from the Global Pertussis Initiative. Lancet Reg. Health West. Pac. 2021;8:100098. doi: 10.1016/j.lanwpc.2021.100098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morozumi M., Hasegawa K., Kobayashi R., Inoue N., Iwata S., Kuroki H., Kawamura N., Nakayama E., Tajima T., Shimizu K., et al. Emergence of Macrolide-Resistant Mycoplasma Pneumoniae with a 23S RRNA Gene Mutation. Antimicrob. Agents Chemother. 2005;49:2302–2306. doi: 10.1128/AAC.49.6.2302-2306.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weisblum B. Erythromycin Resistance by Ribosome Modification. Antimicrob. Agents Chemother. 1995;39:577–585. doi: 10.1128/AAC.39.3.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pesingi P.V., Singh B.R., Pesingi P.K., Bhardwaj M., Singh S.V., Kumawat M., Sinha D.K., Gandham R.K. MexAB-OprM Efflux Pump of Pseudomonas Aeruginosa Offers Resistance to Carvacrol: A Herbal Antimicrobial Agent. Front. Microbiol. 2019;10:2664. doi: 10.3389/fmicb.2019.02664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fong W., Timms V., Sim E., Pey K., Nguyen T., Sintchenko V. Genomic and Transcriptomic Variation in Bordetella spp. Following Induction of Erythromycin Resistance. J. Antimicrob. Chemother. 2022;77:3016–3025. doi: 10.1093/jac/dkac272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hardy E., Pupo E., Santana H., Guerra M., Castellanos-Serra L.R. Elution of Lipopolysaccharides from Polyacrylamide Gels. Anal. Biochem. 1998;259:162–165. doi: 10.1006/abio.1998.2603. [DOI] [PubMed] [Google Scholar]
- 59.Cimolai N., Zaher A., Trombley C. Correlation of Erythromycin Agar Dilution Susceptibility Testing with Disc Diffusion Susceptibility for Bordetella Pertussis. Int. J. Antimicrob. Agents. 1997;9:113–116. doi: 10.1016/S0924-8579(97)00032-0. [DOI] [PubMed] [Google Scholar]
- 60.Wang Z., Han R., Liu Y., Du Q., Liu J., Ma C., Li H., He Q., Yan Y. Direct Detection of Erythromycin-Resistant Bordetella Pertussis in Clinical Specimens by PCR. J. Clin. Microbiol. 2015;53:3418–3422. doi: 10.1128/JCM.01499-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cassiday P.K., Tobin-D’Angelo M., Watson J.R., Wu K.H., Park M.M., Sanden G.N. Co-Infection with Two Different Strains of Bordetella Pertussis in an Infant. J. Med. Microbiol. 2008;57:388–391. doi: 10.1099/jmm.0.47602-0. [DOI] [PubMed] [Google Scholar]
- 62.Cimolai N. Pharmacotherapy for Bordetella Pertussis Infection. I. A Synthesis of Laboratory Sciences. Int. J. Antimicrob. Agents. 2021;57:106258. doi: 10.1016/j.ijantimicag.2020.106258. [DOI] [PubMed] [Google Scholar]
- 63.Yao S.M., Liaw G.J., Chen Y.Y., Yen M.H., Chen Y.H., Mu J.J., Chiang C.S. Antimicrobial Susceptibility Testing of Bordetella Pertussis in Taiwan Prompted by a Case of Pertussis in a Paediatric Patient. J. Med. Microbiol. 2008;57:1577–1580. doi: 10.1099/jmm.0.2008/002857-0. [DOI] [PubMed] [Google Scholar]
- 64.Halperin S.A., Bortolussi R., Langley J.M., Miller B., Eastwood B.J. Seven Days of Erythromycin Estolate Is as Effective as Fourteen Days for the Treatment of Bordetella Pertussis Infections. Pediatrics. 1997;100:65–71. doi: 10.1542/peds.100.1.65. [DOI] [PubMed] [Google Scholar]
- 65.Langley J.M., Halperin S.A., Boucher F.D., Smith B. Azithromycin Is as Effective as and Better Tolerated than Erythromycin Estolate for the Treatment of Pertussis. Pediatrics. 2004;114:e96–e101. doi: 10.1542/peds.114.1.e96. [DOI] [PubMed] [Google Scholar]
- 66.Carlsson R.M., von Segebaden K., Bergström J., Kling A.M., Nilsson L. Surveillance of Infant Pertussis in Sweden 1998–2012; Severity of Disease in Relation to the National Vaccination Programme. Eurosurveillance. 2015;20:21032. doi: 10.2807/1560-7917.ES2015.20.6.21032. [DOI] [PubMed] [Google Scholar]
- 67.Winter K., Harriman K., Zipprich J., Schechter R., Talarico J., Watt J., Chavez G. California Pertussis Epidemic, 2010. J. Pediatr. 2012;161:1091–1096. doi: 10.1016/j.jpeds.2012.05.041. [DOI] [PubMed] [Google Scholar]
- 68.Bortolussi R., Miller B., Ledwith M., Halperin S. Clinical Course of Pertussis in Immunized Children. Pediatr. Infect. Dis. J. 1995;14:870–874. doi: 10.1097/00006454-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 69.Kwantes B.W., Joynson D.H.M., Williams W.O. Bordetella Pertussis Isolation in General Practice: 1977–79 Whooping Cough Epidemic in West Glamorgan. J. Hyg. 1983;90:149. doi: 10.1017/S0022172400028825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jahnmatz M., Richert L., al-Tawil N., Storsaeter J., Colin C., Bauduin C., Thalen M., Solovay K., Rubin K., Mielcarek N., et al. Safety and Immunogenicity of the Live Attenuated Intranasal Pertussis Vaccine BPZE1: A Phase 1b, Double-Blind, Randomised, Placebo-Controlled Dose-Escalation Study. Lancet Infect. Dis. 2020;20:1290–1301. doi: 10.1016/S1473-3099(20)30274-7. [DOI] [PubMed] [Google Scholar]
- 71.Damron F.H., Barbier M., Dubey P., Edwards K.M., Gu X.-X., Klein N.P., Lu K., Mills K.H.G., Pasetti M.F., Read R.C., et al. Overcoming Waning Immunity in Pertussis Vaccines: Workshop of the National Institute of Allergy and Infectious Diseases. J. Immunol. 2020;205:877–882. doi: 10.4049/jimmunol.2000676. [DOI] [PMC free article] [PubMed] [Google Scholar]