Abstract
In the era of vaccine hesitancy, highlighted by the current SARS-CoV2 pandemic, there is an acute need to develop an approach to reduce and address apprehension towards vaccinations. We sought to map and present an overview of existing educational interventions for healthcare providers (HCPs) on strategies to engage in effective vaccine discussion. We applied the Joanna Briggs Institute methodology framework in this scoping review. We searched five relevant databases (MEDLINE, CINAHL, EMBASE, PsycInfo, and SCOPUS) and grey literature through the Google search engine using keywords and subject headings that were systematically identified. We identified 3384 citations in peer-reviewed literature and 41 citations in grey literature. After screening for our inclusion criteria, we included 28 citations from peer reviewed literature and 16 citations from grey literature for analysis. We identified a total of 41 unique education interventions. Interventions were available from multiple disciplines, training levels, clinical settings, and diseases/vaccines. Interventions predominantly centered around two foci: knowledge sharing and communication training. Most interventions identified from peer-reviewed literature were facilitated and were applied with multiple modes of delivery. Interventions from grey literature were more topical and generally self-directed. We identified several gaps in knowledge. Firstly, accessibility and generalizability of interventions was limited. Secondly, distribution of interventions did not adequately address nursing and pharmacy disciplines, and did not cover the breadth of medical specialties for whom vaccine discussions apply. Thirdly, no interventions addressed self monitoring and the clinicians’ recognition and management of emotions during difficult conversations. There is a need to address this gap and provide available, credible and comprehensive educational interventions that will support our healthcare providers in effective communication with vaccine hesitant patients.
Keywords: Communication, Education, Healthcare Providers, Multidisciplinary, Vaccine, Vaccine Hesitancy
1. Introduction
According to the World Health Organization, vaccine hesitancy is one of the top ten threats to global health, along with other major threats such as climate and air pollution, and HIV [80]. Over the past two years, the SARS-COV2 virus has emerged as a worldwide public health threat with devastating impacts globally. Although hard to predict, we can foresee that future pandemics will occur more frequently, spread more rapidly, with increased morbidity and mortality; there is more frequent animal-human interaction due to agricultural progress, climate change and increased land use with population growth resulting in increased risk of pathogen spillover, disease amplification and spread [22]. There is little we can do to control the virulence and transmissibility of a future pathogen or strain with pandemic potential. We can, however, control our ability to mitigate the impact by addressing preventative strategies such as vaccinations [36], [60] . Despite recent advances in vaccine development, an immunization program can only be as effective as its uptake, and public skepticism of vaccination is growing [10]. The definition of vaccine hesitancy varies depending on the context, including the specific vaccine and target population [27]. However in the current context, we define vaccine hesitancy as the behaviours, beliefs about vaccine safety and efficacy, attitudes about mandates, and trust towards vaccines. Recent work recognizes vaccine hesitancy as stemming from people’s experiences with illness, biomedical institutions and interventions and injustice, and their relationship with government and the scientific community [4], [8], [40]. In the era of vaccine hesitancy and pandemic threats, there is an acute need to develop an approach to reduce and address apprehension towards vaccinations [25].
Healthcare providers (HCPs) not only have the unique opportunity to address and educate patients about vaccinations in their respective roles, they are often seen by the public as the most trusted source of information regarding vaccination [52], [62]. Their recommendations continue to hold a significant positive influence in the vaccination decision-making process [63], [79], [89]and the relationship is the cornerstone of vaccine confidence [26]. HCPs cited their attitudes towards vaccination, knowledge of vaccinations and preparedness with adequate training as enabling factors to engage in difficult conversations, especially with those who demonstrate reluctance or hesitancy towards vaccination [66].
Recent systematic reviews have explored the aspects of HCP attitudes and knowledge [48], [49]but we did not identify any reviews that summarized available literature on interventions addressing preparedness in HCPs specifically. Only one scoping review by Karras et al. [44]examined the availability of dialogue-based resources to support HCP, which provided some limited insight on the topic. In a comprehensive systematic review, Dube et al. [26] found that most interventions focused on information sharing and education about vaccination to both HCP and patients alike. Furthermore, one study demonstrated that vaccination-related curriculum content across medicine, nursing and pharmacy training was highly variable, with a median of 12–23 h, where only 21 % of participants felt they received adequate vaccination teaching during training [67]. Content is often focused on vaccination principles [67]and HCP trainees have consistently identified a gap in teaching of communication strategies and practical skills [75], [42].
Enabling HCPs to effectively engage in vaccine discussions therefore must involve providing training in practical skills and communication strategies to enhance provider preparedness, in addition to provision of knowledge and encouraging the acceptance of vaccinations. The discussion of vaccines is a complex interaction requiring verbal and nonverbal communication skills, active listening, recognizing and addressing denialism and engaging in a longitudinal process [24], [64], [90]. In addition, the overall social-emotional competence of the provider [88], emotion regulation after difficult conversations, and self-debriefing techniques [33], [78] have been described as a tenet of effective persuasion.
A recent global survey demonstrates differences in attitudes and acceptance of vaccines by geography and associated contexts including age and sex distribution, income, education and trust in government [46]. Vaccine communication strategies need to take into account local contexts to increase efficacy. Our pragmatic approach, focused on the North American context, recognizes this cultural context of vaccine hesitancy as we aim to identify, explore, and map the literature on existing vaccine hesitancy educational tools for healthcare providers who provide vaccine counseling to patients. In our scoping review, we conducted a grey literature review of North American interventions. We expanded our scope of primary literature to the global context, without geographic limitation. While these interventions may be less applicable to the local context, the rigor of the review process may provide valuable insights that can be extrapolated with respect to methodology and evaluation. The results of this scoping review will identify the gaps in literature and inform the development of a multidisciplinary educational program for healthcare provider trainees to prepare them for their future roles in vaccine advocacy, promotion and delivery.
2. Methods
2.1. Defining the intervention
We conducted a scoping review of peer-reviewed and grey literature to identify, map and present an overview of existing educational interventions within our area of interest and identify gaps for further research. The proposed review was guided by the methodological framework proposed by the Joanna Briggs Institute (JBI) [2]: (i) Defining and aligning the objectives and questions, (ii) Developing and aligning the inclusion criteria with the objectives and questions, (iii) Describing the planned approach to evidence searching, selection, data extraction, and presentation of the evidence, (iv) Searching for the evidence, (v) Selecting the evidence, (vi) Extracting the evidence, (vii) Analyzing of the evidence, (viii) Presenting the results, and (ix) Summarizing the evidence in relation to the purpose of the review. A comprehensive published protocol can be accessed at https://osf.io/jxcrz/. We reported our process according to the PRISMA Extension for Scoping Reviews [82].
2.2. Research question
-
1.What educational tools aimed at addressing vaccine hesitancy are currently available for HCP use in the peer-reviewed and grey literature?
-
a.Within these tools, are there components that address self monitoring and the clinicians’ recognition and management of emotions during difficult conversations?
-
a.
2.3. Search strategy
a. English language peer-reviewed literature.
Key search terms that addressed vaccine hesitancy and a healthcare provider population were applied to an initial exploratory search within two databases (MEDLINE and EMBASE) in order to identify ‘seed’ articles. Retrieved ‘seed’ articles were analyzed for text words and index terms to ensure comprehensiveness. With librarian assistance, we selected five relevant databases to ensure a broad range of disciplines were included: MEDLINE (Ovid MEDLINE(R) ALL), CINAHL (EBSCOhost CINAHL), EMBASE (Embase Classic + Embase), PsycInfo (APA PsycInfo), and SCOPUS. Identified keywords and subject headings were applied to each database in November 2021, with no restriction on language, study design, publication date or country of origin in order to broadly capture all relevant interventions (Supplemental Figure S1). All citations were imported to the systematic-review software Covidence (Veritas Health Innovation, 2014) for title and abstract screening, and removal of duplicates.
b. French language peer-reviewed literature.
The original English strategy was applied to each of the databases with an additional limiter set to filter French literature only, based on consultation from an academic librarian. This ensured consistency with the search strategy while highlighting the French literature for our bilingual author, LB, to review. The results were imported into Covidence and duplicates of the English language search were removed, followed by a manual review to ensure accuracy.
c. Grey literature environmental scan.
A grey literature environmental scan was conducted to examine educational interventions and resources published on the Internet. This secondary search involved 1) reviewing targeted websites of relevant health organizations and agencies based on the recommendations of subject matter experts on the research team, and 2) searching key search terms that addressed vaccine hesitancy and a healthcare provider population using the Google search engine. Data was collected using Microsoft Excel (Microsoft Corporation, 2018). During the searching process, the names of relevant websites/ organizations and URL were recorded. Each of the websites were ‘hand-searched’ or searched using the websites’ search bar/ database for potentially relevant documents (e.g. FAQs, webinars, etc.). Relevant data including a brief resource description were recorded next to the accompanying organization name and were tracked for further screening. The grey literature environmental scan was conducted in November 2021.
2.4. Study selection
a. English language peer-reviewed literature.
The two primary reviewers conducted a pilot screen of a random sample of citations to evaluate inter-user agreement and consistency. Disagreements were resolved through discussion and amendment of inclusion and exclusion criteria until 75 % agreement was achieved (Supplemental Figure S2).
Screening was conducted in accordance with the finalized inclusion and exclusion criteria (Supplemental Table S1). Initial screening of title and abstracts was conducted by AL and MP, and disagreements were resolved through a third reviewer MF. Selected abstracts then underwent full-text screening by AL and MP, and disagreements were resolved through discussion until consensus was achieved. After citation screening and selection, the reference lists of accepted full-text citations were manually screened by AL and MP for additional relevant source citations through the same process.
b. Grey literature environmental scan.
Two members of the research team (MF and HM) conducted the grey literature environmental scan using the Google search engine. A third reviewer MP later conducted the search using the same strategy to ensure that key resources from identified health organizations and agencies were captured as well as any other relevant resources that may have been missed. It is important to note that it is impossible to review and capture all retrieved results due to their volume. Therefore, the reviewers relied on relevancy ranking within Google search engines to sort through webpages to find the most relevant and useful results. Through this process the most relevant results are brought to the top of the search results [38].
MF, HM, and MP reviewed the final list of resources and came to a consensus on which resources should be included or removed based on the inclusion and exclusion criteria (Supplemental Table S1). The list of relevant resources underwent final review by key subject matter experts on the research team (SD, CC). Additionally during this step, all resources found from outside of North America were excluded as the purpose of the grey literature environmental scan was to identify vaccine hesitancy resources in the North American landscape.
2.5. Critical appraisal
In accordance with the JBI scoping review framework, a critical appraisal was not completed.
2.6. Data charting
a. English language peer-reviewed literature.
We developed an extraction tool on Microsoft Excel (Microsoft Corporation, 2018) to comprehensively collect and organize relevant information about each intervention aimed at addressing vaccine hesitancy. Information collected included: study characteristics (design, year and location), target population, intended vaccine (if any), aim(s) of the intervention, details of the intervention (duration, setting, mode and materials), measurements of intervention effectiveness, and whether the intervention addressed emotional capacity and regulation in healthcare providers.
b. Grey literature environmental scan.
Similar to the English language peer-reviewed literature, we developed an extraction tool on Microsoft Excel (Microsoft Corporation, 2018) to organize relevant resources aimed at addressing vaccine hesitancy. Information collected included: document title and organization, year, type of resource (e.g. e-learning module), type of intervention (e.g. mobile app), country of origin, target population, intended vaccine (if any), summary of resource, and measurements of resource effectiveness (if any).
2.7. Data analysis
A comprehensive descriptive analysis was conducted to outline the characteristics of each study and the details of each intervention. Qualitative analysis for emerging themes of self monitoring and management of emotions in HCPs was not conducted as no citation was identified that adequately addressed this element.
3. Results
3.1. Search results and study selection
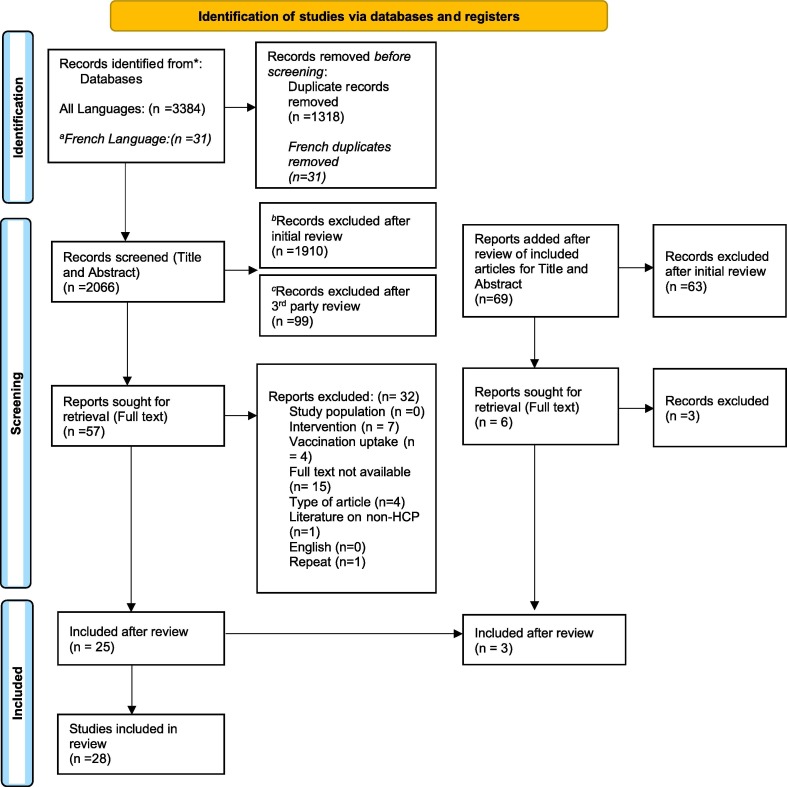
Our search identified a total of 3384 citations in peer-reviewed literature. A dedicated French-language search identified 31 citations, all of which were duplicates of previously identified citations. We screened 2066 citations after removal of duplicates. After a full-text review of 57 citations, we included 25 citations for data extraction. Through manual review of references in included citations, we screened an additional 69 citations, completed full-text review of 6 citations and included an additional 3 citations for data extraction. Therefore, a total of 28 peer-reviewed citations were included (Fig. 1 ).
Fig. 1.
PRISMA Diagram. aA french specific search was conducted, and duplicates were manually reviewed by a bilingual author, b1910 records were excluded as they did not meet the inclusion criteria after initial review. 1132 were excluded for incorrect study population/context, 688 were excluded for lack of intervention, 43 were excluded for lack of discussion of vaccines, 12 were excluded for no full text available, 23 were excluded for type of article, 4 were excluded for non-english articles, 7 were excluded due to repetition, 1 was excluded for literature on non health care providers.c99 records were excluded after a third party reviewer examined records classified as inconclusive by the first two reviewers. 46 were excluded for incorrect study population/context, 41 were excluded for lack of intervention, 8 were excluded for lack of discussion on vaccines, 2 were excluded for the type of article, 1 was excluded due to repetition, 1 was excluded for literature on non health care providers, and 0 were excluded for full text availability and english language.
The grey literature environmental scan initially yielded 43 potential educational interventions and resources for screening. After the screening process, a total of 16 resources that met eligibility criteria remained and were included in the scoping review. These resources were primarily delivered in the form of e-learning modules, presentations, handbooks in the form of reports, and websites.
3.2. Content Summary
We identified a total of 41 unique interventions that were specifically targeted at the HCP population. 26 interventions were identified from the 28 citations found in peer-reviewed literature (P1-P26). Two interventions were evaluated in different manners, resulting in two citations each (P6, P21). 16 interventions were identified through the grey literature environmental scan (G1-G16), with the “The HPV Vaccine: Same Way, Same Day App” identified in both (G1). The grey literature environmental scan identified two resources from academic institutions (G2, G15), nine resources from healthcare provider associations (G3-G4, G8-G10, G12-G14, G16), and five from government health agencies (G1, G5-G7, G11). A summary of identified interventions are provided in Table 1 and Table 2 . Interventions were classified systematically by potential implementation strategies in Supplemental Table S2 and S3 [68].
Table 1.
Summary of interventions identified through the peer-reviewed literature search.
| Identifier | Intervention Title (author, reference number) | Study Setting | Year | Type of Resource | Summary of Resource | Target |
|---|---|---|---|---|---|---|
| Trainees | ||||||
| P1 | Pahud et al. Collaboration for Vaccine Education and Research (CoVER) Curriculum[65] |
Postgraduate Pediatric and Family Medicine Residency Curriculum | 2020 | Online modules and role-play simulation | A curriculum with four asynchronous, interactive online modules (vaccine fundamentals, vaccine preventable diseases, vaccine safety, and vaccine communication strategies) followed by locally implemented face-to-face training over one hour. The curriculum was delivered over a period of 6 months. | Pediatric residents, family residents |
| P2 | Schnaith et al. Human Papillomavirus (HPV) Vaccination Curriculum[76] |
Undergraduate Medical School extracurricular | 2018 | Lecture, video and simulation | A three-part curriculum involving a didactic presentation by a physician on HPV, an educational video on implementing both the presumptive method and the Corroborate, About me, Science, and Explain/advise (C.A.S.E.) method with vaccine hesitant parents, and a simulation role-play with three scenarios. The curriculum was delivered over one day, but the time required was not well described. | Medical students |
| P3 | Barton et al. Announce-Inquire-Mirror-Secure (AIMS) Method for Healthy Conversations[3] |
Postgraduate Residency Curriculum | 2021 | Online modules and physical training | A two-part curriculum with a one-hour online learning module on the principles of vaccinology followed by a one-hour live training session on the AIMS method. The curriculum was delivered over one week. | Pediatric residents |
| P4 | Coleman & Lehman Flipped Classroom and Case-Based Curriculum[18] |
Postgraduate Pediatric Clerkship Curriculum | 2017 | Video podcast, powerpoint slides, in-person workshop | A 90-minute in-class workshop where students, in faculty facilitated groups, work through a case with a scenario and guided questions. The workshop is preceded by an hour-long podcast on vaccine education provided one week prior. | Medical students |
| P5 | Nold & Deem High-fidelity Ethics Simulation Experience[61] |
Baccalaureate Nursing Program Pediatrics Course | 2020 | Assignment, Simulation | A role-play simulation experience scenario involving an encounter with parental vaccine-refusal during a routine pediatric wellness visit, constructed to lead to multiple possible conversational pathways. Prior to the experience, students complete an assignment to familiarize themselves with the patient chart, review the vaccine schedule and plan for the encounter. The curriculum was delivered over one day, but the time required was not well described. | Nursing students |
| P6 | Real et al. Virtual Reality Curriculum[70] |
Postgraduate Pediatric Academic Clinic | 2017 | Virtual Simulation | A 15 min virtual reality simulation delivered through a headset with three simulated scenarios where participants counseled caregiver avatars with vaccine hesitancy. | Pediatric residents |
| Real et al. Virtual Reality Curriculum[71] | ||||||
| P7 | Real et al. The HPV Vaccine: Same Way, Same Day App[72] |
Postgraduate pediatric residency extra-curricular | 2021 | Tablet/Phone application, simulation | An app was designed for pediatricians to improve their HPV vaccine recommendation skills. It consists of an animated video discussing HPV disease epidemiology and evidence-based communication strategies, followed by a role-play select-response virtual simulation scenario with feedback provided by a virtual coach. Time required for this intervention was not described. | Pediatric residents |
| P8 | Vyas et al. Vaccine hesitancy learning unit[88] |
Undergraduate pharmacy curriculum |
2018 | SImulation, video, module | A learning unit with an initial standardized patient simulation encounter followed by feedback, self-reflection and a formal coursework on vaccine hesitancy. The following week, students participated in a second simulated patient encounter. The curriculum was delivered over 90 min each, in a period of 2 weeks. |
Pharmacy students |
| P9 | Vorsters et al. Summer school on vaccinology[87] |
Summer School for Pre-clinical Trainees | 2010 | Interactive teaching, physical training | A 4 day in-person curriculum covering 8 domains of vaccinology, with 75 learning objectives and competences (Rationale, context and history of immunisation, Key aspects of immunology, Key aspects of vaccines, Vaccine-preventable diseases, Immunisation policy and schedules, Future perspectives, Communication, Practical skills). | Pre-service trainees |
| P10 | Visalli et al. Health education intervention to improve vaccination knowledge and attitudes[86] |
Undergraduate Midwifery University Course | 2021 | Provided materials, debate | An educational intervention concerning all aspects of vaccinations (general characteristics, current legislation about mandatory and recommended vaccines, vaccination of particular groups of people including pregnant women) through provided materials and slides, followed by a debate to clarify any remaining concerns. The intervention was delivered over four hours. | Midwifery students |
| P11 | Morhardt et al. Vaccine curriculum to engage vaccine-hesitant families[58] |
Postgraduate pediatric,residency curriculum | 2016 | Slides, video, simulation | A four-part curriculum with a simulated patient encounter with a vaccine-hesitant parent, a series of self-directed lectures on vaccine-preventable illnesses, vaccine safety and administration, personal experience with a family affected by vaccine-preventable illnesses, and communication techniques with role-play opportunities, followed by a second simulated patient encounter. The curriculum was delivered over four hours. | Pediatric residents |
| Non-Trainees | ||||||
| P12 | Cates et al. Protect Them[12] |
Pediatric and family medicine practices | 2020 | Asynchronous online course with gamification | A course designed to increase vaccine knowledge, enhance interpersonal communication skills, and offer systems-level strategies to support vaccination. The course was delivered live for 4 weeks over three waves, and then on-demand for 3 months. | Physicians, nurses, nurse practitioner, other medical staff |
| P13 | Chamberlain et al. VaxChat[15] |
Obstetrical group practices | 2019 | Video tutorial | An hour-long, evidence-based video tutorial with the goal to improve obstetric care providers’ ability to promote maternal vaccines. | Physicians, midwives, nurses, nurse practitioner,medical assistant |
| P14 | Cotugno et al.No name. [19] |
Psychiatric unit | 2017 | Physical training | An intervention given by pharmacists to staff working on a psychiatric unit. Goal was to increase the rate of influenza vaccination through education on influenza, proper vaccine assessment, effective use of electronic medical records, vaccine ordering and procurement. Time required for the intervention was not described. | Pharmacists |
| P15 | Gagneur et al. Motivational Interviewing (MI) Workshop[32] |
Immunisation Public health clinics | 2019 | In-person training workshop | A workshop to increase MI knowledge and MI-skills for nurses to feel confident to apply these to their daily vaccination work routine in clinical practice, especially among vaccine hesitant parents. Workshops were conducted two days, three months apart. 7 h of training on day 1, and 4 h on day two. | Nurses |
| P16 | Glanternik et al. Effective Communication without Confrontation (ECC)[34] |
Clinical sites | 2020 | Presentation, communication training, simulation | A communication training tool that increases comfort level and perceived effectiveness when communicating with vaccine-hesitant parents. Training includes a presentation on communication techniques, interactive role play sessions using non confrontational communication such as motivational interviewing. Time required for this intervention was not described. | Pediatric physicians, family physicians |
| P17 | Lockhart et al. Communication Intervention[50] |
Pediatric and family medicine clinics | 2018 | Provided resources, in-person training | A communication intervention that consisted of a fact sheet library, website for parents called “iVac,” compilation of disease images, parental decision aid, communication training using a presumptive approach and motivational interviewing techniques. Time required for the intervention was not described. | Physicians, physician assistant, nurses |
| P18 | Maurici et al. Consultation and Relational Empathy Measure (CARE) to assess an immunization specific communication course[56] |
Immunization Centres at a local health unit | 2018 | Lectures, simulation | A measure used to assess a three day course about empathy and communication skills to patients in vaccination centers using a family and patient centered care approach (PFCC). The course consisted of 4 sections with each section consisting of a lecture and review of the topic, followed by role-playing and simulations, over three days. | Physicians, nurses |
| P19 | Brewer et al. Train the trainer workshop[6] |
Primary care clinics |
2021 | Videos, in-person training, simulation | A workshop to train providers to communicate about vaccinations more effectively through approaches such as the “Announcement Approach Training” (AAT). The workshop consisted of training a facilitator, followed by the facilitator training and teaching others on AAT. The official AAT workshop consisted of three sections: review evidence, build skills, and practice. The train-the-trainer workshop was 2 h, followed by 1 h of the AAT workshop. | Physicians,physician assistant, nurses, nurse practitioner,medical assistants |
| P20 | Reno et al. 5-component provider communication intervention[74] |
Pediatric and Family Practices | 2018 | Toolkit | A communication training toolkit encouraging providers to initiate a conversation using the presumptive approach, followed by implementation of motivational interviewing (MI) techniques, customized vaccine fact sheets, a set of disease images, a decision aid for parents, an educational tailored-messaging website for parents. Time required for this intervention was not described. | Physicians, physician assistant, nurses, medical assistants |
| P21 | Reno et al. Motivational Interviewing and Communication Techniques[73] |
Pediatric and Family Practices | 2018 | Video, Physical training | An intervention aimed at improving provider communication. Consists of a 40 min background video with key components of the communication style, and specific examples. A 1-hour in person training session focusing on demonstrating the techniques, and another 1- hour in person session that provided feedback on the providers' communication technique and suggestions for improvement. | Physicians, physician assistant, nurses practitioner, doctor of osteopathy |
| Dempsey et al. 5 Component Communication Intervention[23] | ||||||
| P22 | Shen et al. Aspire Framework[77] |
Pharmacies | 2021 | Framework | A 6-step framework that can support pharmacists when communicating with community members who have questions and/or concerns about vaccines. The goal is to increase vaccine uptake in the community. Time required for this intervention was not described. | Pharmacists |
| P23 | Zolezzi et al. OARS method[92] |
Independent | 2021 | Framework | A communication method for pharmacists to use during their daily encounters with patients, specifically for vaccine hesitant individuals. OARS (Open questioning,Affirming, Reflective listening, and Summarizing) . Time required for this intervention was not described. |
Pharmacists |
| P24 | Brewer et al. Presumptive “announcements” or participatory “conversations” Training[5] |
Pediatric and Family Clinic | 2017 | Presentation, communication training, assignment | Training sessions conducted with two groups, an announcement group and a conversation group. Each session consisted of four parts, review evidence, build skills, practice, and application to practice. Each of the four sessions lasted approximately-one hour. | Physicians |
| Both | ||||||
| P25 | Kumar et al. Brief Provider Training Video on HPV[45] |
Sample of four pediatric practices with multidisciplinary providers including trainees | 2019 | Video | A 20 min training video with didactic teaching and clinical vignettes to address previously reported provider-related barriers to HPV vaccination. | Physicians, nurses, residents, allied health professionals |
| P26 | Marcus, Bilma Engaging in Medical Education with Sensitivity (EMES) Initiative[54] |
Single Community | 2020 | Workshop (live and streamed) | A multi-faceted community-centered approach involving: Providing evidence directly to parents in the community Teaching parents to read and interpret data Hosting a CNE approved workshop for providers to improve communication with patients Engage para-health professionals Time required for this intervention was not described. |
Physicians, residents, nurses, nurse practitioner, doulas, community members |
Table 2.
Summary of interventions identified through the grey literature environmental scan.
| Identifier | Organization and Resource Name | Year | Type of Resource | Summary of Resource |
|---|---|---|---|---|
| G1 | Centers for Disease Control and Prevention HPV Vaccine: Same Way, Same Day[41] |
2018 | Mobile app | An app to enhance the abilities of providers to practice techniques to introduce and discuss the HPV vaccine with parents and patients, including those who may be hesitant to immunize. This includes well produced animated videos of clinical encounters. |
| G2 | University of Calgary Vaccine Hesitancy Guide[47] |
2021 | Text-based cases | A comprehensive online guide to support better clinical conversations about vaccines. The guide presents guidance, scripts, and resources for HCWs to help navigate conversations about COVID-19 vaccines with hesitant patients. |
| G3 | American Academy of Pediatrics Challenging Cases: Vaccine Hesitancy[14] |
2019 | Elearning Module | A course that provides strategies to promote vaccine confidence in vaccine-hesitant parents in a time efficient and effective manner, including case studies on infant vaccination and MMR vaccination. Focuses on vaccine communications for pediatricians. |
| G4 | American Association of Colleges of Nursing Preparing Nursing Students to Effectively Address Vaccine Hesitancy[69] |
2021 | Didactic Lecture/ Webinar | A webinar that provides educators with tools and information to share with nursing students. Topics include the history and current state of vaccine hesitancy, the Immunization Resources for Undergraduate Nursing project, and how students can apply these resources to address vaccine hesitancy. |
| G5 | World Health Organization Conversations to build trust in vaccination: A training module for health workers that you can download and work through with colleagues[91] |
2017 | PowerPoint Presentation | A practical and adaptable training module aimed at helping healthcare workers address vaccine hesitancy. This module highlights key communication principles, responses to common concerns, and motivational interviewing strategies. |
| G6 | Centers for Disease Control and Prevention Building Confidence in COVID-19 Vaccines Among Your Patients[13] |
2021 | PowerPoint Presentation | A presentation that highlights tips for healthcare teams to build confidence in COVID-19 vaccines among their patients. This includes information about COVID-19 vaccines, mRNA vaccine technology, vaccine safety monitoring, elements of vaccine confidence, strategies for building vaccine confidence and communicating with patients. |
| G7 | BC Center for Disease Control Immunization Communication Tool[17] |
2021 | Handbook | A tool that provides health care workers with information and tools needed to communicate effectively about vaccines and address vaccine hesitancy. Contents include a 5-step approach to discussing vaccines and addressing vaccine hesitancy, answers to common questions, motivational interviewing strategies, immunization stories, and techniques to reduce injection pain. |
| G8 | Canadian Paediatric Society Our best shot at beating COVID-19: Overcoming vaccine hesitancy in 2021[51] |
2021 | Elearning Module | A module providing healthcare workers with tools and skills needed for discussing COVID-19 vaccines with parents, guardians, and children. The module helps providers counter COVID-19 misinformation, initiate discussion regarding vaccine-related issues, address hesitancy, and build public confidence regarding the safety and efficacy of COVID-19 vaccines. |
| G9 | Alberta Medical Association Addressing COVID-19 vaccine hesitancy[1] |
2021 | Comprehensive Resource Hub | A resource hub with conversation tools for discussing vaccines with patients. Resources include a vaccine hesitancy guide, PrOTCT PLAN for the COVID-19 vaccine discussion, and FAQs. |
| G10 | Doctors Manitoba Guide to Responding to Vaccine Hesitancy[39] |
NA | Comprehensive Resource Hub | A resource hub containing guidance for healthcare workers when discussing COVID-19 vaccines with patients. This includes advice for communicating with patients such as recognizing the nuances around patient views, the importance of the messenger and approach, and tangible guidance. |
| G11 | Government of Canada Addressing vaccine hesitancy in the context of COVID-19: A primer for health care providers[36] |
2021 | Evidence-based webpage | An interactive webpage intended to support health care providers in better understanding and addressing COVID-19 vaccine hesitancy, in their practice and beyond. Topics include, information on vaccine hesitancy, drivers of vaccine hesitancy, and strategies for building vaccine confidence. |
| G12 | Canadian Medical Protective Association Vaccinating: Doing it safely, and addressing vaccine hesitancy and refusal[83] |
2021 | Evidence-based webpage | An online article that addresses discussing vaccines with patients, obtaining informed consent, treating unvaccinated patients, and what to do when patients or legal guardians are hesitant or refuse vaccinations. |
| G13 | Center for Effective Practice COVID-19: Vaccines[20] |
2021 | Comprehensive resource hub | A tool that addresses how to speak with patients regarding vaccine hesitancy. Resources include, the PrOTCT framework, compiled up-to-date facts on COVID-19 vaccines, insights into understanding vaccine hesitancy in Black communities and Indigenous communities. |
| G14 | American Pharmacist Association Building Vaccine Confidence[7] |
2021 | Interactive tool | A comprehensive set of resources designed to strengthen vaccine confidence among patients and communities by providing information on how to build vaccine confidence in yourself, your team, and in your patients and the community. This tool also includes a Vaccine Confidence Playbook used to inform pharmacist–patient conversations regarding COVID-19 vaccines. |
| G15 | Center for Public Interest Communications at the University of Florida Guide to COVID-19 vaccine communications[38] |
2021 | Handbook | A handbook focused on principles for building trust to address vaccine hesitancy. Principles include working within worldviews, using timing to your advantage, choosing the right messengers, making narratives clear, the importance of relationships, changing social norms to gain acceptance, evoking the right emotions, and being explicit and transparent about motivations. |
| G16 | Pediatric Infectious Diseases Societies Vaccine Education from Training to Practice[84] |
NA | Elearning Modules | A Comprehensive Vaccine Education Program offering strategies to combat vaccine misinformation and address vaccine hesitancy. This is achieved by enhancing vaccine knowledge and confidence in having discussions with patients and parents and enhancing access for medical providers to reliable, up-to-date and accurate vaccine information. |
Collectively, the purpose of the interventions aimed to increase vaccine uptake and decrease vaccine hesitancy in patients, through education of HCPs. Interventions predominantly centered around two foci: knowledge sharing (P1-2, P4-5, P8-9, P11, P14-16, P19, P21, P24) and communication training (P1-3, P5, P7, P9, P11, P12, P15-23, P26). Many interventions included both components, and the more comprehensive interventions were better captured in the peer-reviewed literature (P1-2, P5, P9, P11, P15-16, P19, P21,). Self-directed, facilitated and participatory approaches were described. In interventions that were evaluated, the self-directed components had the least consistent uptake (P1, P6-7, P13, P18, P22-23).
While one intervention did evaluate the impact on exhibited empathy in HCP, no intervention was found to target or specifically address the recognition and management of HCP emotions during difficult conversations (P18).
3.3. Context Summary
Included interventions targeted HCPs from different disciplines at different stages of training. 17 interventions were multi-disciplinary (P12-P13, P17-P21, P25-P26, G2, G5-G8, G11, G13, G15). When interventions were discipline specific, medical providers including medical students, residents, physicians, and physician assistants were the most commonly targeted HCP group with 15 interventions (P1-P5, P6-P7, P11, P16, P24, G3, G9, G10, G12, G16). Interestingly, these interventions were designed for pediatric and family medicine providers only, and no other medical practitioner group was represented. Nursing, pharmacy and midwifery providers also had specific interventions described, although much less frequently (P5, P8, P10, P14, P15, P22-P23, G4, G14). When considering stages of training, there was a fairly equal distribution. Twelve interventions were specific to the undergraduate and postgraduate trainee level across disciplines (P1-P11, G4), 16 interventions were applied for providers in practice (P12-P24, G9, G10, G12) and 13 interventions were not practice level-specific (P25-P26, G2-G3, G5-G8, G11, G13-G16). Reflective of this distribution, 11 interventions were applied in the curricular and extracurricular settings (P1-P11), while 11 were applied in clinical practice, as described in the peer-reviewed literature (P6, P12-P14, P16, P17, P19-P21, P24-P25). Five interventions were applied in alternative settings (P15, P18, P22, P23, P26). Included interventions originated from several countries including the United States, Canada (P15), Italy (P10, P18), and Belgium (P9). Two studies did not have a described population (P22-P23).
Human papillomavirus was the most common disease and vaccine addressed by our included interventions (P1, P2, P7, P12, P17, P19-P21, P24-P25). The SARS-COV2 virus and vaccine was also well represented, but predominantly in our grey literature scan (P23, G2, G6, G8-G11, G13, G15). Only one peer-reviewed intervention was identified in this particular subgroup at the time this scoping review was conducted (P23). Twenty-one interventions were not disease or vaccine specific, representing just over half our included interventions. A summary of intervention contexts are provided in Table 3 .
Table 3.
Summary of interventions specific to various target populations (discipline, practice level, disease/vaccine, setting).
| Target Group | Number of Interventions | Intervention |
|---|---|---|
| Healthcare Provider Discipline | ||
| Medical Provider | 14 | P1-P5, P6-P7, P11, P16, P24; G3, G9, G10, G12, G16 |
| Nursing | 3 | P5, P15; G4 |
| Pharmacy | 5 | P8, P14, P22-P23; G14 |
| Other Allied Health | 1 (midwife) | P10 |
| Multidisciplinary | 17 | P12-P13, P17-P21, P25-P26; G2, G5-G8, G11, G13, G15 |
| Not specified | 1 | P9 |
| Practice Level | ||
| Trainee | 12 | P1-P11, G4 |
| Non-Trainee | 16 | P12-P24; G9, G10, G12 |
| Not specified | 13 | P25-P26; G2-G3, G5-G8, G11, G13-G16 |
| Disease and Vaccine | ||
| HPV | 10 | P1, P2, P7, P12, P17, P19-P21, P24-P25 |
| Influenza | 1 | P14 |
| COVID | 9 | P23; G2, G6, G8-G11, G13, G15 |
| Multiple | 21 | P3-P6, P8-P11, P13, P15-P16, P18, P22, P26; G3-G5, G7, G12, G14, G16 |
|
Intervention Setting (peer reviewed literature only) | ||
| Curriculum | 7 | P1, P3-P5, P8, P10, P11 |
| Extra-curricular | 3 | P2, P7, P9 |
| Clinical Practice | 11 | P6, P12-P14, P16, P17, P19-P21, P24-P25 |
| Community | 3 | P15, P18, P26 |
| Pharmacies | 1 | P22 |
| Independent | 1 | P23 |
3.4. Modes of delivery
Delivery of each intervention is summarized in Table 1. In peer-reviewed literature, more than half were multi-modal (P1-P5, P8-P11, P16-P19, P21, P24). It was more common in interventions targeting trainees to include a simulation component (8/11 interventions in trainees, 3/13 interventions in non-trainees and 0/2 interventions in those targeting both). Only seven interventions were delivered without an in-person component (P7, P12, P13, P20, P22, P23, P25).
In contrast, our grey literature environmental scan identified primarily self-directed interventions, which were predominantly delivered online, in the form of e-learning modules (few of which were interactive) (G3, G8, G16), websites (G2, G4-G6, G9-G14), developed handbooks (G7, G15) and a mobile app (G1). They were presumably cost-effective and time-efficient, although effectiveness and uptake were not evaluated as part of the interventions. One intervention was delivered as a webinar (G4).
3.5. Accessibility and generalizability of interventions
While most interventions were adequately described in peer-reviewed literature for a general understanding, few provided enough details and sufficient relevant materials for reproducibility (Supplemental Table 4). When available, educational materials were typically found in appendices. One citation referenced a website link which was not accessible (P9). Content references were consistently provided in interventions identified in our grey literature scan (Supplemental Table 5). With respect to prerequisite materials, one author group published two interventions using novel technologies, with virtual reality simulation (P6) and a phone and tablet application (P7). Both were innovative but required up-front investment and development.
Most interventions were delivered over a reasonable amount of time for generalizability. Ten interventions were delivered over approximately 4 h or less at a time (P3, P4, P8, P10, P11, P15, P17-19, P21). Five interventions were delivered in 1 h or less (P1, P6, P13, P24-P25). The longest intervention delivered consecutively was a 4-day in-person training curriculum (P9). Ten interventions did not specify the time required (P2, P5, P7, P12, P14, P16, P20, P22-P23, P26). Overall, we found that interventions for HCPs ranged over a period of 20 min to 6 months (Table 1). In our grey literature environmental scan, only one intervention clearly stated the required length of time, which was a self-directed e-learning module that required up to 9 h (G18). Eight interventions described in peer-reviewed literature allowed for asynchronous delivery (P1, P12-P13, P17, P20, P22-P23, P25). In our grey literature environmental scan, 14/15 unique interventions identified were self-directed and would provide similar flexibility (G2-G3, G5-G16).
Cost was not outlined in interventions identified from peer-reviewed literature. Within grey literature resources, 14 were accessible without a fee (G1-G3, G5-G7, G9-G16). However, two of the identified resources required a registration fee, which may limit access to its contents (G4, G8). Among the resources that had a cost, both were self-directed e-learning modules developed by healthcare provider associations. These resources were offered free of charge to respective associations’ members.
3.6. Evaluation of interventions
23/26 interventions identified in peer-reviewed literature were evaluated (P1-P21, P24-P25). Two interventions were referenced with two separate citations each, as they underwent separate evaluative processes (P6, P21). Seven interventions were evaluated in a randomized manner (P3, P6, P13, P17, P20, P21, P24). Overall, interventions increased HCP self-perceived confidence and comfort in engaging vaccine-hesitant individuals (P1, P2, P6, P8, P11-P13, P15-P16, P19, P21, P25), with only one study that evaluated for this demonstrating no significant change (P3). Vaccine attitudes in HCP were not found to consistently change with interventions.
The most common evaluative method was baseline and post-intervention questionnaires (P1-P4, P8, P10-P11, P15-P16, P18-P21, P25). Four interventions relied primarily on qualitative feedback and thematic analysis (P5, P7, P9, P17). Three studies included a component of standardized grading using simulated encounters (P3, P8, P11), and all three showed global gains in respective scoring systems across multiple domains. In particular, Vyas et al. demonstrated larger gains in areas of communication dealing with creating a positive environment, and found less conflict escalation after intervention (P8). Five interventions utilized electronic medical records or registry data to assess rate of vaccine refusal in a clinical setting (P6, P14, P19, P21, P24). Generally, increased compliance with vaccinations and decreased rates of refusal were seen. However, Brewer et al. identified mixed results depending on the patient age group and type of communication training provided (P24). No formal evaluations were available for grey literature resources. Information on informal evaluations was not provided by the organizations.
4. Discussion
4.1. Summary
This scoping review explored the availability of existing educational interventions targeted at HCPs to enable effective communication with vaccine hesitant individuals in the North American context. We identified a wide range of existing interventions described in both published peer-reviewed literature and grey literature. Our findings suggest that as a whole, these interventions were knowledge and communication-focused, and were able to create a positive impact on providers’ self-perceived confidence in and likelihood of addressing vaccine-hesitant individuals. However, HCP attitudes did not consistently demonstrate change. Only five studies evaluated objective clinical outcomes of the applied interventions. There was a suggestion that these interventions may result in a reduction in vaccine refusal, which is promising but inconclusive due to the limited translational data. From our review of the literature, there is an overwhelming amount of available interventions but little guidance on how to select and implement the appropriate intervention for a particular clinical context. While many interventions were evaluated, there were no comparative studies to help inform this decision.
Through our review process, it became apparent that interventions identified through our primary literature search tended to be multi-modal and more robustly evaluated. However, the grey literature environmental scan was essential in identifying interventions that were more topical, especially in the current clinical context given the SARS-COV2 virus global pandemic. Rapid advancements in vaccinology have been identified as a potential barrier for HCP [27] and therefore the provision of up-to-date information is important to mitigate this challenge and increase HCP knowledge and comfort. We found that only one peer-reviewed intervention specifically addressed the SARS-COV2 vaccine, while we identified nine in our grey literature environmental scan. Thus, we found both searches provided important insights on the current landscape of literature.
4.2. Gaps in knowledge
Accessibility of interventions were found to be limiting. Potential reproducibility was assessed based on provided and available resources. We found that few interventions in peer-reviewed literature could be applied without obtaining further information, based on the described methods and provided materials by authors/creators. Cost for implementation is an important factor to consider, and few identified resources did require registration which further limits accessibility. Generalizability was assessed based on intervention time and setting. While data on the time for each intervention was not consistently provided, most facilitated interventions were intended for delivery within four hours. While shorter interventions are expected to broaden potential applicability, a correlation between effect size and length of intervention has been shown in continuing medical education [53]. There remains no clear recommendation on the optimal duration of an intervention. Consideration should be made for potential impacts on knowledge translation and sustainability of effect. Self-directed interventions, as defined by those that were learner led and completed at one’s own time and pace, were particularly common in our grey literature environmental scan. Self-directed interventions offer flexibility, and are of increasing importance in the realm of advancing digital and mobile technologies, but can be somewhat limited by user-uptake and learner desire for assuming learning responsibility [21]. Finally, there was a distribution of interventions across disciplines, clinical settings, and in both trainees and non-trainees, although representation was variable. It should be recognized that a disproportionate amount of interventions were designed specifically for medical providers, despite the fact that pharmacists, nurses and alternative healthcare providers all play an essential and significant role in informing vaccine decisions [29], [37]. A recent scoping review by Cassidy et al. [11] highlighted that several barriers are perceived by pharmacists and nurses to address vaccine hesitancy, emphasizing the ongoing need to develop interventions targeted to these populations and identified barriers [11]. Further exploration would be required to determine whether a multidisciplinary educational intervention would provide more value, as compared to the more discipline-specific educational interventions. Within the medical provider population, pediatric providers were the most common group targeted. In parallel, childhood diseases such as HPV were the most common topic of discussion for the interventions identified.
Engaging vaccine-hesitant individuals in conversation is acknowledged as a difficult and high-stakes conversation, underpinned by differences in opinions and values of patients and providers [30]. While expertise (knowledge), HCP attitudes towards vaccinations and communication strategies are important components, it has been increasingly recognized that the emotional state of the provider also influences their ability to navigate these conversations [16], [55]. Anxiety, sadness, empathy, frustration and inadequacy are the most commonly described emotions in providers and nearly all providers expressed emotional distress in one study [55]. Self-monitoring, as a part of moment-to-moment self-regulation, allows providers to recognize limitations and respond to emotional responses of both patients and self. This practice is required for reflection and subsequent action to de-escalate high-stakes conversations and engage in problem solving around complexities in order to restore trust and communicate effectively [16], [31], [28]. No interventions in our scoping review were found to adequately educate HCPs to engage in self-monitoring to shift the conversational approach.
4.3. Limitations
There are several limitations to this scoping review. To ensure we captured as much relevant literature as possible, we included both peer-reviewed and grey literature. Despite our attempts to be as comprehensive as possible, this is still reflective of only interventions that have been formalized and described in an online format. Interventions may exist in an informal setting, which is not well captured by our scoping review. While our peer-reviewed literature did not include any geographic restrictions, our grey literature environmental scan was focused on North American sources only. Furthermore, it was not possible to determine whether all available resources were captured through our grey literature environmental scan due to the millions of results and related pages yielded from Google search engines. Secondly, while our search strategy did not restrict for language, our inclusion was restricted to the English and French language. French was specifically included given our Canadian context. We expect this may marginally limit comprehensiveness but is unlikely to introduce bias [59]. Finally, we elected to review the characteristics and evaluation of each intervention based only on available information, and chose not to contact individual authors to clarify details or provide additional resources. We recognize that as a result, key information may be absent or prone to underlying assumptions. However, we felt this was reflective of real-life interpretation by general readers.
5. Conclusion
In conclusion, the recent SARS-COV2 pandemic has increased recognition of vaccine hesitancy and has been contrasted by the rapid advances in vaccinology and immunology. The strategic development of strategies to translate these advances into practice are of utmost importance. HCPs across all disciplines have unique and complementary roles in addressing vaccine hesitancy. There is a need for available, credible, and comprehensive resources that will best support our HCPs in effective communication with vaccine hesitant patients.
This scoping review is the first to comprehensively explore the current scope of peer-reviewed educational interventions for HCPs in addressing vaccine hesitancy that are available. We further complemented this with a context-specific examination of North American grey literature. We summarized the variety of interventions described across multiple disciplines, training levels, clinical settings, and diseases/vaccines. However, the accessibility and generalizability of interventions is somewhat problematic. In particular, it is recognized that patients rely on advice from multiple HCP disciplines in the vaccine decision process, and our review suggests that current educational interventions may not adequately reflect this. Additionally, interventions have generally been focused on knowledge sharing and communication training, and a significant gap in knowledge in addressing HCP self-monitoring and emotional regulation was identified. Therefore, this scoping review informs the need for an intervention that is developed to: 1) maximize dissemination potential, 2) address the unique needs of each HCP discipline, and 3) recognize the role of internal self-regulation as a contributor to external communication and relationship building.
Funding
This project was supported by the Public Health Agency of Canada Immunize Partnership Fund [grant # 2122-HQ-000334].
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: CC has previously received grant funding from drug companies for investigator driven research (GSK, Pfizer, Merck & Co) and honoraria/speaker fees (GSK, Pfizer, Merck & Co, Federation of Women in Medicine). SH participated in advisory board meeting for AstraZeneca, GSK, Pfizer, Seqirus and Valenva SE. SH has also received grant funding from drug companies for investigator driven research (GSK, Valneva SE). The other authors do not have anything to declare.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Sherilyn Houle reports a relationship with AstraZeneca that includes: board membership. Sherilyn Houle reports a relationship with GSK that includes: board membership and funding grants. Sherilyn Houle reports a relationship with Pfizer Inc that includes: board membership. Sherilyn Houle reports a relationship with Seqirus Inc. that includes: board membership. Sherilyn Houle reports a relationship with Valneva SE that includes: board membership and funding grants. Cora Constantinescu reports a relationship with Federation of Women in Medicine that includes: speaking and lecture fees. Cora Constantinescu reports a relationship with GSK that includes: funding grants and speaking and lecture fees. Cora Constantinescu reports a relationship with Pfizer Inc that includes: funding grants and speaking and lecture fees. Cora Constantinescu reports a relationship with Merck & Co Inc that includes: funding grants and speaking and lecture fees].
Acknowledgements
We would like to thank Dr. Alix Hayden and Patrick Labelle for their guidance in the protocol development.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.09.093.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
No data was used for the research described in the article.
References
- 1.Addressing vaccine hesitancy in the context of COVID-19: A primer for health care providers. Alberta Medical Association n.d. https://www.albertadoctors.org/about/COVID-19/vaccine-positive-clinic-toolkit/addressing-vaccine-hesitancy.
- 2.Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. JBI, 2020. Available from https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-01
- 3.Barton S.M., Calhoun A.W., Bohnert C.A., Multerer S.M., Statler V.A., Bryant K.A., et al. Standardized Vaccine-Hesitant Patients in the Assessment of the Effectiveness of Vaccine Communication Training. J Pediatr. 2022;241 doi: 10.1016/j.jpeds.2021.10.033. 203–11.e1. [DOI] [PubMed] [Google Scholar]
- 4.Bednarczyk R.A. Examining the “why” of vaccine hesitancy. Health Psychol. 2018;37:316–317. doi: 10.1037/hea0000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brewer N.T., Hall M.E., Malo T.L., Gilkey M.B., Quinn B., Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. 2017:139. doi: 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brewer N.T., Mitchell C.G., Alton Dailey S., Hora L., Fisher-Borne M., Tichy K., et al. HPV vaccine communication training in healthcare systems: Evaluating a train-the-trainer model. Vaccine. 2021;39:3731–3736. doi: 10.1016/j.vaccine.2021.05.038. [DOI] [PubMed] [Google Scholar]
- 7.Building Vaccine Confidence. American Pharmacist Association n.d. https://vaccineconfident.pharmacist.com/.
- 8.Butler R, MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP). Vaccine 2015;33:4176–9. https://doi.org/10.1016/j.vaccine.2015.04.038. [DOI] [PubMed]
- 10.Cascini F., Pantovic A., Al-Ajlouni Y., Failla G., Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine. 2021;40 doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cassidy C., Langley J., Steenbeek A., Taylor B., Kennie-Kaulbach N., Grantmyre H., et al. A Behavioral analysis of nurses’ and pharmacists' role in addressing vaccine hesitancy: scoping review. Hum Vaccin Immunother. 2021;17:4487–4504. doi: 10.1080/21645515.2021.1954444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cates J.R., Diehl S.J., Fuemmeler B.F., North S.W., Chung R.J., Hill J.F., et al. Toward Optimal Communication About HPV Vaccination for Preteens and Their Parents: Evaluation of an Online Training for Pediatric and Family Medicine Health Care Providers. J Public Health Manag Pract. 2020;26:159–167. doi: 10.1097/PHH.0000000000001022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC COVID-19 Response Vaccine Task Force. Building Confidence in COVID-19 Vaccines Among Your Patients: Tips for the Healthcare Team, 2021. https://www.cdc.gov/vaccines/covid-19/downloads/VaccinateWConfidence-Immunization-Coordinators_508.pdf
- 14.Challenging Cases: Vaccine Hesitancy. American Academy of Pediatrics. n.d. https://shop.aap.org/challenging-cases-vaccine-hesitancy/_gl=1*138zbx1*_ga*ODIzNDgwMjI5LjE2MDI1OTc5NjM.*_ga_FD9D3XZVQQ*MTYzNjEyMjc3Ni40LjEuMTYzNjEyMjg0OS4w&_ga=2.187712616.1947371175.1636122790-823480229.1602597963.
- 15.Chamberlain A.T., Limaye R.J., O’Leary S.T., Frew P.M., Brewer S.E., Spina C.I., et al. Development and acceptability of a video-based vaccine promotion tutorial for obstetric care providers. Vaccine. 2019;37:2532–2536. doi: 10.1016/j.vaccine.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng A., LaDonna K., Cristancho S., Ng S. Navigating difficult conversations: the role of self-monitoring and reflection-in-action. Med Educ. 2017;51:1220–1231. doi: 10.1111/medu.13448. [DOI] [PubMed] [Google Scholar]
- 17.Chilton et al. Immunization Communication Tool. Immunize BC; BC Centre for Disease Control; n.d. http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Immunization/Vaccine%20Safety/ICT-2021.pdf
- 18.Coleman A., Lehman D. A Flipped Classroom and Case-Based Curriculum to Prepare Medical Students for Vaccine-Related Conversations with Parents. MedEdPORTAL. 2017;13:10582. doi: 10.15766/mep_2374-8265.10582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cotugno S., Morrow G., Cooper C., Cabie M., Cohn S. Impact of pharmacist intervention on influenza vaccine assessment and documentation in hospitalized psychiatric patients. Am J Health Syst Pharm. 2017;74:S90–S94. doi: 10.2146/ajhp160755. [DOI] [PubMed] [Google Scholar]
- 20.COVID-19: Vaccines. Centre for Effective Practice n.d. https://tools.cep.health/tool/covid-19-vaccines/.
- 21.Curran V., Gustafson D.L., Simmons K., Lannon H., Wang C., Garmsiri M., et al. Adult learners’ perceptions of self-directed learning and digital technology usage in continuing professional education: An update for the digital age. J Adult Contin Educ. 2019;25:74–93. doi: 10.1177/1477971419827318. [DOI] [Google Scholar]
- 22.Das Neves CG. IPBES (2020) workshop report on biodiversity and pandemics of the intergovernmental Platform on biodiversity and ecosystem services 2020. https://vetinst.brage.unit.no/vetinst-xmlui/handle/11250/2828557. Accessed 7 February 2022
- 23.Dempsey A.F., Pyrznawoski J., Lockhart S., Barnard J., Campagna E.J., Garrett K., et al. Effect of a Health Care Professional Communication Training Intervention on Adolescent Human Papillomavirus Vaccination: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2018;172:e180016. doi: 10.1001/jamapediatrics.2018.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diethelm P., McKee M. Denialism: what is it and how should scientists respond? Eur J Public Health. 2009;19:2–4. doi: 10.1093/eurpub/ckn139. [DOI] [PubMed] [Google Scholar]
- 25.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dubé E, Gagnon D, MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015;33:4191–203. https://doi.org/10.1016/j.vaccine.2015.04.041. [DOI] [PubMed]
- 27.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Durning S.J., Cleary T.J., Sandars J., Hemmer P., Kokotailo P., Artino A.R. Perspective: Viewing “Strugglers” Through a Different Lens: How a Self-Regulated Learning Perspective Can Help Medical Educators With Assessment and Remediation. Acad Med. 2011;86:488. doi: 10.1097/ACM.0b013e31820dc384. [DOI] [PubMed] [Google Scholar]
- 29.Dybsand L.L., Hall K.J., Carson P.J. Immunization attitudes, opinions, and knowledge of healthcare professional students at two Midwestern universities in the United States. BMC Med Educ. 2019;19:242. doi: 10.1186/s12909-019-1678-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards K.M., Hackell J.M., Committee on infectious diseases, the committee on practice and ambulatory medicine. Countering Vaccine Hesitancy. Pediatrics. 2016:138. doi: 10.1542/peds.2016-2146. [DOI] [PubMed] [Google Scholar]
- 31.Epstein R.M., Siegel D.J., Silberman J. Self-monitoring in clinical practice: a challenge for medical educators. J Contin Educ Health Prof. 2008;28:5–13. doi: 10.1002/chp.149. [DOI] [PubMed] [Google Scholar]
- 32.Gagneur A., Bergeron J., Gosselin V., Farrands A., Baron G. A complementary approach to the vaccination promotion continuum: An immunization-specific motivational-interview training for nurses. Vaccine. 2019;37:2748–2756. doi: 10.1016/j.vaccine.2019.03.076. [DOI] [PubMed] [Google Scholar]
- 33.Gerges S., Peter E., Bowles S.K., Diamond S., Bucci L.M., Resnick A., et al. Pharmacists as vaccinators: An analysis of their experiences and perceptions of their new role. Hum Vaccin Immunother. 2018;14:471–477. doi: 10.1080/21645515.2017.1403695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glanternik J.R., McDonald J.C., Yee A.H., Howell Ba A., Saba K.N., Mellor R.G., et al. Evaluation of a Vaccine-Communication Tool for Physicians. J Pediatr. 2020;224 doi: 10.1016/j.jpeds.2020.06.007. 72–8.e1. [DOI] [PubMed] [Google Scholar]
- 36.Government of Canada. Addressing vaccine hesitancy in the context of COVID-19: A primer for health care providers nd. https://www.canada.ca/en/public-health/services/diseases/2019-novel -coronavirus-infection/health-professionals/vaccines/vaccine-hesitancy-primer.html
- 37.Grundy Q., Bero L.A., Malone R.E. Marketing and the Most Trusted Profession: The Invisible Interactions Between Registered Nurses and Industry. Ann Intern Med. 2016;164:733–739. doi: 10.7326/M15-2522. [DOI] [PubMed] [Google Scholar]
- 38.Guide to COVID-19 vaccine communications. Center for Public Interest Communications at the University of Florida n.d. https://covid19vaccinescommunicationprinciples.org/downloads/.
- 39.Guide to Responding to Vaccine Hesitancy. Doctors Manitoba n.d. https://doctorsmanitoba.ca/managing-your-practice/covid-19/vaccine-resource-centre/guide-to-responding-to-vaccine-hesitancy.
- 40.Hornsey M.J., Harris E.A., Fielding K.S. The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychol. 2018;37:307–315. doi: 10.1037/hea0000586. [DOI] [PubMed] [Google Scholar]
- 41.HPV Vaccine: Same Way, Same Day. CDC n.d. https://www.cdc.gov/vaccines/ed/courses.html#hpv-same.
- 42.Ildarabadi E., Karimi Moonaghi H., Heydari A., Taghipour A., Abdollahi M.A. Vaccination learning experiences of nursing students: a grounded theory study. J Educ Eval Health Prof. 2015;12:29. doi: 10.3352/jeehp.2015.12.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karras J., Dubé E., Danchin M., Kaufman J., Seale H. A scoping review examining the availability of dialogue-based resources to support healthcare providers engagement with vaccine hesitant individuals. Vaccine. 2019;37:6594–6600. doi: 10.1016/j.vaccine.2019.09.039. [DOI] [PubMed] [Google Scholar]
- 45.Kumar M.M., Boies E.G., Sawyer M.H., Kennedy M., Williams C., Rhee K.E. A Brief Provider Training Video Improves Comfort With Recommending the Human Papillomavirus Vaccine. Clin Pediatr. 2019;58:17–23. doi: 10.1177/0009922818805217. [DOI] [PubMed] [Google Scholar]
- 46.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature medicine. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leslie, M., Fadaak, R., & Pinto, N. Vaccine Hesitancy Guide. VH Guide n.d. https://www.vhguide.ca/.
- 48.Li M., Luo Y., Watson R., Zheng Y., Ren J., Tang J., et al. Healthcare workers’ (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. 2021 doi: 10.1136/postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 49.Lin C., Mullen J., Smith D., Kotarba M., Kaplan S.J., Tu P. Healthcare Providers’ Vaccine Perceptions, Hesitancy, and Recommendation to Patients: A Systematic Review. Vaccines (Basel) 2021:9. doi: 10.3390/vaccines9070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lockhart S., Dempsey A.F., Pyrzanowski J., O’Leary S.T., Barnard J.G. Provider and Parent Perspectives on Enhanced Communication Tools for Human Papillomavirus Vaccine-Hesitant Parents. Acad Pediatr. 2018;18:776–782. doi: 10.1016/j.acap.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 51.MacDonald N.E., Desai S., Gerstein B. Working with vaccine-hesitant parents: An update. Paediatrics & Child Health. 2018;23 doi: 10.1093/pch/pxy144. 561–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.MacDougall D.M., Halperin B.A., MacKinnon-Cameron D., Li L., McNeil S.A., Langley J.M., et al. The challenge of vaccinating adults: attitudes and beliefs of the Canadian public and healthcare providers. BMJ Open. 2015;5:e009062. doi: 10.1136/bmjopen-2015-009062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mansouri M., Lockyer J. A meta-analysis of continuing medical education effectiveness. Journal of continuing education in the health professions. 2007:6–15. doi: 10.1002/chp.88. [DOI] [PubMed] [Google Scholar]
- 54.Marcus B. A nursing approach to the largest measles outbreak in recent U.S history: Lessons learned battling homegrown vaccine hesitancy. OJIN: The. Online Journal of Issues in Nursing. 2020:25. doi: 10.3912/OJIN.Vol25No01Man03. [DOI] [Google Scholar]
- 55.Martin E.B., Jr, Mazzola N.M., Brandano J., Luff D., Zurakowski D., Meyer E.C. Clinicians’ recognition and management of emotions during difficult healthcare conversations. Patient Educ Couns. 2015;98:1248–1254. doi: 10.1016/j.pec.2015.07.031. [DOI] [PubMed] [Google Scholar]
- 56.Maurici M., Arigliani M., Dugo V., Leo C., Pettinicchio V., Arigliani R., et al. Empathy in vaccination counselling: a survey on the impact of a three-day residential course. Hum Vaccin Immunother. 2019;15:631–636. doi: 10.1080/21645515.2018.1536587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morhardt T., McCormack K., Cardenas V., Zank J., Wolff M., Burrows H. Vaccine curriculum to engage vaccine-hesitant families: Didactics and communication techniques with simulated patient encounter. MedEdPORTAL. 2016;:12. doi: 10.15766/mep_2374-8265.10400. [DOI] [Google Scholar]
- 59.Morrison A., Polisena J., Husereau D., Moulton K., Clark M., Fiander M., et al. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28:138–144. doi: 10.1017/S0266462312000086. [DOI] [PubMed] [Google Scholar]
- 60.Nguyen-Van-Tam J.S., Hampson A.W. The epidemiology and clinical impact of pandemic influenza. Vaccine. 2003;21:1762–1768. doi: 10.1016/s0264-410x(03)00069-0. [DOI] [PubMed] [Google Scholar]
- 61.Nold L., Deem M.J. A Simulation Experience for Preparing Nurses to Address Refusal of Childhood Vaccines. J Nurs Educ. 2020;59:222–226. doi: 10.3928/01484834-20200323-09. [DOI] [PubMed] [Google Scholar]
- 62.NORC at the University of Chicago. Surveys of Trust in the U.S. Health Care System. ABIM Foundation 2021.
- 63.Omer S.B., Salmon D.A., Orenstein W.A., deHart M.P., Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 64.Opel D.J., Heritage J., Taylor J.A., Mangione-Smith R., Salas H.S., Devere V., et al. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics. 2013;132:1037–1046. doi: 10.1542/peds.2013-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pahud B., Elizabeth Williams S., Lee B.R., Lewis K.O., Middleton D.B., Clark S., et al. A randomized controlled trial of an online immunization curriculum. Vaccine. 2020;38:7299–7307. doi: 10.1016/j.vaccine.2020.09.043. [DOI] [PubMed] [Google Scholar]
- 66.Paterson P., Meurice F., Stanberry L.R., Glismann S., Rosenthal S.L., Larson H.J. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700–6706. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 67.Pelly L.P., Pierrynowski Macdougall D.M., Halperin B.A., Strang R.A., Bowles S.K., Baxendale D.M., et al. THE VAXED PROJECT: an assessment of immunization education in Canadian health professional programs. BMC Med Educ. 2010;10:86. doi: 10.1186/1472-6920-10-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Powell B.J., Waltz T.J., Chinman M.J., Damschroder L.J., Smith J.L., Matthieu M.M., et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science. 2015 Dec;10(1):1–4. doi: 10.1186/s13012-015-0209-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Preparing Nursing Students to Effectively Address Vaccine Hesitancy. American Association of Colleges Of Nursing 2021. https://www.aacnnursing.org/Professional-Development/Webinar-Info/sessionaltcd/WFR21_03_17.
- 70.Real F.J., DeBlasio D., Beck A.F., Ollberding N.J., Davis D., Cruse B., et al. A Virtual Reality Curriculum for Pediatric Residents Decreases Rates of Influenza Vaccine Refusal. Acad Pediatr. 2017;17:431–435. doi: 10.1016/j.acap.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 71.Real F.J., DeBlasio D., Ollberding N.J., Davis D., Cruse B., Mclinden D., et al. Resident perspectives on communication training that utilizes immersive virtual reality. Educ Health. 2017;30:228–231. doi: 10.4103/efh.EfH_9_17. [DOI] [PubMed] [Google Scholar]
- 72.Real F.J., Rosen B.L., Bishop J.M., McDonald S., DeBlasio D., Kreps G.L., et al. Usability Evaluation of the Novel Smartphone Application, HPV Vaccine: Same Way, Same Day. Among Pediatric Residents. Acad Pediatr. 2021;21:742–749. doi: 10.1016/j.acap.2020.11.023. [DOI] [PubMed] [Google Scholar]
- 73.Reno J.E., O’Leary S., Garrett K., Pyrzanowski J., Lockhart S., Campagna E., et al. Improving Provider Communication about HPV Vaccines for Vaccine-Hesitant Parents Through the Use of Motivational Interviewing. J Health Commun. 2018;23:313–320. doi: 10.1080/10810730.2018.1442530. [DOI] [PubMed] [Google Scholar]
- 74.Reno J.E., Thomas J., Pyrzanowski J., Lockhart S., O’Leary S.T., Campagna E.J., et al. Examining strategies for improving healthcare providers’ communication about adolescent HPV vaccination: evaluation of secondary outcomes in a randomized controlled trial. Hum Vaccin Immunother. 2019;15:1592–1598. doi: 10.1080/21645515.2018.1547607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sarnquist C., Sawyer M., Calvin K., Mason W., Blumberg D., Luther J., et al. Communicating about vaccines and vaccine safety: what are medical residents learning and what do they want to learn? J Public Health Manag Pract. 2013;19:40–46. doi: 10.1097/PHH.0b013e3182495776. [DOI] [PubMed] [Google Scholar]
- 76.Schnaith A.M., Evans E.M., Vogt C., Tinsay A.M., Schmidt T.E., Tessier K.M., et al. An innovative medical school curriculum to address human papillomavirus vaccine hesitancy. Vaccine. 2018;36:3830–3835. doi: 10.1016/j.vaccine.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shen A.K., Tan A.S.L. Trust, influence, and community: Why pharmacists and pharmacies are central for addressing vaccine hesitancy. J Am Pharm Assoc. 2022;62:305–308. doi: 10.1016/j.japh.2021.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shipton E.E., Bate F., Garrick R., Steketee C., Shipton E.A., Visser E.J. Systematic Review of Pain Medicine Content, Teaching, and Assessment in Medical School Curricula Internationally. Pain Ther. 2018;7:139–161. doi: 10.1007/s40122-018-0103-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Smith L.E., Amlôt R., Weinman J., Yiend J., Rubin G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35:6059–6069. doi: 10.1016/j.vaccine.2017.09.046. [DOI] [PubMed] [Google Scholar]
- 80.Ten threats to global health in 2019. World Health Organization 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 82.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 83.Vaccinating: Doing it safely, and addressing vaccine hesitancy and refusal. Canadian Medical Protective Association 2021. https://www.cmpa-acpm.ca/en/advice-publications/browse-articles/2021/vaccinating-doing-it-safely-and-addressing-vaccine-hesitancy-and-refusal.
- 84.Vaccine Education from Training to Practice. Pediatric Infectious Diseases Societies n.d. https://pids.org/education-training/vaccine-education-program/.
- 86.Visalli G., Facciolà A., Mazzitelli F., Laganà P., Pietro D.I., A. Health education intervention to improve vaccination knowledge and attitudes in a cohort of obstetrics students. J Prev Med Hyg. 2021;62:E110–E116. doi: 10.15167/2421-4248/jpmh2021.62.1.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vorsters A., Tack S., Hendrickx G., Vladimirova N., Bonanni P., Pistol A., et al. A summer school on vaccinology: Responding to identified gaps in pre-service immunisation training of future health care workers. Vaccine. 2010;28:2053–2059. doi: 10.1016/j.vaccine.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 88.Vyas D., Galal S.M., Rogan E.L., Boyce E.G. Training Students to Address Vaccine Hesitancy and/or Refusal. Am J Pharm Educ. 2018;82:6338. doi: 10.5688/ajpe6338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wiley K.E., Massey P.D., Cooper S.C., Wood N., Quinn H.E., Leask J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: a cross sectional survey. Vaccine. 2013;31:3972–3978. doi: 10.1016/j.vaccine.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 90.World Health Organization. Best Practice Guidance: How to respond to vocal vaccine deniers in public. In: WHO Regional Office for Europe. 2016.
- 91.World Health Organization. Conversations to build trust in vaccination:A training module for health Workers. 2017.
- 92.Zolezzi M., Paravattil B., El-Gaili T. Using motivational interviewing techniques to inform decision-making for COVID-19 vaccination. Int J Clin Pharm. 2021;43:1728–1734. doi: 10.1007/s11096-021-01334-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
References
Further Reading
- 9.COVID-19 in Canada: A Six-month Update on Social and Economic Impacts. Statistics Canada n.d. https://www150.statcan.gc.ca/n1/pub/11-631-x/11-631-x2020004-eng.htm.
- 35.Godin K., Stapleton J., Kirkpatrick S.I., Hanning R.M., Leatherdale S.T. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4:138. doi: 10.1186/s13643-015-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Isenor J.E., Edwards N.T., Alia T.A., Slayter K.L., MacDougall D.M., McNeil S.A., et al. Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis. Vaccine. 2016;34:5708–5723. doi: 10.1016/j.vaccine.2016.08.085. [DOI] [PubMed] [Google Scholar]
- 57.Microsoft Excel. Microsoft Corporation 2018. https://office.microsoft.com/excel.
- 81.Health T.L.P. A Pandemic Era. Lancet Planet Health. 2021;5:e1. doi: 10.1016/S2542-5196(20)30305-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Veritas Health Innovation. Covidence 2014. https://www.covidence.org/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data was used for the research described in the article.