Abstract
The WD repeat containing antisense to TP53 (WRAP53) gene codifies an antisense transcript for tumor protein p53 (TP53), stabilization (WRAP53α), and a functional protein (WRAP53β, WDR79, or TCAB1). The WRAP53β protein functions as a scaffolding protein that is important for telomerase localization, telomere assembly, Cajal body integrity, and DNA double-strand break repair. WRAP53β is one of many proteins known for containing WD40 domains, which are responsible for mediating a variety of cell interactions. Currently, WRAP53 overexpression is considered a biomarker for a diverse subset of cancer types, and in this study, we describe what is known about WRAP53β’s multiple interactions in cell protein trafficking, Cajal body formation, and DNA double-strand break repair and its current perspectives as a biomarker for cancer.
Keywords: WRAP53, genomic instability, carcinogenesis, TP53, telomerase
1. Introduction
Cancers arise through a series of mutations or genetic alterations that give the cell the ability to override pro-apoptotic and anti-proliferative signals, allowing it to reach the hallmarks of replicative immortality, invasion, and metastasis [1,2,3].
Several molecular mechanisms work to make it possible for cells to acquire genetic changes, whether at the level of nucleotides or chromosomes. Tumorigenesis is seen as an imbalance between cell cycle control, rates of mutation acquisition, and the loss of functions in tumor suppressor genes [4,5].
Genomic instability and replicative immortality are hallmarks of cancer cells [6,7,8]. In normal cells, once telomere shortening reaches critical levels, a molecular signal is activated, consequently inducing the state of senescence or apoptosis, allowing protection of genome integrity [9,10,11,12]. Short telomeres and high levels of telomerase expression are often reported in human cancers as an intrinsic consequence of tumor genomic instability [13,14,15].
Telomere critical shortening, and consequently genomic instability, is avoided by the activation of the response to DNA damage. DNA damage causes a halt in cell cycle progression, and there are checkpoint proteins that block this progression to the S phase so that the genetic material is repaired. If the DNA damage is extensive, making it impossible to repair, then the pathways to trigger senescence and death are activated [9,15,16]. The beginning and progression of the carcinogenesis process is marked by the loss of function of DNA repair genes, which contributes to genomic instability, promoting cancer progression [17,18,19].
The study of molecular mechanisms and the genetic pathways that lead to tumor genomic instability is a challenge and has been widely studied over the years in several tumor models [3,13]. WRAP53 is responsible for an antisense transcript of p53 and also encodes a protein with WD40 domains that acts as a scaffold protein participating in important cellular events such as telomerase assembly, the formation of Cajal bodies, and DNA double-strand break repair [20,21,22].
WD40 repeat motifs (WDRs) range from 40 to 60 amino acids, containing a conserved glycine-histidine motif at the beginning and being terminated with tryptophan dipeptides (W) and aspartic acid (D). Interaction with multiprotein complexes occurs in their existing WD40 repeats within a domain [23,24,25]. Several WD-repeat proteins are encoded in the human genome and are involved in cellular activities such as chromatin assembly, gene transcription, RNA metabolism, cell cycle regulation, and apoptosis [23,24,25,26,27,28]. WD-repeat proteins are already known to be involved in tumorigenesis (Receptor for Activated C Kinase 1 (RACK1), cilia and flagella associated protein 52 (WDRPUH), Endonuclein (PWP1) and serine/threonine kinase receptor-associated protein (STRAP)) and also act as tumor suppressants (F-box and WD repeat domain containing 7 (FBW7) and serina/treonina quinase 11 (STK11)) [29,30,31,32,33,34].
Mutations in WRAP53β are responsible for disorders such as spinal muscular atrophy (SMA), a neurodegenerative disease that in its most common form causes death by age two, and congenital dyskeratosis, a biological disorder associated with telomere shortening. Mutations in its WD40 domain impair telomerase traffic to telomeres, resulting in their progressive shortening. Overexpression of WRPA53 is linked to carcinogenic transformation, indicating an oncogenic property [35,36,37,38,39,40,41,42,43].
In this context, it is of great importance that we always strive for innovation in the search of new strategies for cancer management. The identification of new biomarkers that may be efficiently targeted and provide a significant improvement to a patient’s prognosis is a crucial step in this search and a current goal in many oncologic studies [44]. In this review, we seek to discuss the cellular roles of WRAP53, its possible pathways in carcinogenesis as an oncogene, and a molecular biomarker to be investigated in cancer prognoses.
2. WRAP53 Characterization and Cellular Roles
The WRAP53 gene is found in chromosome 17 and codifies both an antisense transcript for TP53 stabilization (WRAP53α) and a functional protein containing WD40 repeats that regulates telomere elongation and DNA double-strand break repairs (DDRs), referred to as WRAP53β, WDR79, or TCAB1. The WRAP53γ transcript remains, with its functions unknown [22,45,46].
The protein WRAP53β may be found both in the cytoplasm, where it is responsible for translocation of the survival of motor neuron 1 (SMN1) protein across the cell, and in highly active metabolic regions in the nucleus, known as Cajal bodies [36]. Initially described as a nucleolar accessory body, these structures were originally identified in 1903 by Santiago Ramón y Cajal [47].
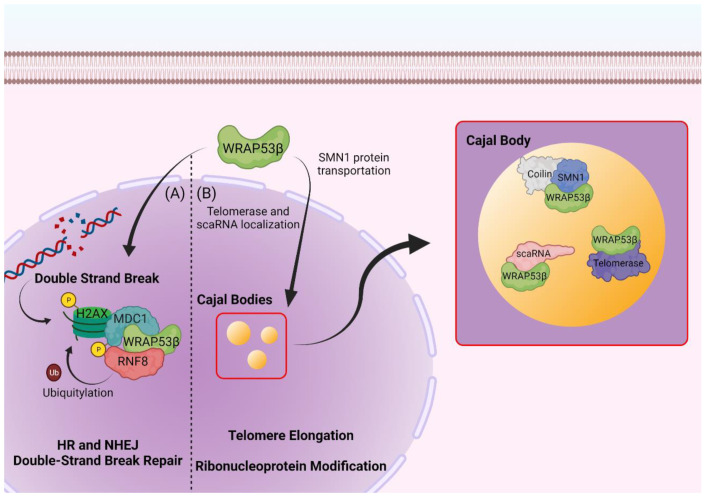
Cajal bodies are involved in important nuclear functions such as ribonucleoprotein maturation, RNA polymerase assembly, and telomerase biogenesis [48,49,50,51]. They are characterized by the presence of the protein coilin which, due to its interaction with other proteins and RNAs, probably plays a structural role in the assembly of Cajal bodies (Figure 1) [52,53]. Reductions in cellular levels of WRAP53β or its overexpression lead to the rupture of these bodies and prevents the formation of new Cajal bodies, also causing an incorrect location of coilin to occur in the nucleoli [36]. These structures are composed of a diversity of specific ribonucleoproteins (RNPs) that are complexes composed of a non-coding RNA and its associated proteins. This includes small nuclear spliceosomal RNPs (snRNPs), Cajal body specific RNPs (scaRNPs), nucleolar RNPs (snoRNPs), and RNP telomerase components [35,54,55]. Stable RNAs from eukaryotic cells go through extensive post-transcriptional modifications that are much more abundant in ribosomal RNA (rRNA) and small nuclear RNAs (snRNAs). The modifications to rRNAs are carried out in the cell′s nucleoli by snoRNPs, while snRNAs are guided to Cajal bodies for further modification by scaRNPs [21,54,56].
Figure 1.
WRAP53β roles in cellular homeostasis. (A) WRAP53β mediates MDC1 and RNF8 interaction at DNA double-strand breaks. Phosphorylation of histone H2AX at DNA damage sites by DNA protein kinases induces its binding to MDC1, which in turn binds to RNF8 through WRAP53β-mediated activity. RNF8 then ubiquitylates the phosphorylated histone and triggers recruitment and accumulation of DNA damage repair machinery at the break point. (B) WRAP53β is essential for Cajal body stability and nuclear function maintenance. WRAP53β mediates SMN1 protein localization in Cajal bodies through transport from the cytoplasm to the nucleus. WRAP53β is also responsible for interacting with and ensuring the activity of the metabolic active telomerase enzyme and for correctly localizing scaRNAs to Cajal bodies, where they will mature and suffer post-transcriptional modifications. Created with BioRender.com (accessed on 30 March 2022).
2.1. WRAP53 and Telomerase
WRAP53β associates with scaRNAs as well as telomerase RNA (TERC) and directs them to Cajal bodies for post-transcriptional modifications [21]. C/D box domain scaRNAs are linked to the methylation of snRNAs, while scaRNAs containing H/ACA box domains are responsible for uridine isomerization [20,21,57,58].
TERC or hTR, when used to refer to human telomerase, is an scaRNA of the H/ACA class. The localization of scaRNAs to the Cajal bodies is accomplished through a common element known as the CAB box, where WRAP53β associates directly to promote correct RNA targeting. Mutations in the CAB box that disrupt the interaction of WRAP53β or its depletion result in in a mislocalization of scaRNAs to the nucleoli [20,21,58].
Telomere elongation happens through human telomerase (hTERT) activity, an enzyme that specializes in the synthesis of TTAGGG repeats at the chromosome’s ends [59,60]. Mature telomerase enzyme contains TERC alongside a complex of associated proteins and the telomerase reverse transcriptase (TERT) [6,60]. WRAP53β associates to TERC, localizing the telomerase complex to the Cajal bodies and later to the telomeres themselves [20,21].
Due to its binding to telomerase’s core components but not to the assembly factors, WRAP53β is considered an important active component of the enzyme, as much as it is important for the proper localization of telomerase in Cajal bodies and its activity in proper DDR, which is essential for genomic stability, and mutations that disrupt these functions may be correlated with cancer progression [20,61,62].
2.2. DNA Repair
As a response to DNA double-strand breaks, the cellular machinery has at least five major repair pathways, which are homologous (HR) or non-homologous (NHEJ) repair by nucleotide excision (NER), mismatch repair (MMR), recombination pathway orbase excision repair (BER), and by forming protein complexes that accumulate at sites of damage [17,63,64]. WRAP53β is directly involved in both pathways of double-strand break repair by mediating the interaction of ring finger protein 8 (RNF8) and mediator of DNA damage checkpoint 1 (MDC1) through simultaneously and independently binding to the fork head-associated domains of both proteins [62,65].
The recruitment of ubiquitin-dependent DNA repair factors happens in damage sites where WRAP53β forms a complex with the phosphorylated histone γH2AX alongside MDC1 and RNF8, which is important for RNF8 ubiquitination of proteins in the damaged chromatin and recruitment of the DDR machinery composed of factors such as tumor protein p53 binding protein 1 (TP53BP1), RAD51 recombinase (RAD51), and DNA repair-associated BRCA1 (BRCA1) [17,35,62,65].
The overexpression of WRAP53β allows for a faster repair of double-strand breaks through HR or NHEJ, which points toward the important role of this protein in the orientation of DDR machinery and the maintenance of proper genome integrity [62,66].
2.3. Protein Trafficking
Human SMN1 has been a topic of interest in the health field because despite the wide variety of SMA phenotypes, deletions or intragenic mutations in SMN1 can be found in all forms of SMA [55,67,68,69]. The localization and transport of the SMN1 protein to the Cajal bodies is regulated by WRAP53β, and together with gem (Gemin) 2-8 and STRAP, they form the SMN complex responsible for the assembly of snRNPs in the cytoplasm [35,36].
WRAP53β transports the SMN1 protein after cytoplasmic binding by first recruiting it to the nucleus, where it will facilitate interaction with the nuclear pore importinβ and then reach the Cajal bodies [36].
The exact role of SMN1 in Cajal bodies remains unclear, but it is likely involved in more than the transport of newly assembled snRNPs. Depletion of SMN1 disrupts the Cajal bodies, indicating that SMN is vital for the assembly and activity of these structures [70].
2.4. WRAP53 and Diseases
Due to its participation in several complex cellular processes, WRAP53 seems to act both as a tumor suppressor and as an oncogene. Its nuclear or cytoplasmic location may explain some behaviors, being correlated with the regulation of telomerase, survival, and the regulation of factors that involve DNA repair. WRAP53β dysfunction is linked to many diseases which, when associated with the accumulation of DNA damage or defective repair, contribute to the initiation and progression of tumorigenesis [22,35,36,37,71].
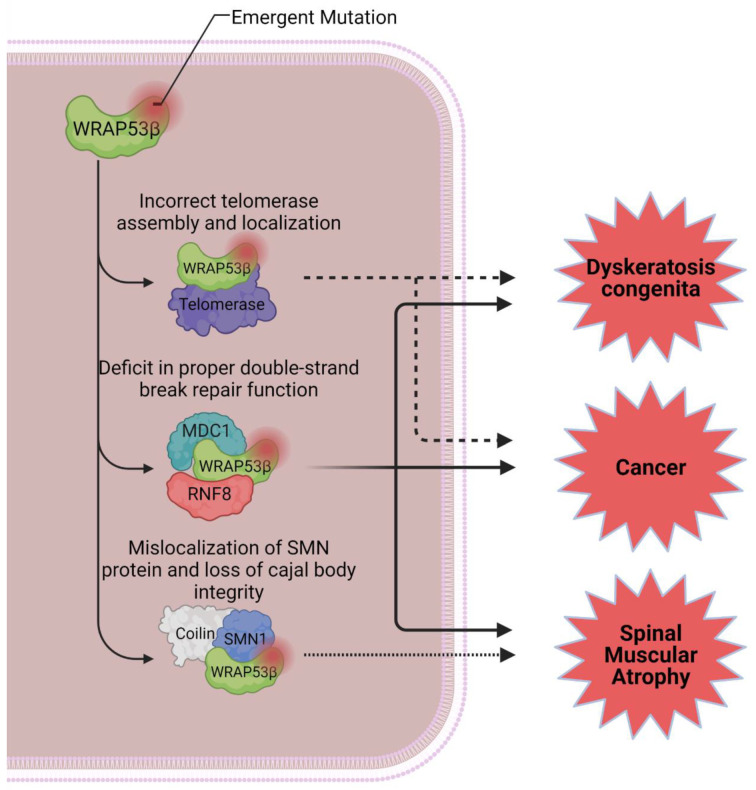
In 1993, WRAP53 was reported for the first time as a driver for dyskeratosis congenita, a metabolic disturbance associated with telomere shortening and characterized in patients by the triad of dysplastic nails, reticular pigmentation of the upper chest or neck, and oral leukoplakia [37]. This rare hereditary condition encompasses many mutations of the telomerase enzymatic complex, which usually results in bone marrow failure and other manifestations in multiple organs, such as lung and liver fibrosis, developmental defects, and cancer [38,39,40].
Eleven genes have been reported to promote dyskeratosis: dyskerin pseudouridine synthase 1 (DKC1), telomerase reverse transcriptase (TERT), telomerase RNA component (TERC), TERF1 interacting nuclear factor 2 (TINF2), WRAP53, NOP10 ribonucleoprotein (NOP10), CST telomere replication complex component 1 (CTC1), regulator of telomere elongation helicase 1 (RTEL1), poly(A)-specific ribonuclease (PARN), NHP2 ribonucleoprotein (NHP2), and tripeptidyl peptidase 1 (TPP1), all associated with telomeric homeostasis [42,43,72,73,74,75].
Mutations in WRAP53β associated with dyskeratosis are all found in the highly conserved domain of WD40 repeats. This domain is one of the most important for WRAP53β activity in a variety of cellular processes, serving as a scaffolding for multiple molecule interactions [38,40,42]. Mutations in the WD40 domain result in decreased WRAP53β nuclear levels., which intervene in telomerase traffic to telomeres, and dysfunctional traffic is reported in the most aggressive form of the disease, as it results in the telomeres’ progressive shortening [42,43,75].
Telomere shortening may be reverted through hTERT activity. However, this enzyme is strictly limited in human cells [6,76]. Telomerase activity and telomere maintenance are related to cell immortality in cancer, germ cells, and embryonic stem cells [7,8,13,77]. A consequence of disruption or loss of telomere function is chromosome instability, which may lead to cancer progression, genetic fusions, karyotype abnormalities, and predicting poor patient prognoses [78,79,80]. Leukemogenesis onset, for example, is highly associated with what happens due to loss of structural integrity in the chromosome ends [81].
WRAP53 implication in leukemias was suggested by Nogueira et al. [82], in which the overexpression of TERT in patients with acute lymphoblastic leukemia (ALL) proved to be a common biomarker indifferent to the ALL subtype. In addition, WRAP53 showed a strong interaction with TERT in a protein–protein interaction (PPI) network. Dysregulated TERT activity was described as one of the many essential factors for leukemia emergence, and it has been depicted as a common alteration in leukemogenesis [83,84,85].
Evaluation of telomerase activity, together with the integrity of the telomeres, has emerged as an important prognostic toll in hematological cancers [86,87,88]. The genomic instability in leukemia derived from telomere disorders is one of the major factors responsible for acquired therapeutic resistance due to karyotype abnormalities and activation of the cell pathways that allow for an escape of the proposed therapeutic mechanisms [89,90,91,92].
Another pathological state associated with WRAP53 mutation-driven pathways is SMA, a disease first described by Werdnig and Hoffmann in 1890 and commonly referred to as the main genetic cause of infant mortality. SMA affects not only motor neurons but also other organs. Respiratory failure is a common cause of SMA in childhood, which in turn can result in death [41,67,93,94].
The reduction in functional SMN1 levels due to defective WRAP53β mediated by defective traffic is seen in severe forms of SMA. The cellular prejudice in this state does not happen due to low availability of SMN1; rather, this is due to defective binding of WRAP53β with SMN1 and the consequent mislocalization of the protein in the cell nucleus [35,36,70].
In addition to progressive telomere shortening, maintenance failures in the Cajal bodies and deficits in WRAP53β-mediated repair of double-strand breaks are also consequences of WRAP53 mutations (Figure 2). These combined deficiencies may explain, in part, the clinical manifestations seen in patients with dyskeratosis and SMA.
Figure 2.
Impacts of WRAP53β mutations in pathological states. Improper binding of WRAP53β to telomerase components leads to progressive shortening of telomeres and is highly implied as a determining factor for the severity of dyskeratosis congenita and for the onset of malignancies. Mutations impairing its ability to mediate DNA double-strand break repairs are also worrisome in the general context of genome stability and may be linked to diverse biological events observed in WRAP53β-deficient cells. Lastly, mutations in WRAP53β or in SMN1 that lead to deficient interactions between the two proteins result in mislocalization of SMN1 in the nucleus and consequent loss of Cajal bodies’ structural integrity, inducing the spinal muscular atrophy phenotype. Created with BioRender.com (accessed 30 March 2022).
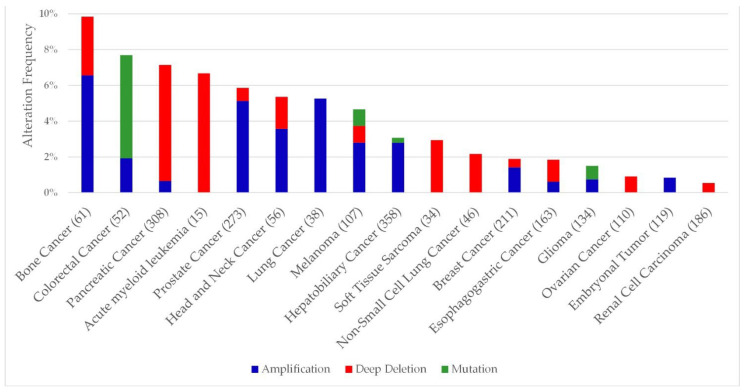
3. WRAP53 as a Potential Novel Biomarker for Cancer
WRAP53 is a natural, highly conserved antisense transcript for the TP53 gene, a well-known oncodriver, meaning that it can regulate TP53 expression through mRNA modulation [22,95,96,97,98]. Dependence on a gene for survival or growth of a cancer cell is known as “oncogene dependence” [99,100]. Genetic alterations such as mutations or deletions involving WRAP53 are present in several types of cancer (Figure 3) (cBioPortal, accessed on 12 August 2022).
Figure 3.
Frequency of genetic alterations present in the WRAP53 gene in cancer cell lines. A minimum change limit of 0.5% was applied in the creation of the graph (cBioPortal, accessed on 12 August 2022). The numbers in parentheses represent the number of patients analyzed.
Thus, WRAP53 overexpression is related not only to carcinogenesis onset but also tumor development and progression, which leads to being pointed out as an oncogene [101]. Table 1 comprises a series of clinical studies that point to malignant onset or the worst patient prognosis due to WRAP53 mutant expression.
Table 1.
WRAP53 abnormal expression or mutation in cancer.
| Cancer Subtype | Biological Samples and Methodology | Molecular Mechanisms | Clinical Status | Clinical Outcome or Overall Survival (OS) | Referen-ce |
|---|---|---|---|---|---|
| NSCLC | Patient samples; A549, H1299 95-C, 95-D, HTB182, and HBE and in vivo | WRAP53β plays an important role in tumorigenesis regulating cell cycle progression and apoptosis. | N.I | N.I | [101] |
| H1299 and A549 cells | WRAP53β induced clonal proliferation through mediation of USP7-MDM2-TP53 pathway. | N.I | N.I | [102] | |
| H1299 and A549 cells | WRAP53β induced clonal proliferation through UHRF1 activity. | N.I | N.I | [103] | |
| Patient samples | WRAP53β overexpression may act as an independent biomarker to predict a poor prognosis. | Patients with primary NSCLC and not previously treated with radiotherapy | WRAP5β expression was an unfavorable prognostic factor related to low overall survival rates. | [104] | |
| Patient samples; A549 and SPC-A-1 cells | Overexpression of WRAP53β reported as a poor prognostic factor, and its downregulation reduced cell proliferation. | Patients with pathological stages I–IV | WRAP53β was present in all patients. | [105] | |
| Esophageal squamous cell carcinoma | Patient samples; KYSE150, KYSE180, EC109, and EC9706 cells | Overexpression of WRAP53β was correlated with tumor infiltration, clinical stage, and lymph node metastasis. | Patient’s selected at the first diagnosis and without the use of radiotherapy | Presence of altered expression of WRAP53β in 95.6% of cases. | [106] |
| Colorectal cancer | Patient samples | WRAP53β is overexpressed in the primary rectal tumor compared with the normal mucosa. | Patients with stages I, IIA+IIIA+IIIB, and IIIC+IV of the disease | In the group without radiotherapy or metastasis, WRAP53β expression was associated with a worse prognosis. | [107] |
| in silico analysis of clinicopathological features | WRAP53β is a biomarker of prognoses for young patients. | Patients with stages: I, II, III, IV, and stage 0 and missing cases | WRAP53β was shown to be differentially expressed between the young and elderly groups. | [108] | |
| Patient samples | Overexpression of cytoplasmic or nuclear WRAP53β is indicative of poor prognosis. | N.I | Patients with high expression of cytoplasmic WRAP53β have a low OS and DFS, while its nuclear presence impairs the radiotherapy response. | [109] | |
| Patient samples | Overexpression WRAP53β is reported for colorectal cancer. | Patients with stages I, II, III, and IV of the disease | Cancer patients in the necrotic state had a strong expression of WRAP53β. | [110] | |
| In silico analysis of TCGA database; SW480, HT-29, HCT116, and LoVo cells and in vivo | The elimination of WRAP53β reduced tumor cell proliferation and invasion. | N.I | Higher expression of WRAP53β was observed in colorectal cancer tissues than in normal tissues. | [111] | |
| Hepatocellular carcinoma | Patient samples | WRAP53α has clinical value as a promising biomarker with precision in primary screening in hepatocarcinoma and HCV. | Patients with primary HCC and patients with chronic HCV infection | Patients with positive WRAP53α RNA are related to a lower DFS. | [112] |
| Ovarian cancer | Patient samples | The rs2287498 polymorphism is associated with increased risk of invasive ovarian cancer. | Patients with invasive epithelial ovarian cancer in non-Hispanic white women | N.I | [113] |
| Patient samples; A2780 and SKOV-3 cells | Low nuclear expression of WRAP53β correlates with aggressiveness and poor prognosis of epithelial ovarian cancer. | Patients with serous, endometrioid, mucinous, and other tumors | Aggressive disease, poor prognosis, and reduced survival of the patients. | [114] | |
| Patient samples | SNPs located in WRAP53-TP53 regions rs1042522, rs2287497, and rs2287498 are more strongly associated with a risk of ovarian cancer. | N.I | N.I | [115] | |
| Breast cancer | Patient samples | WRAP53β was shown to be a potential prognostic biomarker. | Patients with a primary breast tumor | The cellular localization of WRAP53β is linked to prognosis and OS. | [116] |
| Patient samples | Polymorphisms linked to TP53 or WRAP53 rs2287499 and rs2287498 may be associated with estrogen receptor (ER)-negative breast cancer. | Patients with stage I and II disease and invasive breast cancer | N.I | [117] | |
| Patient samples and in silico analysis | SNPs rs2287499 and rs1042522 may play an important role in breast cancer susceptibility. | N.I | N.I | [118] | |
| Head and neck carcinomas | Patient samples; U2OS, HeLa, H1299, HEK293, HCT116, HDF, AG06814, and MCF10A cells | Overexpression of WRAP53β is a marker of poor prognosis. | N.I | WRAP53β expression levels were higher in patients with recurrent disease. | [119] |
| Patient samples; HSC-3, Cal-27, and CNE1 ACC2 cells and in vivo | WRAP53β is overexpressed in clinical specimens as well as carcinoma cell lines. | Human nasopharyngeal carcinoma tissue samples and nasopharyngitis tissues | N.I | [120] | |
| Patient samples | Cytoplasmic WRAP53β is a potential predictive marker for poor response to chemoradiotherapy. | Patients treated for primary stage T2N0 or T3N0 glottic laryngeal SCC | A worse DFS and a tendency for worse OS in those patients where WRAP53β was more present in the cytoplasm compared with patients with nuclear staining. | [121] | |
| Patient samples; LK0412 and LK0949 cells | WRAP53β plays an important role in radiotherapy response, and its nuclear localization may be a promising biomarker for overall survival. | Patients with stages T1,T2,T3, N0, N1, and N2 | Patients with nuclear expression of WRAP53β demonstrated greater overall survival than those with non-nuclear staining. | [122] | |
| Hep-2 cells | WRAP53β can be an ideal target for increasing radiosensitivity. | N.I | N.I | [123] | |
| Testicular germ cell tumors | In silico analysis of 168 unique telomere-related genes | Overexpression of WRAP53 can induce telomere lengthening. | Primary tumor samples | In testicular germ cell tumors of the non-seminoma, subtype WRAP53 was overexpressed. | [124] |
| Nasopharyngeal carcinoma associated with EBV | Patient samples; CNE1, CNE1-LMP1, NP69, HOK, and B95-8 cells | EBV increases the expression of WRAP53β in vitro and, consequently, overactivates the enzymatic activity of telomerase. Its downregulation reduced cell proliferation. | N.I | N.I | [125] |
WRAP53: WD repeat containing antisense to TP53; NSCLC: non-small cell lung cancer; USP7: ubiquitin specific peptidase 7; MDM2: MDM2 proto-oncogene; TP53: tumor protein p53; UHRF1: ubiquitin-like with PHD and ring finger domains 1; SNPs: single-nucleotide polymorphisms; EBV: Epstein–Barr virus; OS: overall survival; N.I: not informed; DFS: disease-free survival; HCC: hepatocellular carcinoma; HCV: Hepatitis C virus.
A total of 25 articles was included in this review which described the results in patients affected by different types of cancer, such as lung (5), esophageal (1), colorectal (5), hepatocellular (1), ovarian (3), and breast cancer (3), head and neck carcinomas (5), testicular germ cell tumors (1), and nasopharyngeal cancer (1), in addition to studies with cell lines and in vivo models. These data show a WRAP53 correlation, with important tumorigenesis events highlighted for lung cancer, head and neck tumors, and colorectal carcinomas. We especially focused our discussion on showing the different roles of WRAP53 in cell biology, showing that structural alterations or alterations in its expression levels can lead to a tumorigenesis process while, on the other hand, its regulation proves to be beneficial in cancer prognosis.
4. WRAP53 as a Prognostic Factor in Cancer
Abnormal cellular molecular pathways triggering uncontrolled cell proliferation is one of the main recent research topics in cancer. Currently, the overexpression of WRAP53 transcripts has been pointed out as a biomarker for a large cohort of cancer subtypes, such as colorectal, hepatocellular, head and neck, breast, ovarian, and esophageal squamous cell cancers [106,107,108,112,114,116,119,120].
Kamel et al. [112] analyzed WRAP53α expression in conjunction with other prognostic factors and showed that high expression can serve as a novel diagnostic and prognostic biomarker in hepatocellular carcinoma (HCC) and hepatitis C (HCV). In addition, WRAP53α was useful in verifying recurrence-free survival that considers the time from diagnosis to the development of the first evidence of the disease. About 60% of patients who are diagnosed with HCC are at an advanced disease stage with the occurrence of metastases, since early disease detection usually fails due to the absence of specific symptoms. However, patients who are diagnosed at an early stage have a 3-year survival global rate with surgical intervention of >93%, and thus, biomarkers allowing the detection of HCC at an early stage are necessary to improve the prognoses of these patients [126,127,128].
Overexpression of WRAP53β is observed in a wide range of human cancer cell lines [119]. Recent studies indicate that its overexpression is also related to telomerase activation and the depth of tumor invasion and lymph node metastasis, suggesting a potential role of WRAP53β in cellular mobility and immortality and partly explaining its oncogenic properties, as telomerase reactivation is reported in 90% of all human cancers [106,111,124,129].
Aside from being reported in primary colorectal cancer tumors, overexpression of WRAP53β has also been reported in rectal tumors with ongoing necrosis and is indicated as a poor prognostic factor [107,110]. In colorectal cancer, tumor necrosis is observed in more advanced stages of the disease and is a marker of poor prognosis [130,131].
In non-small cell lung cancer (NSCLC), overexpression of WRAP53β promoted cell proliferation [101,102,103]. It was observed that WRAP53β localized and interacted with USP7, reducing the ubiquitination of MDM2 proto-oncogene (MDM2) and p53, prolonging its half-life and increasing its stability [102]. It is already known that proteins with WD40 repeats play an important role in the ubiquitin–proteasome processes, allowing the formation of multiple protein complexes [25,132,133]. Until then, this was an unknown function of WRAP53β.
On the other hand, WRAP53β knockdown impairs the growth of cancer cells, inducing cell cycle arrest and apoptosis through mitochondrial pathways. This decreases the potential for invasion both in vitro and in vivo and increases the radiosensitivity of these cells [101,105,106,107,111,119,120,123], but it has no effect on the radiosensitivity of normal human fibroblasts, which indicates that cancer cells are overly dependent on WRAP53β [119]. In addition, the knockdown of WRAP53β in cancer cells induces massive apoptosis within 48 h to 72 h, reducing tumor growth [101,105,111,119,120,123], while compared with telomerase, silencing this result is expected within 4 weeks [134].
The knockdown effects of WRAP53β on NSCLC are related to negative regulation of cyclins (cyclin D1 and cyclin E), CDKs (CDK2, CDK4, and CDK6) and checkpoint proteins P-RbS795 and S807/811 [101,105]. It is already known that one of the processes for the cell cycle to occur is the activation of protein kinase followed by cyclins and CDKs [135]. Negative regulation of WRAP53β induced a stop in the G1 phase of the cell cycle, which in turn prevented progression to phase S [101,105,111]. Apoptosis mediated by WRAP53β occurs through the activation of caspase-9 and caspase-3 [101], which is consistent with other studies [119,120].
Yuan et al. [105] identified 534 proteins interacting with WRAP53β using A549 cells through bioinformatics tools and identified the following proteins: DKC1, GAR1, RUVBLI, HSPA2, and PKM, which are proteins that function in the processing and modification of the rRNA, components of RNA polymerase II, and delivery of aminoacyl tRNAs and participate in aerobic glycolysis [136,137,138,139]. The interaction of WRAP53β with these key proteins provides new insights into the understanding and new discoveries of mechanisms of interaction.
Furthermore, microarray data of the head and neck carcinomas cellular line shows that WRAP53β might affect multiple processes and cellular pathways, such as the p53 signaling pathway, apoptosis pathway, cell cycle, JAK-STAT signaling pathway, and PI3K-AKT signaling pathway [120]. As previously mentioned, WRAP53β depletion affects cancer cell survival by influencing proliferation and apoptosis. Therefore, its involvement in these pathways was expected. The dysregulation of the pathways associated with these biological processes is related to neoplasms and autoimmune diseases [140,141,142,143].
WRAP53β expression is related to the depth of tumor invasion [106]. In vitro studies indicated that WRAP53β knockdown in different cell lines (Cal-27, ACC2, HSC-3, and HCT116) reduced the tumor cell invasion capacity, showing that WRAP53β influences and facilitates tumor cell invasion [111,120]. Invasion is one of the main features present in advanced-stage tumors in several cancer subtypes [144,145,146].
Zhu et al. [111] evaluated the oncogenic potential of WRAP53β using animal models with colorectal cancer where, after removal of the xenografts, it was observed that animals with knockout of WRAP53β expression showed a decrease in the formation and growth of tumor cells. The in vivo findings are consistent with the studies of Sun et al. [120], who also evaluated this potential using xenografts in mice with oral squamous cell carcinoma Cal-27 cells. The analysis revealed that both the volume and weight of the tumors were significantly lower in the WRAP53β knockdown mice when compared with the control group.
The first time WRAP53 was described in cancer was after an analysis of the common genetic variation of TP53 and its flanking genes, and these data showed that the single nucleotide polymorphisms (SNPs) rs2287499 and rs2287498 were significantly linked to increased development of ER-negative breast cancer [117], and the same rs2287498 SNPs have also been linked to aggressive ovarian cancer [113,115]. The presence of SNPs in the WRAP53 gene generates an amino acid change, namely rs2287499 (R68G), an Arg/Gly polymorphism, and rs2287498 (F150F), a Phe/Phe polymorphism [113,117,118], and the presence of these alterations in TP53 and WRAP53 may affect their products, causing a vulnerability to cancer and failure to respond to therapy [115,147]. Epidemiological studies have extensively discussed the involvement of polymorphisms in a variety of cancers [148,149,150].
To analyze the potential of WRAP53β in selecting suitable patients for radiotherapy, Qiu et al. [123] analyzed the effects of its knockdown and associated it with an effective radiotherapy response. Since primary tumors have an increased expression of WRAP53β, radiotherapy may not be effective [107]. Its subcellular location is also taken into account in the evaluation of patients who benefit or do not benefit from radiotherapy. The nuclear localization of WRAP53β is associated with a better response to radiotherapy and a better course of the disease [116,122], while the predominant cytoplasmic location may be a predictive marker of poor response and lower disease-free survival rate [109,121]. Since 60% of tumor patients receive irradiation as part of their treatment [151], a biomarker to select suitable patients for radiotherapy is of extreme relevance.
Hedström et al. [114] demonstrated that low nuclear expression of WRAP53β is correlated with a fourfold increased risk of death from ovarian cancer. Low levels of nuclear expression showed a deregulation of the factors involved in the response to DNA damage, which in turn resulted in an increase in genomic instability. This is consistent with studies that have shown that the loss of the WRAP53β protein results in defective repair of DNA double-strand breaks [62].
Wang et al. [125] reported that the EBV increased the expression of WRAP53β in vitro, which is also likely associated with the overactivation of telomerase, and the involvement of WRAP53β in DNA damage repair pathways may partly account for its overexpression in EBV infections associated with nasopharyngeal carcinoma. One of the mechanisms by which EBV induces cellular immortality is the overactivation of telomerase in both epithelial cells and B lymphocytes through its main oncoprotein LMP-1 [152,153,154,155]. In particular, LMP-1 has been reported to activate TERT via the PI3K-AKT pathway [156].
In short, high levels of WRAP53 transcripts were observed to be present in a variety of tumor cell lines. In addition, WRAP53β knockdown is associated with in vivo tumor reduction and the induction of apoptosis of tumor cell lines. Human tumor cells are sensitive to WRAP53β inhibition. These findings highlight the role of WRAP53 in cancer, both in vitro and in vivo, and present it as a potentially promising new target for cancer therapy.
5. Conclusions
The clinical and experimental data analyzed in this review demonstrate that excessive telomere shortening, accented telomerase activity, and WRAP53β overexpression are present in a diverse subset of malignant phenotypes. Its different locations and functions render this protein as involved in several important cellular processes, such as the organization and formation of Cajal bodies, repair of DNA double-strand breaks, and the interaction and localization of hTERT and TP53. In addition to being commonly reported in cancer, loss of WRAP53β has been associated with dyskeratosis congenita and SMA. However, more clinical and experimental investigations are still needed for a better understanding of the role of WRAP53 and its transcripts in the mechanisms involved in tumorigenesis so that it may be addressed as potential new biomarker in cancer and a target in the development of new treatments.
Author Contributions
Invitation received, C.A.M.-N.; conceptualization, R.B.G., C.B.M. and C.A.M.-N.; provision of data and subsequent analysis and interpretation, R.B.G., C.B.M., L.d.C.P., F.M.C.d.P.P., I.V.B., L.d.C.P., R.M.R., M.O.d.M.F., M.E.A.d.M., A.S.K. and C.A.M.-N.; writing—original draft preparation, R.B.G., C.B.M. and C.A.M.-N.; writing—review and editing, R.B.G., C.B.M. and C.A.M.-N.; funding acquisition, A.S.K. and C.A.M.-N. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or data interpretation; in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This study was supported by the Brazilian funding agencies Coordination for the Improvement of Higher Education Personnel (CAPES) to C.B.M., the National Council of Technological and Scientific Development (CNPq grant number 404213/2021-9 to C.A.M.-N. and Productivity in Research PQ scholarships to M.O.d.M.F., M.E.A.d.M., and A.S.K.), and the Cearense Foundation of Scientific and Technological Support (FUNCAP grant number P20-0171-00078.01.00/20 to F.M.C.d.P.P., M.O.d.M.F., and C.A.M.-N.). We also thank PROPESP/UFPA for the publication payment.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hanahan D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022;12:31–46. doi: 10.1158/2159-8290.CD-21-1059. [DOI] [PubMed] [Google Scholar]
- 2.Hanahan D., Weinberg R.A. Hallmarks of Cancer: The Next Generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Hanahan D., Weinberg R.A. The Hallmarks of Cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 4.Basu A. DNA Damage, Mutagenesis and Cancer. Int. J. Mol. Sci. 2018;19:970. doi: 10.3390/ijms19040970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kopnin B.P. Targets of Oncogenes and Tumor Suppressors: Key for Understanding Basic Mechanisms of Carcinogenesis. Biochemistry. 2000;65:2–27. [PubMed] [Google Scholar]
- 6.McNally E.J., Luncsford P.J., Armanios M. Long Telomeres and Cancer Risk: The Price of Cellular Immortality. J. Clin. Investig. 2019;129:3474–3481. doi: 10.1172/JCI120851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vogelstein B., Kinzler K.W. The Path to Cancer—Three Strikes and You’re Out. N. Engl. J. Med. 2015;373:1895–1898. doi: 10.1056/NEJMp1508811. [DOI] [PubMed] [Google Scholar]
- 8.Shay J.W. Telomerase and Cancer. Hum. Mol. Genet. 2001;10:677–685. doi: 10.1093/hmg/10.7.677. [DOI] [PubMed] [Google Scholar]
- 9.De Lange T. Telomere-Related Genome Instability in Cancer. Cold Spring Harb. Symp. Quant. Biol. 2005;70:197–204. doi: 10.1101/sqb.2005.70.032. [DOI] [PubMed] [Google Scholar]
- 10.Jafri M.A., Ansari S.A., Alqahtani M.H., Shay J.W. Roles of Telomeres and Telomerase in Cancer, and Advances in Telomerase-Targeted Therapies. Genome Med. 2016;8:69. doi: 10.1186/s13073-016-0324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kong F., Zheng C., Xu D. Telomerase as a “Stemness” Enzyme. Sci. China Life Sci. 2014;57:564–570. doi: 10.1007/s11427-014-4666-6. [DOI] [PubMed] [Google Scholar]
- 12.Palm W., de Lange T. How Shelterin Protects Mammalian Telomeres. Annu. Rev. Genet. 2008;42:301–334. doi: 10.1146/annurev.genet.41.110306.130350. [DOI] [PubMed] [Google Scholar]
- 13.Barthel F.P., Wei W., Tang M., Martinez-Ledesma E., Hu X., Amin S.B., Akdemir K.C., Seth S., Song X., Wang Q., et al. Systematic Analysis of Telomere Length and Somatic Alterations in 31 Cancer Types. Nat. Genet. 2017;49:349–357. doi: 10.1038/ng.3781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang K., Liu T., Liu L., Liu J., Liu C., Wang C., Ge N., Ren H., Yan K., Hu S., et al. TERT Promoter Mutations in Renal Cell Carcinomas and Upper Tract Urothelial Carcinomas. Oncotarget. 2014;5:1829–1836. doi: 10.18632/oncotarget.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muñoz-Espín D., Serrano M. Cellular Senescence: From Physiology to Pathology. Nat. Rev. Mol. Cell Biol. 2014;15:482–496. doi: 10.1038/nrm3823. [DOI] [PubMed] [Google Scholar]
- 16.Kastan M.B., Bartek J. Cell-Cycle Checkpoints and Cancer. Nature. 2004;432:316–323. doi: 10.1038/nature03097. [DOI] [PubMed] [Google Scholar]
- 17.Chatterjee N., Walker G.C. Mechanisms of DNA Damage, Repair, and Mutagenesis. Environ. Mol. Mutagen. 2017;58:235–263. doi: 10.1002/em.22087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nagy Á., Munkácsy G., Győrffy B. Pancancer Survival Analysis of Cancer Hallmark Genes. Sci. Rep. 2021;11:6047. doi: 10.1038/s41598-021-84787-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carter S.L., Eklund A.C., Kohane I.S., Harris L.N., Szallasi Z. A Signature of Chromosomal Instability Inferred from Gene Expression Profiles Predicts Clinical Outcome in Multiple Human Cancers. Nat. Genet. 2006;38:1043–1048. doi: 10.1038/ng1861. [DOI] [PubMed] [Google Scholar]
- 20.Venteicher A.S., Abreu E.B., Meng Z., McCann K.E., Terns R.M., Veenstra T.D., Terns M.P., Artandi S.E. A Human Telomerase Holoenzyme Protein Required for Cajal Body Localization and Telomere Synthesis. Science. 2009;323:644–648. doi: 10.1126/science.1165357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tycowski K.T., Shu M.-D., Kukoyi A., Steitz J.A. A Conserved WD40 Protein Binds the Cajal Body Localization Signal of ScaRNP Particles. Mol. Cell. 2009;34:47–57. doi: 10.1016/j.molcel.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahmoudi S., Henriksson S., Corcoran M., Méndez-Vidal C., Wiman K.G., Farnebo M. Wrap53, a Natural P53 Antisense Transcript Required for P53 Induction upon DNA Damage. Mol. Cell. 2009;33:462–471. doi: 10.1016/j.molcel.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 23.Stirnimann C.U., Petsalaki E., Russell R.B., Müller C.W. WD40 Proteins Propel Cellular Networks. Trends Biochem. Sci. 2010;35:565–574. doi: 10.1016/j.tibs.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Xu C., Min J. Structure and Function of WD40 Domain Proteins. Protein Cell. 2011;2:202–214. doi: 10.1007/s13238-011-1018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schapira M., Tyers M., Torrent M., Arrowsmith C.H. WD40 Repeat Domain Proteins: A Novel Target Class? Nat. Rev. Drug Discov. 2017;16:773–786. doi: 10.1038/nrd.2017.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li D., Roberts R. Human Genome and Diseases:¶WD-Repeat Proteins: Structure Characteristics, Biological Function, and Their Involvement in Human Diseases. Cell. Mol. Life Sci. 2001;58:2085–2097. doi: 10.1007/PL00000838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suganuma T., Pattenden S.G., Workman J.L. Diverse Functions of WD40 Repeat Proteins in Histone Recognition: Figure 1. Genes Dev. 2008;22:1265–1268. doi: 10.1101/gad.1676208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jain B.P., Pandey S. WD40 Repeat Proteins: Signalling Scaffold with Diverse Functions. Protein J. 2018;37:391–406. doi: 10.1007/s10930-018-9785-7. [DOI] [PubMed] [Google Scholar]
- 29.Xie X., Wang Z., Chen Y. Association of LKB1 with a WD-Repeat Protein WDR6 Is Implicated in Cell Growth Arrest and P27Kip1 Induction. Mol. Cell Biochem. 2007;301:115–122. doi: 10.1007/s11010-006-9402-5. [DOI] [PubMed] [Google Scholar]
- 30.Welcker M., Clurman B.E. FBW7 Ubiquitin Ligase: A Tumour Suppressor at the Crossroads of Cell Division, Growth and Differentiation. Nat. Rev. Cancer. 2008;8:83–93. doi: 10.1038/nrc2290. [DOI] [PubMed] [Google Scholar]
- 31.Halder S.K., Anumanthan G., Maddula R., Mann J., Chytil A., Gonzalez A.L., Washington M.K., Moses H.L., Beauchamp R.D., Datta P.K. Oncogenic Function of a Novel WD-Domain Protein, STRAP, in Human Carcinogenesis. Cancer Res. 2006;66:6156–6166. doi: 10.1158/0008-5472.CAN-05-3261. [DOI] [PubMed] [Google Scholar]
- 32.Honoré B., Baandrup U., Nielsen S., Vorum H. Endonuclein Is a Cell Cycle Regulated WD-Repeat Protein That Is up-Regulated in Adenocarcinoma of the Pancreas. Oncogene. 2002;21:1123–1129. doi: 10.1038/sj.onc.1205186. [DOI] [PubMed] [Google Scholar]
- 33.Adams D.R., Ron D., Kiely P.A. RACK1, A Multifaceted Scaffolding Protein: Structure and Function. Cell Commun. Signal. 2011;9:22. doi: 10.1186/1478-811X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva F.P., Hamamoto R., Nakamura Y., Furukawa Y. WDRPUH, A Novel WD-Repeat—Containing Protein, Is Highly Expressed in Human Hepatocellular Carcinoma and Involved in Cell Proliferation. Neoplasia. 2005;7:348–355. doi: 10.1593/neo.04544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Henriksson S., Farnebo M. On the Road with WRAP53Î2: Guardian of Cajal Bodies and Genome Integrity. Front. Genet. 2015;6:91. doi: 10.3389/fgene.2015.00091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahmoudi S., Henriksson S., Weibrecht I., Smith S., Söderberg O., Strömblad S., Wiman K.G., Farnebo M. WRAP53 Is Essential for Cajal Body Formation and for Targeting the Survival of Motor Neuron Complex to Cajal Bodies. PLoS Biol. 2010;8:e1000521. doi: 10.1371/journal.pbio.1000521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Savage S.A. In: Dyskeratosis Congenita. Adam M.P., Everman D.B., Mirzaa G.M., Pagon R.A., Wallace S.E., Bean L.J.H., Gripp K.W., Amemiya A., editors. GeneReviews®, University of Washington; Seattle, WA, USA: 1993. [Google Scholar]
- 38.Bergstrand S., Böhm S., Malmgren H., Norberg A., Sundin M., Nordgren A., Farnebo M. Biallelic Mutations in WRAP53 Result in Dysfunctional Telomeres, Cajal Bodies and DNA Repair, Thereby Causing Hoyeraal–Hreidarsson Syndrome. Cell Death Dis. 2020;11:238. doi: 10.1038/s41419-020-2421-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Magnusson T., Godby R.C., Bachiashvili K., Jamy O. First Report of Novel Heterozygous WRAP53 p.Ala522Glyfs*8 Mutation Associated Dyskeratosis Congenita. Br. J. Haematol. 2022;196:27–29. doi: 10.1111/bjh.17883. [DOI] [PubMed] [Google Scholar]
- 40.Shao Y., Feng S., Huang J., Huo J., You Y., Zheng Y. A Unique Homozygous WRAP53 Arg298Trp Mutation Underlies Dyskeratosis Congenita in a Chinese Han Family. BMC Med. Genet. 2018;19:40. doi: 10.1186/s12881-018-0549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barkats M. Amyotrophie Spinale Infantile. Médecine/Sci. 2020;36:137–140. doi: 10.1051/medsci/2020010. [DOI] [PubMed] [Google Scholar]
- 42.Zhong F., Savage S.A., Shkreli M., Giri N., Jessop L., Myers T., Chen R., Alter B.P., Artandi S.E. Disruption of Telomerase Trafficking by TCAB1 Mutation Causes Dyskeratosis Congenita. Genes Dev. 2011;25:11–16. doi: 10.1101/gad.2006411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dokal I. Dyskeratosis Congenita. Hematology. 2011;2011:480–486. doi: 10.1182/asheducation-2011.1.480. [DOI] [PubMed] [Google Scholar]
- 44.Kansagra A., Dahiya S., Litzow M. Continuing Challenges and Current Issues in Acute Lymphoblastic Leukemia. Leuk. Lymphoma. 2018;59:526–541. doi: 10.1080/10428194.2017.1335397. [DOI] [PubMed] [Google Scholar]
- 45.Venteicher A.S., Artandi S.E. TCAB1: Driving Telomerase to Cajal Bodies. Cell Cycle. 2009;8:1329–1331. doi: 10.4161/cc.8.9.8288. [DOI] [PubMed] [Google Scholar]
- 46.Farnebo M. Wrap53, a Novel Regulator of P53. Cell Cycle. 2009;8:2343–2346. doi: 10.4161/cc.8.15.9223. [DOI] [PubMed] [Google Scholar]
- 47.Gall J.G. The Centennial of the Cajal Body. Nat. Rev. Mol. Cell Biol. 2003;4:975–980. doi: 10.1038/nrm1262. [DOI] [PubMed] [Google Scholar]
- 48.Gall J.G. Cajal Bodies: The First 100 Years. Annu. Rev. Cell Dev. Biol. 2000;16:273–300. doi: 10.1146/annurev.cellbio.16.1.273. [DOI] [PubMed] [Google Scholar]
- 49.Cristofari G., Adolf E., Reichenbach P., Sikora K., Terns R.M., Terns M.P., Lingner J. Human Telomerase RNA Accumulation in Cajal Bodies Facilitates Telomerase Recruitment to Telomeres and Telomere Elongation. Mol. Cell. 2007;27:882–889. doi: 10.1016/j.molcel.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 50.Cioce M., Lamond A.I. Cajal Bodies: A Long History of Discovery. Annu. Rev. Cell Dev. Biol. 2005;21:105–131. doi: 10.1146/annurev.cellbio.20.010403.103738. [DOI] [PubMed] [Google Scholar]
- 51.Lafarga M., Tapia O., Romero A.M., Berciano M.T. Cajal Bodies in Neurons. RNA Biol. 2017;14:712–725. doi: 10.1080/15476286.2016.1231360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Machyna M., Neugebauer K.M., Staněk D. Coilin: The First 25 Years. RNA Biol. 2015;12:590–596. doi: 10.1080/15476286.2015.1034923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tucker K.E., Berciano M.T., Jacobs E.Y., LePage D.F., Shpargel K.B., Rossire J.J., Chan E.K.L., Lafarga M., Conlon R.A., Matera A.G. Residual Cajal Bodies in Coilin Knockout Mice Fail to Recruit Sm SnRNPs and SMN, the Spinal Muscular Atrophy Gene Product. J. Cell Biol. 2001;154:293–308. doi: 10.1083/jcb.200104083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kiss T. Biogenesis of Small Nuclear RNPs. J. Cell Sci. 2004;117:5949–5951. doi: 10.1242/jcs.01487. [DOI] [PubMed] [Google Scholar]
- 55.Praveen K., Wen Y., Gray K.M., Noto J.J., Patlolla A.R., van Duyne G.D., Matera A.G. SMA-Causing Missense Mutations in Survival Motor Neuron (Smn) Display a Wide Range of Phenotypes When Modeled in Drosophila. PLoS Genet. 2014;10:e1004489. doi: 10.1371/journal.pgen.1004489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Deryusheva S., Gall J.G. ScaRNAs and SnoRNAs: Are They Limited to Specific Classes of Substrate RNAs? RNA. 2019;25:17–22. doi: 10.1261/rna.068593.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kiss T. Small Nucleolar RNAs. Cell. 2002;109:145–148. doi: 10.1016/S0092-8674(02)00718-3. [DOI] [PubMed] [Google Scholar]
- 58.Richard P. A Common Sequence Motif Determines the Cajal Body-Specific Localization of Box H/ACA ScaRNAs. EMBO J. 2003;22:4283–4293. doi: 10.1093/emboj/cdg394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Herrmann M., Pusceddu I., März W., Herrmann W. Telomere Biology and Age-Related Diseases. Clin. Chem. Lab. Med. (CCLM) 2018;56:1210–1222. doi: 10.1515/cclm-2017-0870. [DOI] [PubMed] [Google Scholar]
- 60.Artandi S.E., DePinho R.A. Telomeres and Telomerase in Cancer. Carcinogenesis. 2010;31:9–18. doi: 10.1093/carcin/bgp268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jády B.E., Richard P., Bertrand E., Kiss T. Cell Cycle-Dependent Recruitment of Telomerase RNA and Cajal Bodies to Human Telomeres. Mol. Biol. Cell. 2006;17:944–954. doi: 10.1091/mbc.e05-09-0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Henriksson S., Rassoolzadeh H., Hedström E., Coucoravas C., Julner A., Goldstein M., Imreh G., Zhivotovsky B., Kastan M.B., Helleday T., et al. The Scaffold Protein WRAP53β Orchestrates the Ubiquitin Response Critical for DNA Double-Strand Break Repair. Genes Dev. 2014;28:2726–2738. doi: 10.1101/gad.246546.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Iyama T., Wilson D.M. DNA Repair Mechanisms in Dividing and Non-Dividing Cells. DNA Repair. 2013;12:620–636. doi: 10.1016/j.dnarep.2013.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ciccia A., Elledge S.J. The DNA Damage Response: Making It Safe to Play with Knives. Mol. Cell. 2010;40:179–204. doi: 10.1016/j.molcel.2010.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rassoolzadeh H., Coucoravas C., Farnebo M. The Proximity Ligation Assay Reveals That at DNA Double-Strand Breaks WRAP53β Associates with ΓH2AX and Controls Interactions between RNF8 and MDC1. Nucleus. 2015;6:417–424. doi: 10.1080/19491034.2015.1106675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rassoolzadeh H., Böhm S., Hedström E., Gad H., Helleday T., Henriksson S., Farnebo M. Overexpression of the Scaffold WD40 Protein WRAP53β Enhances the Repair of and Cell Survival from DNA Double-Strand Breaks. Cell Death Dis. 2016;7:e2267. doi: 10.1038/cddis.2016.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lefebvre S., Bürglen L., Reboullet S., Clermont O., Burlet P., Viollet L., Benichou B., Cruaud C., Millasseau P., Zeviani M., et al. Identification and Characterization of a Spinal Muscular Atrophy-Determining Gene. Cell. 1995;80:155–165. doi: 10.1016/0092-8674(95)90460-3. [DOI] [PubMed] [Google Scholar]
- 68.Rochette C., Gilbert N., Simard L. SMN Gene Duplication and the Emergence of the SMN2 Gene Occurred in Distinct Hominids: SMN2 Is Unique to Homo Sapiens. Hum. Genet. 2001;108:255–266. doi: 10.1007/s004390100473. [DOI] [PubMed] [Google Scholar]
- 69.Lefebvre S., Burlet P., Liu Q., Bertrandy S., Clermont O., Munnich A., Dreyfuss G., Melki J. Correlation between Severity and SMN Protein Level in Spinal Muscular Atrophy. Nat. Genet. 1997;16:265–269. doi: 10.1038/ng0797-265. [DOI] [PubMed] [Google Scholar]
- 70.Hebert M.D., Poole A.R. Towards an Understanding of Regulating Cajal Body Activity by Protein Modification. RNA Biol. 2017;14:761–778. doi: 10.1080/15476286.2016.1243649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dokal I. Dyskeratosis Congenita in All Its Forms. Br. J. Haematol. 2000;110:768–779. doi: 10.1046/j.1365-2141.2000.02109.x. [DOI] [PubMed] [Google Scholar]
- 72.Tummala H., Walne A., Collopy L., Cardoso S., de la Fuente J., Lawson S., Powell J., Cooper N., Foster A., Mohammed S., et al. Poly(A)-Specific Ribonuclease Deficiency Impacts Telomere Biology and Causes Dyskeratosis Congenita. J. Clin. Investig. 2015;125:2151–2160. doi: 10.1172/JCI78963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Heiss N.S., Knight S.W., Vulliamy T.J., Klauck S.M., Wiemann S., Mason P.J., Poustka A., Dokal I. X-Linked Dyskeratosis Congenita Is Caused by Mutations in a Highly Conserved Gene with Putative Nucleolar Functions. Nat. Genet. 1998;19:32–38. doi: 10.1038/ng0598-32. [DOI] [PubMed] [Google Scholar]
- 74.Vulliamy T., Beswick R., Kirwan M., Marrone A., Digweed M., Walne A., Dokal I. Mutations in the Telomerase Component NHP2 Cause the Premature Ageing Syndrome Dyskeratosis Congenita. Proc. Natl. Acad. Sci. USA. 2008;105:8073–8078. doi: 10.1073/pnas.0800042105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ballew B.J., Savage S.A. Updates on the Biology and Management of Dyskeratosis Congenita and Related Telomere Biology Disorders. Expert Rev. Hematol. 2013;6:327–337. doi: 10.1586/ehm.13.23. [DOI] [PubMed] [Google Scholar]
- 76.Vasko T., Kaifie A., Stope M., Kraus T., Ziegler P. Telomeres and Telomerase in Hematopoietic Dysfunction: Prognostic Implications and Pharmacological Interventions. Int. J. Mol. Sci. 2017;18:2267. doi: 10.3390/ijms18112267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Albanell J., Bosl G.J., Reuter V.E., Engelhardt M., Franco S., Moore M.A.S., Dmitrovsky E. Telomerase Activity in Germ Cell Cancers and Mature Teratomas. JNCI J. Natl. Cancer Inst. 1999;91:1321–1326. doi: 10.1093/jnci/91.15.1321. [DOI] [PubMed] [Google Scholar]
- 78.Fiorini E., Santoni A., Colla S. Dysfunctional Telomeres and Hematological Disorders. Differentiation. 2018;100:1–11. doi: 10.1016/j.diff.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.M’kacher R., Colicchio B., Borie C., Junker S., Marquet V., Heidingsfelder L., Soehnlen K., Najar W., Hempel W.M., Oudrhiri N., et al. Telomere and Centromere Staining Followed by M-FISH Improves Diagnosis of Chromosomal Instability and Its Clinical Utility. Genes. 2020;11:475. doi: 10.3390/genes11050475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mehrotra M., Luthra R., Ravandi F., Sargent R.L., Barkoh B.A., Abraham R., Mishra B.M., Medeiros L.J., Patel K.P. Identification of Clinically Important Chromosomal Aberrations in Acute Myeloid Leukemia by Array-Based Comparative Genomic Hybridization. Leuk. Lymphoma. 2014;55:2538–2548. doi: 10.3109/10428194.2014.883073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Terwilliger T., Abdul-Hay M. Acute Lymphoblastic Leukemia: A Comprehensive Review and 2017 Update. Blood Cancer J. 2017;7:e577. doi: 10.1038/bcj.2017.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nogueira B.M.D., da Costa Pantoja L., da Silva E.L., Mello Júnior F.A.R., Teixeira E.B., Wanderley A.V., da Silva Maués J.H., de Moraes Filho M.O., de Moraes M.E.A., Montenegro R.C., et al. Telomerase (HTERT) Overexpression Reveals a Promising Prognostic Biomarker and Therapeutical Target in Different Clinical Subtypes of Pediatric Acute Lymphoblastic Leukaemia. Genes. 2021;12:1632. doi: 10.3390/genes12101632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lansdorp P.M. Maintenance of Telomere Length in AML. Blood Adv. 2017;1:2467–2472. doi: 10.1182/bloodadvances.2017012112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Keller G., Brassat U., Braig M., Heim D., Wege H., Brümmendorf T.H. Telomeres and Telomerase in Chronic Myeloid Leukaemia: Impact for Pathogenesis, Disease Progression and Targeted Therapy. J. Hematol. Oncol. 2009;27:123–129. doi: 10.1002/hon.901. [DOI] [PubMed] [Google Scholar]
- 85.Davison G.M. Telomeres and Telomerase in Leukaemia and Lymphoma. Transfus. Apher. Sci. 2007;37:43–47. doi: 10.1016/j.transci.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 86.Yik M.Y., Azlan A., Rajasegaran Y., Rosli A., Yusoff N.M., Moses E.J. Mechanism of Human Telomerase Reverse Transcriptase (HTERT) Regulation and Clinical Impacts in Leukemia. Genes. 2021;12:1188. doi: 10.3390/genes12081188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jebaraj B.M.C., Stilgenbauer S. Telomere Dysfunction in Chronic Lymphocytic Leukemia. Front. Oncol. 2021;10:612665. doi: 10.3389/fonc.2020.612665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mascarenhas J.O., Komrokji R.S., Cavo M., Martino B., Niederwieser D., Reiter A., Scott B.L., Baer M.R., Hoffman R., Odenike O., et al. Telomerase Activity, Telomere Length and HTERT Expression Correlate with Clinical Outcomes in Higher-Risk Myelofibrosis (MF) Relapsed/Refractory (R/R) to Janus Kinase Inhibitor Treated with Imetelstat. Hemasphere. 2020;4:1098. [Google Scholar]
- 89.Berardinelli F., Nieri D., Sgura A., Tanzarella C., Antoccia A. Telomere Loss, Not Average Telomere Length, Confers Radiosensitivity to TK6-Irradiated Cells. Mutat. Res. Fundam. Mol. Mech. Mutagen. 2012;740:13–20. doi: 10.1016/j.mrfmmm.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 90.McCaul J.A., Gordon K.E., Minty F., Fleming J., Parkinson E.K. Telomere Dysfunction Is Related to the Intrinsic Radio-Resistance of Human Oral Cancer Cells. Oral Oncol. 2008;44:261–269. doi: 10.1016/j.oraloncology.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 91.Nogueira B.M.D., Machado C.B., Montenegro R.C., de Moraes M.E.A., Moreira-Nunes C.A. Telomere Length and Hematological Disorders: A Review. In Vivo. 2020;34:3093–3101. doi: 10.21873/invivo.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Andor N., Maley C.C., Ji H.P. Genomic Instability in Cancer: Teetering on the Limit of Tolerance. Cancer Res. 2017;77:2179–2185. doi: 10.1158/0008-5472.CAN-16-1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hoffmann J. Ueber Chronische Spinale Muskelatrophie Im Kindesalter, Auf Familiärer Basis. Dtsch. Z. Nervenheilkd. 1893;3:427–470. doi: 10.1007/BF01668496. [DOI] [Google Scholar]
- 94.Werdnig G. Zwei Frühinfantile Hereditäre Fälle von Progressiver Muskelatrophie Unter Dem Bilde Der Dystrophie, Aber Anf Neurotischer Grundlage. Arch. Psychiatr. Nervenkr. 1891;22:437–480. doi: 10.1007/BF01776636. [DOI] [Google Scholar]
- 95.Goh A.M., Coffill C.R., Lane D.P. The Role of Mutant P53 in Human Cancer. J. Pathol. 2011;223:116–126. doi: 10.1002/path.2784. [DOI] [PubMed] [Google Scholar]
- 96.Kandoth C., McLellan M.D., Vandin F., Ye K., Niu B., Lu C., Xie M., Zhang Q., McMichael J.F., Wyczalkowski M.A., et al. Mutational Landscape and Significance across 12 Major Cancer Types. Nature. 2013;502:333–339. doi: 10.1038/nature12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mantovani F., Collavin L., del Sal G. Mutant P53 as a Guardian of the Cancer Cell. Cell Death Differ. 2019;26:199–212. doi: 10.1038/s41418-018-0246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Leroy B., Anderson M., Soussi T. TP53 Mutations in Human Cancer: Database Reassessment and Prospects for the Next Decade. Hum. Mutat. 2014;35:672–688. doi: 10.1002/humu.22552. [DOI] [PubMed] [Google Scholar]
- 99.Weinstein I.B., Joe A. Oncogene Addiction. Cancer Res. 2008;68:3077–3080. doi: 10.1158/0008-5472.CAN-07-3293. [DOI] [PubMed] [Google Scholar]
- 100.Mina M., Raynaud F., Tavernari D., Battistello E., Sungalee S., Saghafinia S., Laessle T., Sanchez-Vega F., Schultz N., Oricchio E., et al. Conditional Selection of Genomic Alterations Dictates Cancer Evolution and Oncogenic Dependencies. Cancer Cell. 2017;32:155–168.e6. doi: 10.1016/j.ccell.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 101.Sun Y., Yang C., Chen J., Song X., Li Z., Duan M., Li J., Hu X., Wu K., Yan G., et al. Overexpression of WDR 79 in Non-small Cell Lung Cancer Is Linked to Tumour Progression. J. Cell Mol. Med. 2016;20:698–709. doi: 10.1111/jcmm.12759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sun Y., Cao L., Sheng X., Chen J., Zhou Y., Yang C., Deng T., Ma H., Feng P., Liu J., et al. WDR79 Promotes the Proliferation of Non-Small Cell Lung Cancer Cells via USP7-Mediated Regulation of the Mdm2-P53 Pathway. Cell Death Dis. 2017;8:e2743. doi: 10.1038/cddis.2017.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen J., Sheng X., Ma H., Tang Z., Yang C., Cao L., Sun Y., Deng T., Feng P., Hu B., et al. WDR79 Mediates the Proliferation of Non-small Cell Lung Cancer Cells by Regulating the Stability of UHRF1. J. Cell Mol. Med. 2018;22:2856–2864. doi: 10.1111/jcmm.13580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Peng J., Zhan Y., Feng J., Fan S., Zang H. Expression of WDR79 Is Associated with TP53 Mutation and Poor Prognosis in Surgically Resected Non-Small Cell Lung Cancer. J. Cancer. 2019;10:3046–3053. doi: 10.7150/jca.30587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yuan X.-S., Cao L.-X., Hu Y.-J., Bao F.-C., Wang Z.-T., Cao J.-L., Yuan P., Lv W., Hu J. Clinical, Cellular, and Bioinformatic Analyses Reveal Involvement of WRAP53 Overexpression in Carcinogenesis of Lung Adenocarcinoma. Tumor Biol. 2017;39:101042831769430. doi: 10.1177/1010428317694309. [DOI] [PubMed] [Google Scholar]
- 106.Rao X., Huang D., Sui X., Liu G., Song X., Xie J., Huang D. Overexpression of WRAP53 Is Associated with Development and Progression of Esophageal Squamous Cell Carcinoma. PLoS ONE. 2014;9:e91670. doi: 10.1371/journal.pone.0091670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang H., Wang D.-W., Adell G., Sun X.-F. WRAP53 Is an Independent Prognostic Factor in Rectal Cancer- a Study of Swedish Clinical Trial of Preoperative Radiotherapy in Rectal Cancer Patients. BMC Cancer. 2012;12:294. doi: 10.1186/1471-2407-12-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang M.-J., Ping J., Li Y., Adell G., Arbman G., Nodin B., Meng W.-J., Zhang H., Yu Y.-Y., Wang C., et al. The Prognostic Factors and Multiple Biomarkers in Young Patients with Colorectal Cancer. Sci. Rep. 2015;5:10645. doi: 10.1038/srep10645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wen Y., Zhao S., Holmqvist A., Hahn-Stromberg V., Adell G., Holmlund B., Pathak S., Peng Z., Sun X.-F. Predictive Role of Biopsy Based Biomarkers for Radiotherapy Treatment in Rectal Cancer. J. Pers. Med. 2020;10:168. doi: 10.3390/jpm10040168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Meng W.-J., Pathak S., Zhang X., Adell G., Jarlsfelt I., Holmlund B., Wang Z.-Q., Zhang A.S., Zhang H., Zhou Z.-G., et al. Expressions of MiR-302a, MiR-105, and MiR-888 Play Critical Roles in Pathogenesis, Radiotherapy, and Prognosis on Rectal Cancer Patients: A Study from Rectal Cancer Patients in a Swedish Rectal Cancer Trial of Preoperative Radiotherapy to Big Database Analyses. Front. Oncol. 2020;10:567042. doi: 10.3389/fonc.2020.567042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhu Y., Ding L., Chen B.-F., Song J.-G., Yao Y.-S. Oncogenic Activity of Wrap53 in Human Colorectal Cancer In Vitro and in Nude Mouse Xenografts. Med. Sci. Monit. 2018;24:6129–6136. doi: 10.12659/MSM.910214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kamel M.M., Matboli M., Sallam M., Montasser I.F., Saad A.S., El-Tawdi A.H.F. Investigation of Long Noncoding RNAs Expression Profile as Potential Serum Biomarkers in Patients with Hepatocellular Carcinoma. Transl. Res. 2016;168:134–145. doi: 10.1016/j.trsl.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 113.Schildkraut J.M., Goode E.L., Clyde M.A., Iversen E.S., Moorman P.G., Berchuck A., Marks J.R., Lissowska J., Brinton L., Peplonska B., et al. Single Nucleotide Polymorphisms in the TP53 Region and Susceptibility to Invasive Epithelial Ovarian Cancer. Cancer Res. 2009;69:2349–2357. doi: 10.1158/0008-5472.CAN-08-2902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hedström E., Pederiva C., Farnebo J., Nodin B., Jirström K., Brennan D.J., Farnebo M. Downregulation of the Cancer Susceptibility Protein WRAP53β in Epithelial Ovarian Cancer Leads to Defective DNA Repair and Poor Clinical Outcome. Cell Death Dis. 2015;6:e1892. doi: 10.1038/cddis.2015.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mędrek K., Magnowski P., Masojć B., Chudecka-Głaz A., Torbe B., Menkiszak J., Spaczyński M., Gronwald J., Lubiński J., Górski B. Association of Common WRAP 53 Variant with Ovarian Cancer Risk in the Polish Population. Mol. Biol. Rep. 2013;40:2145–2147. doi: 10.1007/s11033-012-2273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Silwal-Pandit L., Russnes H., Borgen E., Skarpeteig V., Moen Vollan H.K., Schlichting E., Kåresen R., Naume B., Børresen-Dale A.-L., Farnebo M., et al. The Sub-Cellular Localization of WRAP53 Has Prognostic Impact in Breast Cancer. PLoS ONE. 2015;10:e0139965. doi: 10.1371/journal.pone.0139965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Garcia-Closas M., Kristensen V., Langerød A., Qi Y., Yeager M., Burdett L., Welch R., Lissowska J., Peplonska B., Brinton L., et al. Common Genetic Variation in TP53 and Its Flanking Genes, WDR79 and ATP1B2, and Susceptibility to Breast Cancer. Int. J. Cancer. 2007;121:2532–2538. doi: 10.1002/ijc.22985. [DOI] [PubMed] [Google Scholar]
- 118.Pouladi N., Abdolahi S., Farajzadeh D., Hosseinpour Feizi M.A. Haplotype and Linkage Disequilibrium of TP53-WRAP53 Locus in Iranian-Azeri Women with Breast Cancer. PLoS ONE. 2019;14:e0220727. doi: 10.1371/journal.pone.0220727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mahmoudi S., Henriksson S., Farnebo L., Roberg K., Farnebo M. WRAP53 Promotes Cancer Cell Survival and Is a Potential Target for Cancer Therapy. Cell Death Dis. 2011;2:e114. doi: 10.1038/cddis.2010.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sun C., Luo X., Gou Y., Hu L., Wang K., Li C., Xiang Z., Zhang P., Kong X., Zhang C., et al. TCAB1: A Potential Target for Diagnosis and Therapy of Head and Neck Carcinomas. Mol. Cancer. 2014;13:180. doi: 10.1186/1476-4598-13-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tiefenböck-Hansson K., Haapaniemi A., Farnebo L., Palmgren B., Tarkkanen J., Farnebo M., Munck-Wikland E., Mäkitie A., Garvin S., Roberg K. WRAP53β, Survivin and P16INK4a Expression as Potential Predictors of Radiotherapy/Chemoradiotherapy Response in T2N0-T3N0 Glottic Laryngeal Cancer. Oncol. Rep. 2017;38:2062–2068. doi: 10.3892/or.2017.5898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Garvin S., Tiefenböck K., Farnebo L., Thunell L.K., Farnebo M., Roberg K. Nuclear Expression of WRAP53β Is Associated with a Positive Response to Radiotherapy and Improved Overall Survival in Patients with Head and Neck Squamous Cell Carcinoma. Oral Oncol. 2015;51:24–30. doi: 10.1016/j.oraloncology.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 123.Qiu H., Zhao D.-Y., Yuan L.-M., Zhang G., Xie C.-H. Regulatory Effects of WRAP53 on Radiosensitivity of Laryngeal Squamous Cell Carcinoma Cells. Asian Pac. J. Cancer Prev. 2015;16:2975–2979. doi: 10.7314/APJCP.2015.16.7.2975. [DOI] [PubMed] [Google Scholar]
- 124.Sun H., Kim P., Jia P., Park A.K., Liang H., Zhao Z. Distinct Telomere Length and Molecular Signatures in Seminoma and Non-Seminoma of Testicular Germ Cell Tumor. Brief. Bioinform. 2019;20:1502–1512. doi: 10.1093/bib/bby020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang K., Ge Y., Ni C., Cui B., Du J., Zhang B., Hu X., Chen J., Xiao L., Sun C., et al. Epstein-Barr Virus-Induced up-Regulation of TCAB1 Is Involved in the DNA Damage Response in Nasopharyngeal Carcinoma. Sci. Rep. 2017;7:3218. doi: 10.1038/s41598-017-03156-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chatterjee R., Mitra A. An Overview of Effective Therapies and Recent Advances in Biomarkers for Chronic Liver Diseases and Associated Liver Cancer. Int. Immunopharmacol. 2015;24:335–345. doi: 10.1016/j.intimp.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 127.Altekruse S.F., McGlynn K.A., Reichman M.E. Hepatocellular Carcinoma Incidence, Mortality, and Survival Trends in the United States From 1975 to 2005. J. Clin. Oncol. 2009;27:1485–1491. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Takayama T., Makuuchi M., Kojiro M., Lauwers G.Y., Adams R.B., Wilson S.R., Jang H.-J., Charnsangavej C., Taouli B. Early Hepatocellular Carcinoma: Pathology, Imaging, and Therapy. Ann. Surg. Oncol. 2008;15:972–978. doi: 10.1245/s10434-007-9685-0. [DOI] [PubMed] [Google Scholar]
- 129.Kyo S., Inoue M. Complex Regulatory Mechanisms of Telomerase Activity in Normal and Cancer Cells: How Can We Apply Them for Cancer Therapy? Oncogene. 2002;21:688–697. doi: 10.1038/sj.onc.1205163. [DOI] [PubMed] [Google Scholar]
- 130.Gao J.-F. Relationships of Tumor Inflammatory Infiltration and Necrosis with Microsatellite Instability in Colorectal Cancers. World J. Gastroenterol. 2005;11:2179. doi: 10.3748/wjg.v11.i14.2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pollheimer M.J., Kornprat P., Lindtner R.A., Harbaum L., Schlemmer A., Rehak P., Langner C. Tumor Necrosis Is a New Promising Prognostic Factor in Colorectal Cancer. Hum. Pathol. 2010;41:1749–1757. doi: 10.1016/j.humpath.2010.04.018. [DOI] [PubMed] [Google Scholar]
- 132.Park J., Cho J., Song E.J. Ubiquitin–Proteasome System (UPS) as a Target for Anticancer Treatment. Arch. Pharm. Res. 2020;43:1144–1161. doi: 10.1007/s12272-020-01281-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhang X., Linder S., Bazzaro M. Drug Development Targeting the Ubiquitin–Proteasome System (UPS) for the Treatment of Human Cancers. Cancers. 2020;12:902. doi: 10.3390/cancers12040902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Shammas M.A., Koley H., Batchu R.B., Bertheau R.C., Protopopov A., Munshi N.C., Goyal R.K. Telomerase Inhibition by SiRNA Causes Senescence and Apoptosis in Barrett’s Adenocarcinoma Cells: Mechanism and Therapeutic Potential. Mol. Cancer. 2005;4:24. doi: 10.1186/1476-4598-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Stewart Z.A., Westfall M.D., Pietenpol J.A. Cell-Cycle Dysregulation and Anticancer Therapy. Trends Pharmacol. Sci. 2003;24:139–145. doi: 10.1016/S0165-6147(03)00026-9. [DOI] [PubMed] [Google Scholar]
- 136.Watkins N.J., Bohnsack M.T. The Box C/D and H/ACA SnoRNPs: Key Players in the Modification, Processing and the Dynamic Folding of Ribosomal RNA. Wiley Interdiscip. Rev. RNA. 2012;3:397–414. doi: 10.1002/wrna.117. [DOI] [PubMed] [Google Scholar]
- 137.Qiu X.-B., Lin Y.-L., Thome K.C., Pian P., Schlegel B.P., Weremowicz S., Parvin J.D., Dutta A. An Eukaryotic RuvB-like Protein (RUVBL1) Essential for Growth. J. Biol. Chem. 1998;273:27786–27793. doi: 10.1074/jbc.273.43.27786. [DOI] [PubMed] [Google Scholar]
- 138.Lund A., Knudsen S.M., Vissing H., Clark B., Tommerup N. Assignment of Human Elongation Factor 1α Genes: EEF1AMaps to Chromosome 6q14 AndEEF1A2to 20q13.3. Genomics. 1996;36:359–361. doi: 10.1006/geno.1996.0475. [DOI] [PubMed] [Google Scholar]
- 139.Dayton T.L., Jacks T., vander Heiden M.G. PKM2, Cancer Metabolism, and the Road Ahead. EMBO Rep. 2016;17:1721–1730. doi: 10.15252/embr.201643300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chang M.T., Asthana S., Gao S.P., Lee B.H., Chapman J.S., Kandoth C., Gao J., Socci N.D., Solit D.B., Olshen A.B., et al. Identifying Recurrent Mutations in Cancer Reveals Widespread Lineage Diversity and Mutational Specificity. Nat. Biotechnol. 2016;34:155–163. doi: 10.1038/nbt.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Thomas S., Fisher K., Snowden J., Danson S., Brown S., Zeidler M. Effect of Methotrexate on JAK/STAT Pathway Activation in Myeloproliferative Neoplasms. Lancet. 2015;385:S98. doi: 10.1016/S0140-6736(15)60413-5. [DOI] [PubMed] [Google Scholar]
- 142.Wen X. The PI3K AKT Pathway in the Pathogenesis of Prostate Cancer. Front. Biosci. 2016;21:4443. doi: 10.2741/4443. [DOI] [PubMed] [Google Scholar]
- 143.Jeong E.G., Kim M.S., Nam H.K., Min C.K., Lee S., Chung Y.J., Yoo N.J., Lee S.H. Somatic Mutations of JAK1 and JAK3 in Acute Leukemias and Solid Cancers. Clin. Cancer Res. 2008;14:3716–3721. doi: 10.1158/1078-0432.CCR-07-4839. [DOI] [PubMed] [Google Scholar]
- 144.Brimo F., Wu C., Zeizafoun N., Tanguay S., Aprikian A., Mansure J.J., Kassouf W. Prognostic Factors in T1 Bladder Urothelial Carcinoma: The Value of Recording Millimetric Depth of Invasion, Diameter of Invasive Carcinoma, and Muscularis Mucosa Invasion. Hum. Pathol. 2013;44:95–102. doi: 10.1016/j.humpath.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 145.Fang Y., Wu J., Wang W., Fei X., Zong Y., Chen X., Huang O., He J., Chen W., Li Y., et al. Biologic Behavior and Long-Term Outcomes of Breast Ductal Carcinoma in Situ with Microinvasion. Oncotarget. 2016;7:64182–64190. doi: 10.18632/oncotarget.11639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wang X., Cao Y., Ding M., Liu J., Zuo X., Li H., Fan R. Oncological and Prognostic Impact of Lymphovascular Invasion in Colorectal Cancer Patients. Int. J. Med. Sci. 2021;18:1721–1729. doi: 10.7150/ijms.53555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lin H.-Y., Yang M.-C., Huang C.-H., Wu W.-J., Yu T.-J., Lung F.-W. Polymorphisms of TP53 Are Markers of Bladder Cancer Vulnerability and Prognosis. Urol. Oncol. Semin. Orig. Investig. 2013;31:1231–1241. doi: 10.1016/j.urolonc.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 148.Ran R., Tu G., Li H., Wang H., Mou E., Liu C. Genetic Variants Associated with Thyroid Cancer Risk: Comprehensive Research Synopsis, Meta-Analysis, and Cumulative Epidemiological Evidence. J. Oncol. 2021;2021:9967599. doi: 10.1155/2021/9967599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Li Q., Liu X., Hua R.-X., Wang F., An H., Zhang W., Zhu J.-H. Association of Three 8q24 Polymorphisms with Prostate Cancer Susceptibility: Evidence from a Meta-Analysis with 50,854 Subjects. Sci. Rep. 2015;5:12069. doi: 10.1038/srep12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhu M., Wen X., Liu X., Wang Y., Liang C., Tu J. Association between 8q24 Rs6983267 Polymorphism and Cancer Susceptibility: A Meta-Analysis Involving 170,737 Subjects. Oncotarget. 2017;8:57421–57439. doi: 10.18632/oncotarget.18960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Orth M., Lauber K., Niyazi M., Friedl A.A., Li M., Maihöfer C., Schüttrumpf L., Ernst A., Niemöller O.M., Belka C. Current Concepts in Clinical Radiation Oncology. Radiat. Environ. Biophys. 2014;53:1–29. doi: 10.1007/s00411-013-0497-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ding L., Li L.L., Yang J., Tao Y.G., Ye M., Shi Y., Tang M., Yi W., Li X.L., Gong J.P., et al. Epstein–Barr Virus Encoded Latent Membrane Protein 1 Modulates Nuclear Translocation of Telomerase Reverse Transcriptase Protein by Activating Nuclear Factor-ΚB P65 in Human Nasopharyngeal Carcinoma Cells. Int. J. Biochem. Cell Biol. 2005;37:1881–1889. doi: 10.1016/j.biocel.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 153.Mei Y.-P., Zhu X.-F., Zhou J.-M., Huang H., Deng R., Zeng Y.-X. SiRNA Targeting LMP1-Induced Apoptosis in EBV-Positive Lymphoma Cells Is Associated with Inhibition of Telomerase Activity and Expression. Cancer Lett. 2006;232:189–198. doi: 10.1016/j.canlet.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 154.Terrin L., Dal Col J., Rampazzo E., Zancai P., Pedrotti M., Ammirabile G., Bergamin S., Rizzo S., Dolcetti R., de Rossi A. Latent Membrane Protein 1 of Epstein-Barr Virus Activates the HTERT Promoter and Enhances Telomerase Activity in B Lymphocytes. J. Virol. 2008;82:10175–10187. doi: 10.1128/JVI.00321-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Yang J., Deng X., Deng L., Gu H., Fan W., Cao Y. Telomerase Activation by Epstein-Barr Virus Latent Membrane Protein 1 Is Associated with c-Myc Expression in Human Nasopharyngeal Epithelial Cells. J. Exp. Clin. Cancer Res. 2004;23:495–506. [PubMed] [Google Scholar]
- 156.Yang L., Xu Z., Liu L., Luo X., Lu J., Sun L., Cao Y. Targeting EBV-LMP1 DNAzyme Enhances Radiosensitivity of Nasopharyngeal Carcinoma Cells by Inhibiting Telomerase Activity. Cancer Biol. Ther. 2014;15:61–68. doi: 10.4161/cbt.26606. [DOI] [PMC free article] [PubMed] [Google Scholar]