Abstract
We investigated the conservation and antibody accessibility of inner core epitopes of Neisseria meningitidis lipopolysaccharide (LPS) because of their potential as vaccine candidates. An immunoglobulin G3 murine monoclonal antibody (MAb), designated MAb B5, was obtained by immunizing mice with a galE mutant of N. meningitidis H44/76 (B.15.P1.7,16 immunotype L3). We have shown that MAb B5 can bind to the core LPS of wild-type encapsulated MC58 (B.15.P1.7,16 immunotype L3) organisms in vitro and ex vivo. An inner core structure recognized by MAb B5 is conserved and accessible in 26 of 34 (76%) of group B and 78 of 112 (70%) of groups A, C, W, X, Y, and Z strains. N. meningitidis strains which possess this epitope are immunotypes in which phosphoethanolamine (PEtn) is linked to the 3-position of the β-chain heptose (HepII) of the inner core. In contrast, N. meningitidis strains lacking reactivity with MAb B5 have an alternative core structure in which PEtn is linked to an exocyclic position (i.e., position 6 or 7) of HepII (immunotypes L2, L4, and L6) or is absent (immunotype L5). We conclude that MAb B5 defines one or more of the major inner core glycoforms of N. meningitidis LPS. These findings support the possibility that immunogens capable of eliciting functional antibodies specific to inner core structures could be the basis of a vaccine against invasive infections caused by N. meningitidis.
Septicemia and meningitis caused by Neisseria meningitidis remain a global health problem, especially in young children. N. meningitidis is usually a commensal of the nasopharynx, the only major natural reservoir of this organism. The virulence factors that potentiate the capacity of N. meningitidis to cause invasive disease include capsular polysaccharides, pili (fimbriae) or outer membrane proteins and lipopolysaccharides (LPS) (12, 23, 39, 45, 48, 63, 68). Existing licensed vaccines against capsular serogroups A, C, W, and X are available (15, 20, 51) but generally lack satisfactory immunogenicity in very young children and do not induce long-lasting protective immunity (8, 33, 42, 43, 49). Nonetheless, their utility has been significant in affording protection to selected populations such as the military, travellers, and those at exceptional risk in outbreaks or epidemics (10). The problems are to identify vaccines that are highly effective in infants and to give long-term protection against group B strains. Group B strains have accounted for a substantial, often a majority of invasive N. meningitidis infections in many countries in Europe and the United States (11). Prevention of group B invasive disease represents a particularly difficult challenge in vaccine development since the capsular polysaccharide is very poorly immunogenic and even conjugates have shown disappointing immunogenicity (24). Further, there are concerns about the safety of vaccines whose rationale is to induce antibodies to the group B polysaccharide, a homopolymer of α-linked 2-8 neuraminic acid. The identical polysialic acid is a posttranslational modification of a glycoprotein present on human cells, especially neurons, and is referred to as neural cell adhesion molecule (14). Both theoretical and experimental evidence have been used to argue that the induction of antibodies might result in autoimmune, pathological damage to host tissues. Alternative approaches for developing vaccine candidates against group B N. meningitidis are being actively explored. These include: outer membrane porins (47, 50, 75, 76), transferrin-binding proteins (2), and LPS (19, 25, 27, 38, 69).
The structure of N. meningitidis LPS has been studied in considerable detail by Jennings and coworkers with additional contributions by others (4, 18, 44, 59, 64). The structures of major glycoforms for several immunotypes (L1 to L9) have been published: L1 and L6 (13, 73), L3 (41), L5 (37), L2 (16), L4 and L7 (32), and L9 (26) (Fig. 1). It is known that, in addition to this interstrain variation, individual N. meningitidis strains exhibit extensive phase variation of outer core LPS structures (reviewed in references 3 and 66). The molecular mechanism of this intrastrain variation involves hypermutable loci within the reading frames of several glycosyl transferases (17, 28). Similar mechanisms of phenotypic variation have been reported for other phase-variable surface components of pathogenic Neisseria spp., including Opc (52), Opa (61), and PilC proteins (31). This high-frequency, reversible molecular switching of LPS is mediated by homopolymeric tracts of cytosines or guanines through slippage-like mechanisms that result in frameshifts (17, 28, 60). Despite the extensive antigenic variation of LPS, the inner core of the LPS is relatively highly conserved. Furthermore, key biosynthetic genes for each step have been identified (reviewed in reference 48), and this allows the construction of a series of mutants from which LPS glycoforms of various sizes and complexities can be made available to facilitate the identification of conserved epitopes (29, 30, 64, 65). Our hypothesis is that one or more of these inner core epitopes may be conserved and accessible to antibodies and that a specific immune response to these epitopes could mediate protection. If so, LPS inner core oligosaccharides could be candidate vaccines.
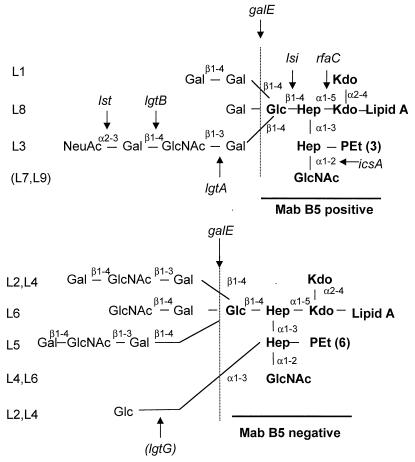
FIG. 1.
Representation of the structure of meningococcal LPS oligosaccharides of immunotypes L1 to L9. Immunotypes are indicated to the extreme left. The vertical line marks the junction between the inner core structures to the right and outer core structures to the left. The epitope recognized by MAb B5 is indicated in boldface (MAb B5 positive). Arabic numerals indicate the linkage between sugars or amino sugars. Alpha and beta indicate the carbon 1 linkage at the nonreducing end of the sugar. Genes for incorporating each of the key sugars or amino sugars into the LPS oligosaccharide in the biosynthetic pathway are indicated with arrows indicating where in the pathway the gene product is required. Abbreviations: Kdo, 2-keto-2-deoxyoctulosonic acid; Gal, galactose: GlcNAc, N-acetylglucosamine; Glu, glucose; Hep, heptose. Immunotype L5 has no PEtn on the second heptose. The gene that adds the glucose to the second heptose (lgtG) is phase variable.
Here we report that a monoclonal antibody (MAb), designated B5, has identified a cross-reacting epitope on the LPS of the majority of naturally occurring but genetically diverse strains of N. meningitidis. Critical to the epitope of strains recognized by the MAb B5 is a phosphoethanolamine (PEtn) on the 3-position of the β-chain heptose (HepII) (Fig. 1). In contrast, all N. meningitidis strains lacking reactivity with MAb B5 are immunotypes characterized by the absence of PEtn substitution or by PEtn substitution at an exocyclic position (i.e., position 6 or 7) of HepII (Fig. 1). Thus, a limited repertoire of inner core LPS variants is found among natural isolates of N. meningitidis strains, and these findings support the possibility that a vaccine might be developed containing a few glycoforms representative of all natural N. meningitidis strains.
MATERIALS AND METHODS
Bacterial strains.
The N. meningitidis strains MC58 and H44/76 (both B:15:P1.7,16 immunotype L3) have been described previously (21, 71). Derivatives of MC58 and H44/76 with defined alterations in LPS were obtained by inactivating the genes, galE (30), lsi (29), lgtA and lgtB (28), rfaC (62), and icsA and icsB (64) (Table 1). Other wild-type N. meningitidis strains used in the study were from three collections: (i) representatives of immunotypes L1 to L12 (46), a (ii) global collection of 34 representative N. meningitidis group B strains (56), and (iii) a global collection of 100 strains from 107 representative N. meningitidis strains of all major serogroups (A, B, C, W, X, Y, and Z) (35).
TABLE 1.
Bacterial strains
| Strain | Relevant immunotype and/or genotype | Source and/or reference |
|---|---|---|
| Neisseria meningitidis | ||
| MC58 | L3 | CSF isolate (71) |
| H44/76 | L3 | 21 |
| MC58 | galE | 30 |
| MC58 | lsi1 (rfaF) | 29 |
| MC58 | lgtA | 28 |
| MC58 | lgtB | 28 |
| H44/76 | rfaC | 62 |
| H44/76 | icsA | 64 |
| H44/76 | icsB | 64 |
| 126E, 35E, H44/76, 89I, M981, M992, 6155, 892257, M978, 120M, 7880, 7889, 3200 | L1 to L12, respectively | 46 |
| BZ157 | L2 | 56 |
| BZ157 | galE | This study |
| 1000 | NT | 56 |
| 1000 | galE | This study |
| NGE30 | NT | 56 |
| NGE30 | galE | This study |
| EG327 | NT | 56 |
| EG327 | galE | This study |
| NGH38 | L2 and L5 | 56 |
| NGH38 | galE | This study |
| EG328 | NT | 56 |
| EG328 | galE | This study |
| 3906, NGH15, BZ133, BZ83, EG329, SWZ107, BZ198, NGH41, NG4/88, 2970, BZ147, NGG40, NGH36, NG3/88, NGF26, NG6/88, NGH38, NGE28, BZ169, 528, DK353, BZ232, DK24, BZ159, BZ10, BZ163, NGP20 | 56 | |
| B40, Z4024, Z4081, Z2491, Z3524, Z3906, Z5826, BZ10, BZ163, B6116/77, L93/4286, NG3/88, NG6/88, NGF26, NGE31, DK24, 3906, EG328, EG327, 1000, B534, A22, 71/94, 860060, NGG40, NGE28, NGH41, 890326, 860800, NG4/88, E32, 44/76, 204/92, BZ8, SWZ107, NGH38, DK353, BZ232, E26, 400, BZ198, 91/40, NGH15, NGE30, 50/94, 88/03415, NGH36, BZ147, 297-0 | 35 | |
| Neisseria lactamica L12, L13, L17, L18, L19, L20, and L22; N. polysaccharea P4; N. mucosa M7; N. cinerea F1; N. elongata I8; N. sicca Q29; N. subflava U37 | B. Spratt & N. Smith | |
| Neisseria gonorrhoeae | ||
| F62, MS11, FA19, FA1090, 179008, 150002, 15253 | R. Goldstein | |
| SN-4 | S. Normavk | |
| P9-2 | M. Virji | |
| Haemophilus influenzae type b | 22 | |
| Eagan, 7004, Rd, 5B33, 3Fe, E3Fi, E1B1 | opsx rfaF orfH | |
| PLAK33 | lpxA | 58 |
| Haemophilus somnus 738 L1 | J. Richards | |
| Nontypeable Haemophilus influenzae 54, 375, 477, 1003, 1008, 1042, 1147, 1231 | J. Eskola | |
| Escherichia coli DH5α | 40 | |
| Salmonella typhimurium LT2 | rfaC rfaI rfaP | 53 |
Capsule-deficient and galE mutants were constructed in six N. meningitidis group B strains obtained from the collection described earlier (56) (Table 1). Other, related Neisseria strains studied included 10 strains of N. gonorrhoeae and the commensal strains N. lactamica (eight strains), N. polysaccharea (one strain), N. mucosa (one strain), N. cinerea (one strain), N. elongata (one strain), N. sicca (one strain), and N. subflava (one strain). Other gram-negative organisms included: Haemophilus influenzae type b (seven strains), H. somnus (one strain), nontypable H. influenzae (eight strains), Escherichia coli (one strain), and Salmonella typhimurium (one strain) and its isogenic LPS mutants (rfaC, rfaP, and rfaI) (Table 1).
Bacterial culture in vitro.
All strains were grown overnight at 37°C on standard brain heart infusion (BHI) medium base (Oxoid) in an atmosphere of 5% CO2.
Bacterial culture in vivo using the chick embryo model.
To determine the accessibility of inner core epitopes of N. meningitidis grown in vivo, the chick embryo model was used (6, 7, 55). The method was modified by using an inoculum of 104 or 105 N. meningitidis organisms in a final volume of 0.1 ml to infect the chorio-allantoic fluid of 10-day-old Pure Sussex chick eggs (obtained from the Poultry Unit, Institute of Animal Health, Compton, Berkshire, United Kingdom). After overnight incubation (37°C), the allantoic fluid (ca. 3 to 5 ml) was removed from the eggs, and the bacteria were recovered after centrifugation at 350 × g for 15 min. The organisms were washed in sterile phosphate-buffered saline (PBS) and stored in Greaves solution (5% bovine serum albumin [BSA], 5% sodium glutamate, 10% glycerol) at −70°C.
LPS extraction.
LPS samples were obtained from an overnight growth of N. meningitidis plated on five BHI plates from which the organisms were scraped and suspended in 30 ml of 0.05% phenol in PBS and incubated at room temperature for 30 min. Alternatively, batch cultures were prepared in fermenters with bacteria from an overnight growth (six plates) in 50 ml of Bacto Todd-Hewitt broth (Difco) to inoculate 2.5 liters of the same medium. For insertion mutant strains, the medium contained 50 μg of kanamycin per ml. After incubation at 37°C for 6 to 8 h, the culture was inoculated into 60 liters of Bacto Todd-Hewitt broth in a New Brunswick Scientific 1F-75 fermenter. After overnight growth (17 h at 37°C), the culture was killed by the addition of phenol (1%) and then chilled to 15°C; the bacteria were then harvested by centrifugation (13,000 × g for 20 min) (72). In either case, the crude LPS was extracted from the bacterial pellet by using the standard hot phenol-water method (74) and purified from the aqueous phase by repeated ultracentrifugation (105,000 × g, 4°C, two times for 5 h) (36).
Tricine gels.
Equivalent amounts of whole-cell (WC) lysates of N. meningitidis strains or purified LPS were boiled in dissociation buffer and separated on standard tricine gels (30 mA for 18 h) (34). Gels were fixed and silver stained according to the manufacturer’s instructions (Bio-Rad). To determine the presence of sialic acid, WC lysates were incubated with 2.5 μl of neuraminidase at 37°C for 18 to 20 h (4 U/ml; Boehringer 1585886) and then with 5 μl of proteinase K at 60°C for 2 to 3 h to remove proteins (Boehringer 1373196) prior to separation on tricine gels (16.5%).
Characterization of LPS from MAb B5-negative strains.
LPS from wild-type and galE, cap mutant MAb B5-negative strains were O deacylated with anhydrous hydrazine as described previously (5). O-Deacylated LPS were analyzed by electrospray mass spectrometry (ES-MS) in the negative ion mode on a VG Quattro (Fisons Instruments) or API 300 (Perkin-Elmer/Sciex) triple quadruple mass spectrometer. Samples were dissolved in water which was diluted by 50% with acetonitrile–water–methanol–1% ammonia (4:4:1:1), and the mixture was enhanced by direct infusion at 4 μl/min. Deacylated and dephosphorylated LPS (L8 odA HF) was prepared according to the following procedure. LPS (160 mg) was treated with anhydrous hydrazine (15 ml) with stirring at 37°C for 30 min. The reaction was cooled (0°C), cold acetone (−70°C, 50 ml) was added gradually to destroy excess hydrazine, and precipitated O-deacylated LPS (L8 odA) was obtained by centrifugation. L8 odA was washed twice with cold acetone and then redissolved in water and lyophilized. The structure of L8 odA was confirmed by negative ion ES-MS before dephosphorylation. L8 odA was dephosphorylated by treatment with 48% aqueous hydrogen fluoride (10 ml) at 0°C for 48 h. The product was dialyzed against water, and the O-deacylated, dephosphorylated LPS sample (L8 odA HF) was lyophilized (50 mg). Loss of phosphate was confirmed by ES-MS.
Molecular modelling.
Molecular modelling of LPS epitopes was carried out as described previously (5). The starting geometry for all sugars was submitted to a complete refinement of bond lengths, valence, and torsion angles by using the molecular mechanics program MM3(92) (Quantum Chemistry Program Exchanger [QCPE], Indiana University, Bloomington, Ind.). All calculations were performed by using the minimized coordinates for the methyl glycoside. The phosphorus groups were generated from standard coordinates (Tripos Software; Alchemy) and minimum energy conformations found in crystal structures. Calculations were performed by the Metropolis Monte Carlo (MMC) method. All pendant groups were treated as invariant except for the phosphorus groups, which were allowed to rotate about the Cx-Ox and Ox-P bonds. The starting angles for the oligosaccharide were taken from the minimum energy conformers calculated for each disaccharide unit present in the molecule. 24-Dimensional MMC calculations of the hexasaccharides with or without PEtn groups attached were carried out with 5,000 macro moves. The graphics were generated by using the Schakal software (Egbert Keller, Kristal-lographisches Institut der Universität, Freiburg, Germany).
Antibodies. (i) Rabbit polyclonal antibody.
We used a rabbit polyclonal antibody specific for group B N. meningitidis capsular polysaccharide obtained by immunizing a rabbit six times subcutaneously with lysates of MC58 at 2-week intervals. The first and second immunizations contained Freund complete adjuvant and Freund incomplete adjuvant, respectively. Serum was obtained from bleed 6. To increase specificity for the group B capsular polysaccharide, rabbit polyclonal antibody (1 ml) was incubated overnight at 4°C with ethanol-fixed capsule-deficient MC58 (5 × 109 organisms/ml). This preadsorbed polyclonal antibody did not react with a capsule-deficient mutant of MC58 as determined by immunofluorescence microscopy.
(ii) MAbs to inner core LPS.
Murine MAbs to H44/76 galE LPS were prepared by standard methods. Briefly, 6- to 8-week-old BALB/c mice were immunized three times intraperitoneally, followed by one intravenous injection with formalin-killed galE mutant whole cells. Hybridomas were prepared by the fusion of spleen cells with SP2/O-Ag 14 (57) as described earlier (9). Putative hybridomas secreting galE-specific antibodies were selected by enzyme-linked immunosorbent assay (ELISA) employing purified LPS from L3 and its galE mutant and L2. Immunoglobulin class, subclass, and light chain were determined by using an isotyping kit (Amersham Canada Ltd., Oakville, Ontario, Canada). Clones were expanded in BALB/c mice after treatment with pristane to generate ascitic fluid. Spent culture supernatant was collected after in vitro culture of hybridoma cell lines. Further testing of galE MAbs was carried out by screening against purified LPS from N. meningitidis L3 lgtA, lgtB, and lgtE mutant strains (Fig. 1), and S. typhimurium Ra and Re mutants. One of the MAbs, MAb B5 (immunoglobulin G3 [IgG3]), was selected for more detailed study.
(iii) Immunotyping MAbs.
To determine the immunotypes of N. meningitidis strains studied, especially L2 and L4 to L6, the following murine MAbs were used in dot blots and whole-cell ELISA: MN42F12.32 (L2 and L5), MN4A8B2 (L3, L7, and L9), MN4C1B (L4, L6, and L9), MN40G11.7 (L6), and MN3A8C (L5) (54).
(iv) Huvec assay.
Cultured human umbilical vein endothelial cells (Huvecs) were prepared as described previously (70) and were infected with strains of N. meningitidis for 3 h at 37°C. N. meningitidis strains were grown either in vitro or in vivo by using the chick embryo model (as described above). The accessibility of the inner core LPS epitopes of whole-cell N. meningitidis to specific MAb B5 was determined by using immunofluorescence and confocal microscopy. Gelatin-coated glass coverslips coated with Huvecs were infected with wild-type N. meningitidis as described previously (71), except that bacteria were fixed with 0.5% paraformaldehyde for 20 min instead of methanol. For accessibility studies, coverslips were washed with PBS, blocked in 3% BSA-PBS, and incubated with MAb B5 culture supernatant and/or preadsorbed polyclonal rabbit anticapsular antibody. Binding of antibody to wild-type N. meningitidis strains was detected by anti-mouse IgG rhodamine (tetramethyl rhodamine isocyanate [TRITC]; Dako) and anti-rabbit IgG fluorescein isothiocyanate (FITC; Sigma). Huvecs were stained with diaminophenylamine DAPI; (4′,6-diamidino-2-phenylindole; 1 μg/ml; Sigma). Mounted coverslips were viewed for immunofluorescence by using appropriate filters (Zeiss microscope with Fluorograbber, Adobe Photoshop, or confocal microscope [Nikon]).
ELISA. (i) Purified LPS ELISA.
A solid-phase indirect ELISA with purified LPS was used to determine the binding specificities of MAbs. Nunc Maxisorp plates were coated overnight with 1.0 μg of purified LPS per well derived from wild-type and mutants. LPS (10 μg/ml) was diluted in 0.05 M carbonate buffer containing 0.02 M MgCl2 (pH 9.8). Nonspecific binding sites were blocked for 1 h with 1% BSA-PBS (Sigma) and washed three times with PBS-Tween 20 (0.05% [vol/vol]; PBS-T). Plates were incubated for 1 h with MAb B5 culture supernatant and washed three times in PBS-T. Primary antibody was detected with anti-mouse IgG-alkaline phosphatase (Sigma and Cedarlane Laboratories, Ltd.) incubated for 1 h, washed three times in PBS-T, and detected with p-nitrophenyl phosphate alkaline phosphatase substrate system (Sigma and Kirkegaard & Perry Laboratories). The reaction was stopped after 1 h with 50 μl of 3 M NaOH, and the absorbance (A405–410) was determined (Dynatech EIA plate reader).
(ii) Inhibition ELISA.
For inhibition ELISA studies, MAb B5 was incubated with purified LPS samples prior to addition to L3 galE LPS-coated plates and then assayed as described above.
(iii) WC ELISA.
WC ELISA was performed by using heat-inactivated lysates of N. meningitidis organisms as described previously (1). Nunc Maxisorp 96-well plates were coated with 100 μl of bacterial suspension (optical density [OD] of 0.1 at A620) overnight at 37°C and blocked with 1% BSA-PBS; an identical protocol was followed as for LPS ELISA.
Dot blots.
Bacterial suspensions prepared as described above (2 μl) were applied to a nitrocellulose filter (45 μm, pore size; Schleicher & Schuell) and allowed to air dry. The same procedure as described for WC ELISA was followed except that the detection substrate was 5-bromo-4-chloro-3-indolyl-phosphate–nitroblue tetrazolium (2 mg/ml; Sigma). The color reaction was stopped after 30 min by several washes with PBS, and the blots were air dried.
RESULTS
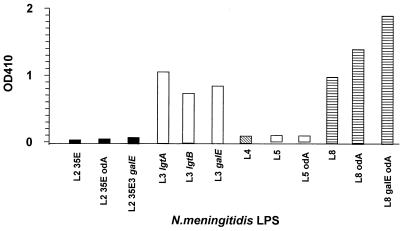
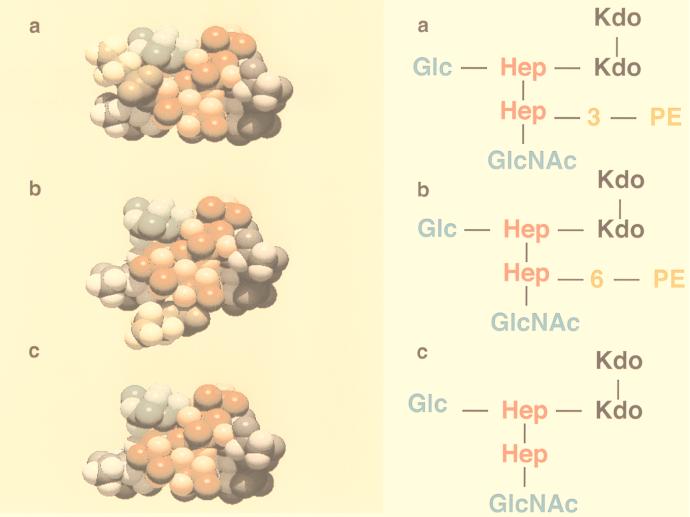
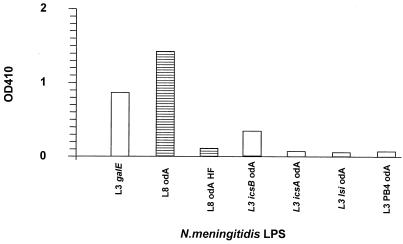
To investigate the potential of inner core LPS structures of N. meningitidis as vaccines, we have studied the reactivity of an isotype IgG3 murine MAb, designated B5, raised against N. meningitidis H44/76 immunotype L3 galE mutant. MAb B5 was one of seven MAbs to the LPS inner core produced against N. meningitidis immunotype L3 galE by standard immunological methods (see Materials and Methods). Preliminary ELISA testing showed that B5 cross-reacted with LPS from the L3 parent strain and with galE (lgtE), lgtA, and lgtB mutants but did not cross-react with S. typhimurium Ra or Re LPS. In order to determine the specific inner core epitope recognized by MAb B5, various N. meningitidis strains of known structure were examined by ELISA for cross-reactivity (Fig. 2). The most significant finding of this analysis was that N. meningitidis immunotype L4 LPS was not recognized by MAb B5. The only structural difference between immunotypes L4 and L3 (which is recognized by MAb B5) is the position of attachment of the PEtn group (Fig. 3). In immunotype L3 LPS the PEtn is attached at the 3-position of HepII, whereas in immunotype L4 LPS the PEtn is attached at the 6- or 7-position (Fig. 3). Additionally, LPS from immunotype L2 and its galE mutant (in which the PEtn group is attached at the 6-position and a glucose residue is present at the 3-position of HepII) are not recognized by MAb B5. Immunotype L5, which has no PEtn in the inner core, is not recognized by B5, whereas immunotype L8 and its galE mutant which have PEtn at the 3-position of HepII are recognized. These results suggest that MAb B5 specifically recognises PEtn when it is attached at the 3-position of HepII. In order to prove the essential inclusion of PEtn in the epitope recognized by MAb B5, immunotype L8 odA LPS was dephosphorylated (48% HF, 4°C, 48 h) (Fig. 3). The absence of PEtn after dephosphorylation was confirmed by ES-MS analysis. As indicated in Fig. 4, dephosphorylation of L8 odA LPS abolished reactivity to MAb B5. To further characterize the epitope recognized by MAb B5, several structurally defined genetic mutants of immunotype L3 were screened for cross-reactivity (Fig. 4). The highly truncated LPS of mutant strain icsB was only weakly recognized, while mutant strain icsA LPS was not recognized by MAb B5. These results suggest that the presence of glucose on the proximal heptose residue (HepI) is not absolutely necessary for binding by B5 but is required for optimal recognition (Fig. 1). Furthermore, MAb B5 does not bind LPS in which both the glucose on the β-chain and the N-acetylglucosamine residue on the β-chain are absent. This suggests that the presence of N-acetylglucosamine is required to present the PEtn residue in the correct conformation for binding by MAb B5. Genetic modifications that produce severely truncated LPS glycoforms were also examined for reactivity with MAb B5. LPS from immunotype L3 lsi which has a trisaccharide of Hep-Kdo-Kdo attached to lipid A, as well as L3 PB4 which only contains the Kdo disaccharide and lipid A, were not recognized by MAb B5 (Fig. 4). Inhibition ELISA studies (data not shown) were in accord with this result, thus confirming the specificity of MAb B5 to the PEtn molecule linked at the 3-position of HepII.
FIG. 2.
Cross-reactivity of MAb B5 with selected immunotypes and mutants of N. meningitidis LPS and O-deacylated (odA) LPS as determined by solid-phase ELISA. LPS glycoforms of immunotypes L2 (35E) (solid bars), L3 (H44/76) (open bars), L4 (89I) (hatched bars), L5 (M981) (open bars), L8 (M978) (horizontal-line-filled bars), wild-type, and respective mutants (galE, lgtA, or lgtB), in a native or O-deacylated form, were coated onto ELISA plates (see Materials and Methods), and the reactivity of MAb B5 was determined by standard ELISA (OD, A410).
FIG. 3.
Space-filling three-dimensional molecular models of the calculated (MMC) lowest-energy states of the core oligosaccharide from galE mutants of L3 (a), L4 (b), and L8-dephosphorylated (c). The Kdo moiety indicated in gray is substituted at the O-5 position by the heptose disaccharide inner core unit (red); HepI provides the point via a glucose residue (dark green) for extension to give α-chain epitopes, while HepII is substituted by an N-acetylglucosamine residue (lighter green) at O-2. PEtn (brown) is shown in O-3 position in the L3 immunotype and O-6 in the L4 immunotype.
FIG. 4.
Cross-reactivity of MAb B5 with genetically modified L3 LPS and chemically modified L8 LPS from N. meningitidis, as determined by solid-phase ELISA. LPS glycoforms of immunotype L8 (M978) (horizontal-line-filled bars) chemically modified by O deacylation and HF treatment and immunotype L3 (H44/76) (open bars) galE, icsB, icsA, lsi, and PB4 mutants (O deacylated) were coated onto ELISA plates (see Materials and Methods), and the reactivity of MAb B5 was determined by standard ELISA (OD, A410).
To demonstrate the ability of MAb B5 to recognize this inner core epitope in encapsulated strains, we devised an assay in which natural isolates of N. meningitidis were studied when they were grown on and became adherent to tissue-cultured cells (i.e., Huvecs). Initially, this methodology was developed by using the fully encapsulated strain MC58. The advantages of using the Huvec assay were that it provided a monolayer of endothelial cells to which the bacteria could adhere and that it provided a biologically relevant environment. Previous attempts with N. meningitidis directly adherent to gelatin- or matrigel-coated coverslips resulted in low numbers of adherent bacteria after repeated washings and high levels of nonspecific background staining.
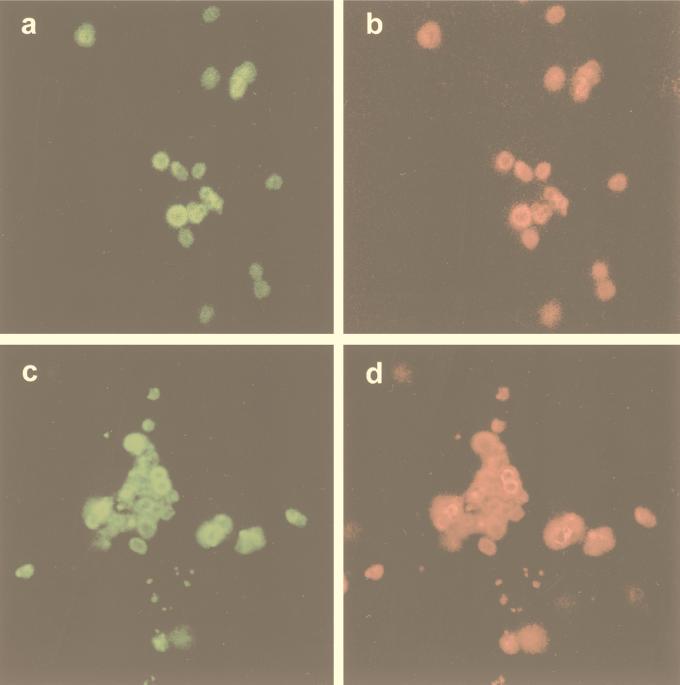
Primary antibodies, MAb B5, and a polyclonal anticapsular antibody were detected by use of anti-mouse TRITC and anti-rabbit FITC, respectively. This demonstrated that an inner core LPS epitope of the fully encapsulated strain (MC58) was accessible to MAb B5 (Fig. 5a and b). Confocal microscopy showed that MAb B5 and anticapsular antibodies colocalized and that the result was consistent irrespective of the sequence in which the antibodies were added. We also investigated, in addition to this in vitro demonstration of accessibility of MAb B5 to inner core LPS, organisms grown in vivo by using the chick embryo model. Strain MC58 (104 organisms/ml) was inoculated into chorioallantoic fluid of 10-day-old chick embryos and harvested the next day to provide ex vivo organisms. The results observed by confocal microscopy were identical to those observed in vitro, that is, MAb B5 and anticapsular antibodies colocalized (Fig. 5c and d). This demonstrated that the inner core LPS epitopes were also accessible in vivo on whole-encapsulated wild-type N. meningitidis.
FIG. 5.
(a and b) Confocal immunofluorescence microscopy of in vitro-grown N. meningitidis MC58 adherent to Huvecs. (a) Fluorescein tagging with rabbit polyclonal antibody specific for group B N. meningitidis capsule. (b) rhodamine tagging of MAb B5 specific for galE LPS. (c and d) Confocal immunofluorescence microscopy of in vivo-grown MC58 organisms stained as described for panels a and b. (c) Anticapsular antibody (green). (d) MAb B5 (red). Magnification, ×2,400 (all four panels).
The observation of double staining of the inner core LPS epitope in the presence of capsule is key to the concept of this approach, and therefore a number of controls were used to confirm the validity of this finding. (i) The first control involved double staining an MAb B5-negative strain (e.g., immunotype L4 strain) with MAb B5 and anti-capsular antibody. This resulted in no reactivity of MAb B5 by using a rhodamine filter but positive reactivity with anticapsular antibody, ruling out a band-passing effect during the recording of the pictures. (ii) The second control involved single staining of encapsulated MAb B5-positive strains with either MAb B5 alone or anticapsular antibody alone, followed by staining with rhodamine or FITC, respectively. When the results were viewed at the appropriate wavelength, there was no cross-reactivity seen during immunofluorescent staining, nor any band-passing effect. (iii) The third control involved double-staining an MAb B5-positive or -negative strain with MAb B5 and anticapsular antibody. This resulted in no capsular staining but either MAb B5-positive or -negative reactivity when viewed on the rhodamine filter. This result excluded cross-reactivity during staining or band-passing effect resulting in artifactual inner core staining.
To survey the extent of MAb B5 reactivity with other N. meningitidis strains, three collections of strains were investigated: (i) 12 strains representative of LPS immunotypes L1 to L12; (ii) 34 group B strains selected to represent genetically diverse isolates from many different countries obtained between the years 1940 and 1988 (56); and (iii) a global collection of 107 genetically diverse strains representing all capsular serogroups, also obtained from different countries from 1940 to 1994 (35).
Of the 12 immunotypes, MAb B5 recognized the LPS of strains in which the inner core oligosaccharide has a PEtn linked to the 3-position of HepII (Table 2 and Fig. 1). Thus, immunotypes L2, L4, and L6 did not react with MAb B5, whereas immunotypes L1, L3, and L7 to L12 were recognized by MAb B5. This confirmed that the presence of PEtn in the 3-position of the HepII is necessary to confer MAb B5 reactivity (Fig. 3).
TABLE 2.
Reactivity of MAb B5 with representative N. meningitidis strains of immunotypes L1 to L12 as determined by WC ELISA, dot blots of lysates, immunofluorescence, and confocal microscopy
| Strain | Serogroup: serotype | Immunotype | WC ELISA (OD, A405)a | Dot blotb | Immunofluorescencec |
|---|---|---|---|---|---|
| 126E | C:3:P1.5,2 | L1 | +1.8 | +++ | + |
| 35E | C:20:P1.1 | L2 | −<0.4 | − | − |
| H44/76 | B:15.P1.7,16 | L3 | +1.3 | +++ | ++ |
| 89I | C:nt:P1.16 | L4 | −<0.4 | − | − |
| M98I | B:4:P1.− | L5 | −<0.4 | ± | − |
| M992 | B:5:P1.7,1 | L6 | −<0.4 | ± | − |
| 6155 | B:nt:P1.7,1 | L7 | +0.8 | ++ | + |
| M978 | B:8:P1.7,1 | L8 | +1.9 | +++ | ++ |
| 892257 | B:4:P1.4 | L8 | +1.9 | ||
| 120M | A:4:P1.10 | L9 | +1.8 | +++ | + |
| 7880 | A:4:P1.6 | L10 | +2.2 | +++ | + |
| 7889 | A:4:P1.9 | L11 | +2.0 | +++ | ++ |
| 3200 | A:4:P1.9 | L12 | +2.1 | +++ | ++ |
+, positive reactivity (OD > 0.4); −, negative reactivity (OD < 0.4).
+++, strongly positive; ++, positive; ±, weakly positive; −, negative.
++, strongly positive; +, positive; −, negative.
To investigate further the MAb B5 reactivity with other group B strains, a collection of genetically diverse strains was studied (56). MAb B5 reactivity was detected in 26 of 34 (76%) of group B N. meningitidis strains tested. This included representative ET-5, ET-37, A4, and Lineage-3 strains. This represents the most complete available collection of hyperinvasive lineages of N. meningitidis group B strains.
We obtained capsule-deficient and galE mutants from six of eight of the MAb B5-negative group B strains (transformations were unsuccessful in the other two strains). These strains were also negative with MAb B5 as determined by dot blot, WC ELISA, or immunofluorescence, with the exception of a BZ157 galE capsule-deficient mutant, which had low-level reactivity as seen both by immunofluorescence and by dot blot. The MAb B5 strains were characterized by using a battery of immunotyping MAbs. We determined the immunotype of the eight MAb B5-negative strains by using combinations of the appropriate MAbs (see Materials and Methods) and dot blots of WC lysates (obtained from P. van der Ley) (Table 3). In addition, structural fingerprinting of the inner core region of MAb B5-negative strains was performed by ES-MS on O-deacylated LPS from five of the respective capsule-deficient galE mutants (1000, NGE30, EG327, BZ157, and NGH38) (Table 4). Strains 1000, NGE30, and EG327 were nontypeable as determined by the use of MAbs, and LPS from these strains lacked PEtn on HepII of the inner core. BZ157, which corresponded to immunotype L2 by MAbs, contained PEtn in the inner core and, by analogy, to L2 at the 6/7-position of HepII (Table 3). NGH38 was immunotype L2 and L5 and was analogous to L2 as determined by structural analysis. Those strains that were nontypeable failed to react with MAbs that recognize L3,7,9, L6, L2,5, and L4,6,9. However, 15 of 17 MAb B5-negative N. meningitidis strains (all serogroups) were positive for L2,5, and all MAb B5-positive strains were positive for L3,7,9. No reaction with any immunotyping MAbs was observed with 8 of 32 MAb B5-negative strains and 24 of 68 of MAb B5-positive strains.
TABLE 3.
Correlation between reactivity with MAb B5, immunotyping, and location of PEtn on HepII of the inner core
| Strain | MAb B5 | Immunotypea | Position of PEtn on HepII
|
|
|---|---|---|---|---|
| O-3 | O-6 | |||
| MC58 | + | L3 and L7 | + | − |
| 1000 | − | NT | − | − |
| NGE30 | − | NT | − | − |
| EG327 | − | NT | − | − |
| BZ157b | − | L2 and L5 | − | + |
| BZ157c | + | L3 and L7 | + | − |
| NGH38 | − | L2 and L5 | − | + |
NT, nontypeable. MN4A8B2 (L3, 7, 9), MN42F12.32 (L2,5), MN4C1B (L4,6,9), and MN40G11.7 (L6).
BZ157, MAb B5-negative variant.
BZ157, MAb B5-positive variant.
TABLE 4.
Negative-ion ES-MS data and proposed compositions of O-deacylated LPS from galE capsule-deficient mutant N. meningitidis MAb B5-negative strainsa
| Strain | Observed ions (m/z)
|
Molecular mass (Da)
|
Proposed composition | |||
|---|---|---|---|---|---|---|
| (M-2H)2− | (M-H)− | Observed | Calculated | Lipid Ab | ||
| 1000 | 1,213.0 | 2,427.6 | 2,427.7 | 2,427.2 | 1,075 | 2Glc, GlcNAc, 2Hep, 2 Kdo, Lipid A |
| 1,252.9 | 2,507.8 | 2,507.8 | 2,507.2 | 1,155 | 2Glc, GlcNAc, 2Hep, 2 Kdo, Lipid A | |
| 1,314.5 | 2,630.9 | 2,630.9 | 2,630.3 | 1,278 | 2Glc, GlcNAc, 2Hep, 2 Kdo, Lipid A | |
| NGH38 | 1,293.8 | 2,589.5 | 2,589.3 | 2,589.3 | 952 | 3Glc, GlcNAc, 2Hep, PEtn, 2Kdo, Lipid A |
| EG327 | 1,151.2 | 2,304.4 | 2,304.4 | 2,304.1 | 952 | 2Glc, GlcNAc, 2Hep, 2 Kdo, Lipid A |
| NGE30 | 1,132.1 | 2,265.1 | 1,075 | Glc, GlcNAc, 2Hep, 2 Kdo, Lipid A | ||
| 1,396.1 | 2,793.4 | 2,793.7 | 2,792.5 | 1,075 | 3Glc, 2GlcNAc, 2Hep, 2 Kdo, Lipid A | |
| 1,436.0 | 2,873.7 | 2,873.9 | 2,872.5 | 1,155 | 3Glc, 2GlcNAc, 2Hep, 2 Kdo, Lipid A | |
| 1,498.0 | 2,997.2 | 2,997.1 | 2,995.6 | 1,278 | 3Glc, 2GlcNAc, 2Hep, 2 Kdo, Lipid A | |
| BZ157 | 1,274.6 | 2,551.4 | 2,550.3 | 1,075 | 2Glc, GlcNAc, 2Hep, PEtn, 2Kdo, Lipid A | |
| 1,314.8 | 2,631.1 | 2,631.2 | 2,630.3 | 1,155 | 2Glc, GlcNAc, 2Hep, PEtn, 2Kdo, Lipid A | |
| 1,376.4 | 2,754.4 | 2,754.5 | 2,753.4 | 1,278 | 2Glc, GlcNAc, 2Hep, PEtn, 2Kdo, Lipid A | |
| 1,457.5 | 2,916.6 | 2,916.6 | 2,915.6 | 1,278 | 3Glc, GlcNAc, 2Hep, PEtn, 2Kdo, Lipid A | |
Average mass units were used for calculation of molecular weight based on proposed composition as follows: Glc, 162.15; Hep, 192.17; GlcNAc, 203.19; Kdo, 220.18; PEtn, 123.05. Hep, heptose; Kdo, 3-deoxy-d-manno-octulosonic acid; Glc, glucose; GlcNAc, N-acetylglucosamine; PEtn, phosphoethanolamine.
As determined by MS-MS analyses.
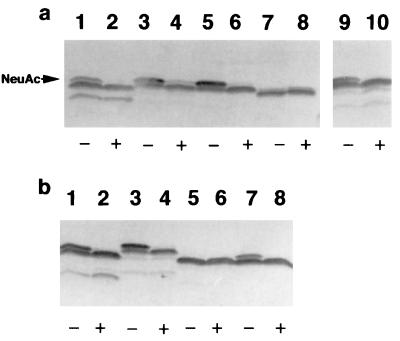
To determine if the degree of sialylation of the LPS was a factor in the ability of MAb B5 to recognize its inner core epitope, MAb B5-negative strains were examined by LPS gels. MAb B5 reactivity was unaffected by varying the state of sialylation through exposure to neuraminidase as described in Materials and Methods (Fig. 6). Furthermore, strain MC58, with which the MAb B5 reacted strongly, was found to be highly sialylated (Fig. 6), and this finding was confirmed by ES-MS of purified O-deacylated LPS (data not shown). Therefore, our data did not support a contribution of sialylation to the lack of MAb B5 reactivity.
FIG. 6.
Silver-stained tricine gels of LPS preparations (10 μg/lane) from N. meningitidis group B strains which were not reactive with MAb B5. These LPS preparations were either not treated (−) or treated with neuraminidase (+) to show the presence of sialic acid. (a) MAb B5-negative strains: lanes 1 and 2, NGE30; lanes 3 and 4, BZ157; lanes 5 and 6, EG328; lanes 7 and 8, 1000; lanes 9 and 10, 3906. (b) MAb B5-negative strains: lanes 1 and 2, EG327; lanes 3 and 4, NGH38; lanes 5 and 6, NGH15; and MAb B5-positive strain: lanes 7 and 8, MC58. The presence of sialic acid is indicated (NeuAc). This band was seen in untreated (−) and removed in treated (+) neuraminidase preparations.
With respect to the other Neisseria species, MAb B5 also recognized the inner core LPS of five strains of N. gonorrhoeae (F62, MS11, FA19, 179008, and 150002) (two were negative) and (at least) two strains of N. lactamica (L19 and L22). However, MAb B5 did not react with one strain each of N. polysaccharea (M7), N. mucosa (F1), N. cinerea (I8), N. elongata (Q29), N. sicca (Q39), and N. subflava (U37). Also, MAb B5 did not react with E. coli (DH5 alpha) or S. typhimurium (LT2) or its isogenic LPS mutants (rfaC, rfaI, and rfaP).
Finally, we investigated the reactivity of MAb B5 with 100 strains that included representatives of serogroups A, B, C, W, X, Y, and Z (35). Of these strains, 70% were MAb B5 positive. Clustering according to genetic relatedness was evident. For example, none of the MAb B5-negative strains were in the ET5 complex. Among group A strains, MAb B5-positive and -negative strains also fell into distinct clusters. For example, lineages I to III and lineage A4 were positive, and lineage IV to VI was negative. This collection, together with the one described earlier (56), represents the most complete set available for known hyperinvasive lineages in all major serogroups of N. meningitidis strains.
DISCUSSION
The prerequisites for any candidate N. meningitidis group B vaccine would be that it contain a highly conserved epitope(s) that is found in all group B strains and is accessible to antibodies in the presence of capsule. Our approach has combined genetics, structural analysis, and immunobiology to define candidate epitopes in inner core LPS of N. meningitidis group B. This study used murine MAb B5, isotype IgG3, which was raised to a genetically defined immunotype L3 galE mutant in order to specifically target inner core LPS epitopes. The epitope(s) recognized by MAb B5 was defined by cross-reactivity studies with purified LPS glycoforms of known structure. MAb B5 recognized all LPS glycoforms in which the PEtn is at the 3-position of HepII (immunotypes L1, L3, L7, L8, and L9) and failed to react with immunotypes where PEtn is at the 6- or 7-position (L2, L4, and L6) or absent from HepII (L5) (Fig. 1). MAb B5 reacted with 70% of the N. meningitidis strains tested from the two most complete sets of N. meningitidis strains available worldwide (35, 56). Of these strains, 76% of the N. meningitidis group B strains tested were positive with MAb B5, and 70% of a collection that included all N. meningitidis serogroups tested were positive with MAb B5. Therefore, it may be envisaged that a vaccine containing a limited number of glycoforms, representing all the possible PEtn positions (none, 3, and 6/7) on HepII of the inner core, would cover 100% of N. meningitidis group B strains.
The LPS structures of MAb B5-negative strains were confirmed by structural analysis. Two structural variants were recognized: one variant without PEtn in the inner core LPS (e.g., NGE30, EG327, and 1000) and the other with PEtn group on HepII (e.g., BZ157 and NGH38) at the 6- or 7-position instead of the 3-position.
With a view to developing inner core LPS epitopes as vaccine candidates, it is significant that there were no effects of the capsule on MAb B5 accessibility, as shown by colocalization of the anticapsular antibody and MAb B5 in wild-type organisms (MC58) grown in vitro and in vivo and visualized by confocal microscopy (Fig. 5). Nor did the presence or absence of sialic acid have an effect, since both MAb B5-positive and -negative strains had high sialylation states, as shown by tricine gels (Fig. 6) and confirmed by ES-MS (data not shown).
There was no evidence of phase variation in MAb B5-positive or -negative strains in this study, except for one strain (BZ157) which had a very low level of MAb B5-positive strains in parent and galE mutant (0.06%) (data not shown). Structural analysis of LPS extracted from these two variants is currently under investigation.
Three-dimensional space-filling models of the inner core LPS of L3 and L4 immunotypes show that the position of the PEtn, either the 3- or the 6-position, respectively (Fig. 3, shown in brown), alters the accessibility and conformation of PEtn in the inner core epitope. The most striking example of the importance of PEtn for MAb B5 reactivity was observed when PEtn was removed from the immunotype L8 (MAb B5 positive) by treatment with hydrogen fluoride, which totally abolished MAb B5 reactivity.
Previous studies with oligosaccharide conjugates in mice and rabbits have demonstrated that PEtn is important in immunogenicity and in the functional activity of polyclonal antibodies (67). These studies identified two sets of polyclonal antibodies. One set resulting from L1 and L3,7,9 oligosaccharides had PEtn in the 3-position of HepII, were immunogenic, and had opsonophagocytic (OP) activity and chemiluminescence in oxidative burst reaction but had no serum bactericidal activity. The other set of antibodies resulting from L2 conjugates (6- or 7-position or without PEtn at HepII) were poorly immunogenic and had greatly reduced OP activity and chemiluminescence (67). Future studies will look at the safety and immunogenicity of inner core LPS conjugates (PEtn at the 3-position of HepII and alternative glycoforms) and the functional ability of these polyclonal antibodies in opsonic and serum bactericidal assays, initially in mice and rabbits. Preliminary studies with MAb B5 in an OP assay with N. meningitidis MC58 and donor human polymorphonuclear cells suggests MAb B5 is opsonic in the presence of complement and that the uptake of N. meningitidis bacteria correlates with an oxidative burst reaction within the neutrophil (data not shown). MAb B5 does not appear to have any significant serum bactericidal activity with N. meningitidis MC58; however, this is not unexpected in view of its isotype (IgG3). The functionality of MAb B5 is currently under further investigation.
In conclusion, MAb B5 recognizes a conserved inner core epitope in which the PEtn is at the 3-position of HepII. This epitope was present in 76% of N. meningitidis group B strains and in 70% of all N. meningitidis serogroups and was accessible in the presence of capsule. A limited number of alternative glycoforms have been identified that are not recognized by MAb B5 where the PEtn is either absent or at an exocyclic position of HepII. Therefore, a vaccine containing a limited number of glycoforms might give 100% coverage of all N. meningitidis group B strains.
ACKNOWLEDGMENTS
This work was supported by Programme grants from the Medical Research Council (E.R.M.) and Wellcome Trust (E.R.M. and K.M.). Funding was also provided by the Oxford Regional Health Authority Research and Development Programme (J.P. and G.B.), the National Meningitis Trust (E.R.M. and J.P.), and Chiron vaccines (E.R.M. and J.R.). M.P.J. was supported by a grant from the NHMRC (96/1084).
We thank D. W. Griffith for large-scale production of bacterial cells, P. Thibault and D. Krajcarski for recording ES-MS, and J. Eskola for providing NTHi strains obtained as part of the Finnish Otitis Media Cohort Study.
REFERENCES
- 1.Abdillahi H, Poolman J T. Typing of group-B Neisseria meningitidis with monoclonal antibodies in the whole-cell ELISA. J Med Microbiol. 1988;26:177–180. [PubMed] [Google Scholar]
- 2.Al’Aldeen A A, Cartwright K A. Neisseria meningitidis: vaccines and vaccine candidates. J Infect. 1996;33:153–157. doi: 10.1016/s0163-4453(96)92081-2. [DOI] [PubMed] [Google Scholar]
- 3.Andersen S R, Kolberg J, Hoiby E A, Namork E, Caugant D A, Froholm L O, Jantzen E, Bjune G. Lipopolysaccharide heterogeneity and escape mechanisms of Neisseria meningitidis: possible consequences for vaccine development. Microb Pathog. 1997;23:139–155. doi: 10.1006/mpat.1997.0143. [DOI] [PubMed] [Google Scholar]
- 4.Apicella M A, Griffiss J M, Schneider H. Isolation and characterization of lipopolysaccharides, lipooligosaccharides, and lipid A. Methods Enzymol. 1994;235:242–252. doi: 10.1016/0076-6879(94)35145-7. [DOI] [PubMed] [Google Scholar]
- 5.Brisson J R, Uhrinova S, Woods R J, van der Zwan M, Jarrell H C, Paoletti L C, Kasper D L, Jennings H. NMR and molecular dynamics of the conformational epitope of the type III group B Streptococcus capsular polysaccharide and derivatives. Biochemistry. 1997;36:3278–3292. doi: 10.1021/bi961819l. [DOI] [PubMed] [Google Scholar]
- 6.Buddingh G J, Polk A. Meningococcal infection of the chick embryo. Science. 1937;86:20–21. doi: 10.1126/science.86.2218.20. [DOI] [PubMed] [Google Scholar]
- 7.Buddingh G J, Polk A. Experimental meningococcal infection of the chick embryo. J Exp Med. 1939;70:485–498. doi: 10.1084/jem.70.5.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cadoz M. Potential and limitations of polysaccharide vaccines in infancy. Vaccine. 1998;16:1391–1395. doi: 10.1016/s0264-410x(98)00097-8. [DOI] [PubMed] [Google Scholar]
- 9.Carlin N I, Gidney M A, Lindberg A A, Bundle D R. Characterization of Shigella flexneri-specific murine monoclonal antibodies by chemically defined glycoconjugates. J Immunol. 1986;137:2361–2366. [PubMed] [Google Scholar]
- 10.Centers for Disease Control. Availability of meningococcal vaccine in single-dose vials for travellers and high-risk persons. Morbid Mortal Weekly Rep. 1990;39:763. [PubMed] [Google Scholar]
- 11.Centers for Disease Control. Communicable disease weekly report. Vol. 7 1997. , no. 14. Centers for Disease Control, Atlanta, Ga. [Google Scholar]
- 12.DeVoe I W. The meningococcus and mechanisms of pathogenicity. Microbiol Rev. 1982;46:162–190. doi: 10.1128/mr.46.2.162-190.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Fabio J L, Michon F, Brisson J R, Jennings H J. Structure of L1 and L6 core oligosaccharide epitopes of Neisseria meningitidis. Can J Chem. 1990;68:1029–1034. [Google Scholar]
- 14.Finne J, Leinonen M, Makela P H. Antigenic similarities between brain components and bacteria causing meningitis. Implications for vaccine development and pathogenesis. Lancet. 1983;ii:355–357. doi: 10.1016/s0140-6736(83)90340-9. [DOI] [PubMed] [Google Scholar]
- 15.Frasch C E. Vaccines for prevention of meningococcal disease. Clin Microbiol Rev. 1989;2(Suppl.):S134–S138. doi: 10.1128/cmr.2.suppl.s134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gamian A, Beurret M, Michon F, Brisson J R, Jennings H J. Structure of the L2 lipopolysaccharide core oligosaccharides of Neisseria meningitidis. J Biol Chem. 1992;267:922–925. [PubMed] [Google Scholar]
- 17.Gotschlich E C. Genetic locus for the biosynthesis of the variable portion of Neisseria gonorrhoeae lipooligosaccharide. J Exp Med. 1994;180:2181–2190. doi: 10.1084/jem.180.6.2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffiss J M, O’Brien J P, Yamensaki R, Williams G D, Rice P A, Schneider H. Physical heterogenicity of neisserial lipopolysaccharides reflects oligosaccharides that differ in apparent molecular weight, chemical composition, and antigenic expression. Infect Immun. 1987;55:1792–1800. doi: 10.1128/iai.55.8.1792-1800.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu X X, Tsai C M. Preparation, characterization, and immunogenicity of meningococcal lipooligosaccharide-derived oligosaccharide-protein conjugates. Infect Immun. 1993;61:1873–1880. doi: 10.1128/iai.61.5.1873-1880.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herbert M A, Heath P T, Mayon-White R T. Meningococcal vaccines for the United Kingdom. Commun Dis Rep CDR Rev. 1995;5:R130–R135. [PubMed] [Google Scholar]
- 21.Holten E. Serotypes of Neisseria meningitidis isolated from patients in Norway during the first six months of 1978. J Clin Microbiol. 1979;9:186–188. doi: 10.1128/jcm.9.2.186-188.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hood D W, Deadman M E, Allen T, Masoud H, Martin A, Brisson J R, Fleischman R, Venter J C, Richards J C, Moxon E R. Use of the complete genome sequence information of Haemophilus influenzae Rd to investigate lipopolysaccharide biosynthesis. Mol Microbiol. 1996;22:951–965. doi: 10.1046/j.1365-2958.1996.01545.x. [DOI] [PubMed] [Google Scholar]
- 23.Jennings H J. The capsular polysaccharide of group B Neisseria meningitidis as a vehicle for vaccine development. Contrib Microbiol Immunol. 1989;10:151–165. [PubMed] [Google Scholar]
- 24.Jennings H J, Lugowsji H C. Immunochemistry of groups A, B, and C meningococcal polysaccharide-tetanus toxoid conjugates. J Immunol. 1981;127:1011–1018. [PubMed] [Google Scholar]
- 25.Jennings H J, Lugowski C, Ashton F E. Conjugation of meningococcal lipopolysaccharide R-type oligosaccharides to tetanus toxoid as route to a potential vaccine against group B Neisseria meningitidis. Infect Immun. 1984;43:407–412. doi: 10.1128/iai.43.1.407-412.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jennings H J, Johnson K J, Kenne L. The structure of an R-type oligosaccharide core obtained from some lipopolysaccharides of Neisseria meningitidis. Carbohydr Res. 1983;121:233–241. doi: 10.1016/0008-6215(83)84020-8. [DOI] [PubMed] [Google Scholar]
- 27.Jennings H J, Beurret M, Gamian A, Michon F. Structure and immunochemistry of meningococcal lipopolysaccharides. Antonie Leeuwenhoek. 1987;53:519–522. doi: 10.1007/BF00415511. [DOI] [PubMed] [Google Scholar]
- 28.Jennings M P, Hood D W, Peak I R, Virji M, Moxon E R. Molecular analysis of a locus for the biosynthesis and phase-variable expression of the lacto-N-neotetraose terminal lipopolysaccharide structure in Neisseria meningitidis. Mol Microbiol. 1995;18:729–740. doi: 10.1111/j.1365-2958.1995.mmi_18040729.x. [DOI] [PubMed] [Google Scholar]
- 29.Jennings M P, Bisercic M, Dunn K L, Virji M, Martin A, Wilks K E, Richards J C, Moxon E R. Cloning and molecular analysis of the lsi1 (rfaF) gene of Neisseria meningitidis which encodes a heptosyl-2-transferase involved in LPS biosynthesis: evaluation of surface exposed carbohydrates in LPS mediated toxicity for human endothelial cells. Microb Pathog. 1995;19:391–407. doi: 10.1006/mpat.1995.0074. [DOI] [PubMed] [Google Scholar]
- 30.Jennings M P, van der Ley P, Wilks K E, Maskell D J, Poolman J T, Moxon E R. Cloning and molecular analysis of the galE gene of Neisseria meningitidis and its role in lipopolysaccharide biosynthesis. Mol Microbiol. 1993;10:361–369. [PubMed] [Google Scholar]
- 31.Jonsson A B, Nyberg G, Normark S. Phase variation of gonococcal pili by frameshift mutation in pilC, a novel gene for pilus assembly. EMBO J. 1991;10:477–488. doi: 10.1002/j.1460-2075.1991.tb07970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kogan G, Uhrin D, Brisson J R, Jennings H J. Structural basis of the Neisseria meningitidis immunotypes, including the L4 and L7 immunotypes. Carbohydr Res. 1997;298:191–199. doi: 10.1016/s0008-6215(96)00305-9. [DOI] [PubMed] [Google Scholar]
- 33.Lepow M L, Beeler J, Randolph M, Samuelson J S, Hankins W A. Reactogenicity and immunogenicity of a quadrivalent combined meningococcal polysaccharide vaccine in children. J Infect Dis. 1986;154:1033–1036. doi: 10.1093/infdis/154.6.1033. [DOI] [PubMed] [Google Scholar]
- 34.Lesse A J, Campagnari A A, Bittner W E, Apicella M A. Increased resolution of lipopolysaccharides and lipopoligosaccharides utilizing tricine-sodium dodecyl sulfate-polyacrylamide gel electrophoresis. J Immunol Methods. 1990;126:109–117. doi: 10.1016/0022-1759(90)90018-q. [DOI] [PubMed] [Google Scholar]
- 35.Maiden M C J, Bygraves J A, Feil E, Morelli G, Russell J E, Urwin R, Zhang Q, Zhou J, Zurth K, Caugant D A, Feavers I M, Achtman M, Spratt B G. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Proc Natl Acad Sci USA. 1998;95:3140–3145. doi: 10.1073/pnas.95.6.3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masoud H, Moxon E R, Martin A, Krajcarski D, Richards J C. Structure of the variable and conserved lipopolysaccharide oligosaccharide epitopes expressed by Haemophilus influenzae serotype b Eagan. Biochemistry. 1997;36:2091–2103. doi: 10.1021/bi961989y. [DOI] [PubMed] [Google Scholar]
- 37.Michon F, Beurret M, Gamian A, Brisson J R, Jennings H J. Structure of the L5 lipopolysaccharide core oligosaccharide of Neisseria meningitidis. J Biol Chem. 1990;265:7243–7247. [PubMed] [Google Scholar]
- 38.Moxon E R, Hood D, Richards J C. Bacterial lipopolysaccharides: candidate vaccines to prevent Neisseria meningitidis and Haemophilus influenzae infections. Adv Exp Med Biol. 1998;435:237–243. doi: 10.1007/978-1-4615-5383-0_22. [DOI] [PubMed] [Google Scholar]
- 39.Nassif X, Marceau M, Pujol C, Pron B, Beretti J L, Taha M K. Type-4 pili and meningococcal adhesiveness. Gene. 1997;192:149–153. doi: 10.1016/s0378-1119(96)00802-5. [DOI] [PubMed] [Google Scholar]
- 40.Neidhardt F C. Derivations and genotypes of some mutant derivatives of Escherichia coli K-12. In: Neidhardt F C, Curtiss III R, Ingraham J L, Lin E C C, Low K Jr, Magasanik B, Reznikoff W S, Riley M, Schaechter M, Umbarger H E, editors. Escherichia coli and Salmonella. 2nd ed. Washington, D.C: ASM Press; 1996. pp. 2460–2488. [Google Scholar]
- 41.Pavliak V, Brisson J R, Michon F, Uhrin D, Jennings H J. Structure of the sialylated L3 lipopolysaccharide of Neisseria meningitidis. J Biol Chem. 1993;268:14146–14152. [PubMed] [Google Scholar]
- 42.Peltola H, Safary A, Kayhty H, Karanko V, Andre F E. Evaluation of two tetravalent (ACYW135) meningococcal vaccines in infants and small children: a clinical study comparing immunogenicity of O-acetyl-negative and O-acetyl-positive group C polysaccharides. Pediatrics. 1985;76:91–96. [PubMed] [Google Scholar]
- 43.Peltola H, Makela H, Kayhty H, Jousimies H, Herva E, Hallstrom K, Sivonen A, Renkonen O V, Pettay O, Karanko V, Ahvonen P, Sarna S. Clinical efficacy of meningococcus group A capsular polysaccharide vaccine in children three months to five years of age. N Engl J Med. 1977;297:686–691. doi: 10.1056/NEJM197709292971302. [DOI] [PubMed] [Google Scholar]
- 44.Poolman J T. Polysaccharides and membrane vaccines. In: Mizrahi A, editor. Bacterial vaccines. New York, N.Y: Wiley-Liss; 1990. pp. 57–86. [PubMed] [Google Scholar]
- 45.Poolman J T. Bacterial outer membrane protein vaccines. The meningococcal example. Adv Exp Med Biol. 1996;397:73–77. doi: 10.1007/978-1-4899-1382-1_11. [DOI] [PubMed] [Google Scholar]
- 46.Poolman J T, Hopman C T P, Zanen H C. Problems in the definition of meningococcal serotypes. FEMS Microbiol Lett. 1982;13:339–348. [Google Scholar]
- 47.Poolman J T, van der Ley P, Tommassen J P M. Surface structures and secreted products of meningococci. 1995. pp. 21–34. . K. Cartwright (ed.), Meningococcal disease. John Wiley & Sons, Inc., New York, N.Y. [Google Scholar]
- 48.Preston A, Mandrell R E, Gibson B W, Apicella M A. The lipooligosaccharides of pathogenic gram-negative bacteria. Crit Rev Microbiol. 1996;22:139–180. doi: 10.3109/10408419609106458. [DOI] [PubMed] [Google Scholar]
- 49.Reingold A L, Broome C V, Hightower G W, Ajello G A, Bolaw C, Adambauw E E, Jones C, Phillips H, Tiendrebeogo H, Yada A. Age-specific differences in duration of clinical protection after vaccination with polysaccharide A vaccine. Lancet. 1985;ii:114–118. doi: 10.1016/s0140-6736(85)90224-7. [DOI] [PubMed] [Google Scholar]
- 50.Rosenqvist E, Hoiby E A, Wedege E, Bryn K, Kolberg J, Klem A, Ronnild E, Bjune G, Nokleby H. Human antibody responses to meningococcal outer membrane antigens after three doses of the Norwegian group B meningococcal vaccine. Infect Immun. 1995;63:4642–4652. doi: 10.1128/iai.63.12.4642-4652.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rosenstein N, Levine O, Taylor J P, Evans D, Plikaytis B D, Wenger J D, Perkins B A. Efficacy of meningococcal vaccine and barriers to vaccination. JAMA. 1998;279:435–439. doi: 10.1001/jama.279.6.435. [DOI] [PubMed] [Google Scholar]
- 52.Sakari J, Pandit N, Moxon E R, Achtman M. Variable expression of the Opc outer membrane protein in Neisseria meningitidis is caused by size variation of a promoter containing poly-cytidine. Mol Microbiol. 1994;13:207–217. doi: 10.1111/j.1365-2958.1994.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 53.Schnaitman C A, Klena F D. Genetics of lipopolysaccharide biosynthesis in enteric bacteria. Microbiol Rev. 1993;57:655–682. doi: 10.1128/mr.57.3.655-682.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scholten R J, Kuipers B, Valkenburg H A, Dankert J, Zollinger W D, Poolman J T. Lipo-oligosaccharide immunotyping of Neisseria meningitidis by a whole-cell ELISA with monoclonal antibodies. J Med Microbiol. 1994;41:236–243. doi: 10.1099/00222615-41-4-236. [DOI] [PubMed] [Google Scholar]
- 55.Schroten H, Deadman M, Moxon E R. Development of chick embryo models for analysis of bacterial virulence factors. Pediatr Grenzgeb. 1995;34:319–324. [Google Scholar]
- 56.Seiler A, Reinhardt R, Sakari J, Caugant D A, Achtman M. Allelic polymorphisms and site-specific recombination in the opc locus of Neisseria meningitidis. Mol Microbiol. 1996;19:841–856. doi: 10.1046/j.1365-2958.1996.437970.x. [DOI] [PubMed] [Google Scholar]
- 57.Shulman M, Wilde C D, Kohler G. A better cell line for making hybridomas secreting specific antibodies. Nature. 1978;276:269–270. doi: 10.1038/276269a0. [DOI] [PubMed] [Google Scholar]
- 58.Steeghs L, den Hartog R, den Boer A, Zomer B, Roholl P, van der Ley P. Meningitis bacterium is viable without endotoxin. Nature. 1998;392:449–450. doi: 10.1038/33046. [DOI] [PubMed] [Google Scholar]
- 59.Stephens D S, McAllister C F, Zhou D, Lee F K, Apicella M A. Tn916-generated, lipooligosaccharide mutants of Neisseria meningitidis and Neisseria gonorrhoeae. Infect Immun. 1994;62:2947–2952. doi: 10.1128/iai.62.7.2947-2952.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stern A, Meyer T F. Common mechanism controlling phase and antigenic variation in pathogenic neisseriae. Mol Microbiol. 1987;1:5–12. doi: 10.1111/j.1365-2958.1987.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 61.Stern A, Brown M, Nickel P, Meyer T F. Opacity genes in Neisseria gonorrhoea: control of phase and antigenic variation. Cell. 1986;47:61–71. doi: 10.1016/0092-8674(86)90366-1. [DOI] [PubMed] [Google Scholar]
- 62.Stoiljkovic I, Hwa V, Larson J, Lin L, So M, Nassif X. Cloning and characterization of the Neisseria meningitidis rfaC gene encoding alpha-1,5-heptosyltransferase I. FEMS Microbiol Lett. 1997;151:41–49. doi: 10.1111/j.1574-6968.1997.tb10392.x. [DOI] [PubMed] [Google Scholar]
- 63.Tonjum T, Koomey M. The pilus colonization factor of pathogenic neisserial species: organelle biosynthesis and structure/function relationships—a review. Gene. 1997;192:155–163. doi: 10.1016/s0378-1119(97)00018-8. [DOI] [PubMed] [Google Scholar]
- 64.van der Ley P, Kramer M, Martin A, Richards J C, Poolman J T. Analysis of the icsBA locus required for biosynthesis of the inner core region from Neisseria meningitidis lipopolysaccharide. FEMS Microbiol Lett. 1997;146:247–253. doi: 10.1111/j.1574-6968.1997.tb10201.x. [DOI] [PubMed] [Google Scholar]
- 65.van der Ley P, Kramer M, Steeghs L, Kuipers B, Andersen S R, Jennings M P, Moxon E R, Poolman J T. Identification of a locus involved in meningococcal lipopolysaccharide biosynthesis by deletion mutagenesis. Mol Microbiol. 1996;19:1117–1125. doi: 10.1046/j.1365-2958.1996.464992.x. [DOI] [PubMed] [Google Scholar]
- 66.van Putten J P, Robertson B D. Molecular mechanisms and implications for infection of lipopolysaccharide variation in Neisseria. Mol Microbiol. 1995;16:847–853. doi: 10.1111/j.1365-2958.1995.tb02312.x. [DOI] [PubMed] [Google Scholar]
- 67.Verheul A F, Braat A K, Leenhouts J M, Hoogerhout P, Poolman J T, Snippe H, Verhoef J. Preparation, characterization, and immunogenicity of meningococcal immunotype L2 and L3,7,9 phosphoethanolamine group-containing oligosaccharide-protein conjugates. Infect Immun. 1991;59:843–851. doi: 10.1128/iai.59.3.843-851.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Verheul A F, Snippe H, Poolman J T. Meningococcal lipopolysaccharides: virulence factor and potential vaccine component. Microbiol Rev. 1993;57:34–49. doi: 10.1128/mr.57.1.34-49.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Verheul A F, Van Gaans J A, Wiertz E J, Snippe H, Verhoef J, Poolman J T. Meningococcal lipopolysaccharide (LPS)-derived oligosaccharide-protein conjugates evoke outer membrane protein- but not LPS-specific bactericidal antibodies in mice: influence of adjuvants. Infect Immun. 1993;61:187–196. doi: 10.1128/iai.61.1.187-196.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Virji M, Kayhty H, Ferguson D J P, Alexandrescu C, Heckels J E, Moxon E R. Interactions of Haemophilus influenzae with cultured human endothelial cells. Microb Pathog. 1991;10:231–245. doi: 10.1016/0882-4010(91)90057-h. [DOI] [PubMed] [Google Scholar]
- 71.Virji M, Kayhty H, Ferguson D J P, Heckels J E, Moxon E R. The role of pili in the interactions of pathogenic Neisseria with cultured human endothelial cells. Mol Microbiol. 1991;5:1831–1841. doi: 10.1111/j.1365-2958.1991.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 72.Wakarchuk W, Martin A, Jennings M P, Moxon E R, Richards J C. Functional relationships of the genetic locus encoding the glycosyltransferase enzymes involved in expression of the lacto-N-neotetraose terminal lipopolysaccharide structure in Neisseria meningitidis. J Biol Chem. 1996;271:19166–19173. doi: 10.1074/jbc.271.32.19166. [DOI] [PubMed] [Google Scholar]
- 73.Wakarchuk W W, Gilbert M, Martin A, Wu Y, Brisson J R, Thibault P, Richards J C. Structure of an alpha-2,6-sialylated lipooligosaccharide from Neisseria meningitidis immunotype L1. Eur J Biochem. 1998;254:626–633. doi: 10.1046/j.1432-1327.1998.2540626.x. [DOI] [PubMed] [Google Scholar]
- 74.Westphal O, Jann J K. Bacterial lipopolysaccharides extraction with water-phenol and further applications of the procedure. Methods Carbohydr Chem. 1965;5:83–91. [Google Scholar]
- 75.Wetzler L M. Immunopotentiating ability of neisserial major outer membrane proteins. Use as an adjuvant for poorly immunogenic substances and potential use in vaccines. Ann N Y Acad Sci. 1994;730:367–370. doi: 10.1111/j.1749-6632.1994.tb44295.x. [DOI] [PubMed] [Google Scholar]
- 76.Zollinger W D, Moran E E, Devi S J, Frasch C E. Bactericidal antibody responses of juvenile rhesus monkeys immunized with group B Neisseria meningitidis capsular polysaccharide-protein conjugate vaccines. Infect Immun. 1997;65:1053–1060. doi: 10.1128/iai.65.3.1053-1060.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]