Abstract
Due to the increase in the population with special needs and the significant difficulty in their dental management, it is essential to analyze the caries prevalence in this group of patients. The systematic review was conducted following the PRISMA statement. A search was performed on 9 May 2022 and updated on 5 June 2022, in three databases: Pubmed, Scielo, and Cochrane library. Studies involving the analysis of caries in permanent teeth in patients with special needs were included. A total of 1277 studies were analyzed and 21 studies were selected. Quality assessments were performed using an adapted version of the STROBE guidelines. Among the analyzed groups (intellectual disabilities, human immunodeficiency virus infection, schizophrenia, down syndrome, drug addicts, adult heart transplant, kidney disease, diabetic, autism, psychiatric patients, cerebral palsy, and hemophilia), the highest prevalence of caries was observed in patients with intellectual disability, without differences between genders. However, there is a need for more studies with standardized methods for caries diagnosis to further investigate the prevalence of caries in permanent teeth in patients with special needs.
Keywords: caries prevalence, permanent teeth, special needs
1. Introduction
The concept of patients with “special needs” includes any individual whose physical, intellectual, social, or emotional abilities fall outside what is viewed as typical concerning development and standards [1]. This idea may not coincide with the classic concept of disability. Disability has sometimes been related to six specific disabilities: hearing, vision, cognition, mobility, self-care, and independent living. It is worth highlighting that 25.7% of non-institutionalized adults in the USA reported a disability [2].
The increase in the number of adults with dependency-inducing disabilities can be explained by the increase in the population over 65 years of age. This age group presents the higher prevalence of disabilities, which can diminish their life expectancy and quality of life [3].
People with disabilities often have associated oral complications. This is related to the difficulty they can experience when eating, especially when chewing, and maintaining proper oral hygiene; which can increase the susceptibility of their teeth to decay and their gums to swelling [4].
Dental caries is a multifactorial disease that involves interactions between the tooth structure, the microbial biofilm formed on the tooth surface, sugars, and salivary and genetic factors [5].
People with severe disabilities tend to have a high number of carious lesions. This may be related to difficulties in providing accessible oral health care and treatments, and with the patients’ socioeconomic context [6,7,8].
Among the main factors that participate in the increased cariogenic risk, the following are worth mentioning: xerostomia, secondary to the consumption of anxiolytics and anticholinergic drugs; the consumption of drugs that incorporate sugary vehicles; special diets, including those that require frequent intakes; hypotonia of the cheeks, lips, or tongue; motor dysfunction of hands and arms; and demotivation due to the continuous perception of illness [4,9].
The difficulty in the management of this group of patients in the dental clinic in terms of the possible drug interactions or behavior management is another barrier. Most of the patients with physical or mental disabilities cannot find or access adapted or qualified dental services at local dental clinics or even hospitals. In addition, current dental healthcare policies do not fully address this critical oral health problem [10].
Caries prevention and control, defined as the decision making and preventive and restorative treatment strategies, require initiatives, both at an individual and a collective level. For example, to control the emergence and development of dental caries, there is a need to inform and motivate the patients and their caregivers, giving dietary advice, oral care instructions, and individualized recommendations [11].
Due to the increase in the population with special needs and the significant difficulty of their dental management, it is essential to analyze the caries prevalence in this group of patients so that public dental health programs can address their needs.
2. Material and Methods
This systematic review was carried out following the PRISMA 2020 protocol (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) [12] for systematic reviews. It was previously registered in Open Science Framework (OSF) Registries (https://osf.io/6fv3p (accessed on 17 June 2022)).
As a guide for the study of the systematic review, the following question is posed: “What is the prevalence of caries in permanent teeth in patients with special needs?”.
2.1. Inclusion Criteria
Articles were included according to the following criteria: (I) published in English; (II) patients with all permanent teeth; (III) patients with special needs; (IV) measurement of caries prevalence in permanent teeth; (V) specified the type of special need in relation to caries; and (VI) published in the last 10 years.
Exclusion criteria were the following: (I) languages other than English; (II) measurement of caries prevalence in deciduous teeth; (III) no measurement of caries prevalence; (IV) no relation of caries with the type of special need; (V) systematic reviews; (VI) meta-analysis; and (VII) literature reviews.
2.2. Search Strategy
2.2.1. Databases
An initial bibliography search was conducted on 9 May 2022 and updated on 5 June 2022 on the MEDLINE database using the PubMed search engine, Scielo, and Cochrane library.
2.2.2. Search Terms
The search was conducted by MPPL, it included 5 mesh (Medical Subject Heading) terms: “Caries”, “Special needs”, “Patient special needs”, “Mentally special needs” and “Physical special needs” related to each other with the Boolean operators “OR” and “AND” that were used to join the search terms: (Caries) AND ((Special needs) OR (Patient special needs) OR (Mentally special needs) OR (Physical Special Needs)) (Table 1).
Table 1.
Search strategy.
| Search Strategy | #1 | Caries |
| #2 | (Special Needs) OR (Patient Special Needs) OR (Mentally Special Needs) OR (Physical Special Needs) | |
| #1 AND #2 | (Caries) AND ((Special Needs) OR (Patient Special Needs) OR (Mentally Special Needs) OR (Physical Special Needs)) | |
| Database | Search Strategy | Findings |
| MEDLINE | #1 | 66,103 |
| #2 | 431,625 | |
| #1 AND #2 | 1212 | |
| SciELO | #1 | 2469 |
| #2 | 1091 | |
| #1 AND #2 | 16 | |
| Cochrane Library | #1 | 7792 |
| #2 | 4145 | |
| #1 AND #2 | 49 |
2.2.3. Study Selection
Following the inclusion and exclusion criteria, the articles from the last eleven years (from 2012 to 2022) were selected using the Endnote X9.3.1 manager (Clarivate, London, UK). The titles and abstracts of 1266 articles were analyzed by MRPL and MPPL after discarding duplicates. If the information was inconclusive, the full text was read. In addition, a manual search of the selected studies was carried out to find additional eligible studies.
2.2.4. Data Extraction
For the bibliometric analysis, the years of publication, the city, and the journals were considered. For the synthesis of the methodology of the included studies, a summary table was made with the following data: type of special need, study type, samples, groups, mean age of participants, gender, type of caries evaluation, DMFT, decayed, caries prevalence, and comparison of caries with the control group.
2.3. Quality Evaluation
Two investigators (M.P.P.-L. and F.J.R.-L.) performed the quality assessment of the included studies using an adapted version of the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) guidelines [11]. All included studies were scored according to ten specific criteria obtained from items 5, 6, 7, 8, 10, 12, and 15 from the original checklist. Each item was scored as positive (✓) when the requirement was met and negative (✕) when not fulfilled.
After the individual assessment by each investigator, studies with 8 to 10 points were categorized as low risk of bias, 5–7 were considered a moderate risk, and those with 4 or less were selected as high risk of bias.
Final study scores for each rater were collected and scrutinized for discrepancies. A consensus decision resolved any disagreement between raters. Once consensus was reached for all study ratings, overall quality scores were collected by adding these criteria, with the maximum score being 10.
3. Results
3.1. Study Selection and Flow Diagram
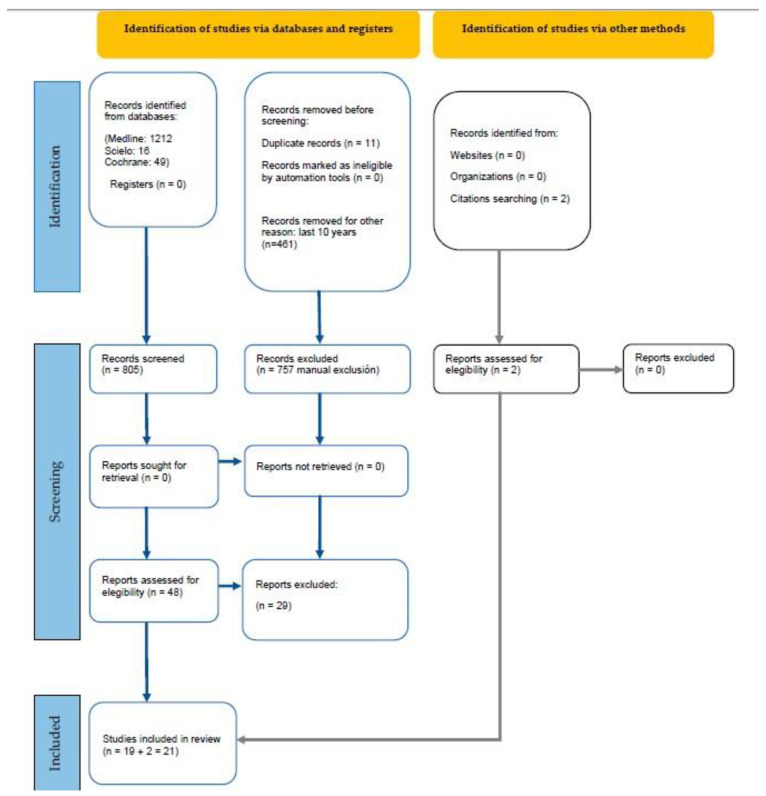
The search found 1277 preliminary references related to adults with special needs and caries: 1212 from Medline, 16 from Scielo, and 49 from Cochrane. After discarding 11 duplicate studies and 461 for being published more than 10 years ago, the remaining 805 records were analyzed. After analyzing the title and abstract of the records, 686 studies were excluded since they did not fit the inclusion criteria. The full texts of the remaining 48 articles were analyzed, from which 29 were excluded: 12 because they did not specify the disease; 3 because they were a review; 1 because it was a systematic review; 1 because it was in German; 8 because they analyzed caries in permanent and deciduous dentition at once; and 4 because they did not specify if patients had carious lesions. Two additional studies were found by citation searching and met the inclusion criteria. Finally, 21, articles were selected for their qualitative analysis (Figure 1).
Figure 1.
Systematic flow diagram representing the inclusion of studies according to the PRISM2A 2020 Declaration.
3.2. Study Characteristics
3.2.1. Bibliometric Analysis
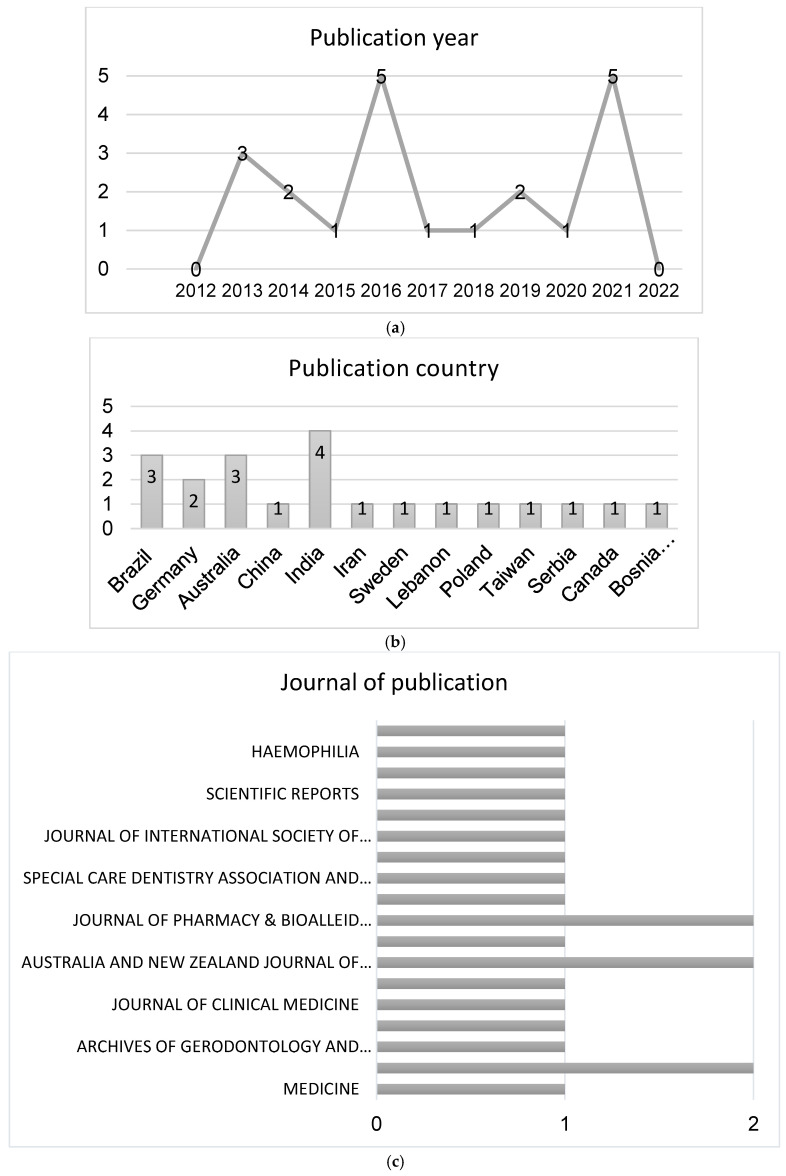
The maximum number of publications was observed in 2016 and 2021 (five articles per year), followed by 2013 (three articles), and 2014 and 2019 (two articles per year). Lastly, only one publication was observed in 2015, 2017, 2018, and 2020. A slight increase in the number of publications regarding this matter has been observed in the last years. Interestingly, less articles were published in 2020 compared with 2019 and 2021. This may be explained by the coronavirus disease (COVID) outbreak, where patients with special needs were considered as a group at risk. The number of patients with special needs is increasing with the increase in life expectancy; therefore, an increase in the number of this type of article is expected in the coming years (Figure 2).
Figure 2.
Bibliometric analysis: distribution of included studies by year of publication (a), country (b), and journal (c).
Regarding the countries of publication, the highest productivity can be seen in the continent of Asia with eight publications: India has four publications; China has one publication; Iran has one publication; Lebanon has one publication; and Taiwan has one publication. Europe has six publications: two publications in Germany; one in Sweden; one in Poland; one in Serbia; and one in Bosnia and Herzegovina. America has four publications: three publications in Brazil and one publication in Canada. Finally, Oceania has three publications in Australia (Figure 2).
The distribution of publication by journals was heterogeneous. Only three journals repeated two times: “BMC Oral Health”, “Australia and New Zealand Journal of Psychiatry”, and “Journal of Pharmacy & BioAllied Sciences”. From the twenty-one publications selected, six journals were about oral health (Community Dental Health, Archives of Gerodontology and Geriatrics, BMC Oral Health, International Journal of Dental Hygiene, Special Care Dentistry Association, and Wiley Periodicals, International Dental Journal) (Figure 2).
3.2.2. Study Types
Two studies were “case-control” and nineteen were “cross-sectional” (Table 2).
3.2.3. Sample and Groups
The selected studies involved human participants: 23,114 patients were analyzed. The sample size was heterogeneous between studies. The study with fewer patients was Porovic et al. [13], with 33 patients. The study by Fernandez et al. [14] had the highest quantity of “case” patients (3525).
3.2.4. Type of Patients with Special Needs
Among the group of patients with special needs, the highest number were those with intellectual disabilities, being studied 8 times [14,15,16,17,18,19,20], followed by human immunodeficiency virus infection (3 times) [21,22,23], and schizophrenia [24,25,26] and down syndrome [1,13] (2 times each). Finally, other groups of patients with special needs were only studied once: drug addicts [27], adult heart transplant [28], kidney disease [29], diabetic [30], autism [31], psychiatric patients [32], cerebral palsy, and hemophilia [26] (Table 2).
3.2.5. Caries Diagnosis
From the twenty-one selected studies, only two studies [21,31] used radiographies to diagnose caries, and two used a self-reported diagnosis via a survey [15,29]. All studies performed an oral examination except one, which was self-reported [23].
3.2.6. Caries Prevalence
Nine studies compared the prevalence of caries in patients with special needs with that of healthy patients [15,17,21,25,26,27,28,29,31] and found a difference between drug addicts and patients with an intellectual disability and healthy patients. However, patients with autism, heart transplant, kidney disease, hemophilia, schizophrenia, and HIV did not exhibit any difference in the DMFT (decayed, missing, and filled teeth) index compared with healthy patients. Another study on patients with an intellectual disability did not find differences from healthy patients. Only four studies [16,18,19,20] analyzed the differences between gender in caries experience, and only Ningrum et al. [16] found differences in patients with intellectual disabilities: male patients exhibited a higher number of carious lesions.
The highest DMFT scores were observed in diabetic patients [30] (27.1 and 25.8), followed by schizophrenia patients [25] (20.5), HIV patients [22,23] (15.14 and 15.6), and 14.9 in autism patients [31]. The highest decayed scores were observed in intellectual disability patients [16,17] (7.55 and 5.52) and HIV patients [17] (6.86 and 5.36). The highest prevalence of caries was observed in patients with intellectual disability [19,20] (89.4% and 95.5%), followed by psychiatric patients [32] (87.3%), and schizophrenia [25] (82.2%).
Table 2.
Summary of Main Results of Included Studies.
| Author and Year | Type of Special Patient | Study Type | Sample and Groups |
Gender and Relation with Caries |
Age (Mean Age) and Relation with DMFT |
Caries Evaluation | DMFT and Decayed Teeth |
Caries Prevalence | More Caries than HP |
|---|---|---|---|---|---|---|---|---|---|
| Agarwal et al., 2021 [24] | Schizophrenia | CS | 111 | M: 74.4% F: 25.3% N.I. |
34.73 y DMFT increase with age |
OE | M: 3.0 F: 3.1 All: 3.09 Decayed N.I. |
N.I. | N.I. |
| Arora et al., 2019 [27] | Drug addicts | Case- Control |
Case: 100 Control: 100 |
Case: 100 male Control: 100 male N.I. |
Case: 30.8 y Control: 29.8 y N.I. |
OE | Case: 5.71 Control 2.45 Decayed N.I. |
N.I. | Yes |
| Blomqvist et al., 2015 [31] | Autism spectrum disorder | CS | Autism: 47 Control: 69 |
M: 53.2% F: 46.8% N.I. |
33 y N.I. |
OE, RE | Autism: 14.9 Control: 15.9 Decayed: Autism: 4.9 Control: 10.3 |
N.I. | No |
| Cao et al., 2018 [28] | Adult heart transplant (AHT) | CS |
AHT: 81 Control: 63 |
AHT M: 69.1% F: 30.9% Control M: 63.5% F: 36.5% N.I. |
AHT: 47.7 Control: 49.6 N.I. |
OE |
AHT: 3 Control: 3 |
AHT: 80.2% Control: 79.4% |
No |
| Diab et al., 2017 [15] | Intellectual disabilities | CS |
Case: 510 Survey: 1877 |
N.I. | Age brackets from 12 to 44 DMFT increase with age |
ID: OE Survey: SR |
12 y: 4.27 15 y: 4.80 35–44 y: 12.71 Decayed: ID 12: 3.90 15: 4.01 35–44: 3.17 Survey: 12: 5.14 15: 6.80 35–44: 7.20 |
N.I. | No |
| Fernandez et al., 2016 [14] | Intellectual disabilities | CS | Poland: 1549 Romania: 1683 Slovenia: 293 |
Poland: M: 69% F: 31% Romania: M: 60% F: 40% Slovenia: M: 64% F: 36% N.I. |
Poland: 23.2 y Romania 22.9 y Slovenia 27.8 y N.I. |
OE | N.I. | Poland: 41% Romania: 19% Slovenia 61% |
N.I. |
| Goud et al., 2021 [32] | Psychiatric patients | CS | 150 | M: 60% F: 40% |
33.79 y N.I. |
OE | 4.06 Decayed: 3.4 |
87.3% | N.I. |
| Kapellas et al., 2021 [29] | Kidney disease | CS |
Case: 102 Control: 312 Survey: 4775 |
Case M: 39.2% F: 60.8% Control M: 55.8% F: 44.2% Survey: M: 49.7% F: 50.3% N.I. |
Case: 48.1 Control: 40.01 Survey: 44.84 N.I. |
Case and control: OE Survey: SR |
Case: 0.86 Control: 9.72 Survey: 14.01 Decayed Case: 3.17 Control: 3.02 Survey: 0.59 |
N.I. | No |
| Liberali et al., 2013 [21] | HIV | CS |
92–93: 54 9–10: 60 |
92–93 M: 90.7% F: 9.3% 9–10 M: 96.7% F: 3.3% N.I. |
92–93 Age brackets from 25 to 50+ 9–10 Age brackets from 25 to 50+ N.I. |
OE RE |
92–93: 15.6 9–10: 8.7 AM: 15.3 Decayed 1992: 2.4 2009: 0.6 AM: 0.6 |
92–93: 51.9% 9–10: 35% Control: 24.2% |
No |
| Lima et al., 2019 [30] | Diabetic | CS |
Diabetics from Fortaleza: 60 Diabetics from Rouen: 60 |
FOR: M: 50% F: 50% Rouen: M: 50% F: 50% N.I. |
Fortaleza Age brackets from 25 to 85+ Rouen: Age brackets from 25 to 85+ N.I. |
OE |
Fortaleza 27.1 Rouen: 25.8 Decayed Fortaleza 0.5 Rouen 1.7 |
FOR 50% Rouen 38.9% |
N.I. |
| Ningrum et al., 2020 [16] | Intellectual disability | CS | 65 | M: 48% F: 52% Male |
22 y N.I. |
OE | N.I. Decayed F: 3.00 M: 7.55 |
N.I. | N.I. |
| Oliveira et al., 2013 [17] | Intellectual disability | CS |
ID: 103 Siblings: 103 |
ID: M: 60% F: 40% Siblings M: 40% F: 60% N.I. |
Age brackets from 12 to 36 N.I. |
OE | ID: 6.36 Siblings: 5.06 Decayed: ID: 3.52 Siblings: 2.03 |
ID: 55.3% Siblings: 40.1% |
Yes |
| Petrovic et al., 2016 [18] | Intellectual disability | CS | 726 | M: 62.75% F: 37.25%
|
Age bracets from 12 to 20+ No differences between age |
OE | 12–20: 3.89 +20: 4.83 M: 4.73 F: 3.90 Decayed: 4.37 |
N.I. | N.I. |
| Pini et al., 2016 [1] | Down syndrome Cerebral palsy Intellectual disability |
CS | DS: 17 CP: 13 ID: 17 |
DS M: 41% F: 59% CP M: 69% F: 31% ID M: 59% F: 41% N.I. |
Age brackets from 12 to 55 N.I. |
OE | DS: <10:47% >10: 52% CP: <10: 69% >10: 30% ID: <10 53% >10: 47% Decayed: N.I. |
N.I. | N.I. |
| Porovic et al., 2016 [13] | Down syndrome | CS | 33 | M: 63.6% F: 36.4% N.I. |
From 19 to 45 N.I. |
OE | 15.96 Decayed: 3.57 |
N.I. | N.I. |
| Rezaei-Soufi et al., 2014 [22] | HIV | CS | HIV T 50 HIV WT 50 |
Treatment M: 71.4% F: 28.6% Control M: 81.8% F: 18.2% N.I. |
Case: 36 y Control: 38 y N.I. |
OE | Case: 15.14 Control: 14.45 Decayed Case: 6.86 Control: 5.36 |
Treatment: 34.52% Control: 27.42% |
N.I. |
| Rungsiyanont et al., 2012 [23] | HIV | CS | 299 | M: 28.6% F: 71% N.I. |
36.7 y N.I. |
SR | N.I. | 65.9% | N.I. |
| Schmidt et al., 2021 [19] | Intellectual disability | CS | 132 | M: 49.2% F: 51.8% No differences between gender |
35.2 y DMFT increased with age |
OE | All: 9.5 M:9.9 F: 9.2 Decayed All: 0.5 M: 0.5 F: 0.6 |
All: 89.4% M: 87.1% F: 91% |
N.I. |
| Schulte et al., 2013 [20] | Intellectual disability | CS | 428 | M: 51.4% F: 48.6% No differences between gender |
All: 35.5 y M: 36.7 y F: 34.3 y DMFT increased with age |
OE | All:12.25 M: 12.42 F: 12.09 Decayed M: 2.14 F: 1.83 |
All: 95.5% Caries free: 4.4% M: 95.7% F: 95.4% |
N.I. |
| Wey et al., 2016 [25] | Schizophrenia | CS |
Case: 543 Survey: 8332 |
M: 66.7% F: 33.3% N.I. |
54.8 y DMFT increased with age |
Case: OE Survey: SR |
Case: 20.5 Survey: 11.6 Decayed Case: 3.48 Survey: 1.70 |
Case: 82.2% Survey: 89.3% |
No |
| Zaliunienne et al., 2014 [26] | Haemophilia | Case-Control |
Case: 75 Control: 72 |
M: 100% N.I. |
Age bracets from 11 to 60 N.I. |
OE, RE | Case: 9.4 Control: 9.3 Decayed: Case: 3.1 Control: 2.7 |
N.I. | No |
HIV T: HIV with treatment; HIV WT: HIV without treatment; M: male; F: female; HP: healthy patient; N.I: no information; OE: oral exploration; SR: self-reported; RE: radiograph exploration; AM: aged matched; DMFT: decayed, missing, and filled teeth; DS: down syndrome; CP: cerebral palsy; ID: intellectual disability.
3.3. Quality Assessment
All observational studies were analyzed using adapted STROBE guidelines for rating observational studies [33] (Table 3). One study had a score of 4, two studies had a score of 5, four had a score of 6, seven had a score of 7, five had a score of 8, and two had a score of 9 (Table 4). Three studies were classified as having a high risk of bias, five as moderate risk of bias, and three as low risk of bias.
Table 3.
Checklist of 10 criteria based on an adapted version of the STROBE guidelines for assessing the quality of observational studies.
| Methods | ||
|---|---|---|
| Configuration | 1 | Describes the setting, participating locations, relevant dates (period of recruitment, exposure, follow-up, data collection). |
| Participants | 2 | Gives the inclusion and exclusion criteria (including paired or control groups) |
| 3 | Describes the disease studied. | |
| Variables | 4 | Clearly defines the diagnostic criteria (ICDAS, light, Rx…). |
| Data/measurement sources | 5 | Measure of caries by itself. |
| Study size | 6 | Explains how the study sample size was arrived at. |
| Statistical methods | 7 | Describes statistical methods, including those used to control for confounders. |
| 8 | Describes any methods used to examine subgroups and interactions. | |
| Results | ||
| Descriptive data | 9 | Provides characteristics of study participants (e.g., demographic, clinical, social) and reports on exposures and potential confounders. |
| Result data | 10 | Measures and presents exposure data. |
Table 4.
Results of quality assessment using an adapted version of the STROBE guidelines.
| Items | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total Score | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agarwal et al., 2021 [24] | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | 7 | Moderate |
| Arora et al., 2019 [27] | ✕ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | 5 | High |
| Blomqvist et al., 2015 [31] | ✕ | ✓ | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 7 | Moderate |
| Cao et al., 2018 [28] | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✕ | ✓ | ✓ | 6 | Moderate |
| Diab et al., 2017 [15] | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 8 | Low |
| Fernández et al., 2016 [14] | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✕ | ✕ | ✕ | ✓ | 4 | High |
| Goud et al., 2021 [32] | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✓ | ✓ | 7 | Moderate |
| Kapellas et al., 2021 [29] | ✕ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 6 | Moderate |
| Liberali et al., 2013 [21] | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 8 | Low |
| Lima et al., 2019 [30] | ✕ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 6 | Moderate |
| Ningrum et al., 2020 [16] | ✓ | ✓ | ✓ | ✕ | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | 7 | Moderate |
| Oliveira et al., 2013 [17] | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 9 | Low |
| Petrovic et al., 2016 [18] | ✕ | ✕ | ✕ | ✓ | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | 5 | High |
| Pini et al., 2016 [1] | ✓ | ✕ | ✓ | ✓ | ✕ | ✕ | ✓ | ✓ | ✓ | ✓ | 7 | Moderate |
| Porovic et al., 2016 [13] | ✓ | ✕ | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 7 | Moderate |
| Rezaei-Soufi et al., 2013 [22] | ✕ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | 6 | Moderate |
| Rungsiyanont et al., 2012 [23] | ✓ | ✓ | ✓ | ✕ | ✓ | ✓ | ✕ | ✕ | ✓ | ✓ | 7 | Moderate |
| Schmidt et al., 2021 [19] | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 8 | Low |
| Schulte et al., 2013 [20] | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 8 | Low |
| Wey et al., 2016 [25] | ✓ | ✓ | ✓ | ✕ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 8 | Low |
| Zalumienne et al., 2014 [26] | ✓ | ✓ | ✓ | ✓ | ✓ | ✕ | ✓ | ✓ | ✓ | ✓ | 9 | Low |
Each item was scored as positive (✓) when the requirement was met and negative (✕) when not fulfilled.
Only criteria #10 “Measures and presents exposure data” was fulfilled by all selected studies. Criteria #9 “Provides characteristics of study participants (e.g., demographic, clinical, social) and reports on exposures and potential confounders” and criteria #3 “Describes the disease studied” were assessed by 20 of the 21 selected studies. Criteria #7 “Describes statistical methods, including those used to control for confounders” was assessed by 19 of the 21 selected studies. Criteria #2 “Gives the inclusion and exclusion criteria (including paired or control groups)” was assessed by 18 of the 21 selected studies. Criteria #1 “Describes the setting, participating locations, relevant dates (period of recruitment, exposure, follow-up, data collection)” and criteria #5 “Measure of caries by itself” were assessed by 14 of the 21 selected studies. Criteria #8 “Describes any methods used to examine subgroups and interactions, and reports on exposures and potential confounders” was assessed by 10 of the 21 selected studies. Criteria #4 “Clearly define the diagnostic criteria of caries (ICDAS, light, Rx” was assessed by 8 of the 21 selected studies. Finally, criteria #6 “Explains how the study sample size was arrived at,” was assessed by only 2 of the 21 selected studies.
4. Discussion
This systematic review aimed to analyze the caries prevalence in permanent teeth in patients with special needs. The increased knowledge of the groups with higher prevalence and risk of caries could be helpful to design and implement specific dental programs to help the oral health of this group of patients.
Regarding the methodology followed in the studies, the evaluation and diagnosis of caries was performed in most studies via visual examination by a dentist. However, this type of diagnosis is subjective and can differ from one professional to another. There are other types of techniques for caries detection such as quantitative light-induced fluorescence (QLF), Diagnodent (DD), fiber-optic transillumination (FOTI), electrical conductance (EC), or near-infrared imaging (NIRI) among others [34,35]. Only two studies used oral and radiographic examination [21,31], which is more specific than only oral examination for caries diagnosis. In addition, three studies used “self-reported diagnosis of caries” [23,25,29], which cannot be considered a reliable diagnostic method because the general population cannot diagnose accurately without dental training.
DMFT index is classified in five levels: 0.0–4.9 very low, 5.0–8.9 low, 9.0–13.9 moderate, 14.0–17.9 high, and more than 18 very high [36]. Seventeen of the twenty-one selected studies measured DMFT index among the sample of patients with special needs: HIV [20,21] and autism [31] had a high index (15.6, 15.14, and 14.9, respectively), and patients with diabetes mellitus [30] and schizophrenia [25] had a very high index (27.1, 25.8, and 20.5, respectively). DMFT index in autism was lower (14.9) than the control group (15.9). These results coincide with those from Corridore et al. [37]. Kapellas et al. [29] showed that the DMFT in the case group was 10.86, the control group was 9.72, and the survey group was 14.01. Still, the results from the last group were self-reported by the patient, and consequently they may not be accurate.
In the analysis of decayed teeth, Kapellas et al. [29] reported a score of 3.17 in the “case” group, 3.02 in the “control” group, and 0.59 in the survey group. The score was the highest in the group of patients with special needs, but the differences with the control group were not significant. In the case of the survey group, the decayed teeth score is less than the other two, but, again, these results should be interpreted with caution since the diagnosis was self-reported. Arora et al. [27] analyzed the drug addicts group and concluded that there were statistical differences between groups in the DMFT index (5.71 in the “case” group and 2.45 in the “control” group). This could be explained by the increased vulnerability and diminished oral-health-related quality of life in drug addicts depending on the type of drug [38], although this study had a high risk of bias. Another group of studies [19,20] analyzed the differences between the DMFT index in men and women with an intellectual disability and did not find significant differences.
The DMFT index was used in nineteen of the twenty-one studies, which is a subjective index since it does not describe how caries are identified as caries. In addition, the DMFT index does not reflect the number of active caries since it also measures absences (which can be extractions performed for other reasons, such as orthodontics or fracture, and the patient’s agenesis) and fillings. There are other indexes such as ICDAS (The International Caries Detection and Assessment System) or ICCMS (The International Caries Classification and Management System), which describe and specify when a black stain can be considered as caries [39,40,41].
Six studies analyzed the DMFT index concerning age; five concluded that DMFT increased with age, which agrees with other studies [42,43]. It could be explained because when the age rises, the number of patients with edentulism increases, increasing the DMFT index [25]. Four of the selected studies analyzed the DMFT in relation to gender; three concluded there is no relation with gender, which agrees with other authors such as Mohammadi et al. [42].
The last study of the prevalence of caries in the general population is from the World Health Organization from the year 2000. The prevalence of caries in permanent teeth is between 25% and 50% [44], being below the data obtained in some of the studies: patients with HIV with a prevalence of 65.9% [23], intellectual disability with a prevalence of 89.4% and 95.5% [19,20], psychiatric patients [32] with 87.3%, schizophrenia [25] with 82.2% and, finally, adults with a heart transplant [28] with 80.2%. However, in this study, the control group had a prevalence of 79.4%, which was higher than in the other studies. The prevalence of caries was analyzed in eleven of the twenty-one selected studies. The highest prevalence was found in the intellectual disability group [19,20] with 89.4% and 95.5%. This could be explained because this type of patient usually has the worst oral hygiene and needs their caregivers help to maintain it [45].
It should be highlighted that this study has a series of limitations: the concept of “special needs patient” is too broad, and it covers a wide range of patients with different types of needs; some of them need the help of a caregiver, others do not; and the kind of medication required for each group is different. All these variants made some groups more vulnerable to present caries than other.
5. Conclusions
The prevalence of caries in permanent teeth in patients with special needs seems to be higher than the general population. Based on the results of the included studies, patients with HIV present a prevalence of 65.9%, patients with intellectual disability present a prevalence of 89.4% and 95.5%, psychiatric patients 87.3%, schizophrenia 82.2% and, finally, adults with a heart transplant 80.2%. However, there is a need for more studies with standardized caries diagnosis methods to further investigate the caries prevalence in permanent teeth in patients with special needs.
Author Contributions
Conception and design of the study, M.P.P.-L. and M.R.P.-L.; acquisition of data, M.P.P.-L.; analysis and interpretation of data, M.P.P.-L. and F.J.R.-L.; drafting the manuscript, M.P.P.-L., F.J.R.-L. and M.R.P.-L.; revising the manuscript critically for important intellectual content, F.J.R.-L.; approval of the version of the manuscript to be published, M.P.P.-L., M.R.P.-L. and F.J.R.-L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest related to this article.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pini D.D.M., Meridional B.F., Fröhlich P.C.G.R., Rigo L. Oral health evaluation in special needs individuals. Einstein. 2016;14:501–507. doi: 10.1590/s1679-45082016ao3712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okoro C.A., Hollis N.D., Cyrus A.C., Griffin-Blake S. Prevalence of Disabilities and Health Care Access by Disability Status and Type among Adults—United States, 2016. MMWR. Morb. Mortal. Wkly. Rep. 2018;67:882–887. doi: 10.15585/mmwr.mm6732a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Courtney-Long E.A., Carroll D.D., Zhang Q.C., Stevens A.C., Griffin-Blake S., Armour B.S., Campbell V.A. Prevalence of Disability and Disability Type among Adults—United States, 2013. MMWR Morb. Mortal. Wkly. Rep. 2015;64:777–783. doi: 10.15585/mmwr.MM6429a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teo C.H.K., Mahesh M.N., Lim G.X.D. Oral health status and barriers to care in a multiethnic mixed disability center: Rethinking disability community dental services. Spéc. Care Dent. 2020;40:344–355. doi: 10.1111/scd.12483. [DOI] [PubMed] [Google Scholar]
- 5.Pitts N.B., Zero D.T., Marsh P.D., Ekstrand K., Weintraub J.A., Ramos-Gomez F., Tagami J., Twetman S., Tsakos G., Ismail A. Dental caries. Nat. Rev. Dis. Prim. 2017;3:17030. doi: 10.1038/nrdp.2017.30. [DOI] [PubMed] [Google Scholar]
- 6.Scully C., Kumar N., Diz Dios P. Hot topics in special care dentistry. Dent. Update. 2009;36:187. [PubMed] [Google Scholar]
- 7.Alwattban R.R., Alkhudhayr L.S., Ali S.N.A.-H., Farah R.I. Oral Health-Related Quality-of-Life According to Dental Caries Severity, Body Mass Index and Sociodemographic Indicators in Children with Special Health Care Needs. J. Clin. Med. 2021;10:4811. doi: 10.3390/jcm10214811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Ogayyel S., Ali S.A.-H. Comparison of dental treatment performed under general anesthesia between healthy children and children with special health care needs in a hospital setting, Saudi Arabia. J. Clin. Exp. Dent. 2018;10:e963–e969. doi: 10.4317/jced.55060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glassman P., Anderson M., Jacobsen P., Schonfeld S., Weintraub J., White A., Gall T., Hammersmark S., Isman R., Miller C.E., et al. Practical protocols for the prevention of dental disease in community settings for people with special needs: The protocols. Spéc. Care Dent. 2003;23:160–164. doi: 10.1111/j.1754-4505.2003.tb00304.x. [DOI] [PubMed] [Google Scholar]
- 10.Mubayrik A.B. The Dental Needs and Treatment of Patients with Down Syndrome. Dent. Clin. N. Am. 2016;60:613–626. doi: 10.1016/j.cden.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Chávez E.M., Wong L.M., Subar P., Young D.A., Wong A. Dental Care for Geriatric and Special Needs Populations. Dent. Clin. N. Am. 2018;62:245–267. doi: 10.1016/j.cden.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021;10:89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porovic S., Zukanovic A., Juric H., Dinarevic S. Oral Health of Down Syndrome Adults in Bosnia and Herzegovina. Mater. Socio Med. 2016;28:437–439. doi: 10.5455/msm.2016.28.437-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rojas C.F., Wichrowska-Rymarek K., Pavlic A., Vinereanu A., Fabjanska K., Kaschke I., Marks L.A. Oral health needs of athletes with intellectual disability in Eastern Europe: Poland, Romania and Slovenia. Int. Dent. J. 2016;66:113–119. doi: 10.1111/idj.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diab H.A., Hamadeh G.N., Ayoub F. A survey of oral health in institutionalized population with intellectual disabilities: Comparison with a national oral health survey of the normal population. J. Int. Soc. Prev. Community Dent. 2017;7:141–147. doi: 10.4103/jispcd.JISPCD_65_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ningrum V., Wang W.-C., Liao H.-E., Bakar A., Shih Y.-H. A special needs dentistry study of institutionalized individuals with intellectual disability in West Sumatra Indonesia. Sci. Rep. 2020;10:153. doi: 10.1038/s41598-019-56865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oliveira J.S., Prado Júnior R.R., de Sousa Lima K.R., de Oliveira Amaral H., Moita Neto J.M., Mendes R.F. Intellectual disability and impact on oral health: A paired study. Spec. Care Dent. 2013;33:262–268. doi: 10.1111/scd.12015. [DOI] [PubMed] [Google Scholar]
- 18.Petrovic B.B., Peric T.O., Markovic D.L., Bajkin B.B., Petrovic D., Blagojevic D.B., Vujkov S. Unmet oral health needs among persons with intellectual disability. Res. Dev. Disabil. 2016;59:370–377. doi: 10.1016/j.ridd.2016.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt P., Egermann M., Sauerland C., Schulte A.G. Caries Experience of Adults with Intellectual Disability in the Western Part of Germany. J. Clin. Med. 2021;10:2602. doi: 10.3390/jcm10122602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulte A.G., Freyer K., Bissar A. Caries experience and treatment need in adults with intellectual disabilities in two German regions. Community Dent. Health. 2013;30:39–44. [PubMed] [Google Scholar]
- 21.Liberali S., Coates E., Freeman A., Logan R., Jamieson L., Mejia G. Oral conditions and their social impact among HIV dental patients, 18 years on. Aust. Dent. J. 2013;58:18–25. doi: 10.1111/adj.12031. [DOI] [PubMed] [Google Scholar]
- 22.Rezaei-Soufi L., Davoodi P., Abdolsamadi H.R., Jazaeri M., Malekzadeh H. Dental Caries Prevalence in Human Immunodeficiency Virus Infected Patients Receiving Highly Active Anti-Retroviral Therapy in Kermanshah, Iran. Cell J. 2014;16:73–78. [PMC free article] [PubMed] [Google Scholar]
- 23.Rungsiyanont S., Vacharotayangul P., Lam-Ubol A., Ananworanich J., Phanuphak P., Phanuphak N. Perceived dental needs and attitudes toward dental treatments in HIV-infected Thais. AIDS Care. 2012;24:1584–1590. doi: 10.1080/09540121.2012.663884. [DOI] [PubMed] [Google Scholar]
- 24.Agarwal D., Kumar A., Manjunath B.C., Kumar V., Sethi S. Oral health perception and plight of patients of schizophrenia. Int. J. Dent. Hyg. 2020;19:121–126. doi: 10.1111/idh.12467. [DOI] [PubMed] [Google Scholar]
- 25.Wey M.C., Loh S., Doss J.G., Abu Bakar A.K., Kisely S. The oral health of people with chronic schizophrenia: A neglected public health burden. Aust. N. Z. J. Psychiatry. 2015;50:685–694. doi: 10.1177/0004867415615947. [DOI] [PubMed] [Google Scholar]
- 26.Zaliuniene R., Aleksejuniene J., Peciuliene V., Brukiene V. Dental health and disease in patients with haemophilia—A case-control study. Haemophilia. 2014;20:e194–e198. doi: 10.1111/hae.12325. [DOI] [PubMed] [Google Scholar]
- 27.Arora P.C., Ragi K.G.S., Arora A., Gupta A. Oral Health Behavior and Treatment Needs among Drug Addicts and Controls in Amritsar District: A Case-controlled Study. J. Neurosci. Rural Pract. 2019;10:201–206. doi: 10.4103/jnrp.jnrp_309_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao Y., Chen X., Jia Y., Lv Y., Sun Z. Oral health status of adult heart transplant recipients in China: A cross-sectional study. Medicine. 2018;97:e12508. doi: 10.1097/MD.0000000000012508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kapellas K., Hughes J.T., Cass A., Maple-Brown L.J., Skilton M.R., Harris D., Askie L.M., Hoy W., Pawar B., McKenzie K., et al. Oral health of aboriginal people with kidney disease living in Central Australia. BMC Oral Health. 2021;21:50. doi: 10.1186/s12903-021-01415-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lima D.L., Saintrain M.V., Neri J.R., Beck O., Malet P., Moizan J.A., Doucet J. Oral health complications in Brazilian and French diabetic older people: A comparative study. Arch. Gerontol. Geriatr. 2019;84:103905. doi: 10.1016/j.archger.2019.103905. [DOI] [PubMed] [Google Scholar]
- 31.Blomqvist M., Bejerot S., Dahllöf G. A cross-sectional study on oral health and dental care in intellectually able adults with autism spectrum disorder. BMC Oral Health. 2015;15:81. doi: 10.1186/s12903-015-0065-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goud V., Kannaiyan K., Rao B.V., Abidullah M., Dharani V., Nayak M. Oral Health Status and Treatment Needs of Psychiatric Outpatients Aged 18–64 Years in District Civil Hospital, Raichur, Karnataka: A Cross-Sectional Study. J. Pharm. Bioallied Sci. 2021;13((Suppl. S1)):S598–S601. doi: 10.4103/jpbs.JPBS_776_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 34.Hoskin E.R., Keenan A.V. Can we trust visual methods alone for detecting caries in teeth? Evid. Based Dent. 2016;17:41–42. doi: 10.1038/sj.ebd.6401165. [DOI] [PubMed] [Google Scholar]
- 35.Vanella V., Castagnola R., Marigo L., Grande N.M., Plotino G. A comparison of near-infrared imaging with other diagnostic tools for dental caries. Minerva Dent. Oral Sci. 2021;70:214–222. doi: 10.23736/S2724-6329.21.04527-7. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization . Global Data on Dental Caries Prevalence (DMFT) in Adults Aged 35–44 Years Global Oral Data Bank, Oral Health/Area Profile Programme. World Health Organization; Geneva, Switzerland: 2000. [Google Scholar]
- 37.Corridore D., Zumbo G., Corvino I., Guaragna M., Bossù M., Polimeni A., Vozza I. Prevalence of oral disease and treatment types proposed to children affected by Autistic Spectrum Disorder in Pediatric Dentistry: A Systematic Review. Clin. Ter. 2020;171:e275–e282. doi: 10.7417/CT.2020.2226. [DOI] [PubMed] [Google Scholar]
- 38.Sharma A., Singh S., Mathur A., Aggarwal V.P., Gupta N., Makkar D.K., Batra M., Gijwani D. Route of Drug Abuse and its Impact on Oral Health-Related Quality of Life among Drug Addicts. Addict. Health. 2018;10:148–155. doi: 10.22122/ahj.v10i3.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ekstrand K.R., Gimenez T., Ferreira F.R., Mendes F.M., Braga M.M. The International Caries Detection and Assessment System—ICDAS: A Systematic Review. Caries Res. 2018;52:406–419. doi: 10.1159/000486429. [DOI] [PubMed] [Google Scholar]
- 40.Pitts N.B., Ekstrand K., The ICDAS Foundation International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Community Dent. Oral Epidemiol. 2013;41:e41–e52. doi: 10.1111/cdoe.12025. [DOI] [PubMed] [Google Scholar]
- 41.Abreu-Placeres N., Newton J.T., Pitts N., Garrido L.E., Ekstrand K.R., Avila V., Martignon S. Understanding dentists’ caries management: The COM-B ICCMS™ questionnaire. Community Dent. Oral Epidemiol. 2018;46:545–554. doi: 10.1111/cdoe.12388. [DOI] [PubMed] [Google Scholar]
- 42.Abbass M.M., Abubakr N., Radwan I.A., Rady D., El Moshy S., Ramadan M., Ahmed A., Al Jawaldeh A. The potential impact of age, gender, body mass index, socioeconomic status and dietary habits on the prevalence of dental caries among Egyptian adults: A cross-sectional study. F1000Research. 2019;8:243. doi: 10.12688/f1000research.17892.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Varenne B., Petersen P.E., Ouattara S. Oral health status of children and adults in urban and rural areas of Burkina Faso, Africa. Int. Dent. J. 2004;54:83–89. doi: 10.1111/j.1875-595X.2004.tb00260.x. [DOI] [PubMed] [Google Scholar]
- 44.Kassebaum N.J., Smith A.G.C., Bernabé E., Fleming T.D., Reynolds A.E., Vos T., Murray C.J.L., Marcenes W., GBD 2015 Oral Health Collaborators Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990–2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017;96:380–387. doi: 10.1177/0022034517693566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ward L., Cooper S.A., Hughes-McCormack L., MacPherson L., Kinnear D. Oral health of adults with intellectual disabilities: A systematic review. J. Intellect. Disabil. Res. 2019;63:1359–1378. doi: 10.1111/jir.12632. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.